Abstract
BACKGROUND
Globally, breast cancer (BC) has become the leading cause of mortality in women. Awareness and early detection can curb the growing burden of BC and are the first step in the battle against BC. The aim of this qualitative study was to explore the awareness and perceived barriers concerning the early detection of BC.
METHODS
A total of 20 focus group discussions (FGDs) were conducted during May 2013–March 2014. Pre-existing themes were used to conduct FGDs; each FGD group consisted of an average of ~10 women (aged ≥18–70 years) who came to participate in a BC awareness workshop. All FGDs were audio taped and transcribed verbatim. The transcripts were inductively analyzed using ATLAS.ti. Based on emerged codes and categories, thematic analysis was done, and theory was developed using the grounded theory approach.
RESULTS
Data were analyzed in three major themes: i) knowledge and perception about BC; ii) barriers faced by women in the early presentation of BC; and iii) healthcare-seeking behavior. The findings revealed that shyness, fear, and posteriority were the major behavioral barriers in the early presentation of BC. Erroneously, pain was considered as an initial symptom of BC by most women. Financial constraint was also mentioned as a cause for delay in accessing treatment. Social stigma that breast problems reflect bad character of women also contributed in hiding BC symptoms.
CONCLUSIONS
Lack of BC awareness was prevalent, especially in low socioeconomic class. Women’s ambivalence in prioritizing their own health and social and behavioral hurdles should be addressed by BC awareness campaigns appropriately suited for various levels of social class.
Keywords: breast cancer, prevention behavior, early detection, awareness, barriers, India
Introduction
Breast cancer (BC) is one of the commonest cancers in women globally, with >1.7 million new cases every year and 522,000 deaths, making it the most frequently diagnosed cancer among women in 140 of 184 countries worldwide according to GLOBOCAN 2012.1 From 2008 to 2012, BC incidence increased by >20%, while BC deaths increased by 14%.1 However, the rise in BC incidence has been steeper in low-and middle-income countries,2 including India, where published reports from different cancer registries indicate rising trends in BC incidence.3 In India, there are >145,000 new cases of BC every year with >70,000 deaths, both numbers being higher than any other cancer site in both genders.1
The high number of BC deaths is due to the fact that ~70% of women with BC present at late stage.4 This is also reflected in the fact that the five-year survival rate of BC in India has not changed much from ~60% since 1995.5 One of the major reasons behind late presentation and high morbidity/mortality is lack of BC awareness in the population6,7 compounded with a lack of population-level methods for screening/early detection.8
The main recognized methods of screening/early detection involve mammography, clinical breast examination (CBE), and breast self-examination (BSE).9 Regarding BSE, the American Cancer Society and other leading cancer agencies have recommended monthly BSE in women,10 and we have discovered BSE to be very strongly associated with early presentation in our studies.11 Diagnosis at an earlier stage allows women more treatment choices and consequently a greater chance of long-term survival and a better quality of life.10
However, many myths related to BC and its treatments still exist, particularly among Asian women.12,13 The majority of them are not aware of common early signs and symptoms of BC, which translates into low screening rates and late stages at diagnosis.12,13 Several studies have shown that barriers to diagnosis and treatment can be addressed by increasing women’s awareness of BC.13,14 A positive correlation also exists between BC awareness and screening practice.13
It is now a well-established fact that awareness and early detection can curb the growing burden of the disease and is the first step in the battle against the BC. However, there is a paucity of studies that explore the various factors behind the lack of BC awareness in India. Hence, the current qualitative study was conducted to explore the perceived barriers concerning early detection of BC among women of Delhi.
Methods
Study design and setting
This was a qualitative study performed on diverse sections of women in the capital city of India, Delhi, to explore the perceived barriers concerning early detection of BC. Qualitative assessment was carried out using focus group discussions (FGDs) before an intervening BC awareness campaign by the Indian Cancer Society (ICS). FGD was opted to elicit participant’s responses because it is a well-suited qualitative approach to explore public topics and is a good way to identify group norms and cultural values.15 Grounded theory approach was used to generate theory. The term grounded theory reflects the concept that theory emerging from this type of work is grounded in the data.16 Emerging categories were defined and redefined using the method of constant comparison from unstructured or semistructured qualitative data.17
Study population and sample
Participants for the FGDs were selected using the convenience sampling method.18 As per their availability and convenience, participants were included randomly for the FGDs. Out of total 35 BC awareness campaigns, only 20 host organizations granted permission for the pre-workshop FGDs. A total of 194 women with age ranging from 18 to 70 years were interviewed at 20 FGDs during the study period of May 2013–March 2014. As per availability of the participants, group size ranged from five to 15 with an average size of 10 participants per group. The selection criteria for inclusion of the participants were women aged ≥18 years and ≤70 years, residence in Delhi for at least a year, and being literate. Efforts were made to include diverse sections of the society for the FGDs. Women who participated were employees from multinational companies (MNCs), non-governmental organizations (NGOs), students, school teachers (secondary to high school), housewives from residential areas, and women from slum areas (Table 1). A slum area can be defined as a heavily populated urban informal settlement characterized by substandard housing and squalor. Most lack reliable sanitation services, supply of clean water, reliable electricity, timely law enforcement, and other basic services.19 Table 1 provides the detailed demographics of the women participants in Delhi.
Table 1.
