Abstract
Introduction
Discussions about sexual health are uncommon in clinical encounters, despite the sexual dysfunction associated with many common health conditions. Understanding of the importance of sexual health and sexual satisfaction among US adults is limited.
Aim
To provide epidemiologic data on the importance of sexual health for quality of life and people’s satisfaction with their sex lives and to examine how each is associated with demographic and health factors.
Methods
Data are from a cross-sectional, self-report questionnaire from a sample of 3515 English-speaking US adults recruited from an online panel that uses address-based probability sampling.
Main Outcome Measures
We report ratings of importance of sexual health to quality of life (single item with 5-point response) and the PROMIS® Satisfaction with Sex Life score (5 items, each with 5-point responses, scores centered on the US mean).
Results
High importance of sexual health to quality of life was reported by 62.2% of men (95% CI, 59.4%–65.0%) and 42.8% of women (95% CI, 39.6%–46.1%; P < .001). Importance of sexual health varied by sex, age, sexual activity status, and general self-rated health. For the 55% of men and 45% of women who reported sexual activity in the previous 30 days, satisfaction with sex life differed by sex, age, race/ethnicity (among men only), and health. Men and women in excellent health had significantly higher satisfaction than participants in fair or poor health. Women with hypertension reported significantly lower satisfaction (especially younger women), as did men with depression or anxiety (especially younger men).
Conclusion
In this large study of US adults’ ratings of the importance of sexual health and satisfaction with sex life, sexual health was a highly important aspect of quality of life for many participants, including participants in poor health. Moreover, participants in poorer health reported lower sexual satisfaction. Accordingly, sexual health should be a routine part of clinicians’ assessments of their patients. Health care systems that state a commitment to improving patients’ overall health must have resources in place to address sexual concerns. These resources should be available for all patients across the life span.
Keywords: Quality of Life, Self-Report, Sexual Behavior, Cross-Sectional Studies, Male, Female
Introduction
It has been over 15 years since Laumann et al1 identified sexual dysfunction as an “important public health concern” in the pages of JAMA. Many common health conditions and their treatments are associated with sexual dysfunction, including diabetes, hypertension, coronary artery disease, cancer, anxiety, and depression.2 Despite the high prevalence of these conditions, discussions about sexual health are uncommon in clinical encounters, perhaps in part due to underlying assumptions that sexual health is not a priority.3–8 Patients may assume their clinicians will tell them if sexual side effects are associated with a disease or its treatments; clinicians may assume patients will initiate discussions about sexual health if it is important to them. In a study of older adults (ages 57–85), Lindau et al9 found that relatively few rated sex as unimportant. Yet, our understanding of the importance of sexual health for people of all ages and in various health states remains limited.
Moreover, while many studies have examined risk factors for specific sexual problems10 less is known about individuals’ global evaluations of sexual satisfaction and whether satisfaction differs by demographic and health characteristics. Multiple factors interact to determine sexual satisfaction, including but not limited to culturally influenced expectations about sex and sexuality,11 sexual communication and sexual practices within couples,12,13 and, in a study limited to older women, age, race/ethnicity, and mental health.14 Conceptually related to satisfaction (though not equivalent), bother or distress about sexual dysfunction appears to increase both men’s and women’s willingness to discuss a sexual problem with a physician, and in women also drives decisions to seek treatment.15
A better understanding of the importance of sexual health to quality of life and global evaluations of sexual satisfaction in diverse populations is needed to help guide future research efforts, including the development of interventions to enhance patient-provider communication about sexual concerns associated with common conditions and their treatments.. To this end, this study sought to provide epidemiologic data on the importance of sexual health to quality of life and sexual satisfaction among a large sample of diverse US adults and to examine how each is associated with sex, age, race/ethnicity, and health factors.
Methods
Study Population
Data for this study were collected during testing of version 2.0 of the Patient-Reported Outcomes Measurement Information System® (PROMIS®) Sexual Function and Satisfaction (SexFS) measure in a large, cross-sectional, population-based sample of US adults in KnowledgePanel® (GfK). The panel is an address-based probability sample drawn from the US Postal Service Computerized Delivery Sequence File, which includes 97% of households in the United States. Selected panel members who do not have a computer with Internet access are provided with one.
In June 2013, after a pilot test in a convenience sample of 30 participants, 10,129 English-speaking panel members 18 years or older were invited to participate in our survey. Of those, 4443 (43.9%) viewed the informed consent form, which included the description, “The study will help researchers understand how illness affects different areas of people’s lives, particularly their sex lives.” Of those who viewed the consent form, 3667 (82.5%) consented to participate and 3515 (95.9%) completed the survey. A target sample size of 3500 participants was based on previously planned psychometric analyses for measure development. However, this sample size also provided sufficient statistical power for the multivariable modeling presented here. With a sample size of 3500 equally allocated in 2 groups, we had greater than 90% statistical power to detect a difference in 2 proportions of 0.06 or less and greater than 90% statistical power to detect a less than 1.1 point difference in T-scores between 2 means.
The self-administered online questionnaire included approximately 177 items. Skip patterns determined the particular set of items participants received depending on their sex and sexual activity status. Content included all candidate items for the SexFS version 2.0 and items capturing sociodemographic and health characteristics. For a survey of this length, KnowledgePanel participants receive an incentive equivalent to $6. The institutional review board of the XXXXX approved the study, and all participants provided informed consent.
Variables
Importance of sexual health was measured with an item we developed that asked, “How important is sexual health to your quality of life?” Response options include “not at all,” “a little bit,” “somewhat,” “quite a bit,” and “very.” We considered modeling importance as ordinal using ordinal logistic regression or even as continuous using simple linear regression, but a chi-square score test showed significant violation of the proportional odds assumption (P < .0001) within an ordinal logistic regression model, signaling that the response increments are not linear with respect to the covariates. Thus, for use in the models and presentation in the tables, we dichotomized responses into high importance (ie, “quite a bit” or “very”) and low importance (ie, “not at all,” “a little bit,” or “somewhat”).
