Abstract
The event of mutations in the surface antigen gene of hepatitis B virus (HBV) results in undetectable hepatitis B surface antigen with positive/negative anti-hepatitis B core (anti-HBc) antibody status in serum and this phenomenon is named occult hepatitis B infection (OBI). The presence of anti-HBc antibody in serum is an important key for OBI tracking, although about 20% of OBI cases are negative for anti-HBc antibody. The diagnosis of OBI is mainly based on polymerase chain reaction (PCR) and real-time PCR assays. However, real-time PCR is a more reliable method than PCR. OBI is a great issue for the public health problem and a challenge for the clinical entity worldwide. The persistence of OBI may lead to the development of cirrhosis and hepatocellular carcinoma. With regard to OBI complications, the screening of HBV DNA by the highly sensitive molecular means should be implemented for: (1) patients with a previous history of chronic or acute HBV infection; (2) patients co-infected with hepatitis C virus/human immunodeficiency virus; (3) patients undergoing chemotherapy or anti-CD20 therapy; (4) recipients of organ transplant; (5) blood donors; (6) organ transplant donors; (7) thalassemia and hemophilia patients; (8) health care workers; (9) patients with liver related disease (cryptogenic); (10) hemodialysis patients; (11) patients undergoing lamivudine or interferon therapy; and (12) children in time of HBV vaccination especially in highly endemic areas of HBV. Active HBV vaccination should be implemented for the close relatives of patients who are negative for OBI markers. Thus, the goal of this review is to evaluate the rate of OBI with a focus on status of high risk groups in different regions of the world.
Keywords: Nested polymerase chain reaction, Occult hepatitis B infection, Cryptogenic, Real-time polymerase chain reaction
Core tip: Occult hepatitis B infection (OBI) is defined as negative hepatitis B surface antigen and positive/negative anti-hepatitis B core immunoglobulin G status but hepatitis B virus (HBV) DNA is detectable in serum and liver tissue. Genotypes A, C, G, E and D have been found among patients with OBI in different regions of the world. Genotype D is the only dominant genotype among Iranian OBI patients. OBI has been reported among many high risk groups, including blood donors, liver transplant recipients, patients co-infected with hepatitis C virus/human immunodeficiency virus, patients undergoing immunosuppressive therapy or hemodialysis, patients with liver cirrhosis, cryptogenic liver disease, or abnormal alanine transaminase, healthcare workers, patients with lymphoma or rheumatoid arthritis. It is recommended that to manage and reduce OBI and HBV carriage, the screening of HBV DNA be implemented among high risk groups by means of highly sensitive molecular assays periodically. In addition, comprehensive investigations are needed to understand the epidemiology of OBI worldwide.
INTRODUCTION
Hepatitis B virus (HBV) infection is a considerable global health problem and approximately two billion of the world population have been infected, of which 250 million live with HBV infection[1]. HBV infection is linked with a wide range of clinical manifestations, including acute or fulminant hepatitis to various forms of chronic infection, including asymptomatic carriers, chronic hepatitis, cirrhosis, and hepatocellular carcinoma (HCC). Although the implementation of screening tests for hepatitis B surface antigen (HBsAg) has significantly reduced the spread of HBV infection among blood donors, it fails to detect occult HBV infection (OBI) cases. In the 1970s, a new form of clinical HBV infection was reported in a patient with acute hepatitis, who was positive for anti-hepatitis B core (anti-HBc) immunoglobulin G (IgG), but negative for HBsAg[2]. Subsequently, by developing highly sensitive molecular means, the clinical entity of OBI was characterized, which resulted in the concept of “occult” or “silent” HBV infection[3,4]. The presence of mutations was demonstrated in the preS1, preS2 and S regions of the HBsAg gene, which results in undetectable HBsAg by enzyme-linked immunosorbant assay[5-8]. In the absence of serum HBsAg, low quantity of HBV DNA even < 200 IU/mL was detected in the serum and liver tissue biopsy by real-time polymerase chain reaction (PCR), and this new form of clinical entity of HBV infection was called OBI[9,10]. OBI is a clinical class of HBV infection and can appear in two forms: seropositive OBI and seronegative OBI. In seropositive OBI, serum HBV DNA is detectable and both anti-HBc/anti-hepatitis B surface (HBs) IgGs are positive or only anti-HBc IgG is positive, while in seronegative OBI, only HBV DNA is detectable in serum/or liver tissue, but anti-HBc IgG/anti-HBs IgGs are negative in serum[4]. The clinical feature of OBI remains unknown and more studies are required to understand the characteristics of OBI among the high risk group worldwide. With the present data on the OBI, several groups are believed to be at risk of OBI. The reactivation of OBI may take place in individuals with a previous history of HBV infection along with immunosuppression or chemotherapy status. Lastly, to prevent the spread of OBI, the screening of HBV DNA should be implemented in blood donors, immunosuppressive patients, organ transplant donors, organ transplant recipients, and individuals with acute rheumatoid arthritis before and after treatment with anti-tumor necrosis factor (TNF)-α[11]. In this paper, a search of MEDLINE database was performed to retrieve suitable articles to explain the epidemiology, diagnosis and prevention of OBI.
DEFINITION OF OBI
Most of OBI cases are asymptomatic and clinically not well defined. OBI has been investigated only in high risk groups with different serological and molecular descriptions. Several definitions of OBI have been described. In the international workshop (2008) in Italy, OBI was defined as the detection of HBV DNA in the liver (with or without HBV DNA in serum) without HBsAg[12]. OBI can be defined by the presence of HBV DNA in serum or liver tissue with either seropositive or seronegative status. Seropositive OBI is characterized by the detection of anti-HBc antibody with or without anti-HBs antibody, while seronegative OBI is described by undetectable both anti-HBc and anti-HBs antibodies. Seropositive OBI accounts for the enormous majority of OBI cases which can be attributed to the larger proportion of resolved HBV infections. It has been reported that more than 20% of OBI cases are seronegative for all the HBV markers[13]. In chronic occult infections, viral covalently closed circular DNA (cccDNA) persists as an episome in the nucleus of infected cells. Although the clinical features between OBI-seropositive and OBI-seronegative cases remain entirely cryptic, OBI may be exhibited in one of three clinical forms: (1) in a window period of acute HBV infection; (2) detectable HBV DNA and undetectable HBsAg in patient serum without a previous history of overt HBV infection; and (3) in patients with a history of chronic HBV infection. At present there is no standard assay for diagnosis of OBI in liver tissue or in serum, and the only reliable method is the detection of HBV DNA by nested PCR or real-time PCR. It has been illustrated that the application of real-time PCR possesses better outcomes provided that the specific primers are capable to cover all HBV genotypes[14]. The viral load lower than 200 IU/mL has been defined for OBI diagnosis, interestingly, in more than 90% of OBI patients, the viral load in serum was reported to be around 20 IU/mL[15]. Several mechanisms and factors may affect or suppress the HBV replication, which result in mutations in the HBsAg gene, although host immune response and epigenetic factors also play crucial roles in OBI (Figure 1).
Figure 1.
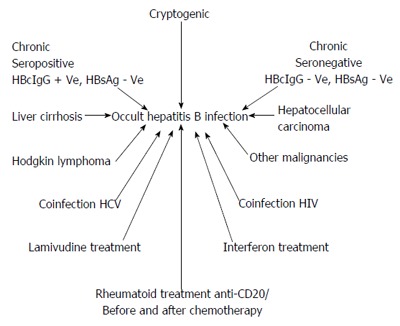
Schematic representation of clinical entity of occult hepatitis B infection. HCV: Hepatitis C virus; HIV: Human immunodeficiency virus; HBsAg: Hepatitis B surface antigen.
PREVALENCE OF OBI
The prevalence of OBI varies from region to region worldwide. This variability relies upon the sensitivity of HBV DNA detection assays, the sample size, and the detection of HBV DNA in liver tissue and serum by nested PCR or real-time PCR. The prevalence of OBI varies from 1% to 87% in different regions of the world[16,17]. OBI has been reported even in some geographical regions with low HBV endemicity[16]. The prevalence of OBI among the general population has been reported to be 45.5% with genotypes B and C[18] in China, and 1.7%-6.6% with genotype C2[19,20] in South Korea. In Taiwan, the prevalence was 10.9% in HBV vaccinated children[21] and 0.11% in blood donors[22]. In Egypt, it varied from a low 4.1% to high 26.8% in hemodialysis patients[23,24]. In Iran the prevalence of OBI has been reported to be 2 in 50000 in blood donors[25] and 14% in cryptogenic patients[26], while the prevalence of seropositive OBI was 2.27%[27] and 0% among blood donors[28].
MOLECULAR MECHANISMS OF OBI
Mutations in the “a” determinant of HBsAg
A mutation in the “a” determinant of the surface antigen is one of the known mechanisms which may result in OBI. Mutations in the HBsAg gene bring about the structural arrangement of the protein, which may lead to undetectable HBsAg by commercially HBsAg test kits[29]. The occurrence of sG145R mutation in the “a” determinant of the HBsAg gene also results in OBI[29]. It has been shown that the sG145R mutation in the HBsAg gene leads to a low binding affinity to monoclonal antibody against HBsAg[30]. In addition, within the “a” determinant several other mutations have been shown to cause a low affinity to monoclonal antibody against HBsAg[30-32].
Mutations in the pre S1 and preS2 regions
Mutations in the S region have been associated with reduced expression of HBV surface proteins. Subsequently, mutations in preS1/preS2 promoters are frequently observed in OBI patients, which make HBsAg become undetectable[33,34].
RNA splicing
Splicing steps have a critical effect on gene expression in HBV. In patients with OBI, it has been found that the substitution of nt G-to-A at position 458 of the surface gene interferes with the splicing of S gene mRNA and was associated with a lack of HBsAg expression and low replication of HBV DNA[35].
POSSIBLE OBI OUTCOMES OF LAMIVUDINE OR INTERFERON THERAPY
Treatment of chronic patients with lamivudine may result in amino acid changes in YMDD motif, in HBV polymerase Q563S and in sS207R surface genes, and thus contributes to OBI[36]. The nucleotide deletions in the pre-S1 and pre-S2 regions following the interferon therapy have resulted in the low replication of HBV DNA with low detection of HBsAg in cell culture systems[37].
