Abstract
Ulnar styloid impaction syndrome involves repetitive friction between an excessively long ulnar styloid and the carpus, resulting in chondromalacia, synovitis, and pain. The arthroscopic diagnosis, evaluation, and management of this syndrome are not well characterized. We present a patient with chronic wrist pain of unknown origin, culminating with arthroscopic findings demonstrating substantial loss of articular cartilage on both the lunate and triquetrum. The patient successfully underwent operative ulnar styloid excision, ultimately resolving chronic wrist pain symptomology.
Keywords: long ulnar styloid, ulnar styloid impaction, ulnocarpal abutment, chronic wrist pain, wrist arthroscopy
Chronic ulnar-sided wrist pain is a familiar conundrum encountered by hand surgeons. Contributing factors to this pain are myriad as a consequence of the elaborate ligamentous and osseous structures that coalesce at this site. Ulnocarpal impaction syndrome was described initially in 1991 as a degenerative condition of the ulnar aspect of the wrist in patients with static or dynamic positive ulnar variance.1 In 1997, a similar manifestation of symptoms, termed ulnar styloid impaction syndrome, was described in a subset of eight patients exhibiting neutral or negative ulnar variance with a long ulnar styloid process.2 In contrast to the classic ulnocarpal impaction syndrome,1 this cohort displayed radiographic evidence of chondromalacia of the proximal triquetrum and ulnar styloid as opposed to the classic chondromalacia of the proximal pole of the lunate and ulnar head.2 3
Accurate assessment of the ulnar styloid length is quantified by the ulnar styloid process index (USPI); this technique controls for variability conferred by radiographic magnification, bone size, and ulnar variance as a ratio of ulnar styloid length minus ulnar variance to the width of the ulnar head.4 The ulnar styloid–capitate ratio (SCR) is reported as a more reliable method to define and compare ulnar styloid length; it is obtained from neutral posteroanterior radiographs with the third carpometacarpal joint in profile and the third metacarpal collinear with the radius.5 The average ulnar styloid length is deemed between 3 and 6 mm based on a radiographic study by Biyani et al.6 An ulnar styloid of excessive length is characterized with an USPI greater than 0.21 ± 0.07, SCR greater than 0.18 ± 0.05, and/or a styloid length greater than 6 mm.2 5 6 Among these diagnostic modalities, USPI is most valuable for identification of impaction potential, while SCR is recommended to compare ulnar styloid between individuals.5
In previous reports, ulnar styloid impaction syndrome has been identified radiographically and managed with operative intervention.2 3 7 We report a case of ulnar styloid impaction syndrome due to a long ulnar styloid in a patient with chronic wrist pain diagnosed by wrist arthroscopy and treated by ulnar styloid ostectomy.
Case Report
A 34-year-old, right-hand-dominant man with a remote history of distal radius and ulna fractures presented to our outpatient hand clinic with a complicated history of right wrist pain. The pain originated from a punching bag injury to the right hand sustained 18 months prior. Following this, he waited 3 months prior to evaluation by an orthopedic surgeon with unremitting, diffuse dorsal wrist pain. Based on clinical documentation, his pain was exacerbated by compression around the hand and resisted pronation activities, but allowed for push-ups and pull-ups. He subsequently obtained X-ray imaging of his right hand (see Fig. 1) showing no acute fractures, no lytic or blastic lesions, minimal arthritic changes at the radioscaphoid articulation, and no significant gapping or opening of the scapholunate interval. The patient was further evaluated with magnetic resonance imaging (MRI) of the right wrist for suspected ligamentous injury. The MRI suggested a possible partial tear of the palmar aspect of the scapholunate ligament and nonspecific changes of the proximal carpal bones (see Fig. 2). Based upon these findings, the patient was managed with a corticosteroid injection into the dorsal aspect of the wrist overlying the scapholunate ligament.
Fig. 1.

Preoperative posteroanterior X-ray.
Fig. 2.
