Abstract
Background: Death certification represents an excellent source for mortality statistics and appropriate public health surveillance. Errors in reporting the cause of death impede the development of national health policies and, accordingly, allocation of resources. The aim of this study was to determine the frequency of errors in the cause of death and to identify factors that may be associated with inaccuracies in death certificates.
Methods: A cross-sectional study of all natural death certifications in a defined Greek region was conducted over the period 2006-2010. Specific criteria for major and minor errors were adopted for the evaluation of death certificates.
Results: A total of 5,828 death certificates due to natural causes were identified. Major errors were found in 64.6 % of them with almost every death certificate having a minor error. Major error rate did not differ per year (p =0.65). Most commonly encountered major errors were a non-acceptable cause of death (31.2 %) and an incorrect sequencing (16.8 %). Factors affecting their frequency were the age of the deceased (older than 80 years, p =0.025), the area of certificate completion (rural and semi-urban, p <0.001) and doctor’s grade (consultant, p <0.026).
Conclusions: High rate of recording errors at death certification influences the accuracy of the cause of death in a defined region in Southern Greece. Due to their impact on mortality statistics and health policies, standard practices of death certification should be established. Coordinated educational interventions are expected to play a significant role on this. Hippokratia 2016, 20(1): 19-25
Keywords: Death certificate, errors, mortality, public health, health policy
Introduction
The information documented on death certificates, such as decedent’s characteristics and cause of death, constitute an important source of information for routine data and vital statistics. These records are used to describe populations’ health profile and to monitor secular changes in population mortality. Death certification provides data valuable for guiding health policies by setting targets and priorities for health promotion and appropriate allocation of resources for preventive and treatment health programs. Also, death certificates can be used to evaluate the effectiveness of medical services as well as the usefulness of programs developed to address diseases with high mortality.
Furthermore, death certificates help in interpreting inter-country differences in mortality rates and etiological factors. In an attempt to facilitate such processes, the World Health Organization (WHO) established an international medical cause of death certificate tool in order to ensure reproducibility and comparability within and among different countries. Specifically, in Europe, a manual on causes of death certification was first published in 20031,2.
However, inaccurate causes of death are frequent with errors ranging from 39% to 61% in population-based studies3-5. In hospital-based studies, major errors range from 32 to 45%6-11 with some degree of error in death certificates accounting for up to 99%9-11. Advances in education have improved the reporting accuracy but did not eliminate malpractice12,13. Such bias has proved significant enough to confound the estimated prevalence of diseases. Misreports vary by cause of death. Coronary heart disease appears to be over-reported14,15 whereas diabetes mellitus seems to be under-reported16-18. However, in death certification, the overall estimation of the burden of cancer has been considered as accurate19,20.
As a result, only a few countries can use mortality statistics derived from death certificates to reliably support development and implementation of specific policies. Greece is classified as providing low-quality data21,22 with the exception of deaths related to road accidents and suicides/homicides23. This study aims to determine the frequency and types of error in the cause of death and to identify factors associated with inaccuracies in death certificates.
Methods
Setting and data source
A retrospective descriptive study of all original medical death certificates from the prefecture of Laconia over the period 2006-2010 was conducted. Laconia, a prefecture located in Southern Greece (Peloponnese), consists of four municipalities with a total population of approximately one hundred thousand people. Death certificates were collected from 22 competent registries. The study was approved by the Hellenic Data Protection Authority (Ref. No: Γ/ΕΞ/4556-1/20-10-2011). No funding was received.
In this population-based study, certificates for non-natural deaths, forensic findings, perinatal deaths, certificates from foreign countries and death certificates in which the underlying cause of death could not be clearly identified were excluded. The cause of death was recorded. Certificates were examined for the terminology and sequence of events leading to death according to WHO guidelines1. The causes of death were recorded according to the ICD-10 classification of diseases24. This study was not validated due to lack of medical records and information from the autopsy.
Death certificates were evaluated with criteria used in previous studies6,12,25. Errors were classified as major if they could have an impact on the accurate identification of the underlying cause of death. Major errors included one of the following criteria (mutually exclusive):
Type I: Mechanism of death without an underlying cause. Mechanism of death is defined as a pathophysiological process such as ventricular fibrillation, cardiac arrest, asphyxia, syncope, multiorgan failure, etc. The underlying cause leads to death eventually by such mechanisms. In this type of error, no underlying cause has been reported.
Type II: Non-acceptable cause of death. A cause is recorded without further documentation of what had preceded. In this type of error, causes such as anemia, pulmonary edema, neoplasm, immunocompromised patient, dehydration were the recorded causes without any further explanation on what led to them.
Type III: An improper sequence in immediate, intermediate and underlying causes of death. The death certification provides the ability to distinguish the time sequence of diseases that may have led to death. For example, an acceptable sequence may be arterial hypertension, congestive heart failure, acute pulmonary edema. An improper sequence is an error that records unacceptable sequences; in our example congestive heart failure, acute pulmonary edema, arterial hypertension.
