Summary
Acute myeloid leukemia (AML) is now recognized to be an imprecise term that refers to a range of myeloid malignancies which have different genetical etiologies, clinical characteristics, and therapeutic sensitivities. Targeting the MLL1 and DOT1L histone modification complexes, both alone and in combination, showed activity against AML driven by an NPM1 mutant protein in several pre-clinical models, and may represent a new treatment direction for this devastating disease.
Progress in the development of effective novel therapeutics for treatment of acute myeloid leukemia (AML) has been generally disappointing, and clinical outcomes remain generally suboptimal. The notable exception to this trend is the remarkable advances seen in acute promyelocytic leukemia (APL), with remission and long term survival rates improving from less than 15% to greater than 90% over the past fifty years(1). These improvements occurred following the recognition of APL as a clinical entity distinct from other forms of AML, with different underlying biology and hence potential unique therapeutic sensitivities. While mechanistic understanding of successful targeted therapy in APL occurred after clinical success it did provide a template for how improved disease definition into subgroups based on underlying etiology rather than phenotype may provide opportunities for targeted intervention. It is now clear that APL is not a special case, and that earlier morphology and cytogenetic based classifications did not adequately reflect the diverse genetic etiology of the broad class of myeloid malignancies labeled as acute myeloid leukemia (AML).
Technological advances over the past decade have allowed high throughput DNA sequencing of thousands of primary AML patient samples (2). This has revealed a catalog of recurrent somatic mutations in less than eighty genes or genomic regions, which can be used to segregate AML patients into one of approximately one dozen subgroups with potentially differing predictive and prognostic significance. In the recently updated World Health Organization (WHO) diagnostic classification, AML with mutated nucleophosmin (NPM1mut) is now recognized as a distinct subset, with the presence of this somatic mutation now superseding traditional morphological descriptors such as multilineage dysplasia(3). NPM1 mutations are found in 25-30% of AML patients, making it the second most common recurrent somatic mutation and the distinguishing feature of the largest genomic subgroup (2).
NPM1 ordinarily functions as an intracellular chaperone, and when mutated is characterized by aberrant cytoplasmic localization detectable by immunohistochemistry. While greater than 50 variants of NPM1 mutation have been described, almost all are four base pair insertions within exon 12, which lead to a frameshift and premature truncation of the NPM1 protein. NPM1 mutations are found in adult AML patients of all ages, but are less common in children, particularly those under three years of age(4). Patients with NPM1mut AML commonly have co-mutated DNMT3A and/or FLT3-ITD, and are associated with a characteristic gene expression profile including downregulation of CD34 and HOX gene upregulation. Mutations in NPM1 are typically seen in association with normal karyotype AML(NKAML); approximately 85% of NPM1mut is NK-AML and greater than 50% of NK-AML has an NPM1 mutation(5).
Despite the clear clinical relevance of NPM1mut as a potential target for AML therapy, its mechanism of action remains incompletely understood. Several lines of investigation have suggested that enforced expression of HOX genes, especially HOXA7/9/10 (hereafter referred to as the “HOXA cluster”), and the HOX binding factor MEIS1 are important for the oncogenic ability of the NPM1 mutant protein, and it has been speculated that cytoplasmic sequestration of proteins by the NPM1mut indirectly leads to enforced expression of HOXA cluster and MEIS1 genes (6). The HOXA cluster has been shown to be an important regulator of myeloid differentiation in mammals; these genes are highly expressed in hematopoietic stem and progenitor cells, and their expression becomes extinguished as cells differentiate to monocytes and neutrophils. Of note, several other recurrent chromosomal abnormalities associated with AML in humans, including MLL1 translocations, NUP98 translocations, and monosomy 7 are associated with overexpression of the HOXA cluster and MEIS1, suggesting that enforced expression of these genes may be a common pathway associated with AML. Indeed, gene expression profile studies have shown that this HOXA cluster is overexpressed in approximately half of all AML patients, and HOXA cluster overexpression is mutually exclusive with favorable cytogenetic [(inv 16), t(8;21), or t(15;17) features (6)
Kuhn and colleagues (7) predicted that wild type (WT) MLL1 might be a critical regulator of HOXA cluster expression in the context of NPM1mut AML. They used CRISPR-Cas9 reagents to perform a structure/function analysis of MLL1 in the context of NPM1mut AML, and found that the menin-MLL1 binding surface was required for the leukemogenic effect of NPM1mut mutant protein. Realizing that this finding suggested an indirect mechanism to target NPM1mut, the authors proceeded to show that a small molecule inhibitor of MLL1-menin binding (designated MI-503) could down-regulate expression of HOXA cluster genes and MEIS1. This gene downregulation was accompanied by growth inhibition and increased differentiation of the AML cells. Given that MEIS1 has previously been shown to be an important upstream regulator of FLT3 (8), the authors showed that FLT3 expression was also suppressed by treatment with MI-503(8). Using both xenotransplant and NPM1mut knock-in models, the authors showed that MI-503 treatment was also effective in vivo; this treatment was also associated with loss of menin binding at the Hox and Meis1 loci (7).