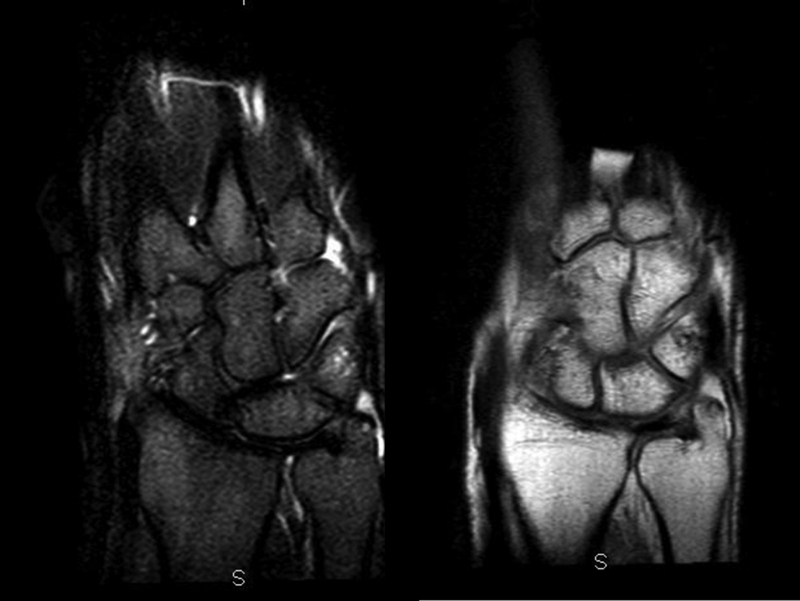
Preoperative MRI.
In the ensuing 13 months after receiving the corticosteroid injection, the patient experienced relief of his right wrist pain, after which he reported to our clinic with a 6-week history of episodic right wrist pain. In the months leading to his presentation, the patient admits to sustaining a series of nonspecific falls on the outstretched right wrist of unknown significance. On physical examination, his wrist had a benign appearance, without ecchymosis, edema, erythema, or skin lesions. Full range of motion was present and the patient did not demonstrate any neurologic deficits. There was slight swelling around the volar wrist and minimal pain with resisted extension. He was tender to palpation at the base of the third metacarpal. The scaphoid shift test and fovea test were negative, and the distal radioulnar joint was stable.
The patient was instructed to wear a splint for 4 weeks; upon follow-up, he displayed continued wrist pain. Grip strength was evaluated (JAMAR Hydraulic hand dynamometer, North Coast Medical, Gilroy, CA) as 70 pounds on the right and 120 pounds on the left. The decision was then made for wrist arthroscopy as a diagnostic and potentially therapeutic intervention.
Operative Technique
Under regional nerve block and pneumatic tourniquet control, a standard wrist arthroscope was introduced through the dorsal 3–4 portal of the involved wrist. Visual evaluation yielded prestyloid ulnar-sided synovitis and fibrillation with large lesions with articular cartilage loss of the lunate and triquetrum (see Fig. 3). The articular surfaces from the midcarpal view visualizing the proximal carpal row and the midcarpal row were intact. The triangular fibrocartilage complex displayed laxity laterally. The lunatotriquetral ligament was lax with radial-sided fibrillation and synovitis. A motorized shaver was introduced into the 3–4 and 6U portals for partial synovectomy and debridement. Sterile dressings were applied, tourniquet released, and splint applied.
Fig. 3.
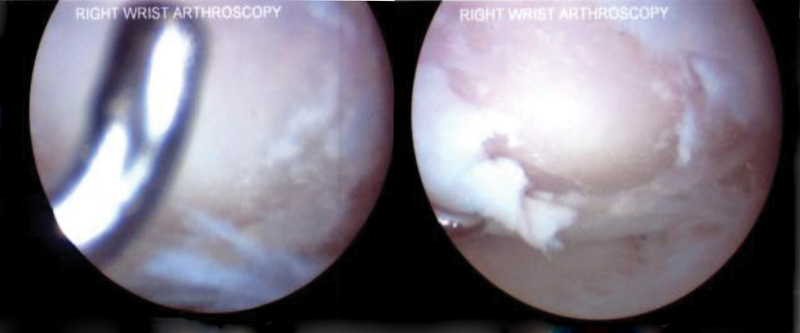
Arthroscopic images showing impaction and full-thickness chondral loss of the triquetrum.
