Abstract
Study objective
We determine whether renal point-of-care limited ultrasonography (PLUS) used in conjunction with the Sex, Timing, Origin, Nausea, Erythrocytes (STONE) clinical prediction score can aid identification of emergency department (ED) patients with uncomplicated ureteral stone or need for urologic intervention.
Methods
This was a prospective observational study of adult ED patients undergoing computed tomography (CT) scan for suspected ureteral stone. The previously validated STONE score classifies patients into risk categories of low (≈10%), moderate (≈50%), or high (≈90%) for symptomatic stone. Renal PLUS assessed for presence of hydronephrosis before CT scanning. The primary outcomes of symptomatic ureteral stone or acutely important alternative finding were abstracted from CT reports. The secondary outcome, urologic intervention, was assessed by 90-day follow-up interview and record review.
Results
Of 835 enrolled patients, ureteral stone was identified in 53%, whereas 6.5% had an acutely important alternative finding on CT. Renal PLUS modestly increased sensitivity for symptomatic stone among low and moderate STONE score categories. Moderate or greater hydronephrosis improved specificity from 67% (62% to 72%) to 98% (93% to 99%) and 42% (37% to 47%) to 92% (86% to 95%) in low- and moderate-risk patients, with likelihood ratios of 22 (95% CI, 4.2-111) and 4.9 (95% CI, 2.9-8.3), respectively. Test characteristics among high-risk patients were unchanged by renal PLUS. For urologic intervention, any hydronephrosis was 66% sensitive (57% to 74%), whereas moderate or greater hydronephrosis was 86% specific overall (83% to 89%) and 81% (69% to 90%) sensitive and 79% 95% CI, (73-84) specific among patients with the highest likelihood of symptomatic stone.
Conclusion
Hydronephrosis on renal PLUS modestly improved risk stratification in low- and moderate-risk STONE score patients. The presence or absence of hydronephrosis among high-risk patients did not significantly alter likelihood of symptomatic stone but may aid in identifying patients more likely to require urologic intervention.
Introduction
Background
Kidney stones are common and recurrent, and complaints concerning kidney stones result in an estimated 2.1 million annual visits to US emergency departments (EDs).1 Computed tomography (CT) imaging is now performed in more than 70% of patients receiving a diagnosis of ureterolithiasis.2 Despite the significant increase in CT use for renal colic, there has not been a significant change in patient-centered outcomes, including hospital admissions or identification of alternate diagnoses.3,4 Ultrasonography use in patients with suspected renal colic is common outside the United States, but CT scanning remains the first-line imaging modality for renal colic in US EDs.5-7 Although consultant-performed ultrasonography may be obtained, point-of-care limited ultrasonography (PLUS) offers immediate information at the bedside and is available continuously.8,9 Hydronephrosis, an indirect sign of an obstructing stone, can be identified by providers with various levels of training and may correlate with stone size.10,11
Importance
A clinical prediction score for symptomatic ureteral stone may be able to reduce unnecessary imaging in patients with flank pain by identifying those with high likelihood of CT-diagnosed, uncomplicated, symptomatic stone and a low risk of acutely important alternative findings. We previously derived and validated a clinical prediction tool, the Sex, Timing, Origin, Nausea, Erythrocytes (STONE) score, which reliably risk stratifies patients, using 5 clinically available risk factors (Table 1).12 By identifying hydronephrosis in patients with suspected renal colic, clinician-performed PLUS could improve the performance of the STONE score and better categorize patients into low- and high-risk groups for kidney stone or alternative findings.
Table 1.
Components of the STONE score for uncomplicated ureteral stone in ED patients with suspected renal colic.
| Factor | Definition | Level | Points |
|---|---|---|---|
| Sex | |||
| Female patient | 0 | ||
| Male patient | 2 | ||
| Timing | Duration of pain from onset to presentation, h | ||
| >24 | 0 | ||
| 6–24 | 1 | ||
| <6 | 3 | ||
| Origin | Race | ||
| Black | 0 | ||
| Nonblack | 3 | ||
| Nausea | Presence of nausea and vomiting | ||
| None | 0 | ||
| Nausea only | 1 | ||
| Vomiting | 2 | ||
| Erythrocytes | Hematuria on urine dip | ||
| Absent | 0 | ||
| Present | 3 | ||
| Total | 0–13 |
Point total probability of symptomatic stone on CT: 0 to 5=low (<10%), 6 to 9=moderate (10% to 90%), and 10 to 13=high (>90%).
Goals of This Investigation
We hypothesized that adding renal PLUS to the previously validated STONE score would improve identification of patients with uncomplicated, symptomatic ureteral stone. Furthermore, we assessed whether the presence of hydronephrosis could reliably identify patients at higher risk for subsequent urologic intervention. Finally, we propose a suggested diagnostic pathway with management recommendations that could reduce unnecessary imaging-related radiation in patients with suspected renal colic.
Materials and Methods
Study Design and Setting
This prospective, observational study was conducted between May 2011 and February 2013 at 2 sites: the Yale–New Haven Hospital ED, an urban, academic, Level I trauma center and teaching hospital with more than 80,000 annual visits, and the Shoreline Medical Center, a freestanding, suburban ED with approximately 20,000 annual visits. A proportion of patients included in this analysis were enrolled during the validation trial of the original STONE score.12
Selection of Participants
Adult patients presenting to the ED and undergoing an unenhanced, or flank pain, protocol CT scan of the abdomen and pelvis for suspected renal colic were approached for enrollment. This study was approved by the Human Investigation Committee of the Yale Institutional Review Board, and written informed consent was obtained from all patients. Patients were excluded from enrollment if they refused or were unable to consent, were pregnant, were prisoners, or did not speak English as their primary language.
