Abstract
While adoptive transfer of autologous tumor antigen-specific T cell immunotherapy can produce remarkable clinical efficacy, most patients do not achieve durable complete responses. We hypothesized that reducing susceptibility of T cells to activation-induced cell death (AICD), which increases during the rapid in vitro expansion of therapeutic T cells before their infusion, might improve the persistence of adoptively transferred cells. Our investigations revealed that repetitive stimulation of the T cell receptor (TCR) induced AICD, as a result of activating the DNA damage response pathway through ATM-mediated Ser15 phosphorylation of p53. Activation of this DNA damage response pathway also occurred upon antigen-specific restimulation in TCR-transduced TIL1383I T cells prepared for adoptive transfer to patients as part of a clinical trial. Notably, treatment with the antioxidant N-acetyl cysteine (NAC) significantly reduced upregulation of the DNA damage marker γH2AX, subsequent ATM activation and cell death. In the Pmel mouse model of melanoma, the presence of NAC during ex vivo T cell expansion improved the persistence of adoptively transferred cells, reduced tumor growth and increased survival. Taken together, our results offer a preclinical proof of concept for the addition of NAC to current therapeutic T cell expansion protocols, offering immediate potential to improve the quality and therapeutic efficacy of adoptive T cell therapeutics infused into patients.
Keywords: Adoptive T cell therapy, p53, ATM, γH2AX, DNA damage, cell death, antioxidant, N-acetyl cysteine, melanoma
Introduction
Metastatic melanoma continues to increase both in incidence rates and in mortality. Traditional standard-of-care for metastatic, stage IV melanoma has a five-year survival rate of only 15.2%, whereas rates for clinical trials utilizing the adoptive transfer of autologous, melanoma-specific T cells are upwards of 40% (1,2). In the process of adoptive cell therapy (ACT), melanoma-specific T cells are derived either from tumor infiltrating lymphocytes (TIL) cultured from a surgical resection of the tumor or from patient peripheral blood mononuclear cells (PBMCs) engineered with a melanoma specific T cell receptor (TCR). To generate sufficient cells for patient infusion, therapeutic T cells are activated and rapidly expanded prior to reinfusion into a lymphodepleted patient (3).
The disparity between responding and non-responding patients following ACT has been shown to correlate with the persistence of the cells after transfer (4). One of the factors that may contribute to poor persistence is activation induced cell death (AICD). AICD, which is induced upon repetitive stimulation of the TCR, is a necessary mechanism of peripheral tolerance restricting the scope of an immune response towards escalation into a host damaging pathology (5). However, in the context of melanoma immunotherapy, premature deletion of therapeutic T cells through AICD would be detrimental. T cells that have been subjected to the intense polyclonal TCR stimulation during a rapid expansion protocol (REP) are more sensitive to AICD when co-cultured with melanoma tumor cells in vitro (6) whereas younger, less differentiated T cells, which are less susceptible to AICD, are superior at in vivo tumor control (7–9). As strategies that increase resistance to AICD may bolster the durability of therapeutic T cells leading to enhanced anti-tumor efficacy, a more precise understanding of the pathways governing AICD is merited.
In this study, we show that TCR restimulation results in increased expression of the double-strand DNA damage markers γH2AX and p-SMC-1, activation of ATM, as well as phosphorylation and nuclear accumulation of p53. Activation of this signaling cascade was significantly inhibited by the anti-oxidant N-acetyl cysteine (NAC) and ex vivo culture of T cells in NAC improved outcomes in a preclinical animal model.
Materials and Methods
Cells, activation, and culture
Normal healthy donor apheresis cells were purchased from Key Biologics, Inc. or Research Blood Components. Cells from melanoma patients were obtained with consent as part of an IRB and FDA approved clinical trial (NCT01586403). PBMCs were isolated by Ficoll density gradient, activated with plate-bound anti-CD3 (5μg/mL) and anti-CD28 (2μg/mL) for 3 days, washed, and cultured in Iscove's Modified Dulbecco's Medium supplemented with 10% FBS, 100 IU/mL rIL-2 (Peprotech), and 10ng/mL rIL-15 (Shenandoah), for at least 5 days prior to TCR restimulation. Alternatively, patient PBMCs for the clinical trial were activated with 50ng/mL anti-human CD3 antibody (OKT3) for 2-3 days and transduced with either a lenti- or retrovirus by spinoculation on retronectin coated plates. The viral construct expressed TIL1383I TCR and truncated CD34 as a marker of expression (10). Transduced cells were cultured for several days, purified based on CD34 expression (CliniMACs) using CD34+ reagent and placed back in culture for several more days until undergoing a secondary REP (3). For Pmel studies, a single-cell suspension of splenocytes was prepared from Pmel-1 TCR transgenic mice. Cells were cultured in RPMI supplemented with 10% FBS, 100U/mL rIL-2, and stimulated with 1μg/mL of gp10025-33 peptide (AnaSpec) with or without 10mM NAC. Melanoma cell lines (human MEL624 and MEL624-28 and murine B16F10 cells) were obtained in 2013 from Drs. Michael Nishimura (Loyola University, Maywood IL) and Mark Rubinstein (Medical University of South Carolina, Charleston SC). All cells were periodically verified to be free of mycoplasma contamination. Additionally, B16F10 cells were authenticated and confirmed to be free of rodent pathogens by Dr. Rubinstein.
Flow cytometry
For detection of cell death, cells were washed in FACS Buffer (PBS w/ 5% FBS), surface stained for 30 minutes on ice, washed twice in Annexin V binding buffer (10mM HEPES, 140mM NaCl, 2.5mM CaCl2, pH 7.4) and incubated with Annexin V-Cy5 (BioVision) for 15 min prior to acquisition. Cells were surface stained and gated as follows: CD8+ for human PBMC, CD34+CD8+ or CD34+CD4+ for TIL1383I TCR transduced cells, and Vβ13+CD8 + for Pmel cells. For subsequent intracellular staining with phospho-specific fluorochromes, surface stained cells were fixed in 2% pre-warmed (37°C) paraformaldehyde for 20 minutes, washed, and permeabilized with 90% ice-cold methanol for 30 minutes prior to incubation with antibody. Antibodies were p53-PE (BD Pharmingen), p-p53Ser15-AlexaFluor488 (Cell Signal), p-ATMSer1981-PE, γH2AX-PerCP, p-SMC-1-AlexaFluor488 (EMD Millipore), and γH2AX-FITC (BioLegend, for Pmel cells). Intracellular staining of Pmel cells with granzyme B antibody (PE/Cy7 conjugated, eBioscience) was performed using the Transcription Factor Staining Buffer Set (eBioscience) according to vendor protocol. Cells were acquired using the BD LSRFortessa cell analyzer (BD Biosciences) and analyzed using FlowJo software (Tree Star Inc.).
For ImageStream experiments, cells were stained with 250ng/mL Hoechst (Acros Organics) prior to antibody staining. Samples were acquired on the Amnis ImageStream and data was analyzed on IDEAS software (Amnis Corporation) to determine the similarity score between Hoechst and p53 or p-p53Ser15. Events with a similarity score of ≥1 were defined as positive for colocalization.
