Abstract
Objectives:
To determine the role of hemogram parameters such as platelet count (PLT), mean platelet volume (MPV), and the MPV/PLT ratio in predicting the risk of postoperative vomiting (POV) in children after tooth extraction under deep sedation.
Methods:
A total of 100 American Society of Anesthesiology Classification I and II pediatric patients who underwent tooth extraction procedures under a standard anesthetic method were included in the study between 2012 and 2014. The study took place at the Faculty of Dentistry, Department of Oral and Maxillofacial Surgery, Erciyes University, Erciyes, Turkey Fifty patients without POV (group 1) and 50 patients with POV (group 2) were retrospectively selected randomly from the records of 885 consecutive patients. Age, gender, duration of the operation, and preoperative hemogram findings were recorded.
Results:
There was a statistically significant difference between the 2 groups in terms of MPV (p<0.001), PLT (p=0.006), and MPV/PLT (p<0.001) ratio. Mean platelet volume and MPV/PLT ratio were higher in group 2, whereas PLT was higher in group 1.
Conclusion:
The PLT count, MPV, and MPV/PLT ratio may be used to predict POV in children.
Postoperative nausea and vomiting (PONV) are distressing and common complications after outpatient surgery, and may lead to undesirable adverse effects such wound opening, esophagus rupture, bleeding, hematoma, and aspiration of the gastric contents. Postoperative nausea and vomiting complicate recovery, and can lead to delayed patient discharge from the postanesthesia care unit.1 In addition, PONV impairs patient comfort, and may affect their normal daily activities. Various risk factors for PONV were described such as age, female gender, non-smoking status, obesity, previous postoperative nausea and vomiting history, type and duration of anesthesia, and type of surgery. Other risk factors include childhood and younger adulthood, use of volatile anesthetics, and large-dose opioids. A history of migraine, intense preoperative anxiety are also other possible risk factors.2 Tooth extraction is one of the minimally invasive procedures of oral and maxillofacial surgery, and sometimes is difficult to manage in children due to fear and anxiety. Therefore, tooth extraction is generally performed under sedation, or general anesthesia in the pediatric population.3 Hemogram parameters such as neutrophil/lymphocyte (N/L) ratio, mean platelet volume (MPV), and red blood cell volume (RDW) have been associated with several inflammatory diseases as a factor predicting PONV.4,5 Inflammation has a role in the pathogenesis of migraine; elevated RDW is associated with migraine6 and migraine generally occurs together with nausea and vomiting. Also, the N/L ratio has been suggested as a marker for both the presence and severity of hyperemesis gravidarum.7 Serotonin plays an important part in the pathophysiology of PONV, so serotonin-blocking agents are commonly used for its treatment.8 The platelets are known to hold major deposits of serotonin and platelet activation leads to release of this neurotransmitter.9 According to our hypothesis, a platelet count (PLT), or MPV may determine a body’s serotonin level and it plays a role in PONV. Thus, defining objective parameters, which can easily be calculated from blood level may provide additional information to predict PONV risk.
Although several factors have been described to clarify the mechanism of postoperative vomiting (POV), there are no clear data in the literature on the influence of the neutrophil (N) count, lymphocyte (L) count (N/L ratio), MPV, and MPV/PLT ratio on POV. The aim of this study is to assess the role of hemogram parameters, such as PLT, MPV, and MPV/PLT to predict POV in children who had experienced tooth extraction under deep sedation.
Methods
The study protocol was approved by the Local Ethics Committee of Erciyes University. A total of 100 American Society of Anesthesiology Classification I and II pediatric patients, who had undergone a tooth extraction procedure under a standard anesthetic method at the Faculty of Dentistry, Department of Oral and Maxillofacial Surgery, Erciyes University, Erciyes, Turkey were included in the study between 2012 and 2014. Data was obtained from 885 patients records, retrospectively. Fifty patients (control group: group 1) who had no POV, and 50 patients (POV group: group 2) who had POV after tooth extraction were selected randomly. Inclusion criteria were the absence of severe organ dysfunction, no contraindication for general anesthesia, patients between the age 2-15 years, and if the patient used midazolam as premedication and propofol for maintaining the anesthesia without an anti-emetic. The exclusion criteria were severe organ dysfunction, migraine, chronic renal and liver disease, autoimmune disease, hematological problems, patients who had an allergy to the drugs, and patients who were prescribed an anti-emetic as premedication. Also, those patients needing more than 3 teeth extracted were excluded from the study.
