Abstract
Aneurysmal subarachnoid hemorrhage (SAH) typically carries a poor prognosis. Growing evidence indicates that overabundant production of nitric oxide (NO) may be responsible for a large part of the secondary injury that follows SAH. Although SAH modulates the activity of all three isoforms of nitric oxide synthase (NOS), the inducible isoform, NOS-2, accounts for a majority of NO-mediated secondary injuries after SAH. Here, we review the indispensable physiological roles of NO that must be preserved, even while attempting to downmodulate the pathophysiologic effects of NO that are induced by SAH. We examine the effects of SAH on the function of the various NOS isoforms, with a particular focus on the pathological effects of NOS-2 and on the mechanisms responsible for its transcriptional upregulation. Finally, we review interventions to block NOS-2 upregulation or to counteract its effects, with an emphasis on the potential therapeutic strategies to improve outcomes in patients afflicted with SAH. There is still much to be learned regarding the apparently maladaptive response of NOS-2 and its harmful product NO in SAH. However, the available evidence points to crucial effects that, on balance, are adverse, making the NOS-2/NO/peroxynitrite axis an attractive therapeutic target in SAH.
Keywords: Heparin, nitric oxide (NO), NOS-1, NOS-2, NOS-3, subarachnoid hemorrhage (SAH)
Introduction
Subarachnoid hemorrhage (SAH) causes profound morbidity and mortality in approximately 30,000, often otherwise healthy, Americans yearly.[1] While the hemorrhage is responsible for severe, frequently fatal initial brain injury, many surviving patients undergo a secondary decline in the days following the insult. This well-established phenomenon of delayed neurologic deficit (DND) accounts for approximately one-third of the morbidities and mortalities associated with SAH.[2] Importantly, because of the delay between the ictal event and development of DND, this secondary injury is thought to be preventable. A comprehensive mechanistic understanding of DND would allow for the development of targeted therapies to improve the poor outcomes of many patients afflicted with SAH.
Despite years of study, the mechanisms of DND remain incompletely understood. Early surgical and radiographic observations of pathological blood vessel narrowing following SAH supported a vasospasm theory of DND whereby blood products in the subarachnoid space lead to vessel narrowing, resulting in reduced blood flow, cerebral ischemia, and ultimately infarction. While vasospasm undoubtedly accounts for some aspects of DND, recently obtained clinical evidence challenges its predominance. Nimodipine, the only formally approved therapy to prevent DND following SAH, is largely ineffective at preventing angiographic vasospasm.[3] Conversely, clazosentan, a medication that is highly effective at preventing radiographic vasospasm, does not improve clinical outcome.[4] Other mechanisms of DND include microthrombosis, free radical injury, loss of cerebral autoregulation, and inflammation.[5] The modern view is that DND, rather than being a simple problem of vascular dysregulation, actually results from a confluence of multiple pathological processes.
One molecule that has emerged at the center of this process is nitric oxide (NO).[6] Originally characterized as “endothelium-derived relaxing factor,” NO is a ubiquitous signaling molecule that has a crucial role in a variety of physiological processes.[7,8,9] In the vasculature, NO is important not only as a vasodilator but also for maintaining endothelial function, preventing vascular smooth muscle cell growth, inhibiting platelet aggregation, and blocking leukocyte adhesion. Furthermore, NO is an important part of the inflammatory process — phagocytes generate large quantities of NO in response to inflammatory stimuli, with NO acting as a potent cytotoxic agent. Moreover, NO reacts with superoxide to form peroxynitrite, a powerful biological oxidant with the potential to mediate significant bystander tissue injury.[10] Given that disordered vessel contractility, endothelial dysfunction, inflammation, and free radical injury are all considered to be central to the broader process of DND, abnormal NO metabolism is uniquely positioned to serve as a central mediator of DND in SAH.
The potentially harmful effects of NO in SAH have emerged from a broader trend in studies of neuropathology, which have shown deleterious effects of NO in neurodegeneration,[11] traumatic brain injury,[12] and stroke.[13] The generation of NO in excessive, destructive quantities following a brain injury results largely from activation of the inducible isoform of nitric oxide synthase (iNOS or NOS-2), which occurs in response to inflammatory stimuli. Given its broad role in various CNS pathologies, the mechanisms controlling NOS-2 upregulation have been studied extensively. The object of this review is to situate the regulation of NOS-2 within the broader pathology of SAH to discuss the molecular mechanisms that result in its upregulation and to explore methods to ameliorate the effects of NOS-2 upregulation, with the hope of fostering the development of novel therapeutics to target the NOS-2/NO/peroxynitrite axis.
Physiologic Roles of Nitric Oxide: Overview
Nitric oxide in vascular tone
NO is best known for its role in vasodilation. In response to a wide variety of physiologic stimuli including shear stress, platelet-derived factors and cytokines, vascular endothelial cells upregulate NOS, which generates NO from the amino acid, L-arginine.[14] Once generated, NO readily diffuses into adjacent smooth muscle cells of the vasculature where it interacts with soluble guanylate cyclase to generate cyclic GMP, initiating a chain of secondary signaling events that culminate in smooth muscle cell relaxation and dilation of blood vessels. This mechanism of action is present throughout the body but is of particular importance in the vasculature of the brain where NO signaling tightly controls cerebral blood flow.[15,16]
Apart from its direct vasodilatory actions, NO plays a significant role in modulating endogenous vasoconstrictive agents. Endothelin-1 (ET-1), an endogenous small peptide vasoconstrictor of particular importance in SAH, is one such molecule.[17] Pharmacologic blockade of NO production in both rats[18] and humans[19] induces significant systemic vasoconstriction and concurrent hypertension that is partially reversed by the blockade of endothelin signaling, suggesting an important antagonistic role between these two molecules in normal physiology. Mechanisms for this interaction are complex, including both direct and downstream inhibitions of ET-1 signaling[20] and modulation of ET-1 transcription.[21,22] Similarly, NO has important antagonistic interactions with a variety of small molecule vasoconstrictors. Experimental evidence suggests that endothelial NO production counteracts adrenergic signaling in the peripheral vasculature of both rats[23,24] and humans.[25] In the pulmonary vasculature, NO inhibits the vasoconstrictive actions of serotonin via chemical modification of its receptor.[26] Finally, NO inhibits cerebral endothelial production of thromboxane, a potent vasoconstrictor.[27] Thus, NO not only acts as a vasodilator but also provides a physiologic counterbalance to a variety of vasoconstrictors, a set of findings particularly relevant in diseases of increased vasoconstrictive tone such as SAH.
Nitric oxide in inflammation
NO plays an important role in inflammation. Generated by phagocytes such as macrophages and neutrophils in response to inflammatory stimuli, NO is a potent antimicrobial, both on its own and as a precursor to the powerful oxidant, peroxynitrite, which mediates a variety of antimicrobial effects.[28,29] Multiple lines of evidence derived from preclinical and clinical researches suggest a significant role of NO in the defense against a variety of pathogens including bacteria, protozoa, and fungi.[30] Although essential for the host defense, NO can induce bystander damage to the body's own tissues, as occurs in the excessive inflammatory response of sepsis. Similar to its role in vasodilation, the role of NO in inflammatory processes is ubiquitous throughout the body.
Nitric Oxide Synthases
Throughout the body, cells such as macrophages, neurons, and endothelial cells generate NO primarily through a class of enzymes known collectively as nitric oxide synthases (NOS). Three isoforms of this enzyme exist, NOS-1, NOS-2, and NOS-3. Although all share a common synthetic mechanism, the three isoforms differ in the mechanisms of expression, predominant cell type of expression, and physiologic roles.[31] Starting from the precursor arginine, the NOS enzymes catalyze serial nicotinamide adenine dinucleotide phosphate (NADPH)-mediated oxygenation of the guanidine residue to yield citrulline and NO. Both the NOS-1 and NOS-3 isoforms require physiologically elevated levels of calcium to function. In contrast, NOS-2 uniquely binds to calmodulin to allow continued function even in cellular environments with low Ca2+ concentrations, allowing it to function as a “calcium independent” isoform.
The NOS isoforms differ significantly in both the predominant cell type that expresses them and the mechanism of expression.[7] NOS-1, or neuronal NOS (nNOS), is widely expressed by neurons of both the central and peripheral nervous systems in humans and other vertebrates. A constitutively expressed enzyme, its activity is modulated primarily by intracellular calcium. The NO generated by NOS-1 is important for long-term potentiation, neuronal plasticity, and central regulation of blood pressure.
NOS-3, or endothelial NOS (eNOS), is primarily expressed by vascular endothelial cells. NOS-3, like NOS-1, is constitutively expressed and depends primarily on the modulation of intracellular calcium for control of its activity. The NO generated by NOS-3 acts as a vasodilator, playing important roles in both systemic and cerebral blood flows but it also inhibits platelet aggregation and leukocyte adhesion.
NOS-2, or inducible NOS (iNOS), differs from its counterparts as it is not constitutively expressed. Instead, expression of NOS-2 relies on various signaling events such as cytokines to induce its expression. Although principally expressed in phagocytes such as macrophages,[32] NOS-2 can be induced in a wide variety of cell types including microglia and astrocytes.[33] Once induced, NOS-2 continues to produce NO regardless of the calcium concentration, allowing for NO production 100-1,000 times greater than the constitutive isoforms. NOS-2 activity is ultimately terminated only by degeneration of the enzyme. This ability to generate large quantities of NO is consistent with the role of NOS-2 in inflammatory processes as a mediator of cytotoxicity. Thus, while all NOS isoforms generate the same product, NO, the different isoforms play decisively different physiologic roles.
Nitric Oxide and Pathologic Vasoconstriction Following Subarachnoid Hemorrhage
One hallmark of aneurysmal SAH is vasospasm, the delayed development of marked pathologic constriction of the intracerebral vessels. A number of molecular signals are thought to mediate this constriction. The endothelin molecules, particularly ET-1, represent the best studied class of molecules in this regard. Initial studies of ET-1 identified a strong correlation between elevated cerebrospinal fluid (CSF) concentrations of ET-1 and the development of vasospasm in patients with SAH.[34] Subsequent work identified a number of plausible mechanisms to explain the observed rise in ET-1 including hemoglobin-triggered synthesis in vascular smooth muscle cells,[35] ischemia-induced synthesis in astrocytes,[34] and inflammation-provoked production in infiltrating leukocytes.[36] Clinical trials of the ET-1 antagonist, clazosentan, confirm the primacy of ET-1 in mediating vasospasm. Although ultimately ineffective at improving outcomes in SAH, ET-1 blockade nevertheless led to a marked reduction in vasospasm in patients with SAH.[4] In addition to ET-1, a number of other molecular signals may contribute to vasospasm. Thromboxanes present an important class of platelet-derived vasoconstrictors with a potential role in vasospasm. Following SAH, vascular endothelial cells demonstrate increased contractility in response to thromboxane receptor activation[37] and platelet release of thromboxane is augmented in patients with vasospasm following SAH.[38] Consistent with these findings, inhibition of thromboxane synthesis improves vasospasm in a canine SAH model.[39] Other lines of experimental evidence suggest that serotonin, another platelet-derived vasoconstrictor, plays a role in the development of vasospasm following SAH. Intracisternal injection of platelet-rich plasma in dogs induces vasospasm in a manner analogous to SAH, a finding correlated with an increase in perivascular serotonergic neurons.[40] In rats, experimental SAH upregulates arterial expression of serotonin receptors, with a concurrent increase in contractility in response to serotonin.[41] Consistent with these experimental observations, use of selective serotonin uptake inhibitors is a risk factor for severe vasospasm in patients with SAH.[42] Thus, SAH induces arterial vasospasm by modulating a number of vasoconstrictive signaling pathways.
