Abstract
Purpose
A 40-question postal survey was developed to gain insight into the nature of difficulties experienced by patients due to rheumatoid arthritis (RA), as well as patient perceptions and priorities regarding their RA treatment
Patients and methods
A total of 3000 Lower Saxony, Germany members of Rheuma-Liga (RL), a patient support group for people with RA, were invited to participate between July 1, and August 20, 2009. The questionnaire was divided into four sections: (1) patient demographics, (2) quality of life (QOL), (3) treatment expectations and, (4) patient perceptions of RL. The questionnaire could be completed in writing or via the internet.
Results
Of 959 respondents (response rate = 32.0%), 318 had diagnosed RA and were included in the analysis. The respondents were mostly retired (71.2%), female (83.3%), and >60 years of age (63.5%). Members’ responses indicated that most were generally satisfied with their current treatment (67.3%), considered it efficacious (84.0%), and reported minimal (none or little) side-effects (61.2%). Patient involvement in treatment decisions, however, was reportedly low (49.6% felt insufficiently involved). Patients’ primary impairments were reflected in their treatment priorities: mobility (97.0%), ability to run errands/do shopping (97.1%), do the housework (95.6%), and be independent of others (94.2%). The primary service provided by RL and used by respondents was physiotherapy (70.6%), which was reported to benefit physical function and mood by over 90.0% of respondents.
Conclusion
RA had a detrimental effect upon respondents’ quality of life, specifically impairing their ability to perform daily tasks and causing pain/emotional distress. Independence and mobility were strong priorities for respondents. Physical therapy, provided by RL, was felt to help both physical and mental/emotional health.
Keywords: rheumatoid arthritis, patient survey, quality of life, patient satisfaction
Introduction
Rheumatoid arthritis (RA) is a progressive, inflammatory disorder, leading to joint degradation and functional impairment.1 The condition is associated with increased mortality through development of cardiovascular disease (CVD) with accelerated atherosclerosis.2,3 Consensus from numerous studies in developed-world populations suggests that the current prevalence of RA is between 0.5% and 2.0% of the adult population, and that this figure has begun to increase in recent years.2,4,5 Risk factors for RA include gender (prevalence of RA female:male, ~3:1), age (peak incidence at 55–64 years of age for women, 65–74 years of age for men), and smoking.6
RA has a substantial impact upon patients’ quality of life (QOL) as a result of continuous pain, functional disability, reduced mobility and loss of independence in daily life.7,8 Increasing pain is associated with a higher degree of depression, even amongst patients who feel their condition to be well controlled.9 Indeed, much of the patient’s burden from RA results from its impact upon the patients’ overall sense of well-being; consequently, the use and acceptance of QOL measures in assessing treatment efficacy in RA has become an increasingly important measure of patient health.10–13 The five most important outcomes for RA patients are: pain, joint damage, fatigue, activities of daily living and mobility.14,15 In addition, patient reported outcomes (PROs) have been shown to be an important indicator for long-term disease progression.16 The importance of these aspects has recently been emphasized by EULAR (the European League Against Rheumatism) when consideration of patients’ perspectives and priorities in treatment decisions was defined as one overarching principle of care for RA patients.17
While changes in the QOL of RA patients have been studied extensively in clinical trials, relatively little information is available for real-life RA patient populations. Indeed, publications on RA patients have noted that randomized controlled clinical trials do not truly reflect the spectrum of real-life patients encountered in the clinic, for example because their disease activity is lower or higher, they have more/other comorbidities and use more/other concomitant medications.18–21 Therefore, analysis of real-life data is of use for comparison with that reported from clinical results and may more accurately reflect the broader patient population, regardless of potentially confounding factors that are typically and necessarily avoided when defining clinical study populations. Here we report the results of a patient questionnaire obtained from members in Lower Saxony, Germany of a patient organization for rheumatic diseases (Rheuma-Liga, RL). As optimal treatment requires a clear understanding of the patients’ needs, the aim of this study was to assess patients’ QOL as well as their perceived needs and expectations for treatment and support.
Materials and methods
Rheuma-Liga and patient selection
The survey was developed to obtain feedback from the RL members with regard to the extent and nature of their functional impairment and disabilities due to RA, as well as their perception and priorities in terms of their overall RA treatment, and support services provided by RL. The aims of the RL organization are to raise awareness about rheumatic and musculoskeletal diseases (RMDs), improve the QOL for people with RMDs and campaign for the improvement of medical treatment, psychological, and social support. The RL is an independent organization and has 16 regional sections which comprehensively cover Germany. In total, RL has about 260,000 members and is the largest patient organization in Germany. Between July 1 and August 20, 2009, 3000 of the 55,000 members of RL in Lower Saxony were randomly selected from the member list. A written questionnaire in German language was sent by mail. Patients had the option of returning the completed questionnaire by post or completing the questionnaire online.
Questionnaire structure
The RL questionnaire comprised 40 questions divided into four sections relating to: (1) patient demographics, (2) QOL in RA, (3) treatment expectations, and (4) patient perceptions of RL. The questionnaire, translated into English from the original German, is provided in full in Appendix 1. All responses, including medical histories, and diagnostic and therapeutic information, were provided directly by the respondents without guidance of medical personnel.
Section 1: patient demographics
Questions 1 to 8 recorded patients demographics and medical history including gender, age group, employment status, type of rheumatic condition, severity of rheumatic disease, time since diagnosis and age at time of RA diagnosis.
Section 2: quality of life in RA
Questions 9 to 19 related to QOL and were derived from the validated measures Nottingham Health Profile (NHP)22 and SF-36 Health Survey,23 although were not validated in the adapted format used; license agreement for use of sections from the SF-36 was obtained from Quality-Metric Inc, (Lincoln, RI, USA). Patients were asked to use subjective scales to assess their impairment.
Briefly, questions 9 to 15 assessed general health, impact of RA on the patients’ life and mental health, current QOL, perception of pain, work-related productivity, and social participation. Questions 16 to 18 assessed the patient’s ability to perform everyday tasks/activities and the degree of their dependence upon others in their daily lives. Finally, question 19 asked patients to personally rate the importance of specific aspects of daily living.