Sexual satisfaction was measured using the PROMIS SexFS version 2.0 Satisfaction With Sex Life scale.16 The PROMIS SexFS is a state-of-the-art, patient-reported outcome measure developed using robust qualitative and quantitative methods.16–22 The satisfaction scale includes 5 items to assess how satisfying and pleasurable the person regards his or her sex life in the past 30 days, with no limitation on how the person defines “sex life.” Internal consistency reliability is high in the US general population (Cronbach’s alpha = 0.94). The scale is scored on the T-metric, with a score of 50 centered on the mean for sexually active US adults and an SD of 10 points. Higher scores indicate greater satisfaction.
We modeled age as a continuous variable. Sexual activity status was based on an item that asked whether the respondent had any type of sexual activity (ie, masturbation, oral sex, or sexual intercourse) in the previous 30 days. Race and ethnicity data were captured by 2 questions (consistent with the reporting requirements of the National Institutes of Health) but combined into a single variable with 4 categories for the analysis due to small numbers in some categories. Data on health conditions were captured by questions asking whether a doctor or other health care provider had ever told the respondent they had the condition, except in the case of hypertension, for which the participant was asked whether they currently had high blood pressure. General self-rated health was measured with a single item (ie, “In general, would you say your health is excellent, very good, good, fair, or poor?”). This item is a predictor of mortality; in a meta-analysis of 22 studies, poor self-rated health was associated with a twofold higher risk of mortality than excellent health.23 We treated general self-rated health as a categorical variable in the models, combining “fair” and “poor” health because of small numbers.
Statistical Analysis
We weighted the data to approximate the English-speaking US adult population with respect to sex, age, race/ethnicity, education level, and geographic region. We report percentages of participants who indicated high importance of sexual health with 95% CIs by sex, sexual activity status, race/ethnicity, and health. We used local regression (LOESS) curves to describe relationships between importance and age separately by sex. We modeled relationships between importance of sexual health and age, sexual activity status, race/ethnicity, and health using logistic regression with adjustment for the complex survey design. We conducted an omnibus likelihood ratio test of all 2-way interactions between age and sexual activity status with each other and with the rest of the race/ethnicity and health variables. When the omnibus test was statistically significant, we used a likelihood ratio test for each individual interaction and added the significant interactions to the models. However, to ease interpretation of the results, we retained interactions in the final models only if they remained significant. Graphical diagnostics suggested that age was better modeled by adding a quadratic term (ie, age2), so we included both a linear term and a quadratic term in all analyses involving age.
The analysis of satisfaction with sex life followed the same approach as the analysis of importance, except that we analyzed satisfaction scores as continuous scores and restricted the analysis to respondents who reported engaging in sexual activity in the previous 30 days. We also tested a cubic term for age (ie, age3), but the model fit best with the quadratic term. We report means and corresponding 95% CIs for the satisfaction scores; relationships to other variables are based on a multivariable general linear model.
We included specific health conditions in the models, as well as general self-rated health, to capture aspects of health not covered by the particular diagnoses and to serve as a broader indicator of health status. However, we were concerned that the general self-rated health variable might obscure the effects of the individual diagnoses, as an individual’s rating of overall health may be based in part on diagnosed conditions. Therefore, in a sensitivity analysis, we estimated the models after removing the general self-rated health variable. In the Results section, we indicate when results were different between the 2 models. For all analyses, we considered a 2-tailed α level of 0.05 to be significant.
Results
The study population was weighted to approximate the US population, and their demographic and health characteristics are summarized in Table 1.
Table 1.
Characteristics of the Study Sample by Sex and Sexual Activity Status
| Characteristic | Sexually Active in the Past 30 Days |
Not Sexually Active in the Past 30 Days |
||
|---|---|---|---|---|
| Women (n = 1202) |
Men (n = 1463) |
Women (n = 536) |
Men (n = 272) |
|
| Age, mean (SD), y | 43.7 (16.6) | 45.0 (15.1) | 54.8 (19.3) | 52.5 (19.3) |
| Race/ethnicity, No. (%)a | ||||
| Asian, non-Hispanic | 37 (3.1) | 63 (4.3) | 17 (3.2) | 12 (4.3) |
| Black or African American, non-Hispanic | 159 (13.2) | 146 (10.0) | 62 (11.6) | 35 (12.8) |
| White, non-Hispanic | 815 (67.8) | 995 (68.0) | 380 (71.0) | 190 (69.7) |
| Multiple or other races, non-Hispanic | 153 (12.7) | 39 (2.7) | 52 (9.8) | 11 (3.9) |
| Hispanic or Latino ethnicity | 153 (12.7) | 219 (15) | 52 (9.8) | 25 (9.3) |
| Health conditions, No. (%)a | ||||
| Arthritis or rheumatism | 238 (20.1) | 202 (14.1) | 185 (35.1) | 55 (21.1) |
| Cancer | 51 (4.3) | 55 (3.9) | 62 (11.7) | 30 (11.6) |
| Coronary artery disease or heart disease | 72 (6.0) | 143 (9.8) | 63 (11.7) | 45 (16.7) |
| Depression or anxiety | 290 (24.2) | 248 (17.3) | 168 (31.8) | 45 (16.9) |
| Diabetes mellitus (Type 1 or 2) | 127 (10.7) | 142 (9.9) | 85 (16.3) | 45 (17.3) |
| Hypertension | 230 (19.3) | 380 (26.7) | 200 (37.8) | 77 (29.3) |
| General self-rated health, No. (%)a | ||||
| Excellent | 221 (18.7) | 272 (19.0) | 62 (11.9) | 47 (17.9) |
| Very good | 461 (38.8) | 567 (39.6) | 160 (30.6) | 80 (30.3) |
| Good | 330 (27.8) | 422 (29.4) | 190 (36.3) | 67 (25.2) |
| Fair | 143 (12.1) | 147 (10.3) | 88 (16.8) | 54 (20.4) |
| Poor | 31 (2.6) | 24 (1.7) | 23 (4.5) | 16 (6.2) |
Percentages are weighted to approximate the US population.
