Abstract
Aims:
To evaluate the effectiveness of the International Nosocomial Infection Control Consortium (INICC) Multidimensional Hand Hygiene Approach in Turkey and analyse predictors of poor hand hygiene compliance.
Design:
An observational, prospective, interventional, before-and-after study was conducted from August 2003 to August 2011 in 12 intensive care units (ICU) of 12 hospitals in 11 cities. The study was divided into a baseline and a follow-up period and included random 30-minute observations for hand hygiene compliance in ICU. The hand hygiene approach included administrative support, supplies availability, education and training, reminders in the workplace, process surveillance, and performance feedback.
Results:
We observed 21,145 opportunities for hand hygiene. Overall hand hygiene compliance increased from 28.8% to 91% (95% CI 87.6–93.0, p 0.0001). Multivariate and univariate analyses showed that several variables were significantly associated with poor hand hygiene compliance: males vs. females (39% vs. 48%; 95% CI 0.79–0.84, p 0.0001), ancillary staff vs. physicians (35% vs. 46%, 95% CI 0.73–0.78, p 0.0001), and adult vs. pediatric ICUs (42% vs. 74%, 95% CI 0.54–0.60, p 0.0001).
Conclusions:
Adherence to hand hygiene was significantly increased with the INICC Hand Hygiene Approach. Specific programmes should be directed to improve hand hygiene in variables found to be predictors of poor hand hygiene compliance.
Keywords: Developing countries, hand hygiene, infection control, intensive care unit, International Nosocomial Infection Control Consortium, multidimensional approach
Introduction
The effectiveness of hand hygiene before patient contact to prevent cross infection was demonstrated back in the 19th century, when Semmelweis assessed the relation between reduced mortality from puerperal sepsis and improved hand antisepsis (Raju, 1999). Since then it has been reported in the scientific literature that improved hand hygiene practice reduces healthcare associated infection (HCAI) rates and antimicrobial resistance (Simmons et al., 1990; Rosenthal et al., 2005; Pittet et al., 2009).
HAIs pose a threat to patient safety, causing patient mortality and morbidity (Jarvis, 1996). Most studies of HCAIs have been from developed countries (Safdar et al., 2001), while in developing countries this public health problem had not been systematically studied until the International Nosocomial Infection Control Consortium (INICC) began to measure and analyse HCAI rates with standardised definitions and methods (Rosenthal et al., 2006, 2008a,b, 2010a, 2012b).
Successful interventions to improve hand hygiene have been reported from high-income countries (Lam et al., 2004) and limited-resource countries (Rosenthal et al., 2003, 2005, 2013; Allegranzi et al., 2010). In 2005, the World Health Organization (WHO) launched the programme ‘Clean Care is Safer Care’ to promote hand hygiene worldwide, and in 2009, it published guidelines including a combination of previously published data and a new formulation for alcohol hand rub products, among several other recommendations (Pittet et al., 2009).
There are no previous publications showing hand hygiene compliance in the hospitals of Turkey. The purpose of this INICC study was to establish the baseline hand hygiene compliance rate by healthcare workers (HCWs) before patient contact in 12 ICUs in 12 hospitals in 11 cities of Turkey. Additionally, this study analyses risk factors for poor adherence, and evaluates the impact of implementing an INICC Multidimensional Hand hygiene Approach (IMHHA). This which includes the following elements: (1) Administrative support, (2) Availability of supplies, (3) Education and training, (4) Reminders in the workplace (5) Process surveillance, and (6) Performance feedback.
Methods
Background on INICC
The INICC is an international, non-profit, open, multi-centric HCAI surveillance network with a methodology based on the United States’ Centers for Disease Control/National Healthcare Safety Network (NHSN) (Horan et al., 2008). INICC is the first research network established to measure and control HCAIs in hospitals worldwide through the analysis of standardised data collected on a voluntary basis by its member hospitals. Gaining new members since its international inception in 2002, INICC now comprises nearly 1,000 hospitals in 200 cities of 50 countries in Latin America, Asia, Africa, Middle East, and Europe, and has become the only source of aggregate standardised international data on the epidemiology of HCAI internationally (Rosenthal et al., 2012b).
Study setting
This study was conducted in 12 ICUs of 12 INICC member academic hospitals from 11 cities in Turkey, which were successively incorporated into the study over a period of eight years.
Each hospital has an infection control team (ICT) with at least one infection control practitioner (ICP) and one physician, but this number of members is variable depending on the ICU. The ICT member in charge of process surveillance at each hospital has at least two years of experience in monitoring of HCAI rates and infection control practices.
Professional categories of HCWs included nurses, physicians, and ancillary staff (including paramedical technicians, nurse aides, laboratory team members, radiology team members, physiotherapists, patient care technicians, paramedical personnel and patient lift teams).
The study protocol was approved by the Institutional Review Boards at each hospital.
Study design
An observational, prospective, cohort, interventional, before-and-after multi-centric study was conducted from August 2003 through to August 2011. The study was divided into two periods: baseline and follow-up. Baseline period for hand hygiene compliance included episodes documented at each hospital during their first three months of participation, and the follow-up period included episodes after the fourth month of participation. Each ICU started to participate in the study at different times, and therefore had different lengths of follow-up. For all ICUs the length of the baseline period is exactly the same (three months), and their average follow-up period was 20.4 months (range 6–72). For compliance rate comparison, the ICUs were aligned independently of the date at which they started to participate in the study.