Adoptive Cell Transfer
All animal experiments were performed with approval by the Institutional Animal Care and Use Committee at the Medical University of South Carolina. Eight week old female C57BL/6 wild-type mice (NCI) were subcutaneously injected with 3×105 B16F10 murine melanoma cells. Tumors were measured using calipers and tumor area (mm2) calculated by multiplying the length and width of two perpendicular measurements. Mice were randomized into treatment groups to ensure equal distribution in tumor size at initiation of the experiment. One day prior to adoptive cell transfer, mice were lymphodepleted through total body irradiation (5Gy, nonmyeloablative). Pmel cells (2×106) cultured in the absence or presence of 10mM NAC were adoptively transferred via retro-orbital injection. To determine persistence of transferred Pmel cells in circulation, blood samples were collected from the tail vein 5 days post transfer. For biodistribution analysis, mice were sacrificed 6 days after adoptive transfer. Spleens and tumors were processed into single cell suspensions by mechanical dissociation. Tumors were further digested in 1mg/mL Collagenase II (Sigma) for 30min and TILs were isolated by density gradient separation with Histopaque 1083 (Sigma).
Statistical methods
Linear longitudinal regression, estimated using generalized estimating equations (GEE) was used to model percent staining over time in data shown in Figures 1a, 1b, and 3a. The fitted model was used to create estimated curves over time and linear combinations of model coefficients were used to compare percent staining at different time periods, with p-values calculated based on Wald tests. Data displayed in Figures 1e and 6 d-f were compared using two-sample t-tests, after taking a log transform to correct for skewness. Data in Figures 2, 4 and 5 were analyzed using the paired t-test. In Figure 3b, linear regression, estimated using GEE to account for repeated measures within donor, was used to evaluate differences. Wald tests were used to make comparisons. Analysis of in vivo data was performed using longitudinal linear regression to model tumor size over time. To compare slopes, the log-likelihoods of nested models (one model assuming different slopes per group and the other model assuming that the two groups being compared have the same slope coefficients) were tested using a likelihood ratio test. The test is based on a chi-square with 2 degrees of freedom. Differences in time of survival were analyzed using a log rank test and displayed using Kaplan-Meier curves.
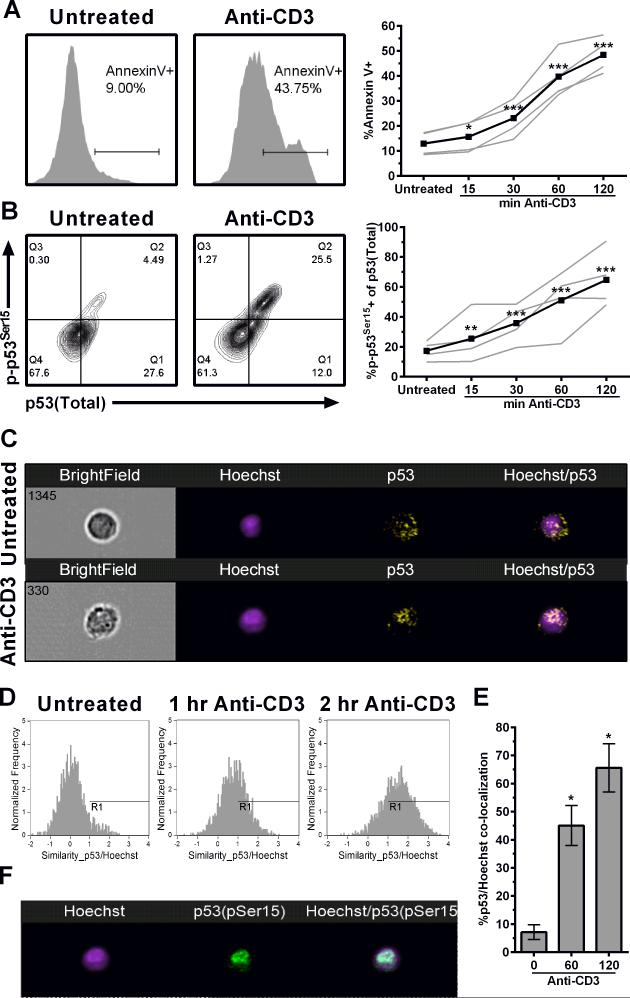
Figure 1. Activation of p53 following TCR restimulation.
(A) Annexin V surface staining and (B) p53 expression among CD8+ T cells following TCR restimulation. Representative contour plots show p53 and p-p53Ser15 120 min after TCR restimulation. Time course experiments are shown in the right panels with each of the four donors (grey lines) and the mean of all donors (black line). (C-F) ImageStream analysis of CD8+ T cells stained with Hoechst, p53, and p-p53Ser15. Representative images show localization of p53 (C) and p-p53Ser15 (F) relative to Hoechst stained nucleus. (D) Representative similarity histogram of cells co-stained with p53 and Hoechst after TCR restimulation. (E) Quantification (mean ± SEM) of co-localization of p53 and Hoechst staining (n=2). *p<0.05, **p<0.01, and ***p<0.0001.
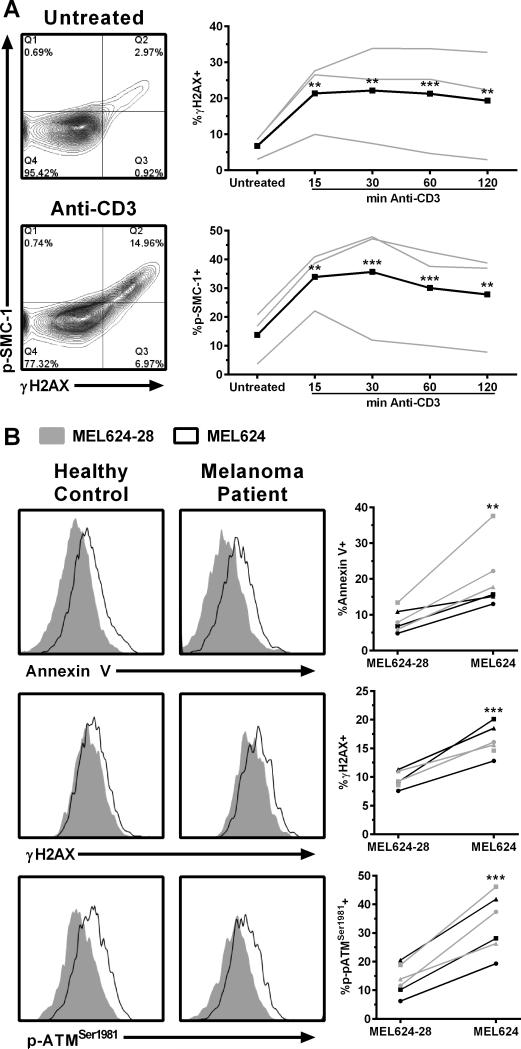
Figure 3. Activation of DNA damage markers in response to anti-CD3 and antigen-specific TCR restimulation.