DOT1L is an H3K79 histone methyltransferase that is known to interact with MLL1 fusion partners such as AF9 and AF10; this interaction is important for oncogenic mis-regulation of HOXA cluster gene expression in cells with MLL1-fusions (9). Moreover, DOT1L histone methyltransferase activity is critical for proper regulation of HOXA cluster gene expression in wild type hematopoietic cells. The authors had previously shown that DOT1L inhibitors could decrease the oncogenic potential of MLL fusion proteins, by decreasing HOXA and MEIS gene expression. Because the enforced expression of HOXA and MEIS1 in NPM1mut leukemic cells was associated with H3K79 di/tri-methylation, the authors tested the potential for a small molecule inhibitor of DOT1L, designated EPZ4777, to decrease leukemic cell growth and HOX/MEIS1 gene expression in NPM1mut AML cells (7). Treatment of an NPM1mut knock-in model in vivo showed a survival advantage accompanied by myeloid differentiation in the treated mice, similar to the findings with the menin-MLL1 inhibitor.
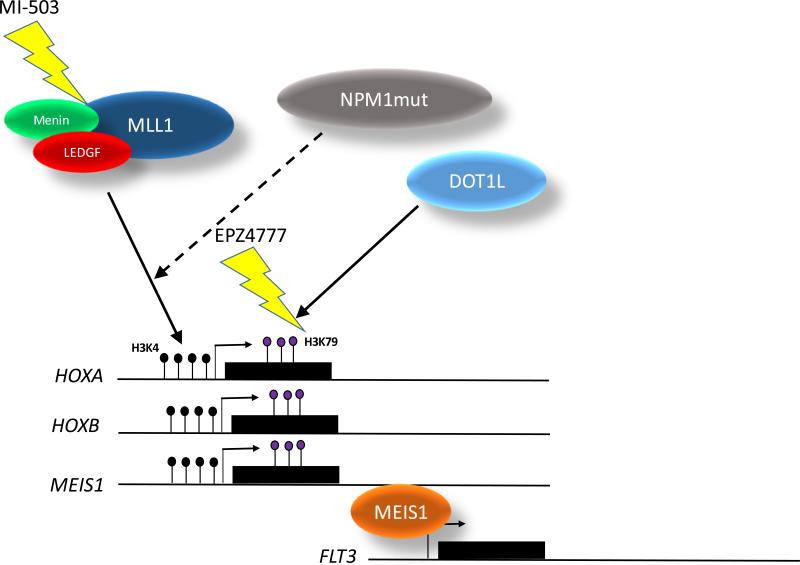
Combination of the menin-MLL1 inhibitor (MI-503) and DOT1L inhibitor (EPZ4777) led to synergistic suppression of HOXA/MEIS1 expression, and growth, accompanied by monocytic and myeloid differentiation of NPM1mut cells. In vivo, combination of MI-503 and EPZ4777 led to increased survival and decreased numbers of leukemia initiating cells. The downregulation of MEIS1 seen in these experiments was associated with a marked decrease in FLT3 expression; this finding is consistent with the observation that FLT3 has been shown to be a direct transcriptional target of MEIS1 (8). The concomitant targeting of menin-MLL1 binding and DOT1L may enable the simultaneous indirect targeting of both NPM1mut and FLT3 (Figure 1); this approach is of potential clinical relevance given that combined mutations of NPM1 and FLT3 are common in AML patients, and predict an unfavorable outcome. The authors also showed that several HOXB cluster genes important for normal or malignant hematopoiesis, such as HOXB2, B3, B4, and B8 were downregulated by one or both of these agents.
Figure. Simultaneous inhibition of menin-MLL1 binding and DOT1L methyltransferase activity leads to decreased HOX, MEIS1, and FLT3 expression, resulting in leukemic cell death.
The MLL1 complex, including MLL1, menin, and LEDGF methylates H3K4 residues at the HOXA, HOXB, and MEIS1 loci, leading to transcriptional activation of the loci. This action is facilitated by NPM1mut protein through an unknown mechanism. MI-503 disrupts menin-MLL1 binding, leading to loss of HOXA, HOXB, and MEIS1 expression. DOT1L methylates H3K79 residues, enabling transcriptional elongation; DOT1L methyltransferase activity is inhibited by EPZ4777. MEIS1 protein stimulates FLT3 transcription. Black lollipops represent H3K4 residues; purple lollipops represent H3K79 residues.
These experiments highlight the potential of targeting HOX and MEIS1 expression by indirect means. This strategy is important since HOX and MEIS1 proteins have been regarded as difficult targets, given their hydrophobic binding surfaces. Moreover, the HOXA cluster genes, and to a lesser extent, the HOXB cluster, are often coordinately regulated in AML patients(6), suggesting that targeting a single HOX protein may not be effective, due to a functional redundancy among these HOX genes. For instance, although HOXA9 is the HOX gene most commonly overexpressed in leukemia, an MLL-AF9 fusion can transform HOXA9 −/− hematopoietic cells, indicating that HOXA9 expression is not required for leukemic transformation (10). The experiments by Kuhn et al suggest a clever means to circumvent this problem, by attacking a critical regulator upstream of HOX and MEIS1 genes.
