ABSTRACT
Background:
Helicobacter pylori has been extensively studied since 1982 it is estimated that 50% of the world population is affected. The literature lacks studies that show the change of its prevalence in the same population over time.
Aim:
To compare the prevalence of H. pylori in 10 years interval in a population that was submitted to upper endoscopy in the same endoscopy service.
Method:
Observational, retrospective and cross-sectional study comparing the prevalence of H. pylori in two samples with 10 years apart (2004 and 2014) who underwent endoscopy with biopsy and urease. Patients were studied in three consecutive months of 2004, compared to three consecutive months of 2014. The total number of patients was 2536, and 1406 in 2004 and 1130 in 2014.
Results:
There were positive for H. pylori in 17 % of the sample as a whole. There was a significant decrease in the prevalence from 19.3% in 2004 to 14.1% in 2014 (p<0.005).
Conclusion:
There was a 5.2% reduction in the prevalence of H. pylori comparing two periods of three consecutive months with 10 years apart in two equivalent population samples.
HEADINGS: Helicobacter pylori, Endoscopy, Urease test
RESUMO
Racional:
Helicobacter pylori vem sendo amplamente estudado desde 1982 estimando-se que 50% da população mundial esteja afetada. A literatura carece de estudos que mostrem a mudança de sua prevalência em uma mesma população ao longo do tempo.
Objetivo:
Comparar a prevalência do H.pylori no intervalo de 10 anos em população que realizou endoscopia digestiva alta no mesmo serviço de endoscopia.
Método:
Estudo observacional, retrospectivo e transversal, comparando a prevalência de H. pylori em duas amostras com intervalo de 10 anos (2004 e 2014) que realizaram endoscopia digestiva alta com biópsias e teste da urease para a pesquisa de H. pylori. Foram estudados pacientes em três meses consecutivos de 2004, comparados aos de três meses consecutivos de 2014. O número total de pacientes avaliados foi 2536, sendo 1406 em 2004 e 1130 em 2014.
Resultados:
Constatou-se resultado positivo para H.pylori em 17% da amostra como um todo. Houve queda significativa da prevalência de H.pylori de 19,3% em 2004 para 14,1% em 2014 (p<0.005).
Conclusão:
Houve redução de 5,2% da prevalência de H. pylori comparando-se dois períodos de três meses consecutivos com intervalo de 10 anos em duas amostras populacionais equivalentes.
INTRODUCTION
Gastric micro-organisms were observed for more than 100 years 7 , but its association with gastric diseases was recognized from 1982, when Marshall and Warren identified and subjected to culture the bacteria Campylobacter pyloridis later reclassified as Helycobacter pylori (HP) 7 , 21 .
This gram-negative bacterium, a spiral, microaerophilic aspect, quite resistant and may remain alive for long periods of time outside the human body, water, vegetable and feces. Contamination of water supply reservoirs in developing countries can serve as an environmental source. Using the polymerase chain reaction technique, HP was found in most water samples from supply reservoirs in endemic infected areas 7 . In a study conducted in South Korea, analyzing risk factors for HP, there was contamination of 3% natural source of water, 92% in the city reservoirs and 66% in bottled water 20 .
HP has been diagnosed throughout the world and in all age groups. It is estimated that 50% of the world population is infected 7 . It was isolated in animals, milk, raw vegetables, feces, vomiting and water. Its transmission is oral-oral and fecal-oral between humans, with a higher prevalence in the low-income population, where contamination begins during childhood linked with poor housing, food and hygiene 1 , 12 , 20 , 27 , 29 . In developing countries, where most children are infected before age 10, the adult prevalence reaches 80% before 50 years 7 . Several studies indicate that decrease in incidence and prevalence of HP progressively in the last 20 years is related to the industrialization and improvement of health and socio-cultural conditions in different countries 1 , 16 , 20 , 24 , 27 , 28 , 29 .