(A) Analysis of DNA damage markers among CD8+ T cells after TCR restimulation with anti-CD3. Representative contour plots show γH2AX and p-SMC-1 levels 120 min after TCR restimulation. Time course experiments are shown in the right panels with each of the four donors (grey lines) and the mean of all donors (black line). Similar results were obtained in three independent experiments, except for pSMC-1, which was analyzed only twice. (B) Antigen-specific TCR restimulation of CD34+CD8+ T cells from 3 healthy donors (gray lines) or 3 melanoma patients (black lines) after overnight restimulation with MEL624 or MEL624-28 cells. Similar results were obtained in a repeat experiment using the same donors and additional experiments with 4 different donors. **p<0.01, ***p<0.001.
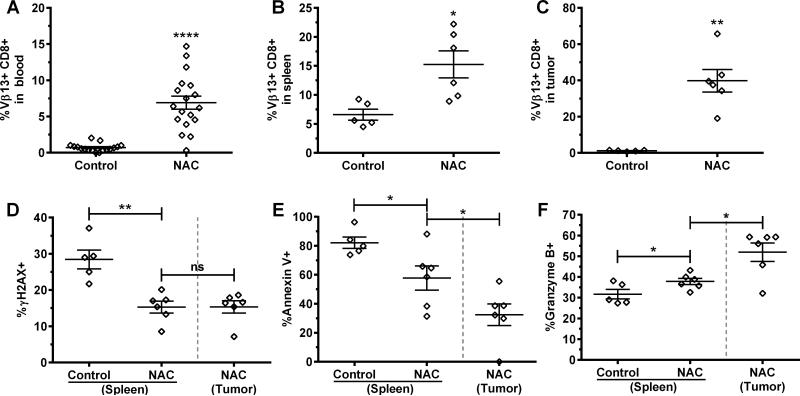
Figure 6. Analysis of Pmel splenocytes after adoptive transfer.
(A) The persistence of Vβ13+CD8+ cells in the blood was assessed 5 days after adoptive transfer. The presence of Vβ13+CD8+ cells in the spleen (B) and tumor (C) was determined on day 6. Vβ13+CD8+ populations were analyzed for DNA damage (D), cell death (E) and granzyme B expression (F). *p<0.05, **p<0.01, ***p<0.001, ****p<0.0001.
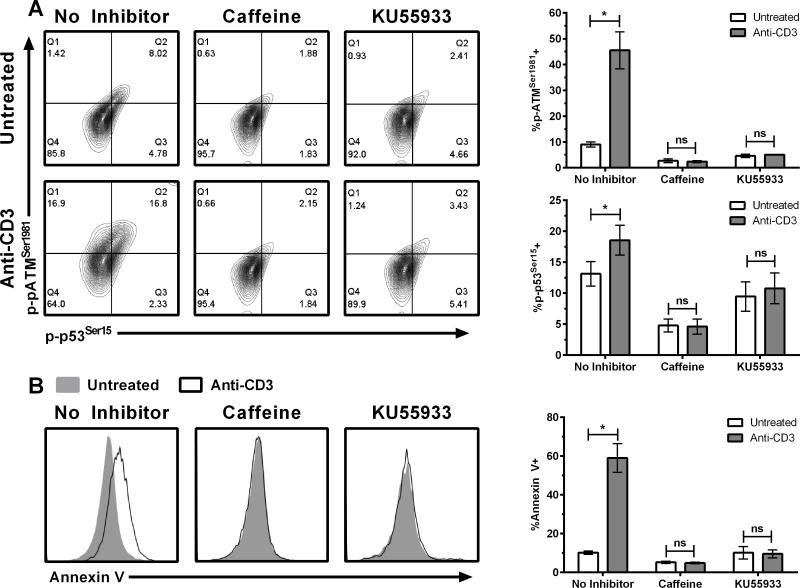
Figure 2. Activation of ATM following TCR restimulation.
(A) Phosphorylation of p53 and ATM and (B) Annexin V staining in CD8+ T cells 120 min after TCR restimulation. Data shown are representative results (left panels) and averages ± SEM from 3 donors (right panels). Caffeine (10mM) or KU-55933 (100uM) was added one hour before restimulation of the TCR with anti-CD3. *p<0.05, ns=not significant.
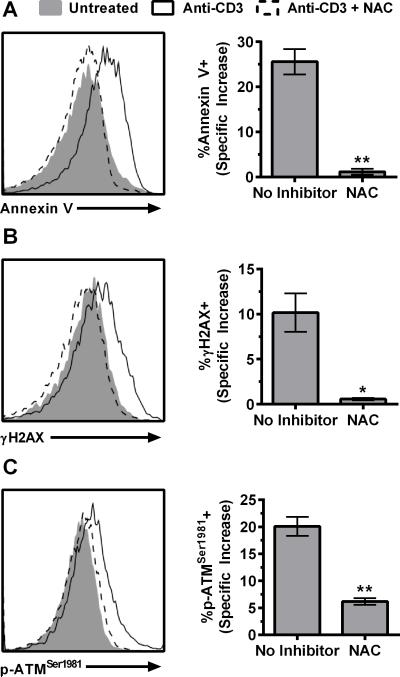
Figure 4. Inhibition of DNA damage response pathway activation by N-acetyl cysteine.
(A) Annexin V, (B) γH2AX, and (C) ATM phosphorylation were assessed in CD8+ T cells 240 min after TCR restimulation following pretreatment with NAC (50mM) for 60min. Background staining was subtracted to show specific increase in response to anti-CD3 treatment between untreated and NAC treated groups. Data shown are from the mean ± SEM from 3 donors. Similar results were obtained in a repeat experiment. *p<0.05, **p<0.01.
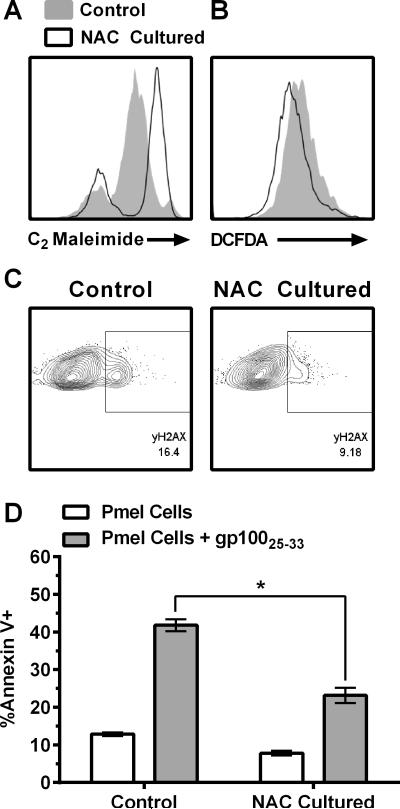
Figure 5. The effect of N-acetyl cysteine on transgenic Pmel splenocytes.
(A) Surface thiol levels and (B) ROS levels from Vβ13+CD8+ Pmel splenocytes cultured in the absence or presence of 10mM NAC. (C) Assessment of DNA damage marker γH2AX expression after TCR restimulation. Similar results were obtained in multiple experiments. (D) Annexin V staining among Vβ13+CD8+ Pmel co-cultured with irradiated splenocyte in the absence (white bars) or presence of TCR restimulation using gp10025-33 peptide (grey bars). Data shown are the average ± SEM from 2 mice. *p<0.05, n=2.