Type IV: Multiple and independent causes of death. In this major error, multiple causes of death have been recorded in the same line or different lines. These causes did not follow necessarily common pathophysiological pathways. For example, various recorded causes of death included acute respiratory failure and dementia or acute renal failure and syncope. Examples of independent causes of death included immunosuppression and heart failure or chronic obstructive pulmonary disease (COPD) and neoplasms etc.
Minor errors were defined as those that could not influence or confound the identification of the underlying cause of death. Minor errors included any of the following criteria (not mutually exclusive):
i) Absence of time intervals between underlying causes and mechanism of death.
ii) Use of abbreviations.
iii) Mechanism of death and underlying cause with incomplete information. For example, mechanism of death: acute pulmonary edema, and underlying cause: congestive heart failure without any further information.
Apart from error classification, information collected from death certificates included: 1. Decedent’s characteristics (gender, age, and the municipality of residence) and 2. Physician’s characteristics, such as Specialty [Internal Medicine and subspecialties (internist), General Surgery and subspecialties (surgeon), or General Practitioner (GP)], and Level of training [specialized (board certified), in training (resident), or rural doctor]. Specialized physicians’ experience was reviewed only for those working in the Greek National Health System and classified based on the specialist’s grade (Consultant B, Consultant A, Associate Head Physician, Head Physician). The place of death was recorded and categorized as i. private home, ii. private clinic/nursing homes, iii. primary health care center, iv. secondary hospital, and v. tertiary hospital.
Descriptive statistics were calculated as percentages with 95% confidence intervals. Correlations were evaluated by Yates corrected Chi-square test. Logistic regression analyzed the possible association between various factors as well as the type of errors. Statistical significance was set at p <0.05. The Statistical Package for Social Sciences (SPSS Inc., Chicago, USA) version 16 was used for statistical analysis.
Results
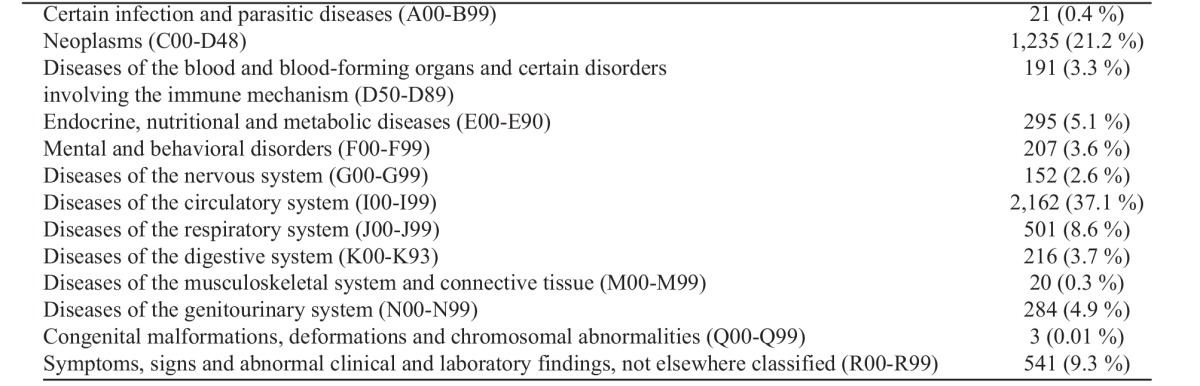
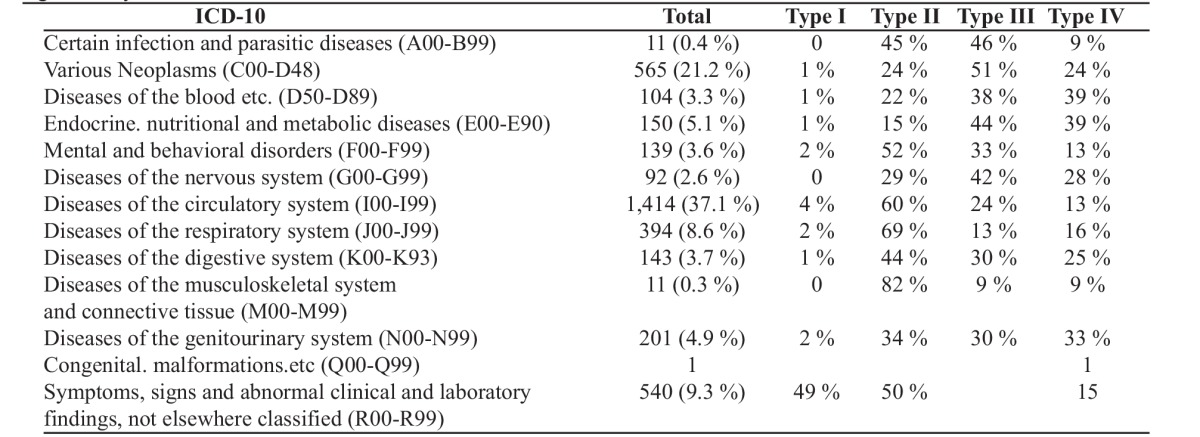
A total of 6,388 death certificates were collected from 22 registries. After excluding 85 of them for unnatural death, 406 for forensic findings, 10 from overseas and 59 in which the cause of death could not be identified, 5,828 (91.2 %) death certificates were finally analyzed. Almost half were male, and 3,667 (62.9 %) were over 80 years old. The majority of death certificates was documented in Sparta (2,163, 37.1 %) and were completed by an internist (internal medicine or subspecialties) (3,935, 74.9 %). Home was referred as the place of death in 2,557 (43.9 %) certificates. Only 2,938 (51.2 %) of the certificates were completed by the attending physician (Table 1). Cardiovascular diseases were the leading cause of death accounting for 37.1 % of the certificates followed by various malignancies (21.2 %), and respiratory diseases (8.6 %). All causes of death according to ICD-10 classification groups are presented in Table 2.