OBI and chronic hepatitis C virus infection
The mutations in the HBsAg gene have been observed among patients coinfected with hepatitis C virus (HCV)[38-40]. Several studies have reported that low HBV DNA replication occurs in patients coinfected with HCV infection. It has been described that about one-third of patients with chronic HCV infection had detectable serum HBV DNA but undetectable HBsAg[41,42]. The presence of OBI in chronic HCV infected patients increases the risk of HCC[43,44]. When the coexistence of both HBV and HCV genomes occurs in the same hepatocyte, the replication of HBV is inhibited due to the interference of HCV molecules, which therefore results in the creation of OBI with low replication of HBV DNA[45]. Moreover, the HBX protein is a transactivator and activates HBV promoters and enhances HBV gene transcription[46,47]. The HCV core protein can interact with HBV X gene and prevent HBV gene transcription[48]. In addition, HCV “core”, NS2 and NS5A proteins could strongly inhibit HBV replication[34,43,49-51]. Table 1 shows the distribution of OBI among patients with HCV infection[52-66].
Table 1.
Profile of various studies on occult hepatitis B infection in patients with hepatitis C virus infection
| Ref. | Years | Study population | OBI |
| Fukuda et al[52] | 1999 | 65 patients with HCV-related liver disease | 34/65 (52.3%) |
| Kao et al[53] | 2002 | 210 patients with HCV-related liver disease | 31/210 (14.8%) |
| Besisik et al[54] | 2003 | 33 HCV positive patients on hemodialysis | 12/33 (36.4%) |
| Georgiadou et al[55] | 2004 | 187 patients with HCV-related liver disease | 49/187 |
| Khattab et al[56] | 2005 | 53 patients with chronic HCV infection | 4/53 (7.5%) |
| Goral et al[57] | 2006 | 50 HCV positive patients on hemodialysis | 0/50 |
| Branco et al[43] | 2007 | 46 patients with HCV-related liver disease | 9/46 (19.5%) |
| Toyoda et al[58] | 2007 | 95 HCV positive patients with HCC | 2/95 (2.1%) |
| Shetty et al[59] | 2008 | 44 HCV positive patients with liver cirrhosis | 22/44 (50%) |
| Tamori et al[60] | 2009 | 50 HCV positive patients with HCC | 21/50 (42%) |
| Chen et al[61] | 2010 | 126 patients with chronic HCV infection | 6/126 (5%) |
| Jang et al[62] | 2011 | 32 patients with chronic HCV infection | 9/32 (28.1%) |
| Joukar et al[63] | 2012 | 59 HCV positive patients on hemodialysis | 0/59 |
| Vakili Ghartavol et al[64] | 2013 | 50 patients with chronic HCV infection | 18/50(36%) |
| Kishk et al[65] | 2014 | 162 patients with chronic HCV infection | 3/162 (1.85%) |
| Mandour et al[66] | 2015 | 210 patients with chronic HCV infection | 53/210 (25.2%) |
HCC: Hepatocellular carcinoma; HCV: Hepatitis C virus.
HCC
While the prevalence of OBI among patients with HCV related liver disease is controversial, some data have approved this issue. For improving treatment and consequence of OBI, it is recommended that the screening of anti-HBc and HBV DNA be implemented for pretreatment of HCV-infected patients.
Coinfection of OBI with human immunodeficiency virus infection
Both HBV and human immunodeficiency virus (HIV) share the same rout of transmission. Mostly the coinfection of OBI and HIV occurs among intravenous drug users. It was found that coinfection of HIV and HBV may lead to faster progression of liver fibrosis, development of cirrhosis and HCC, even without coinfection with HIV[67]. The persistence of coinfection of OBI and HIV may result in severe and sometimes fulminant hepatitis[68]. The low HBV replication and undetectable surface antigen may be due to host cell epigenetic genome and polymorphisms in host cytokine and chemokine receptors[68-70]. Mutations in the X, precore/core, and Pol regions of HBV genome may result in mutations within the preS/S open reading frame and bring about OBI[29-51]. However, the effect of HIV components in HBV genome to lead to OBI remains unknown. While the occurrence of OBI may be related to host immune response and co-infections with HCV[50,51] or HIV[67,68], it has been postulated that HIV components are not major factors for the occurrence of OBI[71,72]. Table 2 shows the distribution of co-existence of OBI with HIV infection in different countries[73-86].
Table 2.
Rates of occult hepatitis B infection among HIV positive patients in some countries
| Ref. | Country | Prevalence % | Year |
| Vargas et al[73] | Chile | 0/192 (0) | 2016 |
| Alvarez-Muñoz et al[74] | Mexico | 24/49 (49.0) | 2014 |
| Chadwick et al[75] | England | 15/335 (4.5) | 2014 |
| Coffin et al[76] | Canada | 19/45 (42.0) | 2014 |
| Dapena et al[77] | Spain | 6/254 (2.4) | 2013 |
| Khamduang et al[78] | Thailand | 47/200 (23.5) | 2013 |
| Bell et al[79] | Africa | 45/298 (15.1) | 2012 |
| Panigrahi et al[80] | India | 12/112 (10.7) | 2012 |
| Bagaglio et al[81] | Italy | 9/29 (31.0) | 2011 |
| Gupta et al[82] | India | 24/53 (45.3) | 2010 |
| Hakeem et al[83] | Scotland | 2/70 (2.8) | 2010 |
| Morsica et al[84] | Italy | 27/175 (15) | 2009 |
| Azadmanesh et al[85] | Iran | 3/22 (13.6) | 2008 |
| Tsui et al[86] | United States | 8/400 (2.0) | 2007 |
Thus, with regard to the aforementioned data for improving treatment and outcomes of OBI, it is recommended that the screening of anti-HBc and HBV DNA be carried out for pretreatment of HIV patients.
BLOOD TRANSFUSION AND OBI PROBLEM
Blood transfusion is a main risk factor for transmission of OBI provided that the screening of blood donors is done with less security[87,88]. In the most developed countries, to boost blood safety, the nucleic acid amplification testing (NAT) has been established for screening of blood donors for detection of HCV, HIV and HBV or OBI. It is well documented that the application of NAT for HBV DNA, HCV RNA and HIV RNA detection is more sensitive than serological HBsAg, HCVAb, and HIV Ab tests[89,90]. Thus, the implementation of HBV-DNA detection by NAT is more sensitive than HBsAg assay as a preventive measure for HBV or OBI transmission via blood transfusion[89,90]. The prevalence of OBI among blood donors varies from country to country and has been reported in South Korea (HBV DNA, 0.016%)[91], India (anti-HBc, 10.22%; HBV DNA, 0.15%)[92], Turkey (anti-HBc, 20%; HBV DNA, 0)[93], Egypt (anti-HBc, 22.7%; HBV DNA, 22.7%)[94] and Iran (0% OBI)[95], (HBVDNA, 2/5000)[25], (anti-HBc, 20%; HBV DNA, 0)[93], (HBV DNA, 12.2%)[96]. In the most developing countries the screening of HBV among blood donors relies only on serological detection of HBsAg. While the screening of HBV by the NAT is expensive, it is effective in reducing the transmission of OBI via blood transfusion and blood products[89,90]. The detection of anti-HBc is a good test for OBI tracking, but it accounts for about 80% of OBI cases[97,98]. Thus, with regard to what was stated previously the implementation of anti-HBc test for blood donors can be considered a second safeguard policy for reducing the transmission of HBV via blood transfusion[99,100], although NAT is more sensitive and effective than serological HBsAg test as a preventive measure for HBV or OBI transmission via blood transfusion.
OBI AND HEAMODIALYSIS
Heamodialysis (HD) patients are at high risk of viral bloodborne infections (HBV, HIV, and HCV)[101-103] and tracking of the diagnosed liver disease based on aminotransferase levels in HD patients is difficult. Mostly aminotransferase is suppressed by reduced immune competence which results in weak inflammatory reactions and consequently reduces hepatocyte destruction[104]. It has been hypothesized that status of chronic uremia in HD patients may suppress the inflammatory reactions in the liver and consequently, no hepatocyte destruction will occur[105,106]. Therefore, the evaluation of quantitative HBV DNA was found to be the most efficient method to evaluate OBI in HD patients[101]. The prevalence of OBI has been studied in many countries, but varies from region to region worldwide. In Tehran, OBI was studied among HD patients by Ramezani et al[107], and they isolated HBV DNA in 1% of 100 HBsAg negative HD patients. In Tehran, Aghakhani et al[108] detected HBV DNA in 9/289 (3.1%) HD patients, who were negative for HBsAg but positive for HBcIgG. In Ahvaz, Neisi et al[109] detected HBV DNA in 10/250 (4%) of HD patients, who were negative for HBsAg but positive for anti-HBc. Also in Ahvaz, Rastegarvand et a[110] isolated HBV DNA in 6/216 (2.9%) HD patients, who were negative for HBsAg but positive for anti-HBc. The prevalence of OBI in HD patients was also reported in Spain (58%)[111], Egypt (26.9%)[24], United Kingdom (2.2%)[101], Greece (20.4%)[112] and Italy (0%)[113].
It is recommended that all the patients on HD be routinely screened for viral bloodborne infections (HBV, HIV and HCV), including OBI, using highly sensitive molecular techniques to prevent nosocomial transmission.
OBI AND CRYPTOGENIC LIVER DISEASE
The rate of cryptogenic liver diseases varies greatly in different regions of the world. Patients with long-term persistent ALT abnormality or with the lack of overt viral detection and autoimmune markers, have been shown to be positive for HBV DNA (OBI)[114]. While the etiology of cryptogenic liver disease remains unknown, the association of occult hepatitis C has been reported in patients with abnormal alanin aminotransaminase[115]. OBI has been regarded as an additional risk factor for progression of liver cirrhosis and HCC[26,116]. The prevalence of OBI in cryptogenic chronic liver disease varies from 3.88% to 55.6%[117,118]: in Brazil, 4.4%[119]; in China, 28.3%[120]; and in Iran, 1.9%[121], 10%[114], and India 9.5%[122]. With regard to the mentioned data, it is recommended that for improving treatment and management, the sera and PBMCs or liver biopsy of patients with cryptogenic hepatitis be screened for HBV DNA by highly sensitive molecular means before developing signs of cirrhosis or HCC.
OBI IN CRYPTOGENIC CIRRHOSIS AND HCC
Liver cirrhosis is an endangering public health problem worldwide. Most of liver cirrhosis patients may progress to upper gastrointestinal bleeding, hepatic encephalopathy, and HCC. HBV infection or OBI, HCV infection or occult HCV, and alcohol consumption are major etiologies for development of liver cirrhosis[123-125].