INICC Multidimensional Hand Hygiene Approach (IMHHA)
The IMHHA is implemented at each hospital from the beginning of their participation in INICC. The approach includes the following six components that are applied simultaneously: 1. Administrative support; 2. Availability of supplies; 3. Education and training; 4. Reminders in the workplace; 5. Process surveillance; and 6. Performance feedback. Although the components are presented individually, they are interactive elements that must concur for the effective implementation of any ‘multidimensional’ approach.
1. Administrative support
Hospital administrators of the participating hospitals agreed and committed to the study, attended infection control meetings to discuss study findings, and allocated supplies of hand hygiene products.
2. Availability of supplies
During the study period, alcohol hand rub bottles were available at the ICU entrances, at nursing stations and near the site of patient care (individual patient room entrances, at bedside tables and/or on the feet of patient beds). Sinks with water supply, soap and paper towels were available at the ICU entrances, nursing stations, and common areas of ICUs.
3. Education and training
At the study’s ICUs, the ICT members provided 30-minute education sessions to HCWs in each work shift, at the beginning of the study period and at regular times periodically (every month, every two months, and every six months, depending on the ICU) during the follow-up period. Education included information about indications of hand hygiene, and the correct procedures and technique for hand hygiene.
4. Reminders in the workplace
Posters and reminders were displayed all around the hospital settings (i.e. hospital entrance, corridors, ICT office, ICU entrances, nursing stations, beside each sink, and beside each alcohol hand rub bottle). They included simple instructions on hand hygiene performance, in line with the contents of the education and training program.
5. Process surveillance
Process surveillance of hand hygiene practices consisted of the registrations of potential opportunities for hand hygiene, (Pittet et al., 2009) and the actual number of hand hygiene episodes, either with water and soap or alcohol hand rub. HCWs’ hand hygiene practice was directly monitored by an observer, a member of the ICT, who received training sessions by means of a manual for reporting (Rosenthal et al., 2008a; Pittet et al., 2009). To improve data inter-reliability, observers used standardised monitoring processes, following a standardised protocol and completing hand hygiene surveillance forms that contained a standardised questionnaire to monitor hand hygiene practices (Rosenthal et al., 2008a). Observations were conducted unobtrusively (that is, without interference from the observer) at specific time periods selected at random, distributed over three times a week, for one hour each time and during all work shifts (morning, afternoon and evening). HCWs were not aware of the schedule of the monitoring period. The monitoring included hand hygiene compliance before patient contact, and before an aseptic task. Because we started the study in August 2003 the ‘Five Moments for Hand Hygiene’ proposed by the WHO was not published until 2009. Potential confounders of hand hygiene included type of ICU, professional category, sex, work shift, and type of contact.
6. Performance feedback
Every month, the INICC Headquarters team prepares and sends to each participating ICU a final month-by-month report on compliance with hand hygiene. These charts contain a running tally of hand hygiene compliance by HCWs of the ICUs, and compliance comparing several variables, such as sex, HCW professional status, ICU type, contact type, and work shift. These charts were reviewed at monthly ICT meetings and also posted in the ICUs to give performance feedback to the HCWs of the participating ICUs (Rosenthal et al., 2008a) The performance feedback process started in the third month of participation in this approach. (Rosenthal et al., 2008a).
Training of the infection control team for process surveillance
The ICT member investigators were self-trained with a procedure manual sent from the INICC Headquarters in Buenos Aires, specifying how to carry out the hand hygiene process surveillance and how to fill in the INICC forms (Rosenthal et al., 2008a). ICT members had continuous telephone, email and webinar access to a support team at the INICC Headquarters.
Data collection and processing
Completed INICC process surveillance forms of hand hygiene were sent monthly by ICT members from each participating ICU to the INICC Headquarters. The team at the INICC Headquarters uploaded the data into a database, analysed and sent to ICT members of each participating ICU a report of hand hygiene compliance, showing hand hygiene compliance by month, by sex, by HCW profession, by ICU, by work shift, and by type of contact. (Rosenthal et al., 2008a).
Statistical methods
Univariate analysis of variables associated with poor hand hygiene, and of impact of hand hygiene approach
The aggregated independent variables (sex of HCWs, profession of HCWs, type of ICU, type of contact, etc.) of all observed hand hygiene opportunities and hand hygiene compliance during the entire study, and comparison of hand hygiene compliance during the baseline period and during the follow-up period were compared using Fisher’s exact test for dichotomous variables and unmatched Student’s t-test for continuous variables. Relative risk (RR) ratios were calculated for comparisons of analysed variables associated with hand hygiene using EPI Info V6. 95% confidence intervals (CI) were calculated using VCStat (Castiglia, Argentina). p-values <0.05 by two-tailed tests were considered significant.
Multivariate analysis of variables associated with poor hand hygiene
The aggregated described independent variables of all observed hand hygiene opportunities and hand hygiene compliance during all of the study were compared using logistic regression for dichotomous and continuous variables. Odds ratios (OR) with 95% CI were calculated for comparisons of analysed variables associated with hand hygiene using PASW Statistics 18. p-values <0.05 by two-tailed tests were considered significant.