Results
AICD is accompanied by nuclear accumulation of p53 and its rapid phosphorylation on Ser15
Inhibition of p53 can protect T cells from AICD following TCR restimulation (11). p53 plays a crucial role in coordinating the cellular stress response and determines fate through either activating repair or cell death pathways (12). In unstressed cells, p53 levels are repressed through proteasomal degradation via the E3-ubiquitin ligase HDM2. In response to stress, p53 is phosphorylated and the resulting conformational change results in dissociation from HDM2 (13). To evaluate the role of p53 in AICD, the TCR of activated human PBMCs was restimulated with anti-CD3, which results in a time-dependent increase in surface expression of the cell death marker Annexin V (Fig. 1a). Levels of p53, as well as the status of the most commonly phosphorylated residue (Ser15) was evaluated upon TCR restimulation. Restimulation of the TCR stabilized the expression of total p53 (~2.94-fold increase) and increased the percentage of phosphorylation on Ser15 by 3.72-fold within two hours (Fig. 1b). A key role of p53 in cellular stress is its function as a transcription factor with nuclear accumulation serving as a hallmark of p53 activation (14). We observed that the amount of p53 localizing to the Hoechst stained nucleus within 2 hours of TCR restimulation increased approximately 9-fold (Fig. 1c-e). Additionally, nearly all (>97%) of the Ser15-phosphorylated p53 was detected in the nucleus (Fig. 1f). Together, these data demonstrate that induction of AICD following TCR restimulation is accompanied by phosphorylation of p53 on Ser15 and accumulation in the nucleus.
Activation of the serine kinase ATM occurs upstream of p53 phosphorylation and is required for AICD
Phosphorylation of p53 on Ser15 is primarily a function of the PI3K-like serine kinase ataxia telangiectasia mutated (ATM) (15). ATM is activated via recruitment to the DNA damage sensing MRN complex followed by autophosphorylation on Ser1981 and engagement in downstream kinase activity including the phosphorylation of p53 on Ser15 (16). Activation of AICD following TCR restimulation resulted in a 4.6-fold increase in phosphorylated ATM that coincided with phosphorylation of p53 (Fig. 2a). To confirm that ATM was required for p53 phosphorylation, we preincubated cells with the ATM inhibitors caffeine or KU-55933 (17,18). Both inhibitors completely prevented the phosphorylation of ATM and p53 (Fig. 2a), suggesting that ATM activity is necessary for the phosphorylation of p53 on Ser15 following TCR restimulation. Furthermore, ATM inhibition nearly completely (>99%) prevented cell death resulting from TCR restimulation (Fig. 2b). Together these data suggest that ATM activity is responsible for the phosphorylation of p53 and is a novel upstream requisite factor in the onset of AICD.
TCR restimulation results in DNA damage
The upregulation of p-ATMSer1981 and p-p53Ser15 is indicative of a classically defined DNA damage response pathway (19). However, this pathway can be activated in response to oxidative stress or hypoxia in the absence of DNA damage (16). As oxidative stress has already been implicated in the onset of AICD (20), we determined whether evidence of bona fide DNA damage is detected following TCR restimulation by examining the status of γH2AX and p-SMC-1, two well defined markers of double strand DNA breaks (21). Both γH2AX and p-SMC-1 expression increased greater than 3-fold within 15 min of TCR restimulation (Fig. 3a). These data indicate that evidence of DNA damage parallels the onset of ATM activation and suggest that TCR restimulation results in DNA damage and subsequent activation of the DNA damage response pathway leading to AICD.
To determine the clinical relevance of these findings, we obtained T cells that had been prepared for adoptive cell transfer as part of an ongoing clinical trial (NCT01586403). In this trial, patient autologous PBMCs are transduced with the HLA-A2 restricted TIL1383I TCR that recognizes the 368-376 peptide epitope of human tyrosinase, a commonly expressed melanoma associated antigen (10,22). Transduced cells from melanoma patients and healthy donors were restimulated in an antigen-specific manner with HLA-A2+ MEL624 melanoma cells (and HLA-A2− MEL624-28 cells as a negative control). As shown in Figure 3b, antigen-specific restimulation of the TCR by MEL624 cells resulted in significant increases in γH2AX (1.7-fold), p-ATMSer1981 (2.5-fold), and Annexin V staining (2.4-fold) compared to MEL624-28 cells. The increase in these markers did not differ between cells derived from melanoma patients and healthy controls. Similar results were obtained in CD4+ T cells (Supplementary Fig. 1). Taken together, these results suggest that the DNA damage response pathway is also triggered upon both polyclonal and antigen-specific restimulation of the TCR.
The anti-oxidant N-acetyl cysteine reduces the yH2AX-ATM-mediated DNA damage response and AICD following TCR restimulation
AICD is dependent on the generation of reactive oxygen species (ROS) (20,23). To determine whether ROS are the cause of DNA damage following TCR restimulation, we preincubated cells with the anti-oxidant N-acetyl cysteine (NAC, 50mM) prior to TCR restimulation. We confirmed that restimulation of the TCR results in elevation of ROS and that pre-incubation with NAC significantly diminishes this response (Supplementary Fig. 2). Pretreatment with NAC also prevented the increase in Annexin V staining (Fig. 4a) and reduced activation of γH2AX and p-ATM by 94% and 69%, respectively (Fig. 4b&c). These results suggest that ROS generated upon TCR restimulation play a role in activation of the DNA damage response pathway.
Ex vivo expansion in N-acetyl cysteine increases the persistence and function of adoptively transferred T cells improving tumor control and survival in vivo
Kesarwani et al. have shown that ex vivo treatment with NAC improves recovery of T cells harvested from the spleens of non-tumor bearing mice two days post transfer (24). However, the effect of culturing cells in NAC on AICD susceptibility and long-term persistence, particularly within the tumor microenvironment, remains to be determined. Therefore, we evaluated the potential benefit of NAC in the Pmel transgenic model (25). To determine whether the protective effect of NAC in human T cells extended to mouse T cells, we performed an initial in vitro characterization of the Pmel cells. Pmel splenocytes expanded in 10mM NAC exhibited enhanced anti-oxidant capacity denoted by an increase in surface thiols (Fig. 5a) and decreased expression of the oxidative stress marker DCFDA (Fig. 5b). Furthermore, antigen-specific TCR restimulation using gp10025-33 peptide diminished upregulation of γH2AX (Fig. 5c) and significantly protected cells from AICD (Fig. 5d), suggesting that the NAC protective effect from activation of the DNA damage response pathway following TCR restimulation also occurs in the Pmel model.
