Abstract
Background
Correction of metabolic acidosis (MA) with nutritional therapy or bicarbonate administration is widely used in chronic kidney disease (CKD) patients. However, it is unknown whether these interventions reduce insulin resistance (IR) in diabetic patients with CKD. We sought to evaluate the effect of MA correction on endogenous insulin action in diabetic type 2 (DM2) CKD patients.
Methods
A total of 145 CKD subjects (83 men e 62 women) with DM2 treated with oral antidiabetic drugs were included in the study and followed up to 1 year. All patients were randomly assigned 1:1 to either open-label (A) oral bicarbonate to achieve serum bicarbonate levels of 24–28 mmol/L (treatment group) or (B) no treatment (control group). The Homeostatic model assessment (HOMA) index was used to evaluate IR at study inception and conclusion. Parametric and non-parametric tests as well as linear regression were used.
Results
At baseline no differences in demographic and clinical characteristics between the two groups was observed. Average dose of bicarbonate in the treatment group was 0.7 ± 0.2 mmol/kg. Treated patients showed a better metabolic control as confirmed by lower insulin levels (13.4 ± 5.2 vs 19.9 ± 6.3; for treated and control subjects respectively; p < 0.001), Homa-IR (5.9[5.0-7.0] vs 6.3[5.3–8.2]; p = 0.01) and need for oral antidiabetic drugs. The serum bicarbonate and HOMA-IR relationship was non-linear and the largest HOMA-IR reduction was noted for serum bicarbonate levels between 24 and 28 mmol/l. Adjustment for confounders, suggests that serum bicarbonate rather than treatment drives the effect on HOMA-IR.
Conclusions
Serum bicarbonate is related to IR and the largest HOMA-IR reduction is noted for serum bicarbonate between 24 and 28 mmol/l. Treatment with bicarbonate influences IR. However, changes in serum bicarbonate explains the effect of treatment on HOMA index. Future efforts are required to validate these results in diabetic and non-diabetic CKD patients.
Trial registration
The trial was registered at www.clinicaltrial.gov (Use of Bicarbonate in Chronic Renal Insufficiency (UBI) study - NCT01640119)
Keywords: CKD, Diabetes, Metabolic acidosis, Homa-test, Sodium bicarbonate
Background
Incidence of chronic kidney disease (CKD) as well as the prevalence of diabetic subjects among CKD patients are steadily increasing [1, 2]. As renal function declines, metabolic acidosis and insulin resistance (IR) commonly arise. Among others, these metabolic complications are associated with serious consequences on bones and nutritional status [3, 4] and likely contribute to some of the abysmal risk of death associated with CKD.
Insulin resistance (IR) is characterized by suboptimal biological responses of the liver, skeletal muscle and adipose tissue to normal amounts of insulin secreted [4]. Conditions such as metabolic acidosis, anemia, inflammation, hyperactivity of the Renin-Angiotensin-Aldosterone System (RAAS), vitamin D deficiency, physical inactivity, excess of fat mass as well as nitrogen catabolites accumulation have all been implicated in IR in CKD subjects [5]. Notably, several clinical consequences have been linked to IR. Indeed, IR may promote endothelial dysfunction and portends increased cardiovascular mortality. Although evidence is not conclusive, some data also suggest that IR is a harbinger of CKD incidence and progression. Based on these lines of evidence, it is conceivable that IR represents a modifiable risk factor and a potential therapeutic target to improve CKD outcome [4–6].
The association between metabolic acidosis, IR and the cardiovascular risk has been documented in the scientific literature since 1924 [7]. However, in spite of the fact that correction of metabolic acidosis with nutritional therapy and/or oral administration of sodium bicarbonate in CKD is widely used [8–10], it is unknown whether correction of metabolic acidosis reduces IR and/or improves insulin effects on target cells in diabetic subjects.
We aim to evaluate whether metabolic acidosis correction by sodium bicarbonate administration may improve peripheral endogen insulin utilization by target organs in diabetic subjects with CKD treated with oral antidiabetic drugs.
Methods
For current analyses, we analyzed the first 145 subjects (83 men and 62 women) with Diabetes Mellitus type 2 not treated with insulin participating in the Use of Bicarbonate in Chronic Renal Insufficiency (UBI) study (NCT NCT01640119) with at least 1 year of follow-up. The UBI study protocol has been published previously [11]. Briefly, the UBI study is an on-going multi-center, open-label, randomized controlled study designed to test the impact of metabolic acidosis correction on CKD progression to End Stage Renal Disease (ESRD). CKD-3b-4 patients of 18 to 80 year of age, able to provide written informed consent and serum bicarbonate levels below 24 mEql/l are randomized (allocation ratio 1:1) to either oral sodium bicarbonate (treatment group) or conventional therapy for CKD (control group). Study investigators are free to adjust medications to achieve the targets for glycated hemoglobin, bone mineral metabolism, blood pressure, anemia, iron status, dyslipidemia as suggested by guidelines on CKD patients’ management available at the time of the study design [11]. The randomization process is centralized to ensure allocation concealment. Patients with evidence of neoplastic diseases, autoimmune diseases, chronic heart failure NYHA class III-IV, uncontrolled arterial hypertension, severe peripheral arterial disease (defined as limb amputation), cerebrovascular disease, neobladder or ureterosigmoidostomy, severe metabolic acidosis (defined as serum bicarbonate <18 mEq/l) or use of calcium carbonate in the 3-month prior to study inclusion are excluded from the trial. Oral sodium bicarbonate is administered at the dose of 0.5 mmol/kg of body weight (1 g of sodium bicarbonate contains 11.9 mmol – initial dose about 3–4 g) two times a day until the achievement of the desired serum bicarbonate target of 24–28 mmol/l. If a serum value of 28 mmol/l is exceeded, the administration of bicarbonate is tapered each 3 days until the desired serum target level is achieved [11].
Demographic, clinical and laboratory characteristics
Demographic and clinical characteristics were assessed as study inception. Self-reported variables included age, sex. Medical chart reviews were conducted to determine the presence of diabetes mellitus status or the use of oral antidiabetic medications, history of atherosclerotic cardiovascular disease (ASCVD) and the use of different medications. History of ASCVD was a composite measure that included myocardial infarction, angina, and peripheral and cerebrovascular disease. Blood pressure was measured after a 15 to 20 min rest, using a manual aneroid sphygmomanometer.
