Abstract
Background
Telehealth has been defined as the remote delivery of healthcare services using information and communication technology. Where resource-limited health systems face challenges caused by the increasing burden of chronic diseases and an aging global population, telehealth has been advocated as a solution for changing and improving the paradigm of healthcare delivery to cope with these issues. The aim of this systematic review is to investigate the effect of telehealth interventions on two indicators: hospitalization rate and length of stay.
Materials and Methods
The reviewers searched the PubMed, ScienceDirect, and Springer electronic databases from January 2005 to November 2013. A search strategy was developed using a combination of the following search keywords: impact, effect, telehealth, telemedicine, telecare, hospitalization, length of stay, and resource utilization. Both randomized controlled trials and observational studies were included in the review. To be included in the review, articles had to be written in English. The results of study were compiled, reviewed, and analyzed on the basis of the review aims.
Results
This systematic review examined 22 existing studies with a total population of 19,086 patients. The effect of telehealth on all-cause hospitalization was statistically significant in 40 percent of the related studies, whereas it was not statistically significant in 60 percent. Similarly, the effect of telehealth on the all-cause length of stay was statistically significant in 36 percent of the studies and nonsignificant in 64 percent.
Conclusion
Considering the fact that hospitalization rate and length of stay can be confounded by factors other than telehealth intervention, studies examining the effect of the intervention on these indicators must take into account all other factors influencing them. Otherwise any judgment on the effect of telehealth on these indicators cannot be valid.
Keywords: telehealth, telemedicine, impact, length of stay, hospital admission
Introduction
Telehealth has been defined as the remote delivery of healthcare services using information and communication technology.1 The term is broader than telemedicine and covers a variety of physician and nonphysician services.2 The wide availability of the Internet accompanied by the increasing pace of technological advances has provided new opportunities for telehealth.3
Where resource limited-health systems face challenges caused by an increasing burden of chronic diseases and the aging global population,4, 5 telehealth has been advocated as a solution for changing and improving the current paradigm of healthcare delivery to cope with these issues.6, 7 However, its opponents continue to criticize it.8, 9, 10, 11, 12
Several systematic reviews have investigated the effects of various telehealth interventions on aspects of healthcare and healthcare delivery, and they have infrequently found consistent results of those interventions.13, 14, 15, 16, 17, 18, 19 Few systematic reviews of the effects of telehealth interventions on hospital indicators have been conducted. These reviews have been restricted to populations of patients with particular types of diseases, or they have investigated particular effects of telehealth, for instance the socioeconomic effect, and have reported that the positive effects of telehealth on those aspects could not be generalized beyond those particular studies.20, 21 To the best of our knowledge, no systematic review has been conducted to explore the effect of telehealth interventions on hospital indicators among different types of patients regardless of disease type.
In this analysis, studies of the effect of telehealth interventions on two main hospital indicators were reviewed. The outcome of the studies reviewed could be positive, negative, or neutral. Therefore, conflicting results are to be expected. This article presents the reported evidence on the effect of telehealth and the characteristics of those reports. The intention of this article is not to assess or pass judgment on the value of telehealth.
Methodology
Criteria for Considering Studies for the Review
Both randomized controlled trials and observational studies were included in the review. Systematic reviews or other types of studies were excluded. All forms of telehealth interventions ranging from telephone to two-way videoconferencing (either asynchronous or real-time technologies) were included in this review. In the studies, patients receiving any type of telehealth interventions were compared with those receiving usual face-to-face care. No limitation was set for the participants or the country of the study.
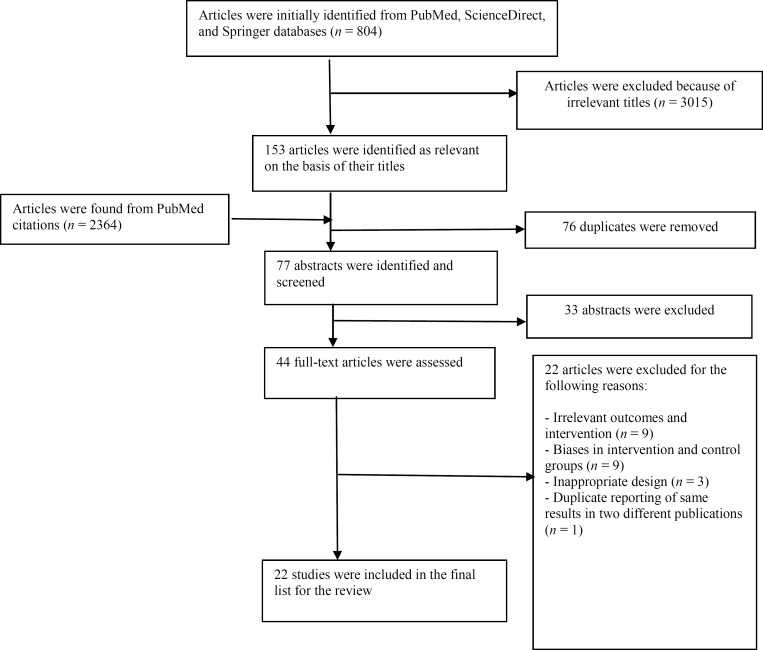
Studies were included if they reported objective measures of hospitalization or length of stay. Studies in which outcomes were related to any institution other than hospital, such as home care facilities or correctional facilities, were excluded from this review. Papers had to be written in English to be included. Articles with any bias toward possible influencing effects on the outcomes were also excluded. For instance, if the severity of disease differed between the intervention group and the control group in a study, the study was excluded. Figure 1 illustrates the process of selecting studies for the detailed review.
Figure 1.
Flowchart Representing the Selection of Studies for the Systematic Review of the Effects of Telehealth on Hospitalization Indicators
Search Methods for Identification of Studies
The reviewers searched the PubMed, ScienceDirect, and Springer electronic databases for articles published from January 2005 to November 2013. A search strategy was developed using a combination of the following keywords: impact, effect, telehealth, telemedicine, telecare, hospitalization, length of stay, and resource utilization.
Data Extraction
Eligible papers were reviewed independently by the reviewers using a data extraction form that was developed for the purpose of this review and contained the following data elements:
Name of the author
Year of publication
Size of population in both the intervention and control groups
The country in which the study took place
Title of the study
Design type of the study
Devices used for the telehealth intervention
The specified aim of the telehealth intervention
The type of intervention (i.e., real-time vs. asynchronous)
Participants’ type of illness
Indicators on hospitalization rate or length of stay
The statistical significance of the effect of the telehealth intervention on each of the indicators
In the process of the review and the data extraction, any disagreement among the investigators was resolved utilizing team discussion to achieve consensus.
Assessing Risk of Bias
The quality of studies was assessed using a mixed-method assessment tool. Depending on the study design, a range of criteria were used to assess the risk of bias. Criteria considered for assessing the studies included the following:
A clear description of randomization
Allocation concealment or blinding
Completeness of outcome data
Quality of outcome reporting
Sampling and sample justification
Control of confounding factors
Results
Basic Characteristics of the Studies
A summary of the basic characteristics of all 22 studies included in the review is provided in Table 1. As can be seen, 14 of the 22 studies were randomized controlled trials, and 8 studies used an observational method design. The age of the population in all studies ranged from 55 to 77 years except for one that was conducted on a population of infants. The purpose of the telehealth interventions in the studies included the following:
Monitoring
Education
Supporting
Measuring
Managing
Consultation
Table 1.