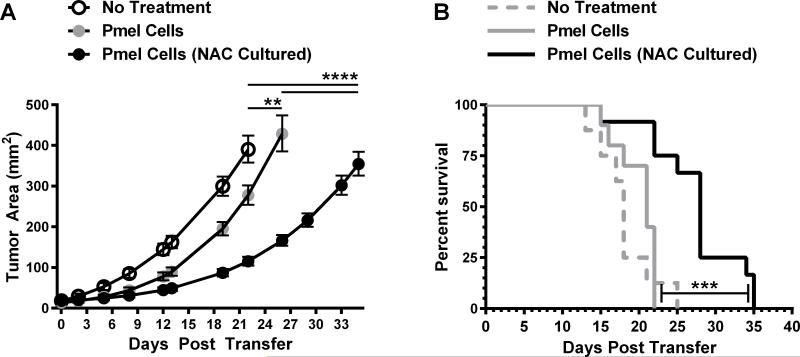
Next, Pmel cells cultured in the absence or presence of NAC were adoptively transferred into C57BL/6J mice challenged with B16F10 murine melanoma cells. Culturing Pmel cells in NAC significantly increased the persistence of Vβ13+CD8+ cells in the blood and spleens of recipient mice (Fig. 6a&b). Strikingly, in mice receiving Pmel cells cultured in NAC, close to 40% of T cells within the tumor were Vβ13+CD8+ positive, whereas effector T cells from Pmel cells cultured in the absence of NAC were scarcely detectable (~1.2%, Fig. 6c).
We also analyzed cells isolated from spleens and tumors for susceptibility to DNA damage and cell death. Because insufficient Vβ13+CD8+ cells were recovered from tumors of mice that received control cells, we compared Pmel cells isolated from tumors of mice receiving NAC treated cells to the corresponding splenocytes. Among Pmel T effector cells that trafficked to the spleen, about 30% had detectable γH2AX (Fig. 6d). Expanding Pmel cells in the presence of NAC prior to adoptive cell transfer reduced the γH2AX positive population by half regardless of whether cells trafficked to the spleen or the tumor (Fig. 6d). Restimulation of cells isolated from spleen or tumor with gp10025-33 peptide shows that a majority of Pmel T effector cells become Annexin V positive and that ex vivo culture in NAC resulted in a significant decrease in Annexin V expression among cells that had trafficked to the spleen or the tumor (Fig. 6e). In addition, we found that granzyme B expression inversely correlated with Annexin V staining and that the strongest expression was observed on Vβ13+CD8+ NAC expanded cells that had trafficked to the tumor (Fig. 6f).
To determine whether the effects of culturing Pmel cells in the presence of NAC prior to adoptive transfer extended to anti-tumor activity, we adoptively transferred Pmel cells expanded in the absence or presence of NAC into B16F10 challenged mice. As expected, Pmel cells are capable of significantly delaying tumor growth compared to mice receiving no cells (Fig. 7a, p=0.0025), although under the conditions we used, this did not translate into a significant survival benefit (Fig. 7b). In contrast, transfer of Pmel cells that had been cultured in NAC resulted in highly significant delays in tumor growth compared to mice receiving no cells (p<0.0001) and to mice receiving Pmel cells cultured in the absence of NAC (p<0.0001). Expansion of cells in NAC also significantly increased median survival time compared to mice receiving no cells (p=0.0004) or those receiving Pmel cells (Fig. 7b, p=0.0002). Together these results suggest that expanding therapeutic T cells in the presence of NAC prior to adoptive transfer, can result in a long lasting benefits following transfer that enhance persistence, tumor control, and survival.
Figure 7. The impact of ex vivo culture in N-acetyl cysteine on tumor growth and survival.
(A) Tumor growth and (B) survival was determined for up to 35 days after adoptive transfer in untreated mice (n=8), Pmel treated mice (n=10), and mice receiving NAC treated PMEL cells (n=12). **p<0.01, ***p<0.001, ****p<0.0001.
Discussion
Adoptive transfer of melanoma specific T cells has generated curative responses upwards of 40% in patients receiving this experimental therapy, with persistence being the predominant correlative of therapeutic success (1,4). The required REP used to generate sufficient T cells for infusion increases susceptibility to AICD and may constrain the persistence of the adoptively transferred cells (6). The possibility that increasing AICD resistance among therapeutic T cells may improve their anti-tumor cytotoxic functionality led us to elucidate the mechanisms and pathways responsible for AICD to identify possible points of intervention.
The pharmacological inhibition of p53 can protect activated T cells from death following TCR restimulation (11), and we have recently demonstrated that T cells from p53-knockout mice are likewise protected from AICD (26). However, the activation status of p53 has not previously been investigated. Our data show that repetitive stimulation of the TCR results in stabilization and phosphorylation of p53 on its N-terminal Ser15 residue (Fig. 1). Phosphorylation of p53 on Ser15 prevents nuclear export, leading to nuclear accumulation and enhanced p53 nuclear transcriptional activity (27), which is consistent with the increase in total p53 and nuclear localization of phosphorylated p53 in our study (Fig. 1). p53 is most notably regarded as the “guardian of the genome” as it reliably initiates programmed cell death in cells that have been compromised by DNA damage or other irreparable cellular stressors. Consequently, nearly 50% of all cancers have either eliminated or functionally inactivated p53, and T cells from p53-knockout mice eventually deviate into lymphomas (28,29). However, emerging evidence suggests that in the immune system, p53 plays a more nuanced role in homeostasis than just maintaining genomic integrity. For example, Watanabe et al. demonstrated that p53 expression is critical to prevent non-specific proliferation of T cells in response to IL-2 (30). p53 also reduces autoimmunity by influencing the differentiation of T cells through repression of STAT3 mediated differentiation of Th17 cells in favor of promoting T regulatory cells (31). Conversely, loss of p53 expression or function exaggerates autoimmunity and co-associates with many autoimmune conditions where defective AICD is also problematic, including arthritis (32–36), multiple sclerosis, (37,38), and Crohn's disease (39,40). Our data suggest that activation of p53 plays a critical role in T cell death and offers a potential explanation for the co-association between p53 and autoimmune disorders. However, given that p53 plays pleiotropic roles in immune regulation and lack of expression is associated with cancer development, it is unlikely that targeting p53 is a suitable strategy to improve function of adoptively transferred cells.
While p53 can be activated by a variety of cellular stressors, it is chiefly a responder to DNA damage. Indeed, our data support a rapid incursion of DNA damage evidenced by the phosphorylation and activation of two DSB repair proteins, H2AX and SMC-1, within 15min of TCR restimulation (Fig. 3). The serine kinase ataxia telangiectasia mutated (ATM) acts as the primary liaison between a DNA damage insult and the activation of p53. ATM derives its name from being the “mutated” kinase responsible for the onset of the neurodegenerative disorder ataxia telangiectasia (A-T). As ATM is functionally inactivated in A-T patients, T cells from these patients are resistant to phosphorylation of p53 on Ser15 and fail to undergo cell death in response to DNA damaging insults (41,42). Similar to functional inactivation of ATM in A-T patients, we found that inhibition of ATM by both caffeine and the pharmacological inhibitor KU-55933 prevented phosphorylation of p53 on Ser15 and protected T cells from death upon TCR restimulation (Fig. 2). These results suggest that ATM-mediated phosphorylation of p53 on Ser15 may play a novel role as a requisite factor in the onset AICD.
