Abstract
The purpose of this study is to describe one potential intervention model designed to slow decline to disability for individuals at-risk for dementia due to Mild Cognitive Impairment. Strategy training is a treatment model that focuses on behavioral activation through addressing barriers to daily activities. Strategy training encourages development of goals and plans to address self-identified impaired processes, and it maintains or improves individuals’ ability to perform desired activities. Progression to dementia may be slowed due to the link between engagement in daily activities and production of biological factors associated with neurocognitive health. We demonstrated that an older adult with Mild Cognitive Impairment is able to develop goals, establish effective plans, and engage in daily activities through the strategy training intervention model.
Keywords: Strategy training, non-pharmacological intervention, mild cognitive impairment, dementia, cognition
INTRODUCTION
Dementia is costly on personal and societal levels, and is a growing public health concern. The Alzheimer’s Association predicts that the prevalence of older adults with dementia may triple to an estimated 16 million individuals by the year 2050 (Alzheimer’s Association, 2014). Mild Cognitive Impairment (MCI) is a state between normal cognitive aging and dementia. Older adults with MCI develop dementia at a rate of 10–15% per year (Mitchell & Shiri-Feshki, 2009). As a result, older adults with MCI are at-risk for disability associated with dementia. The ability to delay or reverse progression to dementia for these older adults would have a tremendous public health impact.
NEED FOR NON-PHARMACOLOGICAL INTERVENTIONS
Numerous interventions have been proposed to delay or reverse progression but none have been widely effective (Cooper, Li, Lyketsos, & Livingston, 2013). Results from pharmaceutical trials have been largely disappointing (Birks & Flicker, 2006; Farina, Isaac, Clark, Rusted, & Tabet, 2012; Russ & Morling, 2012; Russ, 2014; Yue et al., 2012). Non-pharmacological interventions have focused on cognitive remediation, physical activity, and coping strategies, and none of these approaches have been robustly effective in delaying or reversing progression to dementia (Austrom & Lu, 2009; Barnes et al., 2009; Belleville et al., 2006; Rovner, Casten, Hegel, & Leiby, 2012). Interventions that focus on delaying disability are limited even though research suggests that individuals with MCI demonstrate impaired performance in daily activities (Reppermund et al., 2013; Rodakowski et al., 2014). A focus on performance or engagement in daily activities may be a promising alternative, as enhanced engagement has been connected to positive health outcomes and decreased engagement has been associated with disability (Colcombe et al., 2006; Cooper et al., 2013). Furthermore, individuals with MCI retain the capacity to problem solve and develop effective strategies to manage daily activities (Fernández-Ballesteros, Zamarrón, Tárraga, Moya, & Iñiguez, 2003; Mufson et al., 2003). Thus, an intervention that helps individuals with MCI develop effective strategies in the course of daily activities may delay disability and may slow progression to dementia. Progression to dementia may be slowed by increased engagement in daily activities as several mechanisms, in addition to neurocognitive and emotional health, link engagement in daily activities to biological factors (Butters et al., 2008; Cassilhas et al., 2012; Kivipelto et al., 2001; Radák et al., 2001). Due to these linkages, greater engagement in activities may modify the production of biological factors associated with neurocognitive health, and thereby decrease risk of further cognitive and mental health.