Given the importance of NO as a physiologic counterbalance to endogenous vasoconstrictors, the marked augmentation of vasoconstrictive signals following SAH implies that even a mild decrease in NO in the perivascular compartment could lead to significant vessel contraction. In consistence with this hypothesis, experimental evidence derived from goat models suggests that loss of endothelial NO availability partially explains the observation of increased ET-1-induced vasoconstriction following experimental SAH.[43] Analogous experiments evaluating enhanced serotonin vasoconstriction following SAH demonstrate similar findings.[44] Blood products in the subarachnoid space are thought to reduce NO bioavailability by a variety of mechanisms including malfunction of NO-generating enzymes,[45] production of NOS-inhibiting metabolites,[46] and sequestration of NO by the vast amounts of extracellular hemoglobin acting as an NO “sink.”[47,48,49] In accordance with this hypothesis, NO-based therapies such as intracarotid infusion of NO donors in primates,[50] intracisternal injection of NO donors in rabbits,[51] and intrathecal administration of the NO precursor nitroprusside in humans[52] all ameliorate SAH-associated vasospasm.
Although a loss of NO bioavailability fits well with the aforementioned data, direct experimental examinations of NO production following SAH suggest a more complex metabolism than simple loss of basal production. Although NO production does appear to be globally decreased immediately following experimental SAH, there is a relatively rapid restoration toward normal levels in most areas of the brain in the hours following hemorrhage.[53] Studies evaluating the effects of inhibition of NO synthesis on cerebral blood flow following SAH suggest similar kinetics,[54] namely, an immediate loss and relatively rapid restoration of endothelial NO production. A three-phase model has emerged in which SAH initially results in a hyperacute loss of NO availability followed by restoration to normal levels and then augmentation of production over the next 72 h.[6] This model challenges the hypothesis that vasospasm following SAH results in the simple loss of NO availability.
Nitric Oxide and its Metabolites Following Subarachnoid Hemorrhage In Humans
Given that the early prevailing theories of DND were dominated by vasospasm, reports of an apparent “increase” in NO bioavailability in SAH were unexpected. Although direct measurement of NO production following SAH is not practical, given its reactivity and short biological half-life, several groups evaluated the levels of its metabolic products, nitrites, and nitrates, along with the levels of these metabolites vis-à-vis vasospasm and clinical outcomes. Studies of CSF almost uniformly demonstrated elevated levels of NO metabolites. When evaluating CSF levels of NO metabolites in patients with aneurysmal SAH, Suzuki et al.[55] noted an increase at all time points compared to healthy controls, with the degree of increase correlating with the quantity of cisternal blood. Several other studies yielded similar findings.[56,57,58] Only one study to date identified marginally lower levels of NO metabolites in the CSF of SAH patients compared to healthy controls[59] although the timing and means of CSF collection in this study were not well-documented.
The finding of elevated NO metabolites in the CSF following SAH is now relatively well-established but the relationship between this finding and vasospasm or DND is still to be resolved. While some groups report an increase in NO products in the CSF that correlates with vasospasm,[56,59] others report a relative decrease in NO products that correlates with vasospas,[55] and there are still others who report no clear relationship.[57,58] In a rat model of SAH, evidence of peroxynitrite-mediated perivascular injury was found on a pathological review of rats demonstrating vasospasm but not in those without vasospasm,[60] a finding consistent with a role of excessive NO in mediating vasospasm. To our knowledge, a comparable finding has not been reported in human arteries.
At the very least, the finding of elevated NO metabolites in the CSF suggests that early hypotheses postulating reduced bioavailability of NO as being responsible for DND were overly simplistic. Recent theories of DND postulate that the presence of blood and blood products in the subarachnoid space initiates multiple pathophysiological events including not only vasospasm but also inflammatory and free radical injury to the adjacent cortex. NO is an important mediator of the inflammatory response, and in the context of inappropriate or exaggerated inflammation, excess NO production can be harmful. Reactive nitrogen species (RNS), especially peroxynitrite, are capable of disrupting cellular metabolism,[61] irreversibly damaging DNA,[62] and ultimately causing cell death.[63]
Apart from examining CSF, another approach to determine the role of NO in DND has been to examine NO metabolites in microdialysis samples of cortical tissues. Microdialysis of parenchymal tissues has successfully demonstrated a relationship between NO metabolites and brain oxygenation.[64] Some microdialysis studies report an association between locally elevated NO metabolites and poor outcomes,[65] whereas others fail to find such a relationship.[66]
The aforementioned conflicting findings in humans regarding NO metabolites and DND should perhaps not be surprising. The baseline characteristics of patients including the severity and location of SAH, comorbidities and the medications used to treat them, the timing of CSF or dialysate sampling, cohort sizes, and numerous other variables were invariably poorly controlled. It is likely that different brain compartments are differentially affected by NO — the vascular smooth muscle may well experience a reduced bioavailability, whereas inflamed cortical tissues may well experience an overabundance of NO. CSF represents a distant and imprecise proxy for intraparenchymal activity of NO. As a bulk substrate, CSF cannot capture important compartmental, regional, cellular, and temporal variations in NO production that may be crucially important for biological activity. Similarly, the volume of tissue sampled in microdialysis studies is necessarily small and similar to CSF; dialysate cannot capture important compartmental, regional, and cellular variations in NO production. The resolution of these discrepant findings and the advancement in understanding of the undoubtedly complex roles of NO in SAH await technical advances in methodologies that will permit global and regional assessments of NO or its metabolites at high spatial and temporal resolutions in the human brain.
Nitric Oxide Synthase Expression Following Subarachnoid Hemorrhage
The constitutive NOS isoforms (NOS-1, NOS-3) undergo complex changes in regulation following SAH. NOS-1 is primarily downregulated following SAH,[67,68] with loss of function in adventitial nerve fibers correlating with the degree of vasospasm. NOS-3, in contrast, exhibits a more complex pattern of expression following SAH, with decreases in endothelial expression[69,70] and increases in parenchymal expression.[45,69,71] The clinical ramifications of these changes are unclear, as both NOS-1 and NOS-3 are primarily controlled at the posttranslational level by intracellular calcium. The metabolic environment of the CNS following SAH may induce malfunction of these enzymes, particularly NOS-3.[46] The general consensus is that loss of enzymatic function of these constitutive isoforms contributes to the pathophysiology of SAH via impaired vasodilation, a topic that is the subject of an excellent recent review.[72]
In contrast to the constitutive isoforms of NOS, inducible NOS (NOS-2) undergoes unambiguous upregulation following SAH. In a rat model of SAH induced by endovascular perforation, NOS-2-positive mononuclear cells and neutrophils infiltrate the subarachnoid space as early as 24 h after SAH.[73] The areas of highest NOS-2 expression correlate closely with histological evidence of peroxynitrite-mediated cell injury and vasospasm.[74] In the same model, blockade of NOS-2 with the selective inhibitor, aminoguanidine, prevents the development of post-SAH vasospasm. A murine endovascular model of SAH produces similar results, with upregulation of NOS-2 in both the vasculature and cortex.[75] Overexpression of CuZn superoxide dismutase in this model protects against SAH-induced vasospasm and results in decreased NOS-2 expression,[76] further supporting the pathological role of NOS-2. In a rat model of vasospasm induced by double injection of blood into the cisterna magna, the degree of vasospasm correlates with the degree of NOS-2 expression.[77]
The findings in these models of SAH are consistent with the limited clinical data available. In an evaluation of NOS isoform expression in cerebral tissues taken during clipping of a ruptured aneurysm, NOS-2 expression was significantly increased compared to unruptured controls and unique among NOS isoforms; NOS-2 hyperexpression alone correlated with vasospasm.[71] Thus, SAH rapidly induces NOS-2, best accounting for clinical studies demonstrating elevated NO production following SAH.
Mechanisms of Nos-2 Upregulation Following Subarachnoid Hemorrhage
Under normal conditions, NOS-2 upregulation represents an appropriate response to infectious organisms, allowing for the clearance of pathogens via the production of cytotoxic levels of NO. Proinflammatory agents such as lipopolysaccharide, free radicals, and cytokines are principal inducers of NOS-2 upregulation. SAH results in the appearance of numerous proinflammatory molecules derived from blood and blood breakdown products such as thrombin, methemoglobin, heme, and Fe3+. In addition, the abrupt increase in intracranial pressure following aneurysmal SAH can induce global cerebral ischemia, with possible reperfusion injury. These events ultimately contribute to NOS-2 expression through several mechanisms, as given below.
Toll-like receptors
Toll-like receptors (TLRs) are a first-line of defense against pathogens and play an essential role in mediating innate and adaptive immune responses.[78,79] TLR-4 is expressed by microglia and to a lesser extent, by neurons and astrocytes following SAH.[80] Hemoglobin breakdown products including methemoglobin,[81,82,83] heme,[84,85] and hemin[86] can activate TLR-4. Of these, methemoglobin alone, due to its high solubility, rapidly diffuses throughout the CSF, enabling global activation of TLR-4 throughout the CNS. Experiments in rats,[87] rabbits,[88] and mice[80,89] all demonstrate evidence of TLR-4 activation following experimental SAH. In ischemic CNS injury, TLR-4 activation induces the expression of NOS-2, and TLR-4 knockout mice demonstrate decreased expression of NOS-2 following experimental stroke.[90,91] In a rat model of hypoxia, knockdown of TLR-4 results in reduced NOS-2 expression following hypoxic injury.[78] Given the presence of TLR-4 ligands in the form of hemoglobin metabolites, upregulation of TLR-4 receptors, and the capacity of TLR-4 to induce NOS-2, activation of TLR-4 forms a plausible mechanism to account for NOS-2 upregulation following SAH. However, direct experimental confirmation of this phenomenon is lacking.
Cytokines
Multiple inflammatory cytokines are upregulated and are thought to mediate delayed injury following SAH including interleukin-1b (IL-1β)[92,93] and tumor necrosis factor (TNF).[94,95] These proinflammatory cytokines can upregulate NOS-2.[96] IL-1β may be particularly relevant to SAH — in a cell culture model of SAH employing rat vascular smooth muscle cells, the combination of hemoglobin and IL-1β induces NOS-2 transcription, with hemoglobin markedly augmenting IL-1β induction of NOS-2 in spite of hemoglobin's relatively poor ability to upregulate the enzyme by itself.[97] The inflammatory response to SAH rather than the blood products themselves may be responsible for the upregulation of NOS-2 following SAH[97] although further work along these lines is required for clarification.
Reactive oxygen species
The reactive oxygen species (ROS) and free radicals generated following SAH play an important role in NOS-2 upregulation. ROS derive from several sources following SAH including disrupted cellular respiration, extracellular methemoglobin in the subarachnoid space, and upregulation of certain enzymes including NOS-2 itself.[98] Several lines of evidence demonstrate the importance of oxidative stress in NOS-2 induction following SAH. In a mouse cell culture model of SAH, cerebral endothelial cells exposed to ferrous citrate complexes upregulate NOS-2.[99] The addition of the antioxidant N-acetyl cysteine to the cultures blocks NOS-2 upregulation, arguing for the importance of free radicals in inducing NOS-2. More direct evidence for the role of ROS in mediating NOS-2 induction following SAH derives from transgenic mice engineered to overexpress the potent antioxidant enzyme CuZn superoxide dismutase (CuZn-SOD).[75] Immunohistochemical studies 24 h after SAH demonstrate decreased NOS-2 expression in the vascular wall of SOD-transgenic mice compared to wild-type controls.[75] Taken together, these experiments demonstrate the importance of ROS in NOS-2 regulation following SAH.