The age, gender, duration of the operations, preoperatively routine hemogram findings such as white blood cell (WBC), hemoglobin (HGB), N/L ratio, red blood cell (RBC) count, hematocrit (HCT) levels, mean corpuscular volume (MCV), mean corpuscular hemoglobin (MCH), mean corpuscular hemoglobin concentration (MCHC), red blood cell distribution width (RDW), mean platelet volume, platelet count, and the MPV/PLT ratio were recorded for both groups.
Anesthetic protocol
A standard anesthetic sedation method was applied to all patients. All patients were premedicated intravenously with 0.1 mg/kg midazolam just before taking them to the operating room and intravenous deep sedation was applied with 1-1.5 mg/kg propofol during the tooth extraction procedure. Noninvasive monitoring procedures were applied to all the patients and supplemental oxygen (3-4 L/min) was administered via a nasal mask, in all cases, during and after the procedure. After providing an adequate level of sedation, 1-2 ml of local anesthetic solution (articaine) was applied to each tooth to be extracted. No other analgesic was used for the patients. Intraoperative fluid management consisted of administration of 5% dextrose with 0.3% saline intravenous sufficient to correct for half of the preoperative fluid deficit in the first hour, followed by according to body weight until oral intake. If vomiting occurred in the post-anesthesia care unit, patients were treated with a suitable dosage of ondansetron (DEMO S A Pharmaceutical Industry, Athens, Greece), according to the child’s weight.
Statistical analysis
Histogram and q-q plots were examined and the Shapiro-Wilk test was applied to assess data normality. Levene’s test was used for variance homogeneity. To compare the differences between groups, an independent samples t test or Mann-Whitney U test was performed. Receiver operating characteristic (ROC) curves were performed to test the predictive performances of MPV, PLT, and MPV/PLT markers to identify vomiting in pediatric patients who underwent tooth extraction under deep sedation. The areas under these curves were calculated with 95% confidence intervals and calculated each other (namey, MPV, PLT and MPV/PLT markers). The Youden index was applied to determine optimal cut-off values for each marker. Sensitivity, specificity, positive and negative predictive values, positive and negative likelihood ratios were calculated with 95% confidence intervals. The ROC analysis was applied using an easy ROC tool (http://www.biosoft.hacettepe.edu.tr/easyROC/),10 while the remaining analysis was applied in R 3.1.1 (www.r-project.org) software; p<0.05 was considered statistically significant.
Results
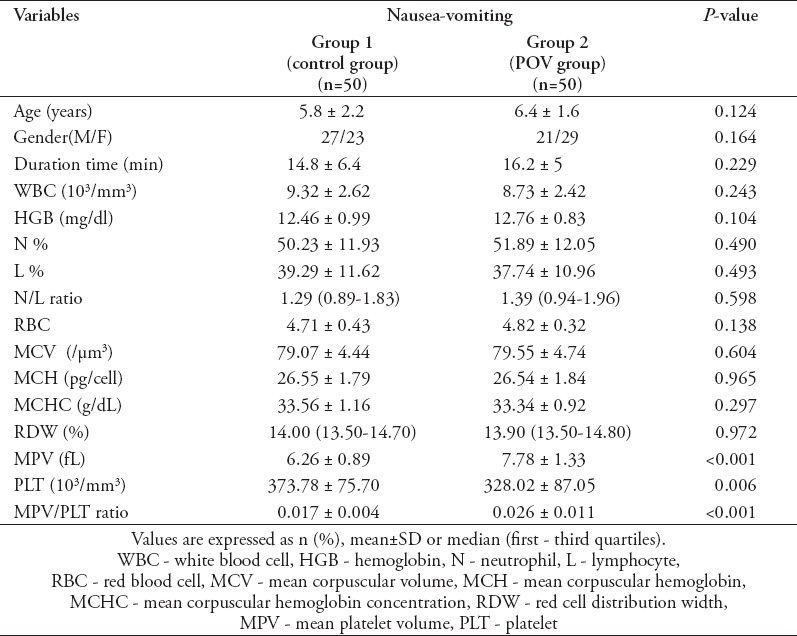
There were no statistical differences between the gender, age, and duration of surgery (p>0.05, Table 1). Also, there were no statistical differences between the groups in terms of WBC, HGB, N/L ratio, RBC, MCV, MCH, MCHC, and RDW (p>0.05, Table 1). There were significantly statistical differences between the groups in terms of MPV, PLT, and the MPV/PLT ratio (Table 1). These differences were caused by a significant increase of MPV and, therefore, in the MPV/PLT ratio in the POV group, which also occurred in the control group because of a decrease of PLT.