This bacterium is biochemically characterized as being urease-dependent, being of importance to invasive and noninvasive diagnostic tests 9 , 15 , 18 , 19 , 22 , 24 , 25 , 27 , 28 , 29 .
The recommendation of the American College of Gastroenterology in 2007 is to realize HP urease test in patients with dyspepsia, active ulcer or history of ulcer, lymphomas, in chronic use of proton pump inhibitors and steroid anti-inflammatories 3 ; in anemic patients with vitamin B12 and iron deficiency; and asymptomatic patients with a family history of gastric cancer or in families with HP treatment 4 , 9 , 10 , 23 , 24 , 29 . In Brazil, the III HP Brazilian Consensus in 2012, had as one of the goals disclose and guide dietetic and hygiene measures to the population, develop strategies with the Ministry of Health to improve sanitation and water reservoirs and guide health professionals regarding HP prevention , diagnosis and treatment 2 , 3 , 4 , 6 , 9 , 11 , 12 , 14 , 25 , 30 .
In São Paulo, SP, Brazil, the total estimated population in 2015 was 11,968,000 people. The study of HP prevalence in two periods with an interval of 10 years, in a population with similar characteristics, can provide information on how this infection is behaving over time and help to orientate prevention and treatment. It is likely that, as in other countries, can be detected changes in prevalence in accordance with the dietetic and hygiene changing conditions of each region 7 , 20 , 29 .
Thus, this epidemiological study aims to compare the prevalence of HP in the 10 year range in population that held endoscopy in the same endoscopy service and with the same population characteristics.
METHOD
This is an observational, retrospective and cross study comparing the prevalence of HP in two groups of patients, 10 years apart (2004 and 2014) who underwent endoscopy with biopsy and urease test for HP systematically done in the Service of Digestive Endoscopy, Diagnostic Center and Endoscopic Therapy of São Paulo, 9 of July Hospital, São Paulo, SP, Brazil.
The total number of patients who underwent endoscopy in 2004 was 6121 patients, and in 2014 to 6352. Were assessed those who underwent tests in three consecutive months (January, February and March) of 2004 (n=1406) and 2014 (n=1130), a total of 2536 patients. Were excluded patients on anticoagulant treatment and unable to perform biopsies. All endoscopies were with sedation by midazolam and fentanyl citrate.
Systematically were done three biopsies (antrum, incisura angularis and gastric body) and urease test in all endoscopies. The following variables were analyzed: year, gender, HP test results, age, gross appearance of the mucosa (normal endoscopy or pathological changes).
Statistical analysis
The data were submitted to the Pearson chi-square test.
RESULTS
The collected data are summarized in Table 1.
TABLE 1. Descriptive data analysis .
| Variables | Total number of patients n=2536(100%) | Patients HP+ n=432(100%) | Patients HP- n=2104(100%) |
| Year | |||
| Total 2004 | 1406 (100%) | 272 (19.3%) | 1134 (80.7%) |
| Total 2014 | 1130 (100%) | 160 (14.1%) | 970 (85.9%) |
| Gender | |||
| Total female | 1624 (100%) | 256 (15.7%) | 1368 (84.3%) |
| Total male | 912 (100%) | 176 (19.3%) | 736 (80.7%) |
| HP resultsTotal sample | |||
| 2536 (100%) | 432(17.0%) | 2104(83.0%) | |
| Age | |||
| < 10 y | 2536 (100%) | 432 (100%) | 2104 (100%) |
| 09 (0.4%) | 01 (0.2%) | 08 (0.4%) | |
| 11-20 y | 69 (2.7%) | 04 (1.0%) | 65 (3.1%) |
| 21-30 y | 377 (14.8%) | 61 (14.2%) | 316(15.0%) |
| 31-40 y | 526 (20.7%) | 80 (18.5%) | 446(21.2%) |
| 41-50 y | 484 (19.2%) | 190(43.8%) | 294(14.0%) |
| 51-60 y | 534 (21.0%) | 45 (10.4%) | 489(23.3%) |
| Over 61 y | 537 (21.2%) | 51 (11.9%) | 486(23.0%) |
| Normal endoscopy/with alterations | |||
| Total normal endoscopies | 134 (100%) | 22 (16.5%) | 112 (83.5%) |
| Total endoscopies with alterations | 2402 (100%) | 410 (17.0%) | 1992 (83.0%) |
In 2004 the prevalence of HP was equal to 19.3%; already in 2014 it dropped down to 14.1%.