Ischemia
Immediately following aneurysmal rupture, the brain may experience transient global ischemia, as intracranial pressure equilibrates with mean arterial pressure.[100] Clinically, this period of globally diminished perfusion corresponds to loss of consciousness, and has been shown to be highly predictive of mortality and delayed cerebral ischemia following SAH.[101] Transient global cerebral ischemia upregulates NOS-2 in rodents.[102,103,104] Although direct examination of the effects of ischemia on NOS-2 expression in the context of SAH does not exist, ischemic injury presents a plausible source for NOS-2 elevation following SAH.
Proinflammatory transcription factors that upregulate NOS-2 after subarachnoid hemorrhage
While multiple agents and conditions present in the CNS contribute to upregulation of NOS-2 following SAH, the upregulation of NOS-2 ultimately depends on activation of one or more transcriptional pathways, the most pertinent of which are reviewed here.
Nuclear factor-kB
Nuclear factor-κB (NF-κB) is a transcription factor closely associated with NOS-2. The promoter region for the human NOS-2 gene contains multiple canonical NF-kB binding sites.[105] Furthermore, small molecule and peptide inhibitors of NF-κB prevent upregulation of NOS-2 in response to known stimulants, consistent with a central role of this transcription factor in NOS-2 expression.[106,107] As a constitutively expressed factor, NF-κB is bound in the cytosol of cells by its inhibitor, IkB. IkB is degraded as a result of a variety of inflammatory signaling pathways, thereby activating NF-kB and allowing it to translocate to the nucleus. Activation of NF-κB occurs in multiple models of SAH.[88,108,109] Multiple triggers including TLR-4 activation, cytokine signaling, and ROS induce NOS-2 expression via activation of NF-κB in various models of SAH.[33] In consistence with this understanding, blockade of NF-κB by various agents including estradiol,[110] N-acetylcysteine,[99] and overexpression of superoxide dismutase[75] leads to decreased expression of NOS-2 following SAH.
Hypoxia-inducible factor 1
Hypoxia-inducible factor 1 (HIF-1) is a transcription factor that is activated in response to hypoxia.[111,112] A heterodimeric DNA-binding complex that consists of one α and one β subunit, HIF-1 binds to the promoter elements of target genes that promote an adaptive response to hypoxia, such as erythropoietin and vascular endothelial growth factor.[113,114,115] While constantly degraded under aerobic conditions, under hypoxic conditions degradation of the HIF-1α subunit ceases, allowing formation of the active heterodimer and transcriptional activation of HIF responsive genes.[116,117] NOS-2 transcription is under the control of HIF-1.[118,119] Given the possibility of hypoxia secondary to hypoperfusion immediately following the ictus as well as the possibility of later ischemia secondary to vasospasm, upregulation of HIF-1 following SAH seems likely. Experimental evidence is largely consistent with this hypothesis, with multiple models demonstrating an increase in cerebral HIF-1 activity following SAH.[120,121] Thus, elevated levels of HIF-1 may contribute to the observed elevation of NOS-2 after SAH.
Nuclear factor of activated T-cells
Closely related to NF-κB, nuclear factor of activated T-cells (NFAT) is a transcription factor most commonly associated with adaptive immunity and T cell activation.[122] During ischemic brain injury, there is an increase in intracellular calcium concentration leading to activation of calcineurin, a calcium-dependent phosphatase, which subsequently activates NFAT via dephosphorylation.[123] NFAT isoform expression has been documented in diverse cell populations of the CNS such as neurons, astrocytes, macrophages, and microglia.[124,125,126,127] While the relationship between NFAT and NOS-2 is poorly explored in the CNS, experimental evidence in other cell types suggests a close connection between the activation of NFAT and NOS-2 induction. Activation of calcineurin in cardiomyocytes potently induces NOS-2 via a NFAT-mediated mechanism[128] while inhibition of NFAT blocks NOS-2 upregulation in activated macrophages.[129] Although activation of calcineurin-NFAT activity has not been directly studied in SAH, it may plausibly contribute to upregulation of NOS-2.
Nos-2 Therapeutics After Subarachnoid Hemorrhage
Blockade of NOS-2 upregulation
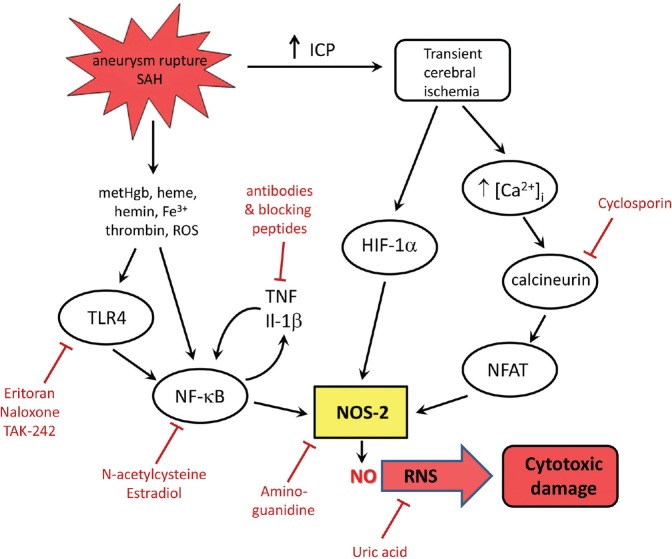
Given NOS-2's essential lack of posttranslational controls, prevention of NOS-2 upregulation represents an attractive therapeutic strategy. Several therapeutic targets are available to block NOS-2 upregulation following SAH [Figure 1]. Blockade of TLR-4 represents one such strategy, as TLR-4 ligation activates several pathways culminating in NOS-2 upregulation including the activation of NF-κB through proinflammatory signaling cascades, induction of cytokines in microglia, and activation of phagocytes with subsequent generation of ROS. Blockade of TLR-4 can be achieved through a variety of small molecule antagonists such as eritoran[130] and TAK-242.[131] The opioid antagonist, naloxone, which also blocks TLR-4,[132] may represent an interesting possibility as it is well-established clinically and has shown efficacy in treating vasospasm in a small case series.[133] Clinically approved peroxisome proliferator-activated receptor γ (PPAR-γ) agonists such as rosiglitazone downregulate TLR-4 in both cell culture[134] and in animal models[135] of SAH.
Figure 1.
Inflammatory and ischemic cascades induced by subarachnoid hemorrhage that lead to NOS-2 upregulation. Subarachnoid hemorrhage (SAH) results in extravasation of large amounts of blood into the subarachnoid space. Erythrocytes lyse, releasing hemoglobin metabolites such as methemoglobin, heme and hemin, which act as TLR-4 ligands, activating NF-kB signaling, causing production of inflammatory cytokines, and upregulating NOS-2 expression. Aneurysmal rupture and vasospasm can cause transient cerebral ischemia, which upregulates HIF-1-dependent genes including NOS-2. Cerebral ischemia increases intracellular Ca2+ concentrations, activating calcineurin-NFAT signaling, which upregulates NOS-2. Upregulation of NOS-2 generates excess NO and peroxynitrite, which mediate significant bystander cellular injury. Several of these pathways are amenable to blockade or modulation, as illustrated
Cytokines produced by activated microglia and infiltrating inflammatory cells are also possible targets for reducing NOS-2 expression. Blockade of inflammatory cytokines such as TNF using antibodies[136] or IL-1β using small peptides[92] has demonstrated preclinical efficacy in preventing neurologic injury following SAH.
Given the variety of elements in the CNS that upregulate NOS-2 following SAH, targeting any single one may not be entirely effective in preventing NOS-2 upregulation. As such, blockade of the transcription factors responsible for NOS-2 upregulation may present a viable strategy. Given its role as the principal upstream mediator of NOS-2 expression in SAH, NF-κB seems an obvious target. Several compounds demonstrating preclinical benefit in SAH including the hormone estradiol[137] and the antioxidant N-acetyl cysteine[138,139] exploit this mechanism to block NOS-2 upregulation. However, one potential problem with NF-κB blockade is timing. Statins, for example, reduce NOS-2 expression via a NF-κB dependent mechanism.[140] However, while statin therapy effectively blocks NF-κB activation[141] and NOS-2 upregulation[142] when given as a pretreatment, its effects on NOS-2 are lost when given immediately following SAH. Also, in cerebral ischemia and most likely other forms of acute CNS injury, NF-κB is “Janus-faced,” responsible not only for early adverse effects but also delayed beneficial effects,[143] rendering broad inhibition potentially deleterious.
Blockade of HIF-1 may also be considered since HIF-1 activators enhance NOS-2 production.[118] However, it is unlikely that targeting HIF-1 will be a viable therapeutic strategy due to off-target effects on potentially beneficial molecules under control of HIF-1 such as erythropoietin.[144] Also, increased HIF-1 activity is required for the therapeutic effects of agents such as isoflurane[145] and deferoxamine[120] in preclinical models of SAH. The use of NOS-2 inhibitors in conjunction with HIF-1 activators or attempts to uncouple NOS-2 production from HIF-1 activation could be of potential benefit although such approaches remain untried.
Blockade of NFAT activation via calcineurin inhibition provides another potentially attractive approach, given the regular use of calcineurin inhibitors such as cyclosporine in transplant medicine. These same drugs block NOS-2 upregulation through an NF-κB-independent mechanism.[146,147] Cyclosporin prevents SAH-induced neurologic injury and vasospasm in several preclinical models.[148,149] However, clinical experience with cyclosporine is conflicting, as one early trial reported no apparent benefit of cyclosporin for the treatment of vasospasm[150] while another pilot study reported some benefit in neurologic status with early cyclosporine administration following SAH.[151] Further research is needed to determine if this mode of action can be successfully translated to the clinic.
Inhibition of NOS-2 activity
Given its pernicious role in SAH, direct blockade of NOS-2 presents an attractive therapeutic option. One such experimental agent is aminoguanidine, a selective NOS-2 inhibitor originally developed for preventing diabetic nephropathy.[152] Experimental work suggests that aminoguanidine may be an effective therapeutic agent in SAH. Employing an endovascular perforation model of SAH in rats, Sayama et al.[74] found that aminoguanidine ameliorated vasospasm following SAH. Similarly, treatment of rabbits with aminoguanidine following experimental SAH significantly reduced the severity of vasospasm.[153] Other NOS-2 inhibitors remain essentially unstudied in the context of SAH but the success of aminoguanidine in experimental studies suggests that NOS-2 inhibition may be a valid strategy to prevent secondary injury following SAH.