Table 1. Data from the 5,828 death certificates collected from 22 registries of the prefecture of Laconia, Greece over the period 2006-2010. Data regarding: i. Deceased age group and gender, ii. municipality and place of death, iii. speciality, training, specialist grade and place of work of physicians iv. percentage of attending physicians who completed death certificates for their patients.
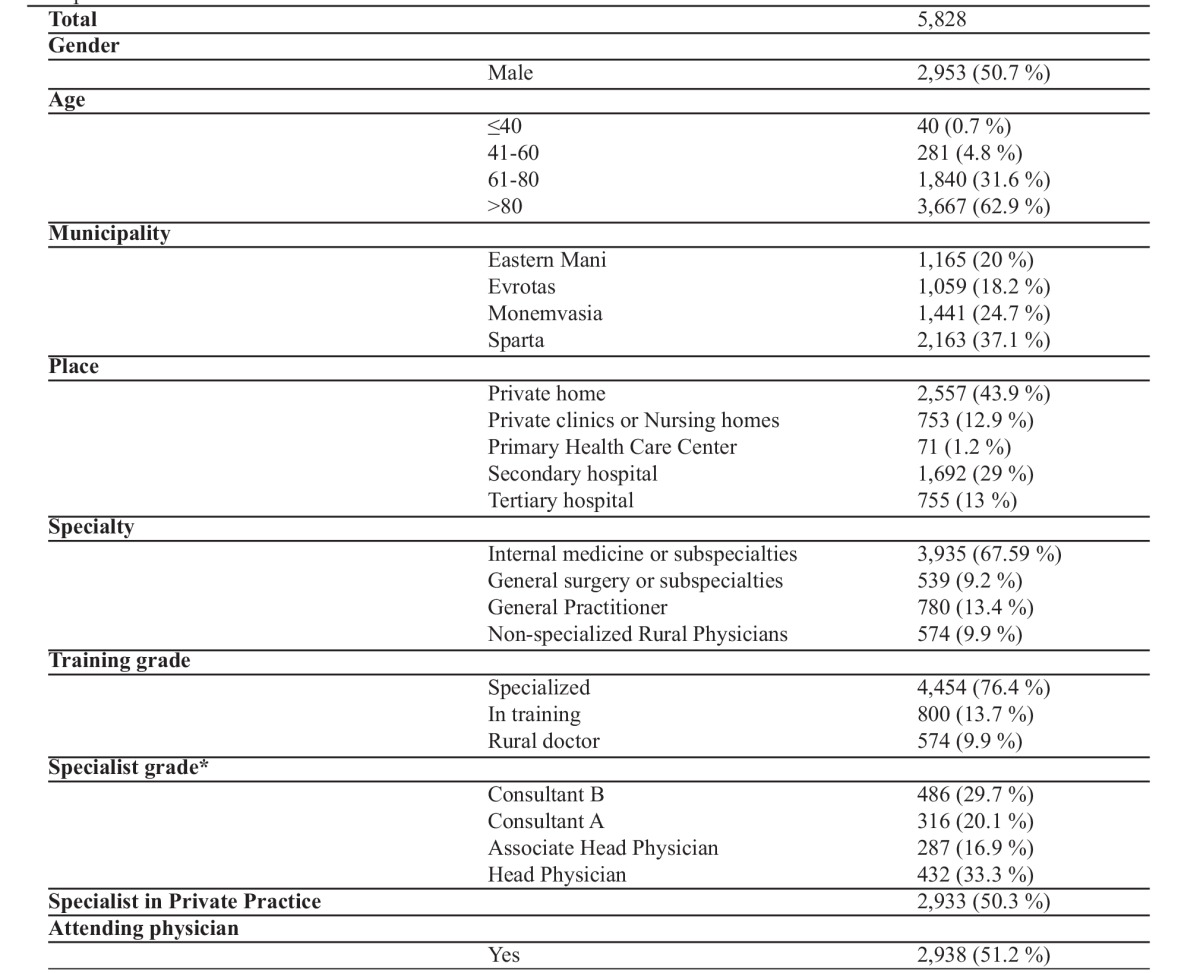
*: in the Greek National Health System there are 4 specialist grades: Consultant B, Consultant A, Associate Head Physician, Head Physician.