Methods of Measurement
Trained research assistants were available during predefined periods to enroll patients, including overnight, weekends, and holidays. Emergency providers were encouraged to identify potential study participants and notify research assistants; however, an automated paging system also notified research assistants whenever an order for an unenhanced CT of the abdomen and pelvis from the ED was placed. Before patients underwent CT, research assistants obtained patient consent, demographics, clinical history, and laboratory data, including point-of-care urine testing and PLUS. Data were entered electronically through tablets into the study database (FileMaker Pro 12; FileMaker Inc., Santa Clara, CA). Both clinicians and research assistants were blinded to the elements of the prediction score at data collection. CT results, including the presence, size, and location of any stones; presence and degree of hydronephrosis; and any alternative findings were abstracted from dictated attending radiologist reports after the visit by research assistants using standardized, electronic data collection forms. Research assistants performing extraction of CT results were blinded to all clinical data, including STONE score and PLUS results, except for laterality of pain.
The STONE score is a clinical prediction score for uncomplicated symptomatic stone that was retrospectively derived and prospectively validated.12 Briefly, the score was assigned according to the Framingham approach,13 in which integer point values are based on the logistic regression model. The following 5 factors were included in our model (Table 1): sex, timing (duration of pain from onset), origin (or race), nausea (or vomiting), and erythrocytes (presence of hematuria). Subsequently, the total score was categorized, with 0 to 5 points as low risk (≈10%), 6 to 9 as moderate risk (≈50%), and 10 to 13 as high risk (≈90%) of patients having a symptomatic stone identified on CT.
Before enrolled patients underwent CT scan, they received PLUS either from an emergency provider directly caring for the patient (attending physician, resident, or midlevel provider) or, if the treating clinician was not available, from another provider (typically a provider doing an ultrasonography rotation). Although providers performing the ultrasonography were aware of the clinical presentation of the patient at ultrasonography, they did not have access to the STONE score. Images of the affected kidney (typically compared to the unaffected side) were obtained with the curvilinear probe of one of the following machines: Sparq (Philips Medical, Andover, MA), Sonosite Turbo (Sonosite Inc, Bothell, WA), or Zonare z.one (Zonare Medical Systems Inc, Mountain View, CA). Dynamic images (cineloop clips) were recorded in Digitial Imaging and Communications in Medicine format.
Images were interpreted at the bedside by the performing clinician, and this interpretation was recorded in real time by the enrolling research assistant with a standardized FileMaker data collection form available through a mobile application. Providers were required to assess for the presence and degree of hydronephrosis (none, mild, moderate, or severe) on the symptomatic side. The presence of renal or ureteral stones was also documented if noted, as well as ureteral jets if present (though assessment for ureteral jets was not required).
Although ultrasonography is an integral part of the training program at our institution, no additional training in bedside renal ultrasonography was given as part of this study. Providers had various levels of ultrasonography training, ranging from beginning an ultrasonography rotation to fellowship-trained attending physicians. A previous publication details the performance characteristics of PLUS by practitioners of different levels at our institution, many of whom participated in this study.10 Our institution has an active point-of-care ultrasonography program, including an emergency ultrasonography fellowship, as well as training requirements for residents that meet or exceed American College of Emergency Physician guidelines.14
Outcome Measures
The primary outcomes in this study were symptomatic stone and acutely important alternate findings on CT. A symptomatic stone was considered present on unenhanced CT if it was located in the collecting system from the renal pelvis to the ureterovesicular junction on the same side as the patient's presenting pain according to the dictated CT report. Signs of obstruction, including the presence and degree of hydronephrosis and hydroureter or perinephric stranding, were recorded. Parenchymal and bladder stones were noted but were not considered symptomatic for this analysis. CT reports explicitly stating “signs of a passed stone” were analyzed as the patient's having had a symptomatic stone. CT results were considered to be acutely important alternate findings if such findings were determined to be the cause of the presenting flank pain and required intervention in the ED (such as administration of antibiotics, hospital admission other than for pain control, or transfer to the operating room). Specific conditions and methods for review of CT radiology reports for both symptomatic stones and acutely important alternate findings have been described previously.15
The secondary outcome, need for urologic intervention, including lithotripsy, ureteral stenting, or surgical stone removal, was determined at 90-day follow-up. Enrolled patients were initially called by research assistants at 90 days to determine whether urologic intervention was performed after discharge. If patients were not reached on initial call, a follow-up telephone call was made and a follow-up letter was sent to the patient's home address. For patients unable to be reached by initial call, follow-up call, or letter, chart review was performed to assess for urologic intervention. Research assistants trained in accepted chart review methods used standardized abstraction forms in FileMaker as previously described15,16 to assess for any urologic procedures documented in our institutional electronic health record within 90 days of the index visit. Patients who could not be contacted or had no subsequent visits after the index visit in their chart were considered lost to follow-up.
Primary Data Analysis
Means, proportions, and associated 95% confidence intervals (CIs) were calculated as appropriate. Given that few patients had severe hydronephrosis on renal PLUS, moderate and severe hydronephrosis were analyzed together as moderate or greater. The test characteristics of renal PLUS (any or moderate or greater hydronephrosis compared with no hydronephrosis) using CT-diagnosed symptomatic stone as the reference were calculated with standard definitions of sensitivity, specificity, and unweighted positive and negative likelihood ratios stratified by STONE score. Odds ratios (ORs) and 95% CIs for the associations of hydronephrosis with symptomatic stone and need for urologic intervention, as well as acutely important alternative finding, were calculated by the Fisher's exact test. Statistical analyses were performed with JMP (version 10.1; SAS Institute, Inc., Cary, NC) and Vassarstats (http://www.vassarstats.net).