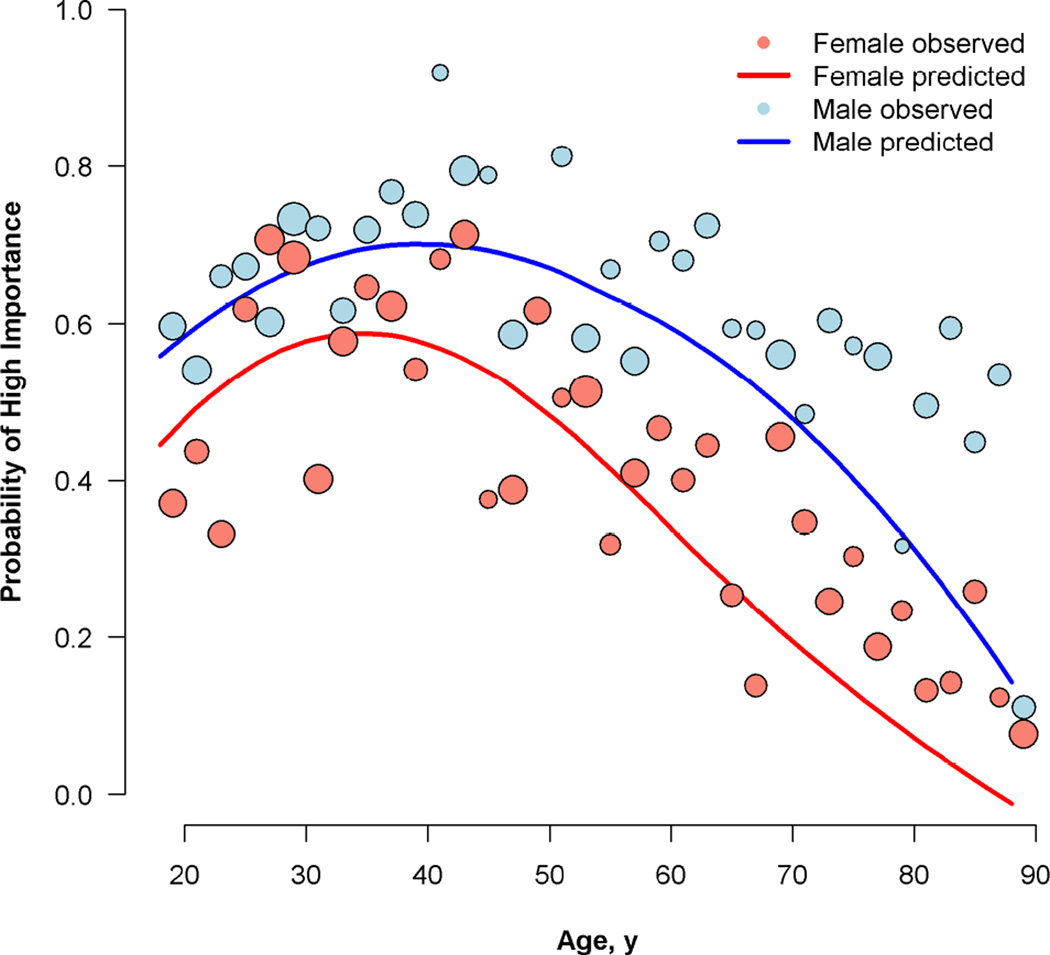
Overall, high importance of sexual health to quality of life was reported by 62.2% of men (95% CI, 59.4%–65.0%) and 42.8% of women (95% CI, 39.6%–46.1%; P < .001). Across all characteristics, importance of sexual health was high for over 50% of sexually active men and 40% of sexually active women (Table 2). Among participants who were not sexually active, fewer reported high importance. The Figure shows the observed relationships between age and the likelihood of rating sexual health as highly important. The apparent curvilinear relationship between age and high importance suggests that more participants in their mid-30s to mid-40s endorsed high importance than either younger or older participants.
Table 2.
High Importance of Sexual Health and Satisfaction With Sex Life Scores Among US Adults
| Characteristic | Sexual Health Very or Quite Important to Quality of Life, Percent (95% CI)a |
Satisfaction With Sex Life, Mean Score (95% CI)b |
||||
|---|---|---|---|---|---|---|
| Sexually Active in the Past 30 Days |
Not Sexually Active in the Past 30 Days |
Sexually Active in the Past 30 Days |
||||
| Women | Men | Women | Men | Women | Men | |
| All participants | 57.0 (53.1–60.9) | 67.6 (64.6–70.5) | 10.7 (7.0–14.4) | 32.7 (25.4–39.9) | 49.1 (48.3–20.0) | 50.7 (50.1–51.4) |
| Race/ethnicity | ||||||
| Black, non-Hispanic | 55.1 (42.9–67.4) | 74.0 (63.4–84.5) | 15.9 (5.1–26.8) | 35.5 (17.7–53.3) | 50.5 (48.1–52.8) | 53.6 (51.3–55.9) |
| White, non-Hispanic | 55.7 (51.3–60.0) | 64.6 (61.2–68.0) | 7.4 (4.1–10.8) | 26.3 (18.9–33.8) | 48.8 (47.9–49.6) | 50.3 (49.6–51.0) |
| Other, non-Hispanic | 59.6 (41.3–77.9) | 59.2 (46.8–71.5) | 29.2 (5.9–52.4) | 63.2 (31.6–94.9) | 50.9 (45.7–56.0) | 49.6 (47.5–51.7) |
| Hispanic or Latino | 64.5 (52.0–76.9) | 81.2 (73.7–88.8) | 14.5 (0.0–32.1) | 58.0 (27.5–88.6) | 48.7 (45.8–51.6) | 51.3 (49.2–53.4) |
| Health conditions | ||||||
| Hypertension | ||||||
| No | 57.8 (53.4–62.2) | 70.2 (66.8–73.6) | 13.2 (7.8–18.5) | 35.6 (26.5–44.7) | 49.4 (48.4–50.3) | 51.6 (50.9–52.4) |
| Yes | 52.5 (43.9–61.2) | 59.8 (53.9–65.7) | 6.7 (2.8–10.6) | 25.8 (15.3–36.2) | 48.1 (46.4–49.9) | 48.5 (47.3–49.7) |