A POTENTIAL TREATMENT MODEL
Interventions that promote behavioral activation may be effective platform to enhance performance and engagement in daily activities. Behavioral activation is a treatment platform that seeks to promote positive environmental reinforcements and reduce negative influences. It has been effective in activating individuals with other neurological and psychiatric disorders (Cuijpers, van Straten, & Warmerdam, 2007; Skidmore, Whyte, Butters, Terhorst, & Reynolds, 2015). Strategy training, adapted from the Cognitive Orientation to Occupational Performance Approach (Dawson et al., 2014; Missiuna, Mandich, Polatajko, & Malloy-Miller, 2001; Polatajko et al., 2001; Skidmore et al., 2014), is one treatment model that focuses on activation through performance of daily activities. Strategy training shares many key components with behavioral activation, including self-selected goal setting, self-evaluation of performance, and problem-solving for daily activities. Strategy training has theoretical underpinnings derived from cognitive, behavioral, and learning theories (Meichenbaum, 1977; Swanson & Hoskyn, 1998). The 4 active ingredients for strategy training are self-select goals, conduct performance analysis, use a global strategy, and guided discovery. All are completed in the context of engagement in daily activities. First, participants self-select goals using a standardized process. Second, participants evaluate performance of self-selected goals to identify barriers to performance. Research shows that individuals with cognitive impairments may learn best when they have the opportunity to problem-solve related to personally motivating goals or activities (Melville, Baltic, Bettcher, & Nelson, 2002; Trombly, Radomski, & Davis, 1998). Participants, then, use a global strategy (Goal – Plan – Do – Check) to engage in activities in an organized and consistent format. Strategy training teaches participants to apply their newly developed strategies to encourage of generalization of strategy use (Dawson et al., 2009; Polatajko, Mandich, Miller, & Macnab, 2001). Finally, therapists guide participant engagement in activities. With guided discovery, the participants determine effective and ineffective strategies, plans, and necessary modifications.
Among individuals with acquired brain injuries and healthy older adults, the benefits of strategy training are being demonstrated (Dawson et al., 2014; Skidmore et al., 2014). The benefits include improved trajectories of recovery after stroke, increased awareness of impaired cognitive processes, and improved generalization of the strategy to other goals (Dawson et al., 2009; McEwen, Huijbregts, Ryan, & Polatajko, 2009; von Cramon, Cramon, & Mai, 1991; Webster & Scott, 1983). Additionally, among older adults with subjective cognitive complaints, strategy training improved engagement in daily activities that were not discussed during the intervention (Dawson et al., 2014). Research suggests that strategy training is a promising intervention approach for individuals with MCI, but it has not been tried.
Interventions that use strategy training early in the disease trajectory may be most effective, because individuals in the early stages of cognitive decline maintain the ability to adapt performance of daily activities. Additionally, evidence that supports the benefits of early intervention to support quality of life (Sperling et al., 2011). Nonetheless, barriers may arise when providing this training to individuals with MCI. Individuals may be become frustrated due to their memory impairments or refuse treatment due to perceived independence in daily activities. Furthermore, previously examined strategy training programs may need to be adjusted to be implemented in the homes of individuals with MCI.
A CASE EXAMPLE
With Institutional Review Board approval (PRO14070341), we recruited a 79 year old white American male with MCI from the University of Pittsburgh’s Alzheimer’s Disease Research Center (ADRC). The ADRC adjudicated him as having amnestic-MCI, multiple domain, using procedures described elsewhere (Beekly et al., 2007). He self-reported difficulty with daily activities, and was community dwelling. He lived with his wife in a suburban private-residence. He was a retired lawyer and former local mayor.
A licensed and registered occupational therapist delivered 12 sessions (60 minutes each over a 6 week period) in the participant’s home. The first session included introduction of the strategy training intervention and identification of goals. We used the Canadian Occupational Performance Measure to generate self-selected and motivating goals (Law et al., 1998; McColl et al., 2006). For this process, the participant described a typical day, identified activities that were problematic. He then rated the importance and estimated his current performance of these activities on 1–10 scales. The therapist described the global strategy (Goal – Plan – Do – Check) with visual cues from the participant workbook. The participant workbook also provided worksheets that facilitated application of the global strategy and performance analysis. Upon completion of the first session, the participant was given the homework of prioritizing identified activities to address in subsequent sessions (Figure 1 displays participant identified goals).
Figure 1.