Results
A total of 2,091 CT scans were obtained during the study period, of which an associated 1,391 patients (66.5%) were assessed for enrollment. The Standards for the Reporting of Diagnostic Accuracy diagram (Figure 1) describes the enrollment and outcomes for the 835 patients (83.2%) included in the analysis. Of these patients, 491 (58.8%) were also included in the validation study of the original STONE score.12 Symptomatic stone was diagnosed on CT in 52.9% of patients (442/835), whereas 54 patients (6.5%) had an acutely important alternate finding identified (Table 2). Hydronephrosis was present on renal PLUS in 46.2% of patients (386/835), with 17.5% (146/835) having moderate or greater hydronephrosis. The sensitivity and specificity (Table 3A) for any hydronephrosis on renal PLUS were 65% (61% to 70%) and 75% (71% to 79%); for moderate or greater hydronephrosis, sensitivity and specificity were 44% (38% to 51%) and 93% (89% to 95%).
Figure 1.
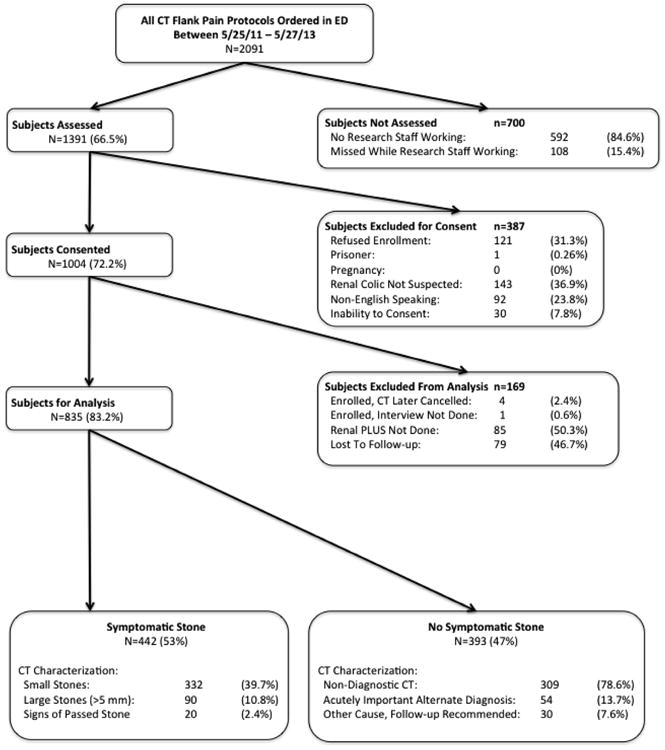
Standards for the Reporting of Diagnostic Accuracy studies (STARD) flow diagram of patient enrollment. Nondiagnostic CT included those for which the cause of pain was not identified, acutely important alternate diagnoses were those requiring intervention in the ED, and other cause with follow-up recommended included incidental findings that required further imaging or evaluation but no intervention.
Table 2.
Demographic characteristics of patients and outcomes.
| Patient Characteristic | n = 835* | |
|---|---|---|
| Age, median, IQR | 46 | 35–56 |
| Female sex | 423 | 50.7 |
| Race | ||
| Asian | 20 | 2.4 |
| Black | 117 | 14.0 |
| White | 682 | 81.7 |
| Other | 16 | 1.9 |
| Hispanic ethnicity | 173 | 20.7 |
| History of kidney stone | 321 | 38.4 |
| History of urologic procedure | 144 | 17.2 |
| Nausea/vomiting | ||
| Nausea alone | 276 | 33.1 |
| Nausea and vomiting | 334 | 40.0 |
| None | 225 | 26.9 |
| Duration of pain at presentation | ||
| <6 h | 233 | 27.9 |
| 6 h to 1 day | 279 | 33.4 |
| >1 day to 1 wk | 234 | 28.0 |
| >1 wk | 86 | 10.3 |
| Hematuria on UA | 641 | 76.8 |
| STONE score (%) | ||
| Low (<20) | 144 | 17.2 |
| Moderate (20–80) | 411 | 49.2 |
| High (>80) | 280 | 33.5 |
| Hydronephrosis on renal PLUS | ||
| None | 449 | 53.8 |
| Any | 386 | 46.2 |
| Moderate or greater | 146 | 17.5 |
| Outcomes | ||
| Acutely important alternate finding | 54 | 6.5 |
| Symptomatic kidney stone on CT | 442 | 52.9 |
| Large (>5 mm) stone† | 90 | 20.4 |
| Urologic intervention† | 133 | 30.1 |
| Lithotripsy† | 71 | 16 .1 |
| Ureteral stent† | 98 | 22.2 |
| Surgical stone removal† | 48 | 10.9 |
| Disposition | ||
| Discharge | 665 | 79.6 |
| Admit or observation | 162 | 19.4 |
| ICU | 7 | 0.8 |
| Directly to operating room | 5 | 0.6 |
| Eloped | 2 | 0.2 |
IQR, Interquartile range; UA, urinalysis; CT, computed tomography; ICU, intensive care unit.
Data are presented as No. (%) unless otherwise indicated.
Percentage of patients among those with stone identified on CT.