Apart from preventing excess NO formation via NOS-2 blockade, counteracting the deleterious effects of ROS and RNS may present additional useful therapeutic strategies. Given the prominent role of oxidative stress in SAH, a number of antioxidants have been studied as potential therapeutics.[98] While a review of antioxidants in SAH is beyond the scope of this article, one class of RNS agents, peroxynitrite scavengers, bears note. In theory, this class of agents could potentially neutralize peroxynitrite while allowing NO to perform important physiologic roles such as vasodilation. Although poorly studied in the context of SAH, peroxynitrite scavengers such as uric acid have demonstrated efficacy in other pathologies involving NOS-2 including MS[154] and stroke.[155]
Pleiotropic Therapeutics
Given the complex nature of NOS-2 upregulation following SAH, approaches targeting any single component of the NOS-2/NO/peroxynitrite axis in SAH may be inadequate. Statins, a class of medications traditionally associated with cardiovascular disease, present one such therapeutic class. Apart from preventing NF-κB activation and concurrent NOS-2 upregulation, statins also reduce ROS and peroxynitrite formation[142] and downregulate IL-1β production[156] following SAH.
Despite their ability to address multiple aspects of NOS-2-mediated pathology, statins have had a disappointing clinical record in SAH. Although initial clinical studies suggested improved outcomes, more recent randomized trials have failed to show a benefit with regard to the rates of death or poor neurologic outcome.[157,158,159] One reason for this failure may be the timing of statin therapy — although preclinical studies demonstrate the benefit of statin therapy following experimental SAH, the effects on vasospasm and neurologic injury were diminished when compared to treatment prior to SAH despite the relatively rapid (30 min) dosing.[45,160] Whether these effects persist with dosing at later times is not clear.
Another pleiotropic agent of interest is heparin, which mediates a variety of anti-inflammatory and antioxidant effects. Heparin can bind numerous inflammatory cytokines and chemokines, and block the activation of NF-κB.[161] In a rat model of SAH, treatment with a nonanticoagulating dose of heparin provides a significant reduction in neural inflammation and cytokine production including IL-1β.[162] Given its potent anti-inflammatory effects, the ability of heparin to reduce NOS-2 induction in response to inflammation both in vitro and in vivo should not be surprising.[163,164] In a rat model of SAH, low-dose heparin is a powerful inhibitor of NOS-2 expression (Simard et al., unpublished). Moreover, heparin can act as an antioxidant and could theoretically prevent ROS/RNS-mediated injury through a variety of mechanisms.[165] In consistence with these findings, early clinical evaluation of heparin in patients with SAH at high risk for DND demonstrated significant promise with regard to preventing vasospasm, infarction, and neurologic deterioration.[166] Thus, heparin and heparinoids provide a promising class of therapeutic intervention for NOS-2-mediated pathology in SAH, addressing both the mechanisms that increase NOS-2 production as well as ameliorating the effects of increased ROS/RNS production.
Summary and Perspectives
Excessive NO production plays a significant role in secondary injury following SAH. However, given the diametrically opposed functions of NO following SAH, including its indispensable role as vasodilator versus its cytotoxic effects, complete blockade of NO production is inadvisable. Fortunately, the pathological increase in NO following SAH can be attributed largely to the activity of NOS-2, making this isoform a preferred target.
The increase in activity of NOS-2 is due to transcriptional upregulation of the enzyme induced by the proinflammatory environment of SAH. Once upregulated, NOS-2 is essentially free of posttranslational controls, and continues to generate cytotoxic amounts of NO until the enzyme is degraded. Several attractive strategies present themselves for targeting NOS-2 [Figure 1] although to date none has been successfully translated. Among the more promising approaches are blockade of NOS-2 upregulation, for example using TLR-4 antagonists, blockade of the enzyme itself using specific NOS-2 inhibitors, prevention of NO-induced bystander injury using peroxynitrite scavengers, and the use of pleiotropic agents such as heparin. As mechanistic understanding of NOS-2 upregulation following SAH improves, newer innovative therapies acting on the NOS-2/NO/peroxyinitrite axis are anticipated.
Financial support and sponsorship
This work was supported in part by grants from the National Heart, Lung, and Blood Institute (HL082517) and the National Institute of Neurological Disorders and Stroke (NS061808) to JMS, and by a Scientist Development Grant (13SDG14370030) from the American Heart Association to CMH.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Shea AM, Reed SD, Curtis LH, Alexander MJ, Villani JJ, Schulman KA. Characteristics of nontraumatic subarachnoid hemorrhage in the United States in 2003. Neurosurgery. 2007;61:1131–8. doi: 10.1227/01.neu.0000306090.30517.ae. [DOI] [PubMed] [Google Scholar]
- 2.Roos YB, de Haan RJ, Beenen LF, Groen RJ, Albrecht KW, Vermeulen M. Complications and outcome in patients with aneurysmal subarachnoid haemorrhage: A prospective hospital based cohort study in the Netherlands. J Neurol Neurosurg Psychiatry. 2000;68:337–41. doi: 10.1136/jnnp.68.3.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Philippon J, Grob R, Dagreou F, Guggiari M, Rivierez M, Viars P. Prevention of vasospasm in subarachnoid haemorrhage. A controlled study with nimodipine. Acta Neurochir (Wien) 1986;82:110–4. doi: 10.1007/BF01456369. [DOI] [PubMed] [Google Scholar]
- 4.Macdonald RL, Higashida RT, Keller E, Mayer SA, Molyneux A, Raabe A, et al. Randomized trial of clazosentan in patients with aneurysmal subarachnoid hemorrhage undergoing endovascular coiling. Stroke. 2012;43:1463–9. doi: 10.1161/STROKEAHA.111.648980. [DOI] [PubMed] [Google Scholar]
- 5.Budohoski KP, Guilfoyle M, Helmy A, Huuskonen T, Czosnyka M, Kirollos R, et al. The pathophysiology and treatment of delayed cerebral ischaemia following subarachnoid haemorrhage. J Neurol Neurosurg Psychiatry. 2014;85:1343–53. doi: 10.1136/jnnp-2014-307711. [DOI] [PubMed] [Google Scholar]
- 6.Sehba FA, Bederson JB. Nitric oxide in early brain injury after subarachnoid hemorrhage. Acta Neurochir Suppl. 2011;110:99–103. doi: 10.1007/978-3-7091-0353-1_18. [DOI] [PubMed] [Google Scholar]
- 7.Förstermann U, Sessa WC. Nitric oxide synthases: Regulation and function. Eur Heart J. 2012;33:829. doi: 10.1093/eurheartj/ehr304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moncada S, Palmer RM, Higgs EA. The discovery of nitric oxide as the endogenous nitrovasodilator. Hypertension. 1988;12:365–72. doi: 10.1161/01.hyp.12.4.365. [DOI] [PubMed] [Google Scholar]
- 9.Moncada S, Higgs EA, Palmer RM. Characterization and biological significance of endothelium-derived relaxing factor. Biochem Soc Trans. 1988;16:484–6. doi: 10.1042/bst0160484. [DOI] [PubMed] [Google Scholar]
- 10.Radi R. Peroxynitrite, a stealthy biological oxidant. J Biol Chem. 2013;288:26464–72. doi: 10.1074/jbc.R113.472936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mukherjee P, Cinelli MA, Kang S, Silverman RB. Development of nitric oxide synthase inhibitors for neurodegeneration and neuropathic pain. Chem Soc Rev. 2014;43:6814–38. doi: 10.1039/c3cs60467e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cherian L, Hlatky R, Robertson CS. Nitric oxide in traumatic brain injury. Brain Pathol. 2004;14:195–201. doi: 10.1111/j.1750-3639.2004.tb00053.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Terpolilli NA, Moskowitz MA, Plesnila N. Nitric oxide: Considerations for the treatment of ischemic stroke. J Cereb Blood Flow Metab. 2012;32:1332–46. doi: 10.1038/jcbfm.2012.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tai SC, Robb GB, Marsden PA. Endothelial nitric oxide synthase: A new paradigm for gene regulation in the injured blood vessel. Arterioscler Thromb Vasc Biol. 2004;24:405–12. doi: 10.1161/01.ATV.0000109171.50229.33. [DOI] [PubMed] [Google Scholar]
- 15.Goadsby PJ, Kaube H, Hoskin KL. Nitric oxide synthesis couples cerebral blood flow and metabolism. Brain Res. 1992;595:167–70. doi: 10.1016/0006-8993(92)91470-y. [DOI] [PubMed] [Google Scholar]
- 16.Akgören N, Fabricius M, Lauritzen M. Importance of nitric oxide for local increases of blood flow in rat cerebellar cortex during electrical stimulation. Proc Natl Acad Sci U S A. 1994;91:5903–7. doi: 10.1073/pnas.91.13.5903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zimmermann M, Seifert V. Endothelin and subarachnoid hemorrhage: An overview. Neurosurgery. 1988;43:863–76. doi: 10.1097/00006123-199810000-00083. [DOI] [PubMed] [Google Scholar]
- 18.Banting JD, Friberg P, Adams MA. Acute hypertension after nitric oxide synthase inhibition is mediated primarily by increased endothelin vasoconstriction. J Hypertens. 1996;14:975–81. [PubMed] [Google Scholar]
- 19.Cardillo C, Kilcoyne CM, Cannon RO, 3rd, Panza JA. Interactions between nitric oxide and endothelin in the regulation of vascular tone of human resistance vessels in vivo. Hypertension. 2000;35:1237–41. doi: 10.1161/01.hyp.35.6.1237. [DOI] [PubMed] [Google Scholar]
- 20.Goligorsky MS, Tsukahara H, Magazine H, Andersen TT, Malik AB, Bahou WF. Termination of endothelin signaling: Role of nitric oxide. J Cell Physiol. 1994;158:485–94. doi: 10.1002/jcp.1041580313. [DOI] [PubMed] [Google Scholar]