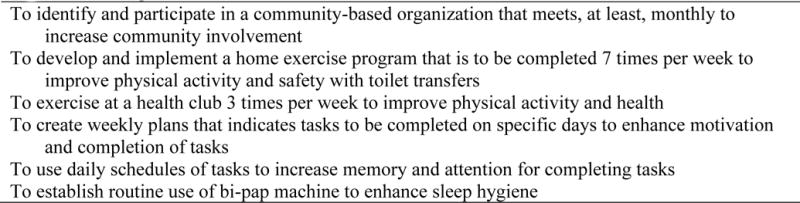
Participant Selected Goals
The second session began with a review of the strategy, and the use of the strategy with the first goal. Using the workbook as a guide, he identified the goals of increasing his energy, mobility, and motivation to engage in daily activities (“goal”). The therapist guided the participant to select one goal and develop a plan to address this goal. The first goal was to increase community involvement through attendance at a monthly community organization. His first plan was to call his local borough office to ask about senior organizations. The participant executed the plan by calling the office and determining which senior groups were available (“do”). He also established when his chosen group’s next meeting would occur. He assessed plan execution (“check”). With the support of guided discovery from the therapist, the participant identified aspects of his plan that were effective and ineffective through performance analysis (Dawson et al., 2014; Skidmore et al., 2014).
The remaining strategy training sessions repeated this process through application of the strategy to improve performance in desired tasks. Transitioning to independence with the global strategy was initiated early in the process through guiding the participant to identify how the plans will continue in the future during the self-assessment process. The entire process was continued until all twelve intervention sessions were completed.
The participant demonstrated satisfaction, adherence, and motivation throughout the sessions. The participant’s depressive symptoms moved from moderate depression severity to no depressive symptoms (Table 1; Kroenke & Spitzer, 2002). For activity limitations and participation restrictions, 10 points is equal to a standard deviation (Jette, Haley, Ni, Olarsch, & Moed, 2008). Thus, the participant demonstrated almost an entire standard deviation change in activity limitations and half a standard deviation change in participation restriction. Sleep quality improved from fairly bad to fairly good (Buysse, Reynolds, Monk, Berman, & Kupfer, 1989). Levels of physical activity remained stable. No formal qualitative methods were employed; however, we informally collected unsolicited comments from the participant. He indicated, “I think that getting into stuff and getting involved a little bit and having a plan makes your memory function a little bit better.” At the end of the intervention sessions, he commented, “what you’ve done for me here is to get me involved in thinking about things to do and get involved in things to do that will get me motivated and moving. That’s the whole point. That was the whole point to begin with.”
Table 1.
Clinical Assessment Findings
| Pre-Intervention | Post-Intervention | |
|---|---|---|
| Patient Health Questionnaire-9 (Gilbody, Richards, Brealey, & Hewitt, 2007) | 10 | 3 |
| Pittsburgh Sleep Quality Index-1 (Buysse, Reynolds, Monk, Berman, & Kupfer, 1989) | 2 | 1 |
| Physical Activity Scale for Elderly (Washburn, Smith, Jette, & Janney, 1993) | 65 | 92 |
| Late-Life Function and Disability Instrument (McDonough et al., 2012) | ||
| Activity Limitation – Score | 52.63 | 61.72 |
| Participation Restriction – Score | 48.56 | 53.33 |
DISCUSSION
Strategy training is one intervention model where individuals address barriers to daily activities and may serve as an intervention that imparts the necessary skills to individuals at-risk for decline. The innovative components of strategy training are that it (1) incorporates self-select goals, (2) encourages performance analysis, (3) uses a global strategy, and (4) integrates guided discovery. As a result, the use of strategy training may equip individuals with MCI with skills and methods to work through and around any identified barrier to a daily activity.