| Coronary artery disease or heart disease | ||||||
| No | 58.0 (53.9–62.0) | 68.8 (65.7–71.9) | 10.7 (6.7–14.6) | 33.8 (25.5–42.0) | 49.2 (48.4–50.1) | 51.3 (50.6–51.9) |
| Yes | 41.8 (27.4–56.2) | 56.3 (46.6–66.0) | 11.0 (0.3–21.7) | 27.4 (13.6–41.3) | 47.4 (44.5–50.3) | 46.0 (43.9–48.1) |
| Arthritis or rheumatism | ||||||
| No | 59.5 (55.1–63.9) | 67.7 (64.5–70.9) | 13.5 (8.3–18.8) | 36.0 (27.4–44.5) | 49.7 (48.8–50.7) | 51.3 (50.6–52.0) |
| Yes | 47.8 (39.6–56.1) | 66.2 (58.9–73.5) | 5.6 (2.0–9.3) | 22.0 (10.0–33.9) | 47.0 (45.3–48.8) | 47.6 (45.9–49.3) |
| Diabetes mellitus (Type 1 or 2) | ||||||
| No | 57.4 (53.3–61.5) | 68.3 (65.2–71.4) | 11.3 (7.1–15.6) | 34.9 (26.6–43.2) | 49.1 (48.3–50.0) | 51.2 (50.5–51.9) |
| Yes | 54.3 (41.5–67.1) | 60.5 (51.1–69.9) | 8.1 (1.7–14.5) | 24.1 (10.8–37.5) | 49.2 (46.6–51.8) | 47.3 (45.3–49.3) |
| Depression or anxiety | ||||||
| No | 55.7 (51.2–60.3) | 67.1(63.8–70.4) | 10.1 (5.9–14.3) | 30.3 (22.4–38.3) | 49.5 (48.5–50.5) | 51.6 (50.9–52.3) |
| Yes | 60.8 (53.4–68.2) | 69.9(63.3–76.5) | 12.0 (4.9–19.2) | 42.3 (25.1–59.5) | 48.1 (46.5–49.7) | 46.7 (45.3–48.1) |
| Cancer | ||||||
| No | 57.3 (53.2–61.3) | 68.1(65.0–71.1) | 10.4 (6.7–14.2) | 34.1 (26.2–42.0) | 49.1 (48.3–50.0) | 51.0 (50.3–51.6) |
| Yes | 44.6 (28.3–60.8) | 53.9(40.9–67.0) | 12.9 (0.0–26.8) | 17.9 (2.6–33.1) | 49.9 (46.4–53.3) | 46.6 (44.4–48.8) |
| General self-rated health | ||||||
| Excellent | 70.0 (61.3–78.7) | 74.2 (67.6–80.7) | 14.9 (0.3–29.4) | 30.1 (15.5–44.7) | 53.4 (51.6–55.3) | 54.9 (53.1–56.0) |
| Very good | 62.7 (56.8–68.6) | 72.1 (67.6–76.5) | 11.7 (4.2–19.3) | 44.0 (29.1–58.8) | 49.9 (48.6–51.2) | 52.5 (51.5–53.4) |
| Good | 44.5 (37.2–51.7) | 59.7 (54.1–65.3) | 7.3 (3.1–11.6) | 27.6 (12.5–42.7) | 47.5 (46.0–48.9) | 48.5 (47.6–49.4) |
| Fair/poor | 51.2 (40.3–62.0) | 61.8 (52.5–71.1) | 11.8 (4.0–19.6) | 27.0 (15.7–38.3) | 45.2 (43.0–47.4) | 44.7 (42.6–46.9) |
Item: “How important is sexual health to your quality of life?” Response options: “Not at all,” “A little bit,” “Somewhat,” “Quite a bit,” and “Very.”
PROMIS Satisfaction With Sex Life score. The US mean score is 50 (SD, 10).
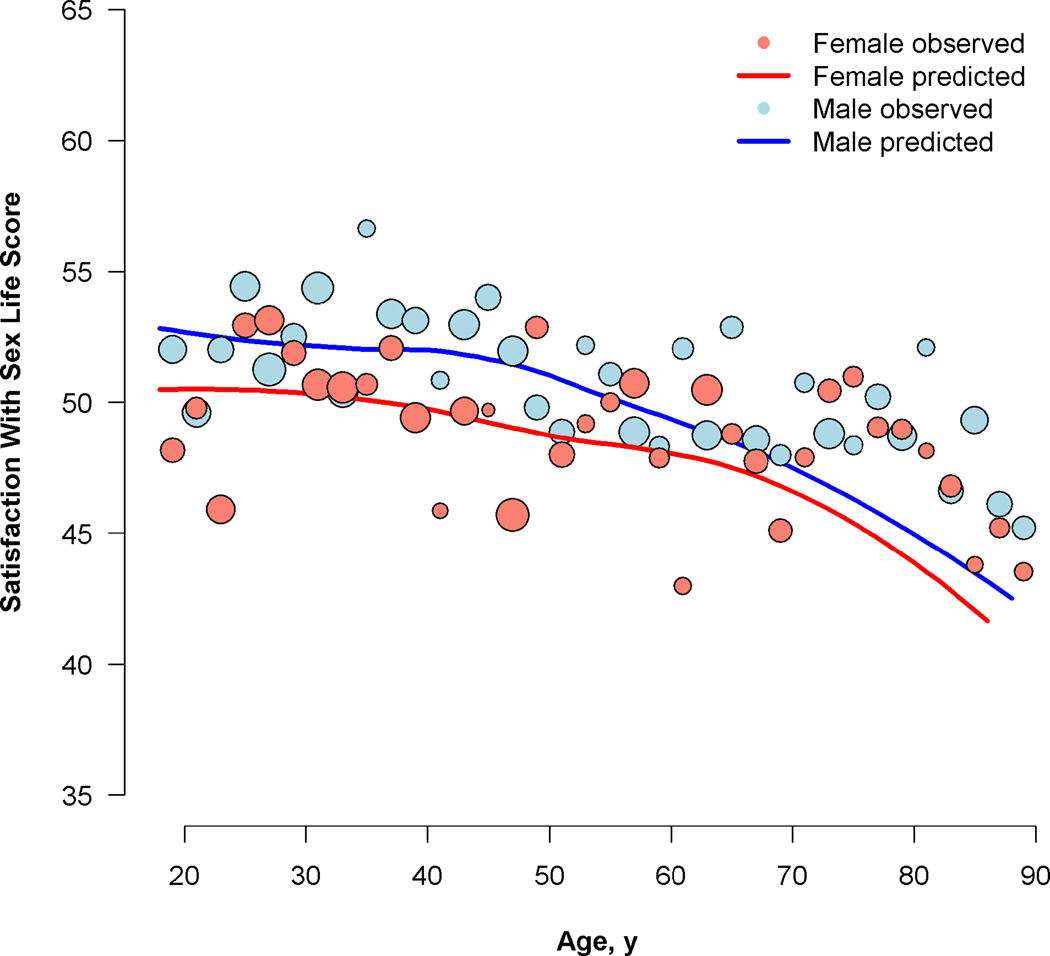
Figure.