Section 3: treatment expectations
Questions 20 to 27 related to patients’ current treatment and treatment perceptions (assessed using subjective scales).
Questions 20 to 24 recorded what type of medication patients’ were currently using, how satisfied they were with their current therapy, their degree of involvement in therapy decision making, the efficacy of their current therapy (in terms of maintaining their lifestyle, reducing pain, slowing joint damage, and avoiding disability) and the impact of treatment side-effects on their health/activity.
Question 25 investigated what facets of an “ideal” treatment were rated as most important by patients. These included rapid symptom relief/rapid signs of improvement, persistence of positive results/no loss of efficacy, simplicity of use, absence of side-effects/no injection site skin reaction, low dose/no need for future increase in dose, administration route/simple to self-administer/no requirement for hospitalization/can be self-administered without assistance, treatment costs and need only take/administer infrequently.
Questions 26 and 27 asked patients what type of treatment they preferred (ie, daily tablets, subcutaneous injection [home or in hospital], intravenous injection [hospital]) and how important self-administration was regarded.
Section 4: patients’ perception of RL
Questions 28 to 40 related to patients’ perceptions of RL and the services it offered to members. These questions asked what reasons patients might have to recommend RL to others, which RL services were of highest importance, how aware patients were of the services offered by RL, how they found out about RL, what services were offered and/or used by the members, and what future activities were of interest to the members.
Full details of all questions and subjective response scales can be found in Appendix 1.
Statistics
Descriptive comparisons were used for all individual questionnaire items.
Results
Demographics
In total, 959 of 3000 patients responded to the questionnaire (response rate = 32.0%); of these, 318 (34.3%) had diagnosed RA and were included in this analysis. A detailed summary of patient demographics is presented in Table 1. The majority of RA patients were female (83.3% vs 16.7% males) and nearly two-thirds (63.5%) of respondents were ≥60 years old. Most respondents were retired (71.2%). The majority of respondents reported severity of rheumatic disease of either moderate (58.5%) or severe (27.5%), with age at onset most commonly reported as between 40–49 years (29.7%) or 50–59 years (30.1%).
Table 1.
Questions 2–8: demographic characteristics of respondents with rheumatoid arthritis (RA)
| Parameter | n | % |
|---|---|---|
| Sex (N = 318) | ||
| Male | 53 | 16.7 |
| Female | 265 | 83.3 |
| Age (years) (N = 318) | ||
| <20 | 0 | 0 |
| 20–29 | 3 | 0.9 |
| 30–39 | 6 | 1.9 |
| 40–49 | 32 | 10.1 |
| 50–59 | 75 | 23.6 |
| ≥60 | 202 | 63.5 |
| Occupation (N = 313) | ||
| Employee | 52 | 16.6 |
| Self-employed | 7 | 2.2 |
| Retired | 223 | 71.2 |
| Student | 1 | 0.3 |
| Unemployed | 6 | 1.9 |
| Unfit for work | 5 | 1.6 |
| Other | 19 | 6.1 |
| Type of rheumatic disease (N = 318) | ||
| Rheumatoid arthritis | 318 | 100.0 |
| Osteoarthritis/degenerative joint diseases | 113 | 35.5 |
| Ankylosing spondylitis | 15 | 4.7 |
| Juvenile arthritis | 1 | 0.3 |
| Fibromyalgia | 51 | 16.0 |
| Psoriatic arthritis | 17 | 5.3 |
| Other | 3 | 0.9 |
| Severity of RA disease (N = 313) | ||
| Very mild | 0 | 0 |
| Mild | 30 | 9.6 |
| Moderate | 183 | 58.5 |
| Severe | 86 | 27.5 |
| Very severe | 14 | 4.5 |
| Time since RA diagnosis (N = 316) | ||
| <1 years | 6 | 1.9 |
| 1–3 years | 24 | 7.6 |
| 3–5 years | 39 | 12.3 |
| 5–10 years | 79 | 25.0 |
| >10 years | 168 | 53.2 |
| Age at time of RA diagnosis (N = 316) | ||
| <20 years | 18 | 5.7 |
| 20–29 years | 22 | 7.0 |
| 30–39 years | 46 | 14.6 |
| 40–49 years | 94 | 29.7 |
| 50–59 years | 95 | 30.1 |
| ≥60 years | 41 | 13.0 |
Details of current therapy
Overall 69.4% of respondents used analgesics for treatment of their RA, 47.4% used disease-modifying anti-rheumatic drugs (DMARDs), 39.8% used corticosteroids, 16.1% used non-steroidal anti-rheumatics, and 7.9% used biological therapies such as tumor necrosis factor (TNF) inhibitors.
Efficacy and tolerability of current treatment
Most respondents (84.0%) rated treatment efficacy as sufficiently effective (ie, improvement) and only 6.8% reported a worsening of their RA under treatment (Table 2). Consistent with this, 67.3% of respondents were “satisfied” with their current therapy, 22.3% were indifferent (“neither satisfied nor dissatisfied”), and 10.4% were “dissatisfied”.
Table 2.
Question 23: effect of current treatment (N = 308)
| Treatment efficacy | % |
|---|---|
| Dramatic improvement | 12.4 |
| Marked improvement | 26.9 |
| Somewhat improved | 44.8 |
| Somewhat worsened | 4.2 |
| Marked worsening | 2.3 |
| Dramatic worsening | 0.3 |
In addition, the majority of respondents (61.2%) reported either “none” (17.8%) or “barely noticeable/does not really bother me” (43.4%) side-effects of their current treatment. However, 9.2% of respondents rated side-effects as “occasionally interfering with their daily activities,” 3.0% reported side-effects as “frequently interfering with daily activities,” and 0.3% recorded that their side-effects were “intolerable”.
Involvement of patients in treatment decisions
The overall involvement of respondents in their treatment decisions was unexpectedly low, and 49.6% of respondents felt they were insufficiently involved in decision making by their rheumatologists (“no or little involvement”). In contrast 19.7% reported that they felt “very much” involved.