The proportion of women in total (64%) was higher than that of men (36%). Of the 1624 women, 256 (15.7%) were HP+ and 1368 (84.3%) HP-. Of the 912 men, 176 (19.3%) were HP+ and 736 (80.7%) HP-.
In the sample as a whole (n=2536) there were 17% (n=432) positive results for HP. In 2004 its prevalence was 19.3% (n=272), and in 2014 dropped to 14.1% (n=160), p<0.005 (Table 2).
TABLE 2. HP result vs. year.
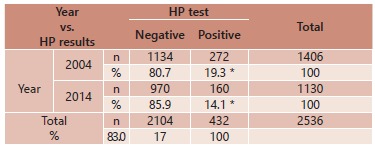
*p<0,005; HP=Helicobacter pylori
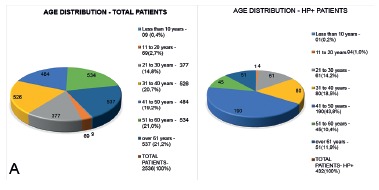
In Figure 1A it can be observed the distribution of all patients (n=2536) by age group. In Figure 1B it can be seen the distribution only HP+ (n=432, 17% of the total sample) distributed for the same age groups.
FIGURE 1. Age distribution vs. presence of HP .
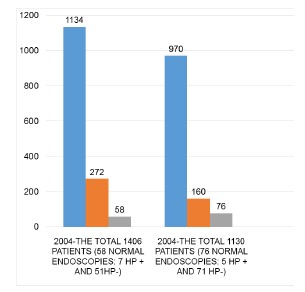
In 2004 from 1406 patients, HP- was seen in 1134 patients, being 51 with normal endoscopy (4.5%) and 1083 showing some alteration (95.5%). Of the 272 patients with PH+ seven had normal endoscopy (2.6%) and 265 related some disease (97.4%). The total of normal endoscopies in 2004 was in 58 patients (Table 3).
TABLE 3. Normal endoscopy, with alterations and HP+/- in 2004+2014, 2004 e 2014.
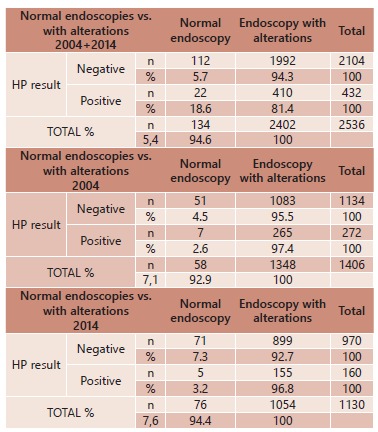
In 2014 from 1130 patients HP- was seen in 970, being 71 with normal endoscopy (7.3%) and 899 with alterations (92.7%). Of the 160 HP+ five had normal endoscopy (3.2%) and 155 with some disease (96.8%). The total of normal endoscopies in 2014 was 76 (Table 3).
There was an increase of normal and HP- endoscopies in 10-year period (4.5% in 2004 and 7.3% in 2014). There was a significant reduction of HP+ in patients with endoscopy with some disease (97.4% in 2004 and 96.8% in 2014) in the same period (Table 3). There was a reduction of 5.2% of HP+ prevalence (19.3% in 2004 to 14.1% in 2014) that was statistically significant (p<0.005). The sample consisted mostly of women (64%). The highest incidence of HP+ in this sample was between 41 and 50 years (43.87%).
