Abstract
Purpose In the presence of early osteoarthritis, changes to the trapeziometacarpal joint (TMJ) often result in pain and is associated with joint instability and a tendency of dorsoradial subluxation. In these instances, arthroscopy may be indicated to: (1) assess the extent of cartilage disease and the laxity of ligaments and to (2) treat TMJ instability. The purpose of our study was to biomechanically analyze which ligaments are the primary stabilizers of the TMJ.
Methods Overall, 11 fresh-frozen human cadaver specimens were dissected and attached to a testing device with the thumb positioned in neutral abduction, neutral flexion, and neutral opposition. The four extrinsic and five intrinsic muscle tendons acting on the TMJ were simultaneously loaded with weights proportional to their physiological cross-sectional area. The dorsal, volar, and ulnar groups of ligaments were dissected. A motion-tracking device, FasTrak (Polhemus Inc., Colchester, VT), was used to study the spatial position of the base of the first metacarpal bone (MC1), before and after random sectioning of each of the ligaments. Statistical analysis of the MC1 translation along the transverse XY plane was performed using one-way analysis of variance and a paired t-test, with a significance level of p < 0.05.
Results After isolated sectioning of the volar or the ulnar ligaments, the MC1 moved dorsoradially with an average of 0.150 mm (standard deviation [SD]: 0.072) and 0.064 mm (SD: 0.301), respectively. By contrast, the destabilization of the MC1 after sectioning of the dorsal ligaments was substantially larger (0.523 mm; SD: 0.0512; p = 0.004).
Conclusion Sectioning of the dorsal ligament group resulted in the greatest dorsoradial translation of the MC1. Consequently, the dorsal ligaments may be regarded as the primary TMJ stabilizers.
Clinical Relevance This study suggests that stabilizing arthroscopic shrinkage of the TMJ should be targeted toward the dorsal TMJ ligaments.
Keywords: TMJ instability, TMJ biomechanics, TMJ ligaments, TMJ arthroscopy, thumb arthroscopy
The trapeziometacarpal joint (TMJ) is complex, with high intrinsic mobility and limited intrinsic stability, offering a wide range of motion.1 This high intrinsic mobility and the intensive use of the thumb in daily activities have been linked to the high prevalence of osteoarthritis (OA) of the TMJ.2 Prearthritic pain is often related to joint instability.3
One potential source of controversy is that older literature emphasizes the role of the anterior oblique ligament (AOL) whereas newer literature demonstrates the importance of the dorsal ligaments in the prevention of dorsoradial subluxation. The volar TMJ ligaments have traditionally been considered as primary joint stabilizers.4 To date, strong emphasis has been placed on surgical procedures focused on the AOL, also known as the “beak ligament,” to provide TMJ stability and restrain dorsoradial subluxation.5 6 7 Recently, several anatomical, histological, and histomorphometric studies have challenged the role of the volar ligaments in TMJ stability. Bettinger et al in 1999 and 2000,8 9 Ladd et al in 2012,10 and finally D'Agostino et al11 in 2014 have determined that the dorsal-radial ligament (DRL) is the strongest and stiffest TMJ ligament, whereas the AOL is relatively weak and compliant and as such identified as a poor stabilizer of the TMJ. Hagert et al12 and Ladd et al10 studied the ultrastructural architecture and the innervation pattern of the DRL and the AOL. They concluded that the dense collagenous morphology and the rich innervation of the DRL are indicative of its important role as a primary TMJ stabilizer and as a ligament with superior proprioceptive qualities. Nevertheless, few biomechanical studies have been conducted to actually support or refute these suspicions based on anatomical, histological, and histomorphometric studies. Previously, only Van Brenk et al,13 have biomechanically investigated the TMJ essential ligaments for the prevention of dorsoradial subluxation of the joint and they identified the DRL as the primary stabilizer.
The aim of this study is to provide a current biomechanical assessment of the stabilizing effect of the three principal TMJ ligament groups: the dorsal, volar, and ulnar ligaments. Identification of the primary stabilizing ligament is clinically essential for arthroscopic TMJ stabilization.
We hypothesized that in neutral TMJ position and under simultaneous physiological muscle loading, the TMJ dorsal ligaments are the primary TMJ stabilizers and act as the primary restraint to the first metacarpal bone (MC1) in dorsoradial subluxation.
Methods
Before the experiments, 14 cadavers were X-rayed by the author, to exclude radiographic TMJ OA. Three of those specimens were excluded from the study.
A total of 11 fresh-frozen human cadaver specimens (5 females and 2 males, 6 right and 5 left hands) with an average age of 73 years (range: 67–80 years) were included. All specimens were dissected and handled according to the ethical guidelines and regulations of the University of Barcelona, Spain.
The specimens were thawed at room temperature and transected at the midforearm. All soft tissue was removed except: (1) thenar muscles and tendons, (2) the TMJ ligaments, (3) the flexor and the extensor retinaculae, (4) all carpal ligaments, (5) the most distal portion of the thumb, and (6) the tendons of the extrinsic muscles.