Patients’ priorities for future treatments
More than 80% of respondents considered the following aspects of treatment to be very important for any potential treatment of RA: persistence of positive clinical response for more than one year (92.0%), absence of side-effects (89.2%), no loss of response over time (82.9%), simple to self-administer (82.3%), and no need for hospitalization (80.4%). In addition, the preferred form of treatment administration was a single tablet daily (81.0%), and 85.3% of respondents considered self-administration, without assistance, to be very important.
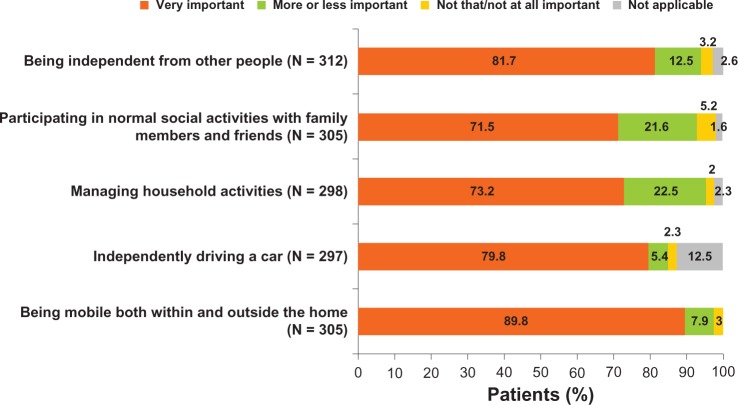
Patient priorities for QOL
Almost all respondents (97.7%) reported that mobility inside and outside the home was of particular importance to them (Figure 1). Other activities rated to be at least “more or less important” by ≥90% of respondents included: the ability to run errands/do shopping (97.1%), the ability to undertake housework (95.6%), independence from others (94.2%), and participation in normal social activities with family/friends (93.1%).
Figure 1.
How important is independence to you?
Patients’ general QOL assessment
For all QOL questions, overall responses from RA patients who reported an additional concomitant rheumatic disease were more negative (worse QOL) than from respondents with RA alone. Overall, 86.9% of respondents rated their general health as either “reasonable” or “good”, and 87.6% rated their overall QOL as “reasonable” or “good” (Table 3). In contrast, 60.5% of respondents rated the impact of RA upon their lives as “rather bad” or “very bad” (Table 3).
Table 3.
Questions 9–11: general QOL assessment
| General QOL assessment | % |
|---|---|
| General health (N = 314) | |
| Reasonable | 63.7 |
| Good | 23.2 |
| Impact of RA on life (N = 314) | |
| Rather bad | 55.1 |
| Very bad | 5.4 |
| Overall QOL (N = 316) | |
| Reasonable | 60.4 |
| Good | 27.2 |
Abbreviations: RA, rheumatoid arthritis; QOL, quality of life.
Pain and physical, or emotional, problems due to RA
For 27.6% of respondents, the impact of RA on social activities during the previous month was “strong” to “very strong” (Table 4). In addition 49.6% reported their physical impairment in daily work (inside and outside the home) as “rather strongly” to “very strongly” impacted by RA (Table 4).
Table 4.
Impact of pain and physical/emotional problems
| Pain and physical/emotional problems | % |
|---|---|
| Impact of RA on social activities (N = 312) | |
| Moderate | 31.1 |
| Strong | 23.1 |
| Very strong | 4.5 |
| Impairment in daily work (N = 312) | |
| Moderate | 34.6 |
| Rather strong | 39.7 |
| Very strong | 9.9 |
| Pain felt over previous month (N = 312) | |
| Moderate | 50.6 |
| Severe | 22.4 |
| Very severe | 3.5 |
| Emotional problems due to RA (N = 314) | |
| All the time | 0.3 |
| Most of the time | 12.4 |
| Sometimes | 46.5 |
| Seldom | 25.5 |
| Not at all | 15.3 |
Abbreviation: RA, rheumatoid arthritis.
Overall, 25.9% of respondents rated their pain over the previous month as “severe” to “very severe” (Table 4). Emotional problems due to RA (eg, depression or fear) were experienced regularly (ie, “all the time,” “most of the time,” or “sometimes”) by 59.2% of respondents, “seldom” by 25.5%, and “never/not at all” by 15.3%.
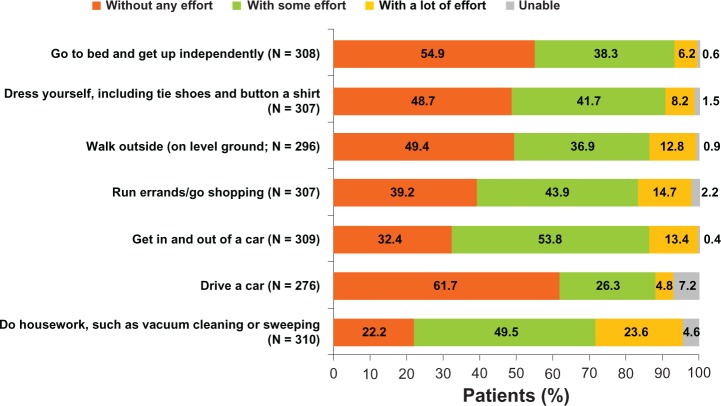
Impact of RA upon daily activities and independence
Most activities of daily living could be performed “without any effort” or “with some effort” by ≥80% of respondents (Figure 2). Housework was possible “with a lot of effort” for 23.6% of respondents, while 5.2% of respondents reported being “unable” to do housework activities. Driving a car was reportedly not possible for 6.9% of respondents (ie, “unable”). Running errands and shopping was possible only “with a lot of effort” for 17.3% and impossible for 3.3% (ie, “unable”).
Figure 2.
How much effort is required for you to undertake the following normal daily activities?