Detailed demographics of 194 women participants in 20 focus group discussions in Delhi, India.
| SOCIODEMOGRAPHIC FACTORS | N (%) |
|---|---|
| Age | |
| 18–30 | 84 (43.3%) |
| 30–50 | 100 (51.5%) |
| Greater than 50 | 10 (5.15%) |
| Marital status | |
| Married | 121 (62.6%) |
| Unmarried | 65 (33.2%) |
| Others | 8 (4.2%) |
| Religion | |
| Hindu | 147 (76.1%) |
| Muslim | 22 (11.3%) |
| Others | 25 (12.9%) |
| Education | |
| High school or less | 83 (42.8%) |
| Graduate | 99 (51.2%) |
| Post graduate | 12 (6.2%) |
| Social/professional background | |
| Employees from MNCs | 19 (9.8%) |
| School teachers (secondary to high school) | 58 (29.9%) |
| Ladies from slum areas | 58 (29.9%) |
| Housewives from residential areas | 30 (15.5%) |
| Students | 19 (9.8%) |
| NGO’s | 10 (5.2%) |
| Average monthly expense | |
| <10,000 | 38 (19.4%) |
| 10–25,000 | 68 (35.1%) |
| 26–50,000 | 67 (34.9%) |
| >50,000 | 21 (10.7%) |
Study tool and measures
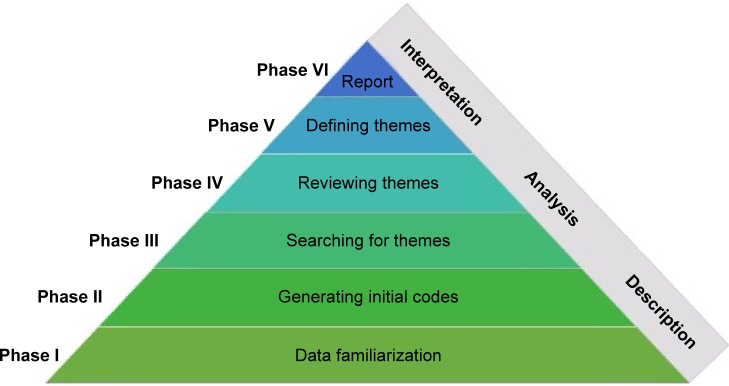
To accomplish the goal of the study, a FGD guide was developed based on the aims and objectives of the study and review of the literature. Experts’ opinions were sought. After addition of experts’ opinions and exclusion of few redundant questions, a total of 15 questions covering four broad areas of BC awareness were included in the FGD guide (Fig. 1).
Figure 1.
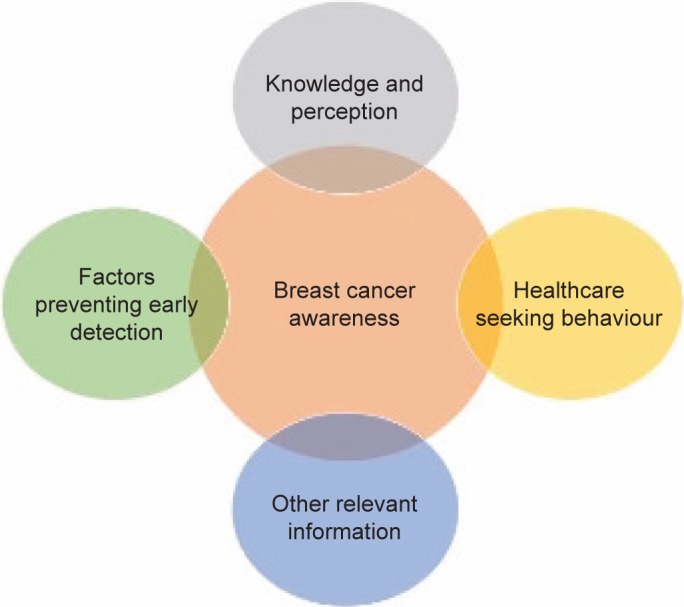
Broad themes associated with breast cancer awareness that were explored in this study involving women participants in 20 FGDs in Delhi, India.
Emphasis was made to evade leading questions and to elicit potential responses from participants. Where required, appropriate probes such as how, if not why, if yes why, where, and who were used to draw relevant information from the participants. Sociodemographic information was also collected at the beginning of the FGDs. In all, 45–60 minutes were fixed to execute each FGD.
To begin the interview, some ice-breaking, broad opening questions were asked such as “Have you ever heard about BC?” “What have you heard about BC?” and “From where you have heard?” Pilot testing was done to validate the discussion guide. Although initially the discussion guide was made using English language, it was later translated into Hindi. As per convenience of the participants and to make it more comprehensive, local terms such as chest breast, inflammation, and wound were used instead of scientific terms.
Data collection and management
As per participants’ agreement and convenience, 10 participants were requested by the organizer of workshop to arrive at the venue an hour before the schedule time for BC awareness workshop. The participants were called and reminded by the organizer to ensure presence of at least 10 participants for the FGD. To avoid any interruptions, a separate place with a round sitting arrangement was requested beforehand from the workshop organizer. An experienced lady researcher with Ph.D. in medical anthropology and proficient in qualitative research method conducted the FGDs. A FGD guide was followed to avoid any information lapse. Rather than following the order of the FGD guide’s questions, discussions were made according to responses of the participants with the sense of avoiding deviation from the subject. Efforts were made to ensure that without overlapping each other’s voice, everyone should get time to share their views and not just one person carried out the whole discussion. Before beginning the discussions, participants were encouraged to share their views irrespective of right and wrong answers. Each FGD lasted for 10–60 minutes depending on participants’ responses and available time before commencement of BC awareness campaign. After the informed consent of the participants, FGDs were audio recorded and verbatim transcribed into computer files. To make data more apprehensive, complete data were manually classified in MS Excel according to different categories and themes. Responses were grouped as per emerged categories. To maintain anonymity, each response was given a unique identification number.
Analysis of data
Qualitative data analysis software, ATLAS.ti (version 7.1.8), was used to manage, analyze, and visualize the data. Verbatim transcriptions of audio-recorded FGDs discussion served as the primary data for the analysis. Diverse groups’ FGDs were loaded as primary documents in the ATLAS.ti software. Thematic analysis was done using guidelines outlined by Braun and Clarke.15,20 Boyatzis has described thematic analysis as a method for identifying, analyzing, and reporting patterns (themes) within data. It minimally organizes and describes your data set in (rich) detail.20 The following steps were followed to analyze the data:
Phase I: familiarizing with the data. Iterative process of reading and re-reading of verbatim transcriptions had provided identification of the patterns engrossed in data.