Subsequently, the four extrinsic and five intrinsic muscles acting on the TMJ (abductor pollicis brevis, flexor pollicis brevis, opponens pollicis, flexor pollicis longus, adductor pollicis, abductor pollicis longus [APL], extensor pollicis brevis [EPB], extensor pollicis longus [EPL], and first dorsal interosseous muscles) were identified and their distal tendon was isolated. Strings were attached to the proximal ends of these tendons. To simulate the muscle tone, all strings were simultaneously loaded with a weight of 150 g (10 N) and additionally weights proportional to each muscle's physiological cross-sectional area (Table 1). This is a validated method, previously used in other biomechanical studies of the wrist and the TMJ ligaments.14 15 16
Table 1. Physiological cross-sectional areas of TMJ muscles and used experimental load.
| Muscle | Cross-sectional area (cm2) | Used load (g) |
|---|---|---|
| EPL | 0.98 | 100 |
| FPL | 2.08 | 200 |
| EPB | 0.47 | 50 |
| APL | 1.93 | 200 |
| APB | 0.68 | 75 |
| FPB | 0.66 | 75 |
| OPP | 1.02 | 100 |
| Addp | 1.04 | 100 |
| FDI | 1.50 | 150 |
Abbreviations: AddP, adductor pollicis; APB, abductor pollicis brevis; APL, abductor pollicis longus; EPB, extensor pollicis brevis; EPL, extensor pollicis longus; FDI, first dorsal interosseous; FPB, flexor pollicis brevis; FPL, flexor pollicis longus; OPP, opponens.
Posteriorly, the seven TMJ stabilizing ligaments were dissected and divided into three groups; dorsal, volar, and ulnar. The dorsal ligaments include: (1) the DRL, (2) the dorsocentral ligament (DCL), and (3) the posterior oblique ligament (POL) (Fig. 1). The volar ligaments contain: (1) the AOL (s-AOL and d-AOL) and (2) the ulnar collateral ligament (UCL) (Fig. 2). The ulnar ligaments comprise: (1) the dorsal trapezium-metacarpal ligament and (2) the intermetacarpal ligament (IML) (Fig. 3).
Fig. 1.
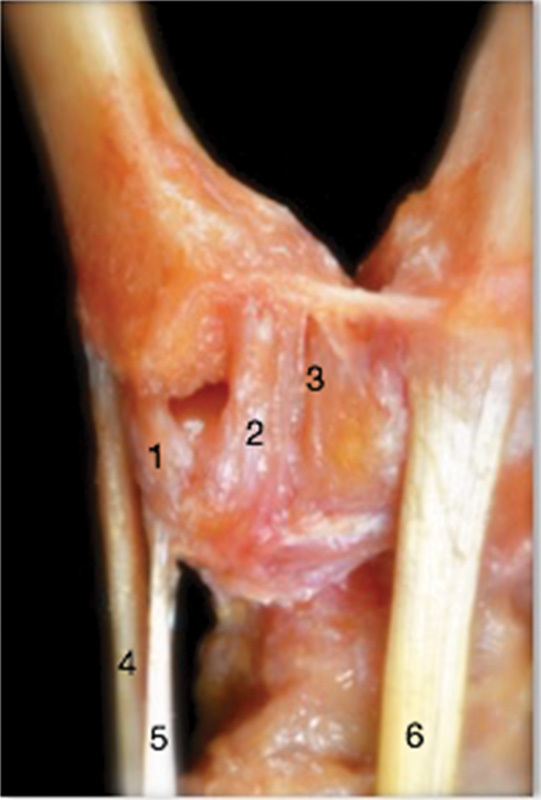
Dorsal view of a right TMJ. The dorsal ligament group includes: the DRL (1) which lies under the APL insertion distal tendon (4); it is close to APL accessory insertion distal tendon (5), the DCL (2), and the POL (3). The ECRL distal tendon is shown as (6). The 1-U TMJ arthroscopic portal passes between DCL (2) and POL (3). 1-U, 1-ulnar portal; APL, abductor pollicis longus; DCL, dorsal central ligament; DRL, dorsoradial ligament; ECRL, extensor carpi radialis longus; POL, posterior oblique ligament; TMJ, trapeziometacarpal joint.
Fig. 2.