Table 2. Causes of death in the 5,828 death certificates, according to International Statistical Classification of Diseases and Related Health Problems, 10th Revision24.
The types of error encountered according to the criteria used in the study are presented in Table 3. Major errors were found in 64.6 % of the certificates with the most frequent major error being a non-acceptable cause of death (31.2 %) (Type II error), using terms such as “sepsis”, “old age”, “stroke” or “metastatic cancer”. Improper sequencing (Type III error) was found in 16.8 % of the certificates. Almost all (99.2 %) certificates had one, and 72.7 % of them had two minor errors. Distributions of major errors according to patients’ demographic data, physicians’ characteristics and ICD-10 classification groups are presented in Table 4 and Table 5.
Table 3. Major errors (mutually exclusive) were found in 64.6 % of the 5,828 death certificates, and minor errors (not mutually exclusive) practically in all certificates. Major errors are arbitrary to the use and interpretation of certificates while minor errors do not prohibit their use.
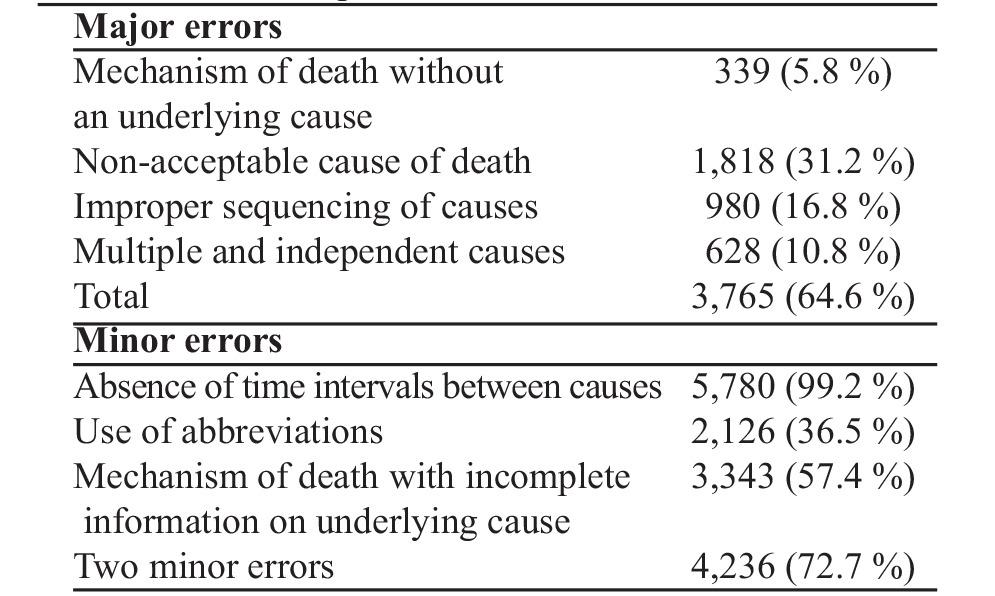
Table 4. Distribution of major errors according to the person who completed the death certificate and the place where certificates were completed. Type I: Mechanism of death without an underlying cause; Type II: Non-acceptable cause of death; Type III: Improper sequence in immediate, intermediate and underlying causes of death; Type IV: Multiple and independent causes of death. Odds ratios (OR) were calculated in each category. Baseline risk as 1 was considered for the subgroups: Age ≤40, Municipality of Sparta, and Consultant B. Only statistically significant ORs are shown.
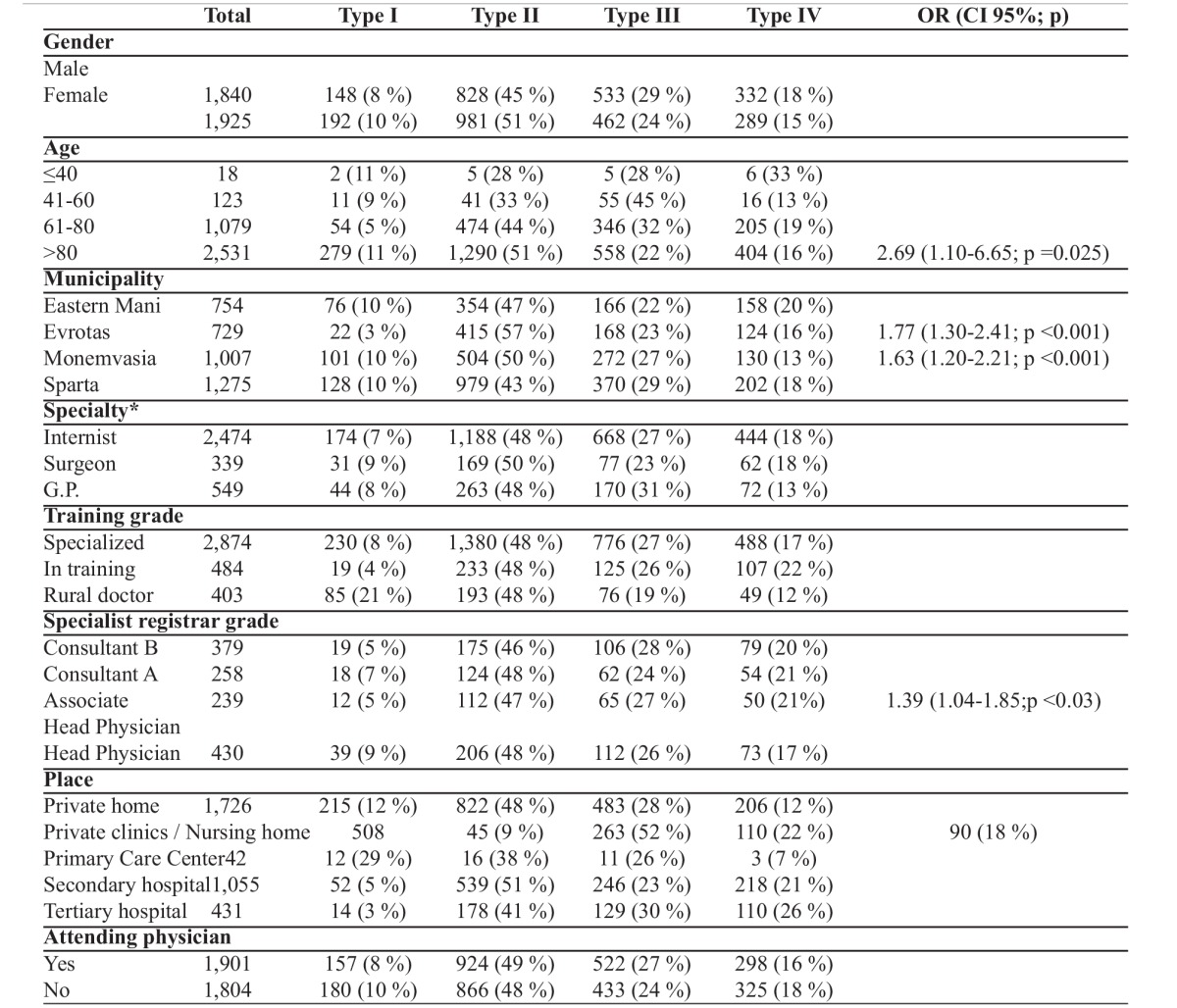
All data are presented as numbers and rounded percentages, OR: Odds ratio, CI 95%: 95% confidence interval, *: Internist: Internal medicine or subspecialties, Surgeon: General surgery or subspecialties, G.P.: General Practitioner.
Table 5. Distribution of major errors according to ICD-10 classification. Type I: Mechanism of death without an underlying cause; Type II: Non-acceptable cause of death; Type III: Improper sequence in immediate, intermediate and underlying causes of death; Type IV: Multiple and independent causes of death. Classification groups and major errors were not statistically significantly associated.
The yearly distribution of major errors did not differ from 2006 to 2010 (p =0.65). Major errors were associated with older age [the older than 80 years age group had an odds ratio of 2.69 (1.10-6.65 95% CI, p =0.025) for certificates with major errors compared to the other age groups)], with certificates from certain rural and semi-urban municipalities (p <0.001) and with certificates completed from associate chief consultants [OR: 1.39 (1.04-1.85 95% CI. p <0.03)]. Surprisingly, the parameter whether the certifier was the attending physician or not, was not associated with the presence of major errors. There were no statistically significant differences between the various ICD-10 classification groups and any major errors. Minor errors, as mentioned above, were present in almost every death certificate.