Phase II: generating initial codes. After familiarization with data, initial codes were generated as per participants’ responses. It is a very important phase to ensure that all actual data extracts are coded and then collated together within each code.20
Phase III: searching for themes. Collating all initial codes had given a long list of codes or information based on participants’ responses in different areas. Based on the list of information, appropriate themes were searched for categorizing the data.
Phase IV: reviewing themes. For refinement of generated themes, a review process was done. It involves the process of merging or splitting of different categories into new categories.
Phase V: defining and naming themes. The emerged new themes were defined and named. This phase allows scope for detailed description of the data.
Phase VI: producing the report. The report was built based on the contents of the emerged themes (Fig. 2).
Figure 2.
Steps followed in this study for qualitative analysis of data involving women participants in 20 FGDs.
Quality control, validity, and reliability of the study
To ensure accuracy and quality control, periodical supervisions were made by the principal investigator (PI) from the Indian Institute of Public Health, Delhi. All audiotaped FGDs, transcriptions, and analyses were supervised by the PI of the project. All audio-taped FGDs were transcribed by the same researcher who had conducted FGDs. Echo questions were made by the researcher to confirm meaning of the participants’ response to ensure internal validity.21 After completion of each audio-taped FGD’s transcription, recordings were played for the second time to make them reliable.21 To increase the internal validity and reliability of the study, anonymous direct verbatim quotations in italic font were used to illustrate particular theme.21 To make internationally comprehensive, the Hindi verbatim has been translated into English language and reported alongside the Hindi verbatim.
Ethical consideration
Ethical approval
Ethical permission to conduct the study was granted by the Public Health Foundation of India’s (PHFI’s) institutional ethics committee (IEC)—letter number TRC-IEC-165/13. Our research complied with the principles of the Declaration of Helsinki.
Results
The demographic characteristics of the participants in this sample were similar to those of women described in our previous publication.22 A thematic analysis of qualitative data revealed different perceptions of women regarding BC. The potential responses were classified into three broad themes. First theme was built based on participants’ existing knowledge and perception regarding BC. Second theme embraced different factors that inhibit early detection of BC. Third theme revealed general healthcare-seeking behaviors of women. As per description given by the participants, each of the themes was further divided into sub-themes and relevant categories. Table 2 provides the theme, sub-themes, and categories grounded in data from 20 FGDs among women in Delhi, India.
Table 2.
Theme, sub-themes, and categories grounded in data from 20 FGDs among women in Delhi, India.
| Theme I: knowledge and perception about BC |
| Prevalence and population at risk |
| Risk factors |
| Symptoms |
| Treatment and prevention |
| Inheritance |
| Attitude towards BC patients |
| Importance of BC awareness programme |
| Theme II: factors preventing women from presenting early with BC |
| Behavioral factors |
| (a) Shyness/hesitation |
| (b) Fear |
| (c) Ambivalence in prioritizing health |
| Myths and misconceptions |
| Lack of information |
| Social stigmas |
| Financial constraint |
| Lack of support |
| (a) Family |
| (b) Medical institutions |
| Theme III: healthcare-seeking behavior |
Theme I: knowledge and perception about BC
A majority of women had heard of the term BC. A few women from slum areas replied that they have not heard about the term BC. Surprisingly, a few school teachers also replied that “first time they are listening the term BC.” Some of the participants described BC and stated, “I have heard about lump nothing much.” A majority of women in each group were less informed or misinformed about the BC. The participants reported different sources of information from which they come to know about the BC. Newspaper and television followed by magazines, posters, peer group, doctor, etc. were the most frequent mentioned source of information regarding BC.
Prevalence and population at risk
Except women from slum areas, most of the participants were found aware of the fact that prevalence of the BC was increasing with time. One woman said, “We know it is increasing but how much that we don’t have any idea.” A majority of the women were found to be uncertain about the population at risk and believed that BC is not possible in men. One woman expressed that “stressed out women may get BC.” Another woman stated that “aged people can be affected.” Women had misconception that “married women are prone to get BC.” One participant added that “BC occurs in adolescent period.”
Risk factors
Regarding risk factors related to BC, most of the women were found aware of the fact that breastfeeding reduces risk for BC. On the other hand, women had lots of myths related to BC risk. Erroneously, most of the women considered specific bra (tight/colored/underwired/puffed/synthetic/unfitted) and tight cloths as reasons for the BC. Most of the women were aware of the harmful effects of reduced physical activities and junk foods.
Symptoms
When asked about symptoms of BC, majority of the women were unaware of symptoms. Very few women described correct symptoms to detect BC. Most of the women incorrectly mentioned painful lump or chest pain as symptoms for BC. Negligible women reported BSE in practice, and none of the women described the correct procedure to detect a lump.
Treatment and prevention
Most of the women belonging to slum areas were not aware of treatment procedures. A majority of the women believed that BC cannot be cured. One woman said, “In the starting stage the person appears to be normal and it suddenly spreads in the body and then it cannot be controlled or cured.” Other women said, “We exactly don’t know what the causes of it are so we can’t tell how to prevent it.” Negligible women reported that they know about the detection methods, including BSE, mammography, and CBE. A few women reported that they had mammography after prescription of the doctor. Women expressed, “It is not included in any routine or general check-ups and I have not put any extra efforts for this.” “Ya even you know I heard about it how to detect and all, but still I am not able to detect because the lumps are quite similar during period you can’t exactly figure it out.” “We don’t check because such a thing never comes to our mind.”
Inheritance
A majority of women were found aware of the fact that BC is not a contagious disease. One woman expressed, “It depends on education. Educated people do not think so.” Women from slum areas believed that BC is contagious and they stated: “who knows about the disease like if anyone has TB it can spread to others as well,” “it can spread by eating food eaten by the diseased,” and “it can spread if we get contact of patient’s fluid.” None of the women were aware of genetic inheritance of BC.