Multivariate analysis of impact of INICC hand hygiene multidimensional approach
Hand hygiene opportunities and hand hygiene compliance during baseline and during follow-up were explored for changes in hand hygiene compliance rates following an ICU joining INICC. We looked at the follow-up period stratified by a nine-month period over the first year, and yearly for the second year through to the seventh year. We present the results of a logistic regression model to consider change in hand hygiene compliance in INICC participating ICUs over time since the beginning of the hand hygiene surveillance. Odds ratios are presented, comparing each time period since the start of the surveillance with the average baseline of three months. This is a large dataset, with 21,667 observations and so we were able to adjust for the effect of each ICU on hand hygiene compliance as a categorical variable in the analysis. Because of the different length of follow-up of each ICU (from nine months to seven years), for each time period only ICUs with follow-up in that time period were included in the baseline period used for calculating the OR of hand hygiene compliance for that period.
Results
From August 2003 to August 2011 (eight years), we recorded a total of 21,667 opportunities for hand hygiene before patient contact, and before aseptic tasks.
The characteristics of the hospitals and ICUs participating in the study are shown in Table 1.
Table 1.
Characteristics of the participating hospitals (from August 2003 to August 2011).
| Data | ICUs, n | HH observations, n |
|---|---|---|
| Type of ICU, n (%) | ||
| Paediatric | 2 (17%) | 1,984 |
| Surgical | 2 (17%) | 4,277 |
| Medical Surgical | 8 (66%) | 15,884 |
| All ICUs | 12 (100%) | 22,145 |
ICU, intensive care unit; HH, hand hygiene.
Predictors of poor hand hygiene compliance
We observed 6,752 procedures in males, and 15,393 in females; 11,651 in nurses, 5,451 in physicians, and 5,043 in ancillary staff; 13,153 were prior to non-invasive patient contacts, and 8,862 prior to invasive procedures; 20,161 in adult ICUs, and 1,984 in paediatric ICUs (PICUs); 13,202 during the morning; 6,852 during the afternoon; and 2,091 during the night shift.
Table 2 shows hand hygiene compliance distribution among the different ICU types in the baseline and intervention periods.
Table 2.
Distribution of hand hygiene compliance by type of intensive care unit.
| ICUs (n) | Baseline period (HH compliance/HH observations) | Intervention period (HH compliance/HH observations) | RR (95% CI) | p-value | |
|---|---|---|---|---|---|
| Medical Surgical | 8 | 21% (401/1,915) | 43% (6,043/13,969) | 2.1 (1.9–2.2) | 0.001 |
| Paediatric | 2 | 70% (332/475) | 76% (1,145/1,509) | 1.1 (0.97–1.2) | 0.120 |
| Surgical | 2 | 19% (82/435) | 44% (1,675/3,842) | 2.3 (2.1–2.5) | 0.001 |
| All | 12 | 29% (815/2,825) | 46% (8,863/19,320) | 1.6 (1.5–1.6) | 0.001 |
ICU, intensive care unit; HH, hand hygiene; RR, relative risk; CI, confidence interval.
Tables 3 and 4 show hand hygiene compliance according to each variable (hospital type, sex, profession of HCW, type of procedure, type of unit and work shift), and association with poor hand hygiene, analysed with univariate and multivariate statistical methods.
Table 3.
Hand hygiene compliance by type of variable. Univariate analysis.
| Variable | % (No. HH / No. opportunities) | Comparison | RR | 95% CI | p-value | |
|---|---|---|---|---|---|---|
| Sex | Female | 48% (7,387/15,393) | F vs M | 0.82 | 0.79–0.84 | 0.0001 |
| Male | 39% (2,651/6,752) | |||||
| HCW | Nurses | 49% (5,738/11,651) | Ns vs Ph | 0.94 | 0.92–0.97 | 0.0001 |
| Physicians | 46% (2,531/5,451) | Ns vs AS | 0.71 | 0.69–0.74 | 0.0001 | |
| Ancillary staff | 35% (1,769/5,043) | Ph vs AS | 0.76 | 0.73–0.78 | 0.0001 | |
| Procedure | Non-invasive | 42% (5,538/13,153) | NI vs I | 0.84 | 0.82–0.86 | 0.0001 |
| Invasive | 50% (4,443/8,862) | |||||
| Unit | Adult ICU | 42% (8,561/20,161) | Ad vs Pe | 0.57 | 0.54–0.60 | 0.0001 |
| Paediatric ICU | 74% (1,477/1,984) | |||||
| Work shift | Morning | 46% (6,056/13,202) | M vs A | 0.99 | 0.97–1.02 | 0.9289 |
| Afternoon | 46% (3,139/6,852) | M vs N | 0.88 | 0.84–0.92 | 0.0001 | |
| Night | 40% (843/2,091) | A vs N | 0.88 | 0.84–0.92 | 0.0001 |
HCW, health care worker; ICU, intensive care unit; AS, ancillary staff; F, female; M, male; Ni, non-invasive; I, invasive; Ad, adult; Pe, Paediatric; M, morning work shift; A, afternoon work shift; N, night work shift; NS, nursing staff; Ph, physicians; AS, ancillary staff.
Table 4.