Findings from this case-example are informative but should be interpreted with caution. This study lacks the methodological rigor of a randomized trial, and it lacks external validity due to the single participant described. However, these finding suggest factors that should be considered in future studies that examine non-pharmacological interventions for individuals with MCI. First, the goals selected by the participant were not simple activities that could be completed and achieved in one session. The participant selected goals related to community involvement and independent living, such as increasing involvement in a community organization and developing an exercise routine. The focus on complex goals aligns with the subtle disability that individuals with MCI experience; research demonstrates that individuals with MCI have variability in cognitively challenging or complex daily activities, but not overt disability in basic daily activities (Rodakowski et al., 2014). Second, similar barriers to activity completion were identified across goals by the participant. Thus, the participant was able to maximize strategies used to reach multiple goals and incorporate them in his daily activities and routines. For example, for increasing involvement in organizations, the participant recognized that his impaired memory may be a barrier. He elected to use a notebook to keep track of tasks, meetings, and other reminders. The strategy of using a notebook or calendar was also employed for completion of the goal for increasing mobility. This aligns with research that suggests that individuals with cognitive impairments may learn best when they encounter barriers and identify their own solutions to those barriers (Meichenbaum, 1977). Third, frequent repetition of the strategy (Goal – Plan – Do – Check) appeared critical in the early sessions; this has been previously reported (Dawson et al., 2014; Skidmore et al., 2014). The repetition allowed the participant to internalize the steps, as was seen through plan execution in the individual intervention sessions. Finally, the participant had a wife. He elected to include her in his plans for transportation. Her involvement was confined to this task; thus, partner support was not critical to his success with the intervention. The ability to independently identify solutions suggests that this intervention could be used with individuals who may not have partner support available.
Developing an intervention that is designed to maintain independence for individuals at-risk for dementia is critical. Interventions focused on the daily activities of older adults may be an effective intervention strategy to enhance performance of daily activities, and potentially neurocognitive and emotional health. In particular, strategy training and its related mechanisms of action should be further explored as a potential intervention to slow the decline in daily activities for individuals with MCI.
Acknowledgments
Funding Sources: This work was supported by the National Institutes of Health under grant numbers KL2 TR000146, P30 MH090333, P50 AG05133, UL1 TR000005 and the UPMC Endowed Chair in Geriatric Psychiatry.
References
- Association A. 2014 Alzheimer’s disease facts and figures. Alzheimer’s & Dementia. 2014;10(2):e47–e92. doi: 10.1016/j.jalz.2014.02.001. http://doi.org/10.1016/j.jalz.2014.02.001. [DOI] [PubMed] [Google Scholar]
- Austrom MG, Lu Y. Long term caregiving: helping families of persons with mild cognitive impairment cope. Current Alzheimer Research. 2009;6(4):392–8. doi: 10.2174/156720509788929291. Retrieved from http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2862360&tool=pmcentrez&rendertype=abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes DE, Yaffe K, Belfor N, Jagust WJ, DeCarli C, Reed BR, Kramer JH. Computer-based cognitive training for mild cognitive impairment: results from a pilot randomized, controlled trial. Alzheimer Disease and Associated Disorders. 2009;23(3):205–10. doi: 10.1097/WAD.0b013e31819c6137. http://doi.org/10.1097/WAD.0b013e31819c6137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beekly DL, Ramos EM, Lee WW, Deitrich WD, Jacka ME, Wu J, Kukull WA. The National Alzheimer’s Coordinating Center (NACC) database: the Uniform Data Set. Alzheimer Disease and Associated Disorders. 2007;21(3):249–58. doi: 10.1097/WAD.0b013e318142774e. http://doi.org/10.1097/WAD.0b013e318142774e. [DOI] [PubMed] [Google Scholar]