In light of the arthroscopic findings consistent with ulnar styloid impingement syndrome, the patient continued to be symptomatic over his next follow-up and subsequently underwent open ulnar styloid ostectomy. A 1.5-cm longitudinal incision was made on the ulnar aspect of the right wrist. The dorsal sensory branches of the ulnar nerve were identified and protected. The ulnar styloid was released from the surrounding soft tissue attachments, and an osteotomy was performed with an oscillating saw. Care was taken to visualize and preserve the ulnotriquetral and ulnolunate ligaments. The patient was placed in a splint for 2 weeks followed by 4 weeks of physical therapy with active range of motion. Postoperative X-rays are shown in Fig. 4.
Fig. 4.
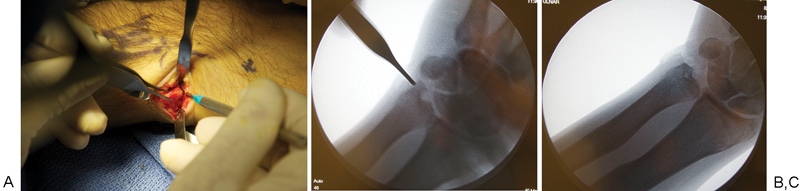
(A) Intraoperative identification of ulnar styloid and its resection. (B, C) Intraoperative images of ulnar styloid identification and final image postresection.
The patient returned 6 weeks after surgery and reported only mild discomfort with ulnar and radial deviation, demonstrating improvement of his ulnar-sided wrist pain. Grip strength was recorded as 100 pounds on the right in contrast to 125 pounds on the left. The patient was instructed to increase grip strengthening and continue active range of motion for the next 2 months followed by returning to his full activities without restrictions.
Discussion
Ulnar-sided wrist pain often presents a complex clinical challenge. Our patient experienced prolonged ulnar-sided wrist pain despite numerous physician evaluations. At a 1-year follow-up, the patient had minimal symptoms with equal grip strengths. Upon the establishment of a definitive diagnosis made only by diagnostic arthroscopy of the wrist and excluding other possible reasons for his symptoms, the pain was attributed to impaction of an excessively long ulnar styloid with the triquetrum and lunate.
Ulnar-sided abutment syndromes often cause longstanding pain on the ulnar side of the wrist from mechanical as well as reactive pathology. Ulnar positive deformity and ulnar prominence often impact the lunate and may cause progressive carpal degeneration. However, this case demonstrates a different pathology as our patient had triquetral impaction in an ulnar neutral distal radioulnar articulation. The symptoms and the underlying pathology were exclusively from a long ulnar styloid process and the impaction was noted only on arthroscopic evaluation with apparent chondromalacia of the triquetrum.
Ulnar styloid impaction syndrome may be an elusive diagnosis without clinical suspicion and adequate work-up. This process begins with accurate physical and radiographic assessments. A provocative test has been described to distinguish symptoms between ulnar styloid impaction and ulnocarpal impaction.2 The patient's elbow should be initially resting on the examination table with the forearm in neutral rotation; the examiner maximally extends the wrist and then rolls the forearm into maximum supination. Sharp pain is indicative of a positive test as the ulnar styloid and triquetrum are approximated by this maneuver. Forearm supination leads to recession of the ulnar head relative to the distal radius, thereby not reproducing pain caused by ulnocarpal impaction.