Hand hygiene compliance by type of variable. Logistic regression, multivariate analysis.
| Variable | Adjusted OR | 95% CI | p-value |
|---|---|---|---|
| Sex (baseline: female) | 1 | ||
| Male | 0.93 | 0.86–1.00 | 0.056 |
| Type of professional (baseline: nurses) | 1 | ||
| Physicians | 1 | 0.94–1.1 | 0.804 |
| Ancillary staff | 0.69 | 0.64–0.75 | 0.001 |
| Type of contact (baseline: invasive) | 1 | ||
| Non-invasive | 0.65 | 0.61–0.96 | 0.001 |
| Type of ICU (baseline: paediatric) | 1 | ||
| Adult ICU | 0.22 | 0.19 – 0.24 | <0.001 |
| Work shift (baseline: morning) | 1 | ||
| Afternoon | 0.97 | 0.91–1.03 | 0.372 |
| Night | 0.65 | 0.59–0.74 | 0.001 |
ICU, intensive care unit; OR, odds ratio; CI, confidence interval.
Components of the INICC Multidimensional Hand Hygiene Approach
During the follow-up period, the six components of the IMHHA were applied simultaneously: 100% counted on administrative support and available supplies for hand hygiene and alcohol hand rub; 100% educated HCWs (42.9% of them every month, 28.6% every three months, 14.3% every six months, and 14.3% every year); 83.3% posted reminders (75% of them at ICU entrance, 58.3% in common ICU areas, 8.3% beside each bed); process surveillance was conducted by 100%; 92.9% provided performance feedback (28.6% of them every month, 7.1% every two months, 28.6% every three months, 21.4% every six months, and 7.1% every year).
Impact of the INICC Multidimensional Hand Hygiene Approach on hand hygiene compliance
In Table 5, we present the results of a logistic regression model to consider change in hand hygiene compliance in INICC participating ICUs over the whole study period. Although we observed a sustainable increase in the adherence of hand hygiene, during the third and fourth years there were only 2 ICUs being followed-up.
Table 5.
Hand hygiene improvement by year of participation.
| Years since joining INICC | HH observations | No. of ICUs included | No. of hospitals included | HH % (95% CI) | Adjusted OR | p-value |
|---|---|---|---|---|---|---|
| First 3 months (baseline) | 2,825 | 12 | 12 | 28.8% (27.2–30.5) | 1.0 | |
| Second 3 months | 7,352 | 12 | 12 | 43.4% (42.2–44.5) | 1.8 (1.6–2.0) | 0.0001 |
| 2nd year | 6,211 | 8 | 8 | 45.5% (44.3–47.9) | 3.2 (2.9–3.6) | 0.0001 |
| 3rd year | 4,467 | 6 | 6 | 48.7% (47.2–50.2) | 3.5 (3.0–4.0) | 0.0001 |
| 4th year | 812 | 3 | 3 | 73.3% (70.1–76.3) | 2.3 (1.8–2.8) | 0.0001 |
| 6th year | 478 | 2 | 2 | 91% (87.6–93.0) | 8.3 (4.9–14.0) | 0.0001 |
INICC, International Nosocomial Infection Control Consortium; HH, hand hygiene; ICU, intensive care units; CI, confidence interval; OR, odds ratio.
NOTE: Comparisons were made using only the ICUs with follow-up. That is, for the comparison of hand hygiene compliance with baseline for the third year, only hospitals with at least 3 years follow-up were included and the same with the following periods.
Use of hand hygiene products over time
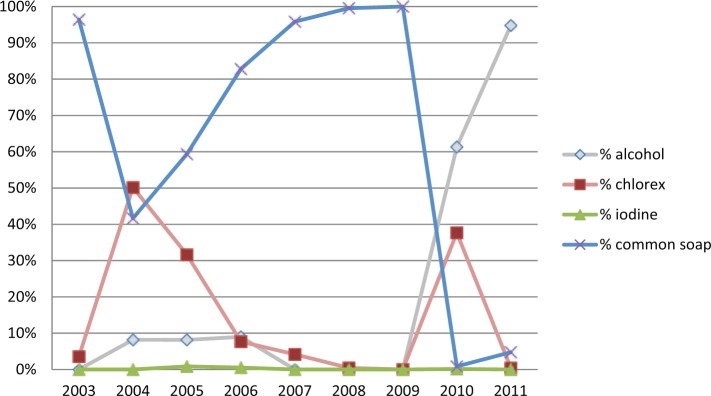
Use of aqueous chlorhexidine for hand washing started in 2004 at 50%, with a gradual reduction to 0% by 2009, a rapid rise to 39% in 2010, and a final decrease to 0% in 2011.
By contrast, alcohol hand rub use started in 2004, with variations ranging from 0% to 10% between 2004 and 2009, and finally rising to 95% in 2011, which was correlated with a sharp decrease in the use of common soap in 2010 (Figure 1).
Figure 1.
Type of product used in hand hygiene over the years of participation.
Discussion
This is the first study that has showed an improvement in hand hygiene compliance in Turkey due to the implementation of the IMHHA. We analysed the impact of the IMHHA in a diverse ICU population from 11 cities in Turkey, showing that the six measures of the IMHHA implemented in each ICU were followed by very substantial improvements in hand hygiene practices.