- Belleville S, Gilbert B, Fontaine F, Gagnon L, Ménard E, Gauthier S. Improvement of episodic memory in persons with mild cognitive impairment and healthy older adults: evidence from a cognitive intervention program. Dementia and Geriatric Cognitive Disorders. 2006;22(5–6):486–99. doi: 10.1159/000096316. http://doi.org/10.1159/000096316. [DOI] [PubMed] [Google Scholar]
- Birks J, Flicker L. Donepezil for mild cognitive impairment. The Cochrane Database of Systematic Reviews. 2006;(3):CD006104. doi: 10.1002/14651858.CD006104. http://doi.org/10.1002/14651858.CD006104. [DOI] [PubMed]
- Butters MA, Young JB, Lopez O, Aizenstein HJ, Mulsant BH, Reynolds CF, Becker JT. Pathways linking late-life depression to persistent cognitive impairment and dementia. Dialogues in Clinical Neuroscience. 2008;10(3):345–57. doi: 10.31887/DCNS.2008.10.3/mabutters. Retrieved from http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2872078&tool=pmcentrez&rendertype=abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Research. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. http://doi.org/10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Cassilhas RC, Lee KS, Fernandes J, Oliveira MGM, Tufik S, Meeusen R, de Mello MT. Spatial memory is improved by aerobic and resistance exercise through divergent molecular mechanisms. Neuroscience. 2012;202:309–17. doi: 10.1016/j.neuroscience.2011.11.029. http://doi.org/10.1016/j.neuroscience.2011.11.029. [DOI] [PubMed] [Google Scholar]
- Colcombe SJ, Erickson KI, Scalf PE, Kim JS, Prakash R, McAuley E, Kramer AF. Aerobic Exercise Training Increases Brain Volume in Aging Humans. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2006;61(11):1166–1170. doi: 10.1093/gerona/61.11.1166. http://doi.org/10.1093/gerona/61.11.1166. [DOI] [PubMed] [Google Scholar]
- Cooper C, Li R, Lyketsos C, Livingston G. Treatment for mild cognitive impairment: systematic review. The British Journal of Psychiatry: The Journal of Mental Science. 2013;203(3):255–64. doi: 10.1192/bjp.bp.113.127811. http://doi.org/10.1192/bjp.bp.113.127811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P, van Straten A, Warmerdam L. Behavioral activation treatments of depression: a meta-analysis. Clinical Psychology Review. 2007;27(3):318–26. doi: 10.1016/j.cpr.2006.11.001. http://doi.org/10.1016/j.cpr.2006.11.001. [DOI] [PubMed] [Google Scholar]
- Dawson D, Gaya A, Hunt A, Levine B, Lemsky C, Polatajko H. Using the Cognitive Orientation to Occupational Performance (CO-OP) with Adults with Executive Dysfunction following Traumatic Brain Injury. Canadian Journal of Occupational Therapy. 2009;76(2):115–127. doi: 10.1177/000841740907600209. http://doi.org/10.1177/000841740907600209. [DOI] [PubMed] [Google Scholar]
- Dawson D, Richardson J, Troyer A, Binns M, Clark A, Polatajko H, Bar Y. An occupation-based strategy training approach to managing age-related executive changes: a pilot randomized controlled trial. Clinical Rehabilitation. 2014;28(2):118–27. doi: 10.1177/0269215513492541. http://doi.org/10.1177/0269215513492541. [DOI] [PubMed] [Google Scholar]
- Farina N, Isaac MGEKN, Clark AR, Rusted J, Tabet N. Vitamin E for Alzheimer’s dementia and mild cognitive impairment. The Cochrane Database of Systematic Reviews. 2012;11:CD002854. doi: 10.1002/14651858.CD002854.pub3. http://doi.org/10.1002/14651858.CD002854.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernández-Ballesteros R, Zamarrón MD, Tárraga L, Moya R, Iñiguez J. Cognitive plasticity in healthy, mild cognitive impairment (MCI) subjects and Alzheimer’s disease patients: A research project in Spain. European Psychologist. 2003;8(3):148–159. [Google Scholar]