During the last phase of the natural course of chronic HBV infection, the inactive carrier phase is represented by HBeAg negativity, anti-HBe positivity, low HBV DNA levels (< 200 IU/mL) with minimal or no fibrosis[14,15]. The rates of spontaneous seroclearance of HBsAg (OBI) among inactive carriers range from 0.5% to 40% per year[126,127]. There have been reports on progression of inactive carriers to cirrhosis[128,129].
The prevalence of OBI among cirrhotic patients varies from region to region worldwide. The prevalence rates of OBI in cirrhotic patients have been reported: in Iran, 14% and 38%[26,130]; India, 38%[131], Italy, 23.4% and 27%[132,133]; Egypt, 2.7%[134]; Japan, 18.1%[135]; France, 60%[136]; United States, 19.4%[137]; Brazil, 20%[138]; China, 32%[139]; and China, 3.88%[117].
The mechanism of liver damage due to OBI is still not well elucidated, but there are some data that described the persistence and transcription of HBV cccDNA in hepatocytes and subsequently, production of cytokines, such as TNF-α and interferon-γ may result in damage to heptocytes[140,141]. The occurrence of mutations in the X region of HBV may bring about a reduction in the ability of the transactivation of X protein, which is essential for viral replication, and also result in low HBV DNA replication and undetectable HBsAg in serum[142].
Liver cancer is considered a major global health problem. Viral hepatitis B and C are main risk factors for the development of liver cancer[135,143]. The prolonged persistence of cccDNA in the hepatocyte nucleus has been detected in patients with HCC[144]. In addition, HBV DNA has been found to be integrated within the host chromosomes of individuals with HCC[145]. Most findings described that OBI is an important risk factor for hastening the progression of liver disease and the development of cirrhosis and HCC[146]. Several studies have documented that in patients with HCC who were negative for all HBV serum markers, including HBsAg, HBV DNA was detected in hepatocytes[147-160].
Several mechanisms may be involved in OBI-induced hepatocarcinogenesis. When HBV DNA is integrated into the host genome, the integrated HBX and truncated pre-S2/S genomic sequences may alter the cellular gene expression and result in the development of HCC[161-163]. OBI DNA, either in the form of free episomes or in integrated forms, is able to replicate, transcribe, and synthesize proteins, at very low levels[144-165].
The advances in molecular approaches have made it possible to disclose several virological features of OBI, and describe different clinical settings. Thus the persistence of OBI is an important risk factor for development of cirrhosis and HCC. But more investigations are needed to understand the relationship between OBI and cryptogenic liver disease. It is recommended that for improving and management of patients in the initial stage of cryptogenic liver diseases, the sera and PBMCs of the patients be screened for HBV DNA by highly sensitive molecular means as a preventive measure before the development of cirrhosis and HCC.
OBI AND TRANSPLANT
Liver transplantation is the only option for patients with end-stage chronic liver disease. But in liver transplant recipients with OBI, the reactivation of HBV is enhanced by the induced immunosuppression factors and rapidly leads to graft failure and death[166-168].
The occult HBV transmission from HBsAg-negative and anti-HBc-positive liver organ donors is possible, especially when the organ liver recipient is negative for all HBV serum markers[169]. Dickson et al[170] reported the de novo HBV infection was developed in 18/23 (78%) liver organ transplant recipients from donors who were positive for anti-HBc compared with 3/651 (0.5%) recipients of organ transplant liver from donors who were negative for anti-HBc (P < 0.0001). Although the prevalence of OBI among kidney or bone marrow transplant recipients is controversial, limited data are available on this subject. Franz et al[171] detected HBV DNA in 1% of 207 kidney transplant recipients negative for HBsAg. Cinzia Lo Giudice et al[5] detected HBV DNA in a bone marrow transplant recipient who was negative for HBsAg and required constant blood transfusion.
For the management and prevention of the consequences of OBI in organ transplant recipients, it is suggested that the screening of HBV DNA be carried out in both donors and organ transplant recipients by highly sensitive molecular means.
EPIGENETIC CHANGES
Methylation
Methylation of cytosines in CpG dinucleotides within CpG islands affects the HBV DNA promoter, which may lead to gene silencing[172]. Methylation was found in both HBV DNA integrated in the host hepatocyte genome as well in the free episomal form of HBV cccDNA[159,168]. Methylation of HBV DNA symbolizes a novel epigenetic mechanism, and it can alter HBV proteins, HBV replication, and HBV virion production, which may lead to OBI[173]. Hypermethylated HBV DNA sequences are frequently detected in HCC patients with OBI[174]. The integrated HBX and carboxy-terminally truncated preS or S polypeptide genes in the host genome may modify the host gene expression and cellular phenotypes and result in the acceleration of growth factor-independent proliferation, metastasis and the development of HCC[175,176].
Acetylation
Both experimental in vivo and in vitro data have shown that HBV replication is regulated by the acetylation of H3/H4 histones bound to viral cccDNA[177]. Besides, the histone deacetylase onto the cccDNA is associated with low HBV replication in vitro and low viremia in vivo[178].
OBI AND HODGKIN AND NON-HODGKIN LYMPHOMAS
The etiology of lymphoma remains unknown, although genetic, environment, and some infectious agents have been implicated in the development of Hodgkin and non-Hodgkin lymphomas. The association between viruses and lymphomas has been investigated, although the precise mechanisms behind this association are still unknown. The hepatotropism and lymphotropism of HBV have been well documented[179,180].
The association between HBV and non-Hodgkin lymphoma has been well investigated[181,182]. In a study conducted by Elbedewy et al[182] in Egypt, HBV DNA was detected in 5/72 (6.94%) of patients with diffuse large B-cell lymphoma who were positive for anti HBc (191). In a study conducted by Kamyar et al[183] in Ahvaz, Iran, HBV DNA was isolated in 3/12 (25%) of patients with Hodgkin lymphoma and in 7/ 29 (24.13%) of patients with non-Hodgkin lymphoma. In this study, the results of sequencing exhibited a substitution of the amino acid proline with leuicin in position 88 of the HBs gene in six patients with Hodgkin or non-Hodgkin lymphoma. Cheung et al[184] in Hong Kong detected HBV DNA in 10/47 (21%) patients with lymphoma who were negative for HBsAg but positive for anti-HBc.
With regard to the aforementioned data, it is recommended that for improving the treatment, patients with Hodgkin and non-Hodgkin lymphomas be screened for HBV DNA by highly sensitive molecular means prior to chemotherapy treatment.
OBI AND HEALTH CARE WORKERS
Health care workers are more often at high risk of HBV infection/OBI than the general population[185,186]. They may contract HBV transmission via exposure to potentially infected material as well as mucosal-cutaneous and percutaneous exposure to HBV from HBV carriers[187]. Most of individuals with OBI are clinically asymptomatic and remain undiagnosed unless a sudden development of cirrhosis or HCC occurred[188]. The prevalence of OBI among health care workers varies from region to region worldwide. The occurrence of OBI was mostly reported in regions of high endemicity of HBV[117]. Table 3 shows the prevalence of OBI among healthcare workers[188-192].
Table 3.
Prevalence of occult hepatitis B infection among healthcare workers
| Ref. | Country | No. of samples | No. of OBI cases | No. of cases positive for anti-HBc | Year |
| Borzooy et al[188] | Iran | 120 | 4 (3.3) | 0 (0) | 2015 |
| Chiarakul et al[189] | Thailand | 36 | 4 (11) | 4 (100) | 2011 |
| Slusarczyk et al[185] | Poland | 961 | 6 (4) | 4 (100%) | 2012 |
| Shim et al[190] | Korea | 334 | 0 | 0 | 2011 |
| Sukriti et al[191] | India | 120 | 6 (5) | 6 (100) | 2008 |
| Yen et al[192] | Taiwan | 250 | 16 (6.4) | 13 (81) | 2005 |
OBI: Occult hepatitis B infection. HBc: Hepatitis B core.
Based on the mentioned data, it is recommended that the screening of HBV DNA be implemented for health care workers. Besides, regardless to OBI, effective HBV vaccination should be carried out for health care workers. Also a booster dose of HBV vaccine should be put into practice for individuals with a low titer of anti-HBs (< 100 IU/mL).
OBI REACTIVATION
In OBI patients, HBV DNA may persist in two forms: episomal free cccDNA or integration into the DNA of hepatocytes. OBI may be generated by subsequently resolved acute HBV infection, occurrence of mutation in “a” determinant of the HBsAg gene, coinfection with HCV or HIV, and cellular epigenetic changes. In OBI, HBsAg is undetectable in serum with positive/negative anti-HBc status[172,175,193]. OBI reactivation may take place with increasing HBV DNA replication in patients during immunosuppression therapy[185,186,189-199]. OBI reactivation was described with enhancing HBV DNA replication in HIV patients during anti-retroviral therapy[200]. OBI reactivation resulted in the development of fulminant hepatitis in patients with cancer who underwent chemotherapy[200,201]. The risk of HBV reactivation is considered as high as 21% to 67% when immunosuppression is distinct, particularly in onco-hematological patients, in those receiving hematopoietic stem cell transplantation and in those treated with the anti-CD20 monoclonal antibody rituximab or with the monoclonal anti-CD52 antibody alemtuzumab, which account for long-lasting immunosuppression[193,194,202-208]. Under these situations, HBV reactivation causes a mortality rate about 20%, due to hepatic failure[209,210]. Seto et al[211] reported reactivation of hepatitis B in lymphoma patients with a past history of HBV infection, who were treatd with rituximab-containing chemotherapy. Hsu et al[212] studied the chemotherapy-induced hepatitis B reactivation in lymphoma patients with resolved HBV infection. Dominguez et al[213] (2015) observed reactivation of OBI in a patient with chronic lymphocytic leukemia after treatment with a rituximab and fludarabine-based regimen. A recent study conducted by Liu et al[214] revealed that reactivation of HBV was observed in patients with breast cancer receiving chemotherapy.
The risk of HBV reactivation in cancer patients receiving chemotherapy is impressed by inducing factors related to the virus, the host and specific immunosuppressive treatment, although the complete dimension of risk remains unknown.
With regard to the aforementioned data, the screening of HBV DNA by highly sensitive molecular means be implemented in all patients before and after immunosuppression status.