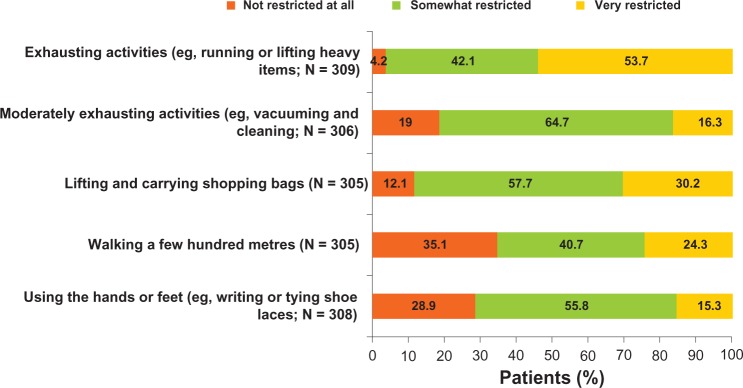
Restriction in daily activities due to RA was frequently reported (Figure 3). For example: 95.8% of respondents reported restriction in strenuous/exhausting activities (53.7% “very restricted” and 42.1% “somewhat restricted”); 87.9% of respondents reported restriction in lifting/carrying shopping bags (30.2% “very restricted” and 57.7% “somewhat restricted”) and 81.1% of respondents reported restriction for moderately strenuous activities such as vacuum cleaning (16.3% “very restricted” and 64.7% “somewhat restricted”).
Figure 3.
Is your health status restricting you in any way, and to what extent?
Over 60% of respondents were at least “more or less” dependent upon a third-party in their day-to-day activities, generally upon their partner or family/friends (Table 5). In contrast, dependence upon medical personnel was markedly lower, with dependence highest upon “other medical specialist” (excludes “nurse/caregiver”) (Table 5).
Table 5.
Third-party dependence (% respondents; N = 262)
| Dependence | Partner | Family/friends | Other medical specialist (excludes “nurse/caregiver”) |
|---|---|---|---|
| More or less | 53.7 | 42.5 | 8.4 |
| Heavily | 8.0 | 3.3 | 1.5 |
Assessment of RL
Respondents most commonly learned of RL from other members (39.8%), their rheumatologist (35.6%), or their general practitioner (29.4%). In all 70.6% of respondents took advantage of RL’s group physiotherapy program, and in most cases no further individual (ie, one-to-one) physiotherapy was offered by the treating physician. The group physiotherapy program was the most commonly stated (and generally the most important) reason for recommending RL to other respondents (indicated by 86.5% of respondents). Furthermore, over 90% of respondents reported the physiotherapy program improved physical performance and mood, and reduced physical complaints.
Most respondents were aware of RL’s different information services, and these were also a common reason for recommending RL to other respondents (68.8%). Overall, >80% of respondents were satisfied with the RL services. The interest in proposed new services was highest for medical support (physiotherapy 92.3%), rehabilitation services (86.3%), help obtaining second medical opinions (87.0%), help communicating with the health insurance (82.7%), and for courses about diet and rheumatism (88.6%), and back training (84.0%).
Discussion
This study was designed to provide a clearer understanding of patient priorities and needs amongst the members of an arthritis patient organization. For this purpose, a questionnaire was developed to obtain insight into patients’ needs, their functional limitations and other disease associated aspects. It was not the intention to develop a new QOL assessment for RA respondents.
The resulting survey was relatively long (40 questions) and was sent to a randomly selected group of RL members who were asked to complete and return the questionnaire. Even though nearly one third of those invited did participate in the survey, the opinions obtained may reflect a selection of the most active or motivated members. This paper addresses only the results from those 34% of respondents who reported a diagnosis of RA, which may also limit conclusions.
As the survey used a non-validated questionnaire the responses were not calibrated to any clinical metric, therefore data could not be normalized against any other patient or healthy population responses and no domain-style summary analyses were possible. Data summaries and comparison were further limited by the lack of common scales between questions/sections. The results must therefore be considered on a subjective, question-by-question basis, and cannot be realistically assessed in a broader context. In addition, the participating population reflected the local RL membership and differed from observed broader RA populations; for example, in gender ratio female:male (5:1 vs 2–3:1 expected), a median age > 60 years, and a median time since diagnosis > 10 years.6 As such, males, as well as younger patients and those patients with shorter disease durations, were under-represented.24,25 While this survey has provided important insight into specific RA patient issues, use of a validated assessment would have resulted in more representative data. For example, use of Short Form-36 (SF-36),23 which is known to be sensitive to clinically relevant signals in RA populations,13 or the SF-12 (a subset of the SF-36 questions), would improve the clinical relevance of the results of this survey. However, the questionnaire was designed to capture different aspects of the disease, including its burden and treatment aspects, as well as information about the performance of RL services. To include these domains, the questionnaire developed was felt to be the most practical way, even though this resulted in some limitations.
Despite these limitations, certain patterns were clear in the responses. In common with many QOL surveys of RA,7,26 participants stated that RA reduced their QOL and caused impairment in daily activities, including restricting their independence and mobility. Indeed, well over half the respondents were dependent upon a third party. Almost unanimously, respondents stated mobility and independence from other people were important to them. The burden of care fell largely upon family and friends rather than medical personnel, likely concealing much of the resulting cost burden.
Current guidelines from EULAR state that “best care” includes explicit patient involvement in treatment decisions.17 It was surprising then, that despite being satisfied with the clinical efficacy of their treatment approximately half of all respondents felt they were insufficiently involved in the clinical decision making process – which directly contradicts current best care guidelines. Increased patient involvement in decision making processes is important in improving patient’s empowerment and may enhance treatment outcomes.27,28 While on the other hand, a lack of patient–doctor communication regarding RA treatment decisions is associated with increased incidence of moderate to severe depression.29 One possible limiting factor to full application of the concept of shared decision in the German clinic is the tight schedule for individual patient visits. This could be improved by increasing the number of physicians, introducing structured patient information and increasing involvement of assistants and nurses.30 With the development of therapeutic options like biologic agents rheumatologists acknowledge the need to involve the patients in the treatment decisions, as this has been shown to improve their adherence to therapy.31 Another driver to implement the concept of shared decision making could be the fact that patient participation is increasingly seen as a quality indicator for medical care within the German health care system.32
The survey results presented here also served to underline the importance of patient support groups, such as RL, as providers of services beneficial for patient health and QOL, such as physiotherapy (not otherwise provided through their physician) and of information on coping with their disease. These services empower patients and help them maximize their independence. In this survey, group physiotherapy was considered important to many respondents and was felt to improve their physical and mental health. It was also of note that assistance in communicating with medical staff (seeking second opinions) and dealing with health insurance companies were amongst the most strongly requested new services from RL. Taken together with the low patient involvement in clinical decisions, this suggests professional support services are still failing to fully engage this patient population, indicating a clear need for greater dialogue between patients (or patient organizations), physicians, and cost carriers/health care services.
