Abstract
Background:
The use of non-sterile gloves (NSG) has become routine in the delivery of health care, often for procedures for which they are not required; their use may increase the risk of cross contamination and is generally not integrated into hand hygiene audit. This paper describes a small-scale application and validation of an observational audit tool devised to identify inappropriate use of NSG and potential for cross contamination.
Methods:
Two observers simultaneously observed the use of NSG during episodes of care in an acute hospital setting. The inter-rater reliability (IRR) of the audit tool was measured corrected for chance agreement using Kappa.
Results:
A total of 22 episodes of care using NSG were observed. In 68.6% (24/35) of procedures there was no contact with blood/body fluid; in 54.3% (19/35) NSG-use was inappropriate. The IRR was 100% for eight of 12 components of the tool. For hand hygiene before and after NSG removal it was 82% (Kappa = 0.72) and 95% (Kappa = 0.87).
Conclusions:
In this small-scale application of a glove-use audit tool we demonstrated over-use and misuse of NSG and potential for cross transmission on gloved hands. The audit tool provides an effective mechanism for integrating glove use into the audit of hand hygiene behaviour.
Keywords: Behaviour, hand hygiene, infection control, standard precautions
Background
The hands of staff are recognised to play a major role in the transmission of infection in healthcare settings (World Health Organization (WHO), 2009a). Hand hygiene is now accepted as an essential component of infection control programmes, and education on hand hygiene is commonly based on the promotion of the ‘5 moments of hand hygiene’ (5MHH) (Sax et al, 2007; World Health Organization, 2009a). The routine use of non-sterile gloves (NSG) in clinical care emerged in the late 1980s when the Centers for Disease Control (CDC) recommended ‘universal precautions’ in response to the emerging AIDS epidemic (CDC, 1987). These precautions required the use of protective clothing for direct contact with blood and some body fluids from any patient on the basis that it was not possible to identify those who were carrying bloodborne viruses (CDC, 1988). Subsequently the recommendations were extended to all body fluids to address the increased risks of contamination associated with such contact and became known as standard precautions (Lynch et al, 1987; Wilson & Breedon, 1990; Pratt et al, 2007). Thus, standard precautions indicate that personal protective equipment (PPE) should be used for any procedure where a risk of direct contact with blood and body fluids (BBF) is anticipated (RCN, 2012; Loveday et al, 2014a). The type of PPE selected should be dictated by the extent of potential exposure to BBF and as most contact involves hands, NSG are the most commonly used form of PPE. However, adequate hand hygiene after glove use and the need to change NSG between procedures on the same patient and between patients, is essential to minimise the risk of infection transmission (World Health Organization, 2009a; Loveday et al, 2014a). If NSG are worn during the delivery of care, but not removed at the points in care where hand hygiene is indicated by the 5MHH, then their use will increase rather than decrease the risk of transmission of infection between patients. Although most studies focus on hand hygiene rather than glove-use behaviour, a few have indicated an emerging problem with an overuse of NSG. These have identified NSG being worn for procedures that do not involve exposure to BBF and that have not been removed in a timely way (Thompson et al, 1997; Prieto and Macleod Clark, 2005; Chau et al, 2011). Other studies have suggested that the use of NSG may have an adverse effect on compliance with the 5MHH (Fuller et al, 2011; Flores and Pevalin, 2006).
A mechanism of feeding back of data on the misuse of NSG is required in order to educate clinical staff about using gloves appropriately and recognising the importance of hand hygiene in the context of their use. Most hospitals in the UK measure compliance with 5MHH using simple audit tools but these do not account for the use of NSG in the delivery of care and are not able to capture data on the specific risks of cross contamination associated with their use. In a previous study we tested an observational audit tool to identify inappropriate NSG use and potential for cross contamination associated with them (Loveday et al, 2014b). We found NSG use was inappropriate in 42% (69 of 163) of episodes and a risk of cross contamination in 37% (60 of 163) because an indication for hand hygiene was missed. In this study we describe the development and application of this audit tool and report on the inter-rater reliability associated with its use.