Probability of High Importance (A) and Satisfaction With Sex Life (B) Scores for US Men and Women by Age
Note: In panel A, the circles represent the proportion of participants who rated the importance of sexual health as high. In panel B, the circles represent the mean satisfaction scores in each 2-year age bin. The size of the plotted bubbles is proportional to the weighted count of observations. The local regression (LOESS) curve of the model-predicted values comes from the final model, which included all covariates.
In the multivariable model of the importance of sexual health for women, the omnibus test of all 2-way interactions involving age and sexual activity status was statistically significant (P = .005); however, no individual interaction term was significant in the final multivariable model. Age, sexual activity status, and general self-rated health were statistically significant in the final multivariable logistic regression model (Table 3 and Figure panel A). The likelihood of reporting high importance of sexual health was greater among women who were sexually active than among women who were not. Fewer women who rated themselves in good, fair, or poor health rated importance of sexual health as high, compared with those who reported excellent health, consistent with the pattern of results in the unadjusted analysis (Table 2). In the sensitivity analysis that removed global self-rated health from the model, the pattern of findings remained the same.
Table 3.
Adjusted Odds of Reporting High Importance of Sexual Health Among US Adults
| Characteristic | High Importance of Sexual Health to Quality of Life, Adjusted Odds Ratio (95% CI)a |
|||
|---|---|---|---|---|
| Womenb |
P Value |
Menb |
P Value |
|
| Age | Not applicable | .02 | Not applicable | < .001 |
| Age2 | Not applicable | .002 | Not applicable | < .001 |
| Sexually active | 8.85 (5.78–13.51) | < .001 | 3.34 (2.27–4.95) | < .001 |
| Race/ethnicity | .22c | .003c | ||
| Black, non-Hispanic | 1.04 (0.62–1.76) | .88 | 1.46 (0.90–2.37) | .12 |
| White, non-Hispanic | 1.00 [Reference] | — | 1.00 [Reference] | — |
| Other, non-Hispanic | 2.12 (0.99–4.53) | .05 | 0.97 (0.52–1.81) | .93 |
| Hispanic or Latino | 1.31 (0.77–2.21) | .32 | 2.40 (1.46–3.95) | < .001 |
| Health conditions | ||||
| Arthritis or rheumatism | 0.82 (0.55–1.22) | .33 | 1.31 (0.92–1.87) | .13 |
| Cancer | 0.98 (0.48–1.98) | .95 | 0.73 (0.43–1.21) | .22 |
| Coronary artery disease or heart disease | 0.94 (0.49–1.81) | .85 | 0.88 (0.58–1.33) | .54 |
| Depression or anxiety | 1.40 (0.98–2.01) | .07 | 1.39 (0.99–1.97) | .06 |
| Diabetes mellitus (Type 1 or 2) | 0.98 (0.59–1.64) | .95 | 0.95 (0.63–1.42) | .80 |
| Hypertension | 1.24 (0.81–1.89) | .32 | 0.76 (0.55–1.04) | .09 |
| General self-rated health | < .001c | .002c | ||
| Excellent | 1.00 [Reference] | — | 1.00 [Reference] | — |
| Very good | 0.75 (0.48–1.17) | .21 | 1.07 (0.73–1.57) | .73 |
| Good | 0.36 (0.22–0.58) | < .001 | 0.59 (0.40–0.88) | .01 |
| Fair/poor | 0.50 (0.27–0.91) | .03 | 0.61 (0.37–1.01) | .05 |
Response of “very” or “quite a bit” to the item, “How important is sexual health to your quality of life?”
Listwise deletion of incomplete cases reduced the number of observations in these models by 4% for women and 6% for men.
Type 3 P value.
In the multivariable model of the importance of sexual health for men, the omnibus test of all 2-way interactions involving age and sexual activity status was not statistically significant (P = .21). Age, sexual activity status, race/ethnicity, and general self-rated health were statistically significant in the final model (Table 3 and Figure panel A). The patterns of results for age, sexual activity status, and general self-rated health were roughly the same as those for women. In addition, the likelihood of rating the importance of sexual health as high varied by race/ethnicity, such that the odds of rating importance as high was more than 2 times higher among Hispanic or Latino men compared with white non-Hispanic men (odds ratio [OR], 2.40; 95% CI, 1.46–3.95) and other non-Hispanic men (OR, 2.47; 95% CI, 1.14–5.34; data not shown). The difference between Hispanic men and black non-Hispanic men was not statistically significant, nor were any other comparisons among men by race/ethnicity. In the sensitivity analysis that removed global self-rated health from the model, hypertension was related to lower odds of rating importance of sexual health as high (OR, 0.69; 95% CI, 0.51–0.95).