Patient priorities of the assessed population were clearly focused on independence, but it remains to be investigated if a younger population would give a substantially different response in this regard. In addition, it may be that those who responded were different in important respects from non-responders, thus limiting the general applicability of the findings. Feedback from patients using the online version of the questionnaire was very poor, which may also suggest response was obtained from a subset population.
In summary, RA imposes a substantial physical and emotional burden upon patients. The highest priorities for patients, however, are mobility, independence, and coping with everyday activities. Physiotherapy and information services help patients cope with their condition day-to-day, and are primarily provided by patient support organizations such as RL. While generally satisfied with their treatment efficacy, patients may benefit from greater involvement in treatment decisions.
Acknowledgments
This study was funded with an unrestricted educational grant by UCB Pharma GmbH to Rheuma-Liga. The authors acknowledge Costello Medical Consulting for editorial and administrative support.
Appendix 1
The Rheuma-Liga patient questionnaire
This questionnaire should help us to learn more about and understand better the experiences and attitudes of persons with rheumatic diseases.
Please check the applicable box or boxes. Please mark only one box per question unless stated otherwise.
| Q1. You are… | A patient with rheumatic disease A health care professional – go to end of questionnaire Other – go to end of questionnaire |
|
| |
| Q2. You are… | A man A woman |
|
| |
| Q3. Your age… | Below 20 20–29 30–39 40–49 50–59 60 or older |
|
| |
| Q4. Your employment status… | Employed (full time or part time) Self-employed Retired Student Unemployed (otherwise) Disabled Other |
|
| |
| Q5. Which kind of rheumatic disease are you suffering from? | Rheumatoid arthritis Arthrosis Ankylosing spondylitis Juvenile arthritis Fibromyalgia Psoriasis arthritis Another type of rheumatic disease. Please specify: |
|
| |
| Q6. How would you rate the degree of severity of your rheumatic disease? | Very low Low Moderate Severe Very severe |
|
| |
| Q7. How long have you been suffering from your rheumatic disease? | Less than one year 1–3 years 3–5 years 5–10 years More than 10 years |
|
| |
| Q8. What was your age at onset of the rheumatic disease? | 19 or younger 20–29 30–39 40–49 50–59 60 or older |
|
| |
| Q9. How would you describe your general health status? | Excellent Very good Good Reasonable Bad |
|
| |
| Q10. Considering the impact of rheumatic disease on your life, how are you doing? | Very good Rather good Rather bad Very bad |
|
| |
| Q11. How would you rate your quality of life today? | Excellent Very good Good Reasonable Bad |
|
| |
| Q12. How would you rate the level of pain in the last month due to your rheumatic disease? | No pain Very low Low Moderate Severe Very severe |
|
| |
| Q13. In the last month, how strongly was your normal work (in- and outside the home) affected by your physical health? | Not at all Somewhat Moderately Rather strongly Very strongly |
|
| |
| Q14. In the last month, how often did you suffer from emotional problems (eg, depressive or anxious moods) as a consequence of your rheumatic disease? | All the time Most of the time Sometimes Seldom Not at all |
|
| |
| Q15. During the last month, how strongly were your social activities with family members, friends or neighbors affected by your physical health or emotional problems? | Not at all Somewhat Moderately Rather strongly Very strongly |
|
| |
| Q16. Would you tell us how much you were affected by your rheumatic disease during your normal daily activities? Are you able to… | |
| Go to bed and get up independently | Without any effort With some effort With a lot of effort Unable |
| Dress yourself, including tie shoes and button a shirt | Without any effort With some effort With a lot of effort Unable |
| Walk outside (on level ground) | Without any effort With some effort With a lot of effort Unable |
| Run errands/go shopping | Without any effort With some effort With a lot of effort Unable |
| Get in and out of a car | Without any effort With some effort With a lot of effort Unable |
| Drive a car | Without any effort With some effort With a lot of effort Unable |
| Do housework, such as vacuum cleaning or sweeping | Without any effort With some effort With a lot of effort Unable |
|
| |
| Q17. To what extent do you depend on… | |
| Your partner | Very much More or less Not at all Not applicable |
| Family, friends, etc | Very much More or less Not at all Not applicable |
| Nurse/caregiver | Very much More or less Not at all Not applicable |
| Other medical specialist staff | Very much More or less Not at all Not applicable |
|
| |
| Q18. The following questions are referring to your activities during a typical day. Is your health status limiting you in any way, and if yes, to what extent? | |
| Exhausting activities, such as running, heavy lifting | Strongly restricted Somewhat restricted Not restricted at all |
| Moderately exhausting activities, such as vacuum cleaning | Strongly restricted Somewhat restricted Not restricted at all |
| Lifting or carrying shopping bags | Strongly restricted Somewhat restricted Not restricted at all |
| Going up some stairs | Strongly restricted Somewhat restricted Not restricted at all |
| Walking a few hundred meters | Strongly restricted Somewhat restricted Not restricted at all |
| Taking a bath by yourself | Strongly restricted Somewhat restricted Not restricted at all |
| Using hands/fingers (for writing, tying shoes) | Strongly restricted Somewhat restricted Not restricted at all |
|
| |
| Q19. For me it is important… | |
| To be independent from other people | Very important More or less important Not that important Not important at all Not applicable |
| To go to work or restart working as soon as possible | Very important More or less important Not that important Not important at all Not applicable |
| To participate in normal social activities with family members and friends | Very important More or less important Not that important Not important at all Not applicable |