A number of important questions remain unanswered. NPM1mut expression is associated with enforced expression of HOXA/B genes and MEIS1; the current study demonstrates that menin-MLL1 interaction as well as DOT1L histone methyltransferase activity are important for this phenomenon. However, the mechanism by which NPM1mut expression leads to HOXA/B and MEIS1 expression remains unknown. Similarly, the mechanism by which DOT1L inhibition leads to decreased HOXA/B and MEIS1 expression in NPM1mut leukemia cells is unclear. In contrast to MLL-AF9 or MLL-AF10 fusions, in which a direct interaction between DOT1L and AF9 or AF10 has been demonstrated, no direct interaction between DOT1L and wild-type MLL1 has been demonstrated. Moreover, the in vivo experiments performed by Kuhn and colleagues to demonstrate synergism between the two agents used ex vivo pre-treatment of NPM1mut cells, presumably due to unfavorable pharmacokinetic or toxicity profiles. Ultimately, this hurdle will need to be cleared before early phase clinical trials using this combination can begin. Finally, NPM1mut AML may be associated with a variety of co-mutated genes and the combinational impact of additional mutations on targeted therapy remains to be elucidated. Despite these questions and caveats, this indirect approach for targeting a very common clinical abnormality remains an attractive goal for treatment of patients with NPM1mut positive AML.
Acknowledgments
Grant support:
This work was supported by the Intramural Research Program of the National Cancer Institute (Grant #s ZIA SC 010378 and ZIA BC 010982 to PDA) and National Heart, Lung and Blood Institute (Grant ZIA HL 006163 to CSH) of the National Institutes of Health.
CSH receives collaborative research funding from Sellas Life Sciences Group AG.
Footnotes
Conflict of Interest:
PDA declares no conflicts of interest.
References
- 1.Platzbecker U, Avvisati G, Cicconi L, Thiede C, Paoloni F, Vignetti M, et al. Improved Outcomes With Retinoic Acid and Arsenic Trioxide Compared With Retinoic Acid and Chemotherapy in Non-High-Risk Acute Promyelocytic Leukemia: Final Results of the Randomized Italian-German APL0406 Trial. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2016 doi: 10.1200/JCO.2016.67.1982. [DOI] [PubMed] [Google Scholar]
- 2.Papaemmanuil E, Gerstung M, Bullinger L, Gaidzik VI, Paschka P, Roberts ND, et al. Genomic Classification and Prognosis in Acute Myeloid Leukemia. The New England journal of medicine. 2016;374:2209–21. doi: 10.1056/NEJMoa1516192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arber DA, Orazi A, Hasserjian R, Thiele J, Borowitz MJ, Le Beau MM, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127:2391–405. doi: 10.1182/blood-2016-03-643544. [DOI] [PubMed] [Google Scholar]
- 4.Brown P, McIntyre E, Rau R, Meshinchi S, Lacayo N, Dahl G, et al. The incidence and clinical significance of nucleophosmin mutations in childhood AML. Blood. 2007;110:979–85. doi: 10.1182/blood-2007-02-076604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Falini B, Martelli MP, Bolli N, Sportoletti P, Liso A, Tiacci E, et al. Acute myeloid leukemia with mutated nucleophosmin (NPM1): is it a distinct entity? Blood. 2011;117:1109–20. doi: 10.1182/blood-2010-08-299990. [DOI] [PubMed] [Google Scholar]
- 6.Collins CT, Hess JL. Role of HOXA9 in leukemia: dysregulation, cofactors and essential targets. Oncogene. 2016;35:1090–8. doi: 10.1038/onc.2015.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kuhn MWM, Song E, Feng Z, Sinha A, Chen C-W, Deshpande AJ, et al. Targeting Chromatin Regulators Inhibits Leukemogenic Gene Expression in NPM1 Mutant Leukemia. Cancer Discov. 2016;xxx:xxx–xxx. doi: 10.1158/2159-8290.CD-16-0237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang GG, Pasillas MP, Kamps MP. Meis1 programs transcription of FLT3 and cancer stem cell character, using a mechanism that requires interaction with Pbx and a novel function of the Meis1 C-terminus. Blood. 2005;106:254–64. doi: 10.1182/blood-2004-12-4664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang X, Chen CW, Armstrong SA. The role of DOT1L in the maintenance of leukemia gene expression. Curr Opin Genet Dev. 2016;36:68–72. doi: 10.1016/j.gde.2016.03.015. [DOI] [PubMed] [Google Scholar]
- 10.Kumar AR, Hudson WA, Chen W, Nishiuchi R, Yao Q, Kersey JH. Hoxa9 influences the phenotype but not the incidence of Mll-AF9 fusion gene leukemia. Blood. 2004;103:1823–8. doi: 10.1182/blood-2003-07-2582. [DOI] [PubMed] [Google Scholar]