Of the total of 2536 endoscopes in both years, only 134 were normal with no mucosal alterations (Figure 2).
FIGURE 2. Distribution of patients HP+, HP- and normals in 2004 and 2014.
DISCUSSION
The variation of HP prevalence in different regions of the world is mainly related to socioeconomic factors 7 , 16 , 20 , 25 , 29 . It is observed that in developed countries it is lower since childhood, and the regions that showed socioeconomic growth in the past 20 years decreased significantly 20 , 29 .
In developing countries, most children are infected before age 10 and the adult prevalence reaches 80% before age 50; in developed countries like the United States, the incidence of HP is rare in children under 10 years and increases to 10% between 18-30 years 7 , 29 .
This is attributed to the fact that in developed societies, the population has access to sanitation, hygiene, health (medical and dental) and guidance for prevention and treatment11,12,14,17,18,19,26,29 30.
Because HP is the most common infection in humans, and as a consequence of its chronic character, may trigger serious diseases with considerable morbidity 1 , 3 , 4 , 5 , 8 , 13 , 19 , 20 , 30 . Comparative study of its prevalence in distinct regions over the years is of great importance to analyze if the health improvement of population translate into reducing the prevalence, as well as guiding strategies and guidelines for the prevention and specific treatment for each area proportional to the degree of socioeconomic and cultural development 2 , 7 , 11 , 12 , 14 , 20 , 26 , 28 , 29 .
Regarding the studied São Paulo population in private service, the prevalence of HP fell significantly in a decade, and there was also a reduction in its incidence in patients with endoscopies with some disease.
It is possible that these findings are a result of greater public awareness of the quality of food, the preventive health care (medical and dental) and discipline following the medical guidelines. It is possible also to believe that an important factor for this favorable development is broad access to information that has been occurring in recent years. If these conditions remain unchanged over time, will happen further decline in this prevalence, as currently already occurs in developed countries.
Further studies are needed in regions with different levels of socioeconomic development, to check the HP prevalence in the population in the coming years.
CONCLUSION
It was observed significant reduction in the prevalence of HP comparing two periods of three consecutive months with an interval of 10 years, in two similar population samples. There was a reduction of 5.2% of HP+ prevalence, falling from 19.3% in 2004 to 14.1% in 2014.
Footnotes
Financial source: none
REFERENCES
- 1.Araújo M. B., Borini P., Guimarães R. C. Etiopathogenesis of peptic ulcer: back to the past? Arquivos de Gastroenterologia. 51(2):155–161. doi: 10.1590/s0004-28032014000200016. [DOI] [PubMed] [Google Scholar]
- 2.Bruyne E.D., Ducatelle R., Foss D., Sanchez M., Joosten M., Zhang G., Smet A., Pasmans F., Haesebrouck F., Flahou B. Oral glutathione supplementation drastically reduces Helicobacter-induced gastric pathologies. Sci. Rep. 2016;6:20169–20169. doi: 10.1038/srep20169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Camilo S. M. P., Almeida É. C. de S., Miranzi B. A. S., Silva J. C., Nomelini R. S., Etchebehere R. M. Endoscopic and histopathologic gastric changes in chronic users of proton-pump inhibitors. Arquivos de Gastroenterologia. 2015;52(1):59–64. doi: 10.1590/S0004-28032015000100013. [DOI] [PubMed] [Google Scholar]