| To manage household activities | Very important More or less important Not that important Not important at all Not applicable |
| To drive a car by myself | Very important More or less important Not that important Not important at all Not applicable |
| To run errands | Very important More or less important Not that important Not important at all Not applicable |
| To do exercise (sports), to be active | Very important More or less important Not that important Not important at all Not applicable |
| To be mobile inside and outside home | Very important More or less important Not that important Not important at all Not applicable |
| To do recreational activities with my children | Very important More or less important Not that important Not important at all Not applicable |
|
| |
| Q20. Which medicine are you using to control your disease? | Analgesics (painkillers) Non-steroidal anti-rheumatics (NSARs) Synthetic disease-modifying anti-rheumatic drugs (DMARDs) (eg, methotrexate) Corticosteroids Biologic therapies (like anti-TNF) Other |
|
| |
| Q21. How satisfied are you with your current therapy? | Very satisfied Satisfied Neither satisfied nor dissatisfied Dissatisfied Not satisfied at all |
|
| |
| Q22. To what extent were you involved in the choice of your therapy/drug? | Not at all Just a little Somewhat Very much |
|
| |
| Q23. The goal of the therapy is to help you maintain your lifestyle, to reduce pain in the joints, to slow down the joint damage and to avoid disability. Considering these aspects, how would you rate the efficacy of your current therapy? | Improved my condition dramatically Improved my condition remarkably Has improved it somewhat Did not make any difference Deteriorated it a little bit Deteriorated my condition remarkably Deteriorated my condition dramatically |
|
| |
| Q24. How would you describe the side effects of your current medication? | There are none There are some side effects which do not really bother me There are some side effects which occasionally interfere with my daily activities Many side effects which frequently interfere with my daily activities The side effects are difficult to bear The side effects are intolerable |
|
| |
| Q25. Imagine what the ideal treatment would look like for you. Then check how you would rate the following aspects using a scale from “very important” to “unimportant”. | |
| Fast relief of symptoms (< 1 week) | Very important More or less important Neither important nor unimportant (indifferent) More or less unimportant Totally unimportant |
| Sustained positive results (>1 year) | Very important More or less important Neither important nor unimportant (indifferent) More or less unimportant Totally unimportant |
| Easy handling of therapy (eg, comfort, patient friendly packaging, etc) | Very important More or less important Neither important nor unimportant (indifferent) More or less unimportant Totally unimportant |
| Fast signs of improvement (< 2 days) | Very important More or less important Neither important nor unimportant (indifferent) More or less unimportant Totally unimportant |
| Absence of side effects (maybe: as little as possible or no side effects) | Very important More or less important Neither important nor unimportant (indifferent) More or less unimportant Totally unimportant |
| Low dose of the drug | Very important More or less important Neither important nor unimportant (indifferent) More or less unimportant Totally unimportant |
| No loss of efficacy over time | Very important More or less important Neither important nor unimportant (indifferent) More or less unimportant Totally unimportant |
| No skin reaction at the injection site | Very important More or less important Neither important nor unimportant (indifferent) More or less unimportant Totally unimportant |
| Type of administration (path of application) | Very important More or less important Neither important nor unimportant (indifferent) More or less unimportant Totally unimportant |
| Treatment costs | Very important More or less important Neither important nor unimportant (indifferent) More or less unimportant Totally unimportant |
| No need to increase the dose in the future | Very important More or less important Neither important nor unimportant (indifferent) More or less unimportant Totally unimportant |
| Easy self-administration | Very important More or less important Neither important nor unimportant (indifferent) More or less unimportant Totally unimportant |
| No need to go to hospital | Very important More or less important Neither important nor unimportant (indifferent) More or less unimportant Totally unimportant |
| Needs to be taken or used rarely (eg, fewer injections required) | Very important More or less important Neither important nor unimportant (indifferent) More or less unimportant Totally unimportant |
|
| |
| Q26. What type of treatment would you prefer? | One tablet once a day Subcutaneous injection, ie, administered below the skin, possibly to self-administer or by someone else at home or in a hospital Intravenous medication, given by a physician or in a hospital |
|
| |
| Q27. How important is self-administration, without help of someone else? | Very important More or less important Neither important nor unimportant (indifferent) More or less unimportant Totally unimportant |
|
| |
| Q28. For what reason would you recommend the Lower-Saxony Rheuma-Liga? (Please check all answers that apply) | To participate in the physical training offered by the Rheuma-Liga To participate in other offerings of the Rheuma-Liga To receive information about dealing with the disease To talk to and communicate with persons who are affected by the same disease To meet new people Other reason such as: |
|
| |
| Q28b. If you have specified more than one reason, which of them was the single most important for you? | To participate in the physical training offered the Rheuma-Liga To participate in other offerings of the Rheuma-Liga To receive information about dealing with diseases To talk to and communicate with persons who are affected by the same disease To meet new people Other reason such as: |
|
| |