Method
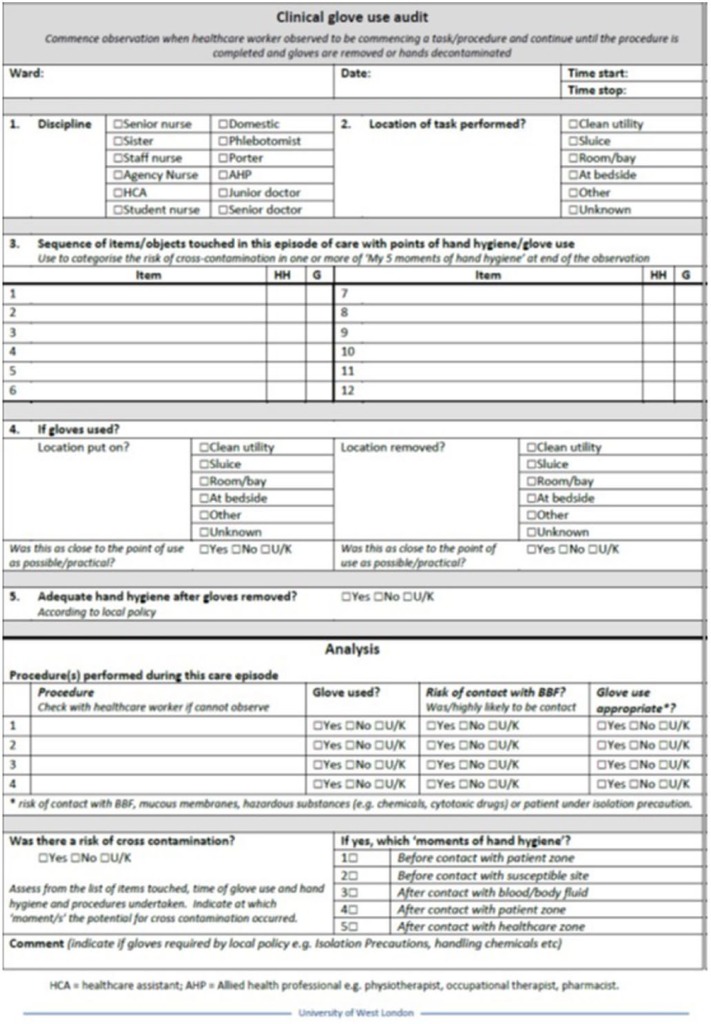
The audit tool has been designed to capture the detail of clinical procedures performed while wearing NSG. It captures data on:
items that were touched during their use
the point when NSG were put on and removed
when hands were washed.
This approach enables glove-use behaviour to be analysed and the risk of cross contamination associated with NSG to be measured. The audit tool has been developed from the original version (Loveday et al, 2014b) in order to record the points during an episode of care where NSG are put on or removed and hands decontaminated (Figure 1). This approach enables the extent of misuse of NSG to be estimated by measuring the proportion of procedures in which gloves are used. The audit episode commences when the healthcare worker (HCW) is observed to be preparing to undertake an episode of care and ends when the HCW completes the episode. Each item touched with the hands during the procedure/s, the order that they are touched and the point at which hand hygiene occurs or gloves are put on/taken off is recorded. On completion of the observation, the information is used to categorise the potential for cross contamination during each episode observed using the criteria shown in Table 1. These criteria have been adapted from the 5MHH for use in the context of the gloved hand with a ‘moment of HH’. They translate to the requirement to remove or change gloves and/or decontaminate hands. Lack of hand hygiene before putting on NSG was not considered as a risk of cross contamination (Rock et al, 2013). Hand hygiene after NSG removal was considered adequate if performed according to the hospital protocol. Appropriateness of NSG use was also assessed for each procedure. It was considered appropriate if the procedure was in the high-risk category of the Fulkerson scale, which lists 15 typical clinical activities ranked according to their risk of hand contamination. High risk activities are those involving contact with body excretions/secretions, mucous membranes or infected patient sites (Larson and Lusk 2006; McLaws et al, 2009). NSG were also considered appropriate for contact with hazardous substances or if required by local policy (e.g. patient under isolation precautions).