CONCLUSION
OBI is a life-threatening public health problem worldwide. The detection of OBI is costly, especially for developing countries, therefore many patients with OBI may remain undiagnosed. OBI is an important risk fact for developing cirrhosis and HCC.
OBI can be controlled in high risk groups, provided that the implementation of highly sensitive molecular means used for detection HBV DNA as a preventive measure.
With regard to the consequence of OBI, for improving the treatment and management, the screening of HBV DNA by real-time PCR should be implemented in the following groups: (1) patients with a previous history of HBV infection; (2) HBV patients coinfected with HCV/HIV; (3) patients undergoing chemtherapy anti-CD20 therapy; (4) recipients of organ transplant; (5) blood donors; (6) organ transplant donors; (7) thalassemia or hemophilia patients; h) health care workers; (8) patients with cryptogenic hepatitis or cryptogenic liver related disease (cirrhosis and HCC); (9) HD patients; (10) patients treated with lamivudine or interferon; and (11) children in time of HBV vaccination, especially in highly endemic areas of HBV. Besides, recent data revealed that reactivation of HBV was observed in patients with breast cancer receiving chemotherapy. Therefore, the screening of OBI should be implemented in patients with breast cancer.
In addition, proper disinfection should be performed for dialysis, endoscopy, colonoscopy and endoscopy units.
The effective HBV vaccination program should be carried out for the close relatives of patients who are negative for OBI. The third generation HBV vaccines containing preS1 and preS2 antigens have been developed with excellent immunogenicity in humans, and rapid antibody responses may be able to control the further incidence of OBI[215,216].
Footnotes
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Iran
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
Conflict-of-interest statement: The author declares that there are no conflicts of interest in the content of this review.
Peer-review started: March 29, 2016
First decision: May 30, 2016
Article in press: July 21, 2016
P- Reviewer: Franz C, Hoshina T, Yeung CY S- Editor: Yu J L- Editor: Wang TQ E- Editor: Zhang FF
References
- 1.World Health Organization. Hepatitis B Fact Sheet N204: Hepatitis B. World Health Organization, 2013. Accessed January 23, 2013. Available from: http://www.who.int/mediacentre/factsheets/fs204/en/
- 2.Tabor E, Hoofnagle JH, Smallwood LA, Drucker JA, Pineda-Tamondong GC, Ni LY, Greenwalt TJ, Barker LF, Gerety RJ. Studies of donors who transmit posttransfusion hepatitis. Transfusion. 1979;19:725–731. doi: 10.1046/j.1537-2995.1979.19680104098.x. [DOI] [PubMed] [Google Scholar]
- 3.Grob P, Jilg W, Bornhak H, Gerken G, Gerlich W, Günther S, Hess G, Hüdig H, Kitchen A, Margolis H, et al. Serological pattern “anti-HBc alone”: report on a workshop. J Med Virol. 2000;62:450–455. doi: 10.1002/1096-9071(200012)62:4<450::aid-jmv9>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 4.Hu KQ. Occult hepatitis B virus infection and its clinical implications. J Viral Hepat. 2002;9:243–257. doi: 10.1046/j.1365-2893.2002.00344.x. [DOI] [PubMed] [Google Scholar]
- 5.Giudice CL, Martinengo M, Pietrasanta P, Bocciardo L, Malavasi C, Rastelli S, Faraci M, Tripodi G. Occult hepatitis B virus infection: a case of reactivation in a patient receiving immunosuppressive treatment for allogeneic bone marrow transplantation. Blood Transfus. 2008;6:46–50. doi: 10.2450/2008.0033-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Raimondo G, Pollicino T, Romanò L, Zanetti AR. A 2010 update on occult hepatitis B infection. Pathol Biol (Paris) 2010;58:254–257. doi: 10.1016/j.patbio.2010.02.003. [DOI] [PubMed] [Google Scholar]
- 7.Kim H, Lee SA, Kim DW, Lee SH, Kim BJ. Naturally occurring mutations in large surface genes related to occult infection of hepatitis B virus genotype C. PLoS One. 2013;8:e54486. doi: 10.1371/journal.pone.0054486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Raimondo G, Pollicino T, Cacciola I, Squadrito G. Occult hepatitis B virus infection. J Hepatol. 2007;46:160–170. doi: 10.1016/j.jhep.2006.10.007. [DOI] [PubMed] [Google Scholar]
- 9.Kim H, Lee SA, Won YS, Lee H, Kim BJ. Occult infection related hepatitis B surface antigen variants showing lowered secretion capacity. World J Gastroenterol. 2015;21:1794–1803. doi: 10.3748/wjg.v21.i6.1794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhu HL, Li X, Li J, Zhang ZH. Genetic variation of occult hepatitis B virus infection. World J Gastroenterol. 2016;22:3531–3546. doi: 10.3748/wjg.v22.i13.3531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sarin SK, Kumar M, Lau GK, Abbas Z, Chan HL, Chen CJ, Chen DS, Chen HL, Chen PJ, Chien RN, et al. Asian-Pacific clinical practice guidelines on the management of hepatitis B: a 2015 update. Hepatol Int. 2016;10:1–98. doi: 10.1007/s12072-015-9675-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Raimondo G, Allain JP, Brunetto MR, Buendia MA, Chen DS, Colombo M, Craxì A, Donato F, Ferrari C, Gaeta GB, et al. Statements from the Taormina expert meeting on occult hepatitis B virus infection. J Hepatol. 2008;49:652–657. doi: 10.1016/j.jhep.2008.07.014. [DOI] [PubMed] [Google Scholar]
- 13.Torbenson M, Thomas DL. Occult hepatitis B. Lancet Infect Dis. 2002;2:479–486. doi: 10.1016/s1473-3099(02)00345-6. [DOI] [PubMed] [Google Scholar]
- 14.Morales-Romero J, Vargas G, García-Román R. Occult HBV infection: a faceless enemy in liver cancer development. Viruses. 2014;6:1590–1611. doi: 10.3390/v6041590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yuen MF, Lee CK, Wong DK, Fung J, Hung I, Hsu A, But DY, Cheung TK, Chan P, Yuen JC, et al. Prevalence of occult hepatitis B infection in a highly endemic area for chronic hepatitis B: a study of a large blood donor population. Gut. 2010;59:1389–1393. doi: 10.1136/gut.2010.209148. [DOI] [PubMed] [Google Scholar]
- 16.Minuk GY, Sun DF, Uhanova J, Zhang M, Caouette S, Nicolle LE, Gutkin A, Doucette K, Martin B, Giulivi A. Occult hepatitis B virus infection in a North American community-based population. J Hepatol. 2005;42:480–485. doi: 10.1016/j.jhep.2004.11.037. [DOI] [PubMed] [Google Scholar]
- 17.Escobedo-Melendez G, Panduro A, Fierro NA, Roman S. High prevalence of occult hepatitis B virus genotype H infection among children with clinical hepatitis in west Mexico. Mem Inst Oswaldo Cruz. 2014;109:728–737. doi: 10.1590/0074-0276140058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fang ZL, Sabin CA, Dong BQ, Wei SC, Chen QY, Fang KX, Yang JY, Huang J, Wang XY, Harrison TJ. Hepatitis B virus pre-S deletion mutations are a risk factor for hepatocellular carcinoma: a matched nested case-control study. J Gen Virol. 2008;89:2882–2890. doi: 10.1099/vir.0.2008/002824-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kang SY, Kim MH, Lee WI. The prevalence of “anti-HBc alone” and HBV DNA detection among anti-HBc alone in Korea. J Med Virol. 2010;82:1508–1514. doi: 10.1002/jmv.21862. [DOI] [PubMed] [Google Scholar]
- 20.Kim H, Kim BJ. Association of preS/S Mutations with Occult Hepatitis B Virus (HBV) Infection in South Korea: Transmission Potential of Distinct Occult HBV Variants. Int J Mol Sci. 2015;16:13595–13609. doi: 10.3390/ijms160613595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mu SC, Lin YM, Jow GM, Chen BF. Occult hepatitis B virus infection in hepatitis B vaccinated children in Taiwan. J Hepatol. 2009;50:264–272. doi: 10.1016/j.jhep.2008.09.017. [DOI] [PubMed] [Google Scholar]
- 22.Su TH, Chen PJ, Chen TC, Cheng HR, Li L, Lin KS, Kao JH, Chen DS, Liu CJ. The clinical significance of occult hepatitis B transfusion in Taiwan--a look-back study. Transfus Med. 2011;21:33–41. doi: 10.1111/j.1365-3148.2010.01036.x. [DOI] [PubMed] [Google Scholar]
- 23.Abu El Makarem MA, Abdel Hamid M, Abdel Aleem A, Ali A, Shatat M, Sayed D, Deaf A, Hamdy L, Tony EA. Prevalence of occult hepatitis B virus infection in hemodialysis patients from egypt with or without hepatitis C virus infection. Hepat Mon. 2012;12:253–258. doi: 10.5812/hepatmon.665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Elgohry I, Elbanna A, Hashad D. Occult hepatitis B virus infection in a cohort of Egyptian chronic hemodialysis patients. Clin Lab. 2012;58:1057–1061. [PubMed] [Google Scholar]
- 25.Alizadeh Z, Milani S, Sharifi Z. Occult hepatitis B virus infection among Iranian blood donors: a preliminary study. Arch Iran Med. 2014;17:106–107. [PubMed] [Google Scholar]