Characteristics of Studies Included in the Systematic Review Examining the Effects of Telehealth on Hospitalization Indicators
| Study Authors | Country | Type of Study | Mean Participant Age in Years | Type of Disease | Purpose of Intervention | Type of Outcome |
|---|---|---|---|---|---|---|
| Wakefield et al.a | United States | RCT | 69 | HF | To support patients after discharge | H, LOS |
| Morguet et al.b | Germany | Obs | 61 | HF | To educate and monitor patients’ body weight, blood pressure, and pulse rate daily | H, LOS |
| Scherr et al.c | Austria | RCT | 66 | HF | To measure patients’ vital parameters (blood pressure, heart rate, body weight) and send them to the monitoring center | H, LOS |
| Dinesen et al.d | Denmark | RCT | 68 | COPD | To assess the patient's data, monitor the patient's disease, and provide advice to the patient | H |
| Bowles et al.e | United States | RCT | 75 | DB, HF | To support patient care; to monitor and instruct patients on self-care and disease management | H |
| Steventon et al.f | England | Obs | 66 | CHD, DB, HF, COPD | To ask patients about current health status and encourage patients to better manage their health conditions | H, LOS |
| Dang et al.g | United States | Obs | 72 | DB, HF, COPD | To monitor and exchange disease-related information between patients and caregivers | H, LOS |
| Steventon et al.h | England | RCT | 70 | DB, HF, COPD | To monitor and educate patients | H, LOS |
| Soran et al.i | United States | RCT | 76 | HF | To monitor and detect early signs and symptoms of heart failure | H, LOS |
| Ferrante et al.j | Argentina | RCT | 65 | HF | To improve patients’ diet and treatment, promote exercise, and regularly monitor symptoms, weight, and edema | H |
| Jia et al.k | United States | Obs | 68 | DB | To answer questions about patients’ symptoms and monitor daily information | H |
| Chen et al.l | Taiwan | Obs | 63 | HF | To educate and communicate (two-way) with patients on diet therapy, fluid restriction, and adverse drug effects | H, LOS |
| Weintraub et al.m | United States | RCT | 69 | HF | To assess variables important to patient care management | H, LOS |
| Steventon et al.n | England | RCT | 75 | SCN | To monitor functions, security and environments of patients | H, LOS |
| Giordano et al.o | Italy | RCT | 57 | HF | To telemonitor and tele-assist | H |
| Webb et al.p | United States | Obs | 0.67 | CoHD | To send echocardiography studies from the community hospital to the tertiary hospital to be interpreted | LOS |
| Dendale et al.q | Belgium | RCT | 76 | HF | To measure body weight, blood pressure, and heart rate and send them to the central computer | H |
| Domingo et al.r | Spain | Obs | 66 | HF | To record weight, heart rate, and blood pressure and send them to the healthcare staff supporting patients via a dedicated web application | H, LOS |
| Schofield et al.s | United States | Obs | 67 | HF | To report and update patient symptoms and vital signs | H, LOS |
| Koehler et al.t | Germany | RCT | 67 | HF | To do daily self-assessment of blood pressure, body weight, and electrocardiography and send the results to the central server | H, LOS |
| Cleland et al.u |
|
RCT | 67 | HF | To assess patients’ symptoms and medication; to measure weight, blood pressure, heart rate, and heart rhythm and communicate the information | LOS |
| Dansky et al.v | United States | RCT | 77 | HF | To take measurements of blood pressure, pulse, weight; to allow two-way, synchronous interaction between nurse and patient | H |
Abbreviations: DB, diabetes; CHD, coronary heart disease; CoHD, congenital heart disease; COPD, chronic obstructive pulmonary disease; H, hospitalization; HF, heart failure; LOS, length of stay; Obs, observational; RCT, randomized controlled trial; SCN, social care needs. Note: All studies in this table had usual care as the control.
Wakefield, B., M. Ward, et al. “Evaluation of Home Telehealth Following Hospitalization for Heart Failure: A Randomized Trial.” Telemedicine and e-Health 14, no. 8 (2008): 753–61.
Morguet, A., P. Kühnelt, et al. “Impact of Telemedical Care and Monitoring on Morbidity in Mild to Moderate Chronic Heart Failure.” Cardiology 111, no. 2 (2008): 134–39.
Scherr, D., P. Kastner, et al. “Effect of Home-based Telemonitoring Using Mobile Phone Technology on the Outcome of Heart Failure Patients after an Episode of Acute Decompensation: Randomized Controlled Trial.” Journal of Medical Internet Research 11, no. 3 (2009): e34.
Dinesen, B., L. Haesum, et al. “Using Preventive Home Monitoring to Reduce Hospital Admission Rates and Reduce Costs: A Case Study of Telehealth among Chronic Obstructive Pulmonary Disease Patients.” Journal of Telemedicine and Telecare 18, no. 4 (2012): 221–25.
Bowles, K., D. Holland, and D. A. Horowitz. “A Comparison of In-person Home Care, Home Care with Telephone Contact and Home Care with Telemonitoring for Disease Management.” Journal of Telemedicine and Telecare 15, no. 7 (2009): 344–50.
Steventon, A., S. Tunkel, et al. “Effect of Telephone Health Coaching (Birmingham OwnHealth) on Hospital Use and Associated Costs: Cohort Study with Matched Controls.” British Medical Journal 347 (2013): f4585.
Dang, S., F. Ma, et al. “Differential Resource Utilization Benefits with Internet-based Care Coordination in Elderly Veterans with Chronic Diseases Associated with High Resource Utilization.” Telemedicine and e-Health 12, no. 1 (2006): 14–23.
Steventon, A., M. Bardsley, et al. “Effect of Telehealth on Use of Secondary Care and Mortality: Findings from the Whole System Demonstrator Cluster Randomised Trial.” British Medical Journal 344 (2012): e3874.
Soran, O., I. Pina, et al. “A Randomized Clinical Trial of the Clinical Effects of Enhanced Heart Failure Monitoring Using a Computer-based Telephonic Monitoring System in Older Minorities and Women.” Journal of Cardiac Failure 14, no. 9 (2008): 711–17.
Ferrante, D., S. Varini, et al. “Long-Term Results after a Telephone Intervention in Chronic Heart Failure: DIAL (Randomized Trial of Phone Intervention in Chronic Heart Failure) Follow-up.” Journal of the American College of Cardiology 56, no. 5 (2010): 372–78.
Jia, H., H. Feng, et al. “A Longitudinal Study of Health Service Utilization for Diabetes Patients in a Care Coordination Home-Telehealth Programme.” Journal of Telemedicine and Telecare 17, no. 3 (2011): 123–26.
Chen, Y., Y. Ho, et al. “Assessment of the Clinical Outcomes and Cost-effectiveness of the Management of Systolic Heart Failure in Chinese Patients Using a Home-based Intervention.” Journal of International Medical Research 38, no. 1 (2010): 242–52.
Weintraub, A., D. Gregory, et al. “A Multicenter Randomized Controlled Evaluation of Automated Home Monitoring and Telephonic Disease Management in Patients Recently Hospitalized for Congestive Heart Failure: The SPAN-CHF II Trial.” Journal of Cardiac Failure 16, no. 4 (2010): 285–92.
Steventon, A., M. Bardsley, et al. “Effect of Telecare on Use of Health and Social Care Services: Findings from the Whole Systems Demonstrator Cluster Randomised Trial.” Age and Ageing 42, no. 4 (2013): 501–8.
Giordano, A., S. Scalvini, et al. “Multicenter Randomised Trial on Home-based Telemanagement to Prevent Hospital Readmission of Patients with Chronic Heart Failure.” International Journal of Cardiology 131, no. 2 (2009): 192–99.
Webb, C., C. Waugh, et al. “Impact of Telemedicine on Hospital Transport, Length of Stay, and Medical Outcomes in Infants with Suspected Heart Disease: A Multicenter Study.” Journal of the American Society of Echocardiography 26 no. 9 (2013): 1090–98.
Dendale, P., G. De Keulenaer, et al. “Effect of a Telemonitoring-facilitated Collaboration between General Practitioner and Heart Failure Clinic on Mortality and Rehospitalization Rates in Severe Heart Failure: The TEMA-HF 1 (TElemonitoring in the MAnagement of Heart Failure) Study.” European Journal of Heart Failure 14, no. 3 (2012): 333–40.
Domingo, M., J. Lupon, et al. “Noninvasive Remote Telemonitoring for Ambulatory Patients with Heart Failure: Effect on Number of Hospitalizations, Days in Hospital, and Quality of Life. CARME (CAtalan Remote Management Evaluation) Study.” Revista Espanola de Cardiologia 64, no. 4 (2011): 277–85.
Schofield, R., S. Kline, et al. “Early Outcomes of a Care Coordination-enhanced Telehome Care Program for Elderly Veterans with Chronic Heart Failure.” Telemedicine and e-Health 11, no. 1 (2005): 20–27.
Koehler, F., S. Winkler, et al. “Impact of Remote Telemedical Management on Mortality and Hospitalizations in Ambulatory Patients with Chronic Heart Failure: The Telemedical Interventional Monitoring in Heart Failure Study.” Circulation 123, no. 17 (2011): 1873–80.
Cleland, J., A. Louis, et al. “Noninvasive Home Telemonitoring for Patients with Heart Failure at High Risk of Recurrent Admission and Death: The Trans-European Network–Home-Care Management System (TEN-HMS) Study.” Journal of the American College of Cardiology 45, no. 10 (2005): 1654–64.
Dansky, K., J. Vasey, and K. Bowles. “Impact of Telehealth on Clinical Outcomes in Patients with Heart Failure.” Clinical Nursing Research 17, no. 3 (2008): 182–99.