Figure 1.
The glove-use audit tool.
Table 1.
Classification of the risk of cross contamination to incorporate the use of gloves (adapted from ‘My 5 moments for hand hygiene’ Sax et al, 2007; WHO, 2009a,b).
| Moment for hand decontamination | Risk of cross contamination | Definition |
|---|---|---|
| 1 Before touching a patient/patient zone | A patient is touched by a contaminated glove/hand | Gloves/hands contaminated if they had contact with any part of the environment outside the patient’s zone before direct contact with the patient’s intact skin. If the HCW touches their own clothing, skin or hair this is not considered part of the ‘patient zone’ |
| 2 Before a clean/aseptic procedure | A contaminated glove/hand touched a susceptible site, e.g. wound, IV access site, phlebotomy | Gloves/hands contaminated if they had touched any other non-sterile objects or patient sites before the aseptic task e.g. patient skin, bed linen. |
| 3 After body fluid exposure risk | A glove/hand touched a surface or patient after contact with blood and body fluids | Gloves/hands contaminated if used for handling urine or assisting a patient on the toilet then touched other surfaces or patients. |
| 4 After touching a patient/patient zone | Gloves used for contact within patient zone not removed or hand hygiene not performed before contact with an object outside patient zone | Gloves/hands contaminated if touched another patient/objects outside patient zone; hand hygiene not performed after glove removal; or one glove/outer glove (where double-gloves used) removed part way through procedure. |
| 5 After touching patients surroundings/healthcare zone | Failure to remove gloves and/or perform hand hygiene after contact with patient surroundings | Gloves not removed or adequate hand hygiene not performed on leaving the healthcare zone. |
We tested the tool in three wards in a large, acute teaching hospital. The Hawthorne effect is the term used to describe the tendency for people’s behaviour to be different when they are being observed in the context of research. It is called the Hawthorne effect because it was first noted in a research study on the effect of changes in working conditions on workers, which was conducted in in a factory of that name (Holden, 2001). In this study the Hawthorne effect was minimised by making the purpose of the observation obscure. In general staff will assume the observation is related to hand hygiene rather than the use of NSG and they are therefore less likely to change their glove-use behaviour during the observation. In addition, auditors would be present on the ward for at least 10 minutes prior to collecting data so that staff become more familiar with their presence and are more likely to exhibit their normal behaviour. Positioning of the auditor is important to ensure that observations can be carried out unobtrusively, however, often clinical tasks or procedures require the patient to be given privacy and care may be delivered behind curtains. Where possible, observers would deduce procedures being undertaken by the equipment being used and confirm by questioning the healthcare worker or patient. Ethical approval was not required for this study as the observations constituted audit of practice and were a normal part of infection control activity.
To estimate the validity of the audit tool, paired observations were captured simultaneously by two observers. The inter-rater reliability (IRR) for each of 11 items documented in the tool was assessed using percentage agreement between observers and corrected for chance using Cohen’s kappa coefficient in Excel (Hripcsak and Heitjan, 2002). Kappa values of 0.41 to 0.6 are considered to demonstrate moderate agreement, 0.61 to 0.8 good and 0.81 or more very good agreement (Viera and Garrett, 2005).
Results
Twenty-two episodes of care were observed in a medical ward (nine), high dependency unit (six) and neurosurgical ward (seven), all of which involved the use of NSG. These were performed by staff nurses (nine episodes), healthcare assistants (nine episodes), student nurses (two episodes) and allied health professionals/phlebotomists (two episodes). There were 35 procedures performed during these episodes, of which 34 were performed using NSG. The number of procedures where there was contact with blood or body fluid and where the use of NSG was deemed appropriate is shown in Table 2.
Table 2.