Baseline hand hygiene compliance (29%) of HCWs in the 12 ICUs from INICC member hospitals was similar to that shown in previous studies, whose hand hygiene compliance rates ranged from 9% to 75% (Pittet et al., 2009). In a recent study conducted in 51 cities of 19 limited-resource countries from Latin America, Asia, the Middle East, and Europe, the baseline hand hygiene compliance was 48.3% (Rosenthal et al., 2013), which is significantly higher than our baseline compliance rate of 29%. This markedly lower baseline of hand hygiene compliance stresses the compelling need to conduct this study to improve hand hygiene compliance in this specific ICU population of Turkey. Our target was to increase adherence to hand hygiene by at least 30%. With the implementation of the IMHHA, overall hand hygiene compliance in our ICUs increased from 28.8% to 91%, although during the third and fourth years there were only two ICUs being followed-up, and thus we cannot generalise these results for all the ICUs that participated in the study.
The results of the multivariate analysis showed that there was higher compliance in females, as also identified in individuals unrelated to health care, such as the findings of Guinan et al., which showed higher compliance by female students (Guinan et al., 1997). Compliance was the highest among nurses, as also shown in a study by Rosenthal et al. in 2005, in which compliance was lower among physicians and ancillary staff compared to nurses (Rosenthal et al., 2005). We also showed the highest hand hygiene compliance was in PICUs. Similarly, in a recent multicentric study, hand hygiene adherence was higher in adult ICUs versus neonatal ICUs (67% vs 81%) (Kowitt et al., 2013; Rosenthal et al., 2013) Watanakunakorn et al. (1998) also found remarkable variations by type of unit, with compliance being 56% in ICUs, compared to 23% in non-ICUs. We also showed that type of contact influenced hand hygiene performance: superficial contacts were associated with lower compliance. In relation to these last findings, Lipsett and Swoboda (2001) showed that lower hand hygiene compliance was found in low-risk situations. Use of hand hygiene products changed, showing an increase in alcohol hand rub use and a reduction in chlorhexidine use, which could be related to increasingly wider promotion of alcohol hand rub by WHO since 2009 (Pittet et al., 2009).
Our approach included administrative support. In 2003, Rosenthal et al. showed that higher hand hygiene adherence was associated with administrative support. We also included the availability of supplies. In 2000, Bischoff et al. showed that the more easily accessible dispensers of alcohol hand rub per bed, the higher the hand hygiene compliance. We also included education and training, which were other basic independent interventions identified to foster adequate hand hygiene performance. As shown in 1990 by Dubbert et al., educational intervention with routine classes improved hand hygiene compliance by 97% over four weeks. Likewise, but within the context of limited-resource countries, Rosenthal et al. (2003) showed HCWs’ education improved hand hygiene adherence, and that compliance increased further if performance feedback was also given. We also included reminders at workplace. In 1989, Conly et al. showed the importance of reminders to raise HCWs’ awareness of the relation between correct hand hygiene performance and HCAI reduction.
We measured 21,667 opportunities for hand hygiene. Every month, the ICT team provided performance feedback on hand hygiene practices to HCWs of each ICU. This is a most motivating aspect of the IMHHA for HCWs, because knowing the outcome of their efforts reflected by the measurement of their practices and the HAI incidence can be a significantly conscious-raising factor to ensure the IMHHA’s effectiveness (Rosenthal et al., 2013). From 1998 in Argentina, (Rosenthal et al., 2003, 2005) and 2002 internationally, (Rosenthal et al., 2006, 2008a,b; 2010a; Rosenthal et al., 2012b) INICC has introduced outcome and process surveillance and feedback on outcomes and performance, combined with training and education, as a means to improve quality in health care to a new level (Rosenthal et al., 2003, 2005).
Throughout the past decade, INICC has undertaken a global effort in America, Asia, Africa, the Middle East, and Europe to respond to the burden of HCAIs, and has achieved extremely successful results, by increasing hand hygiene compliance in developing countries (Rosenthal et al., 2013), improving compliance with other infection control interventions, and consequently reducing the rates of HCAI and mortality (Rosenthal et al., 2010b). There is evidence that participating in INICC has been associated with reductions in central line associated bloodstream infection (CLAB), catheter associated urinary tract infection (CAUTI), ventilator associated pneumonia (VAP) and mortality in adults ICUs in 15 countries and in paediatric ICUs in five countries (Rosenthal et al., 2010b, 2012a,c,e,g). In NICUs in 10 countries INICC has reduced the rate of VAP by 33% (Rosenthal et al., 2012f)
This study has some limitations. First, the INICC did not measure the “My five moments for hand hygiene” as advised by WHO in 2009, because the IMHHA started in 1998 in Argentina, (Rosenthal et al., 2005) and in 2002 internationally (Rosenthal et al., 2008a) that is, several years before the recommendation of WHO was published in 2009. In 2009, INICC included ‘WHO Five Moments for Hand Hygiene’ in its process surveillance forms and manuals (Pittet et al., 2009). Second, this is an observational, before-after, methodology, which implies less strength of evidence than other study designs. Direct observation of adherence typically involves difficulty in assuring interobserver reliability, especially given the broad scope of this research in terms of facilities. Additionally, there might have been a Hawthorne effect at the beginning of the study, and the quality of hand hygiene technique is hard to capture. Finally, in this study we did not include information about HCAI and mortality rates, as there are several INICC publications that focus on these topics in relation to hand hygiene.