Table 3.
| A, Performance of STONE score for symptomatic stone on CT with and without renal PLUS. | |||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| STONE Score | Finding on Renal PLUS | Symptomatic Stone on CT | Se (95% CI) | Sp (95% CI) | LR+ (95% CI) | LR- (95% CI) | |
|
| |||||||
| Yes | No | ||||||
| All patients (n = 835) | |||||||
| Without PLUS | 442 | 393 | NA | NA | NA | NA | |
| Any hydro | 288 | 98 | 65 (61-70) | 75 (71-79) | 2.6 (2.1-3.1) | 0.46 (0.41-0.53) | |
| Moderate of greater | 123 | 23 | 44 (38-51) | 93 (89-95) | 6.1 (4.1-9.3) | 0.60 (0.54-0.67) | |
| Low (n = 144) | |||||||
| Without PLUS | 14 | 130 | 3.2 (1.7-5.3) | 67 (62-72) | 0.1 (0.06-0.16) | 1.5 (1.4-1.6) | |
| Any hydro | 9 | 17 | 64 (36-86) | 87 (80-92) | 4.9 (2.7-8.9) | 0.41 (0.2-0.83) | |
| Moderate or greater | 3 | 2 | 38 (10-74) | 98 (93-99) | 21.6 (4.2-111) | 0.64 (0.37-1.1) | |
| Moderate (n = 411) | |||||||
| Without PLUS | 183 | 228 | 41 (37-46) | 42 (37-47) | 0.71 (0.62-0.82) | 1.4 (1.2-1.6) | |
| Any hydro | 109 | 67 | 60 (52-67) | 71 (64-76) | 2.0 (1.6-2.6) | 0.57 (0.48-0.69) | |
| Moderate or greater | 53 | 15 | 42 (36-48) | 92 (86-95) | 4.9 (2.9-8.3) | 0.64 (0.55-0.74) | |
| High (n = 280) | |||||||
| Without PLUS | 245 | 35 | 55 (51-60) | 91 (88-94) | 6.2 (4.5-8.6) | 0.49 (0.44-0.55) | |
| Any hydro | 170 | 14 | 69 (63-75) | 60 (42-76) | 1.7 (1.1-2.6) | 0.51 (0.41-0.64) | |
| Moderate or greater | 67 | 6 | 47 (39-56) | 78 (57-91) | 2.1 (1.0-4.4) | 0.68 (0.57-0.81) | |
|
| |||||||
| B, Performance of STONE score for urologic intervention with and without renal PLUS. | |||||||
|
| |||||||
| Urologic Intervention | |||||||
|
|
|||||||
| STONE Score | Finding on Renal PLUS | Yes | No | Se (95% CI) | Sp (95% CI) | LR+ (95% CI) | LR- (95% CI) |
|
| |||||||
| All patients (n = 835) | |||||||
| Without PLUS | 113 | 702 | NA | NA | NA | NA | |
| Any hydro | 88 | 298 | 66 (57-74) | 58 (54-61) | 1.6 (1.3-1.8) | 0.59 (0.46-0.75) | |
| Moderate or greater | 48 | 98 | 36 (28-45) | 86 (83-89) | 2.6 (1.9-3.5) | 0.74 (0.65-0.84) | |
| Low (n = 144) | |||||||
| Without PLUS | 9 | 135 | 6.7 (3.3-13) | 81 (78-84) | 0.35 (0.18-0.67) | 1.1 (1.1-1.2) | |
| Any hydro | 4 | 22 | 44 (15-77) | 84 (76-89) | 2.7 (1.2-6.2) | 0.66 (0.37-1.2) | |
| Moderate or greater | 3 | 2 | 33 (9-69) | 99 (94-99) | 23 (4.3-117) | 0.68 (0.43-1.1) | |
| Moderate (n = 411) | |||||||
| Without PLUS | 65 | 346 | 49 (40-58) | 51 (47-55) | 0.99 (0.82-1.2) | 1.0 (0.85-1.2) | |
| Any hydro | 36 | 140 | 55 (43-68) | 60 (54-65) | 1.4 (1.1-1.8) | 0.75 (0.57-0.98) | |
| Moderate or greater | 19 | 49 | 29 (19-42) | 86 (82-89) | 2.1 (1.3-3.3) | 0.82 (0.7-0.96) | |
| High (n = 280) | |||||||
| Without PLUS | 59 | 221 | 44 (36-53) | 69 (65-72) | 1.4 (1.1-1.8) | 0.81 (0.7-0.95) | |
| Any hydro | 48 | 136 | 81 (69-90) | 39 (32-45) | 1.3 (1.1-1.6) | 0.48 (0.28-0.84) | |
| Moderate or greater | 26 | 47 | 44 (31-58) | 79 (73-84) | 2.1 (1.4-3) | 0.71 (0.57-0.89) | |
Hydro, Hydronephrosis; Se, sensitivity; Sp, specificity; LR+, positive likelihood ratio; LR−, negative likelihood ratio.
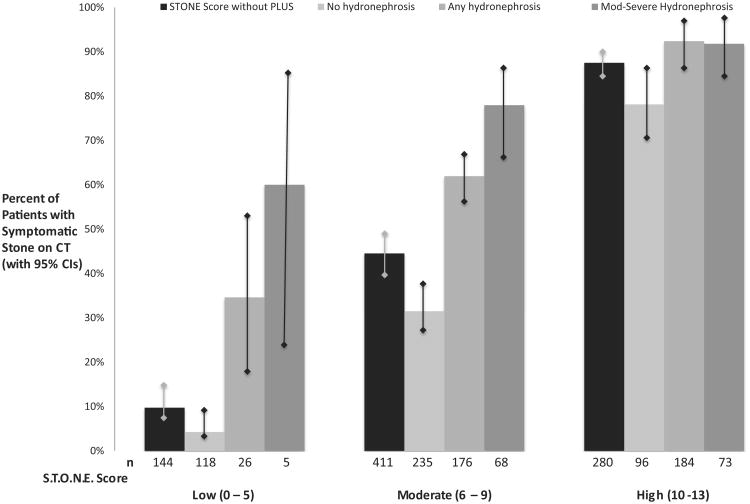
The presence of any hydronephrosis on PLUS increased prevalence of ureteral stone in the low and moderate STONE score groups (Figure 2). No significant difference was observed in high-risk patients by the addition of renal PLUS when the prevalence of symptomatic stone was 87.5% (83.1% to 90.9%). Assessment for any hydronephrosis increased sensitivity in the low and moderate STONE score categories (Table 3A), from 3.2% (1.7%, 5.3%) to 64% (36%, 86%) and 41% (37%, 46%) to 60% (52%, 67%). The presence of moderate or greater hydronephrosis improved specificity from 67% (62% to 72%) to 98% (93% to 99%) and 42% (37% to 47%) to 92% (86% to 95%) in low- and moderate-risk patients, with likelihood ratios of 22 (4.2, 111) and 4.9 (2.9, 8.3), respectively. The use of renal PLUS among patients with a high likelihood of symptomatic stone did not significantly alter test characteristics.