Table 2 illustrates the different devices that were employed to perform the interventions. These include:
Telephones
Mobile phones
Television sets (used as monitors)
Computerized Internet-based devices
Automated self-monitoring devices
Telemeasuring devices
Video cameras
Personal digital assistants
Wireless Bluetooth devices
Table 2.
Summarization of the Effects of Telehealth on Hospitalization Indicators in Studies Included in the Systematic Review
| Study Authors | Intervention Device (Modality) | Sample Size | Follow-up in Months | Statistically Significant Outcomes | |
|---|---|---|---|---|---|
| Hospitalization | Length of Stay | ||||
| Wakefield et al.a |
|
|
12 | Intervention 3: all-cause, SD | None |
| Morguet et al.b | Telephone and the telemonitoring equipment (R) |
|
11 | All-cause, SD Other noncardiac reasons, SD | All-cause, SD Other cardiac reasons, SD |
| Scherr et al.c | Weight scale, sphygmomanometer, mobile phone, and client-server communication through Internet (A) |
|
6 | None | Heart failure, SD |
| Dinesen et al.d | Telehealth monitor system using wireless technology (A, R) |
|
10 | All-cause, SD | None |
| Bowles et al.e |
|
|
2 | None | None |
| Steventon et al.f | Telephone (R) | Intervention: 2,698 Control: 2,698 | 12 | None | None |
| Dang et al.g | Computerized, Internet-based, and in-home messaging and monitoring device for automating the daily monitoring of the enrolled patients by a care coordinator (A) | Congestive heart failure 17, control 17 | Heart failure, SD | None | |
| Chronic obstructive pulmonary disease 17, control 17 | None | None | |||
| Diabetes mellitus 23, control 23 | None | None | |||
| Steventon et al.h | Remote, automatic, and passive monitoring system in addition to peripheral devices including a pulse oximeter, a glucometer, and weighing scales (A) | Intervention: 1,570 Control: 1,584 | 12 | All-cause, SD | All-cause, SD |
| Soran et al.i | Electronic scale and an individualized symptom response system linked via standard phone line to a computerized database (A) |
|
6 | None | None |
| Ferrante et al.j | Telephone (R) |
|
12–48 | Heart failure, SD | None |
| Jia et al.k | Home telehealth device (messaging device) and telephone (R) |
|
48 | None | None |
| Chen et al.l | Telephone (R) |
|
6 | All-cause, SD Heart failure, SD | All-cause, SD Heart failure, SD |
| Weintraub et al.m | Tele-measurement devices and an interactive communication device (A) |
|
3 | None | None |
| Steventon et al.m | Tele-care base unit along with a pendant alarm and up to 27 various peripheral devices (R) |
|
12 | None | None |
| Giordano et al.n | Portable measurement devices transferring data by a fixed or mobile telephone; one lead trace to a receiving station where health professional was available (A) |
|
12 | All-cause, SD Heart failure, SD | None |
| Webb et al.o | Interactive system along with store and forward system (A) |
|
36 | None | All-cause, SD |
| Dendale et al.p | Electronic weight scale, a blood pressure monitoring device along with a cell-phone, central computer (A) |
|
6 | None | None |
| Domingo et al.q | Interactive platform, automated self-monitoring equipment, Internet connection, and television used as monitor (A) |
|
12 | Heart failure, SD Other cardiac reasons, SD | Heart failure, SD Other cardiac reasons, SD |
| Schofield et al.r | In-home messaging device, a secure Internet site, and telephone (A) |
|
6 | All-cause, SD | All-cause, SD |
| Koehler et al.s | Portable measuring devices connected to a personal digital assistant for transferring information via cell phone to telemedicine centers (A) |
|
26 | None | None |
| Cleland et al.t |
|
|
8 | None | None |
| Dansky et al.u | Tele-home-care system: telephone-based communication system with medical peripherals (A, R) |
|
2, 4 | At 2 months: SD (not significant at 4 months) | None |
Abbreviations: A, asynchronous; R, real-time; SD, significant decrease.
vDansky, K., J. Vasey, and K. Bowles. “Impact of Telehealth on Clinical Outcomes in Patients with Heart Failure.” Clinical Nursing Research 17, no. 3 (2008): 182–99.
Wakefield, B., M. Ward, et al. “Evaluation of Home Telehealth Following Hospitalization for Heart Failure: A Randomized Trial.” Telemedicine and e-Health 14, no. 8 (2008): 753–61.
Morguet, A., P. Kühnelt, et al. “Impact of Telemedical Care and Monitoring on Morbidity in Mild to Moderate Chronic Heart Failure.” Cardiology 111, no. 2 (2008): 134–39.
Scherr, D., P. Kastner, et al. “Effect of Home-based Telemonitoring Using Mobile Phone Technology on the Outcome of Heart Failure Patients after an Episode of Acute Decompensation: Randomized Controlled Trial.” Journal of Medical Internet Research 11, no. 3 (2009): e34.
Dinesen, B., L. Haesum, et al. “Using Preventive Home Monitoring to Reduce Hospital Admission Rates and Reduce Costs: A Case Study of Telehealth among Chronic Obstructive Pulmonary Disease Patients.” Journal of Telemedicine and Telecare 18, no. 4 (2012): 221–25.
Bowles, K., D. Holland, and D. A. Horowitz. “A Comparison of In-person Home Care, Home Care with Telephone Contact and Home Care with Telemonitoring for Disease Management.” Journal of Telemedicine and Telecare 15, no. 7 (2009): 344–50.
Steventon, A., S. Tunkel, et al. “Effect of Telephone Health Coaching (Birmingham OwnHealth) on Hospital Use and Associated Costs: Cohort Study with Matched Controls.” British Medical Journal 347 (2013): f4585.
Dang, S., F. Ma, et al. “Differential Resource Utilization Benefits with Internet-based Care Coordination in Elderly Veterans with Chronic Diseases Associated with High Resource Utilization.” Telemedicine and e-Health 12, no. 1 (2006): 14–23.
Steventon, A., M. Bardsley, et al. “Effect of Telehealth on Use of Secondary Care and Mortality: Findings from the Whole System Demonstrator Cluster Randomised Trial.” British Medical Journal 344 (2012): e3874.
Soran, O., I. Pina, et al. “A Randomized Clinical Trial of the Clinical Effects of Enhanced Heart Failure Monitoring Using a Computer-based Telephonic Monitoring System in Older Minorities and Women.” Journal of Cardiac Failure 14, no. 9 (2008): 711–17.
Ferrante, D., S. Varini, et al. “Long-Term Results after a Telephone Intervention in Chronic Heart Failure: DIAL (Randomized Trial of Phone Intervention in Chronic Heart Failure) Follow-up.” Journal of the American College of Cardiology 56, no. 5 (2010): 372–78.
Jia, H., H. Feng, et al. “A Longitudinal Study of Health Service Utilization for Diabetes Patients in a Care Coordination Home-Telehealth Programme.” Journal of Telemedicine and Telecare 17, no. 3 (2011): 123–26.
Chen, Y., Y. Ho, et al. “Assessment of the Clinical Outcomes and Cost-effectiveness of the Management of Systolic Heart Failure in Chinese Patients Using a Home-based Intervention.” Journal of International Medical Research 38, no. 1 (2010): 242–52.
Weintraub, A., D. Gregory, et al. “A Multicenter Randomized Controlled Evaluation of Automated Home Monitoring and Telephonic Disease Management in Patients Recently Hospitalized for Congestive Heart Failure: The SPAN-CHF II Trial.” Journal of Cardiac Failure 16, no. 4 (2010): 285–92.
Steventon, A., M. Bardsley, et al. “Effect of Telecare on Use of Health and Social Care Services: Findings from the Whole Systems Demonstrator Cluster Randomised Trial.” Age and Ageing 42, no. 4 (2013): 501–8.
Giordano, A., S. Scalvini, et al. “Multicenter Randomised Trial on Home-based Telemanagement to Prevent Hospital Readmission of Patients with Chronic Heart Failure.” International Journal of Cardiology 131, no. 2 (2009): 192–99.
Webb, C., C. Waugh, et al. “Impact of Telemedicine on Hospital Transport, Length of Stay, and Medical Outcomes in Infants with Suspected Heart Disease: A Multicenter Study.” Journal of the American Society of Echocardiography 26 no. 9 (2013): 1090–98.
Dendale, P., G. De Keulenaer, et al. “Effect of a Telemonitoring-facilitated Collaboration between General Practitioner and Heart Failure Clinic on Mortality and Rehospitalization Rates in Severe Heart Failure: The TEMA-HF 1 (TElemonitoring in the MAnagement of Heart Failure) Study.” European Journal of Heart Failure 14, no. 3 (2012): 333–40.