Discussion
Death certificates can be used as a tool to depict the population health status as well to monitor the efficacy of public health policies. Absence of reliable data on the cause of death can lead to improper decisions regarding health care. The death certificate is a formal state document, which includes all personal data of the deceased along with the cause of death, accounting for a significant fraction of national statistics.
In this cross-sectional descriptive study, two-thirds of the 5,828 reviewed death certificates, issued from 2006 to 2010, were erroneously completed. This unacceptably high rate of errors is comparable to a previous study conducted in a rural area in Greece, where data over an 8-year period was used (60.6 %)4. The frequency of major errors (64.6 %) was much higher compared to the results of previous publications using similar criteria, where it ranged from 32 % to 45.4 %5,6,10,12. This discrepancy could be the result of age differences. In two studies that included age distributions, one population-based study5 and one hospital-based10, both conducted in South Africa, only 29.4 % and 39 % of the deceased respectively, were older than 60 years, compared to 94.5 % in the current study.
The most common recorded major error in 31 % of the certificates was the non-acceptable cause of death (type II), and this percentage is quite high compared to other studies where it ranged from 4.5 % to 26 %3-5,9,10. Terms such as “senescence”, “infirmity”, “old age”, and “advanced age” were written in the majority of certificates, despite the fact that there are no standards regarding the age group been considered as “old”2. Although death certification in the elderly poses particular problems as they often seem to die “with their diseases” rather than “of their diseases”, certificates should normally have a clear and distinct etiological sequence for the cause of death. Another common non-specific term was “carcinomatosis” or “metastatic cancer” without reference to primary tumor site and “septicemia” or “septic shock” without reference to the primary condition and the type of infection that led to this. Non-specific conditions such as “hypertension” or “cerebrovascular accident” without further information were also common errors. Naghavi et al described in detail the use of «garbage diagnoses» as a well-known problem in the cause of death statistics25. Improper sequence (type III) was found in 16.8 % of certificates, similar to what reported in Canadian6,12, Indian11, American9, and South-African10 hospital-based studies, ranging between 15.8 % and 24 %. On the other hand, in population-based studies, an improper sequence was either lower as in Greece4 and Taiwan3 (6.8 % and 9 % respectively), or higher as in South-Africa (28.7 %)5.