- 26.Hashemi JS, Hajiani E, Masjedizadeh A, Makvandi M, Shayesteh AA, Alavinejad SP, Kadkhodaei A, Shahbazian H, Jasemi F, Karimi M. Occult Hepatitis B Infection in Patients With Cryptogenic Liver Cirrhosis in Southwest of Iran. Jundishapur J Microbiol. 2015;8:e16873. doi: 10.5812/jjm.16873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sharifi-Mood B, Sanei-Moghaddam E, Khosravi S. Occult hepatitis B Virus infection among anti-HBc only positive individuals in the southeast of Iran in high prevalence of HBV infection region. IRCMJ. 2009;11:90–92. [Google Scholar]
- 28.Vaezjalali M, Rashidpour S, Rezaee H, Hajibeigi B, Zeidi M, Gachkar L, Aghamohamad S, Najafi R, Goudarzi H. Hepatitis B viral DNA among HBs antigen negative healthy blood donors. Hepat Mon. 2013;13:e6590. doi: 10.5812/hepatmon.6590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carman WF, Zanetti AR, Karayiannis P, Waters J, Manzillo G, Tanzi E, Zuckerman AJ, Thomas HC. Vaccine-induced escape mutant of hepatitis B virus. Lancet. 1990;336:325–329. doi: 10.1016/0140-6736(90)91874-a. [DOI] [PubMed] [Google Scholar]
- 30.Carman WF, Korula J, Wallace L, MacPhee R, Mimms L, Decker R. Fulminant reactivation of hepatitis B due to envelope protein mutant that escaped detection by monoclonal HBsAg ELISA. Lancet. 1995;345:1406–1407. doi: 10.1016/s0140-6736(95)92599-6. [DOI] [PubMed] [Google Scholar]
- 31.Nainan OV, Khristova ML, Byun K, Xia G, Taylor PE, Stevens CE, Margolis HS. Genetic variation of hepatitis B surface antigen coding region among infants with chronic hepatitis B virus infection. J Med Virol. 2002;68:319–327. doi: 10.1002/jmv.10206. [DOI] [PubMed] [Google Scholar]
- 32.Schilling R, Ijaz S, Davidoff M, Lee JY, Locarnini S, Williams R, Naoumov NV. Endocytosis of hepatitis B immune globulin into hepatocytes inhibits the secretion of hepatitis B virus surface antigen and virions. J Virol. 2003;77:8882–8892. doi: 10.1128/JVI.77.16.8882-8892.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chaudhuri V, Tayal R, Nayak B, Acharya SK, Panda SK. Occult hepatitis B virus infection in chronic liver disease: full-length genome and analysis of mutant surface promoter. Gastroenterology. 2004;127:1356–1371. doi: 10.1053/j.gastro.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 34.Vivekanandan P, Kannangai R, Ray SC, Thomas DL, Torbenson M. Comprehensive genetic and epigenetic analysis of occult hepatitis B from liver tissue samples. Clin Infect Dis. 2008;46:1227–1236. doi: 10.1086/529437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hass M, Hannoun C, Kalinina T, Sommer G, Manegold C, Günther S. Functional analysis of hepatitis B virus reactivating in hepatitis B surface antigen-negative individuals. Hepatology. 2005;42:93–103. doi: 10.1002/hep.20748. [DOI] [PubMed] [Google Scholar]
- 36.Wakil SM, Kazim SN, Khan LA, Raisuddin S, Parvez MK, Guptan RC, Thakur V, Hasnain SE, Sarin SK. Prevalence and profile of mutations associated with lamivudine therapy in Indian patients with chronic hepatitis B in the surface and polymerase genes of hepatitis B virus. J Med Virol. 2002;68:311–318. doi: 10.1002/jmv.10205. [DOI] [PubMed] [Google Scholar]
- 37.Melegari M, Bruno S, Wands JR. Properties of hepatitis B virus pre-S1 deletion mutants. Virology. 1994;199:292–300. doi: 10.1006/viro.1994.1127. [DOI] [PubMed] [Google Scholar]
- 38.Obika M, Shinji T, Fujioka S, Terada R, Ryuko H, Lwin AA, Shiraha H, Koide N. Hepatitis B virus DNA in liver tissue and risk for hepatocarcinogenesis in patients with hepatitis C virus-related chronic liver disease. A prospective study. Intervirology. 2008;51:59–68. doi: 10.1159/000121363. [DOI] [PubMed] [Google Scholar]
- 39.Jansen K, Thamm M, Bock CT, Scheufele R, Kücherer C, Muenstermann D, Hagedorn HJ, Jessen H, Dupke S, Hamouda O, et al. High Prevalence and High Incidence of Coinfection with Hepatitis B, Hepatitis C, and Syphilis and Low Rate of Effective Vaccination against Hepatitis B in HIV-Positive Men Who Have Sex with Men with Known Date of HIV Seroconversion in Germany. PLoS One. 2015;10:e0142515. doi: 10.1371/journal.pone.0142515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lok AS, Everhart JE, Di Bisceglie AM, Kim HY, Hussain M, Morgan TR. Occult and previous hepatitis B virus infection are not associated with hepatocellular carcinoma in United States patients with chronic hepatitis C. Hepatology. 2011;54:434–442. doi: 10.1002/hep.24257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Marusawa H, Osaki Y, Kimura T, Ito K, Yamashita Y, Eguchi T, Kudo M, Yamamoto Y, Kojima H, Seno H, et al. High prevalence of anti-hepatitis B virus serological markers in patients with hepatitis C virus related chronic liver disease in Japan. Gut. 1999;45:284–288. doi: 10.1136/gut.45.2.284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Raouf HE, Yassin AS, Megahed SA, Ashour MS, Mansour TM. Seroprevalence of occult hepatitis B among Egyptian paediatric hepatitis C cancer patients. J Viral Hepat. 2015;22:103–111. doi: 10.1111/jvh.12260. [DOI] [PubMed] [Google Scholar]
- 43.Branco F, Mattos AA, Coral GP, Vanderborght B, Santos DE, França P, Alexandre C. Occult hepatitis B virus infection in patients with chronic liver disease due to hepatitis C virus and hepatocellular carcinoma in Brazil. Arq Gastroenterol. 2007;44:58–63. doi: 10.1590/s0004-28032007000100013. [DOI] [PubMed] [Google Scholar]
- 44.Miura Y, Shibuya A, Adachi S, Takeuchi A, Tsuchihashi T, Nakazawa T, Saigenji K. Occult hepatitis B virus infection as a risk factor for hepatocellular carcinoma in patients with chronic hepatitis C in whom viral eradication fails. Hepatol Res. 2008;38:546–556. doi: 10.1111/j.1872-034X.2007.00316.x. [DOI] [PubMed] [Google Scholar]
- 45.Rodríguez-Iñigo E, Bartolomé J, Ortiz-Movilla N, Platero C, López-Alcorocho JM, Pardo M, Castillo I, Carreño V. Hepatitis C virus (HCV) and hepatitis B virus (HBV) can coinfect the same hepatocyte in the liver of patients with chronic HCV and occult HBV infection. J Virol. 2005;79:15578–15581. doi: 10.1128/JVI.79.24.15578-15581.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Choi BH, Park GT, Rho HM. Interaction of hepatitis B viral X protein and CCAAT/ enhancer-binding protein alpha synergistically activates the hepatitis B viral enhancer II/pregenomic promoter. J Biol Chem. 1999;274:2858–2865. doi: 10.1074/jbc.274.5.2858. [DOI] [PubMed] [Google Scholar]
- 47.Nakatake H, Chisaka O, Yamamoto S, Matsubara K, Koshy R. Effect of X protein on transactivation of hepatitis B virus promoters and on viral replication. Virology. 1993;195:305–314. doi: 10.1006/viro.1993.1381. [DOI] [PubMed] [Google Scholar]
- 48.Chen SY, Kao CF, Chen CM, Shih CM, Hsu MJ, Chao CH, Wang SH, You LR, Lee YH. Mechanisms for inhibition of hepatitis B virus gene expression and replication by hepatitis C virus core protein. J Biol Chem. 2003;278:591–607. doi: 10.1074/jbc.M204241200. [DOI] [PubMed] [Google Scholar]
- 49.Schüttler CG, Fiedler N, Schmidt K, Repp R, Gerlich WH, Schaefer S. Suppression of hepatitis B virus enhancer 1 and 2 by hepatitis C virus core protein. J Hepatol. 2002;37:855–862. doi: 10.1016/s0168-8278(02)00296-9. [DOI] [PubMed] [Google Scholar]
- 50.Dumoulin FL, von dem Bussche A, Li J, Khamzina L, Wands JR, Sauerbruch T, Spengler U. Hepatitis C virus NS2 protein inhibits gene expression from different cellular and viral promoters in hepatic and nonhepatic cell lines. Virology. 2003;305:260–266. doi: 10.1006/viro.2002.1701. [DOI] [PubMed] [Google Scholar]
- 51.Pan Y, Wei W, Kang L, Wang Z, Fang J, Zhu Y, Wu J. NS5A protein of HCV enhances HBV replication and resistance to interferon response. Biochem Biophys Res Commun. 2007;359:70–75. doi: 10.1016/j.bbrc.2007.05.052. [DOI] [PubMed] [Google Scholar]
- 52.Fukuda R, Ishimura N, Niigaki M, Hamamoto S, Satoh S, Tanaka S, Kushiyama Y, Uchida Y, Ihihara S, Akagi S, et al. Serologically silent hepatitis B virus coinfection in patients with hepatitis C virus-associated chronic liver disease: clinical and virological significance. J Med Virol. 1999;58:201–207. doi: 10.1002/(sici)1096-9071(199907)58:3<201::aid-jmv3>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 53.Kao JH, Chen PJ, Lai MY, Chen DS. Occult hepatitis B virus infection and clinical outcomes of patients with chronic hepatitis C. J Clin Microbiol. 2002;40:4068–4071. doi: 10.1128/JCM.40.11.4068-4071.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Besisik F, Karaca C, Akyüz F, Horosanli S, Onel D, Badur S, Sever MS, Danalioglu A, Demir K, Kaymakoglu S, et al. Occult HBV infection and YMDD variants in hemodialysis patients with chronic HCV infection. J Hepatol. 2003;38:506–510. doi: 10.1016/s0168-8278(02)00457-9. [DOI] [PubMed] [Google Scholar]
- 55.Georgiadou SP, Zachou K, Rigopoulou E, Liaskos C, Mina P, Gerovasilis F, Makri E, Dalekos GN. Occult hepatitis B virus infection in Greek patients with chronic hepatitis C and in patients with diverse nonviral hepatic diseases. J Viral Hepat. 2004;11:358–365. doi: 10.1111/j.1365-2893.2004.00513.x. [DOI] [PubMed] [Google Scholar]