| Q29. Do you know anything else offered by the Rheuma-Liga beside the physical training? (Please check all answers that apply) | No Yes, information events Written information material Seminars on various topics Discussion groups Dance groups Occupational therapy groups Strength training Pain management courses Patient education Special insurance rates Special travel rates Counseling in social law “Mobil” member magazine Other such as: |
|
| |
| Q30. How did you find out about the Rheuma-Liga? (Please check all answers that apply) | General practitioner Rheumatologist Other specialist Media outlets Internet Other patients/affected persons |
|
| |
| Q31. How did you find out what the Rheuma-Liga has to offer? (Please check all answers that apply) | General practitioner Rheumatologist Other specialist Media outlets Internet Other patients/affected persons |
|
| |
| Q32. Have you taken advantage of what the Rheuma-Liga has to offer? (Please check all answers that apply) | No Yes, information events Written information material Seminars on various topics Discussion groups Dance groups Occupational therapy groups Strength training Pain management courses Patient education Special insurance rates Special travel rates Counseling in social law “Mobil” member magazine Other |
|
| |
| Q33. Could you imagine yourself using one or more of the following items the Rheuma-Liga has to offer in the future? | |
| Nursing care | Definitely, yes Rather, yes Rather, no Definitely, no |
| Household help organization | Definitely, yes Rather, yes Rather, no Definitely, no |
| Rehabilitation offer (eg, in a rehabilitation center) | Definitely, yes Rather, yes Rather, no Definitely, no |
| Physician and medical care (eg, physical therapy, physiotherapy) | Definitely, yes Rather, yes Rather, no Definitely, no |
| Support in getting a second opinion from a physician in a medical question | Definitely, yes Rather, yes Rather, no Definitely, no |
| Support in dealing with social services offices and administrations | Definitely, yes Rather, yes Rather, no Definitely, no |
| Support in dealing with the health insurance company or pension insurance | Definitely, yes Rather, yes Rather, no Definitely, no |
|
| |
| Q34. Overall, how satisfied are you with the current offer of the Rheuma-Liga? | Very satisfied Rather satisfied Rather dissatisfied Very dissatisfied |
|
| |
| Q35. Could you imagine yourself taking advantage of one or several of the following possible courses offered by the Rheuma-Liga? | |
| Therapeutic back training | Definitely, yes Rather, yes Rather, no Definitely, no |
| Endurance training (eg, walking) | Definitely, yes Rather, yes Rather, no Definitely, no |
| Relaxation techniques/dealing with stress | Definitely, yes Rather, yes Rather, no Definitely, no |
| Nutrition and overweight | Definitely, yes Rather, yes Rather, no Definitely, no |
| Nutrition and osteoporosis | Definitely, yes Rather, yes Rather, no Definitely, no |
| Nutrition and rheumatic disease | Definitely, yes Rather, yes Rather, no Definitely, no |
|
| |
| Q36. Do you participate in the functional training offered by the Rheuma-Liga? | Yes No |
|
| |
| Q37. How did you find out about the functional training courses offered by the Rheuma-Liga? | Friends/relatives/neighbors Other members of the Rheuma-Liga Physiotherapist Physician Health insurer Pension insurance Rehabilitation center Others such as: |
|
| |
| Q38. In addition to the functional training, did your physician prescribe you any individual physiotherapy within the past 3 months? | Yes, more than 10 sessions Yes, 6 to 10 sessions Yes, 3 to 5 sessions Yes, 1 to 2 sessions No |
|
| |
| Q39. How satisfied are you with the following aspects of the functional training? | |
| Course instructor | Very satisfied Rather satisfied Rather dissatisfied Very dissatisfied |
| Group size | Very satisfied Rather satisfied Rather dissatisfied Very dissatisfied |
| Rooms | Very satisfied Rather satisfied Rather dissatisfied Very dissatisfied |
| Hours during which the course takes place | Very satisfied Rather satisfied Rather dissatisfied Very dissatisfied |
| Frequency of the training | Very satisfied Rather satisfied Rather dissatisfied Very dissatisfied |
| Degree of difficulty of the training | Very satisfied Rather satisfied Rather dissatisfied Very dissatisfied |
| The amount to pay for participating in the physical training | Very satisfied Rather satisfied Rather dissatisfied Very dissatisfied |
|
| |
| Q40. According to your opinion, what is the effect of the functional training on the following aspects of your condition? | |
| Physical fitness | Very favorable Somewhat favorable Barely favorable Not favorable |
| Physical discomfort | Very favorable Somewhat favorable Barely favorable Not favorable |
| Mood | Very favorable Somewhat favorable Barely favorable Not favorable |
Footnotes
Disclosure
J Wollenhaupt has served as an advisory board member and received honoraria as a speaker from UCB Pharma GmbH. D Fricke and A Groenewegen are employees of UCB Pharma. The authors report no other conflicts of interest in this work.
References
- 1.Klareskog L, Catrina AI, Paget S. Rheumatoid arthritis. Lancet. 2009 Feb 21;373(9664):659–672. doi: 10.1016/S0140-6736(09)60008-8. [DOI] [PubMed] [Google Scholar]
- 2.Ku IA, Imboden JB, Hsue PY, Ganz P. Rheumatoid arthritis: model of systemic inflammation driving atherosclerosis. Circ J. 2009 Jun;73(6):977–985. doi: 10.1253/circj.cj-09-0274. [DOI] [PubMed] [Google Scholar]
- 3.Szekanecz Z, Koch AE. Vascular involvement in rheumatic diseases: ‘vascular rheumatology’. Arthritis Res Ther. 2008;10(5):224. doi: 10.1186/ar2515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Doran MF, Pond GR, Crowson CS, O’Fallon WM, Gabriel SE. Trends in incidence and mortality in rheumatoid arthritis in Rochester, Minnesota, over a forty-year period. Arthritis Rrheum. 2002;46(3):625–631. doi: 10.1002/art.509. [DOI] [PubMed] [Google Scholar]
- 5.Gabriel SE, Michaud K. Epidemiological studies in incidence, prevalence, mortality, and comorbidity of the rheumatic diseases. Arthritis Res Ther. 2009;11(3):229. doi: 10.1186/ar2669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Symmons D, Turner G, Webb R, et al. The prevalence of rheumatoid arthritis in the United Kingdom: new estimates for a new century. Rheumatol. 2002;41(7):793–800. doi: 10.1093/rheumatology/41.7.793. [DOI] [PubMed] [Google Scholar]