Attitude toward BC patient
Women also shared their views and attitudes toward BC patients. Based on the experiences shared by the participants, it was revealed that women had misconceptions related to BC, which made patients suffer emotionally. Negative perception also makes it difficult for the patient to cope up with the disease. One woman said, “Sometimes the behavior of the people change. I have seen when my relative suffered from BC, blood used to come from her breast. At that time their landlord asked them to leave their house as it can affect his children. Even her husband used to scold her and was not supportive. He was saying her it is better if you die.” Another woman shared, “Cancer causes financial crisis so it ultimately disheartens everybody that spending money will also go waste as patient will surely die soon.” One woman added, “The other thing is society also looks differently toward the patient of cancer because for cancer patients there is a special treatment and the chances of survival are also less.” Women believed that having BC was embarrassing; they stated, “It may be embarrassing as lots of things start happening like hair falling, lot of things to your appearance.” “They are slightly embarrassed because they have to cover up when they remove the breast. Now there is a procedure of implant but earlier it was not there. The initial procedure it is very embarrassing for a woman.”
Importance of BC awareness program
A few women expressed their view on importance of awareness program. They emphasized, “We can be aware and spread knowledge to others as to my daughter, friends, family member etc.” “Awareness campaign can give breakthrough.” One participant added, “Like AIDS and polio awareness program BC awareness should be created in the community.” Another participant supported that view and said, “Just like the other disease, we are having general awareness for them, so we should have for BC also.” One participant gave emphasis by saying, “If we came to know about the causes which cause BC then we will definitely take steps to prevent this, we will implement the things in our life which can prevent all these things.” Other participants of group also appreciated the thought. One more important comment made by the participant was, “It even helps the lower society like sweeper, maid etc. when we pass the message to them they become part of this campaign.” Participant’s views show importance and need for the BC awareness program in the community. To roll out the awareness in complete society, different suggestions were made by the participants. Two participants suggested, “BC awareness campaign should not be only women centric it should be family centric. Campaign should not for women only it should focus husband, kids and other family member as well.” One participant added, “Campaign should be in local language to make everyone understand.”
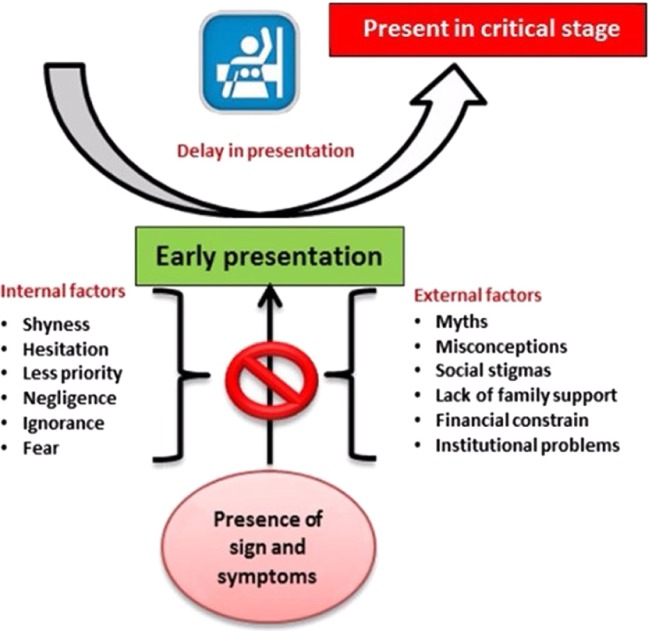
Theme II: factors preventing women from early presentation of BC
Emerged qualitative data exposed different factors that obstructed participants from presenting early even if symptoms of BC were present. Behavioral factors were found as internal barriers that restricted women from presenting early, while prevalent myths, conceptions, and social stigma were found as external hurdles preventing in early presentation. Figure 3 summarizes different factors that disable early presentation.
Figure 3.
Factors preventing women from presenting early with breast cancer as envisaged in this study involving women participants in 20 FGDs in Delhi, India.
Sub-theme I: behavioral factors
The theme behavioral factors embrace participants’ responses related to their behaviors, which prevented them from presenting early. The participants admitted shyness, hesitation, fear, and not prioritizing self-health being the common behaviors inhibiting them from discussing breast-related issues. Based on the participants’ responses, the following sub-themes explicate particular behaviors.
Shyness/hesitation
Irrespective of social class and educational status of the participants, shyness/hesitation was found to be the most frequently mentioned behavioral factor among all FGDs. The presence of a male doctor was found to be one of the important reasons for shyness/hesitation. Women expressed, “Women do not want to go male doctor they do not feel frank with them.” “Feeling shy to show our breast to doctor. Start thinking whether it will be a lady doctor or gent’s doctor. What they will do? What will be the procedure?” “We do not approach to gent’s doctor. We can approach if lady doctor is there.” A few women mentioned that they feel shyness/hesitation even in the presence of a lady doctor. One woman expressed, “It’s a part of woman so if somebody is going to touch you then is not comfortable be it a women doctor.” Other women also reported, “Sometimes we feel shy to show our breast to the doctor if there is even a lady doctor available.” Hesitation to inform male member present in the family was also found to be one of the reasons to avoid approaching doctors. One woman expressed, “Generally male members are present in the house and it is necessary to inform at home if we want to go to the doctor.” It was mentioned that compared to women, girls have more hesitation to discuss breast issues; they expressed, “Sometimes women gets frank but girls have more hesitation and they do not want to come out.”
Fear
In all the FGDs, women perceived cancer as a death. Women expressed their fear with “something you can die of,” “the cancer word itself tells that now the person is not going to live more,” and “if we are diagnosed with this then nothing much can be done.” A few women reported having fear from getting spoiled relationship with husband and other family members in case they have breast-related problem. One woman said, “Women think they will get separated from family if they will tell about their problems.” A majority of women reported that they avoided health check-ups in fear of detecting any big health problems. Women expressed: “people are generally scared they think if something turns up that’s why we will keep on avoiding,” “they think they are sitting peacefully at home and if they will go to doctor, they might be diagnosed with some disease,” and “we sometimes scare also that if we go to the doctor and we will detect with some disease. This is our big fear … all respondents agree to this point.” Fear of society was also found to be one of the hurdles in the early presentation of the BC.