Routine biochemical laboratory measurements were obtained at baseline and completion 12 months of follow-up and analyzed at the facilities usual laboratories as part of the standard patients care. All blood samples were in a fasting condition. Insulin resistance was evaluated via the Homeostatic Model Assessment (HOMA) test at baseline and at completion of 12 months of follow-up.
Finally, 25-OH vitamin D was measured every 3 months; the correction of low levels was started at values lower than 20 ng/ml and stopped at values higher than 50 ng/ml.
Patients using steroids and other drugs interfering directly with glucose levels were excluded from the study.
Insulin resistance measurement and HOMA test
Insulin resistance was assessed indirectly by the Homeostatic model assessment (HOMA) index as suggested by Wallace and coworkers [12]. Briefly, the HOMA index is a mathematical model that allows to calculate insulin sensitivity (HOMA-IR) and evaluate ß pancreatic cell function (HOMA-%B) from fasting plasma glucose and insulin levels [12]. It is a simple test, appropriate to perform in large epidemiological studies that nicely correlates with experimental data obtained with direct measurement techniques such as the euglycemic clamp [13–16].
To perform the HOMA test, blood samples are drawn twice (30 min apart) in 3 consecutive days. Patients are kept at rest, in a fasting status for at least 8 h before the blood sampling. Tobacco use is forbidden for the 12 h before blood tests. The presented values for HOMA test at baseline and study completion are the mean values of the three consecutive blood samples. For HOMA-IR and HOMA-%B calculation, the following formulas are used [12]:
HOMA-IR = (FPI * FPG)/22.5;
HOMA-%B = (20 * FPI)/(FPG - 3.5)
where FPI stands for fasting plasma insulin concentration (mU/l) and FPG stands for fasting plasma glucose (mmol/l) (FPG conversion factor from mg/dl to mmol/l: 10.018).
HOMA-IR estimates of insulin resistance. Normal values are <0.25. Values greater or equal than 5.5 indicate insulin resistance typical of early stages of Diabetes Mellitus. HOMA-B% estimates ß pancreatic cells function. It’s value ranges from 0 % (no pancreatic cell function) to 100 % (all pancreatic cell functioning). FPI and FPG measurements were performed centrally at P.O. “A Landolfi” – Solofra (AV), Italy, via COBAS 6000 or COBAS C 501 (Roche Diagnostics) and IMMULITE 2000 (Siemens Healthcare Global), respectively.
Study objective and endpoint
Current analyses aim at testing the impact of metabolic acidosis correction in CKD 3b-4 diabetic patients with serum bicarbonate <24 mEq/l on insulin resistance evaluated via the Homeostatic Model Assessment (HOMA) test. The HOMA was performed at study inception and after 12 months of treatment with either oral sodium bicarbonate (treatment group) or conventional therapy for CKD (control group).
Statistical analysis
Data are reported as mean ± SD or counts (percentage) when appropriate. Un-paired T-test and Chi-square test were used to assess difference between study groups at baseline and study completion (Tables 1 and 2). The bagplot (Fig. 1) was used to describe the bivariate association of serum bicarbonate and HOMA test in subjects randomized to oral sodium bicarbonate (treated) or conventional therapy (controls) at study inception and completion. Because of the random allocation to treatment groups, the selection criterion was independent of study investigators’ beliefs (i.e., we analyzed data of the first 145 diabetic type 2 patients randomized in the UBI study who completed 1 year of follow-up) and the the optimal balance between groups at study inception, the Wilcoxon rank sum test was used to assess between- and within-group (treated vs control subjects) differences in HOMA-IR and HOMA-%B at study inception as well as completion of 12 months of follow-up (Table 3). Linear regression was used to assess the independent association of treatment and/or metabolic acidosis correction and HOMA test at study completion. First, we tested for the unadjusted association of (i) treatment allocation, (ii) serum bicarbonate values at follow-up and (iii) changes of serum bicarbonate (serum bicarbonate at follow-up – serum bicarbonate at study inception) with HOMA-IR (Table 4). Subsequently, we tested the independent contribution of metabolic acidosis correction (i.e., serum bicarbonate at study completion or changes in serum bicarbonate) vs oral bicarbonate supplementation, forcing both variables in the same regression model (Table 4). However, due to the non-linear relationship between serum bicarbonate (Fig. 2a) or changes in serum bicarbonate (Fig. 2b) and HOMA index at study completion, we tested for an interaction effect of treatment and values of serum bicarbonate at study completion or changes of serum bicarbonates (Table 4). Because of the significant effect modification of serum serum bicarbonate levels on treatment effect on HOMA test and because at visual inspection (Fig. 2a) the association between serum bicarbonate and HOMA test was different for values greater than 28 mmol/l, we performed some additional analyses by applying regression splines with a knot set at serum bicarbonate level of 28 mEq/l and tested for the independent association between serum bicarbonate, treatment and HOMA test at study completion (Table 5). All analyses were conducted as intention-to-treat. Two-tailed probability values ≤ 0.05 were considered statistically significant. Analyses were completed using R version 3.1.3 (2015-03-09) (The R Foundation for Statistical Computing).
Table 1.