Domingo, M., J. Lupon, et al. “Noninvasive Remote Telemonitoring for Ambulatory Patients with Heart Failure: Effect on Number of Hospitalizations, Days in Hospital, and Quality of Life. CARME (CAtalan Remote Management Evaluation) Study.” Revista Espanola de Cardiologia 64, no. 4 (2011): 277–85.
Schofield, R., S. Kline, et al. “Early Outcomes of a Care Coordination-enhanced Telehome Care Program for Elderly Veterans with Chronic Heart Failure.” Telemedicine and e-Health 11, no. 1 (2005): 20–27.
Koehler, F., S. Winkler, et al. “Impact of Remote Telemedical Management on Mortality and Hospitalizations in Ambulatory Patients with Chronic Heart Failure: The Telemedical Interventional Monitoring in Heart Failure Study.” Circulation 123, no. 17 (2011): 1873–80.
Cleland, J., A. Louis, et al. “Noninvasive Home Telemonitoring for Patients with Heart Failure at High Risk of Recurrent Admission and Death: The Trans-European Network–Home-Care Management System (TEN-HMS) Study.” Journal of the American College of Cardiology 45, no. 10 (2005): 1654–64.
In the randomized controlled trials, the follow-up duration for measuring the outcomes ranged from 2 to 26 months, whereas in the observational studies the follow-up duration ranged from 6 to 48 months.
Effect of Telehealth on Hospitalization and Length of Stay
The effect of telehealth on hospitalization and length of stay was categorized on the basis of the reason for admission including all-cause, heart failure, other cardiac conditions, and other noncardiac reasons (see Table 2).22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43
The effect of telehealth on all-cause hospitalization was statistically significant (significant decrease) in 40 percent of the studies that reported hospitalization outcomes, whereas it was not statistically significant in 60 percent of those studies. Similarly, the effect of telehealth on all-cause length of stay was statistically significant (significant decrease) in 36 percent of the studies that reported a length-of-stay outcome, and it was not significant in 64 percent of those studies.
Discussion
This systematic review included 22 existing studies with a total population of 19,086 patients. The basic characteristics of the studies are discussed first, and then more detail regarding the effects of telehealth on hospitalization rate and length of stay is provided.
Age and Diseases in the Population
Although telehealth can be utilized to provide services for different age groups,44 the average age of the population in the included studies was found to be high (i.e., older) in this review. This finding can be attributed to the fact that most previous studies had been conducted on participants with chronic conditions, and about 75 percent of the elderly have at least one chronic disease and 50 percent have at least two chronic conditions.45 The total population in the studies had chronic conditions, which may be a consequence of the realization that patients with chronic conditions impose heavy financial pressures on healthcare systems46 and that these conditions can be managed less expensively and more effectively by using telehealth interventions. The cost savings and increased effectiveness therefore justify the focus of telehealth programs on chronic conditions.47
Moreover, a growing body of evidence supports the use of telehealth as an effective solution for the management and care of chronic conditions.48 The chronic diseases for which telehealth intervention was applied in the studies are diabetes, heart failure, coronary heart disease, chronic obstructive pulmonary diseases, and congenital heart disease, and one study examined social care needs; this range of conditions is similar to the spectrum of diseases found in a study conducted on UK telehealth systems.49
Type of the Studies
More observational studies reported significant effects than randomized controlled trials did. This finding is consistent with those of the systematic review conducted by Louis et al.50 and the results reported by Chaudhry et al., 51 in which no significant effect was found in randomized controlled trial studies in contrast with observational studies. Other reports support this finding.52, 53
Devices Used for the Telehealth Intervention
Different devices from various vendors were used for the telehealth interventions in the included studies. This pattern was consistent with the equipment listed in a study describing the model of information exchange in UK telehealth systems.54 The devices with the highest range of usage were telemonitoring tools; this basic required measurement and communication equipment was ubiquitous. This finding is in accordance with the results of a systematic review emphasizing telemonitoring as a promising patient management mechanism in chronic diseases.55 Telemonitoring has also been referred to as one of the common applications of information technology in the management of chronic diseases56 and as a facilitating technology in care management of chronic conditions.57 The telephone was the device with the second highest usage in the studies. This device was used not only for direct communication between healthcare providers and patients but also as a key component of telemonitoring equipment for transferring remote monitoring data. The prevalent usage of the telephone could be due to its wide availability, high level of acceptability to the majority of the population, and ease of use.
Type of Telehealth Modality
The modality of the technology used for interventions was asynchronous in most of the studies,58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68 as was the case in a systematic review conducted on teleconsultations for diabetes care.69 This finding may be due to the fact that implementation of real-time telehealth interventions can be much more expensive than implementation of asynchronous ones.70, 71 However, different results have been reported regarding the outcomes of interventions using these two modalities. Although one study reported low clinical efficacy of the asynchronous modality compared to real-time interventions, other studies documented no difference in the outcomes of these two modalities.72, 73
Studies of interventions using a hybrid modality (both real-time and asynchronous) were a minority among the included studies. No considerable difference could be observed between the real-time and asynchronous modality interventions in terms of their effects on the hospital indicators that are the subject of this review. The same trend was reported in the systematic review conducted on teleconsultation for diabetes care.74
Country and Place of the Intervention
Not a single study included in this review originated in developing countries. This finding is similar to the results of a systematic review on the use of telehealth in Asian countries, in which no study was found to have been conducted on telehealth interventions in Asia.75 Most of the studies in this review originated in the United States. This finding is in line with existing evidence reported on telehealth trends76, 77 and can be attributed to the substantial investment made by the US federal government in telemedicine networks, technologies, and research.78 In addition, no study was found to have been conducted on rural populations or in medically underserved communities despite the fact that telehealth intervention can provide opportunities to increase individuals’ contact with healthcare services in those types of areas and communities.
Effect of the Intervention on the Hospital Indicators
This systematic review reveals conflicting effects of the telehealth interventions on hospitalization rates in different studies. About 60 percent of the interventions reported no significant effect on the hospitalization rate, and a significant decrease was observed in only 40 percent of the interventions. Although these findings are consistent with the findings of different reviews reporting the weak effect of telehealth on some aspects of healthcare and healthcare delivery,79, 80, 81, 82, 83, 84 they are contrary to other evidence reporting the positive effect of telehealth in different domains of healthcare.85, 86, 87, 88, 89
In terms of the effect of telehealth on length of stay, no significant effect was reported in 64 percent of the studies, and a significant decrease was observed in 36 percent of the studies.
In this review, the telehealth interventions aimed at the education of patients were found to significantly decrease both the hospitalization rate and the length of stay,90, 91, 92 and existing evidence supports this result.93 A study of the effect of electronic education on metabolic control indicators of diabetes confirms the positive effect of tele-education,94 which can be considered to have a transforming effect on patients’ behavior and thereby lead to better self-care management. In fact, patient education is a key element of self-management in chronic disease95 because it enhances patients’ ability to manage their own diseases,96 and it has been discussed in literature as a critical factor for realizing patient-centered care.97, 98 Of course, healthcare professionals’ own attitudes toward the benefit of telehealth is an important factor that influences the ultimate effectiveness of patient education and must not be ignored.99
The mixed outcomes observed in the studies can be attributed to the fact that an independent initiative rather than an integrated telehealth approach was used in each of the studies, and considerable differences exist among telehealth programs and devices in terms of their quality, reliability, and interoperability.100 This variability may influence the intervention outcome, as has been highlighted in the literature.101 In addition, no standard guideline or integrated framework has been established for implementation and evaluation of telehealth programs,102 making their outcomes more difficult to compare. Moreover, the duration of the intervention and its effect on patients’ familiarity with the technology103 may also influence the outcome of telehealth interventions.