- 21.Kourembanas S, McQuillan LP, Leung GK, Faller DV. Nitric oxide regulates the expression of vasoconstrictors and growth factors by vascular endothelium under both normoxia and hypoxia. J Clin Invest. 1993;92:99–104. doi: 10.1172/JCI116604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Weng YH, Kuo CY, Chiu YW, Kuo ML, Liao SL. Alteration of nitric oxide gas on gene expression of endothelin-1 and endothelial nitric oxide synthase by a time- and dose-dependent manner in human endothelial cells. Chin J Physiol. 2009;52:59–64. [PubMed] [Google Scholar]
- 23.Hatanaka Y, Hobara N, Honghua J, Akiyama S, Nawa H, Kobayashi Y, et al. Neuronal nitric-oxide synthase inhibition facilitates adrenergic neurotransmission in rat mesenteric resistance arteries. J Pharmacol Exp Ther. 2006;316:490–7. doi: 10.1124/jpet.105.094656. [DOI] [PubMed] [Google Scholar]
- 24.Kolo LL, Westfall TC, Macarthur H. Nitric oxide decreases the biological activity of norepinephrine resulting in altered vascular tone in the rat mesenteric arterial bed. Am J Physiol Heart Circ Physiol. 2004;286:H296–303. doi: 10.1152/ajpheart.00668.2003. [DOI] [PubMed] [Google Scholar]
- 25.Stefano GB, Murga J, Benson H, Zhu W, Bilfinger TV, Magazine HI. Nitric oxide inhibits norepinephrine stimulated contraction of human internal thoracic artery and rat aorta. Pharmacol Res. 2001;43:199–203. doi: 10.1006/phrs.2000.0765. [DOI] [PubMed] [Google Scholar]
- 26.Nozik-Grayck E, McMahon TJ, Huang YC, Dieterle CS, Stamler JS, Piantadosi CA. Pulmonary vasoconstriction by serotonin is inhibited by S-nitrosoglutathione. Am J Physiol Lung Cell Mol Physiol. 2002;282:L1057–65. doi: 10.1152/ajplung.00081.2001. [DOI] [PubMed] [Google Scholar]
- 27.Miyamoto A, Hashiguchi Y, Obi T, Ishiguro S, Nishio A. Ibuprofen or ozagrel increases NO release and l-nitro arginine induces TXA(2) release from cultured porcine basilar arterial endothelial cells. Vascul Pharmacol. 2007;46:85–90. doi: 10.1016/j.vph.2006.06.018. [DOI] [PubMed] [Google Scholar]
- 28.Gookin JL, Allen J, Chiang S, Duckett L, Armstrong MU. Local peroxynitrite formation contributes to early control of cryptosporidium parvum infection. Infect Immun. 2005;73:3929–36. doi: 10.1128/IAI.73.7.3929-3936.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Olekhnovitch R, Ryffel B, Müller AJ, Bousso P. Collective nitric oxide production provides tissue-wide immunity during Leishmania infection. J Clin Invest. 2014;124:1711–22. doi: 10.1172/JCI72058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fang FC. Antimicrobial reactive oxygen and nitrogen species: Concepts and controversies. Nat Rev Microbiol. 2004;2:820–32. doi: 10.1038/nrmicro1004. [DOI] [PubMed] [Google Scholar]
- 31.Andrew PJ, Mayer B. Enzymatic function of nitric oxide synthases. Cardiovasc Res. 1999;43:521–31. doi: 10.1016/s0008-6363(99)00115-7. [DOI] [PubMed] [Google Scholar]
- 32.Weinberg JB, Misukonis MA, Shami PJ, Mason SN, Sauls DL, Dittman WA, et al. Human mononuclear phagocyte inducible nitric oxide synthase (iNOS): Analysis of iNOS mRNA, iNOS protein, biopterin, and nitric oxide production by blood monocytes and peritoneal macrophages. Blood. 1995;86:1184–95. [PubMed] [Google Scholar]
- 33.Saha RN, Pahan K. Regulation of inducible nitric oxide synthase gene in glial cells. Antioxid Redox Signal. 2006;8:929–47. doi: 10.1089/ars.2006.8.929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Seifert V, Löffler BM, Zimmermann M, Roux S, Stolke D. Endothelin concentrations in patients with aneurysmal subarachnoid hemorrhage. Correlation with cerebral vasospasm, delayed ischemic neurological deficits, and volume of hematoma. J Neurosurg. 1995;82:55–62. doi: 10.3171/jns.1995.82.1.0055. [DOI] [PubMed] [Google Scholar]
- 35.Kasuya H, Weir BK, White DM, Stefansson K. Mechanism of oxyhemoglobin-induced release of endothelin-1 from cultured vascular endothelial cells and smooth-muscle cells. J Neurosurg. 1993;79:892–8. doi: 10.3171/jns.1993.79.6.0892. [DOI] [PubMed] [Google Scholar]
- 36.Fassbender K, Hodapp B, Rossol S, Bertsch T, Schmeck J, Schütt S, et al. Endothelin-1 in subarachnoid hemorrhage: An acute-phase reactant produced by cerebrospinal fluid leukocytes. Stroke. 2000;31:2971–5. doi: 10.1161/01.str.31.12.2971. [DOI] [PubMed] [Google Scholar]
- 37.Ansar S, Larsen C, Maddahi A, Edvinsson L. Subarachnoid hemorrhage induces enhanced expression of thromboxane A2 receptors in rat cerebral arteries. Brain Res. 2010;1316:163–72. doi: 10.1016/j.brainres.2009.12.031. [DOI] [PubMed] [Google Scholar]
- 38.Juvela S, Hillbom M, Kaste M. Platelet thromboxane release and delayed cerebral ischemia in patients with subarachnoid hemorrhage. J Neurosurg. 1991;74:386–92. doi: 10.3171/jns.1991.74.3.0386. [DOI] [PubMed] [Google Scholar]
- 39.Takeuchi H, Tanabe M, Okamoto H, Yamazaki M. Effects of thromboxane synthetase inhibitor (RS-5186) on experimentally-induced cerebral vasospasm. Neurol Res. 1999;21:513–6. [PubMed] [Google Scholar]
- 40.Satoh S, Suzuki Y, Harada T, Ikegaki I, Asano T, Shibuya M, et al. The role of platelets in the development of cerebral vasospasm. Brain Res Bull. 1991;27:663–8. doi: 10.1016/0361-9230(91)90042-i. [DOI] [PubMed] [Google Scholar]
- 41.Hansen-Schwartz J, Hoel NL, Xu CB, Svendgaard NA, Edvinsson L. Subarachnoid hemorrhage-induced upregulation of the 5-HT1B receptor in cerebral arteries in rats. J Neurosurg. 2003;99:115–20. doi: 10.3171/jns.2003.99.1.0115. [DOI] [PubMed] [Google Scholar]
- 42.Singhal AB, Topcuoglu MA, Dorer DJ, Ogilvy CS, Carter BS, Koroshetz WJ. SSRI and statin use increases the risk for vasospasm after subarachnoid hemorrhage. Neurology. 2005;64:1008–13. doi: 10.1212/01.WNL.0000154523.21633.0E. [DOI] [PubMed] [Google Scholar]
- 43.Alabadí JA, Torregrosa G, Miranda FJ, Salom JB, Centeno JM, Alborch E. Impairment of the modulatory role of nitric oxide on the endothelin-1-elicited contraction of cerebral arteries: A pathogenetic factor in cerebral vasospasm after subarachnoid hemorrhage? Neurosurgery. 1997;41:245–53. doi: 10.1097/00006123-199707000-00039. [DOI] [PubMed] [Google Scholar]
- 44.Miranda FJ, Alabadí JA, Torregrosa G, Salom JB, Jover T, Barberá MD, et al. Modulatory role of endothelial and nonendothelial nitric oxide in 5-hydroxytryptamine-induced contraction in cerebral arteries after subarachnoid hemorrhage. Neurosurgery. 1996;39:998–1004. doi: 10.1097/00006123-199611000-00022. [DOI] [PubMed] [Google Scholar]
- 45.Sabri M, Ai J, Knight B, Tariq A, Jeon H, Shang X, et al. Uncoupling of endothelial nitric oxide synthase after experimental subarachnoid hemorrhage. J Cereb Blood Flow Metab. 2011;31:190–9. doi: 10.1038/jcbfm.2010.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jung CS, Oldfield EH, Harvey-White J, Espey MG, Zimmermann M, Seifert V, et al. Association of an endogenous inhibitor of nitric oxide synthase with cerebral vasospasm in patients with aneurysmal subarachnoid hemorrhage. J Neurosurg. 2007;107:945–50. doi: 10.3171/JNS-07/11/0945. [DOI] [PubMed] [Google Scholar]
- 47.Olsen SB, Tang DB, Jackson MR, Gomez ER, Ayala B, Alving BM. Enhancement of platelet deposition by cross-linked hemoglobin in a rat carotid endarterectomy model. Circulation. 1996;93:327–32. doi: 10.1161/01.cir.93.2.327. [DOI] [PubMed] [Google Scholar]
- 48.Siuta M, Zuckerman SL, Mocco J. Nitric oxide in cerebral vasospasm: Theories, measurement, and treatment. Neurol Res Int 2013. 2013 doi: 10.1155/2013/972417. 972417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pluta RM. Delayed cerebral vasospasm and nitric oxide: Review, new hypothesis, and proposed treatment. Pharmacol Ther. 2005;105:23–56. doi: 10.1016/j.pharmthera.2004.10.002. [DOI] [PubMed] [Google Scholar]
- 50.Pluta RM, Oldfield EH, Boock RJ. Reversal and prevention of cerebral vasospasm by intracarotid infusions of nitric oxide donors in a primate model of subarachnoid hemorrhage. J Neurosurg. 1997;87:746–51. doi: 10.3171/jns.1997.87.5.0746. [DOI] [PubMed] [Google Scholar]
- 51.Gabikian P, Clatterbuck RE, Eberhart CG, Tyler BM, Tierney TS, Tamargo RJ. Prevention of experimental cerebral vasospasm by intracranial delivery of a nitric oxide donor from a controlled-release polymer: Toxicity and efficacy studies in rabbits and rats. Stroke. 2002;33:2681–6. doi: 10.1161/01.str.0000033931.62992.b1. [DOI] [PubMed] [Google Scholar]
- 52.Thomas JE, Rosenwasser RH. Reversal of severe cerebral vasospasm in three patients after aneurysmal subarachnoid hemorrhage: Initial observations regarding the use of intraventricular sodium nitroprusside in humans. Neurosurgery. 1999;44:48–58. doi: 10.1097/00006123-199901000-00026. [DOI] [PubMed] [Google Scholar]
- 53.Sehba FA, Schwartz AY, Chereshnev I, Bederson JB. Acute decrease in cerebral nitric oxide levels after subarachnoid hemorrhage. J Cereb Blood Flow Metab. 2000;20:604–11. doi: 10.1097/00004647-200003000-00018. [DOI] [PubMed] [Google Scholar]
- 54.Schwartz AY, Sehba FA, Bederson JB. Decreased nitric oxide availability contributes to acute cerebral ischemia after subarachnoid hemorrhage. Neurosurgery. 2000;47:208–15. doi: 10.1097/00006123-200007000-00042. [DOI] [PubMed] [Google Scholar]
- 55.Suzuki Y, Osuka K, Noda A, Tanazawa T, Takayasu M, Shibuya M, et al. Nitric oxide metabolites in the cisternal cerebral spinal fluid of patients with subarachnoid hemorrhage. Neurosurgery. 1997;41:807–12. doi: 10.1097/00006123-199710000-00008. [DOI] [PubMed] [Google Scholar]
- 56.Woszczyk A, Deinsberger W, Boker DK. Nitric oxide metabolites in cisternal CSF correlate with cerebral vasospasm in patients with a subarachnoid haemorrhage. Acta Neurochir (Wien) 2003;145:257–64. doi: 10.1007/s00701-003-0004-7. [DOI] [PubMed] [Google Scholar]