Radiographically, patients will lack positive ulnar variance and the ulnar styloid may be longer than 3 to 6 mm8 with an USPI greater than 0.21. MRI studies may be misleading as findings of impaction such as chondromalacia are often not identified with adequate sensitivity.9 Neutral posteroanterior X-ray radiographs supporting ulnar styloid impingement in the presence of clinical symptoms of ulnar styloid impaction are diagnostic and sufficient to justify operative intervention.5
Isolated cohorts of patients with ulnocarpal abutment due to a long ulnar styloid have been reported; Topper and colleagues2 first reported a series of eight patients in 1997, Tomaino et al7 further detailed seven patients in 2001, and D'Agostino et al10 described five patients in 2011 with a similar clinical scenario. Each cohort of patients was successfully managed with an ulnar styloid ostectomy without disruption of other anatomic structures. This case is unique in that there are no definitive radiographic or MRI findings suggesting impaction and there is no clear evidence of abutment on physical examination. Diagnosis of our patient was made primarily by arthroscopy as opposed to imaging or physical examination.
Ultimately, this condition of ulnar styloid impaction remains an uncommonly reported entity with limited prospective evidence for patient management. We hope to raise clinical awareness to this pathology and outline a straightforward diagnostic and therapeutic protocol. Future studies may be directed toward elucidating the pathophysiology and expounding upon treatment methodologies.
Statement of Informed Consent
Informed consent was obtained from all individual participants for whom identifying information is included in this article.
Conflict of Interest None.
Note
The authors have no financial disclosures related to this article. This study was conducted at Massachusetts General Hospital, Harvard Medical School in Boston, Massachusetts.
References
- 1.Friedman S L, Palmer A K. The ulnar impaction syndrome. Hand Clin. 1991;7(2):295–310. [PubMed] [Google Scholar]
- 2.Topper S M, Wood M B, Ruby L K. Ulnar styloid impaction syndrome. J Hand Surg Am. 1997;22(4):699–704. doi: 10.1016/S0363-5023(97)80131-1. [DOI] [PubMed] [Google Scholar]
- 3.Tomaino M M. Ulnar impaction syndrome in the ulnar negative and neutral wrist. Diagnosis and pathoanatomy. J Hand Surg [Br] 1998;23(6):754–757. doi: 10.1016/s0266-7681(98)80090-9. [DOI] [PubMed] [Google Scholar]
- 4.Garcia-Elias M. Dorsal fractures of the triquetrum-avulsion or compression fractures? J Hand Surg Am. 1987;12(2):266–268. doi: 10.1016/s0363-5023(87)80285-x. [DOI] [PubMed] [Google Scholar]
- 5.van Der Heijden B, Groot S, Schuurman A H. Evaluation of ulnar styloid length. J Hand Surg Am. 2005;30(5):954–959. doi: 10.1016/j.jhsa.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 6.Biyani A, Mehara A, Bhan S. Morphological variations of the ulnar styloid process. J Hand Surg [Br] 1990;15(3):352–354. doi: 10.1016/0266-7681_90_90018-y. [DOI] [PubMed] [Google Scholar]
- 7.Tomaino M M, Gainer M, Towers J D. Carpal impaction with the ulnar styloid process: treatment with partial styloid resection. J Hand Surg [Br] 2001;26(3):252–255. doi: 10.1054/jhsb.2001.0591. [DOI] [PubMed] [Google Scholar]
- 8.Yanagida H, Ishii S, Short W H, Werner F W, Weiner M M, Masaoka S. Radiologic evaluation of the ulnar styloid. J Hand Surg Am. 2002;27(1):49–56. doi: 10.1053/jhsu.2002.30920. [DOI] [PubMed] [Google Scholar]
- 9.Cerezal L, del Piñal F, Abascal F, García-Valtuille R, Pereda T, Canga A. Imaging findings in ulnar-sided wrist impaction syndromes. Radiographics. 2002;22(1):105–121. doi: 10.1148/radiographics.22.1.g02ja01105. [DOI] [PubMed] [Google Scholar]
- 10.D'Agostino P, Townley W A, Le Viet D, Roulot E. Oblique ulnar styloid osteotomy—a treatment for ulnar styloid impaction syndrome. J Hand Surg Am. 2011;36(11):1785–1789. doi: 10.1016/j.jhsa.2011.07.023. [DOI] [PubMed] [Google Scholar]