Reactive oxygen species (ROS) are generated within 15 minutes of TCR crosslinking (23) and have recently been shown to play a key signaling roles within mitochondria for antigen-specific expansion of T cells (43). However, oxidative stress is also the primary endogenous assailant of DNA damage (44). The accumulation of DNA damage coupled with a diminished capacity for DNA double-strand break repair is a problem associated with aging immune cells that correlates with a decline in immune function and increased senescence (45,46). As T cells proliferate in vitro they accumulate DNA damage and downregulate the DNA repair machinery (47,48). T cells with short telomeres, indicative of a longer replicative history, have higher baseline levels of γH2AX, a delayed DNA repair response, and are also more susceptible to cell death (49,50). Erosion of telomeres correlates with poor persistence and patient responses in clinical trials (51). Taken together, these studies suggest the possibility that increased DNA damage and decreased ability for DNA repair can preferentially lead to elimination of the adoptively transferred cells through AICD. Indeed studies affirm that younger, less differentiated T cells are superior at in vivo tumor control (7,8).
The amount of DNA damage in lymphocytes negatively correlates with the level of intracellular glutathione (52), prompting us to hypothesize that treatment with the glutathione pro-drug N-acetyl cysteine (NAC) may be beneficial. Studies have shown that NAC can increase the proliferative potential and cytokine production of T cells and even restores the functional capacity of PBMCs from advanced stage cancer patients (24,53–55). Indeed, pretreatment of human T cells with NAC decreased γH2AX expression, activation of ATM, and cell death in response to TCR restimulation (Fig. 4). Moreover, adding NAC to the culture medium of Pmel cells bolstered their surface thiol levels, reduced oxidative stress, and as in human T cells, diminished γH2AX levels and susceptibility to cell death (Figs. 5 and 6). Whether NAC prevents the formation of DNA damage or rather enhances p53-mediated DNA repair remains to be determined.
Importantly, ex vivo culture in NAC resulted in long term benefits as adoptively transferred cells appeared to retain resistance to DNA damage and AICD even 6 days after adoptive transfer with no additional NAC supplementation (Fig. 6c&d). The benefits of ex vivo expansion in NAC, translated into increased persistence in the blood, spleen, and tumors of B16F10 challenged mice (Fig. 6a-c). Consistent with the persistence of transferred cells being a key corollary of therapeutic success in the clinic (4), these more durable NAC cultured cells enhanced tumor control and survival of recipient mice (Fig. 7), which supports our premise that protecting T cells from AICD may enhance their therapeutic efficacy. Ex vivo expanded T cells used for adoptive immunotherapy generally acquire an effector memory phenotype (TEM cells) with limited persistence and reduced anti-tumor efficacy compared to central memory phenotype cells (TCM). Kesarwani et al. showed that TCM cells have an increased expression of redox regulators (24) and we determined that TCM cells (CD8+CCR7hi) were more resistant to upregulation of γH2AX following TCR restimulation. However expansion of T cells in the presence of NAC did not increase the proportion of TCM cells, suggesting that increased persistence is likely not due to alterations in memory cell populations (Scheffel MJ et al., manuscript in preparation). A striking observation was that Pmel cells expanded in NAC were found at 33-fold higher levels within the tumor microenvironment (Fig. 6). Whether this accumulation within the tumor is simply due to AICD resistance or whether NAC also has beneficial effects on T cell trafficking will need to be investigated. The impact of NAC on T cell phenotype is currently under further investigation.
ROS are required for signaling in T cell activation but also contribute to cell death susceptibility, indicating a delicate balance is crucial to ensure optimal T cell function. Previously, we have shown that both the c-jun kinase (JNK) inhibitor SP600125 and the ROS scavenger MnTBAP protected cells from AICD and that inhibition of JNK, but not ROS generation, interfered with T cell function (20). Consistent with these findings, altering the anti-oxidative potential of the cells through ex vivo culture in NAC did not appear to impair the cytotoxic function of T cells as NAC cultured cells expressed significantly higher levels of granzyme B (Fig. 6f), which may have contributed to improved tumor control and survival (Fig. 7).
In summary, this study shows that repetitive stimulation of the TCR results in activation of the DNA damage response pathway as evidenced by an increase in two DNA damage response markers (H2AX, SMC-1) and subsequent activation of ATM and p53. Our study suggests an additional layer of regulation whereby an individual T cell would be more or less susceptible to AICD through its ability to repair or succumb to DNA damage induced by TCR restimulation. Importantly, evidence of DNA damage pathway activation was observed in response to antigen-specific restimulation of TIL1383I transduced T cells that are currently being used in a clinical trial (Fig. 3b). This suggests the possibility that adoptively transferred cells may undergo AICD upon encountering tumor antigen that may contribute to poor persistence. As culturing cells in NAC both quelled susceptibility to DNA damage as suggested by significantly reduced expression of γH2AX after adoptive transfer (Fig. 6d) and enhanced tumor control in the Pmel mouse model (Fig. 7), we postulate that expanding therapeutic cells in NAC, which has a long and safe history in clinical use, could be an expeditious improvement to current protocols.
Supplementary Material
Acknowledgements
We thank Dr. Michelle Nelson for technical guidance with the Pmel model and Dr. Chrystal Paulos for many beneficial discussions pertaining to this project.
Funding
All authors received funding from National Institutes of Health Grant P01CA154778. The Cell Evaluation & Therapy Shared Resource of the Hollings Cancer Center, Medical University of South Carolina was in part supported by P30 CA138313. This work was conducted in a facility constructed with support from the National Institutes of Health, Grant Number C06 RR015455 from the Extramural Research Facilities Program of the National Center for Research Resources.