- 56.Khattab E, Chemin I, Vuillermoz I, Vieux C, Mrani S, Guillaud O, Trepo C, Zoulim F. Analysis of HCV co-infection with occult hepatitis B virus in patients undergoing IFN therapy. J Clin Virol. 2005;33:150–157. doi: 10.1016/j.jcv.2004.10.016. [DOI] [PubMed] [Google Scholar]
- 57.Goral V, Ozkul H, Tekes S, Sit D, Kadiroglu AK. Prevalence of occult HBV infection in haemodialysis patients with chronic HCV. World J Gastroenterol. 2006;12:3420–3424. doi: 10.3748/wjg.v12.i21.3420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Toyoda H, Kumada T, Kiriyama S, Sone Y, Tanikawa M, Hisanaga Y, Kanamori A. Prevalence of low-level hepatitis B viremia in patients with HBV surface antigen-negative hepatocellular carcinoma with and without hepatitis C virus infection in Japan: analysis by COBAS TaqMan real-time PCR. Intervirology. 2007;50:241–244. doi: 10.1159/000101911. [DOI] [PubMed] [Google Scholar]
- 59.Shetty K, Hussain M, Nei L, Reddy KR, Lok AS. Prevalence and significance of occult hepatitis B in a liver transplant population with chronic hepatitis C. Liver Transpl. 2008;14:534–540. doi: 10.1002/lt.21284. [DOI] [PubMed] [Google Scholar]
- 60.Tamori A, Hayashi T, Shinzaki M, Kobayashi S, Iwai S, Enomoto M, Morikawa H, Sakaguchi H, Shiomi S, Takemura S, et al. Frequent detection of hepatitis B virus DNA in hepatocellular carcinoma of patients with sustained virologic response for hepatitis C virus. J Med Virol. 2009;81:1009–1014. doi: 10.1002/jmv.21488. [DOI] [PubMed] [Google Scholar]
- 61.Chen LW, Chien RN, Yen CL, Chang JJ, Liu CJ, Lin CL. Therapeutic effects of pegylated interferon plus ribavirin in chronic hepatitis C patients with occult hepatitis B virus dual infection. J Gastroenterol Hepatol. 2010;25:259–263. doi: 10.1111/j.1440-1746.2009.06006.x. [DOI] [PubMed] [Google Scholar]
- 62.Jang JY, Jeong SW, Cheon SR, Lee SH, Kim SG, Cheon YK, Kim YS, Cho YD, Kim HS, Jin SY, et al. Clinical significance of occult hepatitis B virus infection in chronic hepatitis C patients. Korean J Hepatol. 2011;17:206–212. doi: 10.3350/kjhep.2011.17.3.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Joukar F, Mansour-Ghanaei F, Besharati S, Khosh-Sorur M. Occult hepatitis B infection in a hemodialysis population in Guilan province, northern Iran. Hemodial Int. 2012;16:294–297. doi: 10.1111/j.1542-4758.2011.00645.x. [DOI] [PubMed] [Google Scholar]
- 64.Vakili Ghartavol Z, Alavian SM, Amini S, Vahabpour R, Bahramali G, Mostafavi E, Aghasadeghi MR. Prevalence of occult hepatitis B virus in plasma and peripheral blood mononuclear cell compartments of patients with chronic hepatitis C infection in tehran-iran. Hepat Mon. 2013;13:e10134. doi: 10.5812/hepatmon.10134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kishk R, Atta HA, Ragheb M, Kamel M, Metwally L, Nemr N. Genotype characterization of occult hepatitis B virus strains among Egyptian chronic hepatitis C patients. East Mediterr Health J. 2014;20:130–138. [PubMed] [Google Scholar]
- 66.Mandour M, Nemr N, Shehata A, Kishk R, Badran D, Hawass N. Occult HBV infection status among chronic hepatitis C and hemodialysis patients in Northeastern Egypt: regional and national overview. Rev Soc Bras Med Trop. 2015;48:258–264. doi: 10.1590/0037-8682-0037-2015. [DOI] [PubMed] [Google Scholar]
- 67.Mallet V, Vallet-Pichard A, Pol S. The impact of human immunodeficiency virus on viral hepatitis. Liver Int. 2011;31 Suppl 1:135–139. doi: 10.1111/j.1478-3231.2010.02394.x. [DOI] [PubMed] [Google Scholar]
- 68.Mphahlele MJ, Lukhwareni A, Burnett RJ, Moropeng LM, Ngobeni JM. High risk of occult hepatitis B virus infection in HIV-positive patients from South Africa. J Clin Virol. 2006;35:14–20. doi: 10.1016/j.jcv.2005.04.003. [DOI] [PubMed] [Google Scholar]
- 69.Arababadi MK, Pourfathollah AA, Jafarzadeh A, Hassanshahi G, Rezvani ME. Association of exon 9 but not intron 8 VDR polymorphisms with occult HBV infection in south-eastern Iranian patients. J Gastroenterol Hepatol. 2010;25:90–93. doi: 10.1111/j.1440-1746.2009.05950.x. [DOI] [PubMed] [Google Scholar]
- 70.Ahmadabadi BN, Hassanshahi G, Arababadi MK, Leanza C, Kennedy D. The IL-10 promoter polymorphism at position -592 is correlated with susceptibility to occult HBV infection. Inflammation. 2012;35:818–821. doi: 10.1007/s10753-011-9381-x. [DOI] [PubMed] [Google Scholar]
- 71.Pollicino T, Raffa G, Costantino L, Lisa A, Campello C, Squadrito G, Levrero M, Raimondo G. Molecular and functional analysis of occult hepatitis B virus isolates from patients with hepatocellular carcinoma. Hepatology. 2007;45:277–285. doi: 10.1002/hep.21529. [DOI] [PubMed] [Google Scholar]
- 72.Raimondo G, Caccamo G, Filomia R, Pollicino T. Occult HBV infection. Semin Immunopathol. 2013;35:39–52. doi: 10.1007/s00281-012-0327-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Vargas JI, Jensen D, Sarmiento V, Peirano F, Acuña P, Fuster F, Soto S, Ahumada R, Huilcaman M, Bruna M, et al. Presence of anti-HBc is associated to high rates of HBV resolved infection and low threshold for Occult HBV Infection in HIV patients with negative HBsAg in Chile. J Med Virol. 2016;88:639–646. doi: 10.1002/jmv.24384. [DOI] [PubMed] [Google Scholar]
- 74.Alvarez-Muñoz MT, Maldonado-Rodriguez A, Rojas-Montes O, Torres-Ibarra R, Gutierrez-Escolano F, Vazquez-Rosales G, Gomez A, Muñoz O, Torres J, Lira R. Occult hepatitis B virus infection among Mexican human immunodeficiency virus-1-infected patients. World J Gastroenterol. 2014;20:13530–13537. doi: 10.3748/wjg.v20.i37.13530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Chadwick D, Doyle T, Ellis S, Price D, Abbas I, Valappil M, Geretti AM. Occult hepatitis B virus coinfection in HIV-positive African migrants to the UK: a point prevalence study. HIV Med. 2014;15:189–192. doi: 10.1111/hiv.12093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Coffin CS, Mulrooney-Cousins PM, Osiowy C, van der Meer F, Nishikawa S, Michalak TI, van Marle G, Gill MJ. Virological characteristics of occult hepatitis B virus in a North American cohort of human immunodeficiency virus type 1-positive patients on dual active anti-HBV/HIV therapy. J Clin Virol. 2014;60:347–353. doi: 10.1016/j.jcv.2014.04.021. [DOI] [PubMed] [Google Scholar]
- 77.Dapena M, Figueras C, Noguera-Julian A, Fortuny C, de José MI, Mellado MJ, Gavilán C, Falcón-Neyra MD, Navarro ML, de Ory SJ, et al. Implementation of occult hepatitis screening in the Spanish cohort of HIV-infected pediatric patients. Pediatr Infect Dis J. 2013;32:e377–e379. doi: 10.1097/INF.0b013e31828e9b99. [DOI] [PubMed] [Google Scholar]
- 78.Khamduang W, Ngo-Giang-Huong N, Gaudy-Graffin C, Jourdain G, Suwankornsakul W, Jarupanich T, Chalermpolprapa V, Nanta S, Puarattana-Aroonkorn N, Tonmat S, et al. Prevalence, risk factors, and impact of isolated antibody to hepatitis B core antigen and occult hepatitis B virus infection in HIV-1-infected pregnant women. Clin Infect Dis. 2013;56:1704–1712. doi: 10.1093/cid/cit166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Bell TG, Makondo E, Martinson NA, Kramvis A. Hepatitis B virus infection in human immunodeficiency virus infected southern African adults: occult or overt--that is the question. PLoS One. 2012;7:e45750. doi: 10.1371/journal.pone.0045750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Panigrahi R, Majumder S, Gooptu M, Biswas A, Datta S, Chandra PK, Banerjee A, Chakrabarti S, Bandopadhyay D, De BK, et al. Occult HBV infection among anti-HBc positive HIV-infected patients in apex referral centre, Eastern India. Ann Hepatol. 2012;11:870–875. [PubMed] [Google Scholar]
- 81.Bagaglio S, Bianchi G, Danise A, Porrino L, Uberti-Foppa C, Lazzarin A, Castagna A, Morsica G. Longitudinal evaluation of occult hepatitis B infection in HIV-1 infected individuals during highly active antiretroviral treatment interruption and after HAART resumption. Infection. 2011;39:121–126. doi: 10.1007/s15010-011-0093-9. [DOI] [PubMed] [Google Scholar]
- 82.Gupta S, Singh S. Occult hepatitis B virus infection in ART-naive HIV-infected patients seen at a tertiary care centre in north India. BMC Infect Dis. 2010;10:53. doi: 10.1186/1471-2334-10-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hakeem L, Thomson G, McCleary E, Bhattacharyya D, Banerjee I. Prevalence and Immunization Status of Hepatitis B Virus in the HIV Cohort in Fife, Scotland. J Clin Med Res. 2010;2:34–38. doi: 10.4021/jocmr2009.12.1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Morsica G, Ancarani F, Bagaglio S, Maracci M, Cicconi P, Cozzi Lepri A, Antonucci G, Bruno R, Santantonio T, Tacconi L, et al. Occult hepatitis B virus infection in a cohort of HIV-positive patients: correlation with hepatitis C virus coinfection, virological and immunological features. Infection. 2009;37:445–449. doi: 10.1007/s15010-008-8194-9. [DOI] [PubMed] [Google Scholar]