Type IV major error accounts for 2.6 % to 15.3 %3,5,11 of the certificates examined in different studies and Type I for 7 % to 34 %3,8,9. The percentage of certificates with Type IV error was similar to a previous study in rural Greek population4. However, Type I error frequency in the certificates was quite different between the two studies. According to Katsakiori et al4 study, Type I error was the principal one (34.5 %), while an unacceptable cause of death was present in 4.5 % of the certificates, contrary to the results of the current study (5.8 % and 31.2 % respectively). This could be explained by the classification system that was used. Lu et al referred sepsis as a mechanism3 with Katsakiori et al4 using this classification system. On the other hand, according to the criteria of Myers and Farquhal12 which were used in the current study, sepsis is a nonspecific cause. Furthermore, O'Donovan et al26 and McAllum et al27 report that, in cases of sudden death, clinical uncertainty seems to be the most common reason for errors in death recording, especially in general practitioners.
Minor errors were found in almost all death certificates, similarly to previous studies ranging from 78 % to 98 %. Absence of time intervals was the most frequent minor error, as in South African studies5,10. Mechanism with incomplete information on the underlying cause of death was found in 57 % of certificates. In fact, the mechanism of death should not be reported as the immediate cause of death since it is a statement not specifically related to the disease process, and it merely contributes to death. Abbreviations of medical terms were used in one-third of certificates. In the literature, the proportion of mechanism of death as the immediate cause ranges from 20.6 % to 49.7 % while abbreviations rate range from 10.7 % to 46.5 %5,9-11.
The most significant predictor of major errors was the deceased’s age with the probability increasing by 62 % for every 20-year-increase after the age of 40. Similarly, probability increased by 28 % for a 10-year-increase after 59 years in a study involving Taiwanese individuals3 and decreased by 58 % in ages 15-64 years compared to older people in a study from South Africa5. In the study by Katsakiori et al4, errors were present in 63.8 % of death certificates in deceased older than 60 years, and in 39.1 % of younger individuals. Multiple comorbidities of elderly people could be an explanation as in certain cases the physician may not be able to provide an accurate or sole cause.
Furthermore, place of death was associated with the incidence of major errors. In the current study as well as in many previous studies, primary care centers seemed to be more related to major errors compared to secondary and tertiary hospitals3,5 with a probability decreasing by 7 % for an upgrading of hospital level compared to death certificates completed in a private home. Investigating this particular parameter, a Taiwanese study observed a difference of major errors up to 25 % between primary care centers and tertiary hospitals3. On the contrary, this finding was not observed in the study by Katsakiori et al4, probably because the certifying doctors were classified into primary health care physicians working in the regional health center (group A), private physicians and physicians working in hospitals (group B).
In multivariate analysis, deceased’s gender was not associated with major errors. This could be explained by the physicians’ certification practice itself rather than the deceased’s characteristics, as already reported in a study from similar Greek population, while conflicting results were noted in the two South African studies5,10. The common finding of major errors in death certificates led Matherts et al21 to conclude that only 23 of the 106 studied countries had accurate data that could be used to develop health policies. Greece was among the countries of low-quality data, with less than 70 % completion of the certificate and more than 20 % mistaken codes. Mahapatra et al22 observed that even though 31 of 192 countries had high-quality data, they accounted only for 13 % of the world population. Moreover, improvement during the last 50 years was minimal and seen in developed countries. According to the results of the current study, Greece belongs to countries with low-quality data and high percentage of mistaken codes. Bhalla et al23 revealed that only 20 of 83 countries had high-quality data with less than 20 % of mistaken codes. Interestingly, Greece was noted for high-quality data only for deaths due to traffic accidents and suicide/homicide.
According to presented findings, similarly to previous studies, further education on death certification is needed. In a recent study, certification practice seems to be influenced by the educational background. Only 27.1 % of Greek medical students self-evaluated their knowledge in death certification as adequate28, while in a similar French study, 56.8 % of the participating senior medical students felt capable of completing a death certificate29. Not surprisingly, it is mentioned that many physicians reported as their first contact with death certification, the occasion of their first death event30. Educational interventions have resulted in a significant decrease in major but not in minor errors12-13,31. In a recent study, training interventions at eight New York City hospitals led to a decline of reporting heart disease as the cause of death and in more accurate sepsis reporting practices32. Since the role of infection as the primary cause of death is underestimated by current death certificate-based strategies in the USA33, these results are very promising. Educational improvements on the basis of interactive workshops or printed materials, videos and relevant adjustments in the existing programs should be tailored according to the needs and requirements of the medical staff that operate in different environments and conditions.