Appropriateness of glove use for 34 procedures undertaken during episodes of care.
| No | Yes | Unknown | Total | ||||
|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | ||
| Contact with blood and body fluids | 23 | 67.6% | 7 | 20.1% | 4 | 11.4% | 34 (100%) |
| Glove use appropriate | 18 | 52.9% | 15 | 44.1% | 1 | 2.9% | 34 (100%) |
NSG were put on in the bay or outside the patient’s room in 17 or the 22 episodes (77%). A total of 54 items were observed to be touched using NSG. On one of the 22 episodes (5%) a risk of cross contamination was observed after Moment 4. In a further six of the 22 episodes (27%) the curtains surrounding the patient’s bed were touched before contact with the patient and, since this is deemed to be outside the patient zone, it contravened Moment 1.
The validation of the observational audit found high IRR in the paired observations for eight of 12 variables documented in the tool, including the appropriateness of NSG use and risk of cross contamination (see Table 3). In the five discrepant observations related to hand hygiene before or after NSG removal, with four related to hand hygiene being documented as ‘unknown’ rather than ‘yes’ or ‘no’. In two of the 22 episodes there was a minor difference in documentation of the exact point where NSG were removed (IRR 91%; Kappa 0.48); although this Kappa coefficient is likely to be underestimated because of the small sample size and disagreement with this variable was rare (Viera and Garrett, 2005) (Table 3). In addition, there was one minor variation in the description of the procedure being performed (Hygiene needs vs. tidying bed/bedspace) and nine differences noted in specific items touched out of a total of 54 documented items touched (IRR 83%) (Table 4).
Table 3.
Inter-observer agreement for variables in glove-use audit tool.
a) Variables related to 22 episodes of care
| Item | Description | No. (%) agreement |
|---|---|---|
| 1 | Discipline of staff | 22 (100%) |
| 2 | Location gloves put on | 22 (100%) |
| 3 | Location task performed | 22 (100%) |
| 4 | Gloving location appropriate | 22 (100%) |
| 5 | Location gloves removed | 22 (100%) |
Table 4.
Discrepancy in items observed to be touched during procedure.
| Observer 1 | Observer 2 | |
|---|---|---|
| 1 | Call button | Not recorded |
| 2 | Not recorded | Slide sheet |
| 3 | Shower chair | Commode |
| 4 | Not recorded | Toothbrush |
| 5 | Needle & syringe | Not recorded |
| 6 | Not recorded | Table |
| 7 | Not recorded | Sink |
| 8 | Not recorded | Patient property bag |
| 9 | Crockery | Zimmer frame |
b) Variables related to glove removal and hand hygiene pre- and post-gloving during 22 episodes of care
| Item | Description | No. in agreement |
Total no. (%) agreement | Kappa | ||
|---|---|---|---|---|---|---|
| Yes | No | UK | ||||
| 6 | Hand hygiene pre-gloving | 6 | 9 | 3 | 18 (82%) | 0.72 |
| 7 | Hand hygiene after removal | 17 | 0 | 4 | 21 (95%) | 0.87 |
| 8 | Point of glove removal | 20 | 2 | – | 20 (91%) | 0.48 |
c) Variables related to 35 procedures observed during 22 episodes of care
| Item | Description | No. (%) agreement |
|---|---|---|
| 9 | Procedure performed | 35* (100%) |
| 10 | Risk of contact with blood and body fluids | 35 (100%) |
| 11 | Glove use appropriate | 35 (100%) |
| 12 | Risk of cross contamination | 35 (100%) |
minor variation in description for one procedure.
Discussion
Our validation study demonstrated a high level of agreement between observers in documenting the use of NSG using this audit tool, with an inter-observer agreement of 100% for the majority of variables, including appropriateness of use and risk of cross contamination, and Kappa scores of more than 0.7. In this small set of observations we found that half of the procedures where NSG were worn their use was not appropriate since there was no risk of contact with BBF or other indication for their use. In 27% of episodes of care we also found evidence that NSG use was associated with a risk of cross contamination, between the environment and patients or between patients. NSG were put on at a point distant to the patient and therefore contaminated outside the patient zone prior to patient contact. The actual risk of cross infection associated with misuse of NSG has been demonstrated by Girou et al (2004) who sampled NSG after use and recovered pathogens from 86%, even after the application of alcohol hand rub. Snyder et al (2008) also found that NSG become readily contaminated with antibiotic-resistant pathogens as a result of contact with patients or their environment. The widespread use of NSG was observed by Fuller et al (2011), who found that 26% of hand hygiene opportunities involved their use. Other studies have found poor compliance with timely removal of NSG in healthcare episodes involving more than one procedure on the same patient, particularly in the context of patient isolation for infection (Johnson et al, 1990; Patterson et al, 1991; Prieto and Macleod Clark, 2005).