Table 1.
The age, gender, and preoperative hemogram parameters of 100 American Society of Anesthesiology Classification I and II pediatric patients who underwent tooth extraction procedures under a standard anesthetic method.
Receiver operating characteristic curves indicating the predictive performances of MPV, PLT, and MPV/PLT on vomiting in pediatric patients are shown in Figure 1. Area under the curve for the PLT marker was found to have significantly lower values than both MPV and MPV/PLT markers (Figure 1, p<0.05). The optimal cut-off value of MPV was determined at 6.7 fL (Figure 2).
Figure 1.
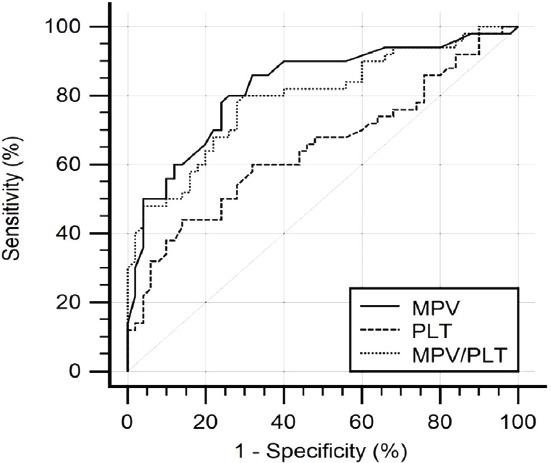
Receiver operating characteristic curves indicating the predictive performances of MPV, PLT, and MPV/PLT on vomiting in pediatric patients. Area under curves (95% confidence intervals) were 0.83 (0.74-0.91), 0.65 (0.55-0.74), and 0.79 (0.70-0.87). Area under curve for PLT marker was found significantly lower than both MPV and MPV/PLT markers (p<0.05). MPV - mean platelet volume, PLT - platelet
Figure 2.
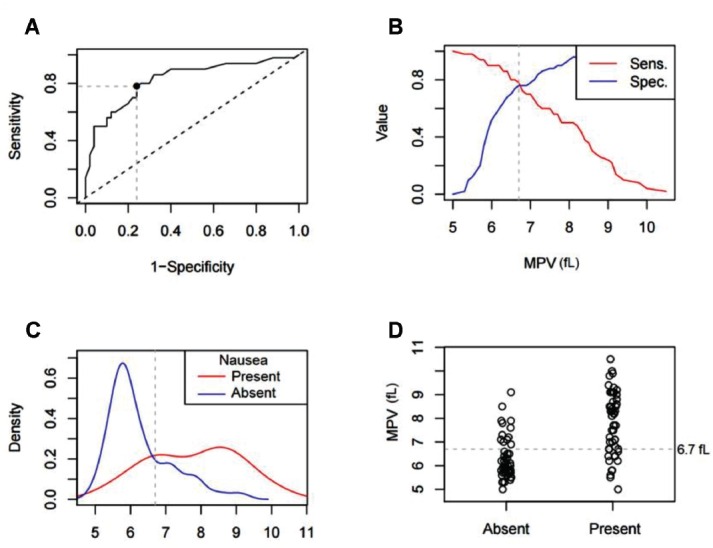
Receiver operating characteristic curves for A) mean platelet volume (MPV) = 6.7 fL, B) Sensitivity (Sens) and C) specificity (Spec) curve in identifying the optimal cut-off value. D) Distribution of MPV value in patients with or without vomiting. MPV distribution around 6.7 fL value in patients with or without vomiting
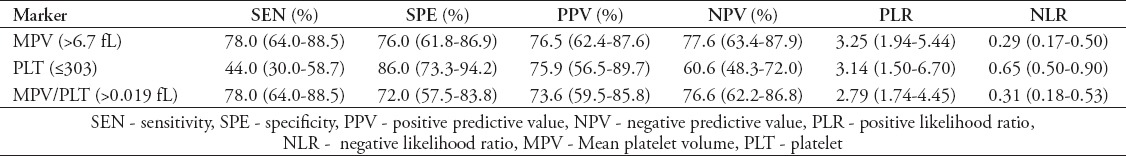
Statistical diagnostic measures of MPV, PLT, and MPV/PLT markers to identify vomiting in pediatric patients are shown in Table 2.