Demographic, clinical, laboratory characteristics and use of oral anti-diabetic medications of patients randomized to oral sodium bicarbonate (Treated) or conventional therapy (controls) at study inception
| Overall | Treated | Control | p-value | |
|---|---|---|---|---|
| (N = 145) | (N = 71) | (N = 74) | ||
| Males, N (%) | 83 (57 %) | 47 (66 %) | 36 (48 %) | NS |
| Age, years | 65.5 ± 11.4 | 64.9 ± 11.8 | 66.0 ± 12.9 | NS |
| Body Weight, kg | 75.5 ± 14.1 | 76.5 ± 14.6 | 73.4 ± 11.2 | NS |
| Cardiovascular disease, N(%) | 36 (25) | 17 (24) | 19 (26) | NS |
| Systolic blood pressure, mmHg | 122 ± 20 | 124 ± 19 | 120 ± 22 | NS |
| Disatolic blood pressure, mmHg | 73 ± 9 | 73 ± 8 | 73 ± 10 | NS |
| Serum Bicarbonate, mEql/l | 21.4 ± 1.9 | 21.2 ± 1.9 | 21.6 ± 2.0 | NS |
| Serum Gucose, mg/dl | 150 ± 44 | 149 ± 41 | 151 ± 47 | NS |
| HbA1C % | 6.76 ± 1.2 | 6.74 ± 1.0 | 6.8 ± 1.4 | NS |
| Serum creatinine,mg/dl | 2.1 ± 0.8 | 2.3 ± 0.8 | 2.0 ± 0.7 | NS |
| BUN, mg/dl | 87 ± 32 | 93 ± 35 | 81 ± 28 | NS |
| Creatinine clearance, ml/min | 33 ± 14 | 32 ± 14 | 35 ± 15 | NS |
| Uric Acid, mg/dl | 5.4 ± 1.8 | 5.6 ± 1.9 | 5.1 ± 1.8 | NS |
| Serum sodium, mEql/l | 139 ± 3 | 139 ± 3 | 139 ± 2 | NS |
| Serum potassium, mEq/l | 4.82 ± 0.7 | 4.85 ± 0.6 | 4.79 ± 0.7 | NS |
| Total serum calcium, mg/dl | 9.13 ± 0.6 | 9.14 ± 0.62 | 9.12 ± 0.58 | NS |
| Serum phosphate, mg/dl | 3.7 ± 0.7 | 3.8 ± 0.7 | 3.7 ± 0.7 | NS |
| Serum albumin, g/dl | 3.86 ± 0.42 | 3.85 ± 0.39 | 3.89 ± 0.46 | NS |
| Hemoglobin, g/dl | 12.3 ± 1.7 | 12.26 ± 1.82 | 12.39 ± 1.68 | NS |
| C-Reactive Protein, mg/l | 11.20 ± 28.1 | 11.08 ± 34.37 | 11.34 ± 18.53 | NS |
| Serum PTH, pg/ml | 122 ± 83 | 119 ± 34 | 124 ± 88 | NS |
| Serum total cholesterol, mg/dl | 154 ± 34 | 158 ± 34 | 151 ± 33 | NS |
| Serum LDL cholesterol, mg/dl | 91 ± 32 | 93 ± 31 | 87 ± 32 | NS |
| Serum HDL cholesterol, mg/dl | 45 ± 14 | 45 ± 12 | 45 ± 16 | NS |
| Serum triglicerides, mg/dl | 134 ± 58 | 130 ± 56 | 138 ± 60 | NS |
| vitamin D (25-OH.D), ng/ml | 39 ± 11 | 39 ± 10 | 38 ± 10 | NS |
| Homa-IR | 7.17 ± 2.4 | 7.13 ± 2.5 | 7.20 ± 2.36 | NS |
| HOMA % B | 49 ± 21 | 50 ± 22 | 48 ± 21 | NS |
| Serum insulin, mcIU | 18.3 ± 6.6 | 17.6 ± 6.1 | 19.0 ± 7.0 | NS |
| Antidiabetic medications | ||||
| Biguanides, number (%) | 98 (67.5) | 52 (73.2) | 46 (62.2) | NS |
| dose, mg/day | 1740 ± 417 | 1760 ± 611 | 1725 ± 670 | NS |
| Solfonylureas, number (%) | 46 (31.7) | 17 (23.9) | 29 (39.2) | NS |
| dose, mg/day | 5.25 ± 1.19 | 5.29 ± 1.38 | 5.23 ± 1.14 | NS |
| Meglitinides, number (%) | 41 (28.3) | 21 (29.6) | 20 (27) | NS |
| dose, mg/day | 3.13 ± 1.35 | 3.52 ± 0.91 | 2.76 ± 1.59 | NS |
| Use of > 1 medication, number (%) | 37 (25.5) | 20 (28.1) | 17 (23) | NS |
| Antihypertensive DRUGS | ||||
| Furosemide, number (%) | 131 (90.3) | 62 (87.3) | 69 (93.3) | NS |
| dose, mg/day | 55 ± 19 | 55 ± 21 | 55 ± 17 | NS |
| ARB inhibitors, number (%) | 75 (51.7) | 37 (23.9) | 38 (39.2) | NS |
| ACE-Inhibitors, number (%) | 74 (51) | 38 (52.1) | 36 (48.6) | NS |
| Beta-blocker (%) | 24 (16.5) | 14 (19.7) | 10 (13.5) | NS |
| Other antihypertensive drugs number (%) | 42 (28.9) | 20 (28.2) | 22 (29.7) | NS |
| Use of > 1 medication, number (%) | 70 (48.3) | 38 (53.5) | 32 (43.2) | NS |
Continuous and dichotomous variables are expressed as mean ± standard deviation or count (%), respectively
Table 2.
Clinical, laboratory characteristics and use of anti-diabetic medications of patients randomized to oral sodium bicarbonate (Treated) or conventional therapy (controls) at study completion
| Overall | Treated | Control | p-value | |
|---|---|---|---|---|
| 145 | 71 | 74 | ||
| Body Weight, kg | 76.1 ± 12.8 | 76.3 ± 12.8 | 73.4 ± 15.0 | NS |
| Systolic blood pressure, mmHg | 123 ± 17 | 125 ± 17 | 121 ± 16 | NS |
| Disatolic blood pressure, mmHg | 74 ± 8 | 76 ± 8 | 72 ± 10 | NS |
| Serum Bicarbonate, mEql/l | 24.2 ± 2.7 | 26.0 ± 2.0 | 22.3 ± 1.9 | 0.0001 |
| Serum Gucose, mg/dl | 118 ± 29 | 110 ± 32 | 127 ± 24 | 0.0001 |
| HbA1C % | 7.2 ± 2.9 | 6.7 ± 0.9 | 7.7 ± 3.7 | 0.028 |
| Creatinine Clearance, ml/min | 30 ± 16 | 32 ± 15 | 31 ± 16 | NS |
| Homa-IR | 6.52 ± 1.8 | 6.1 ± 1.5 | 7.0 ± 2.0 | 0.003 |
| HOMA % B | 52 ± 20 | 55 ± 18 | 49 ± 21 | 0.015 |
| Serum insulin, mcIU | 16.4 ± 6.6 | 13.4 ± 5.2 | 19.9 ± 6.3 | 0.0001 |
| Antidiabetic medications | ||||
| Biguanides, number (%) | 89 (61.4) | 45 (63.3) | 44 (59.4) | NS |
| dose, mg/day | 1570 ± 517 | 1377 ± 457 | 1615 ± 550 | 0.005 |
| Solfonylureas, number (%) | 40 (27.6) | 12 (16.9) | 28 (37.8) | 0.009 |
| dose, mg/day | 5.05 ± 1.29 | 4.89 ± 1.7 | 5.20 ± 1.07 | 0.033 |
| Meglitinides, number (%) | 36 (24.8) | 16 (22.5) | 20 (27) | NS |
| dose, mg/day | 3.13 ± 1.35 | 3.52 ± 0.91 | 2.76 ± 1.59 | 0.0001 |
| Use of > 1 medication, number (%) | 28 (19.3) | 12 (16.9) | 16 (21.6) | NS |
Continuous and dichotomous variables are expressed as mean ± standard deviation or count (%), respectively
Fig. 1.