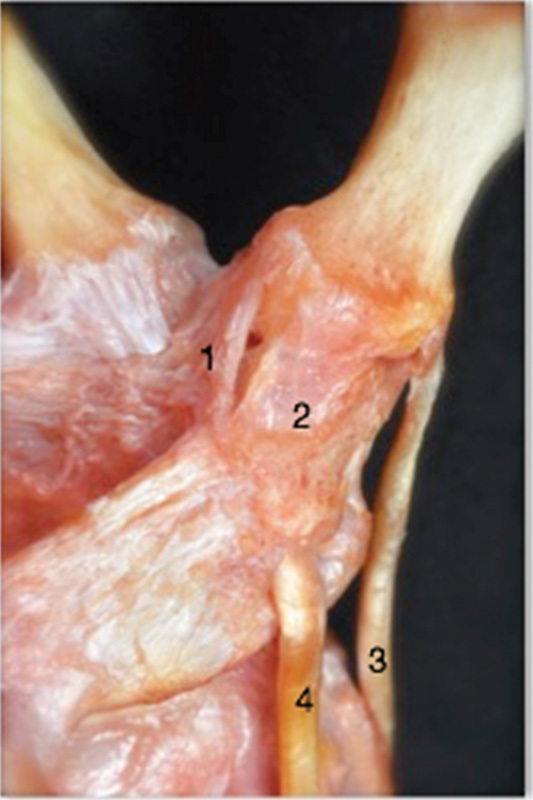
Volar view of a right TMJ. The volar ligament group includes: the UCL (1) and the AOL (2). A ligament-free window is present between the ulnar border of AOL and the radial border of APL (3). The radial border of the FCR tendon (4) is lined with the radial border of AOL (2), RP TMJ arthroscopic portal is just there. AOL, anterior oblique ligament; APL, abductor pollicis longus; FCR, flexor carpi radialis; RP TMJ, volar trapeziometacarpal joint portal; UCL, ulnar collateral ligament.
Fig. 3.
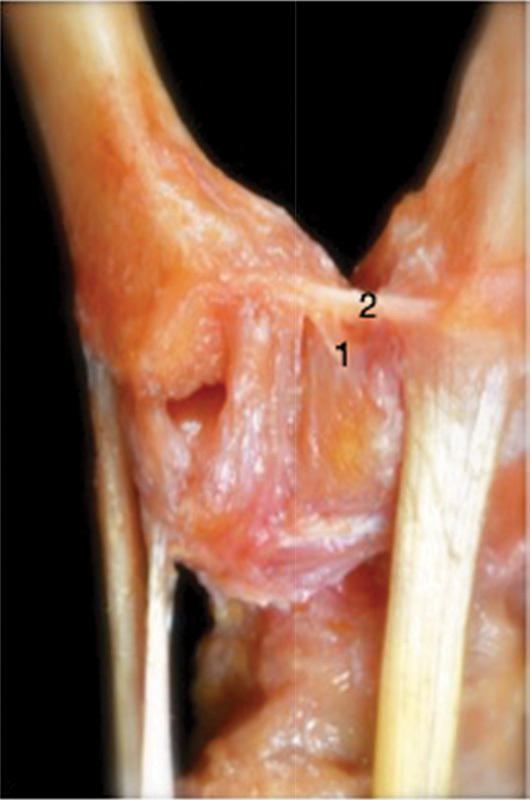
Dorsal view of a right TMJ. The ulnar ligament group comprises: the DTM-1 (1) and the IML (2). DTM-1, dorsal trapezium-metacarpal ligament; IML, intermetacarpal ligament; TMJ, trapeziometacarpal joint.
Finally, following the dissection of the specimens, one 2.4-mm Steinmann pin was drilled across the interphalangeal joint of the thumb to simulate a fully stable joint. Another 2.4-mm Steinmann pin was drilled intramedullary along the third metacarpal bone (MC3), distally to proximally, to guarantee sagittal and coronal stability throughout the entire experiment. The two pins were inserted to ensure that all thumb motion was pertaining to the metacarpophalangeal and TMJs. Following this, the specimens were vertically placed and fixed onto a testing apparatus, with the thumb fixed in 30-degree abduction, 30-degree flexion, and neutral opposition.
A six degree-of-freedom electromagnetic motion-tracking device was used to monitor spatial changes in the base of MC1 position (FasTrak system, Polhemus Inc., Colchester, VT). This system has an accuracy of 0.15 degrees for spatial orientation and 0.08 mm for its marker positioning. This tracking system included: (1) a short-range (2.54–60.9 cm) magnetic field transmitter, fixed on the horizontal surface of the testing jig and (2) three sensors that operate at a frequency of 40 Hz. The first sensor was drilled into the base of the MC1 (mobile sensor), the second one into the base of the MC3 (fixed sensor), and the third one was positioned in the dorsal aspect of the distal radius (fixed sensor). The FasTrak system allows for the evaluation of the spatial position of the three sensors relative to a fixed coordinate system (X, Y, and Z) based on the jig. Since the thumb was fixed in 30-degree abduction, 30-degree flexion, the three axes were defined as follows: (1) X defines the axis between palmar/ulnar through dorsal/radial; (2) Y represents the axis between the dorsal/ulnar and palmar/radial; and, finally (3) Z implicates the axis between proximal/MC1 extension through distal/MC1 flexion (Fig. 4). A baseline was established for each specimen.
Fig. 4.