Conclusions
We showed that the IMHHA improved hand hygiene compliance in 12 ICUs of 12 hospitals in 11 cities of Turkey. It is INICC’s primary objective to foster infection control practices, by freely facilitating elemental and inexpensive resourceful tools to tackle this problem effectively and systematically, leading to greater and steady adherence to infection control programmes and guidelines, such as hand hygiene compliance, and to the correlated reduction of HCAIs and their consequences, such as mortality and extra cost.
Acknowledgments
The authors thank the many healthcare professionals at each member hospital who assisted with the conduct of surveillance in their hospital, including the surveillance nurses, clinical microbiology laboratory personnel, and the physicians and nurses providing care for the patients during the study; without their cooperation and generous assistance this INICC would not be possible; Mariano Vilar and Débora López Burgardt, who work at INICC 1headquarters in Buenos Aires, for their hard work and commitment to achieve INICC goals; the INICC Country Coordinators and Secretaries (Altaf Ahmed, Carlos A. Álvarez-Moreno, Anucha Apisarnthanarak, Luis E. Cuéllar, Bijie Hu, Namita Jaggi, Hakan Leblebicioglu, Montri Luxsuwong, Eduardo A. Medeiros, Yatin Mehta, Ziad Memish, Toshihiro Mitsuda, and Lul Raka,); and the INICC Advisory Board (Carla J. Alvarado, Nicholas Graves, William R. Jarvis, Patricia Lynch, Dennis Maki, Gerald McDonnell, Toshihiro Mitsuda, Cat Murphy, Russell N. Olmsted, Didier Pittet, William Rutala, Syed Sattar, and Wing Hong Seto), who have so generously supported this unique international infection control network.
Footnotes
Declaration of conflicting interest: All authors report no conflicts of interest related to this article. Every hospital’s Institutional Review Board agreed to the study protocol, and participants’ confidentiality was protected by codifying the recorded information, making it identifiable only to the infection control team.
Funding: This work was supported by the INICC headquarters, the corresponding author, and the Foundation to Fight against Nosocomial Infections.
Peer review statement: Not commissioned; blind peer-reviewed.
References
- Anon (2005) WHO launches global patient safety challenge; issues guidelines on hand hygiene in health care. Indian Journal of Medical Sciences 59(10): 461–463. [PubMed] [Google Scholar]
- Allegranzi B, Sax H, Bengaly C, Richet H, Minta DK, Chraiti MN, Sokona FM, Gayet-Ageron A, Bonnabry P, Pittet D. (2010) Successful implementation of the World Health Organization hand hygiene improvement strategy in a referral hospital in Mali, Africa. Infection ontrol and Hospital Epidemiology: The official journal of the Society of Hospital Epidemiologists of America 31(2): 133–141. [DOI] [PubMed] [Google Scholar]
- Bischoff WE, Reynolds TM, Sessler CN, Edmond MB, Wenzel RP. (2000) Handwashing compliance by health care workers: the impact of introducing an accessible, alcohol-based hand antiseptic. Archives of Internal Medicine 160(7): 1017–1021. [DOI] [PubMed] [Google Scholar]
- Conly JM, Hill S, Ross J, Lertzman J, Louie TJ. (1989) Handwashing practices in an intensive care unit: the effects of an educational program and its relationship to infection rates. American Journal of Infection Control 17(6): 330–339. [DOI] [PubMed] [Google Scholar]
- Dubbert PM, Dolce J, Richter W, Miller M, Chapman SW. (1990) Increasing ICU staff handwashing: effects of education and group feedback. Infection Control and Hospital Epidemiology 11(4): 191–193. [DOI] [PubMed] [Google Scholar]
- Guinan ME, McGuckin-Guinan M, Sevareid A. (1997) Who washes hands after using the bathroom? American Jouranl of Infection Control 25(5): 424–425. [DOI] [PubMed] [Google Scholar]
- Horan TC, Andrus M, Dudeck MA. (2008) CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. American Journal of Infection Control 36(5): 309–332. [DOI] [PubMed] [Google Scholar]
- Jarvis WR. (1996) Selected aspects of the socioeconomic impact of nosocomial infections: morbidity, mortality, cost, and prevention. Infection Control and Hospital Epidemiology 17(8): 552–557. [DOI] [PubMed] [Google Scholar]
- Kowitt B, Jefferson J, Mermel LA. (2013) Factors associated with hand hygiene compliance at a tertiary care teaching hospital. Infection Control and Hospital Epidemiology 34(11): 1146–1152. [DOI] [PubMed] [Google Scholar]
- Lam BC, Lee J, Lau YL. (2004) Hand hygiene practices in a neonatal intensive care unit: a multimodal intervention and impact on nosocomial infection. Pediatrics 114(5): e565–571. [DOI] [PubMed] [Google Scholar]