- 4.Carli D. M. de, Pires R. C., Rohde S. L., Kavalco C. M., Fagundes R. B. Peptic ulcer frequency differences related to h. Pylori or aines. Arquivos de Gastroenterologia. 2015;52(1):46–49. doi: 10.1590/S0004-28032015000100010. [DOI] [PubMed] [Google Scholar]
- 5.Chmiela M., Miszczyk E., Rudnicka K. Structural modifications of Helicobacter pylori lipopolysaccharide: An idea for how to live in Peace. World Journal of Gastroenterology. 2014;7(20) 29:9882–9897. doi: 10.3748/wjg.v20.i29.9882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coelho L.G.V., Zaterka S., Maguinilk I, Parente J.M., Passos M.C.F., Moraes-Filho J.P.P. III Consenso Brasileiro sobre Helicobacter pylori. Arquivos de Gastroenterologia. 2012 doi: 10.1590/s0004-28032005000200012. [DOI] [PubMed] [Google Scholar]
- 7.Crowe SE. Bacteriology and epidemiology of Helicobacter pylori infection. Up to Date; 2016. [Google Scholar]
- 8.Crowe SE. Pathophysiology of and imune response to Helicobacter pylori infection. Up to Date; 2016. [Google Scholar]
- 9.Crowe SE. Indications and diagnostic tests for Helicobacter pylori infection. Up to Date; 2016. [Google Scholar]
- 10.Danielli A., Amore G., Scarlato V. Built shallow to maintain homeostasis and persistent infection: Insight into the transcriptional regulatory network of the gastric human pathogen Helicobacter pylori. PLoS Pathogens. 2010;6:6–6. doi: 10.1371/journal.ppat.1000938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Flesch A. G. T., Poziomyck A. K., Damin D. D. C. The therapeutic use of symbiotics. ABCD. Arquivos Brasileiros de Cirurgia Digestiva (São Paulo) 2014;27(3):206–209. doi: 10.1590/S0102-67202014000300012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gebara ECE. Evaluation of the oral cavity of patients with periodontal disease as reservoir of Helicobacter pylori. LILACS; 2004. [Google Scholar]
- 13.Gomes A., Skare T. L., Prestes M. A., Costa M. da S., Petisco R. D., Ramos G. P. Conventional Videoendoscopy can identify Helicobacter pylori gastritis? ABCD. Arquivos Brasileiros de Cirurgia Digestiva (São Paulo) 2016;29(2):73–76. doi: 10.1590/0102-6720201600020002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guarner F., Khan A.G., Garisch J., Eliakim R., Gangl A., Thomsom A., Krabshuis J., tl. Mair. World Gastroenterology Organization Global Guidelines. 2011. Probióticos e Prebióticos. [Google Scholar]
- 15.Jung S. W., Lee S. W. The antibacterial effect of fatty acids on Helicobacter pylori infection. The Korean Journal of Internal Medicine. 2016;31(1):30–35. doi: 10.3904/kjim.2016.31.1.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khedmat H., Afshar R.K, Agah S, Taheri S.,MD. Helicobacter pylori infection in the general population: A Middle Eastern perspective. Caspian Journal of Internal Medicine. 2013;4(4):1–1. [PMC free article] [PubMed] [Google Scholar]
- 17.Lasa J., Zubiaurre I., Dima G., Peralta D., Soifer L. Helicobacter Pylori prevalence in patients with celiac disease: results from a cross-sectional study. Arquivos de Gastroenterologia. 2015;52(2):139–142. doi: 10.1590/S0004-28032015000200012. [DOI] [PubMed] [Google Scholar]
- 18.Lopes AI, Filipa F.V., Oleastro M. Helicobacter pylori infection - recente developments in diagnosis. World Journal of Gastroenterology. 2014;20(28):9299–9313. doi: 10.3748/wjg.v20.i28.9299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Magalhães-Costa M. H. de, Reis B. R. dos, Chagas V. L. A., Nunes T., Souza H. S. P. de, Zaltman C. Focal enhanced gastritis and macrophage microaggregates in the gastric mucosa: potential role in the differential diagnosis between Crohn's disease and ulcerative colitis. Arquivos de Gastroenterologia. 2014;51(4):276–282. doi: 10.1590/S0004-28032014000400003. [DOI] [PubMed] [Google Scholar]