The bagplots describe the association between serum bicarbonate and HOMA test in subjects randomized to oral sodium bicarbonate (Treated) or conventional therapy (controls) at study inception and conclusion. Legend: The inner polygon (called bag) contains 50 % of all points. Observations outside the outermost polygon (called fence) are outliers. The observations between the bag and fence are marked by line segments. The asterisk symbol (*) near the center of the graph represents the bivariate median
Table 3.
HOMA-IR and HOMA-%B at study inception and conclusion in treated and control subjects
| Treated | Control | P value (between group) | |
|---|---|---|---|
| HOMA-IR | |||
| Baseline | 6.4 [5.5–7.9] | 6.4 [5.5–8.2] | 0.915 |
| Study Completion | 5.9 [5.0–7.0] | 6.3 [5.3–8.2] | 0.010 |
| P-value (within group) | 0.004 | 0.572 | |
| HOMA-%B | |||
| Baseline | 50.5 [32.0–67.2] | 43.0 [32.7–62.2] | 0.543 |
| Study Completion | 60.5 [43.5–70.2] | 45.0 [32.7–64.5] | 0.023 |
| P-value (within group) | 0.036 | 0.754 | |
Data are expressed as median [Interquartile range]. Wilcoxon rank sum test is used for between- and within-group comparisons
Table 4.
Predictor of HOMA index at study completion by unadjusted and multivariable adjusted linear regression analyses
| Predictor of HOMA index at study completion | |||
|---|---|---|---|
| Variable | B-coef | Standard Error | P value |
| Unadjusted | |||
| - Treatment (yes vs no) | −0.8740 | 0.3285 | 0.0087 |
| Unadjusted | |||
| - Change in serum bicarbonate (%) | −1.5833 | 0.9462 | 0.0964 |
| Unadjusted | |||
| - Serum bicarbonate at study completion (mmol/l) | −0.14511 | 0.06026 | 0.0173 |
| Adjusted for treatment, change in serum bicarbonate and interaction of change in serum bicarbonate*treatment | |||
| - Treatment (yes vs no) | −1.4604 | 0.5015 | 0.00418 |
| - Change in serum bicarbonate (%) | −3.0382 | 1.8007 | 0.09378 |
| - Interaction test (change in serum bicarbonate*treatment) | 4.9948 | 2.3578 | 0.03591 |
| Adjusted for treatment, serum bicarbonate at follow-up and interaction of serum bicarbonate at followup*treatment | |||
| - Treatment (yes vs no) | −11.6700 | 4.4255 | 0.00931 |
| - Serum bicarbonate at follow-up (mmol/l) | −0.2328 | 0.1106 | 0.03713 |
| - Interaction test (serum bicarbonate at follow-up*treatment) | 0.4476 | 0.1784 | 0.01325 |
*interaction between factors
Fig. 2.
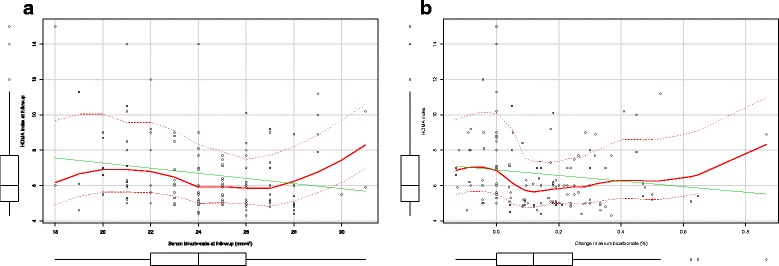
The scatterplots represent the relationship between serum bicarbonate (a) and changes in serum bicarbonate (b) and HOMA index at study completion. Legend: solid green line represents the linear regression line; solid red line represents the smoothed linear regression line
Table 5.
Predictor of HOMA index at study completion by unadjusted and multivariable adjusted spline regression analyses
| Predictor of HOMA index at study completion (further elaborations) | |||
|---|---|---|---|
| Variable | B-coef | Standard Error | P value |
| Unadjusted | |||
| - Serum bicarbonate <28 mmol/l at follow-up | −4.6008 | 1.1804 | 0.00015 |
| - Serum bicarbonate ≥28 mmol/l at follow-up | 1.9360 | 1.0270 | 0.06146 |
| Adjusted for treatment, serum bicarbonate greater/equal or lower than 28 mmol/l | |||
| - Treatment (yes vs no) | −0.3482 | 0.4757 | 0.4654 |
| - Serum bicarbonate <28 mmol/l at follow-up | −3.6980 | 1.7085 | 0.0321 |
| - Serum bicarbonate ≥28 mmol/l at follow-up | 2.2055 | 1.0926 | 0.0454 |
Serum bicarbonate is used as a continuous variable and divided according to ≥ 28 mmol/l (knot). The HOMA-serum bicarbonate levels relationship changes for values of serum bicarbonate greater equal than 28 mmol/l
Results
A total of 145 (57 % men) diabetic type 2, middle-age (65.5 ± 11.4 years) patients on oral antidiabetic medication were included in current analyses. At study inception, no significant differences in anthropometric, clinical and laboratory characteristics between subjects allocated to oral sodium bicarbonate or conventional therapy were observed (Table 1). In particular, treated subjects and controls exhibited similar renal function (mean creatinine clearance: 32 ± 14 ml/min and 35 ± 15 ml/min), serum bicarbonate levels (21.2 ± 1.9 mmol/l and 21.6 ± 2.0 mmol/l), fasting plasma glucose levels (149 ± 41 mg/dl and 151 ± 47 mg/dl), glycated hemoglobin (6.74 ± 1.0 % and 6.80 ± 1.4 %) as well as serum insulin levels (17.6 ± 6.1 mcIU and 19.0 ± 7.0 mcIU) (Table 1). Overall, basal HOMA-IR was 7.17 ± 2.4 and no difference between study groups was noted (median [Interquartile range (IQR)]: 6.4[5.5–7.9] and 6.4[5.5–8.2]; in the bicarbonate and control group, respectively). Of interest, only 4 (5,6 %) and 6 (8.1 %) subjects in the bicarbonate and control group had a HOMA-IR <5. Finally, at baseline HOMA-%B was also comparable between study groups (median [IQR]: 50.5 % [32.0–67.2 %] and 43 % [32.7–62.2 %]; in the bicarbonate and control group, respectively) (Table 1).