- Jette AM, Haley SM, Ni P, Olarsch S, Moed R. Creating a computer adaptive test version of the late-life function and disability instrument. (Series A, Biological Sciences and Medical Sciences).The Journals of Gerontology. 2008;63(11):1246–56. doi: 10.1093/gerona/63.11.1246. Retrieved from http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2718692&tool=pmcentrez&rendertype=abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kivipelto M, Helkala EL, Hänninen T, Laakso MP, Hallikainen M, Alhainen K, Nissinen A. Midlife vascular risk factors and late-life mild cognitive impairment: A population-based study. Neurology. 2001;56(12):1683–9. doi: 10.1212/wnl.56.12.1683. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11425934. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL. The PHQ-9: A new depression diagnostic and severity measure. Psychiatric Annals. 2002;32(9):509–515. [Google Scholar]
- Law M, Baptiste S, Carswell A, McCOll M, Polatajko H, Pollock N. Canadian Occupational Performance Measure. 3rd. Ottawa, ON: CAOT Publications ACE; 1998. [Google Scholar]
- McColl M, Carswell A, Law M, Pollock N, Baptiste S, Polatajko H. Research on the Canadian Occupational Performance Measure: an annotated resource. Ottawa, ON: CAOT Publications ACE; 2006. [Google Scholar]
- McEwen SE, Huijbregts MPJ, Ryan JD, Polatajko HJ. Cognitive strategy use to enhance motor skill acquisition post-stroke: a critical review. Brain Injury. 2009;23(4):263–77. doi: 10.1080/02699050902788493. http://doi.org/10.1080/02699050902788493. [DOI] [PubMed] [Google Scholar]
- Meichenbaum D. Cognitive-Behavior Modification: An Integrative Approach (Google eBook) Springer; 1977. Retrieved from http://books.google.com/books?hl=en&lr=&id=ukmq1rNArdUC&pgis=1. [Google Scholar]
- Melville LL, Baltic TA, Bettcher TW, Nelson DL. Patients’ perspectives on the self-identified goals assessment. The American Journal of Occupational Therapy: Official Publication of the American Occupational Therapy Association. 2002;56(6):650–9. doi: 10.5014/ajot.56.6.650. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12458857. [DOI] [PubMed] [Google Scholar]
- Missiuna C, Mandich AD, Polatajko HJ, Malloy-Miller T. Cognitive Orientation to Daily Occupational Performance (CO-OP) Physical & Occupational Therapy in Pediatrics. 2001;20(2–3):69–81. http://doi.org/10.1080/J006v20n02_05. [PubMed] [Google Scholar]
- Mitchell AJ, Shiri-Feshki M. Rate of progression of mild cognitive impairment to dementia–meta-analysis of 41 robust inception cohort studies. Acta Psychiatrica Scandinavica. 2009;119(4):252–65. doi: 10.1111/j.1600-0447.2008.01326.x. http://doi.org/10.1111/j.1600-0447.2008.01326.x. [DOI] [PubMed] [Google Scholar]
- Mufson EJ, Ikonomovic MD, Styren SD, Counts SE, Wuu J, Leurgans S, DeKosky ST. Preservation of brain nerve growth factor in mild cognitive impairment and Alzheimer disease. Archives of Neurology. 2003;60(8):1143–8. doi: 10.1001/archneur.60.8.1143. http://doi.org/10.1001/archneur.60.8.1143. [DOI] [PubMed] [Google Scholar]
- Polatajko HJ, Mandich AD, Miller LT, Macnab JJ. Cognitive Orientation to Daily Occupational Performance (CO-OP) Physical & Occupational Therapy in Pediatrics. 2001;20(2–3):83–106. http://doi.org/10.1080/J006v20n02_06. [PubMed] [Google Scholar]
- Polatajko HJ, Mandich AD, Missiuna C, Miller LT, Macnab JJ, Malloy-Miller T, Kinsella EA. Cognitive Orientation to Daily Occupational Performance(CO-OP) Physical & Occupational Therapy in Pediatrics. 2001;20(2–3):107–123. http://doi.org/10.1080/J006v20n02_07. [PubMed] [Google Scholar]
- Radák Z, Kaneko T, Tahara S, Nakamoto H, Pucsok J, Sasvári M, Goto S. Regular exercise improves cognitive function and decreases oxidative damage in rat brain. Neurochemistry International. 2001;38(1):17–23. doi: 10.1016/s0197-0186(00)00063-2. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10913684. [DOI] [PubMed] [Google Scholar]