There are some limitations in this study. No attempt was made to validate the accuracy of the underlying cause of death using medical records or information from autopsies, due to lack of available data. Furthermore, this study refers to a prefecture in southern Greece, where physicians’ attitude and training might differ from place to place, especially in areas with university hospitals and medical schools. It would be of interest to conduct a national multicenter study to estimate the difference in the cause and manner of death in the different regions of Greece.
Conclusions
In this study, major errors were found in most death certificates. Therefore, since death certificates do not accurately describe the cause of death, they cannot be used reliably as routine data for epidemiological research and for planning public health policies. Such low-quality data do not allow comparisons at a local, national and international level as they may merely reflect different practices of death certification between the various regions. The burden of each disease that may activate sequences leading to death should be identified from reliable death certificates. Our results suggest that we are quite far away from this. However, the implementation of educational programs, practices already used in the United States and European countries, may eventually improve the quality and reliability of death certification in Greece.
Conflict of Interest
The authors declare no conflict of interest.
References
- 1.WHO (2012), ICD-10 Interactive Self Learning Tool - Cause of death certificate version, for persons that fill in causes of death on a death certificate. Available at: http://www.moh.gov.cy/moh/ moh.nsf/All/9CE89CE81E91903EC22579C600266A75/$file/Manual%20on%20certification%20of%20causes%20of%20death%20in%20Europe.pdf. last accessed: 18/7/2016.
- 2.Italian National Institute of Statistics. Manual on certification of causes of death in Europe. Rome 2003. Available at: http:// apps.who.int/classifications/apps/icd/icd10training/ last accessed: 18/7/2016.
- 3.Lu TH, Shau WY, Shih TP, Lee MC, Chou MC, Lin CK. Factors associated with errors in death certificate completion. A national study in Taiwan. J Clin Epidemiol. 2001;54:232–238. doi: 10.1016/s0895-4356(00)00299-7. [DOI] [PubMed] [Google Scholar]
- 4.Katsakiori PF, Panagiotopoulou EC, Sakellaropoulos GC, Papazafiropoulou A, Kardara M. Errors in death certificates in a rural area of Greece. Rural Remote Health. 2007;7:822. [PubMed] [Google Scholar]
- 5.Burger EH, van der Merwe L, Volmink J. Errors in the completion of the death notification form. S Afr Med J. 2007;97:1077–1081. [PubMed] [Google Scholar]
- 6.Jordan JM, Bass MJ. Errors in death certificate completion in a teaching hospital. Clin Invest Med. 1993;16:249–255. [PubMed] [Google Scholar]
- 7.Cina SJ, Selby DM, Clark B. Accuracy of death certification in two tertiary care military hospitals. Mil Med. 1999;164:897–899. [PubMed] [Google Scholar]
- 8.Smith Sehdev AE, Hutchins GM. Problems with proper completion and accuracy of the cause-of-death statement. Arch Intern Med. 2001;161:277–284. doi: 10.1001/archinte.161.2.277. [DOI] [PubMed] [Google Scholar]
- 9.Pritt BS, Hardin NJ, Richmond JA, Shapiro SL. Death certification errors at an academic institution. Arch Pathol Lab Med. 2005;129:1476–1479. doi: 10.5858/2005-129-1476-DCEAAA. [DOI] [PubMed] [Google Scholar]
- 10.Nojilana B, Groenewald P, Bradshaw D, Reagon G. Quality of cause of death certification at an academic hospital in Cape Town, South Africa. S Afr Med J. 2009;99:648–652. [PubMed] [Google Scholar]
- 11.Shantibala K, Akoijam BS, Usharani L, Singh HN, Laishram J, Singh TA. Death certification in a teaching hospital--a one year review. Indian J Public Health. 2009;53:31–33. [PubMed] [Google Scholar]
- 12.Myers KA, Farquhar DR. Improving the accuracy of death certification. CMAJ. 1998;158:1317–1323. [PMC free article] [PubMed] [Google Scholar]
- 13.Pandya H, Bose N, Shah R, Chaudhury N, Phatak A. Educational intervention to improve death certification at a teaching hospital. Natl Med J India. 2009;22:317–319. [PubMed] [Google Scholar]
- 14.Agarwal R, Norton JM, Konty K, Zimmerman R, Glover M, Lekiachvili A, et al. Overreporting of deaths from coronary heart disease in New York City hospitals, 2003. Prev Chronic Dis. 2010;7:A47. [PMC free article] [PubMed] [Google Scholar]
- 15.Lakkireddy DR, Gowda MS, Murray CW, Basarakodu KR, Vacek JL. Death certificate completion: how well are physicians trained and are cardiovascular causes overstated? Am J Med. 2004;117:492–498. doi: 10.1016/j.amjmed.2004.04.018. [DOI] [PubMed] [Google Scholar]