On average, sexually active women reported Satisfaction With Sex Life scores of 49.1 (95% CI, 48.3–50.0), and sexually active men reported scores of 50.7 (95% CI, 50.1–51.4; P = .002). Table 2 shows the mean satisfaction scores for sexually active participants by sex and by each race/ethnicity and health variable. The circles in Figure panel B show the observed relationships between age and satisfaction by sex; the relationships were not strictly linear.
In the multivariable model of satisfaction for women (Table 4), the omnibus test for all 2-way interactions with age was statistically significant (P < .001). In the final model, the interaction between age and hypertension remained significant. At age 25 years, women with hypertension had estimated satisfaction scores 9 points (ie, almost 1 SD) lower (mean score, 44.0; 95% CI, 39.1–48.9) than women without hypertension (mean score, 53.0; 95% CI, 49.6–56.3). At age 45 years, there was no difference in scores by hypertension status. At age 65 years, women with hypertension had higher satisfaction scores (mean score, 52.8; 95% CI, 49.8–55.7) than women without hypertension (mean score, 48.8; 95% CI, 45.4–52.2), although the CIs overlapped substantially. Satisfaction was lower among women with worse general self-rated heath, such that women in very good health had predicted satisfaction scores 3.5 points lower, women in good health had scores 5.7 points lower, and women in fair/poor health had scores nearly 9 points lower than women in excellent health. In the sensitivity analysis, removing general self-rated health did not change the pattern of results.
Table 4.
Adjusted Satisfaction With Sex Life Among Sexually Active US Adults
| Characteristic | Satisfaction with Sex Life, Coefficient (SE) |
|||
|---|---|---|---|---|
| Womenb |
P Value |
Menb |
P Value |
|
| Age | 0.14 (0.17) | .43 | 0.12 (0.12) | .25 |
| Age2 | −0.003 (0.002) | .16 | −0.002 (0.001) | .08 |
| Race/ethnicity | .16c | .008c | ||
| Black, non-Hispanic | 2.41 (1.28) | .06 | 2.90 (1.04) | .005 |
| White, non-Hispanic | 1.00 | — | 1.00 | — |
| Other, non-Hispanic | 3.05 (2.25) | .18 | −1.64 (1.02) | .11 |
| Hispanic or Latino | −0.22 (1.51) | .88 | 0.26 (1.00) | .80 |
| Health conditions | ||||
| Arthritis or rheumatism | −0.87 (1.06) | .41 | 0.05 (0.94) | .96 |
| Cancer | 2.70 (1.76) | .13 | −1.20 (1.23) | .33 |
| Coronary artery or heart disease | 0.36 (1.65) | .83 | −1.34 (1.13) | .24 |
| Depression or anxiety | −0.33 (0.93) | .73 | −16.31 (6.42) | .01 |
| Diabetes mellitus (Type 1 or 2) | 2.44 (1.31) | .06 | 0.13 (1.16) | .91 |
| Hypertension | −27.02 (8.04) | < .001 | 0.11 (0.74) | .88 |
| General self-rated health | < .001c | <.001c | ||
| Excellent | 1.00 | — | 1.00 | — |
| Very good | −3.46 (1.13) | .002 | −1.19 (0.87) | .17 |
| Good | −5.72 (1.21) | < .001 | −4.84 (0.92) | < .001 |
| Fair/poor | −8.88 (1.66) | < .001 | −7.82 (1.43) | < .001 |
| Age*hypertension | 0.87 (0.34) | .009 | NA | — |
| Age2*hypertension | −0.006 (0.003) | .07 | NA | — |
| Age*depression or anxiety | NA | — | 0.54 (0.27) | .05 |
| Age2*depression or anxiety | NA | — | −0.005 (0.003) | .07 |
| Intercept | 52.30 (3.65) | < .001 | 53.54 (2.70) | < .001 |
PROMIS Satisfaction with Sex Life score. The US mean score is 50 (SD, 10).
Listwise deletion of incomplete cases reduced the number of observations in the models by 4% for women and 5% for men.
Type 3 P value
In the multivariable model of satisfaction for men, the omnibus test for all 2-way interactions with age was statistically significant (P = .03). In the final model, the interaction between age and depression or anxiety remained significant (P = .05), and the difference between men with and without depression or anxiety was more pronounced among younger men. However, in the sensitivity analysis that removed general self-rated health, this interaction was no longer significant. Race/ethnicity was a significant covariate, with higher satisfaction reported by black non-Hispanic men compared with white non-Hispanic men (approximately 3 points) and non-Hispanic men of other races (4.5 points; data not shown). The main effect for depression or anxiety indicated lower satisfaction among men who had a diagnosis of depression or anxiety. General self-rated health was also significant. Specifically, men in fair or poor health had predicted satisfaction scores nearly 8 points lower than men in excellent health. In the sensitivity analysis that removed general self-rated health from the model, coronary artery disease or heart disease was a significant covariate (P = .04; b = −2.48; SE, 1.19).
Discussion
In a nationally representative sample of US adults, more than 50% of sexually active men and more than 40% of sexually active women of all ages rated sexual health as highly important to quality of life. This finding was true even among participants who reported being in fair or poor health or having a chronic health condition. Given that many chronic conditions and their treatments can cause decrements in sexual function, health care providers should consider how best to address what may be a significant, yet unspoken, concern for many patients.
The importance of sexual health varied by sex, age, and sexual activity, consistent with findings from a previous study reporting on importance of sex to adults aged 57 to 85 years.2 In addition, we found that general self-reported health was related to the perceived importance of sexual health, with at least 70% of sexually active women and men who self-reported excellent general health rating sexual health as highly important. None of the particular health conditions we examined were associated with importance ratings.