Possible Effects of Factors Other Than Telehealth
Differences observed in outcomes of telehealth interventions might be a consequence of various factors on which no information was provided in the included studies. Among these factors are the contextual conditions of a telehealth implementation that can influence the outcome.104 It is important to bear in mind that neither technology nor patients act identically in all situations and contexts.105
Outcomes may also vary with the socioeconomic status of patients.106, 107, 108, 109 In some reports, longer length of stay has been attributed to the lack of family support and a significant distance between the hospital and the patient's home.110, 111 Individual patients’ social problems have also been identified as predictors of hospitalization,112 but despite such evidence, this factor has been ignored in most of the existing telehealth studies.113
Differences observed in the effects of telehealth can also be the result of differences in a patient's personal perception of the intervention; this perception affects the acceptability of the intervention,114 and as a result, patients may be more inclined to use one particular type of telehealth intervention rather than other available types.115 More importantly, the quality of the partnership between patients and care providers can also play a significant role in optimizing the potential of telehealth.116
Variation in the severity of illness on admission, the day of admission, and patient comorbidities have also been reported to be important factors influencing length of stay.117, 118, 119 These same factors can influence patient discharge status, the quality of care in a previous hospital stay can influence the likelihood of future patient hospitalization, and the existing hospital bed occupancy rate can also have an effect on length of stay.120, 121, 122
Conclusion
Investigation of the effect of telehealth interventions should not be conducted in a vacuum. Considering the fact that hospitalization and length of stay can be confounded by factors other than telehealth intervention, any study examining the effect of telehealth interventions on these two indicators must be designed to take into account other factors that influence their effectiveness; otherwise, any judgment on the effect of telehealth based on these indicators will not be valid. The conflicting effects observed in telehealth studies could arise from factors other than the intervention itself.
Acknowledgments
The authors would like to thank Dr. Parvin Sarbakhsh for her help.
Contributor Information
Leila R. Kalankesh, Medical informatics and health information technology in School of Management and Medical Informatics and researcher at Tabriz Health Services Management Research Center in Tabriz, Iran.
Faramarz Pourasghar, Medical informatics in School of Management and Medical Informatics at the Tabriz University of Medical Sciences in Tabriz, Iran.
Lorraine Nicholson, IFHIMA (2007-2010), Independent HIM Consultant, Rochdale OL11 2XE, Lancashire, UK.
Shamim Ahmadi, Health information technology at Iran University of Medical Sciences in Tehran, Iran.
Mohsen Hosseini, Health information technology at the School of Management and Medical Informatics at Tabriz University of Medical Sciences in Tabriz, Iran.
Notes
- 1.Higgins C., Dunn E., Conrath D. Telemedicine: An Historical Perspective. Telecommunications Policy. 1984;8(4):307–313. [Google Scholar]
- 2.Weinstein R., Lopez A., et al. Telemedicine, Telehealth, and Mobile Health Applications That Work: Opportunities and Barriers. American Journal of Medicine. 2014;127(3):183–187. doi: 10.1016/j.amjmed.2013.09.032. [DOI] [PubMed] [Google Scholar]
- 3.Fong B., Fong A., Li C. Telemedicine Technologies: Information Technologies in Medicine and Telehealth. Chichester, UK: Wiley; 2011. [Google Scholar]
- 4.Wootton R., Patil N., et al., editors. Telehealth in the Developing World. London, England: Royal Society of Medicine Press; 2009. [Google Scholar]
- 5.Naughton C., Bennett K., Feely J. Prevalence of Chronic Disease in the Elderly Based on a National Pharmacy Claims Database. Age and Aging. 2006;35(6):633–636. doi: 10.1093/ageing/afl106. [DOI] [PubMed] [Google Scholar]
- 6.Chanda K., Shaw J. The Development of Telehealth as a Strategy to Improve Health Care Services in Zambia. Health Information and Libraries Journal. 2010;27(2):133–139. doi: 10.1111/j.1471-1842.2010.00876.x. [DOI] [PubMed] [Google Scholar]
- 7.Roine R., Ohinmaa A., Hailey D. Assessing Telemedicine: A Systematic Review of the Literature. Canadian Medical Association Journal. 2001;165(6):765–771. [PMC free article] [PubMed] [Google Scholar]
- 8.Lovejoy T., Demireva P., et al. Advancing the Practice of Online Psychotherapy: An Application of Rogers’ Diffusion of Innovations Theory. Psychotherapy. 2009;46(1):112–124. doi: 10.1037/a0015153. [DOI] [PubMed] [Google Scholar]
- 9.Klecun-Dabrowska E. Telehealth in the UK: A Critical Perspective. Electronic Journal of Business Research Methods. 2003;2(1):37–46. [Google Scholar]
- 10.May C., Mort M., et al. Evaluation of New Technologies in Health Care Systems: What's the Context? Health Informatics Journal. 2000;6(2):67–70. [Google Scholar]
- 11.Mair F., Whitten P. Systematic Review of Studies of Patient Satisfaction with Telemedicine. British Medical Journal. 2000;320:1517–1520. doi: 10.1136/bmj.320.7248.1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Steele R. Telemedicine in Greenland: The Case for and against Implementation. International Journal of Circumpolar Health. 1998;57(suppl. 1):686–668. [PubMed] [Google Scholar]
- 13.Baron J., McBain H., Newman S. The Impact of Mobile Monitoring Technologies on Glycosylated Hemoglobin in Diabetes: A Systematic Review. Journal of Diabetes Science and Technology. 2010;6(6):1185–1196. doi: 10.1177/193229681200600524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cox N., Alison J., et al. Telehealth in Cystic Fibrosis: A Systematic Review. Journal of Telemedicine and Telecare. 2012;18(2):72–78. doi: 10.1258/jtt.2011.110705. [DOI] [PubMed] [Google Scholar]
- 15.Kowalczyk M., Jara A., Skarmeta A. Home Telehealth Interventions for People with Asthma. Sixth International Conference on Innovative Mobile and Internet Services in Ubiquitous Computing (IMIS 2012) 2012:907–911. [Google Scholar]
- 16.Ekeland A., Bowes A., Flottorp S. Effectiveness of Telemedicine: A Systematic Review of Reviews. International Journal of Medical Informatics. 2010;79(11):736–771. doi: 10.1016/j.ijmedinf.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 17.Wade V., Karnon J., et al. A Systematic Review of Economic Analyses of Telehealth Services Using Real Time Video Communication. BMC Health Services Research. 2010;10(233) doi: 10.1186/1472-6963-10-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huang V., Reich K., Fedorak R.N. Distance Management of Inflammatory Bowel Disease: Systematic Review and Meta-analysis. World Journal of Gastroenterology. 2014;20(3):829–842. doi: 10.3748/wjg.v20.i3.829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Polisena J., Tran K., et al. Home Telemonitoring for Congestive Heart Failure: A Systematic Review and Meta-analysis. Journal of Telemedicine and Telecare. 2010;16(2):68–76. doi: 10.1258/jtt.2009.090406. [DOI] [PubMed] [Google Scholar]
- 20.Polisena J., Tran K., et al. Home Telehealth for Chronic Obstructive Pulmonary Disease: A Systematic Review and Meta-analysis. Journal of Telemedicine and Telecare. 2010;16(3):120–127. doi: 10.1258/jtt.2009.090812. [DOI] [PubMed] [Google Scholar]
- 21.Jennet P., Scott R, et al. Socio-economic Impact of Telehealth: Evidence Now for Health Care in the Future. University of Calgary; 2003.