In Loveday et al (2014b) we found that the decision of healthcare workers to use NSG appeared to be influenced by feelings of disgust and misjudgement about the risk to self, and that NSG-use behaviour was often influenced by co-workers. Although we cannot be sure about the origin of these sentiments, they may have emerged from the widespread publicity about risk of HCAI, strong promotion of hand hygiene as fundamental to preventing infection, and from the promotion of personal protective clothing as part of standard precautions.
Although promotion of the 5MHH framework and the use of alcohol hand gel has become the standard approach to education and training on hand hygiene in healthcare settings (WHO, 2009b), the use of NSG does not fit easily with these principles. Guidance on use of 5MHH suggests that indications for hand hygiene are independent of those that justify the use of NSG and glove use should not replace or alter the performance of hand hygiene. However, when 5MHH was conceived it was assumed that NSG would be used as ‘a second skin to prevent exposure of hand to body fluids’ and that ‘glove removal represents a strong cue to hand hygiene’ (Sax et al, 2007). Unfortunately, our observations suggest that the use of NSG has now been extended to a wide range of clinical activities that do not involve exposure to body fluids and their use compromises the principles of the 5MHH because they are frequently donned outside the patient zone and, in the absence of exposure to body fluid, the trigger to remove them and perform hand hygiene may be lost. For example, we observed that it was common practice to put on gloves in the bay where the NSG dispenser was situated or outside the patient’s room rather than at the bedside. As a result curtains and other equipment outside the patient zone were touched by the gloved hand before contact with the patient. Similarly, donning gloves in the bay precluded the application of alcohol hand gel immediately prior to contact with the patient. Therefore, in using gloves to reduce the risk of infection, HCWs may actually increase the risk of transmission between the environment and patient and between patients through lack of their timely application and removal. It is possible that this was a factor in the contamination of curtains implicated in a recent outbreak of Group A streptococcus (Mahida et al, 2014).
The audit tool also highlights other inconsistencies with 5MHH that are difficult to reconcile, for example a commode moves from outside to inside the patient zone and then returns outside after use, which makes it difficult to categorise the relevant moments of hand hygiene and/or NSG removal. In addition, the surfaces within the patient zone are considered to be continuous with the patient as they are likely to become readily contaminated with their micro-organisms. However, the true microbiological risks associated with this approach are unknown.
There are few examples in the literature of studies evaluating inter-observer agreement of hand hygiene behaviour. McAteer et al (2008) used a simplified audit tool based on the assignment of hand hygiene opportunities to six groups (before and after low risk contact, before and after high risk contact and before and after unobserved contact). They found a kappa for hand hygiene opportunities and hand hygiene actions of 0.68 and 0.77 respectively, but commented that use of the tool required clear standard operating procedures and between four and six hours of training. In most healthcare settings monitoring of compliance with hand hygiene is based on the WHO hand hygiene observation method, although the recommendations to train and validate observers to ensure consistency is probably not commonly performed (Sax et al, 2009). There is little data on the IRR of this method (Steed et al, 2011; Huis et al, 2013).
We suggest that the standard approach to hand hygiene audit needs to be developed to address inappropriate use of NSG and to more accurately reflect non-compliance with 5MHH in situations where gloves are being used. We have shown that our audit tool can be used to provide consistent data about the misuse of NSG and their potential impact on infection control. Infection prevention teams can use this to challenge the over-use of NSG and increase the knowledge and understanding of healthcare workers about the hazards associated with their misuse. The study does have limitations, in particular it represents a small scale assessment of IRR and a larger sample size would be required to provide more robust estimates. In addition, the evaluation was conducted in one hospital and the reliability may vary among other researchers. The method of documenting each item touched and subsequently interpreting the data to identify the risk of cross contamination requires some expertise and careful training of the auditors is required to ensure consistency of results. The findings related to the misuse of NSG may be subject to the Hawthorne effect although this would suggest that true practice involves even more inappropriate use and risk of cross contamination (Holden, 2001).