Our results also provide a picture of overall sexual satisfaction for the 55% of men and 45% of women who were sexually active in the previous month. (Note that while we would expect higher numbers of sexually active adults if we asked people to report beyond the previous month, as in other large-scale studies,1–2 we would also expect greater recall bias with a longer reporting period.) First, we found that satisfaction with sex life peaked in the mid- to late 30s and declined after age 70 years. Second, satisfaction with sex life was associated with general self-rated health; participants in excellent health had significantly higher satisfaction than those in fair or poor health. Third, unlike the ratings of high importance, particular health conditions were associated with lower satisfaction with sex life, namely hypertension for women (especially younger women) and depression or anxiety for men (especially younger men). Other studies have reported increases in particular sexual problems in the context of specific medical conditions – for example, a two-fold increased odds of distressing sexual problems related to desire, arousal, or orgasm for women with depression24 and increased odds of developing cardiovascular problems for men reporting erectile dysfunction,25 – but with few exceptions,26 studies describing the association between particular conditions and sexual satisfaction have been less common.
In interpreting the findings regarding satisfaction with sex life, it is important to note that satisfaction may not reflect physiological function alone. In addition to function, other factors that are likely involved in evaluations of satisfaction include expectations about what level of functioning is normal or ideal, as well as beliefs about what aspects of sexual and intimate experiences should define “satisfaction with sex life.” For example, previous qualitative research suggested that some patients who reported sexual dysfunction after a diagnosis of or treatment for cancer reported high satisfaction, because they adopted a different conceptualization of satisfaction.11 That patients can experience high satisfaction despite clear functional problems suggests an opportunity for interventions that enhance satisfaction, even when anatomical or physiologic problems cannot be addressed. To accommodate such diverse people and experiences, the conceptual definition of the PROMIS Satisfaction with Sex Life scale does not limit how people define their sex life.
Despite at least one previous study suggesting racial/ethnic differences in sexual satisfaction among women,27 our study did not find these differences. However, men’s ratings of both the importance of sexual health and their satisfaction with sex life, though generally high, differed by race/ethnicity. Hispanic or Latino men had higher odds of rating importance as high, and black men reported somewhat higher satisfaction than other men. These results suggest cultural differences in beliefs and values about sexual health. Future research could examine factors such as the role of sexual well-being as part of one’s identity and expectations about what constitutes a satisfying sex life.
Our study has limitations. Despite the large sample size overall, sample sizes for some diagnoses were small (especially cancer), limiting our ability to reach quantifiable conclusions about these conditions, though recent and ongoing research in cancer will improve our understanding of this.28 Also, the results are not generalizable to non-English speaking persons in the US and should be replicated in other contexts, including outside the US and within different sociocultural landscapes. Finally, there is a possibility of survey error. The response rate was somewhat lower than other samples recruited by GfK, perhaps because of the longer length or content of the survey. To reduce errors of nonobservation, we chose GfK’s KnowledgePanel for data collection, given its address-based probabilistic recruitment methodology, multiple techniques to minimize nonresponse, and the multistaged approach to weighting to achieve optimal representativeness. To reduce measurement error, we conducted comprehensive qualitative research before fielding the survey.17,18,21,22 Still, the importance of sexual health to quality of life was measured with a single item and more rigorous approaches should be explored (e.g., contingent valuation or best-worst scaling in the context of a discrete choice experiment).
Conclusions
In this large study of US adults’ ratings of the importance of sexual health and satisfaction with sex life, sexual health was a highly important aspect of quality of life for many participants, including participants in poor health. Moreover, participants in poorer health reported lower sexual satisfaction. Accordingly, sexual health should be part of clinicians’ assessments of their patients. Health care systems that state a commitment to improving patients’ overall health must have resources in place to address sexual concerns. These resources should be available for all patients across the life span.
Take Home Message.
Sexual health is a highly important aspect of quality of life for men and women in the U.S., including those in poor health. Participants in poorer health reported lower sexual satisfaction. Addressing sexual health should be routine in health care.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: None
References
- 1.Laumann EO, Paik A, Rosen RC. Sexual dysfunction in the United States: prevalence and predictors. JAMA. 1999;281(6):537–544. doi: 10.1001/jama.281.6.537. [DOI] [PubMed] [Google Scholar]
- 2.Basson R, Schultz WW. Sexual sequelae of general medical disorders. Lancet. 2007;369(9559):409–424. doi: 10.1016/S0140-6736(07)60197-4. [DOI] [PubMed] [Google Scholar]
- 3.Flynn KE, Reese JB, Jeffery DD, et al. Patient experiences with communication about sex during and after treatment for cancer. Psychooncology. 2012;21(6):594–601. doi: 10.1002/pon.1947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gott M, Galena E, Hinchliff S, Elford H. "Opening a can of worms": GP and practice nurse barriers to talking about sexual health in primary care. Fam Pract. 2004;21(5):528–536. doi: 10.1093/fampra/cmh509. [DOI] [PubMed] [Google Scholar]