- Lipsett PA, Swoboda SM. (2001) Handwashing compliance depends on professional status. Surgical Infections (Larchmt) 2(3): 241–245. [DOI] [PubMed] [Google Scholar]
- Pittet D, Allegranzi B, Boyce J. (2009) The World Health Organization Guidelines on Hand Hygiene in Health Care and their consensus recommendations. Infection Control and Hospital Epidemiology: The official journal of the Society of Hospital Epidemiologists of America 30(7): 611–622. [DOI] [PubMed] [Google Scholar]
- Raju TN. (1999) Ignac Semmelweis and the etiology of fetal and neonatal sepsis. Journal of Perinatology 19(4): 307–310. [DOI] [PubMed] [Google Scholar]
- Rosenthal VD, Alvarez-Moreno C, Villamil-Gomez W, Singh S, Ramachandran B, Navoa-Ng JA, Duenas L, Anyalcin G, Ersoz A, Menco Arrieta P, Bran-de Casares AC, de Jesus Machuca L, Radhakrishnan K, Villanueva VD, Tolentino MC, Turhan O, Keskin S, Gumus E, Dursun O, Kaya A, Kuyucu N. (2012a) Effectiveness of a multidimensional approach to reduce ventilator-associated pneumonia in pediatric intensive care units of 5 developing countries: International Nosocomial Infection Control Consortium findings. American Journal of Infection Control 40(6): 497–501. [DOI] [PubMed] [Google Scholar]
- Rosenthal VD, Bijie H, Maki DG, Mehta Y, Apisarnthanarak A, Medeiros EA, Leblebicioglu H, Fisher D, Alvarez-Moreno C, Khader IA, Del Rocio Gonzalez Martinez M, Cuellar LE, Navoa-Ng JA, Abouqal R, Guanche Garcell H, Mitrev Z, Pirez Garcia MC, Hamdi A, Duenas L, Cancel E, Gurskis V, Rasslan O, Ahmed A, Kanj SS, Ugalde OC, Mapp T, Raka L, Yuet Meng C, Thu le TA, Ghazal S, Gikas A, Narvaez LP, Mejia N, Hadjieva N, Gamar Elanbya MO, Guzman Siritt ME, Jayatilleke K. (2012b) International Nosocomial Infection Control Consortium (INICC) report, data summary of 36 countries, for 2004–2009. American Journal of Infection Control 40(5): 396–407. [DOI] [PubMed] [Google Scholar]
- Rosenthal VD, Guzman S, Safdar N. (2005) Reduction in nosocomial infection with improved hand hygiene in intensive care units of a tertiary care hospital in Argentina. American Journal of Infection Control 33(7): 392–397. [DOI] [PubMed] [Google Scholar]
- Rosenthal VD, Maki DG, Graves N. (2008a) The International Nosocomial Infection Control Consortium (INICC): goals and objectives, description of surveillance methods, and operational activities. American Journal of Infection Control 36(9): e1–12. [DOI] [PubMed] [Google Scholar]
- Rosenthal VD, Maki DG, Jamulitrat S, Medeiros EA, Todi SK, Gomez DY, Leblebicioglu H, Abu Khader I, Miranda Novales MG, Berba R, Ramirez Wong FM, Barkat A, Pino OR, Duenas L, Mitrev Z, Bijie H, Gurskis V, Kanj SS, Mapp T, Hidalgo RF, Ben Jaballah N, Raka L, Gikas A, Ahmed A, Thu le TA, Guzman Siritt ME. (2010a) International Nosocomial Infection Control Consortium (INICC) report, data summary for 2003–2008, issued June 2009. American Journal of Infection Control 38(2): 95–104 e2. [DOI] [PubMed] [Google Scholar]
- Rosenthal VD, Maki DG, Mehta A, Alvarez-Moreno C, Leblebicioglu H, Higuera F, Cuellar LE, Madani N, Mitrev Z, Duenas L, Navoa-Ng JA, Garcell HG, Raka L, Hidalgo RF, Medeiros EA, Kanj SS, Abubakar S, Nercelles P, Pratesi RD. (2008b) International Nosocomial Infection Control Consortium report, data summary for 2002–2007, issued January 2008. American Journal of Infection Control 36(9): 627–637. [DOI] [PubMed] [Google Scholar]
- Rosenthal VD, Maki DG, Rodrigues C, Alvarez-Moreno C, Leblebicioglu H, Sobreyra-Oropeza M, Berba R, Madani N, Medeiros EA, Cuellar LE, Mitrev Z, Duenas L, Guanche-Garcell H, Mapp T, Kanj SS, Fernandez-Hidalgo R. (2010b) Impact of International Nosocomial Infection Control Consortium (INICC) strategy on central line-associated bloodstream infection rates in the intensive care units of 15 developing countries. Infection Control and Hospital Epidemiology 31(12): 1264–1272. [DOI] [PubMed] [Google Scholar]
- Rosenthal VD, Maki DG, Salomao R, Moreno CA, Mehta Y, Higuera F, Cuellar LE, Arikan OA, Abouqal R, Leblebicioglu H. (2006) Device-associated nosocomial infections in 55 intensive care units of 8 developing countries. Annals of Internal Medicine 145(8): 582–591. [DOI] [PubMed] [Google Scholar]
- Rosenthal VD, McCormick RD, Guzman S, Villamayor C, Orellano PW. (2003) Effect of education and performance feedback on handwashing: the benefit of administrative support in Argentinean hospitals. American Journal of Infection Control 31(2): 85–92. [DOI] [PubMed] [Google Scholar]