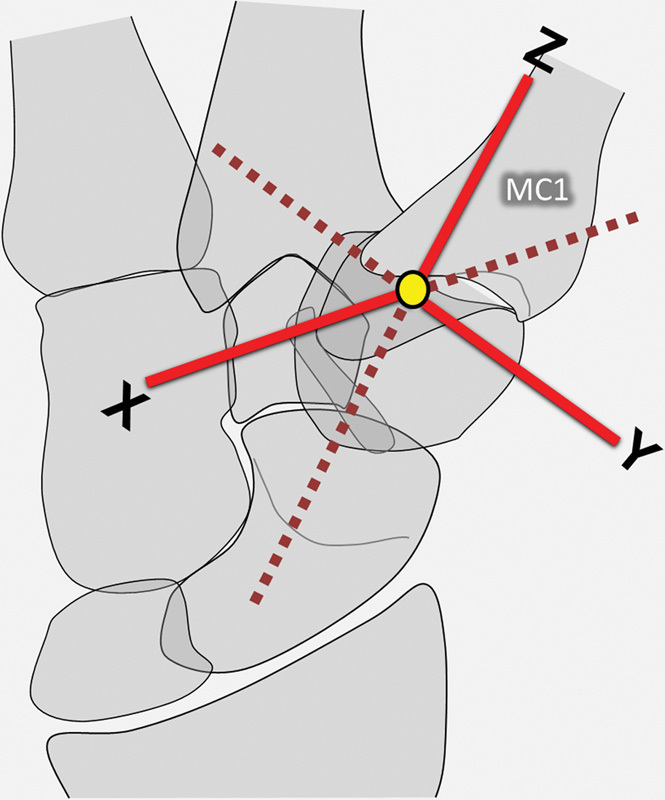
Diagram of the thumb in the testing position with accompanying X, Y, and Z axes. X: defines the axis between palmar/ulnar through dorsal/radial. Y represents the axis between dorsal/ulnar and palmar/radial. Z: implicates the axis between proximal/MC1 extension through distal/MC1 flexion. MC1, first metacarpal bone.
Finally, for each of the 11 specimens, the three ligament groups were randomly and consecutively sectioned, one after another. The order of the ligament group sectioning was randomized. The changes in the distances between the mobile sensor relative to the fixed sensors after each ligament group sectioning, compared against each specimeńs baseline, was attributed to this ligament group. We assumed that sequential sectioning of the ligament complexes did not confound measurements as we avoided accidental manipulation of the three sensors. These changes could be detected on each axis. These data were further analyzed using one-way analysis of variance and a paired t-test. The results were considered statistically significant at p < 0.05.
At the end of the experiment, all specimens were opened up and visually examined to further ensure that there were no signs of TMJ OA, which may have been overlooked by the primary X-ray examination. Only mild early changes of TMJ OA were found in four of the specimens. Those OA changes were restricted to thinning of the TMJ cartilage surface.
Results
The analysis of MC1 translation on X-axis revealed statistically significant data (Fig. 5). After isolated sectioning of the volar or ulnar ligaments, the MC1 moved dorsoradially an average 0.150 mm (standard deviation [SD]: 0.072) and 0.064 mm (SD: 0.301), respectively. In contrast, the destabilization of the MC1 after sectioning of the dorsal ligaments was substantially larger (0.523 mm; SD: 0.0512; p = 0.004).
Fig. 5.
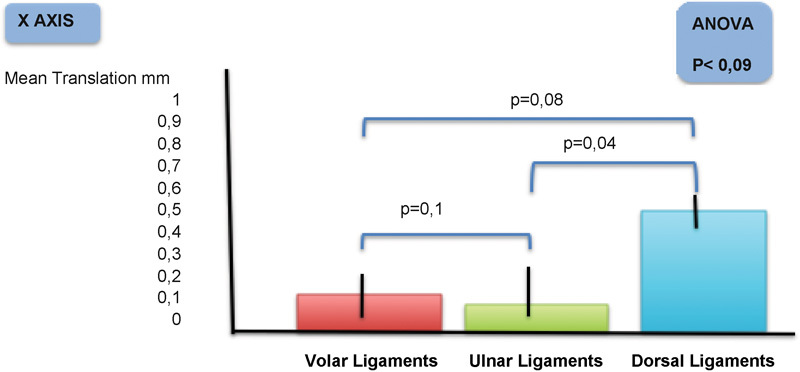
The experiment was designed to evaluate the effectiveness of each TMJ ligament group in retaining dorsoradial translation of the base of the first metacarpal bone. These are the statically significant results. After volar ligaments section, the base of the first metacarpal bone moved dorso/radially with a mean of 0.150 mm. After ulnar ligaments transaction, the base of the first metacarpal bone moved dorsoradially, but less than 0.1 mm. After dorsal ligaments cutting, the base of the first metacarpal bone moved dorsoradially with a mean of 0.523 mm. TMJ, trapeziometacarpal joint.
There were no statistically significant differences when analyzing MC1 translation, after each ligament group sectioning, on the Y or Z axis.