- 57.Ng WH, Moochhala S, Yeo TT, Ong PL, Ng PY. Nitric oxide and subarachnoid hemorrhage: Elevated level in cerebrospinal fluid and their implications. Neurosurgery. 2001;49:622–7. doi: 10.1097/00006123-200109000-00016. [DOI] [PubMed] [Google Scholar]
- 58.Sadamitsu D, Kuroda Y, Nagamitsu T, Tsuruta R, Inoue T, Ueda T, et al. Cerebrospinal fluid and plasma concentrations of nitric oxide metabolites in postoperative patients with subarachnoid hemorrhage. Crit Care Med. 2001;29:77–9. doi: 10.1097/00003246-200101000-00018. [DOI] [PubMed] [Google Scholar]
- 59.Durmaz R, Ozkara E, Kanbak G, Arslan OC, Dokumacioðlu A, Kartkaya K, et al. Nitric oxide level and adenosine deaminase activity in cerebrospinal fluid of patients with subarachnoid hemorrhage. Turk Neurosurg. 2008;18:157–64. [PubMed] [Google Scholar]
- 60.Medele RJ, Stummer W, Reulen HJ, Steiger HJ. Evidence for peroxidative damage by nitric oxide in experimental chronic cerebral vasospasm. Neurol Res. 1996;18:277–80. doi: 10.1080/01616412.1996.11740420. [DOI] [PubMed] [Google Scholar]
- 61.Castro L, Rodriguez M, Radi R. Aconitase is readily inactivated by peroxynitrite, but not by its precursor, nitric oxide. J Biol Chem. 1994;269:29409–15. [PubMed] [Google Scholar]
- 62.Burney S, Niles JC, Dedon PC, Tannenbaum SR. DNA damage in deoxynucleosides and oligonucleotides treated with peroxynitrite. Chem Res Toxicol. 1999;12:513–20. doi: 10.1021/tx980254m. [DOI] [PubMed] [Google Scholar]
- 63.Bonfoco E, Krainc D, Ankarcrona M, Nicotera P, Lipton SA. Apoptosis and necrosis: Two distinct events induced, respectively, by mild and intense insults with N-methyl-D-aspartate or nitric oxide/superoxide in cortical cell cultures. Proc Natl Acad Sci U S A. 1995;92:7162–6. doi: 10.1073/pnas.92.16.7162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Khaldi A, Zauner A, Reinert M, Woodward JJ, Bullock MR. Measurement of nitric oxide and brain tissue oxygen tension in patients after severe subarachnoid hemorrhage. Neurosurgery. 2001;49:33–40. doi: 10.1097/00006123-200107000-00005. [DOI] [PubMed] [Google Scholar]
- 65.Staub F, Graf R, Gabel P, Köchling M, Klug N, Heiss WD. Multiple interstitial substances measured by microdialysis in patients with subarachnoid hemorrhage. Neurosurgery. 2000;47:1106–16. doi: 10.1097/00006123-200011000-00016. [DOI] [PubMed] [Google Scholar]
- 66.Sakowitz OW, Wolfrum S, Sarrafzadeh AS, Stover JF, Lanksch WR, Unterberg AW. Temporal profiles of extracellular nitric oxide metabolites following aneurysmal subarachnoid hemorrhage. Acta Neurochir Suppl. 2002;81:351–4. doi: 10.1007/978-3-7091-6738-0_89. [DOI] [PubMed] [Google Scholar]
- 67.Pluta RM, Thompson BG, Dawson TM, Snyder SH, Boock RJ, Oldfield EH. Loss of nitric oxide synthase immunoreactivity in cerebral vasospasm. J Neurosurg. 1996;84:648–54. doi: 10.3171/jns.1996.84.4.0648. [DOI] [PubMed] [Google Scholar]
- 68.Sehba FA, Chereshnev I, Maayani S, Friedrich V, Jr, Bederson JB. Nitric oxide synthase in acute alteration of nitric oxide levels after subarachnoid hemorrhage. Neurosurgery. 2004;55:671–7. doi: 10.1227/01.neu.0000134557.82423.b2. [DOI] [PubMed] [Google Scholar]
- 69.Hino A, Tokuyama Y, Weir B, Takeda J, Yano H, Bell GI, et al. Changes in endothelial nitric oxide synthase mRNA during vasospasm after subarachnoid hemorrhage in monkeys. Neurosurgery. 1996;39:562–8. doi: 10.1097/00006123-199609000-00026. [DOI] [PubMed] [Google Scholar]
- 70.Park KW, Metais C, Dai HB, Comunale ME, Sellke FW. Microvascular endothelial dysfunction and its mechanism in a rat model of subarachnoid hemorrhage. Anesth Analg. 2001;92:990–6. doi: 10.1097/00000539-200104000-00035. [DOI] [PubMed] [Google Scholar]
- 71.Berra LV, Carcereri De Prati A, Suzuki H, Pasqualin A. The role of constitutive and inducible nitric oxide synthase in the human brain after subarachnoid hemorrhage. J Neurosurg Sci. 2007;51:1–9. [PubMed] [Google Scholar]
- 72.Attia MS, Lass E, Loch Macdonald R. Nitric oxide synthases: Three pieces to the puzzle? Acta Neurochir Suppl. 2015;120:131–5. doi: 10.1007/978-3-319-04981-6_22. [DOI] [PubMed] [Google Scholar]
- 73.Sayama T, Suzuki S, Fukui M. Expression of inducible nitric oxide synthase in rats following subarachnoid hemorrhage. Neurol Res. 1998;20:79–84. doi: 10.1080/01616412.1998.11740488. [DOI] [PubMed] [Google Scholar]
- 74.Sayama T, Suzuki S, Fukui M. Role of inducible nitric oxide synthase in the cerebral vasospasm after subarachnoid hemorrhage in rats. Neurol Res. 1999;21:293–8. doi: 10.1080/01616412.1999.11740934. [DOI] [PubMed] [Google Scholar]
- 75.Saito A, Kamii H, Kato I, Takasawa S, Kondo T, Chan PH, et al. Transgenic CuZn-superoxide dismutase inhibits NO synthase induction in experimental subarachnoid hemorrhage. Stroke. 2001;32:1652–7. doi: 10.1161/01.str.32.7.1652. [DOI] [PubMed] [Google Scholar]
- 76.Kamii H, Kato I, Kinouchi H, Chan PH, Epstein CJ, Akabane A, et al. Amelioration of vasospasm after subarachnoid hemorrhage in transgenic mice overexpressing CuZn-superoxide dismutase. Stroke. 1999;30:867–72. doi: 10.1161/01.str.30.4.867. [DOI] [PubMed] [Google Scholar]
- 77.Widenka DC, Medele RJ, Stummer W, Bise K, Steiger HJ. Inducible nitric oxide synthase: A possible key factor in the pathogenesis of chronic vasospasm after experimental subarachnoid hemorrhage. J Neurosurg. 1999;90:1098–104. doi: 10.3171/jns.1999.90.6.1098. [DOI] [PubMed] [Google Scholar]
- 78.Yao L, Kan EM, Lu J, Hao A, Dheen ST, Kaur C, et al. Toll-like receptor 4 mediates microglial activation and production of inflammatory mediators in neonatal rat brain following hypoxia: Role of TLR4 in hypoxic microglia. J Neuroinflammation. 2013;10:23. doi: 10.1186/1742-2094-10-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Bogdan C. Nitric oxide synthase in innate and adaptive immunity: An update. Trends Immunol. 2015;36:161–78. doi: 10.1016/j.it.2015.01.003. [DOI] [PubMed] [Google Scholar]
- 80.Hanafy KA. The role of microglia and the TLR4 pathway in neuronal apoptosis and vasospasm after subarachnoid hemorrhage. J Neuroinflammation. 2013;10:83. doi: 10.1186/1742-2094-10-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Cox KH, Cox ME, Woo-Rasberry V, Hasty DL. Pathways involved in the synergistic activation of macrophages by lipoteichoic acid and hemoglobin. PLoS One. 2012;7:e47333. doi: 10.1371/journal.pone.0047333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wang YC, Zhou Y, Fang H, Lin S, Wang PF, Xiong RP, et al. Toll-like receptor 2/4 heterodimer mediates inflammatory injury in intracerebral hemorrhage. Ann Neurol. 2014;75:876–89. doi: 10.1002/ana.24159. [DOI] [PubMed] [Google Scholar]
- 83.Kwon MS, Woo SK, Kurland DB, Yoon SH, Palmer AF, Banerjee U, et al. Methemoglobin is an endogenous toll-like receptor 4 ligand-relevance to subarachnoid hemorrhage. Int J Mol Sci. 2015;16:5028–46. doi: 10.3390/ijms16035028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Figueiredo RT, Fernandez PL, Mourao-Sa DS, Porto BN, Dutra FF, Alves LS, et al. Characterization of heme as activator of Toll-like receptor 4. J Biol Chem. 2007;282:20221–9. doi: 10.1074/jbc.M610737200. [DOI] [PubMed] [Google Scholar]
- 85.Belcher JD, Chen C, Nguyen J, Milbauer L, Abdulla F, Alayash AI, et al. Heme triggers TLR4 signaling leading to endothelial cell activation and vaso-occlusion in murine sickle cell disease. Blood. 2014;123:377–90. doi: 10.1182/blood-2013-04-495887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Piazza M, Damore G, Costa B, Gioannini TL, Weiss JP, Peri F. Hemin and a metabolic derivative coprohemin modulate the TLR4 pathway differently through different molecular targets. Innate Immun. 2011;17:293–301. doi: 10.1177/1753425910369020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ma CX, Yin WN, Cai BW, Wu J, Wang JY, He M, et al. Toll-like receptor 4/nuclear factor-kappa B signaling detected in brain after early subarachnoid hemorrhage. Chin Med J (Engl) 2009;122:1575–81. [PubMed] [Google Scholar]
- 88.Zhou ML, Shi JX, Hang CH, Cheng HL, Qi XP, Mao L, et al. Potential contribution of nuclear factor-kappaB to cerebral vasospasm after experimental subarachnoid hemorrhage in rabbits. J Cereb Blood Flow Metab. 2007;27:1583–92. doi: 10.1038/sj.jcbfm.9600456. [DOI] [PubMed] [Google Scholar]
- 89.Zhang T, Su J, Guo B, Zhu T, Wang K, Li X. Ursolic acid alleviates early brain injury after experimental subarachnoid hemorrhage by suppressing TLR4-mediated inflammatory pathway. Int Immunopharmacol. 2014;23:585–91. doi: 10.1016/j.intimp.2014.10.009. [DOI] [PubMed] [Google Scholar]
- 90.Caso JR, Pradillo JM, Hurtado O, Lorenzo P, Moro MA, Lizasoain I. Toll-like receptor 4 is involved in brain damage and inflammation after experimental stroke. Circulation. 2007;115:1599–608. doi: 10.1161/CIRCULATIONAHA.106.603431. [DOI] [PubMed] [Google Scholar]
- 91.Caso JR, Pradillo JM, Hurtado O, Leza JC, Moro MA, Lizasoain I. Toll-like receptor 4 is involved in subacute stress-induced neuroinflammation and in the worsening of experimental stroke. Stroke. 2008;39:1314–20. doi: 10.1161/STROKEAHA.107.498212. [DOI] [PubMed] [Google Scholar]
- 92.Sozen T, Tsuchiyama R, Hasegawa Y, Suzuki H, Jadhav V, Nishizawa S, et al. Role of interleukin-1beta in early brain injury after subarachnoid hemorrhage in mice. Stroke. 2009;40:2519–25. doi: 10.1161/STROKEAHA.109.549592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Hendryk S, Jarzab B, Josko J. Increase of the IL-1 beta and IL-6 levels in CSF in patients with vasospasm following aneurysmal SAH. Neuro Endocrinol Lett. 2004;25:141–7. [PubMed] [Google Scholar]