Figure 2.
Comparison of STONE score with and without renal PLUS for diagnosis of symptomatic ureteral stone on CT. Total number of patients in each risk category of the STONE score (low, moderate, or high) is given with the percentage of patients receiving a diagnosis of symptomatic stone by degree of hydronephrosis on PLUS (none, any, or moderate to severe). Any hydronephrosis includes moderate to severe. Error bars delineate the 95% CIs of the point estimate.
Follow-up was completed by telephone interview and medical record review in 81.4% of patients, whereas 18.6% underwent medical record review alone. Urologic intervention within 90 days was performed for 30.1% of patients (133/442) receiving a diagnosis of symptomatic stone, or 16% of the total study population. Compared with patients without hydronephrosis on renal PLUS, those with any hydronephrosis were more likely to require urologic intervention: 22.8% with any hydronephrosis (OR 2.7; 95% CI 1.8 to 3.9) and 32.9% with moderate or greater hydronephrosis (OR 3.5; 95% CI 2.3 to 5.3) compared with 10% with no hydronephrosis. The prevalence of ureteral stones greater than 5 mm on CT increased with the presence and degree of hydronephrosis on renal PLUS: compared with patients with no hydronephrosis, those with any hydronephrosis were approximately 4 times more likely to have a large stone (17.4% versus 5.1%; OR 3.9; 95% CI 2.4 to 6.4), and those with moderate or greater hydronephrosis were approximately 5 times more likely (28.1% versus 7.1%; OR 5.1; 95% CI 3.2 to 8.1) to have a large stone.
Overall, presence of any hydronephrosis was 66% sensitive (57% to 74%) for urologic intervention, whereas moderate or greater hydronephrosis was 86% specific (83% to 89%) (Table 3B). Stratification of renal PLUS results by STONE score demonstrated improved test characteristics, with improved sensitivity for urologic intervention in patients at highest risk for symptomatic stone and improved specificity for those at lowest risk, particularly if moderate or greater hydronephrosis was present. Of the 59 patients with a high STONE score who received intervention within 90 days of their ED visit, 48 (81%) had some degree of hydronephrosis. Forty-nine of 59 patients (83%) requiring intervention had stones greater than 5 mm, and 42 of 49 (86%) with large stone had hydronephrosis on renal PLUS.
There were 54 acutely important alternate findings identified on CT in 8.3%, 9.0%, and 1.8% of patients in the low, moderate, and high risk STONE score groups, respectively. The presence of hydronephrosis further reduced the risk of alternate diagnosis being identified (OR 0.31; 95% CI 0.16 to 0.60). Twelve patients in this study were found to have a significant alternative diagnosis requiring intervention in the ED if hydronephrosis was observed on renal PLUS (only 2 among patients at high risk for stone, 1 with pyelonephritis and 1 with appendicitis) (Table 4).
Table 4.
Acutely important alternative findings on CT stratified by STONE score and presence of hydronephrosis.
| STONE Score Risk Category | ||||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| All Patients | Low | Moderate | High | |||||
|
|
|
|
|
|||||
| Type of AIAF Identified on CT | All | Hydro on Renal PLUS | All | Hydro on Renal PLUS | All | Hydro on Renal PLUS | All | Hydro on Renal PLUS |
| AAA | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 |
| Appendicitis | 5 | 3 | 1 | 0 | 3 | 2 | 1 | 1 |
| Bowel obstruction or ileus | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 |
| Cholecystitis | 2 | 1 | 0 | 0 | 2 | 1 | 0 | 0 |
| Diverticulitis | 11 | 2 | 2 | 0 | 9 | 2 | 0 | 0 |
| Malignancy/neoplasm/concerning mass | 4 | 0 | 3 | 0 | 1 | 0 | 0 | 0 |
| Mesenteric adenitis | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 0 |
| Ovarian or adnexal pathology | 3 | 0 | 0 | 0 | 3 | 0 | 0 | 0 |
| Pancreatitis | 2 | 0 | 0 | 0 | 1 | 0 | 1 | 0 |
| Pneumonia | 2 | 0 | 1 | 0 | 1 | 0 | 0 | 0 |
| UTI/cystitis/pyelonephritis | 16 | 4 | 3 | 1 | 10 | 2 | 3 | 1 |
| Abscess | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 |
| Colitis/enteritis | 2 | 0 | 1 | 0 | 1 | 0 | 0 | 0 |
| Hematoma | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 |
| IVC thrombus | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| Vesicovaginal fistula | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 |
| AIAF | 54 | 11 | 12 | 1 | 37 | 8 | 5 | 2 |
| Patients | 835 | 386 | 144 | 26 | 411 | 176 | 280 | 184 |
| Percentage | 6.5 | 2.8 | 8.3 | 3.8 | 9.0 | 4.5 | 1.8 | 1.1 |
AAA, Symptomatic abdominal aortic aneurysm; UTI, urinary tract infection; IVC, inferior vena cava; AIAF, acutely important alternative finding on CT.