Table 1 shows patients’ antidiabetic and antihypertensive drugs. Moreover, Table 1 shows 25-OH vitamin D: the two groups did not show statistically significant differences of vitamin D blood levels (39 ± 10 versus 38 ± 10 ng/ml, in treated versus control, respectively)
Mean dose of oral bicarbonate administered was 0.7 ± 0.2 mmol/kg per each patient. At study inception there were no differences between the two groups in the use of oral antidiabetic drugs regarding number of pills, doses, and type of drugs (Table 1). No adverse affects were registered during oral bicarbonate administration.
At study completion, while no differences in renal function and blood pressure control were observed, a significant impact of oral sodium bicarbonate supplementation on serum bicarbonate levels (26.0 ± 2.0 vs 22.3 ± 1.9 mEq/l, in treated and control subjects, respectively) as well as diabetes control and management was apparent (Table 2). Specifically, HOMA-IR decreased in treated (p for within group comparison: 0.004) but not control subjects (p for within group comparison: 0.57) (median [IQR]: 5.9 [5.0–7.0] and 6.3 [5.3–8.2]; p for between groups comparison:0.01) (Fig. 1, Table 3). Similarly, HOMA-%B increased (p for within group comparison: 0.036) in the experimental group (p for within group comparison: 0.754) from a median [IQR] value of 50.5 % [32.0 – 67.2 %] to 60.5 % [43.5 – 70.2 %] while it was unchanged in the control group (median[IQR]: 43.0 [32.7 – 62.2] vs 45 [32.7 – 64.5] for baseline and follow-up, respectively; p value for between comparison at follow-up: 0.023) (Fig. 1, Table 3).
As documented in Fig. 2a and b, serum bicarbonate levels or changes were not linearly associated with insulin resistance. Improvement of serum levels of bicarbonate was associated with HOMA improvement only if metabolic acidosis over-correction (i.e., serum levels of bicarbonate greater than 28 mEq/l) did not occur. Indeed, a significant effect reduction (interaction test for treatement*serum levels of bicarbonate: p = 0.013) of oral bicarbonate supplementation on HOMA index occurred as serum bicarbonate rose (Table 4). To explore whether the effect on insulin resistance was due to the oral bicarbonate administration per se or metabolic acidosis amelioration, we performed splines regression analyses to account for the change in the relationship between serum bicarbonate levels and HOMA index according to metabolic acidosis correction (i.e., below or greater/equal than 28 mEq/l). As reported in Table 5, the benefit associated with metabolic acidosis correction disappeared when serum bicarbonate exceeded 28 mEq/l. Notably, when treatment allocation and serum levels of bicarbonate achieved were both forced into the spline regression model, treatment allocation lost statistical significance (p = 0.465) (Table 5), suggesting that metabolic acidosis correction rather than oral bicarbonate supplementation improves insulin resistance (Table 5).
Discussion
Current findings suggest that metabolic acidosis is linked to insulin resistance in diabetic, Chronic Kidney Disease (CKD) patients and oral bicarbonate administration may correct metabolic acidosis that, in turn, improves insulin sensitivity in this population.
Insulin resistance (or reduced insulin sensitivity) is characterized by suboptimal biological responses of the liver, skeletal muscle and adipose tissue to normal amounts of insulin secreted [4, 5, 17–19]. Several biological processes such as glucose, lipid or protein metabolism as well as single hormonal effects such as glycogen synthesis or glucose oxidation may be affected in this condition [20, 21]. Several factors may contribute to insulin resistance in CKD. Visceral adipose tissue, diet, low physical activity, cigarette smoking, drugs (glucocorticosteroids, thiazide-like diuretics, beta-blockers) may all contribute to insulin resistance [22–24]. However, few lines of evidence also suggest that metabolic acidosis, that commonly complicates CKD, is implicated in suboptimal biological responses to insulin [6, 25].
Hence, metabolic acidosis represents a modifiable risk factor for insulin resistance and an attainable therapeutic target in CKD [4]. Indeed, metabolic acidosis may exert some detrimental effects at the cellular level inducing for example an intra-extracellular shift of cations and in different tissues such as bones and muscles as well as affect nutrition and metabolism [3, 6]. As part of CKD patients’ care, alkali such as sodium bicarbonate administration and/or low protein diet or diet rich in fruit and vegetables are commonly prescribed to avoid or correct metabolic acidosis. Preliminary evidence suggests that metabolic acidosis amelioration may attenuate CKD progression as well as hard outcome [17, 26–28].
Our results confirm and expand previous efforts [25, 29, 30] suggesting that metabolic acidosis correction by sodium bicarbonate administration improves insulin resistance without affecting the overall blood pressure control (Table 2). This is likely due to the better response to insulin of target organs (as suggested by the improvement of both HOMA-IR and HOMA-%B). In contrast with previous experiences [25, 29, 30], Ikizler and coworkers [31] recently failed to demonstrate an association between metabolic acidosis and insulin resistance in a cross-sectional, observational study of 42 patients with CKD stage 3–5. According to these findings, a reduced acid burden improved metabolic acidosis but not insulin sensitivity, measured via the hyperinsulinemic euglycemic clamp method [31]. Although we estimated rather than measured insulin resistance, our results suggest that, at least in diabetic CKD patients, over-correction of metabolic acidosis may also be detrimental since values of serum bicarbonate greater than 28 mEq/l are associated with decreased insulin sensitivity (Fig. 2). While Ikizler and coworkers [31] define metabolic acidosis as a dichotomous variable (i.e., serum bicarbonate level <22 mEq/l), we prospectively explored the association of serum bicarbonate as a continuous variable and insulin resistance over a broad range of values of serum bicarbonate (i.e., from 18 to 31 mEq/l). Current findings suggest that this association is non-linear (Fig. 2) and insulin sensitivity decreases for values of serum bicarbonate below 24 mEq/l and above 28 mEq/l. Of interest, accounting for the non-linear nature of the association also suggest that bicarbonate levels rather than sodium bicarbonate per se, is responsible for the effect on the HOMA index (Table 5).