In conclusion, systematic audit of NSG use indicates the lack of integration between NSG use and 5MHH and a significant potential for cross transmission on gloved hands. Further work is required to determine how widespread this practice is among clinical staff, to understand the drivers of this behaviour and to develop effective interventions to improve appropriate use of NSG.
Footnotes
Declaration of conflicting interest: The authors declare that there is no conflict of interest.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Peer review statement: Not commissioned; blind peer-reviewed.
References
- Centers for Disease Control (1987) Recommendations for prevention of HIV transmission in health-care settings. MMWR 36 (suppl no. 2S). [PubMed] [Google Scholar]
- Centers for Disease Control (1988) Update: universal precautions for prevention of transmission of human immunodeficiency virus, hepatitis B virus and other bloodborne pathogens in healthcare settings. MMWR 37: 377–88. [PubMed] [Google Scholar]
- Chau JP, Thompson DR, Twinn S, Lee DT, Pang SW. (2011) An evaluation of hospital hand hygiene practice and glove use in Hong Kong. Journal of Clinical Nursing 20: 1319–1328. [DOI] [PubMed] [Google Scholar]
- Flores A, Pevalin DJ. (2006) Healthcare workers’ compliance with glove use and the effect of glove use on hand hygiene compliance. British Journal of Infection Control 7: 15–19. [Google Scholar]
- Fuller C, Savage J, Besser S, et al. (2011). “The dirty hand in the latex glove”: A study of hand hygiene compliance when gloves are worn. Infection Control and Hospital Epidemiology 32: 1194–1199. [DOI] [PubMed] [Google Scholar]
- Girou E, Chai SHT, Oppein F, Legrand P, Ducellier D, Cizeau F, Brun-Buisson B. (2004). Misuse of gloves: the foundation for poor compliance with hand hygiene and potential for microbial transmission? Journal Hospital Infection 57: 162–169. [DOI] [PubMed] [Google Scholar]
- Holden JD. (2001) Hawthorne effects and research into professional practice. Journal of Evaluation in Clinical Practice 7: 65–70. [DOI] [PubMed] [Google Scholar]
- Hripcsak G, Heitjan DF. (2002) Measuring agreement in medical informatics reliability studies. Journal of Biomed Informatics 35: 99–110. [DOI] [PubMed] [Google Scholar]
- Huis A, Schoonhoven L, Grol R, et al. (2013) Impact of a team and leaders-directed strategy to improve nurses’ adherence to hand hygiene guidelines: a cluster randomised trial. International Journl of Nursing Studies 50: 464–474. [DOI] [PubMed] [Google Scholar]
- Johnson S, Gerding DN, Olson MM, et al. (1990) Prospective, controlled study of vinyl glove use to interrupt Clostridium difficile nosocomial transmission. American Journal of Medicine 88: 137–140. [DOI] [PubMed] [Google Scholar]
- Larson E, Lusk E. (2006) Evaluating handwashing technique. Journal of Advanced Nursing 53(1): 46–53 [DOI] [PubMed] [Google Scholar]
- Loveday HP, Wilson JA, Pratt RP, et al. (2014a). epic3: National evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. Journal of Hospital Infection 86S1: S1–S70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loveday HP, Lynam S, Singleton J, Wilson J. (2014b). Clinical glove use: healthcare workers actions and perceptions. Journal of Hospital Infection 86: 110–116. [DOI] [PubMed] [Google Scholar]
- Lynch P, Jackson M, Cummings MJ, Stamm WE. (1987). Rethinking the role of isolation practices in the prevention of nosocomial infections. Annals of Internal Medicine 107: 243–246. [DOI] [PubMed] [Google Scholar]