Ambivalence in prioritizing health
A majority of women discussed about women’s behavior concerning their own health. Almost all women emphasized on the fact that a majority of women do not give priority to their health issues. Ignorance, negligence, carelessness, and bearing pain were the common women behaviors claimed by most of the participants that attribute to prolonged or late presentation of the disease. One school teacher expressed her view, “We focus too much on our children, husband and family and neglect ourselves, it is prevalent in Indian women.” Other teachers also admitted, “Until the pain worsens that it becomes unbearable, then only we go for the doctor” and “we become lazy for ourselves not for our husband, children or other family members.” Women from residential communities mentioned the point that “they have tendency to wait and watch and do home remedies to cure their own health problems.” Most of the working women complained that they do not get time for self-care. One woman working in an MNC said, “We can’t afford to be sick. We travel a lot to reach office, we don’t have time to read newspapers or lay down for some time as there are so much other works to do like taking care of children.” Consistently, women from affluent society also believed that women keep ignoring their health problems. Women from slum areas frequently noted women’s tendency to bear pain and financial constraint as barriers to present early. One woman explained, “They have so much small small things to do like making arrangement for water, washing clothes, labor etc. that people can’t think of taking break from their routine life and go to doctor till the time something major has not happened.” One other woman emotionally added, “People whom god has given money can afford treatment while other people who haven’t been given money die.” One school teacher added her view saying that “knowledge and awareness is so much increased that it is not the issue now main point is our own ignorance and negligence, we wait for the things to be worsen.” One more school teacher gave emphasis and said that “preparedness is missing, we think whenever it will happen then we will see what to do, and it is not only for breast cancer it is for each and every disaster.”
Sub-theme II: myths and misconceptions
In-depth FGDs and probes exposed perceived myths and misconceptions concerning BC among the women. Irrespective of educational and occupational status, majority of women considered pain as an initial symptom for BC. They expressed, “Pain is the initial symptom, if we feel pain then only we should get check-up.” A few women belonging to a slum area believed that only educated people could know about early detection. They expressed, “Only educated people can be aware, how can illiterate be aware?” Some women shared, “They are always scared of BC if they feel lump or cyst in the breast.” Majority of women linked BC with complete removal of breast and loss of femininity. Women believed BC cannot be diagnosed at an early stage and frequently mentioned that “it is a big disease and cannot be detected in an early stage.” Women had a strong perception that it cannot be cured, and they expressed, “It suddenly spreads in the body and then it cannot be controlled or cured.” “If we are diagnosed with this then nothing much can be done. This can’t be cured,” “If they will be diagnosed with such kind of disease they will not be able to survive. There is no cure or treatment for cancer. People fear with the name of cancer.” One woman said, “It is said we should not do biopsy. If you disturb anything then it won’t get cure.”
Sub-theme III: lack of information
It could be inferred from all FGDs that most of the participant’s responses concerning BC were ambiguous and based on myths and misinformation. Several women emphasized on the need of awareness programs. Women admitted, “We have heard about breast cancer but our knowledge is not that good. We know very little about it.” Women claimed, “They don’t have proper knowledge, they are not aware so they are not able to detect it.” Women criticized, “There is no awareness like AIDS.” “There is very little awareness about this; awareness has not been created.” Lack of information was frequently mentioned: “people don’t know what exactly it is and till the time they reached the doctor advanced stage has come,” “patient keeps on wandering from one doctor to another or some local healer or keep on taking medicines by asking from pharmacist,” and “the women don’t know what kind of diet she should take to remain healthy.” Women emphasized on the need of awareness campaign. They stated, “hard campaigns are required to knock on your head.” “Unless until we won’t be aware we won’t come out and say other too.”
Sub-theme VI: social stigmas
A majority of women discussed about social stigma associated with BC in the community. Most of the women from slum areas underlined that “people consider BC sexual disease and result of the wrong they did.” They expressed, “People doubt she might have got STI or AIDS.” “Yes, all people consider it as bad if a woman is married. Husband can question her. He may suspect that he did nothing, how it happened to you?” “Other than shyness fear of society is there. You do not know who will put blame on you.” “Women are helpless they cannot openly show their problems.” “Yes it is there in the society. There are people in the society who may think like that.” A few women contradicted and said “different reasons can be for the BC … not necessary intercourse may be the reason for BC.” One woman working in an NGO shared her experience: “Husband will question. I did not squeeze. How did it happen to you? … since I also work for Mahila Aayog such cases come to me where such discussions occur.” One woman emotionally said, “Internal pressure is more” when probed “what do mean by internal pressure?” She signified, “Internal pressure means husband’s pressure, he will blame. I did not do anything, then why did it happen to you?” A discussion with college students and school teachers also revealed social stigmas related to BC in the society. One important point was made by a college student. She stated, “there is zero communication in the family related to breast cancer, it might be reason for increased BC incidence.” Another college student added “in our society women related things are hidden, which is very normal. Indian psyche is like this only; they tend to hide the problem.” One school teacher opinionated, “Our community is still following old tradition.” “People are orthodox.” Other school teacher added, “Uneducated women do not want to expose these things; they think these are wrong things and they should not share these things with society. They do not want to tell anything about breast cancer.”
Although most of the employees from multinationals emphasized, “People don’t have stigma related to BC. People are educated and okay about it.” However, one college student claimed, “Social stigma related to BC is not just the lower level it is there at the upper level as well. BC is not detected because it’s all covered.”
Sub-theme V: financial constraint
A majority of the participants noted fear of financial crisis that might be a consequence of breast health check-up. One NGO worker told, “Many people don’t have money for the treatment so keep on avoiding the symptom.” Women from slum areas attributed inability of early presentation to the lack of money and time. One woman emotionally said, “Going hospital results absenteeism from work and consequently no payment. Then kids have to sleep hungry.” Another woman reiterated “it seems that if we go to the doctor we don’t know how much bill they are going to make.” Contradicting the above point, one woman said, “No it’s not about money, women do not go because they do not want to go for check-up.”