- 22.Wakefield B., Ward M., et al. Evaluation of Home Telehealth Following Hospitalization for Heart Failure: A Randomized Trial. Telemedicine and e-Health. 2008;14(8):753–761. doi: 10.1089/tmj.2007.0131. [DOI] [PubMed] [Google Scholar]
- 23.Morguet A., Kühnelt P., et al. Impact of Telemedical Care and Monitoring on Morbidity in Mild to Moderate Chronic Heart Failure. Cardiology. 2008;111(2):134–139. doi: 10.1159/000119701. [DOI] [PubMed] [Google Scholar]
- 24.Scherr D., Kastner P., et al. Effect of Home-based Telemonitoring Using Mobile Phone Technology on the Outcome of Heart Failure Patients after an Episode of Acute Decompensation: Randomized Controlled Trial. Journal of Medical Internet Research. 2009;11(3):e34. doi: 10.2196/jmir.1252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dinesen B., Haesum L., et al. Using Preventive Home Monitoring to Reduce Hospital Admission Rates and Reduce Costs: A Case Study of Telehealth among Chronic Obstructive Pulmonary Disease Patients. Journal of Telemedicine and Telecare. 2012;18(4):221–225. doi: 10.1258/jtt.2012.110704. [DOI] [PubMed] [Google Scholar]
- 26.Bowles K., Holland D., Horowitz D.A. A Comparison of In-person Home Care, Home Care with Telephone Contact and Home Care with Telemonitoring for Disease Management. Journal of Telemedicine and Telecare. 2009;15(7):344–350. doi: 10.1258/jtt.2009.090118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Steventon A., Tunkel S., et al. Effect of Telephone Health Coaching (Birmingham OwnHealth) on Hospital Use and Associated Costs: Cohort Study with Matched Controls. British Medical Journal. 2013;347:f4585. doi: 10.1136/bmj.f4585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dang S., Ma F., et al. Differential Resource Utilization Benefits with Internet-based Care Coordination in Elderly Veterans with Chronic Diseases Associated with High Resource Utilization. Telemedicine and e-Health. 2006;12(1):14–23. doi: 10.1089/tmj.2006.12.14. [DOI] [PubMed] [Google Scholar]
- 29.Steventon A., Bardsley M., et al. Effect of Telehealth on Use of Secondary Care and Mortality: Findings from the Whole System Demonstrator Cluster Randomised Trial. British Medical Journal. 2012;344:e3874. doi: 10.1136/bmj.e3874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Soran O., Pina I., et al. A Randomized Clinical Trial of the Clinical Effects of Enhanced Heart Failure Monitoring Using a Computer-based Telephonic Monitoring System in Older Minorities and Women. Journal of Cardiac Failure. 2008;14(9):711–717. doi: 10.1016/j.cardfail.2008.06.448. [DOI] [PubMed] [Google Scholar]
- 31.Ferrante D., Varini S., et al. Long-Term Results after a Telephone Intervention in Chronic Heart Failure: DIAL (Randomized Trial of Phone Intervention in Chronic Heart Failure) Follow-up. Journal of the American College of Cardiology. 2010;56(5):372–378. doi: 10.1016/j.jacc.2010.03.049. [DOI] [PubMed] [Google Scholar]
- 32.Jia H., Feng H., et al. A Longitudinal Study of Health Service Utilization for Diabetes Patients in a Care Coordination Home-Telehealth Programme. Journal of Telemedicine and Telecare. 2011;17(3):123–126. doi: 10.1258/jtt.2010.100314. [DOI] [PubMed] [Google Scholar]
- 33.Chen Y., Ho Y., et al. Assessment of the Clinical Outcomes and Cost-effectiveness of the Management of Systolic Heart Failure in Chinese Patients Using a Home-based Intervention. Journal of International Medical Research. 2010;38(1):242–252. doi: 10.1177/147323001003800129. [DOI] [PubMed] [Google Scholar]
- 34.Weintraub A., Gregory D., et al. A Multicenter Randomized Controlled Evaluation of Automated Home Monitoring and Telephonic Disease Management in Patients Recently Hospitalized for Congestive Heart Failure: The SPAN-CHF II Trial. Journal of Cardiac Failure. 2010;16(4):285–292. doi: 10.1016/j.cardfail.2009.12.012. [DOI] [PubMed] [Google Scholar]
- 35.Steventon A., Bardsley M., et al. Effect of Telecare on Use of Health and Social Care Services: Findings from the Whole Systems Demonstrator Cluster Randomised Trial. Age and Ageing. 2013;42(4):501–508. doi: 10.1093/ageing/aft008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Giordano A., Scalvini S., et al. Multicenter Randomised Trial on Home-based Telemanagement to Prevent Hospital Readmission of Patients with Chronic Heart Failure. International Journal of Cardiology. 2009;131(2):192–199. doi: 10.1016/j.ijcard.2007.10.027. [DOI] [PubMed] [Google Scholar]
- 37.Webb C., Waugh C., et al. Impact of Telemedicine on Hospital Transport, Length of Stay, and Medical Outcomes in Infants with Suspected Heart Disease: A Multicenter Study. Journal of the American Society of Echocardiography. 2013;26(9):1090–1098. doi: 10.1016/j.echo.2013.05.018. [DOI] [PubMed] [Google Scholar]
- 38.Dendale P., De Keulenaer G., et al. Effect of a Telemonitoring-facilitated Collaboration between General Practitioner and Heart Failure Clinic on Mortality and Rehospitalization Rates in Severe Heart Failure: The TEMA-HF 1 (TElemonitoring in the MAnagement of Heart Failure) Study. European Journal of Heart Failure. 2012;14(3):333–340. doi: 10.1093/eurjhf/hfr144. [DOI] [PubMed] [Google Scholar]
- 39.Domingo M., Lupon J., et al. Noninvasive Remote Telemonitoring for Ambulatory Patients with Heart Failure: Effect on Number of Hospitalizations, Days in Hospital, and Quality of Life. CARME (CAtalan Remote Management Evaluation) Study. Revista Espanola de Cardiologia. 2011;64(4):277–285. doi: 10.1016/j.recesp.2010.10.032. [DOI] [PubMed] [Google Scholar]
- 40.Schofield R., Kline S., et al. Early Outcomes of a Care Coordination-enhanced Telehome Care Program for Elderly Veterans with Chronic Heart Failure. Telemedicine and e-Health. 2005;11(1):20–27. doi: 10.1089/tmj.2005.11.20. [DOI] [PubMed] [Google Scholar]
- 41.Koehler F., Winkler S., et al. Impact of Remote Telemedical Management on Mortality and Hospitalizations in Ambulatory Patients with Chronic Heart Failure: The Telemedical Interventional Monitoring in Heart Failure Study. Circulation. 2011;123(17):1873–1880. doi: 10.1161/CIRCULATIONAHA.111.018473. [DOI] [PubMed] [Google Scholar]
- 42.Cleland J., Louis A., et al. Noninvasive Home Telemonitoring for Patients with Heart Failure at High Risk of Recurrent Admission and Death: The Trans-European Network–Home-Care Management System (TEN-HMS) Study. Journal of the American College of Cardiology. 2005;45(10):1654–1664. doi: 10.1016/j.jacc.2005.01.050. [DOI] [PubMed] [Google Scholar]
- 43.Dansky K., Vasey J., Bowles K. Impact of Telehealth on Clinical Outcomes in Patients with Heart Failure. Clinical Nursing Research. 2008;17(3):182–199. doi: 10.1177/1054773808320837. [DOI] [PubMed] [Google Scholar]
- 44.Kropf N., Grigsby K. Telemedicine for Older Adults. Home Health Care Services Quarterly. 1999;17(4):1–11. doi: 10.1300/J027v17n04_01. [DOI] [PubMed] [Google Scholar]
- 45.Agency for Healthcare Research and Quality Preventing Disability in the Elderly with Chronic Disease. Research in Action. April 2002;(3) [Google Scholar]
- 46.Kobb R., Hoffman N., et al. Enhancing Elder Chronic Care through Technology and Care Coordination: Report from a Pilot. Telemedicine and eHealth. 2003;9(2):189–195. doi: 10.1089/153056203766437525. [DOI] [PubMed] [Google Scholar]
- 47.Wootton R. Twenty Years of Telemedicine in Chronic Disease Management: An Evidence Synthesis. Journal of Telemedicine and Telecare. 2012;18(4):211–220. doi: 10.1258/jtt.2012.120219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wootton R. Editor's View of Telemedicine. Journal of Telemedicine and Telecare. 2004;10(6):311–317. doi: 10.1258/1357633042602116. [DOI] [PubMed] [Google Scholar]
- 49.Adeogun O., Tiwari A., Alcock J. Models of Information Exchange for UK Telehealth Systems. International Journal of Medical Informatics. 2011;80(5):359–370. doi: 10.1016/j.ijmedinf.2011.01.013. [DOI] [PubMed] [Google Scholar]
- 50.Louis A., Turner T., et al. A Systematic Review of Telemonitoring for the Management of Heart Failure. European Journal of Heart Failure. 2003;5(5):583–590. doi: 10.1016/s1388-9842(03)00160-0. [DOI] [PubMed] [Google Scholar]
- 51.Chaudhry S., Phillips C., et al. Telemonitoring for Patients with Chronic Heart Failure: A Systematic Review. Journal of Cardiac Failure. 2007;13(1):56–62. doi: 10.1016/j.cardfail.2006.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kunz R., Oxman A. The Unpredictability Paradox: Review of Empirical Comparisons of Randomised and Non-randomised Clinical Trials. British Medical Journal. 1998;317(7167):1185–1190. doi: 10.1136/bmj.317.7167.1185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Odgaard-Jensen J., Vist J., et al. Randomisation to Protect against Selection Bias in Healthcare Trials. Cochrane Database Systematic Review. 2011;13(4) doi: 10.1002/14651858.MR000012.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Adeogun O., Tiwari A., Alcock J. Models of Information Exchange for UK Telehealth Systems. [DOI] [PubMed]
- 55.Pare G., Jaana M., Sicotte C. Systematic Review of Home Telemonitoring for Chronic Diseases: The Evidence Base. Journal of the American Medical Informatics Association. 2007;14(3):269–277. doi: 10.1197/jamia.M2270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Celler B., Lovell N., Basilakis J. Using Information Technology to Improve the Management of Chronic Disease. Medical Journal of Australia. 2003;179(5):242–246. doi: 10.5694/j.1326-5377.2003.tb05529.x. [DOI] [PubMed] [Google Scholar]