Footnotes
Conflict of Interest
none
References
- 1.Rosenberg S. Raising the bar: the curative potential of human cancer immunotherapy. Sci Transl Med. 2012;4:127ps8. doi: 10.1126/scitranslmed.3003634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Siegel R, Desantis C, Virgo K, Stein K, Mariotto A, Smith T, et al. Cancer treatment and survivorship statistics, 2012. CA Cancer J Clin. 2012;62:220–41. doi: 10.3322/caac.21149. [DOI] [PubMed] [Google Scholar]
- 3.Riddell S, Greenberg P. The use of anti-CD3 and anti-CD28 monoclonal antibodies to clone and expand human antigen-specific T cells. J Immunol Methods. 1990;128:189–201. doi: 10.1016/0022-1759(90)90210-m. [DOI] [PubMed] [Google Scholar]
- 4.Robbins PF, Dudley ME, Wunderlich J, El-Gamil M, Li YF, Zhou J, et al. Cutting edge: persistence of transferred lymphocyte clonotypes correlates with cancer regression in patients receiving cell transfer therapy. J Immunol. 2004;173:7125–30. doi: 10.4049/jimmunol.173.12.7125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Snow AL, Pandiyan P, Zheng L, Krummey SM, Lenardo MJ. The power and the promise of restimulation-induced cell death in human immune diseases. Immunol Rev. 2010;236:68–82. doi: 10.1111/j.1600-065X.2010.00917.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hernandez-Chacon JA, Li Y, Wu RC, Bernatchez C, Wang Y, Weber JS, et al. Costimulation through the CD137/4-1BB pathway protects human melanoma tumor-infiltrating lymphocytes from activation-induced cell death and enhances antitumor effector function. J Immunother. 2011;34:236–50. doi: 10.1097/CJI.0b013e318209e7ec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tran KQ, Zhou J, Durflinger KH, Langhan MM, Shelton TE, Wunderlich JR, et al. Minimally cultured tumor-infiltrating lymphocytes display optimal characteristics for adoptive cell therapy. J Immunother. 2008;31:742–51. doi: 10.1097/CJI.0b013e31818403d5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gattinoni L, Klebanoff CA, Palmer DC, Wrzesinski C, Kerstann K, Yu Z, et al. Acquisition of full effector function in vitro paradoxically impairs the in vivo antitumor efficacy of adoptively transferred CD8+ T cells. J Clin Invest. 2005;115:1616–26. doi: 10.1172/JCI24480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hombach AA, Abken H. Young T cells age during a redirected anti-tumor attack: Chimeric antigen receptor-provided dual costimulation is half the battle. Front Immunol. 2013;4:5–8. doi: 10.3389/fimmu.2013.00135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Norell H, Zhang Y, McCracken J, Martins da Palma T, Lesher A, Liu Y, et al. CD34-based enrichment of genetically engineered human T cells for clinical use results in dramatically enhanced tumor targeting. Cancer Immunol Immunother. 2010;59:851–62. doi: 10.1007/s00262-009-0810-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chhabra A, Mukherji B. Death receptor-independent activation-induced cell death in human melanoma antigen-specific MHC class I-restricted TCR-engineered CD4 T cells. J Immunol. 2013;191:3471–7. doi: 10.4049/jimmunol.1202350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Murray-Zmijewski F, Slee E, Lu X. A complex barcode underlies the heterogeneous response of p53 to stress. Nat Rev Mol Cell Biol. 2008;9:702–12. doi: 10.1038/nrm2451. [DOI] [PubMed] [Google Scholar]
- 13.Kruse J-P, Gu W. Modes of p53 regulation. Cell. 2009;137:609–22. doi: 10.1016/j.cell.2009.04.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shaulsky G, Goldfinger N, Tosky MS, Levine AJ, Rotter V. Nuclear localization is essential for the activity of p53 protein. Oncogene. 1991;6:2055–65. [PubMed] [Google Scholar]
- 15.Cheng Q, Chen J. Mechanism of p53 stabilization by ATM after DNA damage. Cell cycle. 2010;9:472–8. doi: 10.4161/cc.9.3.10556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Paull TT. Mechanisms of ATM Activation. Annu Rev Biochem. 2015;84:711–38. doi: 10.1146/annurev-biochem-060614-034335. [DOI] [PubMed] [Google Scholar]
- 17.Blasina A, Price BD, Turenne GA, Mcgowan CH. Caffeine inhibits the checkpoint kinase ATM. Curr Biol. 1999;9:1135–8. doi: 10.1016/s0960-9822(99)80486-2. [DOI] [PubMed] [Google Scholar]
- 18.Hickson I, Zhao Y, Richardson C. Identification and characterization of a novel and specific inhibitor of the ataxia-telangiectasia mutated kinase ATM. Cancer Res. 2004;64:9152–9. doi: 10.1158/0008-5472.CAN-04-2727. [DOI] [PubMed] [Google Scholar]
- 19.Banin S, Moyal L, Shieh S-Y, Taya Y, Anderson CW, Chessa L, et al. Enhanced phosphorylation of p53 by ATM in response to DNA damage. Science. 1998;281:1674–7. doi: 10.1126/science.281.5383.1674. [DOI] [PubMed] [Google Scholar]
- 20.Norell H, Martins da Palma T, Lesher A, Kaur N, Mehrotra M, Naga OS, et al. Inhibition of superoxide generation upon T-cell receptor engagement rescues Mart-1(27-35)-reactive T cells from activation-induced cell death. Cancer Res. 2009;69:6282–9. doi: 10.1158/0008-5472.CAN-09-1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Branzei D, Foiani M. Regulation of DNA repair throughout the cell cycle. Nat Rev Mol Cell Biol. 2008;9:297–308. doi: 10.1038/nrm2351. [DOI] [PubMed] [Google Scholar]
- 22.Nishimura MI, Avichezer D, Custer MC, Lee CS, Chen C, Parkhurst MR, et al. MHC Class I-restricted recognition of a melanoma antigen by a human CD4+ tumor infiltrating lymphocyte. Cancer Res. 1999;59:6230–8. [PubMed] [Google Scholar]
- 23.Devadas S, Zaritskaya L, Rhee SG, Oberley L, Williams MS. Discrete generation of superoxide and hydrogen peroxide by T cell receptor stimulation: selective regulation of mitogen-activated protein kinase activation and fas ligand expression. J Exp Med. 2002;195:59–70. doi: 10.1084/jem.20010659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kesarwani P, Al-Khami AA, Scurti G, Thyagarajan K, Kaur N, Husain S, et al. Promoting thiol expression increases the durability of antitumor T-cell functions. Cancer Res. 2014;74:6036–47. doi: 10.1158/0008-5472.CAN-14-1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Overwijk WW, Theoret MR, Finkelstein SE, Surman DR, De Jong LA, Vyth-Dreese FA, et al. Tumor regression and autoimmunity after reversal of a functionally tolerant state of self-reactive CD8+ T cells. J Exp Med. 2003;198:569–80. doi: 10.1084/jem.20030590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Banerjee A, Thyagarajan K, Chatterjee S, Chakraborty P, Kesarwani P, Soloshchenko M, et al. Lack of p53 Augments Anti-Tumor Functions In Cytolytic T Cells. Cancer Res. 2016 Jul 27; doi: 10.1158/0008-5472.CAN-15-1798. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang Y, Xiong Y. A p53 amino-terminal nuclear export signal inhibited by DNA damage-induced phosphorylation. Science. 2001;292:1910–5. doi: 10.1126/science.1058637. [DOI] [PubMed] [Google Scholar]
- 28.Efeyan A, Serrano M. p53: Guardian of the genome and policeman of the oncogenes. Cell Cycle. 2007;6:1006–10. doi: 10.4161/cc.6.9.4211. [DOI] [PubMed] [Google Scholar]