Sub-theme VI: lack of support
Family
Lack of family support was found one of the factors that repress women for early detection. One college student said, “Women do not get that attention in the family, women have to take care of the family but family is never being told that you have to take care about the women.” One more college student added, “Everybody is equal in the family but still only women are running like a hell. This has to be changed.” Consistent response was acquired from housewives; they expressed, “Ladies are very devoted for her family but when she gets ill perception of family members about her changes.” One of the employees from MNC expressed similar views and emphasized, “I don’t think women are given importance in families. Generally they think that women are meant for taking care of her family, husband, and children.” On other hand, contrasting responses were expressed by some school teachers who pointed out, “Now situations have changed. Women get support from family.” To add up, another school teacher said, “It varies from house to house, family to family. In my case females are being given priority in each and every situation but there must be others who may not have the same scenario”; most of the participants agreed to this point. Women from slum areas uttered the same thing—one respondent said, “Many people start saying you always have health problems and it has become routine for you.” Two NGO workers personally shared, “They are suffering from breast pain and during the intercourse when they deny their husband to touch their breast the husband gets annoyed and fights with them.”
Medical institutions
Several women shared their earlier bad experience from government and private hospitals and found reluctant to approach them. One college student shared, “Condition of government hospitals is very bad and in private they are snagging money out of you like hell.” Three women from slum areas shared their experience and blamed that they were given wrong treatments. Women from slum areas frequently mentioned “long waiting time and multiple visits” for not approaching hospitals.
Theme III: healthcare-seeking behavior
Third theme has built based on participants’ responses on general health-care behavior in case of any health problems. In all FGDs, it was found that majority of women wait and watch for automatic cure and tend to approach the health system only in critical health situations. One school teacher said, “When there is lot of trouble then we go to show.” Even employees of MNCs admitted the same. They expressed, “We are very careless for ourselves. We keep on looking for alternatives but avoid approaching doctor.” “When we start feeling that something is going to now aggravate its only fear that pushes us to go to doctor.” Only one employee said, “I go immediately to doctor whenever something happens to me.” Consistent response was found from housewives. One woman expressed fear: “tension remains very high. Sometimes it feels like I keep sleeping over it.” A majority of women from affluent areas also admitted, “Even in case of cough and cold we approach the doctor in extreme conditions.” “We think it will become ok on its own in 2–3 days and we pass time doing home remedies.” “Women don’t care for herself but get alert for husband and children.” A few women from affluent areas opposed the above views. According to them, “now women are aware they look after themselves.” Women from slum areas reported that they preferred unqualified health workers for any health problems. Sometimes due to wrong diagnosis, patients suffer and it causes delay in right treatment. One woman from a slum area shared her experience: “once I had high fever. I approached the unqualified doctor. He just advised me to put wet strips on forehead. When I had no relief he had given few medicines. I did not get relief then I went to hospital. Doctor admitted me in the emergency. Doctor prescribed medicine based on blood and urine test report. Doctor told I was taking wrong medicines. I got cured when I received right medicine.”
Discussion
This is one of the first qualitative studies in the community from India that explores the various issues related to BC awareness and barriers to early presentation. The results obtained from inductively analyzed qualitative data revealed that the level of BC awareness was alarmingly low among the women participants of Delhi. Emerged themes and sub-themes indicated different categories of barriers preventing women to present early while signs and symptoms were visible. Our overall results are consistent with other qualitative studies done in other parts of the world.16,21,23–27 Congruent with other studies, print media, television, and peer group were most frequently mentioned as sources of information related to BC.21,23,28,29
Leading agencies working for BC prevention have recommended monthly BSE to women.10 In the present study, negligible women reported awareness about BSE. A similar result was reported in a qualitative study done by Bodapati and Babu30 in Andhra Pradesh. Compatible with the study on Turkish women,21 we discovered that physicians’ advice was an effective tool for breast screening. Like the study done in Pakistani Muslim women,27 women in this study identified different risk factors for developing BC such as breastfeeding, addiction, environmental factors, and chemicals.
In agreement with other qualitative studies, behavioral factors were identified as a hurdle for the early presentation. In a study on Turkish women, Kissal and Beser21 reported fear and embarrassment as preventing women from early detection of BC; another study23 on Turkish women had shown lack of sensitivity along with neglecting and forgetting as substantially important barriers. Fear of screening results, embarrassment, doubts, worry, and possible pain were also discussed in qualitative studies on Iranian women24 and American women.31
In line with the other literatures,24,32–34 fear of social stigma, losing femininity, and husband’s separation as reported by the participants of the present study prevented women from stepping outside. In line with the study on Iranian women,24 the present study revealed the consideration of breast as a sexual organ due to which women hesitated to visit male doctors. The women in the present study shared, “having breast problem relates to bad character of women.” The participants emphasized awareness programs for men and other family members. A qualitative study from Jordan25 had revealed that men’s knowledge about BC and their attitudes toward their partner’s BC screening was context sensitive and largely unexplored in the literature. Lamyian et al16 also emphasized on spouse advocacy. Consistent with the present study, a qualitative study on Pakistani women also highlighted that breast is viewed as an organ that should be hidden and not discussed openly.27
In this study, women blamed lack of family support and financial constraint for delay in presentation. Parallel results were reported in other qualitative studies as well.24,25 Regarding healthcare-seeking behavior of women, it was found that women had a tendency to tolerate the problem and tended to approach the health system only in critical conditions. Similar findings were reported in a study on Iranian women.16 It was also found that women had an ambivalence toward prioritizing own health. Harmonious with the said result, Taha et al25 also reported that women perceived that their main role is to take care of the family. Women’s ambivalence in prioritizing their own health and social and behavioral hurdles should be addressed by BC awareness campaigns appropriately suited for various levels of social class.