- 57.Parmanto B., Pramana G., et al. iMHere: A Novel mHealth System for Supporting Self-Care in Management of Complex and Chronic Conditions. JMIR Mhealth and Uhealth. 2013;1(2):e10. doi: 10.2196/mhealth.2391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Scherr D., Kastner P., et al. Effect of Home-based Telemonitoring Using Mobile Phone Technology on the Outcome of Heart Failure Patients after an Episode of Acute Decompensation: Randomized Controlled Trial. [DOI] [PMC free article] [PubMed]
- 59.Dang S., Ma F., et al. Differential Resource Utilization Benefits with Internet-based Care Coordination in Elderly Veterans with Chronic Diseases Associated with High Resource Utilization. [DOI] [PubMed]
- 60.Steventon A., Bardsley M., et al. Effect of Telehealth on Use of Secondary Care and Mortality: Findings from the Whole System Demonstrator Cluster Randomised Trial. [DOI] [PMC free article] [PubMed]
- 61.Soran O., Pina I., et al. A Randomized Clinical Trial of the Clinical Effects of Enhanced Heart Failure Monitoring Using a Computer-based Telephonic Monitoring System in Older Minorities and Women. [DOI] [PubMed]
- 62.Weintraub A., Gregory D., et al. A Multicenter Randomized Controlled Evaluation of Automated Home Monitoring and Telephonic Disease Management in Patients Recently Hospitalized for Congestive Heart Failure: The SPAN-CHF II Trial. [DOI] [PubMed]
- 63.Giordano A., Scalvini S., et al. Multicenter Randomised Trial on Home-based Telemanagement to Prevent Hospital Readmission of Patients with Chronic Heart Failure. International Journal of Cardiology. 2009;131(2):192–199. doi: 10.1016/j.ijcard.2007.10.027. [DOI] [PubMed] [Google Scholar]
- 64.Webb C., Waugh C., et al. Impact of Telemedicine on Hospital Transport, Length of Stay, and Medical Outcomes in Infants with Suspected Heart Disease: A Multicenter Study. [DOI] [PubMed]
- 65.Dendale P., De Keulenaer G., et al. Effect of a Telemonitoring-facilitated Collaboration between General Practitioner and Heart Failure Clinic on Mortality and Rehospitalization Rates in Severe Heart Failure: The TEMA-HF 1 (TElemonitoring in the MAnagement of Heart Failure) Study. [DOI] [PubMed]
- 66.Domingo M., Lupon J., et al. Noninvasive Remote Telemonitoring for Ambulatory Patients with Heart Failure: Effect on Number of Hospitalizations, Days in Hospital, and Quality of Life. CARME (CAtalan Remote Management Evaluation) Study. [DOI] [PubMed]
- 67.Schofield R., Kline S., et al. Early Outcomes of a Care Coordination-enhanced Telehome Care Program for Elderly Veterans with Chronic Heart Failure. [DOI] [PubMed]
- 68.Koehler F., Winkler S., et al. Impact of Remote Telemedical Management on Mortality and Hospitalizations in Ambulatory Patients with Chronic Heart Failure: The Telemedical Interventional Monitoring in Heart Failure Study. [DOI] [PubMed]
- 69.Verhoeven F., Tanja-Dijkstra K., et al. Asynchronous and Synchronous Teleconsultation for Diabetes Care: A Systematic Literature Review. Journal of Diabetes Science and Technology. 2010;4(3):666–684. doi: 10.1177/193229681000400323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Loane M., Bloomer S., et al. A Comparison of Real-time and Store-and-Forward Teledermatology: A Cost-Benefit Study. British Journal of Dermatology. 2008;143(6):1241–1247. doi: 10.1046/j.1365-2133.2000.03895.x. [DOI] [PubMed] [Google Scholar]
- 71.Eedy D., Wootton R. Teledermatology: A Review. British Journal of Dermatology. 2001;144(4):696–707. doi: 10.1046/j.1365-2133.2001.04124.x. [DOI] [PubMed] [Google Scholar]
- 72.Loane M., Bloomer S., et al. A Comparison of Real-time and Store-and-Forward Teledermatology: A Cost-Benefit Study. [DOI] [PubMed]
- 73.Loane M.A., Bloomer S.E., et al. A Randomized Controlled Trial to Assess the Clinical Effectiveness of Both Realtime and Store-and-Forward Teledermatology Compared with Conventional Care. Journal of Telemedicine and Telecare. 2000;6(suppl. 1):S1–S3. doi: 10.1258/1357633001933952. [DOI] [PubMed] [Google Scholar]
- 74.Verhoeven F., Tanja-Dijkstra K., et al. Asynchronous and Synchronous Teleconsultation for Diabetes Care: A Systematic Literature Review. [DOI] [PMC free article] [PubMed]
- 75.Durrani H., Khoja S. A Systematic Review of the Use of Telehealth in Asian Countries. Journal of Telemedicine and Telecare. 2009;15(4):175–181. doi: 10.1258/jtt.2009.080605. [DOI] [PubMed] [Google Scholar]
- 76.Barlow J., Singh D., et al. A Systematic Review of the Benefits of Home Telecare for Frail Elderly People and Those with Long-Term Conditions. Journal of Telemedicine and Telecare. 2007;4(13):172–179. doi: 10.1258/135763307780908058. [DOI] [PubMed] [Google Scholar]
- 77.Koch S. Home Telehealth: Current State and Future Trends. International Journal of Medical Informatics. 2006;75(8):565–576. doi: 10.1016/j.ijmedinf.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 78.Doarn C., Pruitt S., et al. Federal Efforts to Define and Advance Telehealth: A Work in Progress. Telemedicine and eHealth. 2014;20(5):409–418. doi: 10.1089/tmj.2013.0336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Alberta Heritage Foundation for Medical Research Socio-economic Impact of Telehealth: Evidence Now for Health Care in the Future.
- 80.Sanders D., Aronsky D. Biomedical Informatics Applications for Asthma Care: A Systematic Review. Journal of American Medical Informatics Association. 2006;13(4):418–427. doi: 10.1197/jamia.M2039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.McLean S., Sheikh A., et al. The Impact of Telehealthcare on the Quality and Safety of Care: A Systematic Overview. PLoS ONE. 2013;8(8):e71238. doi: 10.1371/journal.pone.0071238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Farmer A., Gibson O., et al. A Systematic Review of Telemedicine Interventions to Support Blood Glucose Self-Monitoring in Diabetes. Diabetic Medicine. 2005;22(10):1372–1378. doi: 10.1111/j.1464-5491.2005.01627.x. [DOI] [PubMed] [Google Scholar]
- 83.Jackson C., Bolen S., et al. A Systematic Review of Interactive Computer-assisted Technology in Diabetes Care. Interactive Information Technology in Diabetes Care. 2005;21(2):105–110. doi: 10.1111/j.1525-1497.2005.00310.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bardsley M., Steventon A., Doll H. Impact of Telehealth on General Practice Contacts: Findings from the Whole Systems Demonstrator Cluster Randomised Trial. BMC Health Services Research. 2013;13(395) doi: 10.1186/1472-6963-13-395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Pare G., Jaana M., Sicotte C. Systematic Review of Home Telemonitoring for Chronic Diseases: The Evidence Base. [DOI] [PMC free article] [PubMed]
- 86.Dellifraine J., Dansky K. Home-based Telehealth: A Review and Meta-analysis. Journal of Telemedicine and Telecare. 2008;14(2):62–66. doi: 10.1258/jtt.2007.070709. [DOI] [PubMed] [Google Scholar]
- 87.Martinez A., Everss E., et al. A Systematic Review of the Literature on Home Monitoring for Patients with Heart Failure. Journal of Telemedicine and Telecare. 2006;12(5):234–241. doi: 10.1258/135763306777889109. [DOI] [PubMed] [Google Scholar]
- 88.Clark R., Inglis S., et al. Telemonitoring or Structured Telephone Support Programmes for Patients with Chronic Heart Failure: Systematic Review and Meta-analysis. British Medical Journal. 2007;334(942) doi: 10.1136/bmj.39156.536968.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Polisena J., Tran K., et al. Home Telehealth for Diabetes Management: A Systematic Review and Meta-analysis. Diabetes Obesity and Metabolism. 2009;11(10):913–930. doi: 10.1111/j.1463-1326.2009.01057.x. [DOI] [PubMed] [Google Scholar]
- 90.Morguet A., Kühnelt P., et al. Impact of Telemedical Care and Monitoring on Morbidity in Mild to Moderate Chronic Heart Failure. [DOI] [PubMed]
- 91.Steventon A., Bardsley M., et al. Effect of Telehealth on Use of Secondary Care and Mortality: Findings from the Whole System Demonstrator Cluster Randomised Trial. [DOI] [PMC free article] [PubMed]
- 92.Chen Y., Ho Y., et al. Assessment of the Clinical Outcomes and Cost-effectiveness of the Management of Systolic Heart Failure in Chinese Patients Using a Home-based Intervention. [DOI] [PubMed]
- 93.Purdy S., Paranjothy S., et al. Interventions to Reduce Unplanned Hospital Admission: A Series of Systematic Reviews. Bristol, UK: National Institute for Health Research; 2012. [Google Scholar]
- 94.Moattari M., Hashemi M., Dabbaghmanesh M. The Impact of Electronic Education on Metabolic Control Indicators in Patients with Diabetes Who Need Insulin: A Randomised Clinical Control Trial. Journal of Clinical Nursing. 2013;22(1–2):32–38. doi: 10.1111/j.1365-2702.2012.04200.x. [DOI] [PubMed] [Google Scholar]
- 95.Ritsema T., Bingenheimer J., et al. Differences in the Delivery of Health Education to Patients with Chronic Disease by Provider Type, 2005–2009. Preventing Chronic Disease. 2014;11:130175. doi: 10.5888/pcd11.130175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Jordan J., Briggs A., et al. Enhancing Patient Engagement in Chronic Disease Self-Management Support Initiatives in Australia: The Need for an Integrated Approach. Medical Journal of Australia. 2008;89(10):S9–S13. doi: 10.5694/j.1326-5377.2008.tb02202.x. [DOI] [PubMed] [Google Scholar]
- 97.Gambling T., Long A. The Realisation of Patient-centred Care During a 3-Year Proactive Telephone Counselling Self-Care Intervention for Diabetes. Patient Education and Counseling. 2009;80(2):219–226. doi: 10.1016/j.pec.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 98.Miller E.Telemedicine and the Provider-Patient Relationship: What We Know So Far. Report prepared for the Nuffield Council's Working Party on Medical Profiling and Online Medicine. 2010. Available at http://nuffieldbioethics.org/wp-content/uploads/Miller-E-2010-Evidence-review-Telemedicine-and-the-Provider-Patient-Relationship-what-we-know-so-far.pdf.