Limitations
This study was conducted at an academic tertiary care institution with an active bedside ultrasonography training program, and the generalizability of its results may therefore be limited. However, availability of point-of-care ultrasonography is becoming more widespread in both teaching and community settings. This study included providers of various levels of experience. Previous work from our group has shown that emergency physicians with fellowship training in ultrasonography are better at accurately discerning hydronephrosis, and addition of PLUS by this group may provide more benefit than addition of ultrasonography by nonfellowship-trained emergency physicians.10 Although all of the patients in our study received both ultrasonography and a CT scan, patients were eligible for inclusion only if the provider intended to order CT for suspected renal colic. Thus, some patients with symptomatic stones may not have been included if they were discharged without CT imaging. Because the goal of this investigation was to reduce diagnostic imaging–related radiation, the suggested algorithm is best applied for patients for whom the provider intends to obtain imaging for suspected renal colic.
Discussion
To our knowledge, this study is the first rigorous and large study to demonstrate the utility of combining an objective clinical prediction tool for uncomplicated renal colic with PLUS. The improvement in clinical prediction of ureteral stone by using STONE PLUS was most evident in patients who had low to moderate likelihood of ureteral stone according to history and urinalysis result. The presence of hydronephrosis on PLUS in these groups increases the likelihood of ureteral stone. In patients who are already very likely to have stone according to symptoms and urinalysis result (high STONE score), PLUS may not significantly improve the clinical prediction of ureteral stone. However, the absence of hydronephrosis in patients with high STONE score is associated with a low risk of subsequent need for urologic intervention within 90 days of their ED visit. Conversely, the presence of moderate or severe hydronephrosis potentially identifies low- and moderate-risk STONE score patients at higher risk for subsequent intervention.
Ultrasonography has the potential to aid in the diagnosis of symptomatic stones by visualization of the stones directly or through secondary signs of obstruction, namely, hydronephrosis, without exposing patients to ionizing radiation. However, studies of emergency physician–performed ultrasonography have reported sensitivities ranging from 72% to 97% and specificities ranging from 69% to 83%, which limits the utility of this test in isolation from the clinical scenario.8,11,17-19 A recent multicenter, randomized trial of ED patients with suspected renal colic demonstrated the noninferiority of ultrasonography, including point-of-care ultrasonography, compared with CT with respect to diagnosis of symptomatic stones and identification of significant alternative diagnoses.20 The study concluded that the “results do not suggest that patients should undergo only ultrasonography imaging, but rather that ultrasonography should be used as the initial diagnostic imaging test, with further imaging performed at the discretion of the physician on the basis of clinical judgment.” Nearly half (40%) of the patients in the point-of-care ultrasonography group received a regular-dose CT scan. Specifically, it was not noted or suggested how point-of-care ultrasonography should affect the decision to obtain a CT. Our study adds to this work by helping to discern what PLUS can add to clinical prediction and when it is likely to be most helpful. Being able to stratify patients into groups that are very likely to have a symptomatic stone and very unlikely to have an alternative diagnosis may allow avoidance of CT entirely or guide appropriate use of reduced-dose CT.
The incorporation of PLUS was most helpful for patients with a low or moderate clinical likelihood, which comprised two thirds of our sample. In particular, the presence of moderate or greater hydronephrosis in these groups significantly increased specificity and likelihood of a symptomatic stone being identified on CT. If likelihood of symptomatic stone was high before PLUS, the presence or absence of hydronephrosis did not make a statistically significant difference in likelihood; however, hydronephrosis was associated with the need for urologic intervention. Although previous studies have suggested that the degree of hydronephrosis correlates with stone size,10,11 only 1 retrospective chart review of radiology-performed ultrasonography21 and 1 small prospective study22 assessed the relationship between hydronephrosis and urologic outcomes. Our study confirms and adds to these findings, suggesting PLUS can be useful for identifying patients who may need subsequent urologic intervention. Thus, the presence of hydronephrosis, particularly moderate or greater hydronephrosis, on renal PLUS in patients with high STONE score may suggest the need for closer follow-up or reduced-dose CT to definitively characterize stone size and location.
In accordance with these results, we suggest a diagnostic algorithm for ED patients with suspected renal colic to aid the provider intending to order further imaging (Figure 3). Patients with a high likelihood of symptomatic stone and low likelihood of an important alternate diagnosis may be managed expectantly with a trial of spontaneous passage without further imaging. If providers wish to characterize stone size and location in selected patients (such as patients with high STONE score with persistent pain in the ED or hydronephrosis on renal PLUS), we recommend reduced-dose CT.
Figure 3.
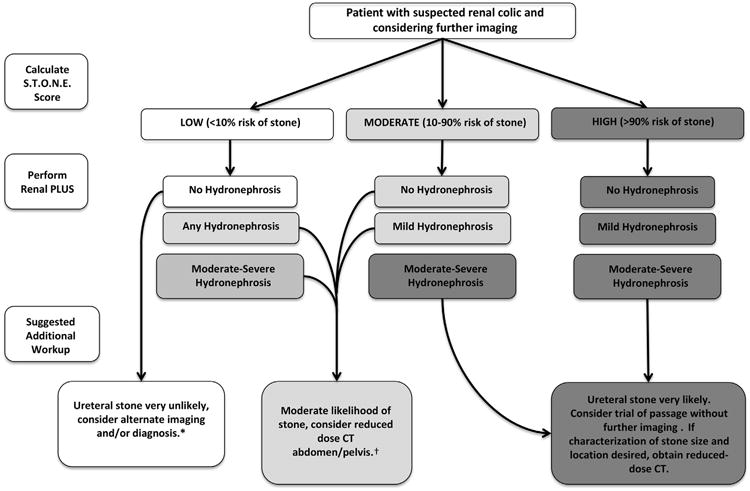
Suggested algorithm incorporating STONE score for symptomatic stone and renal PLUS for diagnosis and management of ED patients with suspected renal colic. Moderate-risk patients with moderate hydronephrosis may be managed similarly to high-risk patients. Renal PLUS does not significantly add to diagnosis of symptomatic stone in high-risk patients, but the absence of hydronephrosis makes the need for urologic intervention unlikely. *Approximately three quarters of CT scans in the low-risk group were nondiagnostic. †Approximately two thirds of low-risk patients with moderate hydronephrosis or moderate-risk patients with any hydronephrosis will have a symptomatic stone. Low- and moderate-risk patients with hydronephrosis are at increased risk of subsequent need of urologic intervention.