Discussion
In 1999, Bettinger et al8 performed anatomic measurements on 37 fresh-frozen hand specimens (average age, 73 years) radiographically screened to include only Eaton stage I and II joints. They identified 16 ligaments stabilizing the trapezium and TMJ. The ligaments were measured after removing bone–ligament–bone complexes, and length, width, thickness, prevalence insertions, fiber orientations, and positions producing ligament tension were recorded. Out of the 16 ligaments, 7 ligaments were identified as MC1 stabilizer: s-AOL, d-AOL, DRL, POL, UCL, IML, and dorsal IML. Among these seven ligaments, the DRL was, on average the widest, the thickest, and the shortest. The authors concluded “theoretically… it seems that the DRL would be an important stabilizer of the TMJ due to the fact that it is the most substantial ligament surrounding the joint.”
Bettinger et al 9 followed up their study for 1 year, reporting on the relative stiffness and strength of TMJ ligaments in 20 fresh-frozen cadavers (average age, 71 years). Among all the TMJ ligaments, they investigated the DRL and the AOL. They found that the DRL could sustain the greatest ultimate load of all ligaments and energy to failure. The AOL had the least stiffness and greatest hysteresis among all ligaments tested. The authors concluded that the DRL was the “strongest, toughest, and stiffest ligament stabling the TMJ.”
In 2012, Ladd et al10 performed a comparative macroscopic and microscopic analysis of the ligaments of the TMJ to define their role in joint stability. A total of 30 cadaveric hands (average age, 76 years) were macroscopically analyzed (ligament width, length, and thickness). The dorsal and volar ligaments were microscopically studied to analyze their sensory innervation. They found that the dorsal ligaments were significantly thicker than the volar ones with a greater cellularity and greater sensory innervation. Their findings refuted the primary importance of the AOL as a TMJ stabilizer and suggested that the AOL, both d-AOL and s-AOL, should be reclassified as a volar capsular complex. They also supported the importance of the DRL as a stabilizer of the TMJ, both from sensory perspective and from a biomechanical perspective.
D'Agostino et al,11 in 2014, also executed an anatomical study of DRL and AOL, on 13 fresh-frozen cadaveric thumbs; they also tested their material properties. They concluded that DRL is the strongest and stiffest ligament of the TMJ, significantly shorter and thicker than the AOL, which is thin, weak, and compliant. They also established than the DRL has a higher stiffness than AOL, making it a more likely candidate to provide TMJ stability. They suggested that, during TMJ stabilizing surgical procedures, the Eaton and Littler concept, relying on the volar ligament, should be reconsidered and that the importance of the DRL should be taken into account when planning surgery.
In 2012, Hagert et al12 published their study on the innervation of the TMJ ligaments. Five TMJ ligaments (DRL, DCL, POL, UCL, and AOL) were harvested from 10 fresh-frozen cadavers (average age, 65 years). The ligaments were stained with a triple-antibody immunofluorescent technique and analyzed under microscopy using a four-level ordinal grading system to quantify the level of innervation. They found the three dorsal ligaments (DRL, DCL, and POL) had more nerve endings than the anterior ligaments. In addition, the AOL had little to no innervation. The authors concluded the density of innervation of dorsal ligaments implies “their importance as primary stabilizers of TMJ.”
Collectively, these studies all suggest that the DRL is the primary TMJ stabilizer. Nevertheless, there is only one biomechanical study performed to study TMJ ligaments capable of refuting or proving these suggestions. In 1998, Van Brenk et al13 performed serial ligament sectioning on six fresh-frozen cadaver specimens. The DRL, referred to as the “dorsoradial collateral ligament,” the palmar oblique ligament, the AOL, and the IML were sectioned with the metacarpal in neutral extension, and flexion. They found that sectioning of the DRL resulted in 1.4 mm of MC1 displacement, compared with 0.08, 0.06, and 0.02 mm for the IML, the AOL, and the palmar oblique ligament, respectively. The authors concluded that reconstruction of the DRL should be considered during reconstructive procedures of the TMJ.
Our biomechanical results support the findings of all these studies that underline the functional importance of the dorsal ligaments;8 9 10 11 12 13 but it also provides two new extensions to all of them. In our biomechanical study, we proceeded to reproduce muscular loading. We simulated simultaneous muscle tone (1N) and isometric muscle contraction of every muscle that acts on the TMJ; the load was not arbitrary and externally applied to the joint as shown in Van Brenk et al study but it was proportional to each muscles cross-sectional area. Another distinguishing point of our experiment is that it was conducted with the MC1 previously placed and held in its position of maximum joint stability; the MC1 translations founded are, therefore, much more relevant. Our study concludes that, when all muscles acting on the TMJ are loaded, and the non-OA thumb is set in neutral position, the base of the MC1 always moves dorsoradially regardless of which ligament has been cut (Fig. 5). The dorsal group, however, induces the most important translation when it is cut (Fig. 5). Based on these findings, we conclude that the dorsal ligament group is the primary restraint to TMJ dorsoradial subluxation.
Hence, all these findings suggest that the dorsal ligaments should always be taken into account when planning an open or arthroscopic stabilization of the TMJ. A recently published article by Ryan et al17 reinforces those experimental research findings. The authors recommend a dorsoradial capsulodesis, performed imbricating the DRL, to treat chronic TMJ instability after acute injury or chronic repetitive use of the thumb. With this technique, four out of the five patients with painful TMJ instability became asymptomatic and were able to resume their occupations without limitations.