- 99.Huha J., Lea T., et al. Perspectives on Wellness Self-Monitoring Tools for Older Adults. International Journal of Medical Informatics. 2013;82:1092–1103. doi: 10.1016/j.ijmedinf.2013.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Farberow B., Hatton V., et al. Caveat Emptor: The Need for Evidence, Regulation, and Certification of Home Telehealth Systems for the Management of Chronic Conditions. American Journal of Medical Quality. 2008;23(3):208–214. doi: 10.1177/1062860608315123. [DOI] [PubMed] [Google Scholar]
- 101.Jennett P., Scott R., et al. Policy Implications Associated with the Socioeconomic and Health System Impact of Telehealth: A Case Study from Canada. Telemedicine and e-Health. 2004;10(1):77–83. doi: 10.1089/153056204773644616. [DOI] [PubMed] [Google Scholar]
- 102.Koch S. Home Telehealth: Current State and Future Trends. [DOI] [PubMed]
- 103.Demitris G., Speedie S., Finkelstein S. Change of Patients’ Perceptions of TeleHomeCare. Telemedicine and e-Health. 2001;7(3):241–248. doi: 10.1089/153056201316970948. [DOI] [PubMed] [Google Scholar]
- 104.Kaminsky E., Rosenqvist U., Holmström I. Telenurses’ Understanding of Work: Detective or Educator. Journal of Advanced Nursing. 2008;65(2):382–390. doi: 10.1111/j.1365-2648.2008.04877.x. [DOI] [PubMed] [Google Scholar]
- 105.Andreassen H. ICT and Patient Roles: Contradictions in E-health Policy. Health Policy and Technology. 2012;1(2):86–92. [Google Scholar]
- 106.Ni H., Nauman D., et al. Factors Influencing Knowledge of and Adherence to Self-Care among Patients with Heart Failure. Archives of Internal Medicine. 1999;159(14):1613–1619. doi: 10.1001/archinte.159.14.1613. [DOI] [PubMed] [Google Scholar]
- 107.Wright S., Verouhis D., et al. Factors Influencing the Length of Hospital Stay of Patients with Heart Failure. European Journal of Heart Failure. 2003;5(2):201–209. doi: 10.1016/s1388-9842(02)00201-5. [DOI] [PubMed] [Google Scholar]
- 108.Perelman J., Closon M. Impact of Socioeconomic Factors on In-patient Length of Stay and Their Consequences in Per Case Hospital Payment Systems. Journal of Health Services Research and Policy. 2011;16(4):197–202. doi: 10.1258/jhsrp.2011.010047. [DOI] [PubMed] [Google Scholar]
- 109.Philbin E., Dec G., et al. Socioeconomic Status as an Independent Risk Factor for Hospital Readmission for Heart Failure. American Journal of Cardiology. 2001;87(12):1367–1371. doi: 10.1016/s0002-9149(01)01554-5. [DOI] [PubMed] [Google Scholar]
- 110.Xiao J., Douglas D., et al. A Delphi Evaluation of the Factors Influencing Length of Stay in Australian Hospitals. International Journal of Health Planning and Management. 1997;12(3):207–218. doi: 10.1002/(SICI)1099-1751(199707/09)12:3<207::AID-HPM480>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 111.Whellan D., Zhao X., et al. Predictors of Hospital Length of Stay in Heart Failure: Findings from Get with the Guidelines. Journal of Cardiac Failure. 2011;17(8):649–656. doi: 10.1016/j.cardfail.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 112.Landi F., Onder G., et al. Comorbidity and Social Factors Predicted Hospitalization in Frail Elderly Patients. Journal of Clinical Epidemiology. 2004;57(8):832–836. doi: 10.1016/j.jclinepi.2004.01.013. [DOI] [PubMed] [Google Scholar]
- 113.Mair F., May C., et al. Factors That Promote or Inhibit the Implementation of E-health Systems: An Explanatory Systematic Review. Bulletin of the World Health Organization. 2012;90(5):357–364. doi: 10.2471/BLT.11.099424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Rahimpour M., Lovella N., et al. Patients’ Perceptions of a Home Telecare System. International Journal of Medical Informatics. 2008;77(7):486–498. doi: 10.1016/j.ijmedinf.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 115.Thurmond V., Boyle D. An Integrative Review of Patients’ Perceptions Regarding Telehealth Used in Their Health Care. Online Journal of Knowledge Synthesis of Nursing. 2002;E9(1):12–32. [PubMed] [Google Scholar]
- 116.Kaminsky E., Rosenqvist U., Holmström I. Telenurses’ Understanding of Work: Detective or Educator. [DOI] [PubMed]
- 117.Xiao J., Douglas D., et al. A Delphi Evaluation of the Factors Influencing Length of Stay in Australian Hospitals. [DOI] [PubMed]
- 118.Whellan D., Zhao X., et al. Predictors of Hospital Length of Stay in Heart Failure: Findings from Get with the Guidelines. [DOI] [PubMed]
- 119.Wang Y., Stavem K., et al. Factors Associated with a Prolonged Length of Stay after Acute Exacerbation of Chronic Obstructive Pulmonary Disease (AECOPD) International Journal of Chronic Obstructive Pulmonary Disease. 2014;2014(9):99–105. doi: 10.2147/COPD.S51467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Hamner J., Ellison K. Predictors of Hospital Readmission after Discharge in Patients with Congestive Heart Failure. Heart and Lung. 2005;34(4):231–239. doi: 10.1016/j.hrtlng.2005.01.001. [DOI] [PubMed] [Google Scholar]
- 121.Polanczyk C., Newton C., et al. Quality of Care and Hospital Readmission in Congestive Heart Failure: An Explicit Review Process. Journal of Cardiac Failure. 2001;7(4):289–298. doi: 10.1054/jcaf.2001.28931. [DOI] [PubMed] [Google Scholar]
- 122.Soyiri I., Reidpath D., Sarran C. Asthma Length of Stay in Hospitals in London 2001–2006: Demographic, Diagnostic and Temporal Factors. PLoS ONE. 2011;6(11):e27184. doi: 10.1371/journal.pone.0027184. [DOI] [PMC free article] [PubMed] [Google Scholar]