Reduced-dose CT can reduce ionizing radiation by more than 80% while maintaining sensitivity and specificity, especially for larger stones that may require intervention, and also identify significant alternative causes of flank pain.23 Reduced-dose CT is recommended by the American College of Radiologists when symptomatic stone is suspected.24 However, less than 2% of CT scans for renal colic in the United States are conducted with a reduced-dose protocol.25 It is likely that this is due to concern about missing alternative diagnoses, and it has been suggested that reduced-dose (and particularly “ultralow”) CT is most appropriately conducted in patients with high likelihood of stone.26 We believe improved risk stratification of patients with the STONE PLUS algorithm may increase appropriate use of this test.
Applying this strategy to our study population, of the 835 regular-dose CT scans obtained, we could potentially safely eliminate 280 (34%) in patients in the high-risk category and 68 (8.1%) for moderate-risk patients with moderate to severe hydronephrosis. Approximately 90% of these patients would have a symptomatic stone and approximately 1% would potentially have a missed alternate diagnosis if no further imaging other than renal PLUS were obtained. Furthermore, low- and moderate-risk patients with hydronephrosis (202/835, or 24% in this population) have a relatively high chance of having a symptomatic stone (58%), for which a low-dose CT is a reasonable option to confirm the diagnosis, rule out alternative causes, and identify larger stones likely to require urologic intervention. Reduced-dose CT in these patients would result in an approximately 80% reduction in dose. Therefore, a complete elimination or significant reduction in delivered dose could be achieved in 58% of patients (478/835) in this population without missing clinically relevant diagnoses.
Our results suggest addition of renal PLUS to the STONE clinical prediction score improves classification of patients with symptomatic stone, particularly in those with low or moderate clinical risk. Furthermore, the presence of at least moderate hydronephrosis is specific for urologic intervention and may identify patients needing further imaging or closer follow-up. Finally, the proposed algorithm has the potential to safely reduce the overuse of CT for renal colic in the ED, and prospective studies of external validation and implementation are warranted.
Editor’s Capsule Summary.
What is already known on this topic
The Sex, Timing, Origin, Nausea, Erythrocytes (STONE) score has been proposed as a means of sorting patients with suspected renal colic as low, moderate, or high risk for the presence of a stone.
What question this study addressed
Does addition of point-of-care limited ultrasonography (PLUS) improve performance of the STONE score in emergency department patients?
What this study adds to our knowledge
In 835 enrolled subjects, addition of PLUS to the STONE score modestly improved sensitivity and specificity for stones and the need for intervention in low- and moderate-risk patients.
How this is relevant to clinical practice
Although the addition of ultrasonography improved STONE score accuracy somewhat, this score (either with or without ultrasonography) requires successful external validation before it can be advocated for routine use.
Acknowledgments
Funding and support: By Annals policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). Funding for this work was provided in part by the Agency for Healthcare Research and Quality (AHRQ) 5R01HS018322. Drs. Gross, Molinaro, Singh, and Moore and Ms. Jessey received salary support from this AHRQ grant. Dr. Gross has also received grant support from Medtronic and Johnson & Johnson and has served on the Scientific Advisory Board for Fair Health, Inc.
Footnotes
Author contributions: BD and CLM conceived the study. CPG, DS, and CLM and obtained research funding. SL and CLM supervised the conduct of the trial and data collection. SL participated in recruitment of patients. AM, SL, RJ, and CLM managed the data, including quality control. CPG and AM provided statistical advice. CPG, AM, and DS provided advisement on study design and methodology. BD, AM, RJ, and CLM analyzed the data. BD drafted the article and all authors contributed substantially to its revision. BD takes responsibility for the paper as a whole.
Presented as an abstract at the Society for Academic Emergency Medicine annual meeting, May 2014, Dallas, TX.