Implications in TMJ Arthroscopy
The isolated arthroscopic stabilizing procedures indicated to treat the nonarthritic unstable TMJ are not clearly established. There are not many articles published on this topic: most of them are limited to TMJ arthritis treatment. Nevertheless, we could extrapolate that the different current arthroscopic procedures able to treat unstable nonarthritic TMJ are: (1) debridement of the synovitis; (2) extension/abduction MC1 osteotomy; (3) thermal capsulorrhaphy, and (4) thermal shrinkage of the lax ligaments with or without temporary K-wire.
The only TMJ ligament to which thermal shrinkage is usually advocated is AOL.18 19 Thermal shrinkage of the dorsal ligaments to treat unstable TMJ has not been published. Because arthroscopic TMJ stabilization techniques can be considered as an evolution of open surgery techniques which considered AOL as the primary TMJ stabilizer ligament. Also, because the dorsal radial TMJ quadrant, where the DRL is located, is arthroscopically difficult to visualize and to reach.20
Five TMJ arthroscopy portals have been described: the thenar (T) or volar, the 1-radial (1-R), the 1-ulnar (1-U), the radial palmar or volar radial (RP), and the dorsal distal (D2). Fig. 6 illustrates the way in which the five TMJ portals and the seven joint ligaments are related.
Fig. 6.
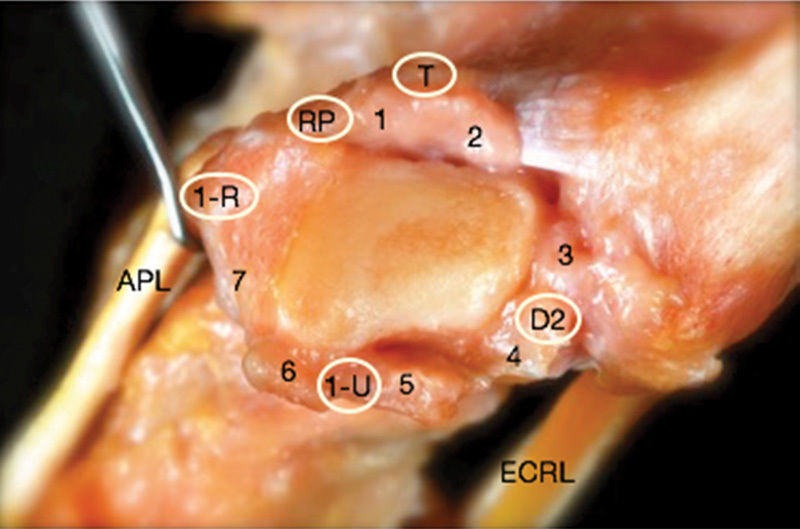
Coronal view of a right trapezium. Ligaments: Volar ligament group, AOL (1) and UCL (2); ulnar ligament group, IML (3) and DTM-1 (4); dorsal ligament group, POL (5), DCL (6), and DRL (7). Tendons: APL, ECRL. Portals: T, RP, 1-R, 1-U, and D2. 1-R, 1-radial portal; 1-U, 1- ulnar portal; AOL, anterior oblique ligament; APL, abductor pollicis longus; D2, dorsal distal portal; DCL, dorsal central ligament; DRL, dorsal-radial ligament; DTM-1, dorsal trapezium-metacarpal ligament; ECRL, extensor carpi radialis longus; IML, intermetacarpal ligament; POL, posterior oblique ligament; RP, radial portal; T, thenar portal; UCL, ulnar collateral ligament.
The 1-U portal, described by Menon,21 is established within 10 mm of the ulnar border of the EPB tendon to avoid damaging the radial artery;22 its plane passes between DCL and POL (Fig. 1): both of them are dorsal ligaments; so the 1-U portal is of limited use to correctly visualize or proceed with the dorsal ligament group.
The 1-R portal, described by Menon,21 is established radial and volar to the APL tendon. It enters the joint radially to the dorsal ligament group. It can be useful to view or act on DRL, DCL, and POL, though the DRL may not always be clearly visualized, as this ligament is directly ulnar to the portal. Triangulation with the T portal can also be difficult.
The RP portal described by Orellana and Chow23 enters the joint through a capsular window, which is radial to the AOL (Fig. 2). It allows a good assessment of the DRL, DCL, and POL, and a complete view of the lateral side of the joint. Nevertheless, triangulation with the T portal can be challenging.
The T portal described by Walsh et al24 is placed by illuminating the thenar eminence with the arthroscope in the 1-U portal. It enters the joint through the bulk of the thenar muscles, approximately 90 degrees from the 1-U portal. It is safe, far away from the neurovascular structures and it is the straightest way to work on dorsal ligaments.