- 94.Wu W, Guan Y, Zhao G, Fu XJ, Guo TZ, Liu YT, et al. Elevated IL-6 and TNF-α levels in cerebrospinal fluid of subarachnoid hemorrhage patients. Mol Neurobiol. 2015 doi: 10.1007/s12035-015-9268-1. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 95.Hanafy KA, Grobelny B, Fernandez L, Kurtz P, Connolly ES, Mayer SA, et al. Brain interstitial fluid TNF-alpha after subarachnoid hemorrhage. J Neurol Sci. 2010;291:69–73. doi: 10.1016/j.jns.2009.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Sheng W, Zong Y, Mohammad A, Ajit D, Cui J, Han D, et al. Pro-inflammatory cytokines and lipopolysaccharide induce changes in cell morphology, and upregulation of ERK1/2, iNOS and sPLA(2)-IIA expression in astrocytes and microglia. J Neuroinflammation. 2011;8:121. doi: 10.1186/1742-2094-8-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Suzuki S, Takenaka K, Kassell NF, Lee KS. Hemoglobin augmentation of interleukin-1 beta-induced production of nitric oxide in smooth-muscle cells. J Neurosurg. 1994;81:895–901. doi: 10.3171/jns.1994.81.6.0895. [DOI] [PubMed] [Google Scholar]
- 98.Ayer RE, Zhang JH. Oxidative stress in subarachnoid haemorrhage: Significance in acute brain injury and vasospasm. Acta Neurochir Suppl. 2008;104:33–41. doi: 10.1007/978-3-211-75718-5_7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Chen LC, Hsu C, Chiueh CC, Lee WS. Ferrous citrate up-regulates the NOS2 through nuclear translocation of NFκB induced by free radicals generation in mouse cerebral endothelial cells. PLoS One. 2012;7:e46239. doi: 10.1371/journal.pone.0046239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Grote E, Hassler W. The critical first minutes after subarachnoid hemorrhage. Neurosurgery. 1988;22:654–61. doi: 10.1227/00006123-198804000-00006. [DOI] [PubMed] [Google Scholar]
- 101.Hop JW, Rinkel GJ, Algra A, van Gijn J. Initial loss of consciousness and risk of delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage. Stroke. 1999;30:2268–71. doi: 10.1161/01.str.30.11.2268. [DOI] [PubMed] [Google Scholar]
- 102.Iadecola C, Zhang F, Casey R, Clark HB, Ross ME. Inducible nitric oxide synthase gene expression in vascular cells after transient focal cerebral ischemia. Stroke. 1996;27:1373–80. doi: 10.1161/01.str.27.8.1373. [DOI] [PubMed] [Google Scholar]
- 103.Grandati M, Verrecchia C, Revaud ML, Allix M, Boulu RG, Plotkine M. Calcium-independent NO-synthase activity and nitrites/nitrates production in transient focal cerebral ischaemia in mice. Br J Pharmacol. 1997;122:625–30. doi: 10.1038/sj.bjp.0701427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Hirabayashi H, Takizawa S, Fukuyama N, Nakazawa H, Shinohara Y. Nitrotyrosine generation via inducible nitric oxide synthase in vascular wall in focal ischemia-reperfusion. Brain Res. 2000;852:319–25. doi: 10.1016/s0006-8993(99)02117-4. [DOI] [PubMed] [Google Scholar]
- 105.Taylor BS, de Vera ME, Ganster RW, Wang Q, Shapiro RA, Morris SM, Jr, et al. Multiple NF-kappaB enhancer elements regulate cytokine induction of the human inducible nitric oxide synthase gene. J Biol Chem. 1998;273:15148–56. doi: 10.1074/jbc.273.24.15148. [DOI] [PubMed] [Google Scholar]
- 106.Pahan K, Sheikh FG, Khan M, Namboodiri AM, Singh I. Sphingomyelinase and ceramide stimulate the expression of inducible nitric-oxide synthase in rat primary astrocytes. J Biol Chem. 1998;273:2591–600. doi: 10.1074/jbc.273.5.2591. [DOI] [PubMed] [Google Scholar]
- 107.Dasgupta S, Jana M, Zhou Y, Fung YK, Ghosh S, Pahan K. Antineuroinflammatory effect of NF-kappaB essential modifier-binding domain peptides in the adoptive transfer model of experimental allergic encephalomyelitis. J Immunol. 2004;173:1344–54. doi: 10.4049/jimmunol.173.2.1344. [DOI] [PubMed] [Google Scholar]
- 108.You WC, Wang CX, Pan YX, Zhang X, Zhou XM, Zhang XS, et al. Activation of nuclear factor-κB in the brain after experimental subarachnoid hemorrhage and its potential role in delayed brain injury. PLoS One. 2013;8:e60290. doi: 10.1371/journal.pone.0060290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Simard JM, Geng Z, Woo SK, Ivanova S, Tosun C, Melnichenko L, et al. Glibenclamide reduces inflammation, vasogenic edema, and caspase-3 activation after subarachnoid hemorrhage. J Cereb Blood Flow Metab. 2009;29:317–30. doi: 10.1038/jcbfm.2008.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Shih HC, Lin CL, Lee TY, Lee WS, Hsu C. 17beta-Estradiol inhibits subarachnoid hemorrhage-induced inducible nitric oxide synthase gene expression by interfering with the nuclear factor kappa B transactivation. Stroke. 2006;37:3025–31. doi: 10.1161/01.STR.0000249008.18669.5a. [DOI] [PubMed] [Google Scholar]
- 111.Vissers MC, Gunningham SP, Morrison MJ, Dachs GU, Currie MJ. Modulation of hypoxia-inducible factor-1 alpha in cultured primary cells by intracellular ascorbate. Free Radic Biol Med. 2007;42:765–72. doi: 10.1016/j.freeradbiomed.2006.11.023. [DOI] [PubMed] [Google Scholar]
- 112.Wenger RH. Cellular adaptation to hypoxia: O2-sensing protein hydroxylases, hypoxia-inducible transcription factors, and O2-regulated gene expression. FASEB J. 2002;16:1151–62. doi: 10.1096/fj.01-0944rev. [DOI] [PubMed] [Google Scholar]
- 113.Lisy K, Peet DJ. Turn me on: Regulating HIF transcriptional activity. Cell Death Differ. 2008;15:642–9. doi: 10.1038/sj.cdd.4402315. [DOI] [PubMed] [Google Scholar]
- 114.Majmundar AJ, Wong WJ, Simon MC. Hypoxia-inducible factors and the response to hypoxic stress. Mol Cell. 2010;40:294–309. doi: 10.1016/j.molcel.2010.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Kaur B, Khwaja FW, Severson EA, Matheny SL, Brat DJ, Van Meir EG. Hypoxia and the hypoxia-inducible-factor pathway in glioma growth and angiogenesis. Neuro Oncol. 2005;7:134–53. doi: 10.1215/S1152851704001115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Fandrey J, Gassmann M. Oxygen sensing and the activation of the hypoxia inducible factor 1 (HIF-1) — Invited article. Adv Exp Med Biol. 2009;648:197–206. doi: 10.1007/978-90-481-2259-2_23. [DOI] [PubMed] [Google Scholar]
- 117.Lu H, Forbes RA, Verma A. Hypoxia-inducible factor 1 activation by aerobic glycolysis implicates the Warburg effect in carcinogenesis. J Biol Chem. 2002;277:23111–5. doi: 10.1074/jbc.M202487200. [DOI] [PubMed] [Google Scholar]
- 118.Melillo G, Taylor LS, Brooks A, Musso T, Cox GW, Varesio L. Functional requirement of the hypoxia-responsive element in the activation of the inducible nitric oxide synthase promoter by the iron chelator desferrioxamine. J Biol Chem. 1997;272:12236–43. doi: 10.1074/jbc.272.18.12236. [DOI] [PubMed] [Google Scholar]
- 119.Palmer LA, Semenza GL, Stoler MH, Johns RA. Hypoxia induces type II NOS gene expression in pulmonary artery endothelial cells via HIF-1. Am J Physiol. 1998;274:L212–9. doi: 10.1152/ajplung.1998.274.2.L212. [DOI] [PubMed] [Google Scholar]
- 120.Hishikawa T, Ono S, Ogawa T, Tokunaga K, Sugiu K, Date I. Effects of deferoxamine-activated hypoxia-inducible factor-1 on the brainstem after subarachnoid hemorrhage in rats. Neurosurgery. 2008;62:232–41. doi: 10.1227/01.NEU.0000311082.88766.33. [DOI] [PubMed] [Google Scholar]
- 121.Wu C, Hu Q, Chen J, Yan F, Li J, Wang L, et al. Inhibiting HIF-1α by 2ME2 ameliorates early brain injury after experimental subarachnoid hemorrhage in rats. Biochem Biophys Res Commun. 2013;437:469–74. doi: 10.1016/j.bbrc.2013.06.107. [DOI] [PubMed] [Google Scholar]
- 122.Macian F. NFAT proteins: Key regulators of T-cell development and function. Nat Rev Immunol. 2005;5:472–84. doi: 10.1038/nri1632. [DOI] [PubMed] [Google Scholar]
- 123.Sobrado M, Ramirez BG, Neria F, Lizasoain I, Arbones ML, Minami T, et al. Regulator of calcineurin 1 (Rcan1) has a protective role in brain ischemia/reperfusion injury. J Neuroinflammation. 2012;9:48. doi: 10.1186/1742-2094-9-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Graef IA, Wang F, Charron F, Chen L, Neilson J, Tessier-Lavigne M, et al. Neurotrophins and netrins require calcineurin/NFAT signaling to stimulate outgrowth of embryonic axons. Cell. 2003;113:657–70. doi: 10.1016/s0092-8674(03)00390-8. [DOI] [PubMed] [Google Scholar]
- 125.Pérez-Ortiz JM, Serrano-Pérez MC, Pastor MD, Martín ED, Calvo S, Rincón M, et al. Mechanical lesion activates newly identified NFATc1 in primary astrocytes: Implication of ATP and purinergic receptors. Eur J Neurosci. 2008;27:2453–65. doi: 10.1111/j.1460-9568.2008.06197.x. [DOI] [PubMed] [Google Scholar]
- 126.Sama MA, Mathis DM, Furman JL, Abdul HM, Artiushin IA, Kraner SD, et al. Interleukin-1beta-dependent signaling between astrocytes and neurons depends critically on astrocytic calcineurin/NFAT activity. J Biol Chem. 2008;283:21953–64. doi: 10.1074/jbc.M800148200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Luoma JI, Zirpel L. Deafferentation-induced activation of NFAT (nuclear factor of activated T-cells) in cochlear nucleus neurons during a developmental critical period: A role for NFATc4-dependent apoptosis in the CNS. J Neurosci. 2008;28:3159–69. doi: 10.1523/JNEUROSCI.5227-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Obasanjo-Blackshire K, Mesquita R, Jabr RI, Molkentin JD, Hart SL, Marber MS, et al. Calcineurin regulates NFAT-dependent iNOS expression and protection of cardiomyocytes: Co-operation with Src tyrosine kinase. Cardiovasc Res. 2006;71:672–83. doi: 10.1016/j.cardiores.2006.05.026. [DOI] [PubMed] [Google Scholar]
- 129.Elloumi HZ, Maharshak N, Rao KN, Kobayashi T, Ryu HS, Mühlbauer M, et al. A cell permeable peptide inhibitor of NFAT inhibits macrophage cytokine expression and ameliorates experimental colitis. PLoS One. 2012;7:e34172. doi: 10.1371/journal.pone.0034172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Shirey KA, Lai W, Scott AJ, Lipsky M, Mistry P, Pletneva LM, et al. The TLR4 antagonist Eritoran protects mice from lethal influenza infection. Nature. 2013;497:498–502. doi: 10.1038/nature12118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Matsunaga N, Tsuchimori N, Matsumoto T, Ii M. TAK-242 (resatorvid), a small-molecule inhibitor of Toll-like receptor (TLR) 4 signaling, binds selectively to TLR4 and interferes with interactions between TLR4 and its adaptor molecules. Mol Pharmacol. 2011;79:34–41. doi: 10.1124/mol.110.068064. [DOI] [PubMed] [Google Scholar]