- 5.Gott M, Hinchliff S, Galena E. General practitioner attitudes to discussing sexual health issues with older people. Soc. Sci. Med. 2004;58(11):2093–2103. doi: 10.1016/j.socscimed.2003.08.025. [DOI] [PubMed] [Google Scholar]
- 6.Lindau ST, Abramsohn E, Gosch K, et al. Patterns and loss of sexual activity in the year following hospitalization for acute myocardial infarction (a United States National Multisite Observational Study) Am J Cardiol. 2012;109(10):1439–1444. doi: 10.1016/j.amjcard.2012.01.355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lindau ST, Surawska H, Paice J, Baron SR. Communication about sexuality and intimacy in couples affected by lung cancer and their clinical-care providers. Psychooncology. 2011;20(2):179–185. doi: 10.1002/pon.1787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sobecki JN, Curlin FA, Rasinski KA, Lindau ST. What we don't talk about when we don't talk about sex: results of a national survey of U.S. obstetrician/gynecologists. J Sex Med. 2012;9(5):1285–1294. doi: 10.1111/j.1743-6109.2012.02702.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lindau ST, Schumm LP, Laumann EO, Levinson W, O'Muircheartaigh CA, Waite LJ. A study of sexuality and health among older adults in the United States. New England Journal of Medicine. 2007;357(8):762–774. doi: 10.1056/NEJMoa067423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McCabe MP, Sharlip ID, Lewis R, et al. Risk Factors for Sexual Dysfunction Among Women and Men: A Consensus Statement From the Fourth International Consultation on Sexual Medicine 2015. J Sex Med. 2016;13(2):153–167. doi: 10.1016/j.jsxm.2015.12.015. [DOI] [PubMed] [Google Scholar]
- 11.Atallah S, Johnson-Agbakwu C, Rosenbaum T, et al. Ethical and Sociocultural Aspects of Sexual Function and Dysfunction in Both Sexes. J Sex Med. 2016;13(4):591–606. doi: 10.1016/j.jsxm.2016.01.021. [DOI] [PubMed] [Google Scholar]
- 12.Gillespie BJ. Correlates of Sex Frequency and Sexual Satisfaction Among Partnered Older Adults. J Sex Marital Ther. 2016:1–21. doi: 10.1080/0092623X.2016.1176608. [DOI] [PubMed] [Google Scholar]
- 13.D AF, Lever J, Gillespie BJ, Garcia JR. What Keeps Passion Alive? Sexual Satisfaction Is Associated With Sexual Communication, Mood Setting, Sexual Variety, Oral Sex, Orgasm, and Sex Frequency in a National U.S. Study. J Sex Res. 2016:1–16. doi: 10.1080/00224499.2015.1137854. [DOI] [PubMed] [Google Scholar]
- 14.McCall-Hosenfeld JS, Jaramillo SA, Legault C, et al. Correlates of sexual satisfaction among sexually active postmenopausal women in the Women's Health Initiative-Observational Study. J Gen Intern Med. 2008;23(12):2000–2009. doi: 10.1007/s11606-008-0820-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Evangelia N, Kirana PS, Chiu G, Link C, Rosen R, Hatzichristou D. Level of bother and treatment-seeking predictors among male and female in-patients with sexual problems: a hospital-based study. J Sex Med. 2010;7(2 Pt 1):700–711. doi: 10.1111/j.1743-6109.2009.01605.x. [DOI] [PubMed] [Google Scholar]
- 16.Weinfurt KP, Lin L, Bruner DW, et al. Development and Initial Validation of the PROMIS((R)) Sexual Function and Satisfaction Measures Version 2.0. J Sex Med. 2015;12(9):1961–1974. doi: 10.1111/jsm.12966. [DOI] [PubMed] [Google Scholar]
- 17.Alexander AM, Flynn KE, Hahn EA, et al. Improving patients' understanding of terms and phrases commonly used in self-reported measures of sexual function. J Sex Med. 2014;11(8):1991–1998. doi: 10.1111/jsm.12599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Flynn KE, Jeffery DD, Keefe FJ, et al. Sexual functioning along the cancer continuum: focus group results from the Patient-Reported Outcomes Measurement Information System (PROMIS(R)) Psychooncology. 2011;20(4):378–386. doi: 10.1002/pon.1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Flynn KE, Lin L, Cyranowski JM, et al. Development of the NIH PROMIS® Sexual Function and Satisfaction Measures in patients with cancer. Journal of Sexual Medicine. 2013;10(Suppl 1):43–52. doi: 10.1111/j.1743-6109.2012.02995.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Flynn KE, Reeve BB, Lin L, Cyranowski JM, Bruner DW, Weinfurt KP. Construct validity of the PROMIS(R) sexual function and satisfaction measures in patients with cancer. Health Qual Life Outcomes. 2013;11:40. doi: 10.1186/1477-7525-11-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fortune-Greeley AK, Flynn KE, Jeffery DD, et al. Using cognitive interviews to evaluate items for measuring sexual functioning across cancer populations: improvements and remaining challenges. Qual Life Res. 2009;18(8):1085–1093. doi: 10.1007/s11136-009-9523-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jeffery DD, Tzeng JP, Keefe FJ, et al. Initial report of the cancer Patient-Reported Outcomes Measurement Information System (PROMIS) sexual function committee: review of sexual function measures and domains used in oncology. Cancer. 2009;115(6):1142–1153. doi: 10.1002/cncr.24134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.DeSalvo KB, Bloser N, Reynolds K, He J, Muntner P. Mortality prediction with a single general self-rated health question. A meta-analysis. J Gen Intern Med. 2006;21(3):267–275. doi: 10.1111/j.1525-1497.2005.00291.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shifren JL, Monz BU, Russo PA, Segreti A, Johannes CB. Sexual problems and distress in United States women: prevalence and correlates. Obstet Gynecol. 2008;112(5):970–978. doi: 10.1097/AOG.0b013e3181898cdb. [DOI] [PubMed] [Google Scholar]
- 25.Hackett G, Krychman M, Baldwin D, et al. Coronary Heart Disease, Diabetes, and Sexuality in Men. J Sex Med. 2016;13(6):887–904. doi: 10.1016/j.jsxm.2016.01.023. [DOI] [PubMed] [Google Scholar]
- 26.Appa AA, Creasman J, Brown JS, et al. The impact of multimorbidity on sexual function in middle-aged and older women: beyond the single disease perspective. J Sex Med. 2014;11(11):2744–2755. doi: 10.1111/jsm.12665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huang AJ, Subak LL, Thom DH, et al. Sexual function and aging in racially and ethnically diverse women. J Am Geriatr Soc. 2009;57(8):1362–1368. doi: 10.1111/j.1532-5415.2009.02353.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Reese JB, Haythornthwaite JA. Importance of sexuality in colorectal cancer: predictors, changes, and response to an intimacy enhancement intervention. Support Care Cancer. 2016 doi: 10.1007/s00520-016-3265-4. [DOI] [PubMed] [Google Scholar]