Table 2.
Statistical diagnostic measures for MPV, PLT, and MPV/PLT markers in identifying vomiting in pediatric patients.
Discussion
Prediction of POV is an important clinical issue for patients after oral surgery. In this retrospective study, we demonstrated preoperatively that a higher MPV value in the MPV/PLT ratio may provide additional information to predict POV risk levels in children whose tooth extraction are performed under deep sedation. Postoperative vomiting was observed in the patients with preoperative MPV values higher than 6.7 fL.
Dental anxiety complicates dental treatments in children. Management of anxious children has been one of the most encountered challenges in dentistry. Most dental procedures can be performed with non-pharmacological behavioral therapies in children. But, sometimes, anesthesia may become necessary for patients.3 Postoperative nausea and vomiting is an important and generally unavoidable problem in outpatient surgery. Postoperative nausea and vomiting impairs patient satisfaction, delays discharge and the return to normal daily activities.11 So, predicting and preventing PONV may provide better results for both patients and physicians during the perioperative period. Duration of anesthesia and type of surgery (plastic, orthopedic shoulder, ear, nose and throat or other) are independent factors that can predict PONV. Intense preoperative anxiety, using inhalation anesthetics, or opioids increases the incidence of PONV.2,3 In this study, the patients who received a standard, intravenous, deep sedation method were selected from the records, and the relationship between the POV and hemogram parameters were researched. In this study, because all children may not give the correct information on nausea, POV but not nausea was evaluated. Although preoperative characteristics of severe anxiety, age, type of anesthesia, and duration time of surgery were standard and similar for the patients investigated, POV was mostly observed in children whose preoperative MPV values were higher than 6.7 fl, and who had higher preoperative MPV/PLT ratios.
The pathogenesis of PONV is complicated and unclear; there is a 25-30% incidence today, especially in outpatient surgery.10 Several certain stimuli stemming from olfactory, visual, vestibular, and psychogenic sources can lead to nausea and vomiting. The vomiting reflex is complex and poorly understood and originates from the emetic and vomiting center. The sensory inputs of the vomiting reflex include the vagus and vestibular nerves, the limbic system, and the cemoreceptor trigger zone. Several neurotransmitters and neuromodulators activate the cemoreceptor trigger zone, which leads to nausea and vomiting by stimulating the vomiting center. Also, the oral procedures, such as the ones occurring during mouth, throat, tonsil surgery add to a potential risk of PONV due to swallowed blood in the stomach.12,13 In addition, tactile stimulation of the pharynx or inflammation or injury to the upper airway may cause to nausea and vomiting. Although perioperative suctioning of the oral cavity may remove secretions or blood and prevent swallowing, suctioning may irritate the oral cavity or throat. This can, in turn, inflame the pharynx, and the inflammation may be a reason for nausea and vomiting. Also, medication may stimulate nausea and vomiting. Less emetogenic anesthesia techniques are generally suggested to avoid PONV.13 Ortiz et al14 reported that intravenous anesthesia with propofol for induction and maintenance in pediatric outpatients undergoing surgery reduces the risk of postoperative nausea compared with inhaled anesthesia. In our study, only midazolam and propofol were used for premedication and maintenance of the chosen anesthetic. Nevertheless, POV complications observed in children after the surgery may be due to several unclear mechanisms. Pediatric patients with POV were treated with ondansterone and intravenous fluid in the postoperative period, whereas the non-POV group had taken only intravenous fluid.
According to the literature, blood parameters were used to predict several diseases. The N/L and platelet/lymphocyte ratios were reported as a simple systemic inflammatory response (SIR) marker, which may easily be evaluated by blood parameters. The N/L ratio possesses diagnostic value in certain pathologies characterized by systemic or local inflammatory responses, such as diabetes mellitus, ulcerative colitis, and inflammatory arthritis.15,16 Kutlucan et al17 reported that PLT counts and MPV remained unchanged in study subjects with metabolic syndrome, which is related to SIR. Kurt et al7 demonstrated that the N/L ratio could be used to determine severity of hyperemesis gravidarum. Hyperemesis gravidarum is a severe form of nausea and vomiting in pregnant women, and elevated serotonin level is found associated with hyperemesis gravidarum and PONV as well.18 In our study, WBC, HGB, N and L counts, N/L ratio, RBC, MCV, MCH, MCHC and RDW had similar values for both the POV and control groups. According to our results, these parameters provide predictable information for POV. But PLT, MPV, and the MPV/PLT ratio was determined as a predicting factor for POV.