- 132.Hutchinson MR, Zhang Y, Brown K, Coats BD, Shridhar M, Sholar PW, et al. Non-stereoselective reversal of neuropathic pain by naloxone and naltrexone: Involvement of toll-like receptor 4 (TLR4) Eur J Neurosci. 2008;28:20–9. doi: 10.1111/j.1460-9568.2008.06321.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Bell BA, Miller JD, Neto NG, O’Neill P, Laughton LM. Effect of naloxone on deficits after aneurysmal subarachnoid hemorrhage. Neurosurgery. 1985;16:498–501. [PubMed] [Google Scholar]
- 134.Wu Y, Zhao XD, Zhuang Z, Xue YJ, Cheng HL, Yin HX, et al. Peroxisome proliferator-activated receptor gamma agonist rosiglitazone attenuates oxyhemoglobin-induced Toll-like receptor 4 expression in vascular smooth muscle cells. Brain Res. 2010;1322:102–8. doi: 10.1016/j.brainres.2010.01.073. [DOI] [PubMed] [Google Scholar]
- 135.Wu Y, Tang K, Huang RQ, Zhuang Z, Cheng HL, Yin HX, et al. Therapeutic potential of peroxisome proliferator-activated receptor γ agonist rosiglitazone in cerebral vasospasm after a rat experimental subarachnoid hemorrhage model. J Neurol Sci. 2011;305:85–91. doi: 10.1016/j.jns.2011.03.006. [DOI] [PubMed] [Google Scholar]
- 136.Jiang Y, Liu DW, Han XY, Dong YN, Gao J, Du B, et al. Neuroprotective effects of anti-tumor necrosis factor-alpha antibody on apoptosis following subarachnoid hemorrhage in a rat model. J Clin Neurosci. 2012;19:866–72. doi: 10.1016/j.jocn.2011.08.038. [DOI] [PubMed] [Google Scholar]
- 137.Lin CL, Dumont AS, Su YF, Dai ZK, Cheng JT, Tsai YJ, et al. Attenuation of subarachnoid hemorrhage-induced apoptotic cell death with 17 beta-estradiol. Laboratory investigation. J Neurosurg. 2009;111:1014–22. doi: 10.3171/2009.3.JNS081660. [DOI] [PubMed] [Google Scholar]
- 138.Guney O, Erdi F, Esen H, Kiyici A, Kocaogullar Y. N-acetylcysteine prevents vasospasm after subarachnoid hemorrhage. World Neurosurg. 2010;73:42–9. doi: 10.1016/j.surneu.2009.06.003. discussion e3. [DOI] [PubMed] [Google Scholar]
- 139.Pereira Filho Nde A, Pereira Filho Ade A, Soares FP, Coutinho LM. Effect of N-acetylcysteine on vasospasm in subarachnoid hemorrhage. Arq Neuropsiquiatr. 2010;68:918–22. doi: 10.1590/s0004-282x2010000600017. [DOI] [PubMed] [Google Scholar]
- 140.Pahan K, Sheikh FG, Namboodiri AM, Singh I. Lovastatin and phenylacetate inhibit the induction of nitric oxide synthase and cytokines in rat primary astrocytes, microglia, and macrophages. J Clin Invest. 1997;100:2671–9. doi: 10.1172/JCI119812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Uekawa K, Hasegawa Y, Ma M, Nakagawa T, Katayama T, Sueta D, et al. Rosuvastatin ameliorates early brain injury after subarachnoid hemorrhage via suppression of superoxide formation and nuclear factor-kappa B activation in rats. J Stroke Cerebrovasc Dis. 2014;23:1429–39. doi: 10.1016/j.jstrokecerebrovasdis.2013.12.004. [DOI] [PubMed] [Google Scholar]
- 142.Sabri M, Ai J, Marsden PA, Macdonald RL. Simvastatin re-couples dysfunctional endothelial nitric oxide synthase in experimental subarachnoid hemorrhage. PLoS One. 2011;6:e17062. doi: 10.1371/journal.pone.0017062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Lo EH. A new penumbra: Transitioning from injury into repair after stroke. Nat Med. 2008;14:497–500. doi: 10.1038/nm1735. [DOI] [PubMed] [Google Scholar]
- 144.Guresir E, Vasiliadis N, Konczalla J, Raab P, Hattingen E, Seifert V, et al. Erythropoietin prevents delayed hemodynamic dysfunction after subarachnoid hemorrhage in a randomized controlled experimental setting. J Neurol Sci. 2013;332:128–35. doi: 10.1016/j.jns.2013.07.004. [DOI] [PubMed] [Google Scholar]
- 145.Milner E, Johnson AW, Nelson JW, Harries MD, Gidday JM, Han BH, et al. HIF-1α mediates isoflurane-induced vascular protection in subarachnoid hemorrhage. Ann Clin Transl Neurol. 2015;2:325–37. doi: 10.1002/acn3.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Hamalainen M, Lahti A, Moilanen E. Calcineurin inhibitors, cyclosporin A and tacrolimus inhibit expression of inducible nitric oxide synthase in colon epithelial and macrophage cell lines. Eur J Pharmacol. 2002;448:239–44. doi: 10.1016/s0014-2999(02)01947-7. [DOI] [PubMed] [Google Scholar]
- 147.Dusting GJ, Akita K, Hickey H, Smith M, Gurevich V. Cyclosporin A and tacrolimus (FK506) suppress expression of inducible nitric oxide synthase in vitro by different mechanisms. Br J Pharmacol. 1999;128:337–44. doi: 10.1038/sj.bjp.0702782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Peterson JW, Nishizawa S, Hackett JD, Bun T, Teramura A, Zervas NT. Cyclosporine A reduces cerebral vasospasm after subarachnoid hemorrhage in dogs. Stroke. 1990;21:133–7. doi: 10.1161/01.str.21.1.133. [DOI] [PubMed] [Google Scholar]
- 149.Xie Z, Lei B, Huang Q, Deng J, Wu M, Shen W, et al. Neuroprotective effect of Cyclosporin A on the development of early brain injury in a subarachnoid hemorrhage model: A pilot study. Brain Res. 2012;1472:113–23. doi: 10.1016/j.brainres.2012.06.053. [DOI] [PubMed] [Google Scholar]
- 150.Manno EM, Gress DR, Ogilvy CS, Stone CM, Zervas NT. The safety and efficacy of cyclosporine A in the prevention of vasospasm in patients with Fisher grade 3 subarachnoid hemorrhages: A pilot study. Neurosurgery. 1997;40:289–93. doi: 10.1097/00006123-199702000-00010. [DOI] [PubMed] [Google Scholar]
- 151.Ryba M, Pastuszko M, Iwanska K, Bidzinski J, Dziewiecki C. Cyclosporine A prevents neurological deterioration of patients with SAH — A preliminary report. Acta Neurochir (Wien) 1991;112:25–7. doi: 10.1007/BF01402450. [DOI] [PubMed] [Google Scholar]
- 152.Abdel-Rahman E, Bolton WK. Pimagedine: A novel therapy for diabetic nephropathy. Expert Opin Investig Drugs. 2002;11:565–74. doi: 10.1517/13543784.11.4.565. [DOI] [PubMed] [Google Scholar]
- 153.Zheng B, Zheng T, Wang L, Chen X, Shi C, Zhao S. Aminoguanidine inhibition of iNOS activity ameliorates cerebral vasospasm after subarachnoid hemorrhage in rabbits via restoration of dysfunctional endothelial cells. J Neurol Sci. 2010;295:97–103. doi: 10.1016/j.jns.2010.04.012. [DOI] [PubMed] [Google Scholar]
- 154.Hooper DC, Spitsin S, Kean RB, Champion JM, Dickson GM, Chaudhry I, et al. Uric acid, a natural scavenger of peroxynitrite, in experimental allergic encephalomyelitis and multiple sclerosis. Proc Natl Acad Sci U S A. 1998;95:675–80. doi: 10.1073/pnas.95.2.675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Llull L, Laredo C, Renú A, Pérez B, Vila E, Obach V, et al. Uric acid therapy improves clinical outcome in women with acute ischemic stroke. Stroke. 2015;46:2162–7. doi: 10.1161/STROKEAHA.115.009960. [DOI] [PubMed] [Google Scholar]
- 156.Ayer RE, Ostrowski RP, Sugawara T, Ma Q, Jafarian N, Tang J, et al. Statin-induced T-lymphocyte modulation and neuroprotection following experimental subarachnoid hemorrhage. Acta Neurochir Suppl. 2013;115:259–66. doi: 10.1007/978-3-7091-1192-5_46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Kramer AH, Fletcher JJ. Statins in the management of patients with aneurysmal subarachnoid hemorrhage: A systematic review and meta-analysis. Neurocrit Care. 2010;12:285–96. doi: 10.1007/s12028-009-9306-9. [DOI] [PubMed] [Google Scholar]
- 158.Kirkpatrick PJ, Turner CL, Smith C, Hutchinson PJ, Murray GD STASH Collaborators. Simvastatin in aneurysmal subarachnoid haemorrhage (STASH): A multicentre randomised phase 3 trial. Lancet Neurol. 2014;13:666–75. doi: 10.1016/S1474-4422(14)70084-5. [DOI] [PubMed] [Google Scholar]
- 159.Wong GK, Chan DY, Siu DY, Zee BC, Poon WS, Chan MT, et al. High-dose simvastatin for aneurysmal subarachnoid hemorrhage: Multicenter randomized controlled double-blinded clinical trial. Stroke. 2015;46:382–8. doi: 10.1161/STROKEAHA.114.007006. [DOI] [PubMed] [Google Scholar]
- 160.McGirt MJ, Lynch JR, Parra A, Sheng H, Pearlstein RD, Laskowitz DT, et al. Simvastatin increases endothelial nitric oxide synthase and ameliorates cerebral vasospasm resulting from subarachnoid hemorrhage. Stroke. 2002;33:2950–6. doi: 10.1161/01.str.0000038986.68044.39. [DOI] [PubMed] [Google Scholar]
- 161.Simard JM, Schreibman D, Aldrich EF, Stallmeyer B, Le B, James RF, et al. Unfractionated heparin: Multitargeted therapy for delayed neurological deficits induced by subarachnoid hemorrhage. Neurocrit Care. 2010;13:439–49. doi: 10.1007/s12028-010-9435-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Simard JM, Tosun C, Ivanova S, Kurland DB, Hong C, Radecki L, et al. Heparin reduces neuroinflammation and transsynaptic neuronal apoptosis in a model of subarachnoid hemorrhage. Transl Stroke Res. 2012;3(Suppl 1):155–65. doi: 10.1007/s12975-012-0166-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Hassanin A, Malek HA, Saleh D. Heparin modulation on hepatic nitric oxide synthase in experimental steatohepatitis. Exp Ther Med. 2014;8:1551–8. doi: 10.3892/etm.2014.1963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Bonmann E, Jüttler E, Krestel HE, Spranger M. Heparin inhibits induction of nitric oxide synthase by cytokines in rat brain microvascular endothelial cells. Neurosci Lett. 1998;253:95–8. doi: 10.1016/s0304-3940(98)00613-2. [DOI] [PubMed] [Google Scholar]
- 165.Engelberg H. Actions of heparin in the atherosclerotic process. Pharmacol Rev. 1996;48:327–52. [PubMed] [Google Scholar]
- 166.Simard JM, Aldrich EF, Schreibman D, James RF, Polifka A, Beaty N. Low-dose intravenous heparin infusion in patients with aneurysmal subarachnoid hemorrhage: A preliminary assessment. J Neurosurg. 2013;119:1611–9. doi: 10.3171/2013.8.JNS1337. [DOI] [PMC free article] [PubMed] [Google Scholar]