Slutsky described the D2 portal25 ulnar to the EPL tendon and 1 cm distal to the v-shaped cleft at the juncture of the index and thumb metacarpal bases. It is useful for the visualization of the dorsal capsular ligaments, provides access to medial osteophytes during an arthroscopic partial trapeziectomy, and aids in the reduction of intra-articular metacarpal base fractures. However, it does not allow a straight instrumentation access to the dorsal ligaments.
Thermal shrinkage should focus on the lax dorsal ligament group, as it has been demonstrated that they are the main TMJ stabilizer. Nevertheless, DRL thermal shrinkage must not be done systematically if unnecessary; and it must not be done without a thorough technique. It has been suggested that the DRL has an important stabilizing and proprioceptive function due to its dense collagen structure and its rich innervation.26 DRL ligamentous innervation contributes to TMJ proprioception and, though, to TMJ muscular control. This muscular control should be always taken into consideration when planning TMJ stabilizing treatments such as surgical intervention and sensory reeducation before or following surgery.
Limitations of the Study
The mean age of the specimens was relatively high (73 years); this fact may have an impact on ligament integrity. However, this is similar to the ages of previously performed studies.8 9 10 11
Three subjects with advanced radiological stages of TMJ OA were excluded, before the study, to ensure sampling of normal anatomy.
This study investigated the TMJ stability only in the neutral thumb position (30-degree abduction, 30-degree flexion, and neutral opposition) as this position presents with maximal TMJ congruency. Therefore, the results only pertain to this TMJ position and this may be a weakness of the study as TMJ ligaments have different stabilizing functions for the TMJ in different thumb positions.
Conclusion
The dorsal ligament group sectioning induces the greatest dorsoradial translation of the MC1 and should, thus, be considered the primary TMJ stabilizer.
TMJ stabilizing arthroscopic procedures should, therefore, focus on the three dorsal TMJ ligaments: (1) the DRL, (2) the DCL, and (3) the POL.
The T portal is the straightest anatomical way to reach them and proceed. The best TMJ arthroscopic portals to visualize these three ligaments are the RP and the D2 portal. Nevertheless, these three portals are interchangeably used during the arthroscopic stabilizing procedure.
DRL thermal shrinkage must not be done systematically as it has been suggested that the DRL has an important TMJ stabilizing and proprioceptive function.
Footnotes
Conflict of Interest None.
References
- 1.Pellegrini V D Jr Pathomechanics of the thumb trapeziometacarpal joint Hand Clin 2001172175–184., vii–viii [PubMed] [Google Scholar]
- 2.Armstrong A L, Hunter J B, Davis T R. The prevalence of degenerative arthritis of the base of the thumb in post-menopausal women. J Hand Surg [Br] 1994;19(3):340–341. doi: 10.1016/0266-7681(94)90085-x. [DOI] [PubMed] [Google Scholar]
- 3.Haara M M, Heliövaara M, Kröger H. et al. Osteoarthritis in the carpometacarpal joint of the thumb. Prevalence and associations with disability and mortality. J Bone Joint Surg Am. 2004;86-A(7):1452–1457. doi: 10.2106/00004623-200407000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Pellegrini V D Jr, Olcott C W, Hollenberg G. Contact patterns in the trapeziometacarpal joint: the role of the palmar beak ligament. J Hand Surg Am. 1993;18(2):238–244. doi: 10.1016/0363-5023(93)90354-6. [DOI] [PubMed] [Google Scholar]
- 5.Burton R I, Pellegrini V D Jr. Surgical management of basal joint arthritis of the thumb. Part II. Ligament reconstruction with tendon interposition arthroplasty. J Hand Surg Am. 1986;11(3):324–332. doi: 10.1016/s0363-5023(86)80137-x. [DOI] [PubMed] [Google Scholar]
- 6.Eaton R G, Lane L B, Littler J W, Keyser J J. Ligament reconstruction for the painful thumb carpometacarpal joint: a long-term assessment. J Hand Surg Am. 1984;9(5):692–699. doi: 10.1016/s0363-5023(84)80015-5. [DOI] [PubMed] [Google Scholar]
- 7.Eaton R G, Littler J W. Ligament reconstruction for the painful thumb carpometacarpal joint. J Bone Joint Surg Am. 1973;55(8):1655–1666. [PubMed] [Google Scholar]
- 8.Bettinger P C, Linscheid R L, Berger R A, Cooney W P III, An K-N. An anatomic study of the stabilizing ligaments of the trapezium and trapeziometacarpal joint. J Hand Surg Am. 1999;24(4):786–798. doi: 10.1053/jhsu.1999.0786. [DOI] [PubMed] [Google Scholar]