- 16.Cheng WS, Wingard DL, Kritz-Silverstein D, Barrett-Connor E. Sensitivity and specificity of death certificates for diabetes: as good as it gets? Diabetes Care. 2008;31:279–284. doi: 10.2337/dc07-1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McEwen LN, Kim C, Haan M, Ghosh D, Lantz PM, Mangione CM, et al. TRIAD Study Group. Diabetes reporting as a cause of death: results from the Translating Research Into Action for Diabetes (TRIAD) study. Diabetes Care. 2006;29:247–253. doi: 10.2337/diacare.29.02.06.dc05-0998. [DOI] [PubMed] [Google Scholar]
- 18.Mühlhauser I, Sawicki PT, Blank M, Overmann H, Richter B, Berger M. Reliability of causes of death in persons with Type I diabetes. Diabetologia. 2002;45:1490–1497. doi: 10.1007/s00125-002-0957-8. [DOI] [PubMed] [Google Scholar]
- 19.German RR, Fink AK, Heron M, Stewart SL, Johnson CJ, Finch JL, et al. Accuracy of Cancer Mortality Study Group. The accuracy of cancer mortality statistics based on death certificates in the United States. Cancer Epidemiol. 2011;35:126–131. doi: 10.1016/j.canep.2010.09.005. [DOI] [PubMed] [Google Scholar]
- 20.Pérez-Gómez B, Aragonés N, Pollán M, Suárez B, Lope V, Llácer A, et al. Accuracy of cancer death certificates in Spain: a summary of available information. Gac Sanit. 2006;20 suppl 3:42–51. doi: 10.1157/13101089. [DOI] [PubMed] [Google Scholar]
- 21.Mathers CD, Fat DM, Inoue M, Rao C, Lopez AD. Counting the dead and what they died from: an assessment of the global status of cause of death data. Bull World Health Organ. 2005;83:171–177. [PMC free article] [PubMed] [Google Scholar]
- 22.Mahapatra P, Shibuya K, Lopez AD, Coullare F, Notzon FC, Rao C, et al. Monitoring Vital Events. Civil registration systems and vital statistics: successes and missed opportunities. Lancet. 2007;370:1653–1663. doi: 10.1016/S0140-6736(07)61308-7. [DOI] [PubMed] [Google Scholar]
- 23.Bhalla K, Harrison JE, Shahraz S, Fingerhut LA; Global Burden of Disease Injury Expert Group. Availability and quality of cause-of-death data for estimating the global burden of injuries. Bull World Health Organ. 2010;88:831–838C. doi: 10.2471/BLT.09.068809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.International Classification of Diseases (ICD) 10th Edition. Available at: http://www.who.int/classifications/icd/en/ last accessed: 18/7/2016.
- 25.Naghavi M, Makela S, Foreman K, O'Brien J, Pourmalek F, Lozano R. Algorithms for enhancing public health utility of national causes-of-death data. Popul Health Metr. 2010;8:9. doi: 10.1186/1478-7954-8-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.O'Donovan BG, Armstrong P, Byrne MC, Murphy AW. Donegal Specialist Training Programme in General Practice. A mixed-methods prospective study of death certification in general practice. Fam Pract. 2010;27:351–355. doi: 10.1093/fampra/cmq012. [DOI] [PubMed] [Google Scholar]
- 27.McAllum C, St George I, White G. Death certification and doctors' dilemmas: a qualitative study of GPs' perspectives. Br J Gen Pract. 2005;55:677–683. [PMC free article] [PubMed] [Google Scholar]
- 28.Lavranos G, Nikolaou A, Koliaki C, Angelidi A, Martinou E, Bakolas G, et al. Comparative assessment of self-reported satisfaction in attaining basic skills in preventive medicine among medical students. Arch Hell Med. 2008;25:184–190. [Google Scholar]
- 29.Franchitto N, Rougé D. Appraisal by Year Six French medical students of the teaching of forensic medicine and health law. Med Sci Law. 2010;50:205–210. doi: 10.1258/msl.2010.010025. [DOI] [PubMed] [Google Scholar]
- 30.Lloyd-Jones DM, Martin DO, Larson MG, Levy D. Accuracy of death certificates for coding coronary heart disease as the cause of death. Ann Intern Med. 1998;129:1020–1026. doi: 10.7326/0003-4819-129-12-199812150-00005. [DOI] [PubMed] [Google Scholar]
- 31.Magrane BP, Gilliland MG, King DE. Certification of death by family physicians. Am Fam Physician. 1997;51:1433–1438. [PubMed] [Google Scholar]
- 32.Ong P, Gambatese M, Begier E, Zimmerman R, Soto A, Madsen A. Effect of cause-of-death training on agreement between hospital discharge diagnoses and cause of death reported, inpatient hospital deaths, New York City, 2008-2010. Prev Chronic Dis. 2015;12:E04. doi: 10.5888/pcd12.140299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Govindan S, Shapiro L, Langa KM, Iwashyna TJ. Death certificates underestimate infections as proximal causes of death in the U.S. PLoS One. 2014;9:e97714. doi: 10.1371/journal.pone.0097714. [DOI] [PMC free article] [PubMed] [Google Scholar]