Clinical trial registration number: NCT01352676
References
- 1.Hyams ES, Korley FK, Pham JC, et al. Trends in imaging use during the emergency department evaluation of flank pain. J Urol. 2011;186:2270–2274. doi: 10.1016/j.juro.2011.07.079. [DOI] [PubMed] [Google Scholar]
- 2.Westphalen AC, Hsia RY, Maselli JH, et al. Radiological imaging of patients with suspected urinary tract stones: national trends, diagnoses, and predictors. Acad Emerg Med. 2011;18:699–707. doi: 10.1111/j.1553-2712.2011.01103.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cupisti A, Pasquali E, Lusso S, et al. Renal colic in Pisa emergency department: epidemiology, diagnostics and treatment patterns. Intern Emerg Med. 2008;3:241–244. doi: 10.1007/s11739-008-0145-z. [DOI] [PubMed] [Google Scholar]
- 4.Türk C, Knoll T, Petrik A, et al. Guidelines on urolithiasis. Eur Assoc Urol. 2011 [Google Scholar]
- 5.Moore CL, Scoutt L. Sonography first for acute flank pain? J Ultrasound Med. 2012;31:1703–1711. doi: 10.7863/jum.2012.31.11.1703. [DOI] [PubMed] [Google Scholar]
- 6.Noble VE, Brown DF. Renal ultrasound. Emerg Med Clin North Am. 2004:651–659. doi: 10.1016/j.emc.2004.04.014. [DOI] [PubMed] [Google Scholar]
- 7.Kartal M, Eray O, Erdogru T, et al. Prospective validation of a current algorithm including bedside US performed by emergency physicians for patients with acute flank pain suspected for renal colic. Emerg Med J. 2006;23:341–344. doi: 10.1136/emj.2005.028589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dalziel PJ, Noble VE. Bedside ultrasound and the assessment of renal colic: a review. Emerg Med J. 2012;30:3–8. doi: 10.1136/emermed-2012-201375. [DOI] [PubMed] [Google Scholar]
- 9.Moak JH, Lyons MS, Lindsell CJ. Bedside renal ultrasound in the evaluation of suspected ureterolithiasis. Am J Emerg Med. 2012;30:218–221. doi: 10.1016/j.ajem.2010.11.024. [DOI] [PubMed] [Google Scholar]
- 10.Herbst MK, Rosenberg G, Daniels B, et al. Effect of provider experience on clinician-performed ultrasonography for hydronephrosis in patients with suspected renal colic. Ann Emerg Med. 2014;64:269–276. doi: 10.1016/j.annemergmed.2014.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goertz JK, Lotterman S. Can the degree of hydronephrosis on ultrasound predict kidney stone size? Am J Emerg Med. 2010;28:813–816. doi: 10.1016/j.ajem.2009.06.028. [DOI] [PubMed] [Google Scholar]
- 12.Moore CL, Bomann S, Daniels B, et al. Derivation and validation of a clinical prediction rule for uncomplicated ureteral stone—the STONE score: retrospective and prospective observational cohort studies. BMJ. 2014;348:g2191. doi: 10.1136/bmj.g2191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sullivan LM, Massaro JM, D'Agostino RB. Presentation of multivariate data for clinical use: the Framingham Study risk score functions. Stat Med. 2004;23:1631–1660. doi: 10.1002/sim.1742. [DOI] [PubMed] [Google Scholar]
- 14.American College of Emergency Physicians. Emergency ultrasound guidelines. Ann Emerg Med. 2009;53:550–570. doi: 10.1016/j.annemergmed.2008.12.013. [DOI] [PubMed] [Google Scholar]
- 15.Moore CL, Daniels B, Singh D, et al. Prevalence and clinical importance of alternative causes of symptoms using a renal colic computed tomography protocol in patients with flank or back pain and absence of pyuria. Acad Emerg Med. 2013;20:470–478. doi: 10.1111/acem.12127. [DOI] [PubMed] [Google Scholar]
- 16.Gilbert EH, Lowenstein SR, Koziol-McLain J, et al. Chart reviews in emergency medicine research: where are the methods? Ann Emerg Med. 1996;27:305–308. doi: 10.1016/s0196-0644(96)70264-0. [DOI] [PubMed] [Google Scholar]
- 17.Erwin B, Carroll B, Sommer F. Renal colic: the role of ultrasound in initial evaluation. Radiology. 1984;152:147–150. doi: 10.1148/radiology.152.1.6729105. [DOI] [PubMed] [Google Scholar]
- 18.Gaspari RJ, Horst K. Emergency ultrasound and urinalysis in the evaluation of flank pain. Acad Emerg Med. 2005;12:1180–1184. doi: 10.1197/j.aem.2005.06.023. [DOI] [PubMed] [Google Scholar]
- 19.Gleyzer A, Sinert R. Emergency ultrasound in the evaluation of flank pain: limited data. Acad Emerg Med. 2006;13:704–705. doi: 10.1197/j.aem.2006.01.012. [DOI] [PubMed] [Google Scholar]
- 20.Smith-Bindman R, Aubin C, Bailitz J, et al. Ultrasonography versus computed tomography for suspected nephrolithiasis. N Engl J Med. 2014;371:1100–1110. doi: 10.1056/NEJMoa1404446. [DOI] [PubMed] [Google Scholar]
- 21.Taylor M, Woo M, Pageau P, et al. Ultrasonography for the prediction of urological surgical intervention in patients with renal colic. Emerg Med J. 2016;33:118–123. doi: 10.1136/emermed-2014-204524. [DOI] [PubMed] [Google Scholar]
- 22.Fields JM, Fishcer JI, Anderson KL, et al. The ability for renal ultrasound and ureteral jet evaluation to predict 30-day outcomes in patients with suspected nephrolithiasis. Am J Emerg Med. 2015;33:1402–1406. doi: 10.1016/j.ajem.2015.07.014. [DOI] [PubMed] [Google Scholar]
- 23.Moore CL, Daniels B, Ghita M, et al. Accuracy of reduced-dose computed tomography for ureteral stones in emergency department patients. Ann Emerg Med. 2015;65:189–198.e2. doi: 10.1016/j.annemergmed.2014.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Coursey CA, Casalino DD, Remer EM, et al. ACR Appropriateness Criteria® acute onset flank pain—suspicion of stone disease. Ultrasound Q. 2012;28:227–233. doi: 10.1097/RUQ.0b013e3182625974. [DOI] [PubMed] [Google Scholar]
- 25.Lukasiewicz A, Bhargavan-Chatfield M, Coombs L, et al. Radiation dose index of renal colic protocol CT studies in the United States: a report from the American College of Radiology National Radiology Data Registry. Radiology. 2014;271:445–451. doi: 10.1148/radiol.14131601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Frei R. Ultra-low CT dose accurately detects renal stones. [Accessed August 10, 2014];Renal Urol News. 2012 :1–3. Available at: http://www.renalandurologynews.com/ultra-low-ct-dose-accurately-detects-renal-stones/article/248315/