Öbrink et al19 evaluated preoperative panels of platelet counts to evaluate the relationship with PONV in females undergoing breast surgery. They concluded that platelet count provided no additional information on PONV, but was associated with Apfel score, which is a measure of clinical risk. Serotonin and platelets, which are thought to be important depositories for serotonin were searched as a predicting factor of PONV.9 Oddby- Muhrbeck et al20 studied the relationship between different neuropeptides and amines (such as vasopressin, gastrin, cholecystokinin, epinephrine, norepinephrine, dopamine, serotonin, and platelet count) and PONV. They obtained a platelet count to determine plasma and whole blood serotonin levels and found 3 different platelet-related factors of PONV. They concluded that platelet count alone was not responsible for PONV. Nevertheless, due to the serotonin receptors located in the cemoreceptor trigger zone, they suggested that platelet characteristics may mirror serotonin function in the CNS, and this would carry a potential relationship between PLT count and PONV. In our study, we observed lower preoperative blood values of PLT and higher MPV values and MPV/PLT ratio in the POV group. A 6.7 fL cut-off level of MPV was determined to be a predicting factor for POV. Although Öbrink et al19 reported a negative correlation between PLT, MPV, and PONV in women undergoing breast cancer surgery. We observed a positive correlation with MPV and the MPV/PLT ratio and a negative correlation with PLT count in a different patient population, which consisted of children undergoing tooth extraction under deep sedation. This result was quite remarkable and supported our hypothesis. In addition, MPV has been reported as a marker of PLT function and activation. It is known that large platelets are hemostatically more active.21 Thus, it could be thought that more active platelets, which present higher MPV, may lead to greater serotonin release; thereby, POV. Platelet count, MPV, and the MPV/PLT ratio may alert anesthesiologists about POV in preoperative visits with patients and lead them to use anti-emetics for premedication in clinical practice.
Study limitations
This is a retrospective study, some records did not adequately determine vomiting.
Postoperative nausea and vomiting is mostly an undesirable, unavoidable complication in the postoperative period. The mechanism and pathophysiology of PONV is quite complex and is not completely understood. Improving possible objective markers for predicting PONV may be useful for the anesthesiologists and surgeons. Our results demonstrated that values of PLT, MPV, and PLT/MPV ratio are cheap markers and may help predict POV in children. Further comprehensive studies are needed with homogeneous patient populations.
Footnotes
References
- 1.Choi SU. Is postoperative nausea and vomiting still the big “little” problem? Korean J Anesthesiol. 2016;69:1–2. doi: 10.4097/kjae.2016.69.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chatterjee S, Rudra A, Sengupta S. Current concepts in the management of postoperative nausea and vomiting. Anesthesiol Res Pract. 2011;2011:748031. doi: 10.1155/2011/748031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ashley PF, Williams CE, Moles DR, Parry J. Sedation versus general anaesthesia for provision of dental treatment to patients younger than 18 years. Cochrane Database Syst Rev. 2015;28:CD006334. doi: 10.1002/14651858.CD006334.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Duksal F, Alaygut D, Güven AS, Erkocoglu M, Demircioglu F. Neutrophil/lymphocyte and C-reactive protein/mean platelet volume ratios indifferentiating between viral and bacterial pneumonias and diagnosing early complications in children. Saudi Med J. 2014;35:442–447. [PubMed] [Google Scholar]
- 5.Boyraz I, Koç B, Boyacı A, Tutoğlu A, Sarman H, Ozkan H. Ratio of neutrophil/lymphocyte and platelet/lymphocyte in patient with ankylosing spondylitis that are treating with anti-TNF. Int J Clin Exp Med. 2014;7:2912–2915. [PMC free article] [PubMed] [Google Scholar]
- 6.Celikbilek A, Zararsiz G, Atalay T, Tanik N. Red cell distribution width in migraine. Int J Lab Hematol. 2013;35:620–628. doi: 10.1111/ijlh.12100. [DOI] [PubMed] [Google Scholar]
- 7.Kurt RK, Güler A, Silfeler DB, Ozçil MD, Karateke A, Hakverdi AU. Relation of inflammatory markers with both presence and severity of hyperemesis gravidarum. Ginekol Pol. 2014;85:589–593. doi: 10.17772/gp/1776. [DOI] [PubMed] [Google Scholar]
- 8.Cubeddu LX, Hoffmann IS, Fuenmayor NT, Finn AL. Efficacy of ondansetron (GR38032F) and the role of serotonin in cisplatin-induced nausea and vomiting. N Engl J Med. 1999;322:810–816. doi: 10.1056/NEJM199003223221204. [DOI] [PubMed] [Google Scholar]
- 9.Xiao R, Beck O, Hjemdahl P. On the accurate measurement of serotonin in whole blood. Scand J Clin Lab Invest. 1998;58:505–510. doi: 10.1080/00365519850186319. [DOI] [PubMed] [Google Scholar]
- 10.Hacettepe University Department of Biostatistics. Biosoft Project. [Cited 2014]. Available from URL: http://www.biosoft.hacettepe.edu.tr/index.html .