- Reppermund S, Brodaty H, Crawford JD, Kochan Na, Draper B, Slavin MJ, Sachdev PS. Impairment in instrumental activities of daily living with high cognitive demand is an early marker of mild cognitive impairment: the Sydney Memory and Ageing Study. Psychological Medicine. 2013:1–9. doi: 10.1017/S003329171200308X. http://doi.org/10.1017/S003329171200308X. [DOI] [PubMed]
- Rodakowski J, Skidmore ER, Reynolds CF, Dew MA, Butters MA, Holm MB, Rogers JC. Can performance on daily activities discriminate between older adults with normal cognitive function and those with mild cognitive impairment? Journal of the American Geriatrics Society. 2014;62(7):1347–1352. doi: 10.1111/jgs.12878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rovner BW, Casten RJ, Hegel MT, Leiby BE. Preventing cognitive decline in older African Americans with mild cognitive impairment: design and methods of a randomized clinical trial. Contemporary Clinical Trials. 2012;33(4):712–20. doi: 10.1016/j.cct.2012.02.016. http://doi.org/10.1016/j.cct.2012.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russ TC. Cholinesterase inhibitors should not be prescribed for mild cognitive impairment. Evidence-Based Medicine. 2014;19(3):101. doi: 10.1136/eb-2013-101687. http://doi.org/10.1136/eb-2013-101687. [DOI] [PubMed] [Google Scholar]
- Russ TC, Morling JR. Cholinesterase inhibitors for mild cognitive impairment. The Cochrane Database of Systematic Reviews. 2012;9:CD009132. doi: 10.1002/14651858.CD009132.pub2. http://doi.org/10.1002/14651858.CD009132.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skidmore ER, Dawson DR, Whyte EM, Butters MA, Dew MA, Grattan ES, Holm MB. Developing complex interventions: lessons learned from a pilot study examining strategy training in acute stroke rehabilitation. Clinical Rehabilitation. 2014;28(4):378–87. doi: 10.1177/0269215513502799. http://doi.org/10.1177/0269215513502799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skidmore ER, Whyte EM, Butters MA, Terhorst L, Reynolds CF. Strategy Training During Inpatient Rehabilitation May Prevent Apathy Symptoms After Acute Stroke. PM & R: The Journal of Injury, Function, and Rehabilitation. 2015;7(6):562–70. doi: 10.1016/j.pmrj.2014.12.010. http://doi.org/10.1016/j.pmrj.2014.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sperling RA, Aisen PS, Beckett LA, Bennett DA, Craft S, Fagan AM, Phelps CH. Toward defining the preclinical stages of Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association. 2011;7(3):280–92. doi: 10.1016/j.jalz.2011.03.003. http://doi.org/10.1016/j.jalz.2011.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swanson HL, Hoskyn M. Experimental Intervention Research on Students with Learning Disabilities: A Meta-Analysis of Treatment Outcomes. Review of Educational Research. 1998;68(3):277–321. http://doi.org/10.3102/00346543068003277. [Google Scholar]
- Trombly CA, Radomski MV, Davis ES. Achievement of Self-Identified Goals by Adults With Traumatic Brain Injury: Phase I. American Journal of Occupational Therapy. 1998;52(10):810–818. doi: 10.5014/ajot.56.5.489. http://doi.org/10.5014/ajot.52.10.810. [DOI] [PubMed] [Google Scholar]
- von Cramon DY, Cramon GM, Mai N. Problem-solving deficits in brain-injured patients: A therapeutic approach. Neuropsychological Rehabilitation. 1991;1(1):45–64. http://doi.org/10.1080/09602019108401379. [Google Scholar]
- Webster JS, Scott RR. The effects of self-instructional training on attentional deficits following head injury. Clinical Neuropsychology. 1983;5(2):69–74. [Google Scholar]
- Yue J, Dong BR, Lin X, Yang M, Wu HM, Wu T. Huperzine A for mild cognitive impairment. The Cochrane Database of Systematic Reviews. 2012;12:CD008827. doi: 10.1002/14651858.CD008827.pub2. http://doi.org/10.1002/14651858.CD008827.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]