- 85.Azadmanesh K, Mohraz M, Aghakhani A, Edalat R, Jam S, Eslamifar A, Banifazl M, Moradmand-Badie B, Ramezani A. Occult hepatitis B virus infection in HIV-infected patients with isolated hepatitis B core antibody. Intervirology. 2008;51:270–274. doi: 10.1159/000160217. [DOI] [PubMed] [Google Scholar]
- 86.Tsui JI, French AL, Seaberg EC, Augenbraun M, Nowicki M, Peters M, Tien PC. Prevalence and long-term effects of occult hepatitis B virus infection in HIV-infected women. Clin Infect Dis. 2007;45:736–740. doi: 10.1086/520989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Candotti D, Allain JP. Transfusion-transmitted hepatitis B virus infection. J Hepatol. 2009;51:798–809. doi: 10.1016/j.jhep.2009.05.020. [DOI] [PubMed] [Google Scholar]
- 88.Allain JP, Candotti D. Diagnostic algorithm for HBV safe transfusion. Blood Transfus. 2009;7:174–182. doi: 10.2450/2008.0062-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Yoshikawa A, Gotanda Y, Minegishi K, Taira R, Hino S, Tadokoro K, Ohnuma H, Miyakawa K, Tachibana K, Mizoguchi H. Lengths of hepatitis B viremia and antigenemia in blood donors: preliminary evidence of occult (hepatitis B surface antigen-negative) infection in the acute stage. Transfusion. 2007;47:1162–1171. doi: 10.1111/j.1537-2995.2007.01234.x. [DOI] [PubMed] [Google Scholar]
- 90.González R, Torres P, Castro E, Barbolla L, Candotti D, Koppelman M, Zaaijer HL, Lelie N, Allain JP, Echevarría JM. Efficacy of hepatitis B virus (HBV) DNA screening and characterization of acute and occult HBV infections among blood donors from Madrid, Spain. Transfusion. 2010;50:221–230. doi: 10.1111/j.1537-2995.2009.02343.x. [DOI] [PubMed] [Google Scholar]
- 91.Seo DH, Whang DH, Song EY, Kim HS, Park Q. Prevalence of antibodies to hepatitis B core antigen and occult hepatitis B virus infections in Korean blood donors. Transfusion. 2011;51:1840–1846. doi: 10.1111/j.1537-2995.2010.03056.x. [DOI] [PubMed] [Google Scholar]
- 92.Makroo RN, Chowdhry M, Bhatia A, Arora B, Rosamma NL. Hepatitis B core antibody testing in Indian blood donors: A double-edged sword! Asian J Transfus Sci. 2012;6:10–13. doi: 10.4103/0973-6247.95043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Findik D, Arslan U, Baykan M. Determination of hepatitis B virus DNA incidence, viral load, and mutations in blood donors with HBsAg and anti-HBs-negative serology and antibodies to hepatitis B core antigen. Eur J Intern Med. 2007;18:571–575. doi: 10.1016/j.ejim.2007.07.001. [DOI] [PubMed] [Google Scholar]
- 94.Kishk R, Nemr N, Elkady A, Mandour M, Aboelmagd M, Ramsis N, Hassan M, Soliman N, Iijima S, Murakami S, et al. Hepatitis B surface gene variants isolated from blood donors with overt and occult HBV infection in north eastern Egypt. Virol J. 2015;12:153. doi: 10.1186/s12985-015-0389-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Sofian M, Aghakhani A, Izadi N, Banifazl M, Kalantar E, Eslamifar A, Ramezani A. Lack of occult hepatitis B virus infection among blood donors with isolated hepatitis B core antibody living in an HBV low prevalence region of Iran. Int J Infect Dis. 2010;14:e308–e310. doi: 10.1016/j.ijid.2009.05.011. [DOI] [PubMed] [Google Scholar]
- 96.Behzad-Behbahani A, Mafi-Nejad A, Tabei SZ, Lankarani KB, Torab A, Moaddeb A. Anti-HBc & amp; HBV-DNA detection in blood donors negative for hepatitis B virus surface antigen in reducing risk of transfusion associated HBV infection. Indian J Med Res. 2006;123:37–42. [PubMed] [Google Scholar]
- 97.Hollinger FB, Sood G. Occult hepatitis B virus infection: a covert operation. J Viral Hepat. 2010;17:1–15. doi: 10.1111/j.1365-2893.2009.01245.x. [DOI] [PubMed] [Google Scholar]
- 98.Meidani M, Rostami M, Hemmati S, Ashrafi F, Gholamnezhad M, Emadi M, Ghasemian R, Ahmadian M. Screening and evaluation of chronic and occult Hepatitis B in chemo - radiotherapy patients with cancer. Adv Biomed Res. 2016;5:85. doi: 10.4103/2277-9175.182216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Said ZN, El-Sayed MH, El-Bishbishi IA, El-Fouhil DF, Abdel-Rheem SE, El-Abedin MZ, Salama II. High prevalence of occult hepatitis B in hepatitis C-infected Egyptian children with haematological disorders and malignancies. Liver Int. 2009;29:518–524. doi: 10.1111/j.1478-3231.2009.01975.x. [DOI] [PubMed] [Google Scholar]
- 100.El-Sherif AM, Abou-Shady MA, Al-Hiatmy MA, Al-Bahrawy AM, Motawea EA. Screening for hepatitis B virus infection in Egyptian blood donors negative for hepatitis B surface antigen. Hepatol Int. 2007;1:469–470. doi: 10.1007/s12072-007-9017-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Sowole L, Labbett W, Patel M, O’Riordan A, Cross J, Davenport A, Haque T. The prevalence of occult hepatitis B virus (HBV) infection in a large multi-ethnic haemodialysis cohort. BMC Nephrol. 2015;16:12. doi: 10.1186/s12882-015-0010-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Marinaki S, Boletis JN, Sakellariou S, Delladetsima IK. Hepatitis C in hemodialysis patients. World J Hepatol. 2015;7:548–558. doi: 10.4254/wjh.v7.i3.548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Lucas GM, Ross MJ, Stock PG, Shlipak MG, Wyatt CM, Gupta SK, Atta MG, Wools-Kaloustian KK, Pham PA, Bruggeman LA, et al. Clinical practice guideline for the management of chronic kidney disease in patients infected with HIV: 2014 update by the HIV Medicine Association of the Infectious Diseases Society of America. Clin Infect Dis. 2014;59:e96–138. doi: 10.1093/cid/ciu617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Yakaryilmaz F, Gurbuz OA, Guliter S, Mert A, Songur Y, Karakan T, Keles H. Prevalence of occult hepatitis B and hepatitis C virus infections in Turkish hemodialysis patients. Ren Fail. 2006;28:729–735. doi: 10.1080/08860220600925602. [DOI] [PubMed] [Google Scholar]
- 105.Fabrizi F, Lunghi G, Martin P. Hepatitis B virus infection in hemodialysis: recent discoveries. J Nephrol. 2002;15:463–468. [PubMed] [Google Scholar]
- 106.Fabrizi F, Poordad FF, Martin P. Hepatitis C infection and the patient with end-stage renal disease. Hepatology. 2002;36:3–10. doi: 10.1053/jhep.2002.34613. [DOI] [PubMed] [Google Scholar]
- 107.Ramezani A, Aghasadeghi MR, Ahmadi F, Razeghi E, Eslamifar A, Banifazl M, Sofian M, Bahramali G, Hekmat S, Aghakhani A. Isolated anti-hbc and occult HBV infection in dialysis patients. Nephrourol Mon. 2015;7:e22674. doi: 10.5812/numonthly.22674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Aghakhani A, Banifazl M, Kalantar E, Eslamifar A, Ahmadi F, Razeghi E, Atabak S, Amini M, Khadem-Sadegh A, Ramezani A. Occult hepatitis B virus infection in hemodialysis patients with isolated hepatitis B core antibody: a multicenter study. Ther Apher Dial. 2010;14:349–353. doi: 10.1111/j.1744-9987.2009.00798.x. [DOI] [PubMed] [Google Scholar]
- 109.Neisi N, Makvandi M, Samarbaf-Zadeh AR. A study on genotypes of hepatitis B virus among hemodialysis patients in Khuzestan province. Jundishapur J Microbiol. 2011;4:65–70. doi: 10.5812/jjm.20834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Rastegarvand N, Makvandi M, Samarbafzadeh A, Rasti M, Neisi N, Pouremamali A, Teimoori A, Shabani A. Molecular Characterization of Pre-Core/Core and S Region of Hepatitis B Virus in Hemodialysis Patients With Occult Hepatitis B Infection. Jundishapur J Microbiol. 2015;8:e23686. doi: 10.5812/jjm.23686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Cabrerizo M, Bartolomé J, De Sequera P, Caramelo C, Carreño V. Hepatitis B virus DNA in serum and blood cells of hepatitis B surface antigen-negative hemodialysis patients and staff. J Am Soc Nephrol. 1997;8:1443–1447. doi: 10.1681/ASN.V891443. [DOI] [PubMed] [Google Scholar]
- 112.Siagris D, Christofidou M, Triga K, Pagoni N, Theocharis GJ, Goumenos D, Lekkou A, Thomopoulos K, Tsamandas AC, Vlachojannis J, et al. Occult hepatitis B virus infection in hemodialysis patients with chronic HCV infection. J Nephrol. 2006;19:327–333. [PubMed] [Google Scholar]
- 113.Fabrizi F, Messa PG, Lunghi G, Aucella F, Bisegna S, Mangano S, Villa M, Barbisoni F, Rusconi E, Martin P. Occult hepatitis B virus infection in dialysis patients: a multicentre survey. Aliment Pharmacol Ther. 2005;21:1341–1347. doi: 10.1111/j.1365-2036.2005.02501.x. [DOI] [PubMed] [Google Scholar]
- 114.Makvandi M, Neisi N, Khalafkhany D, Makvandi K, Hajiani E, Shayesteh AA, Masjedi Zadeh A, Sina AH, Hamidifard M, Rasti M, et al. Occult hepatitis B virus among the patients with abnormal alanine transaminase. Jundishapur J Microbiol. 2014;7:e11648. doi: 10.5812/jjm.11648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Makvandi M, Khalafkhany D, Rasti M, Neisi N, Omidvarinia A, Mirghaed AT, Masjedizadeh A, Shyesteh AA. Detection of Hepatitis C virus RNA in peripheral blood mononuclear cells of patients with abnormal alanine transaminase in Ahvaz. Indian J Med Microbiol. 2014;32:251–255. doi: 10.4103/0255-0857.136553. [DOI] [PubMed] [Google Scholar]