- 11.Cruthirds D, Sims PJ, Louis PJ. Review and recommendations for the prevention, management, and treatment of postoperative and postdischarge nausea and vomiting. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;115:601–611. doi: 10.1016/j.oooo.2012.09.088. [DOI] [PubMed] [Google Scholar]
- 12.Kovac AL. Prevention and treatment of postoperative nausea and vomiting. Drugs. 2000;59:213–243. doi: 10.2165/00003495-200059020-00005. [DOI] [PubMed] [Google Scholar]
- 13.Thompson HJ. The management of post-operative nausea and vomiting. J Adv Nurs. 1999;29:1130–1136. doi: 10.1046/j.1365-2648.1999.00998.x. [DOI] [PubMed] [Google Scholar]
- 14.Ortiz AC, Atallah AN, Matos D, da Silva EM. Intravenous versus inhalational anaesthesia for paediatric outpatient surgery. Cochrane Database Syst Rev. 2014;7:2. doi: 10.1002/14651858.CD009015.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Celikbilek M, Dogan S, Ozbakır O, Zararsız G, Kücük H, Gürsoy S, et al. Neutrophil-lymphocyte ratio as a predictor of disease severity in ulcerative colitis. J Clin Lab Anal. 2013;27:72–76. doi: 10.1002/jcla.21564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Imtiaz F, Shafique K, Mirza SS, Ayoob Z, Vart P, Rao S. Neutrophil lymphocyte ratio as a measure of systemic inflammation in prevalent chronic diseases in Asian population. Int Arch Med. 2012;5:2. doi: 10.1186/1755-7682-5-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kutlucan A, Bulur S, Kr S, Bulur S, Önder E, Aslantaş Y, et al. The relationship between mean platelet volume with metabolic syndrome in obese individuals. Blood Coagul Fibrinolysis. 2012;23:388–390. doi: 10.1097/MBC.0b013e328352e8fa. [DOI] [PubMed] [Google Scholar]
- 18.Cengiz H, Dagdeviren H, Caypinar SS, Kanawati A, Yildiz S, Ekin M. Plasma serotonin levels are elevated in pregnant women with hyperemesis gravidarum. Arch Gynecol Obstet. 2015;291:1271–1276. doi: 10.1007/s00404-014-3572-2. [DOI] [PubMed] [Google Scholar]
- 19.Öbrink E, Eksborg S, Lönnqvist PA, Jakobsson JG. Preoperative platelet count and volume could not help predict PONV in women undergoing breast cancer surgery: A prospective cohort study. Int J Surg. 2015;18:128–131. doi: 10.1016/j.ijsu.2015.03.006. [DOI] [PubMed] [Google Scholar]
- 20.Oddby-Muhrbeck E, Eksborg S, Helander A, Bjellerup P, Lindahl S, Lönnqvist P. Blood-borne factors possibly associated with post-operative nausea and vomiting: an explorative study in women after breast cancer surgery. Acta Anaesthesiol Scand. 2005;49:1346–1354. doi: 10.1111/j.1399-6576.2005.00836.x. [DOI] [PubMed] [Google Scholar]
- 21.Chesnutt JK, Han HC. Platelet size and density affect shear-induced thrombus formation in tortuous arterioles. Phys Biol. 2013;10:056003. doi: 10.1088/1478-3975/10/5/056003. [DOI] [PMC free article] [PubMed] [Google Scholar]