In patients of treatment group assuming Biguanides (45 subjects), bicarbonate administration was higher (not significant) compared to other oral antidiabetic drugs (0.79 ± 0.4 mmol/kg).
Although further work is needed to validate these results in diabetic as well as non-diabetic CKD patients, the clinical relevance of these findings should be evaluated in light of the prevalence of insulin resistance and its associated complications such as hyperinsulinemia, hyperglycemia and hypertriglyceridemia [32]; the widespread use of sodium bicarbonate or alkali supplementation, low protein or vegetarian diet for CKD care [17, 33–40] as well as the safety and relative inexpensiveness of the treatment tested. Aside of confirming the link of bicarbonate and insulin resistance, current results also provide with some guidance for CKD patient care.
Our analyses suffer of a few limitations worth noting. We investigated the relationship of insulin sensitivity and metabolic acidosis in a subgroup of patients (diabetic patients on oral antidiabetic medications) randomized into the Use of Bicarbonate in Chronic Renal Insufficiency (UBI) study (NCT NCT01640119). This study aims at testing the impact of alkali administration and acidosis correction in diabetic and non-diabetic CKD patients on renal function decline. Although we analyzed a subgroup of patients, the analyses were carried out in the first 145 consecutive diabetic patients who completed at least 1 year of follow-up. This selection criterion as well as the random assignment to treatment at study inception are independent of the investigators’ beliefs and influences and we can argue that current findings are similar to a randomized clinical trial (RCT). The well balance of demographic, clinical and laboratory characteristics between groups, further corroborates this point. No power assumption or sample size calculation was performed in light of the exploratory nature of these analyses and the lack of similar data in this domain. Insulin resistance is calculated rather than measured. However, the HOMA test is widely accepted as a reliable and reproducible tool to assess insulin sensitivity in clinical and epidemiological studies [12–16, 41, 42].
Conclusions
In conclusion, current results corroborate the notion that metabolic acidosis promotes insulin resistance and shed some light on the impact of sodium bicarbonate administration in CKD diabetic patients. Although further validation is mandatory, it seems that serum bicarbonate levels rather than the treatment used is relevant to restore insulin sensitivity. Finally, acidosis overcorrection (i.e., serum bicarbonate levels >28 mEq/l) should be avoided since, as metabolic acidosis, is associated with insulin resistance.
Acknowledgements
Authors are indebted to doctors and administrative staff for who assist the Use of Bicarbonate in Chronic Renal Insufficiency (UBI) study conduct. List of investigators: Simona Adesso (Fisciano), Filippo Aucella (S. Giovanni Rotondo), Annamaria Bruzzese (Messina), Giuseppe Conte (Napoli), Adamasco Cupisti (Pisa), Antonella De Blasio (Solofra), Alfonso Frallicciardi (Solofra), Rachele Grifa (San Giovanni Rotondo), Rosa Martino (Solofra), Matteo Piemontese (San Giovanni Rotondo), Maria Luisa Sirico (Solofra), Giuseppe Struzziero (Solofra), Raffaele Tortoriello (Solofra), Fabio Vitale (Ariano Irpino). Authors thank the Italian Society of Nephrology (SIN) for the unrestricted research grant provided.
Funding
all costs connected to the Use of Bicarbonate in Chronic Renal Insufficiency (UBI) study were covered by the Italian National Health Care System and by an unrestricted research grant provided by the Italian Society of Nephrology (SIN).
Availability of data and materials
To comply with the current Italian regulation for sensitive personal data protection, the dataset on which the conclusions of the manuscript rely cannot be either deposited in publicly available repositories or presented in the main paper or additional supporting files. The authors remain at disposal for any additional enquire.
Authors’ contributions
AB performed the statistical analysis; he has been involved in drafting and revising the manuscript. LDM has been involved in drafting the manuscript and revising it. DS has made substantial contributions to acquisition of data, and interpretation of data. SM has made substantial contributions to acquisition of data, and interpretation of data. EDS has made substantial contributions to acquisition of data, and interpretation of data. MC has made substantial contributions to interpretation of data. LDL has made substantial contributions to interpretation of data. PG has made substantial contributions to acquisition of data, and interpretation of data. BDI conceived the study, and participated in its design and coordination. He has made substantial contributions to acquisition of data, interpretation of data and he has been involved in drafting and revising the manuscript. FA has made substantial contribution to acquisition of data. All Authors have given final approval of the version to be published.
Competing interests
Authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The study protocol was approved by the Comitato Etico Campania Nord and each participating site provided institutional Ethical Review Board (information available from editor upon reasonable request). Participants provided written informed consent at study entry. Study procedures were conducted in adherence to the Declaration of Helsinki, Ethical Principles for Medical Research Involving Human Subjects.
Abbreviations
- ASCVD
Atherosclerotic cardiovascular disease
- CKD
Chronic kidney disease
- DM2
Diabetic type 2 patients
- ESRD
End stage renal disease
- HOMA
Homeostatic model assessment
- HOMA-%B
ß pancreatic cell function calculate by Homa test
- HOMA-IR
Calculate insulin resistence by Homa test
- IR
Insulin resistance
- MA
Metabolic acidosis
- NYHA
New York Heart Association
- RAAS
Renin-Angiotensin-Aldosterone System
- UBI
Use of bicarbonate in chronic renal insufficiency
Contributor Information
Antonio Bellasi, Email: antoniobellasi@gmail.com.
Lucia Di Micco, Email: luciadimicco@gmail.com.
Domenico Santoro, Email: santisi@hotmail.com.
Stefania Marzocco, Email: smarzocco@unisa.it.
Mario Cozzolino, Email: mario.cozzolino@unimi.it.
Luca Di Lullo, Email: dilulloluca69@gmail.com.
Pasquale Guastaferro, Email: pasqualeguastaferro@libero.it.