- 20.Malaty H. M., Kim J. G., Kim S. D., Graham D. Y. Prevalence of Helicobacter pylori Infection in Korean Children: Inverse Relation to Socioeconomic Status Despite a Uniformly High Prevalence in Adults. American Journal of Epidemiology. 1996;143(3):257–262. doi: 10.1093/oxfordjournals.aje.a008736. [DOI] [PubMed] [Google Scholar]
- 21.Marchall B.J., Warren J.R. Unidentified curved bacilli in the stomach of patients with gastrites and peptic ulceration. The Lancet; Up to Date; 2016. [DOI] [PubMed] [Google Scholar]
- 22.Mattar R., Villares C. A., Marostegam P. F. F., Chaves C. E., Pinto V. B., Carrilho F. J. Low dose capsule based 13c-urea breath test compared with the conventional 13c-urea breath test and invasive tests. Arquivos de Gastroenterologia. 2014;51(2):133–138. doi: 10.1590/s0004-28032014000200012. [DOI] [PubMed] [Google Scholar]
- 23.Moges F., Kassu A., Mengistu G., Adugna S., Andualem B., Nishikawa T., Ota F. Seroprevalence of Helicobacter pylori in dyspeptic patients and its relationship with HIV infection, ABO blood groups and life style in a university hospital, Northwest Ethiopia. World Journal of Gastroenterology. 2006;12(12):1957–1961. doi: 10.3748/wjg.v12.i12.1957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Oliveira J. G. de, Ferreira C. H. T., Camerin A. C. S., Rota C. A., Meurer L., Silveira T. R. da. Prevalence of infection with cagA-positive Helicobacter Pylori strains among children and adolescents in southern Brazil. Arquivos de Gastroenterologia. 2014;51(3):180–185. doi: 10.1590/s0004-28032014000300003. [DOI] [PubMed] [Google Scholar]
- 25.Patel S.K., Pratap C.B., Jain A.K., Gulati A.K., Nath G. Diagnosis of Helicobacter pylori: what should be the gold standart. World Journal of Gastroenterology. 2014;20(36):12847–12859. doi: 10.3748/wjg.v20.i36.12847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Safavi M., Sabourian R., Foroumadi A. Treatment of Helicobacter pylori infection: current and future insights. World Journal of Clinical Cases. 2016;16(4) 1:5–19. doi: 10.12998/wjcc.v4.i1.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Seo J.H., Park H.K., Park J.S., Yeom J.S., Lim J.Y., Park C.H., Woo H.O., Youn H.S., Jun J.S., Ko G.H., Baik S.C., Lee W.K., Cho M.J., Rhee K.H. Association between gastric ph and Helicobacter pylori infection in children. Pediatric Gastroenterology, Hepatology & Nutrition. 2015;18(4):246–252. doi: 10.5223/pghn.2015.18.4.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Testerman T.L., Morris J. Beyond the stomach: Na updated view of Helicobacter pylori pathogenesis, diagnosis, and treatment. World Journal of Gastroenterology. 2014;20(36):12781–12808. doi: 10.3748/wjg.v20.i36.12781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vinagre I. D. F., Queiroz A. L. de, Silva M. R. da, Júnior, Vinagre R. M. D. F., Martins L. C. Helicobacter Pylori infection in patients with different gastrointestinal diseases from northern Brazil. Arquivos de Gastroenterologia. 2015;52(4):266–271. doi: 10.1590/S0004-28032015000400004. [DOI] [PubMed] [Google Scholar]
- 30.Vomero N. D., Colpo E. Nutritional care in peptic ulcer. Arquivos Brasileiros de Cirurgia Digestiva : ABCD = Brazilian Archives of Digestive Surgery. 27(4):298–302. doi: 10.1590/S0102-67202014000400017. [DOI] [PMC free article] [PubMed] [Google Scholar]