- Mahida N, Beal A, Trigg D, Vaughan N, Boswell T. (2014) Outbreak of invasive group A Streptococcus infection: contaminated patient curtains and cross-infection on an ear, nose and throat ward. Journal of Hospital Infection 87: 141–144. [DOI] [PubMed] [Google Scholar]
- McAteer J, Stone S, Fuller C, Charlett A, Cookson B, Slade R, Michie S. (2008) Development of an observational measure of healthcare worker hand-hygiene behavior: the hand-hygiene observation tool (HHOT). Journal of Hospital Infection 48: 222–229. [DOI] [PubMed] [Google Scholar]
- McLaws M-L, Pantle AC, Fitzpatrick KR, Hughes CF. (2009). Improvements in hand hygiene across New South Wales public hospitals: clean hands save lives, Part III. Medical Journal of Australia 191: S18–25. [DOI] [PubMed] [Google Scholar]
- Patterson JE, Vecchio J, Pantelick E, et al. (1991). Association of contaminated gloves with transmission of Acinetobacter calcoaceticus var. anitratus in an intensive care unit. American Journal of Medicine 91: 479–483. [DOI] [PubMed] [Google Scholar]
- Pratt RJ, Pellowe CM, Wilson JA, et al. (2007). epic2: National evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. Journal of Hospital Infection 65S: 1–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prieto J, Macleod Clark J. (2005) Contact precautions for Clostridium difficile and Methicillin-resistant Staphylococcus aureus (MRSA): assessing the impact of a supportive intervention to improve practice. Journal of Research in Nursing 10(5): 511–526. [Google Scholar]
- Rock C, Harris AD, Reich NG, et al. (2013). Is hand hygiene before putting on nonsterile gloves in the intensive care unit a waste of healthcare worker time? – a randomised controlled trial. American Jouornal of Infection Control 41: 994–996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Royal College of Nursing (2012) Tools of the Trade: RCN Guidance for Healthcare Staff on Glove Use and the Prevention of Contact Dermatitis. Royal College of Nursing: London. [Google Scholar]
- Sax H, Allegranzi B, Uckay L, Larson E, Boyce J, Pittet D. (2007) “My five moments for hand hygiene”: a user-centred design approach to understand, train, monitor and report hand hygiene. Journal of Hospital Infection 67: 9–21. [DOI] [PubMed] [Google Scholar]
- Sax H, Allegranzi B, Chraiti M-N, Boyce J, Larson E, Pittet D. (2009) The World Health Organisation hand hygiene method. American Journal of Infection Control 37: 827–834. [DOI] [PubMed] [Google Scholar]
- Snyder GM, Thom KA, Furono JP, et al. (2008) Detection of methicillin-resistant Staphylococcus aureus and vancomycin-resistant enterococci on the gowns and gloves of healthcare workers. Infection Control and Hospital Epidemiology 29: 583–589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steed C, Kelly JW, Blackhurst D, Boeker S, Diller T, Alper P, Larson E. (2011) Hospital hand hygiene opportunities: where and when(HOW2)? The HOW2 benchmark study. American Journal of Infection Control 39: 19–26. [DOI] [PubMed] [Google Scholar]
- Thompson BL, Dwyer DM, Ussery XT, Denman S, Vacek P, Schwartz B. (1997) Handwashing and glove use in a long-term-care facility. Infection Control and Hospital Epidemiology 19: 97–103. [DOI] [PubMed] [Google Scholar]
- Viera AJ, Garrett JM. (2005) Understanding interobserver agreement: the kappa statistic. Family Medicine 35: 360–363. [PubMed] [Google Scholar]
- Wilson J, Breedon P. (1990) Universal precautions. Nursing Times 86(37): 67–70. [PubMed] [Google Scholar]
- World Health Organization (2009a) WHO Patient Safety. WHO Guidelines on Hand Hygiene in Health care. World Health Organization: Geneva. [Google Scholar]
- World Health Organization (2009b) Hand Hygiene Technical Reference Manual. World Health Organization: Geneva. [Google Scholar]