Biagio Di Iorio, Email: br.diiorio@gmail.com.
on behalf of UBI study investigators:
Simona Adesso, Annamaria Bruzzese, Giuseppe Conte, Adamasco Cupisti, Antonella De Blasio, Alfonso Frallicciardi, Rachele Grifa, Rosa Martino, Matteo Piemontese, Maria Luisa Sirico, Giuseppe Struzziero, Raffaele Tortoriello, and Fabio Vitale
References
- 1.Collaborators GBDRF, Forouzanfar MH, Alexander L, Anderson HR, Bachman VF, Biryukov S, Brauer M, Burnett R, Casey D, Coates MM, et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386(10010):2287–323. doi: 10.1016/S0140-6736(15)00128-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.DALYs GBD, Collaborators H. Murray CJ, Barber RM, Foreman KJ, Abbasoglu Ozgoren A, Abd-Allah F, Abera SF, Aboyans V, Abraham JP, et al. Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990–2013: quantifying the epidemiological transition. Lancet. 2015;386(10009):2145–91. doi: 10.1016/S0140-6736(15)61340-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Simon EE, Hamm LL. A basic approach to CKD. Kidney Int. 2010;77(7):567–9. doi: 10.1038/ki.2009.516. [DOI] [PubMed] [Google Scholar]
- 4.Teta D. Insulin resistance as a therapeutic target for chronic kidney disease. J Ren Nutr. 2015;25(2):226–9. doi: 10.1053/j.jrn.2014.10.019. [DOI] [PubMed] [Google Scholar]
- 5.Garibotto G, Sofia A, Russo R, Paoletti E, Bonanni A, Parodi EL, Viazzi F, Verzola D. Insulin sensitivity of muscle protein metabolism is altered in patients with chronic kidney disease and metabolic acidosis. Kidney Int. 2015;88(6):1419–26. doi: 10.1038/ki.2015.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thomas SS, Zhang L, Mitch WE. Molecular mechanisms of insulin resistance in chronic kidney disease. Kidney Int. 2015;88(6):1233–9. doi: 10.1038/ki.2015.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Souto G, Donapetry C, Calvino J, Adeva MM. Metabolic acidosis-induced insulin resistance and cardiovascular risk. Metab Syndr Relat Disord. 2011;9(4):247–53. doi: 10.1089/met.2010.0108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goraya N, Simoni J, Jo CH, Wesson DE. Treatment of metabolic acidosis in patients with stage 3 chronic kidney disease with fruits and vegetables or oral bicarbonate reduces urine angiotensinogen and preserves glomerular filtration rate. Kidney Int. 2014;86(5):1031–8. doi: 10.1038/ki.2014.83. [DOI] [PubMed] [Google Scholar]
- 9.Loniewski I, Wesson DE. Bicarbonate therapy for prevention of chronic kidney disease progression. Kidney Int. 2014;85(3):529–35. doi: 10.1038/ki.2013.401. [DOI] [PubMed] [Google Scholar]
- 10.Goraya N, Simoni J, Jo CH, Wesson DE. A comparison of treating metabolic acidosis in CKD stage 4 hypertensive kidney disease with fruits and vegetables or sodium bicarbonate. Clin J Am Soc Nephrol. 2013;8(3):371–81. doi: 10.2215/CJN.02430312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Di Iorio B, Aucella F, Conte G, Cupisti A, Santoro D. A prospective, multicenter, randomized, controlled study: the correction of metabolic acidosis with use of bicarbonate in Chronic Renal Insufficiency (UBI) Study. J Nephrol. 2012;25(3):437–40. doi: 10.5301/jn.5000014. [DOI] [PubMed] [Google Scholar]
- 12.Wallace TM, Levy JC, Matthews DR. Use and abuse of HOMA modeling. Diabetes Care. 2004;27(6):1487–95. doi: 10.2337/diacare.27.6.1487. [DOI] [PubMed] [Google Scholar]
- 13.Emoto M, Nishizawa Y, Maekawa K, Hiura Y, Kanda H, Kawagishi T, Shoji T, Okuno Y, Morii H. Homeostasis model assessment as a clinical index of insulin resistance in type 2 diabetic patients treated with sulfonylureas. Diabetes Care. 1999;22(5):818–22. doi: 10.2337/diacare.22.5.818. [DOI] [PubMed] [Google Scholar]
- 14.Stumvoll M, Mitrakou A, Pimenta W, Jenssen T, Yki-Jarvinen H, Van Haeften T, Renn W, Gerich J. Use of the oral glucose tolerance test to assess insulin release and insulin sensitivity. Diabetes Care. 2000;23(3):295–301. doi: 10.2337/diacare.23.3.295. [DOI] [PubMed] [Google Scholar]
- 15.Bonora E, Targher G, Alberiche M, Bonadonna RC, Saggiani F, Zenere MB, Monauni T, Muggeo M. Homeostasis model assessment closely mirrors the glucose clamp technique in the assessment of insulin sensitivity: studies in subjects with various degrees of glucose tolerance and insulin sensitivity. Diabetes Care. 2000;23(1):57–63. doi: 10.2337/diacare.23.1.57. [DOI] [PubMed] [Google Scholar]
- 16.Katsuki A, Sumida Y, Gabazza EC, Murashima S, Furuta M, Araki-Sasaki R, Hori Y, Yano Y, Adachi Y. Homeostasis model assessment is a reliable indicator of insulin resistance during follow-up of patients with type 2 diabetes. Diabetes Care. 2001;24(2):362–5. doi: 10.2337/diacare.24.2.362. [DOI] [PubMed] [Google Scholar]
- 17.de Brito-Ashurst I, Varagunam M, Raftery MJ, Yaqoob MM. Bicarbonate supplementation slows progression of CKD and improves nutritional status. J Am Soc Nephrol. 2009;20(9):2075–84. doi: 10.1681/ASN.2008111205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tessari P, Cecchet D, Cosma A, Puricelli L, Millioni R, Vedovato M, Tiengo A. Insulin resistance of amino acid and protein metabolism in type 2 diabetes. Clin Nutr. 2011;30(3):267–72. doi: 10.1016/j.clnu.2011.02.009. [DOI] [PubMed] [Google Scholar]
- 19.Louard RJ, Fryburg DA, Gelfand RA, Barrett EJ. Insulin sensitivity of protein and glucose metabolism in human forearm skeletal muscle. J Clin Invest. 1992;90(6):2348–54. doi: 10.1172/JCI116124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ballmer PE, McNurlan MA, Hulter HN, Anderson SE, Garlick PJ, Krapf R. Chronic metabolic acidosis decreases albumin synthesis and induces negative nitrogen balance in humans. J Clin Invest. 1995;95(1):39–45. doi: 10.1172/JCI117668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Adabimohazab R, Garfinkel A, Milam EC, Frosch O, Mangone A, Convit A. Does inflammation mediate the association between obesity and insulin resistance? Inflammation. 2016;39(3):994–1003. doi: 10.1007/s10753-016-0329-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liao MT, Sung CC, Hung KC, Wu CC, Lo L, Lu KC. Insulin resistance in patients with chronic kidney disease. J Biomed Biotechnol. 2012;2012:691369. doi: 10.1155/2012/691369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Koppe L, Pelletier CC, Alix PM, Kalbacher E, Fouque D, Soulage CO, Guebre-Egziabher F. Insulin resistance in chronic kidney disease: new lessons from experimental models. Nephrol Dial Transplant. 2014;29(9):1666–74. doi: 10.1093/ndt/gft435. [DOI] [PubMed] [Google Scholar]