Conclusions
This study was one of the first studies from India that provided such a detailed in-depth picture about the various issues related to BC in Indian women and enumerated the barriers that prevent women from visiting the health system so that BC is detected early. Some of the issues related to lack of awareness, fear, familial and social stigma, myths and misconceptions, neglect and lack of priority given to health by women, etc. were captured quite ably by this study. We need to focus more closely on some of these issues, which were brought to the surface by the current study while using these findings to create better ways and better content for targeting populations for increasing BC awareness. Using media and including men while creating awareness about women’s issues are quite important for effective BC control.
Acknowledgments
We wish to acknowledge the valuable support and guidance provided to this project by Dr. Isabel dos Santos Silva and Dr. Jane Wardle. We also extend our gratefulness to the volunteers of the ICS who tirelessly worked toward increasing the awareness of the community regarding cancer. We are also grateful to Ms. Parika Pahwa for her contribution toward this project.
Abbreviations
- ACS
American Cancer Society
- AIDS
acquired immune deficiency syndrome
- BC
breast cancer
- BSE
breast self-Examination
- CBE
clinical breast examination
- FGD
focus group discussion
- ICS
Indian Cancer Society
- IEC
Institutional Ethics Committee
- IIPHD
Indian Institute of Public Health, Delhi
- LMIC
low- and middle-income country
- MNC
multinational company
- NGO
non-governmental organization
- PHFI
Public Health Foundation of India
- STI
sexually transmitted infection
Footnotes
ACADEMIC EDITOR: Goberdhan P. Dimri, Editor in Chief
PEER REVIEW: Three peer reviewers contributed to the peer review report. Reviewers’ reports totaled 823 words, excluding any confidential comments to the academic editor.
FUNDING: This work was supported by a Wellcome Trust Capacity Strengthening Strategic Award to the PHFI and a consortium of UK universities (research grant number F012/RG/SD/15). The authors confirm that the funder had no influence over the study design, content of the article, or selection of this journal.
COMPETING INTERESTS: Authors disclose no potential conflicts of interest.
Paper subject to independent expert single-blind peer review. All editorial decisions made by independent academic editor. Upon submission manuscript was subject to anti-plagiarism scanning. Prior to publication all authors have given signed confirmation of agreement to article publication and compliance with all applicable ethical and legal requirements, including the accuracy of author and contributor information, disclosure of competing interests and funding sources, compliance with ethical requirements relating to human and animal study participants, and compliance with any copyright requirements of third parties. This journal is a member of the Committee on Publication Ethics (COPE).
Author Contributions
Conceived and designed the experiments: AM, SD, SK, JG, and PKD. Analyzed the data: AM and SD. Wrote the first draft of the manuscript: AM and SD. Contributed to the writing of manuscript: AM, SD, SS, SK, JG, and PKD. Agreed with manuscript results and conclusions: AM, SD, SS, JG, SK, and PKD. Jointly developed the structure and arguments for the article: AS and SD. Made critical revisions and approved the final version: AM, SD, SK, SS, JG, and PKD. All authors reviewed and approved the final manuscript.
REFERENCES
- 1.Ferlay JSI, Ervik M, Dikshit R, et al. GLOBOCAN 2012 v10, Cancer Incidence and Mortality Worldwide: IARC Cancer Base No. 11. Lyon, France: International Agency for Research on Cancer; 2013. Available at http://globocan.iarc.fr/Pages/references.aspx. [Google Scholar]
- 2.Benson JR, Jatoi I. The global breast cancer burden. Future Oncol. 2012;8(6):697–702. doi: 10.2217/fon.12.61. [DOI] [PubMed] [Google Scholar]
- 3.Asthana S, Chauhan S, Labani S. Breast and cervical cancer risk in India: update. Indian J Public Health. 2014;58(1):5–10. doi: 10.4103/0019-557X.128150. [DOI] [PubMed] [Google Scholar]
- 4.Sankaranarayanan R, Swaminathan R, Brenner H, et al. Cancer survival in Africa Asia Central America: a population-based study. Lancet Oncol. 2010;11(2):165–173. doi: 10.1016/S1470-2045(09)70335-3. [DOI] [PubMed] [Google Scholar]
- 5.Allemani C, Weir HK, Carreira H, et al. Global surveillance of cancer survival 1995–2009: analysis of individual data for 25,676,887 patients from 279 population-based registries in 67 countries (CONCORD-2) Lancet. 2015;385(9972):977–1010. doi: 10.1016/S0140-6736(14)62038-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ramirez AJ, Westcombe AM, Burgess CC, Sutton S, Littlejohns P, Richards MA. Factors predicting delayed presentation of symptomatic breast cancer: a systematic review. Lancet. 1999;353(9159):1127–1131. doi: 10.1016/s0140-6736(99)02142-x. [DOI] [PubMed] [Google Scholar]
- 7.McDonald S, Saslow D, Alciati MH. Performance and reporting of clinical breast examination: a review of the literature. CA Cancer J Clin. 2004;54(6):345–361. doi: 10.3322/canjclin.54.6.345. [DOI] [PubMed] [Google Scholar]
- 8.Dey S. Preventing breast cancer in LMICs via screening and/or early detection: the real and the surreal. World J Clin Oncol. 2014;5(3):509–519. doi: 10.5306/wjco.v5.i3.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alwan NA, Al-Diwan JK, Wafa’M A-A, Eliessa RA. Knowledge, attitude & practice towards breast cancer & breast self examination in Kirkuk University, Iraq. Asian Pac J Reproduction. 2012;1(4):308–311. [Google Scholar]