- 9.Bettinger P C, Smutz W P, Linscheid R L, Cooney W P III, An K N. Material properties of the trapezial and trapeziometacarpal ligaments. J Hand Surg Am. 2000;25(6):1085–1095. doi: 10.1053/jhsu.2000.18487. [DOI] [PubMed] [Google Scholar]
- 10.Ladd A L, Lee J, Hagert E. Macroscopic and microscopic analysis of the thumb carpometacarpal ligaments: a cadaveric study of ligament anatomy and histology. J Bone Joint Surg Am. 2012;94(16):1468–1477. doi: 10.2106/JBJS.K.00329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.D'Agostino P, Kerkhof F D, Shahabpour M, Moermans J P, Stockmans F, Vereecke E E. Comparison of the anatomical dimensions and mechanical properties of the dorsoradial and anterior oblique ligaments of the trapeziometacarpal joint. J Hand Surg Am. 2014;39(6):1098–1107. doi: 10.1016/j.jhsa.2014.02.025. [DOI] [PubMed] [Google Scholar]
- 12.Hagert E, Lee J, Ladd A L. Innervation patterns of thumb trapeziometacarpal joint ligaments. J Hand Surg Am. 2012;37(4):706–7140. doi: 10.1016/j.jhsa.2011.12.038. [DOI] [PubMed] [Google Scholar]
- 13.Van Brenk B, Richards R R, Mackay M B, Boynton E L. A biomechanical assessment of ligaments preventing dorsoradial subluxation of the trapeziometacarpal joint. J Hand Surg Am. 1998;23(4):607–611. doi: 10.1016/s0363-5023(98)80045-2. [DOI] [PubMed] [Google Scholar]
- 14.Kobayashi M, Garcia-Elias M, Nagy L. et al. Axial loading induces rotation of the proximal carpal row bones around unique screw-displacement axes. J Biomech. 1997;30(11–12):1165–1167. doi: 10.1016/s0021-9290(97)00080-8. [DOI] [PubMed] [Google Scholar]
- 15.Salvà-Coll G, García-Elias M, León-Lopez M T, Llusá-Perez M, Rodríguez-Baeza A. Effects of forearm muscles on carpal stability. J Hand Surg Eur Vol. 2011;36(7):553–559. doi: 10.1177/1753193411407671. [DOI] [PubMed] [Google Scholar]
- 16.Mobargha N Esplugas M Garcia-Elias M Lluch A Megerle K Hagert E The effect of individual isometric muscle loading on the alignment of the base of the thumb metacarpal: a cadaveric study J Hand Surg Eur Vol 2015. (e-pub ahead of print). doi: 10.1177/1753193415597114 [DOI] [PubMed] [Google Scholar]
- 17.Rayan G, Do V. Dorsoradial capsulodesis for trapeziometacarpal joint instability. J Hand Surg Am. 2013;38(2):382–387. doi: 10.1016/j.jhsa.2012.11.009. [DOI] [PubMed] [Google Scholar]
- 18.Badia A. Trapeziometacarpal arthroscopy: a classification and treatment algorithm. Hand Clin. 2006;22(2):153–163. doi: 10.1016/j.hcl.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 19.Chu P J, Lee H M, Chung L J, Shih J T. Electrothermal treatment of thumb basal joint instability. Arthroscopy. 2009;25(3):290–295. doi: 10.1016/j.arthro.2008.10.001. [DOI] [PubMed] [Google Scholar]
- 20.Zhang A Y, Van Nortwick S, Hagert E, Yao J, Ladd A L. Thumb carpometacarpal ligaments inside and out: a comparative study of arthroscopic and gross anatomy from the robert a. Chase hand and upper limb center at stanford university. J Wrist Surg. 2013;2(1):55–62. doi: 10.1055/s-0033-1333683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Menon J. Arthroscopic management of trapeziometacarpal joint arthritis of the thumb. Arthroscopy. 1996;12(5):581–587. doi: 10.1016/s0749-8063(96)90198-x. [DOI] [PubMed] [Google Scholar]
- 22.Lindau T R Mathew P Radial artery pseudoaneurysm in TMC arthroscopy: a case report, a cadaveric study and a systematic review of the literature regarding complications MOJ Orthop Reumatol 20152675. doi: 10.15406/mojor.2015.02.00075 [Google Scholar]
- 23.Orellana M A, Chow J C. Arthroscopic visualization of the thumb carpometacarpal joint: introduction and evaluation of a new radial portal. Arthroscopy. 2003;19(6):583–591. doi: 10.1016/s0749-8063(03)00119-1. [DOI] [PubMed] [Google Scholar]
- 24.Walsh E F, Akelman E, Fleming B C, DaSilva M F. Thumb carpometacarpal arthroscopy: a topographic, anatomic study of the thenar portal. J Hand Surg Am. 2005;30(2):373–379. doi: 10.1016/j.jhsa.2004.11.011. [DOI] [PubMed] [Google Scholar]
- 25.Slutsky D J. The use of a dorsal-distal portal in trapeziometacarpal arthroscopy. Arthroscopy. 2007;23(11):12440–1.244E7. doi: 10.1016/j.arthro.2006.12.020. [DOI] [PubMed] [Google Scholar]
- 26.Ludwig C A, Mobargha N, Okogbaa J, Hagert E, Ladd A L. Altered innervation pattern in ligaments of patients with basal thumb arthritis. J Wrist Surg. 2015;4(4):284–291. doi: 10.1055/s-0035-1564982. [DOI] [PMC free article] [PubMed] [Google Scholar]