- Rosenthal VD, Pawar M, Leblebicioglu H, Navoa-Ng JA, Villamil-Gomez W, Armas-Ruiz A, Cuellar LE, Medeiros EA, Mitrev Z, Gikas A, Yang Y, Ahmed A, Kanj SS, Duenas LL, Gurskis V, Mapp T, Guanche-Garcell H, Fernandez-Hidalgo R, Kubler A. (2013) Impact of the International Nosocomial Infection Control Consortium (INICC) multidimensional hand hygiene approach over 13 years in 51 cities of 19 limited-resource countries from Latin America, Asia, the Middle East, and Europe. Infection Control and Hospital Epidemiology 34(4): 415–423. [DOI] [PubMed] [Google Scholar]
- Rosenthal VD, Ramachandran B, Duenas L, Alvarez-Moreno C, Navoa-Ng JA, Armas-Ruiz A, Ersoz G, Matta-Cortes L, Pawar M, Nevzat-Yalcin A, Rodriguez-Ferrer M, Bran de, Casares A, Linares C, Villanueva VD, Campuzano R, Kaya A, Rendon-Campo LF, Gupta A, Turhan O, Barahona-Guzman N, de Jesus-Machuca L, Tolentino MC, Mena-Brito J, Kuyucu N, Astudillo Y, Saini N, Gunay N, Sarmiento-Villa G, Gumus E, Lagares-Guzman A, Dursun O. (2012c) Findings of the International Nosocomial Infection Control Consortium (INICC), Part I: Effectiveness of a multidimensional infection control approach on catheter-associated urinary tract infection rates in pediatric intensive care units of 6 developing countries. Infection Control and Hospital Epidemiology: The official journal of the Society of Hospital Epidemiologists of America 33(7): 696–703. [DOI] [PubMed] [Google Scholar]
- Rosenthal VD, Ramachandran B, Villamil-Gomez W, Armas-Ruiz A, Navoa-Ng JA, Matta-Cortes LA, Pawar M, Nevzat-Yalcin A, Rodriguez-Ferrer M, Yildizdas RD, Menco A, Campuzano R, Villanueva VD, Rendon-Campo LF, Gupta A, Turhan O, Barahona-Guzman N, Horoz OO, Arrieta P, Brito JM, Tolentino MC, Astudillo Y, Saini N, Gunay N, Sarmiento-Villa G, Gumus E, Lagares-Guzman A, Dursun O. (2012d) Impact of a multidimensional infection control strategy on central line-associated bloodstream infection rates in pediatric intensive care units of five developing countries: findings of the International Nosocomial Infection Control Consortium (INICC). Infection 40(4): 415–423. [DOI] [PubMed] [Google Scholar]
- Rosenthal VD, Rodrigues C, Alvarez-Moreno C, Madani N, Mitrev Z, Ye G, Salomao R, Ulger F, Guanche-Garcell H, Kanj SS, Cuellar LE, Higuera F, Mapp T, Fernandez-Hidalgo R. (2012e) Effectiveness of a multidimensional approach for prevention of ventilator-associated pneumonia in adult intensive care units from 14 developing countries of four continents: findings of the International Nosocomial Infection Control Consortium. Critical Care Medicine 40(12): 3121–3128. [DOI] [PubMed] [Google Scholar]
- Rosenthal VD, Rodriguez-Calderon ME, Rodriguez-Ferrer M, Singhal T, Pawar M, Sobreyra-Oropeza M, Barkat A, Atencio-Espinoza T, Berba R, Navoa-Ng JA, Duenas L, Ben-Jaballah N, Ozdemir D, Ersoz G, Aygun C. (2012f) Findings of the International Nosocomial Infection Control Consortium (INICC), Part II: Impact of a multidimensional strategy to reduce ventilator-associated pneumonia in neonatal intensive care units in 10 developing countries. Infection Control and Hospital Epidemiology 33(7): 704–710. [DOI] [PubMed] [Google Scholar]
- Rosenthal VD, Todi SK, Alvarez-Moreno C, Pawar M, Karlekar A, Zeggwagh AA, Mitrev Z, Udwadia FE, Navoa-Ng JA, Chakravarthy M, Salomao R, Sahu S, Dilek A, Kanj SS, Guanche-Garcell H, Cuellar LE, Ersoz G, Nevzat-Yalcin A, Jaggi N, Medeiros EA, Ye G, Akan OA, Mapp T, Castaneda-Sabogal A, Matta-Cortes L, Sirmatel F, Olarte N, Torres-Hernandez H, Barahona-Guzman N, Fernandez-Hidalgo R, Villamil-Gomez W, Sztokhamer D, Forciniti S, Berba R, Turgut H, Bin C, Yang Y, Perez-Serrato I, Lastra CE, Singh S, Ozdemir D, Ulusoy S. (2012g) Impact of a multidimensional infection control strategy on catheter-associated urinary tract infection rates in the adult intensive care units of 15 developing countries: findings of the International Nosocomial Infection Control Consortium (INICC). Infection 40(5): 517–526. [DOI] [PubMed] [Google Scholar]
- Safdar N, Crnich CJ, Maki DG. (2001) Nosocomial infections in the intensive care unit associated with invasive medical devices. Current Infectious Disease Reports 3(6): 487–495. [DOI] [PubMed] [Google Scholar]
- Simmons B, Bryant J, Neiman K, Spencer L, Arheart K. (1990) The role of handwashing in prevention of endemic intensive care unit infections. Infection Control and Hospital Epidemiology 11(11): 589–594. [DOI] [PubMed] [Google Scholar]
- Watanakunakorn C, Wang C, Hazy J. (1998) An observational study of hand washing and infection control practices by healthcare workers. Infection Control and Hospital Epidemiology 19(11): 858–860. [DOI] [PubMed] [Google Scholar]