- 10.Al-Naggar RA, Al-Naggar DH, Bobryshev YV, Chen R, Assabri A. Practice and barriers toward breast self-examination among young Malaysian women. Asian Pac J Cancer Prev. 2011;12(5):1173–1178. [PubMed] [Google Scholar]
- 11.Stapleton JM, Mullan PB, Dey S, et al. Patient-mediated factors predicting early- and late-stage presentation of breast cancer in Egypt. Psychooncology. 2011;20(5):532–537. doi: 10.1002/pon.1767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pei Lin L, Zakaria NS. Breast cancer and chemotherapy knowledge among undergraduates of health sciences: which traits predict good knowledge? Malays J Med Sci. 2013;20(1):60–68. [PMC free article] [PubMed] [Google Scholar]
- 13.Seah M, Tan SM. Am I breast cancer smart? Assessing breast cancer knowledge among health professionals. Singapore Med J. 2007;48(2):158–162. [PubMed] [Google Scholar]
- 14.McMichael C, Kirk M, Manderson L, Hoban E, Potts H. Indigenous women’s perceptions of breast cancer diagnosis and treatment in Queensland. Aust N Z J Public Health. 2000;24(5):515–519. doi: 10.1111/j.1467-842x.2000.tb00502.x. [DOI] [PubMed] [Google Scholar]
- 15.Waller J, Douglas E, Whitaker KL, Wardle J. Women’s responses to information about overdiagnosis in the UK breast cancer screening programme: a qualitative study. BMJ Open. 2014;3(4):e002703. doi: 10.1136/bmjopen-2013-002703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lamyian M, Hydarnia A, Ahmadi F, Faghihzadeh S, Aguilar-Vafaie ME. Barriers to and factors facilitating breast cancer screening among Iranian women: a qualitative study. East Mediterr Health J. 2007;13(5):1160–1169. doi: 10.26719/2007.13.5.1160. [DOI] [PubMed] [Google Scholar]
- 17.McAllister MF, Evans DG, Ormiston W, Daly P. Men in breast cancer families: a preliminary qualitative study of awareness and experience. J Med Genet. 1998;35(9):739–744. doi: 10.1136/jmg.35.9.739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Given LM. The Sage Encyclopedia of Qualitative Research Methods. SAGE Publications, Inc; Thousand Oaks, California, USA: 2008. [Google Scholar]
- 19.Twenty First Session of the Governing Council, UN HABITAT, 16–20 April 2007, Nairobi, Kenya. Kenya: 2007. pp. 1–3. [Google Scholar]
- 20.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. [Google Scholar]
- 21.Kissal A, Beser A. Knowledge, facilitators and perceived barriers for early detection of breast cancer among elderly Turkish women. Asian Pac J Cancer Prev. 2011;12(4):975–984. [PubMed] [Google Scholar]
- 22.Dey S, Mishra A, Govil J, Dhillon PK. Breat cancer awareness at the community level among women in Delhi, India. Asia Pac J Cancer Prev. 2015;16(13):5243–5251. doi: 10.7314/apjcp.2015.16.13.5243. [DOI] [PubMed] [Google Scholar]
- 23.Ersin F, Bahar Z. Inhibiting and facilitating factors concerning breast cancer early diagnosis behavior in Turkish women: a qualitative study according to the health belief and health development models. Asian Pac J Cancer Prev. 2011;12(7):1849–1854. [PubMed] [Google Scholar]
- 24.Khazaee-pool M, Majlessi F, Foroushani AR, et al. Perception of breast cancer screening among Iranian women without experience of mammography: a qualitative study. Asian Pac J Cancer Prev. 2014;15(9):3965–3971. doi: 10.7314/apjcp.2014.15.9.3965. [DOI] [PubMed] [Google Scholar]
- 25.Taha H, Al-Qutob R, Nystrom L, Wahlstrom R, Berggren V. “Voices of fear and safety” women’s ambivalence towards breast cancer and breast health: a qualitative study from Jordan. BMC Womens Health. 2012;12:21. doi: 10.1186/1472-6874-12-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhang W, Rose SB, Foster A, Pullon S, Lawton B. Breast cancer and breast screening: perceptions of Chinese migrant women living in New Zealand. J Prim Health Care. 2014;6(2):135–142. [PubMed] [Google Scholar]
- 27.Banning M, Hafeez H. Perceptions of breast health practices in Pakistani Muslim women. Asian Pac J Cancer Prev. 2009;10(5):841–847. [PubMed] [Google Scholar]
- 28.Park S, Hur HK, Kim G, Song H. Knowledge, barriers, and facilitators of Korean women and their spouses in the contemplation stage of breast self-examination. Cancer Nurs. 2007;30(1):78–84. doi: 10.1097/00002820-200701000-00014. [DOI] [PubMed] [Google Scholar]
- 29.Sadler GR, Ko CM, Cohn JA, White M, Weldon RN, Wu P. Breast cancer knowledge, attitudes, and screening behaviors among African American women: the Black cosmetologists promoting health program. BMC Public Health. 2007;7:57. doi: 10.1186/1471-2458-7-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bodapati SL, Babu GR. Oncologist perspectives on breast cancer screening in India-results from a qualitative study in Andhra Pradesh. Asian Pac J Cancer Prev. 2013;14(10):5817–5823. doi: 10.7314/apjcp.2013.14.10.5817. [DOI] [PubMed] [Google Scholar]
- 31.Kawar LN. Barriers to breast cancer screening participation among Jordanian and Palestinian American women. Eur J Oncol Nurs. 2013;17(1):88–94. doi: 10.1016/j.ejon.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 32.Filippi MK, Ndikum-Moffor F, Braiuca SL, et al. Breast cancer screening perceptions among American Indian women under age 40. J Cancer Educ. 2013;28(3):535–540. doi: 10.1007/s13187-013-0499-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Engelman KK, Cizik AM, Ellerbeck EF, Rempusheski VF. Perceptions of the screening mammography experience by Hispanic and non-Hispanic White women. Womens Health Issues. 2012;22(4):e395–e401. doi: 10.1016/j.whi.2012.04.006. [DOI] [PubMed] [Google Scholar]
- 34.Al Dasoqi K, Zeilani R, Abdalrahim M, Evans C. Screening for breast cancer among young Jordanian women: ambiguity and apprehension. Int Nurs Rev. 2013;60(3):351–357. doi: 10.1111/inr.12025. [DOI] [PubMed] [Google Scholar]