- 29.Dudgeon C, Chan C, Kang W, Sun Y, Emerson R, Robins H, et al. The evolution of thymic lymphomas in p53 knockout mice. Genes Dev. 2014;28:2613–20. doi: 10.1101/gad.252148.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Watanabe M, Moon KD, Vacchio MS, Hathcock KS, Hodes RJ. Downmodulation of tumor suppressor p53 by T cell receptor signaling is critical for antigen-specific CD4+ T cell responses. Immunity. 2014;40:681–91. doi: 10.1016/j.immuni.2014.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Park JS, Lim MA, Cho M La, Ryu JG, Moon YM, Jhun JY, et al. p53 controls autoimmune arthritis via STAT-mediated regulation of the Th17 cell/Treg cell balance in mice. Arthritis Rheum. 2013;65:949–59. doi: 10.1002/art.37841. [DOI] [PubMed] [Google Scholar]
- 32.Boldizsar F, Kis-Toth K, Tarjanyi O, Olasz K, Hegyi A, Mikecz K, et al. Impaired activation-induced cell death promotes spontaneous arthritis in antigen (cartilage proteoglycan)-specific T cell receptor-transgenic mice. Arthritis Rheum. 2010;62:2984–94. doi: 10.1002/art.27614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yamanishi Y, Boyle DL, Pinkoski MJ, Mahboubi A, Lin T, Han Z, et al. Regulation of joint destruction and inflammation by p53 in collagen-induced arthritis. Am J Pathol. American Society for Investigative Pathology. 2002;160:123–30. doi: 10.1016/S0002-9440(10)64356-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Han Z, Boyle DL, Shi Y, Green DR, Firestein GS. Dominant-negative p53 mutations in rheumatoid arthritis. Arthritis Rheum. 1999;42:1088–92. doi: 10.1002/1529-0131(199906)42:6<1088::AID-ANR4>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 35.Maas K, Westfall M, Pietenpol J, Olsen NJ, Aune T. Reduced p53 in peripheral blood mononuclear cells from patients with rheumatoid arthritis is associated with loss of radiation-induced apoptosis. Arthritis Rheum. 2005;52:1047–57. doi: 10.1002/art.20931. [DOI] [PubMed] [Google Scholar]
- 36.Salmon M, Scheel-Toellner D, Huissoon AP, Pilling D, Shamsadeen N, Hyde H, et al. Inhibition of T cell apoptosis in the rheumatoid synovium. J Clin Invest. 1997;99:439–46. doi: 10.1172/JCI119178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Okuda Y, Okuda M, Bernard CC. Regulatory role of p53 in experimental autoimmune encephalomyelitis. J Neuroimmunol. 2003;135:29–37. doi: 10.1016/s0165-5728(02)00428-9. [DOI] [PubMed] [Google Scholar]
- 38.Moreno M, Negrotto L, Río J, Moubarak R, Martín I, Bustamante MF, et al. Activation-induced cell death in T lymphocytes from multiple sclerosis patients. J Neuroimmunol. 2014;272:51–5. doi: 10.1016/j.jneuroim.2014.04.007. [DOI] [PubMed] [Google Scholar]
- 39.Sturm A, Leite AZA, Danese S, Krivacic KA, West GA, Mohr S, et al. Divergent cell cycle kinetics underlie the distinct functional capacity of mucosal T cells in Crohn's disease and ulcerative colitis. Gut. 2004;53:1624–31. doi: 10.1136/gut.2003.033613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Van Den Brande JMH, Peppelenbosch MP, Van Deventer SJH. Treating Crohn's disease by inducing T lymphocyte apoptosis. Ann N Y Acad Sci. 2002;973:166–80. doi: 10.1111/j.1749-6632.2002.tb04628.x. [DOI] [PubMed] [Google Scholar]
- 41.Canman CE, Lim DS, Cimprich KA, Taya Y, Tamai K, Sakaguchi K, et al. Activation of the ATM kinase by ionizing radiation and phosphorylation of p53. Science. 1998;281:1677–9. doi: 10.1126/science.281.5383.1677. [DOI] [PubMed] [Google Scholar]
- 42.Porcedda P, Turinetto V, Lantelme E, Fontanella E, Chrzanowska K, Ragona R, et al. Impaired elimination of DNA double-strand break-containing lymphocytes in ataxia telangiectasia and Nijmegen breakage syndrome. DNA Repair (Amst) 2006;5:904–13. doi: 10.1016/j.dnarep.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 43.Sena LA, Li S, Jairaman A, Prakriya M, Ezponda T, Hildeman DA, et al. Mitochondria are required for antigen-specific T cell activation through reactive oxygen species signaling. Immunity. 2013;38:225–36. doi: 10.1016/j.immuni.2012.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Marnett LJ. Oxyradicals and DNA damage. Carcinogenesis. 2000;21:361–70. doi: 10.1093/carcin/21.3.361. [DOI] [PubMed] [Google Scholar]
- 45.Mayer PJ, Lange CS, Bradley MO, Nichols WW. Age-dependent decline in rejoining of X-ray-induced DNA double-strand breaks in normal human lymphocytes. Mutat Res. 1989;219:95–100. doi: 10.1016/0921-8734(89)90019-2. [DOI] [PubMed] [Google Scholar]
- 46.Barnett YA, Barnett CR. DNA damage and mutation: Contributors to the age-related alterations in T cell-mediated immune responses? Mech Ageing Dev. 1998;102:165–75. doi: 10.1016/s0047-6374(98)00018-9. [DOI] [PubMed] [Google Scholar]
- 47.Hyland P, Barnett C, Pawelec G, Barnett Y. Age-related accumulation of oxidative DNA damage and alterations in levels of in human CD4 + T cell clones in vitro. Mech Ageing Dev. 2001;122:1151–67. doi: 10.1016/s0047-6374(01)00254-8. [DOI] [PubMed] [Google Scholar]
- 48.Neri S, Pawelec G, Facchini A, Mariani E. Microsatellite instability and compromised mismatch repair gene expression during in vitro passaging of monoclonal human T lymphocytes. Rejuvenation Res. 2007;10:145–56. doi: 10.1089/rej.2006.0510. [DOI] [PubMed] [Google Scholar]
- 49.Hao LY, Strong MA, Greider CW. Phosphorylation of H2AX at short telomeres in T cells and fibroblasts. J Biol Chem. 2004;279:45148–54. doi: 10.1074/jbc.M403924200. [DOI] [PubMed] [Google Scholar]
- 50.Drissi R, Wu J, Hu Y, Bockhold C, Dome JS. Telomere shortening alters the kinetics of the DNA damage response after ionizing radiation in human cells. Cancer Prev Res. 2011;4:1973–81. doi: 10.1158/1940-6207.CAPR-11-0069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Shen X, Zhou J, Hathcock KS, Robbins P, Powell DJ, Rosenberg SA, et al. Persistence of tumor infiltrating lymphocytes in adoptive immunotherapy correlates with telomere length. J Immunother. 2007;30:123–9. doi: 10.1097/01.cji.0000211321.07654.b8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lenton KJ, Therriault H, Fülöp T, Payette H, Wagner JR. Glutathione and ascorbate are negatively correlated with oxidative DNA damage in human lymphocytes. Carcinogenesis. 1999;20:607–13. doi: 10.1093/carcin/20.4.607. [DOI] [PubMed] [Google Scholar]
- 53.Kalamasz D, Long S, Taniguchi R, Buckner JH, Berenson RJ, Bonyhadi M. Optimization of human T-cell expansion ex vivo using magnetic beads conjugated with anti-CD3 and anti-CD28 antibodies. J Immunother. 2004;27:405–18. doi: 10.1097/00002371-200409000-00010. [DOI] [PubMed] [Google Scholar]
- 54.Eylar E, Rivera-Quinones C, Molina C, Báez I, Molina F, Mercado CM. N-acetylcysteine enhances T cell functions and T cell growth in culture. Int Immunol. 1993;5:97–101. doi: 10.1093/intimm/5.1.97. [DOI] [PubMed] [Google Scholar]
- 55.Mantovani G, Macciò A, Melis G, Mura L, Massa E, Mudu M. Restoration of functional defects in peripheral blood mononuclear cells isolated from cancer patients by thiol antioxidants alpha-lipoic acid and N-acetyl cysteine. Int J cancer. 2000;86:842–7. doi: 10.1002/(sici)1097-0215(20000615)86:6<842::aid-ijc13>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.