- 7.Haroon N, Aggarwal A, Lawrence A, Agarwal V, Misra R. Impact of rheumatoid arthritis on quality of life. Mod Rheumatol. 2007;17(4):290–295. doi: 10.1007/s10165-007-0604-9. [DOI] [PubMed] [Google Scholar]
- 8.Strand V, Singh JA. Newer biological agents in rheumatoid arthritis: impact on health-related quality of life and productivity. Drugs. 2010;70(2):121–145. doi: 10.2165/11531980-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 9.Taylor P, Manger B, Alvaro-Gracia J, et al. Patient perceptions concerning pain management in the treatment of rheumatoid arthritis. J Int Med Res. 2010;38(4):1213–1224. doi: 10.1177/147323001003800402. [DOI] [PubMed] [Google Scholar]
- 10.Graninger W, Gross WL, Raspe H. Quality of life in rheumatic diseases. [Lebensqualität bei rheumatischen Erkrankungen] Zeitschrift fur Rheumatologie. 2010;69(3):197. doi: 10.1007/s00393-009-0569-5. German. [DOI] [PubMed] [Google Scholar]
- 11.Her M, Kavanaugh A. Patient-reported outcomes in rheumatoid arthritis. Curr Opin Rheumatol. 2012;24(3):327–334. doi: 10.1097/BOR.0b013e3283521c64. [DOI] [PubMed] [Google Scholar]
- 12.Khanna D, Tsevat J. Health-related quality of life – an introduction. Am J Manag Care. 2007;13(9):S218–S223. [PubMed] [Google Scholar]
- 13.Tugwell P, Idzerda L, Wells GA. Generic quality-of-life assessment in rheumatoid arthritis. Am J Manag Care. 2007;13(9):S224–S236. [PubMed] [Google Scholar]
- 14.Bartlett SJ, Hewlett S, Bingham CO, 3rd, et al. Identifying core domains to assess flare in rheumatoid arthritis: an OMERACT international patient and provider combined Delphi consensus. Ann Rheum Dis. 2012;71(11):1855–1860. doi: 10.1136/annrheumdis-2011-201201. [DOI] [PubMed] [Google Scholar]
- 15.Sanderson T, Hewlett S, Richards P, Morris M, Calnan M. Utilizing qualitative data from nominal groups: exploring the influences on treatment outcome prioritization with rheumatoid arthritis patients. J Health Pshychol. 2012;17(1):132–142. doi: 10.1177/1359105311410758. [DOI] [PubMed] [Google Scholar]
- 16.Felson DT, Smolen JS, Wells G, et al. American College of Rheumatology/European League Against Rheumatism provisional definition of remission in rheumatoid arthritis for clinical trials. Arthritis Rheum. 2011;63(3):573–586. doi: 10.1002/art.30129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smolen JS, Landewe R, Breedveld FC, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs. Ann Rheum Dis. 2010;69(6):964–975. doi: 10.1136/ard.2009.126532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kievit W, Fransen J, Oerlemans AJ, et al. The efficacy of anti-TNF in rheumatoid arthritis, a comparison between randomised controlled trials and clinical practice. Ann Rheum Dis. 2007;66(11):1473–1478. doi: 10.1136/ard.2007.072447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sokka T, Pincus T. Eligibility of patients in routine care for major clinical trials of anti-tumor necrosis factor alpha agents in rheumatoid arthritis. Arthritis Rheum. 2003;48(2):313–318. doi: 10.1002/art.10817. [DOI] [PubMed] [Google Scholar]
- 20.Wolfe F, Michaud K, Dewitt EM. Why results of clinical trials and observational studies of antitumour necrosis factor (anti-TNF) therapy differ: methodological and interpretive issues. Ann Rheum Dis. 2004;63(Suppl 2):ii13–ii17. doi: 10.1136/ard.2004.028530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zink A, Strangfeld A, Schneider M, et al. Effectiveness of tumor necrosis factor inhibitors in rheumatoid arthritis in an observational cohort study: comparison of patients according to their eligibility for major randomized clinical trials. Arthritis Rheum. 2006;54(11):3399–3407. doi: 10.1002/art.22193. [DOI] [PubMed] [Google Scholar]
- 22.Hunt SM, McEwan T. The development of a subjective health indicator. Soc of Health and Illness. 1980;2:231–246. doi: 10.1111/1467-9566.ep11340686. [DOI] [PubMed] [Google Scholar]
- 23.Ware JE, Sherbourne CD. The MOS 36-Item Short-Form Health Survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 24.Zink A, Listing J, Klindworth C, Zeidler H, German Collaboratrive Arthritis C The national database of the German Collaborative Arthritis Centres: I. Structure, aims, and patients. Ann Rheum Dis. 2001;60(3):199–206. doi: 10.1136/ard.60.3.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Groessl EJ, Ganiats TG, Sarkin AJ. Sociodemographic differences in quality of life in rheumatoid arthritis. Pharmaco Economics. 2006;24(2):109–121. doi: 10.2165/00019053-200624020-00002. [DOI] [PubMed] [Google Scholar]
- 26.Mili F, Helmick CG, Moriarty DG. Health related quality of life among adults reporting arthritis: analysis of data from the Behavioral Risk Factor Surveillance System, US, 1996–1999. J Rheumatol. 2003;30(1):160–166. [PubMed] [Google Scholar]
- 27.Barton JL. Patient preferences and satisfaction in the treatment of rheumatoid arthritis with biologic therapy. Patient Prefer Adherence. 2009;3:335–344. doi: 10.2147/ppa.s5835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ortendahl M. Shared decision-making based on different features of risk in the context of diabetes mellitus and rheumatoid arthritis. Ther Clin Risk Manag. 2007;3(6):1175–1180. [PMC free article] [PubMed] [Google Scholar]
- 29.Barton JL, Imboden J, Graf J, Glidden D, Yelin EH, Schillinger D. Patient-physician discordance in assessments of global disease severity in rheumatoid arthritis. Arthritis Care Res. 2010;62(6):857–864. doi: 10.1002/acr.20132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kruger K, Karberg K. Treat-to-target from the perspective of office-based rheumatology. [Treat-To-Target aus der Sicht der niederge-lassenen Rheumatologie] Zeitschrift fur Rheumatologie. 2011 Oct;70(8):664–669. doi: 10.1007/s00393-011-0852-0. German. [DOI] [PubMed] [Google Scholar]
- 31.Griffith J, Carr A. What is the impact of early rheumatoid arthritis on the individual? Best practice and research. Clinical rheumatology. 2001 Mar;15(1):77–90. doi: 10.1053/berh.2000.0127. [DOI] [PubMed] [Google Scholar]
- 32.Harter M, Muller H, Dirmaier J, Donner-Banzhoff N, Bieber C, Eich W. Patient participation and shared decision making in Germany – history, agents and current transfer to practice. Z Evld Fortbild Qual Gesundhwes. 2011;105(4):263–270. doi: 10.1016/j.zefq.2011.04.002. [DOI] [PubMed] [Google Scholar]