- 24.de Boer IH, Zelnick L, Afkarian M, Ayers E, Curtin L, Himmelfarb J, Ikizler TA, Kahn SE, Kestenbaum B, Utzschneider K. Impaired glucose and insulin homeostasis in moderate-severe CKD. J Am Soc Nephrol. 2016. [DOI] [PMC free article] [PubMed]
- 25.Mandel EI, Curhan GC, Hu FB, Taylor EN. Plasma bicarbonate and risk of type 2 diabetes mellitus. CMAJ. 2012;184(13):E719–25. doi: 10.1503/cmaj.120438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rebholz CM, Coresh J, Grams ME, Steffen LM, Anderson CA, Appel LJ, Crews DC. Dietary acid load and incident chronic kidney disease: results from the ARIC study. Am J Nephrol. 2015;42(6):427–35. doi: 10.1159/000443746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kraut JA, Madias NE. Metabolic acidosis of CKD: an update. Am J Kidney Dis. 2016;67(2):307–17. doi: 10.1053/j.ajkd.2015.08.028. [DOI] [PubMed] [Google Scholar]
- 28.Raphael KL. Approach to the treatment of chronic metabolic acidosis in CKD. Am J Kidney Dis. 2016;67(4):696–702. doi: 10.1053/j.ajkd.2015.12.016. [DOI] [PubMed] [Google Scholar]
- 29.Farwell WR, Taylor EN. Serum bicarbonate, anion gap and insulin resistance in the National Health and Nutrition Examination Survey. Diabet Med. 2008;25(7):798–804. doi: 10.1111/j.1464-5491.2008.02471.x. [DOI] [PubMed] [Google Scholar]
- 30.Kobayashi S, Maesato K, Moriya H, Ohtake T, Ikeda T. Insulin resistance in patients with chronic kidney disease. Am J Kidney Dis. 2005;45(2):275–80. doi: 10.1053/j.ajkd.2004.09.034. [DOI] [PubMed] [Google Scholar]
- 31.Ikizler HO, Zelnick L, Ruzinski J, Curtin L, Utzschneider KM, Kestenbaum B, Himmelfarb J, de Boer IH. Dietary acid load is associated with serum bicarbonate but not insulin sensitivity in chronic kidney disease. J Ren Nutr. 2016;26(2):93–102. doi: 10.1053/j.jrn.2015.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Leyking S, Fliser D. Insulin resistance in CKD. Clin J Am Soc Nephrol. 2014;9(4):638–40. doi: 10.2215/CJN.01290214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shah SN, Abramowitz M, Hostetter TH, Melamed ML. Serum bicarbonate levels and the progression of kidney disease: a cohort study. Am J Kidney Dis. 2009;54(2):270–7. doi: 10.1053/j.ajkd.2009.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mahajan A, Simoni J, Sheather SJ, Broglio KR, Rajab MH, Wesson DE. Daily oral sodium bicarbonate preserves glomerular filtration rate by slowing its decline in early hypertensive nephropathy. Kidney Int. 2010;78(3):303–9. doi: 10.1038/ki.2010.129. [DOI] [PubMed] [Google Scholar]
- 35.Raphael KL, Wei G, Baird BC, Greene T, Beddhu S. Higher serum bicarbonate levels within the normal range are associated with better survival and renal outcomes in African Americans. Kidney Int. 2011;79(3):356–62. doi: 10.1038/ki.2010.388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Banerjee T, Crews DC, Wesson DE, Tilea A, Saran R, Rios Burrows N, Williams DE, Powe NR, Centers for Disease C, Prevention Chronic Kidney Disease Surveillance T Dietary acid load and chronic kidney disease among adults in the United States. BMC Nephrol. 2014;15:137. doi: 10.1186/1471-2369-15-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Scialla JJ, Appel LJ, Astor BC, Miller ER, 3rd, Beddhu S, Woodward M, Parekh RS, Anderson CA, African American Study of Kidney D, Hypertension Study G Net endogenous acid production is associated with a faster decline in GFR in African Americans. Kidney Int. 2012;82(1):106–12. doi: 10.1038/ki.2012.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Scialla JJ, Anderson CA. Dietary acid load: a novel nutritional target in chronic kidney disease? Adv Chronic Kidney Dis. 2013;20(2):141–9. doi: 10.1053/j.ackd.2012.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chauveau P, Combe C, Fouque D, Aparicio M. Vegetarianism: advantages and drawbacks in patients with chronic kidney diseases. J Ren Nutr. 2013;23(6):399–405. doi: 10.1053/j.jrn.2013.08.004. [DOI] [PubMed] [Google Scholar]
- 40.Scialla JJ, Appel LJ, Wolf M, Yang W, Zhang X, Sozio SM, Miller ER, 3rd, Bazzano LA, Cuevas M, Glenn MJ, et al. Plant protein intake is associated with fibroblast growth factor 23 and serum bicarbonate levels in patients with chronic kidney disease: the Chronic Renal Insufficiency Cohort study. J Ren Nutr. 2012;22(4):379–88. doi: 10.1053/j.jrn.2012.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Garcia-Estevez DA, Araujo-Vilar D, Fiestras-Janeiro G, Saavedra-Gonzalez A, Cabezas-Cerrato J. Comparison of several insulin sensitivity indices derived from basal plasma insulin and glucose levels with minimal model indices. Horm Metab Res. 2003;35(1):13–7. doi: 10.1055/s-2003-38385. [DOI] [PubMed] [Google Scholar]
- 42.Hermans MP, Levy JC, Morris RJ, Turner RC. Comparison of insulin sensitivity tests across a range of glucose tolerance from normal to diabetes. Diabetologia. 1999;42(6):678–87. doi: 10.1007/s001250051215. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
To comply with the current Italian regulation for sensitive personal data protection, the dataset on which the conclusions of the manuscript rely cannot be either deposited in publicly available repositories or presented in the main paper or additional supporting files. The authors remain at disposal for any additional enquire.