- 116.Saitta C, Tripodi G, Barbera A, Bertuccio A, Smedile A, Ciancio A, Raffa G, Sangiovanni A, Navarra G, Raimondo G, et al. Hepatitis B virus (HBV) DNA integration in patients with occult HBV infection and hepatocellular carcinoma. Liver Int. 2015;35:2311–2317. doi: 10.1111/liv.12807. [DOI] [PubMed] [Google Scholar]
- 117.Hou J, Wang Z, Cheng J, Lin Y, Lau GK, Sun J, Zhou F, Waters J, Karayiannis P, Luo K. Prevalence of naturally occurring surface gene variants of hepatitis B virus in nonimmunized surface antigen-negative Chinese carriers. Hepatology. 2001;34:1027–1034. doi: 10.1053/jhep.2001.28708. [DOI] [PubMed] [Google Scholar]
- 118.Youssef A, Yano Y, Utsumi T, abd El-alah EM, abd El-Hameed Ael-E, Serwah Ael-H, Hayashi Y. Molecular epidemiological study of hepatitis viruses in Ismailia, Egypt. Intervirology. 2009;52:123–131. doi: 10.1159/000219385. [DOI] [PubMed] [Google Scholar]
- 119.Ferrari TC, Xavier MA, Vidigal PV, Amaral NS, Diniz PA, Resende AP, Miranda DM, Faria AC, Lima AS, Faria LC. Occult hepatitis B virus infection in liver transplant patients in a Brazilian referral center. Braz J Med Biol Res. 2014;47:990–994. doi: 10.1590/1414-431X20143782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Fang Y, Shang QL, Liu JY, Li D, Xu WZ, Teng X, Zhao HW, Fu LJ, Zhang FM, Gu HX. Prevalence of occult hepatitis B virus infection among hepatopathy patients and healthy people in China. J Infect. 2009;58:383–388. doi: 10.1016/j.jinf.2009.02.013. [DOI] [PubMed] [Google Scholar]
- 121.Kaviani MJ, Behbahani B, Mosallaii MJ, Sari-Aslani F, Taghavi SA. Occult hepatitis B virus infection and cryptogenic chronic hepatitis in an area with intermediate prevalence of HBV infection. World J Gastroenterol. 2006;12:5048–5050. doi: 10.3748/wjg.v12.i31.5048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Srivastava A, Mathias A, Yachha SK, Aggarwal R. Occult hepatitis B infection in children with chronic liver disease. Eur J Gastroenterol Hepatol. 2015;27:375–377. doi: 10.1097/MEG.0000000000000294. [DOI] [PubMed] [Google Scholar]
- 123.Ansari N, Makvandi M, Samarbaf-Zadeh AR. Hepatitis B virus genotyping among patients with cirrhosis. Jundishapur J Microbiol. 2015;8:e14571. doi: 10.5812/jjm.14571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Carreño V. Seronegative occult hepatitis C virus infection: clinical implications. J Clin Virol. 2014;61:315–320. doi: 10.1016/j.jcv.2014.09.007. [DOI] [PubMed] [Google Scholar]
- 125.Rasineni K, Penrice DD, Natarajan SK, McNiven MA, McVicker BL, Kharbanda KK, Casey CA, Harris EN. Alcoholic vs non-alcoholic fatty liver in rats: distinct differences in endocytosis and vesicle trafficking despite similar pathology. BMC Gastroenterol. 2016;16:27. doi: 10.1186/s12876-016-0433-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Chu CM, Liaw YF. HBsAg seroclearance in asymptomatic carriers of high endemic areas: appreciably high rates during a long-term follow-up. Hepatology. 2007;45:1187–1192. doi: 10.1002/hep.21612. [DOI] [PubMed] [Google Scholar]
- 127.McMahon BJ, Holck P, Bulkow L, Snowball M. Serologic and clinical outcomes of 1536 Alaska Natives chronically infected with hepatitis B virus. Ann Intern Med. 2001;135:759–768. doi: 10.7326/0003-4819-135-9-200111060-00006. [DOI] [PubMed] [Google Scholar]
- 128.Liaw YF, Tai DI, Chu CM, Chen TJ. The development of cirrhosis in patients with chronic type B hepatitis: a prospective study. Hepatology. 1988;8:493–496. doi: 10.1002/hep.1840080310. [DOI] [PubMed] [Google Scholar]
- 129.Weissberg JI, Andres LL, Smith CI, Weick S, Nichols JE, Garcia G, Robinson WS, Merigan TC, Gregory PB. Survival in chronic hepatitis B. An analysis of 379 patients. Ann Intern Med. 1984;101:613–616. doi: 10.7326/0003-4819-101-5-613. [DOI] [PubMed] [Google Scholar]
- 130.Anvari FA, Alavian SM, Norouzi M, Mahabadi M, Jazayeri SM. Prevalence and molecular analysis of occult hepatitis B virus infection isolated in a sample of cryptogenic cirrhosis patients in iran. Oman Med J. 2014;29:92–96. doi: 10.5001/omj.2014.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Agarwal N, Naik S, Aggarwal R, Singh H, Somani SK, Kini D, Pandey R, Choudhuri G, Saraswat VA, Naik SR. Occult hepatitis B virus infection as a cause of cirrhosis of liver in a region with intermediate endemicity. Indian J Gastroenterol. 2003;22:127–131. [PubMed] [Google Scholar]
- 132.Squadrito G, Cacciola I, Alibrandi A, Pollicino T, Raimondo G. Impact of occult hepatitis B virus infection on the outcome of chronic hepatitis C. J Hepatol. 2013;59:696–700. doi: 10.1016/j.jhep.2013.05.043. [DOI] [PubMed] [Google Scholar]
- 133.Sagnelli E, Imparato M, Coppola N, Pisapia R, Sagnelli C, Messina V, Piai G, Stanzione M, Bruno M, Moggio G, et al. Diagnosis and clinical impact of occult hepatitis B infection in patients with biopsy proven chronic hepatitis C: a multicenter study. J Med Virol. 2008;80:1547–1553. doi: 10.1002/jmv.21239. [DOI] [PubMed] [Google Scholar]
- 134.Emara MH, El-Gammal NE, Mohamed LA, Bahgat MM. Occult hepatitis B infection in egyptian chronic hepatitis C patients: prevalence, impact on pegylated interferon/ribavirin therapy. Virol J. 2010;7:324. doi: 10.1186/1743-422X-7-324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Matsuoka S, Nirei K, Tamura A, Nakamura H, Matsumura H, Oshiro S, Arakawa Y, Yamagami H, Tanaka N, Moriyama M. Influence of occult hepatitis B virus coinfection on the incidence of fibrosis and hepatocellular carcinoma in chronic hepatitis C. Intervirology. 2008;51:352–361. doi: 10.1159/000187720. [DOI] [PubMed] [Google Scholar]
- 136.Mrani S, Chemin I, Menouar K, Guillaud O, Pradat P, Borghi G, Trabaud MA, Chevallier P, Chevallier M, Zoulim F, et al. Occult HBV infection may represent a major risk factor of non-response to antiviral therapy of chronic hepatitis C. J Med Virol. 2007;79:1075–1081. doi: 10.1002/jmv.20943. [DOI] [PubMed] [Google Scholar]
- 137.Hui CK, Lau E, Wu H, Monto A, Kim M, Luk JM, Lau GK, Wright TL. Fibrosis progression in chronic hepatitis C patients with occult hepatitis B co-infection. J Clin Virol. 2006;35:185–192. doi: 10.1016/j.jcv.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 138.Silva Cd, Gonçales NS, Pereira JS, Escanhoela CA, Pavan MH, Gonçales FL. The influence of occult infection with hepatitis B virus on liver histology and response to interferon treatment in chronic hepatitis C patients. Braz J Infect Dis. 2004;8:431–439. doi: 10.1590/s1413-86702004000600007. [DOI] [PubMed] [Google Scholar]
- 139.Chan HL, Tsang SW, Leung NW, Tse CH, Hui Y, Tam JS, Chan FK, Sung JJ. Occult HBV infection in cryptogenic livercirrhosis in an area with high prevalence of HBV infection. Am J Gastroenterol. 2002;97:1211–1215. doi: 10.1111/j.1572-0241.2002.05706.x. [DOI] [PubMed] [Google Scholar]
- 140.Germanidis G, Hytiroglou P, Zakalka M, Settas L. Reactivation of occult hepatitis B virus infection, following treatment of refractory rheumatoid arthritis with abatacept. J Hepatol. 2012;56:1420–1421. doi: 10.1016/j.jhep.2011.10.011. [DOI] [PubMed] [Google Scholar]
- 141.Martin CM, Welge JA, Shire NJ, Shata MT, Sherman KE, Blackard JT. Cytokine expression during chronic versus occult hepatitis B virus infection in HIV co-infected individuals. Cytokine. 2009;47:194–198. doi: 10.1016/j.cyto.2009.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Uchida T, Saitoh T, Shinzawa H. Mutations of the X region of hepatitis B virus and their clinical implications. Pathol Int. 1997;47:183–193. doi: 10.1111/j.1440-1827.1997.tb04479.x. [DOI] [PubMed] [Google Scholar]
- 143.Tan YJ. Hepatitis B virus infection and the risk of hepatocellular carcinoma. World J Gastroenterol. 2011;17:4853–4857. doi: 10.3748/wjg.v17.i44.4853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Wong DK, Yuen MF, Poon RT, Yuen JC, Fung J, Lai CL. Quantification of hepatitis B virus covalently closed circular DNA in patients with hepatocellular carcinoma. J Hepatol. 2006;45:553–559. doi: 10.1016/j.jhep.2006.05.014. [DOI] [PubMed] [Google Scholar]
- 145.Raimondo G, Burk RD, Lieberman HM, Muschel J, Hadziyannis SJ, Will H, Kew MC, Dusheiko GM, Shafritz DA. Interrupted replication of hepatitis B virus in liver tissue of HBsAg carriers with hepatocellular carcinoma. Virology. 1988;166:103–112. doi: 10.1016/0042-6822(88)90151-1. [DOI] [PubMed] [Google Scholar]
- 146.Shi Y, Wu YH, Wu W, Zhang WJ, Yang J, Chen Z. Association between occult hepatitis B infection and the risk of hepatocellular carcinoma: a meta-analysis. Liver Int. 2012;32:231–240. doi: 10.1111/j.1478-3231.2011.02481.x. [DOI] [PubMed] [Google Scholar]
- 147.Shafritz DA, Shouval D, Sherman HI, Hadziyannis SJ, Kew MC. Integration of hepatitis B virus DNA into the genome of liver cells in chronic liver disease and hepatocellular carcinoma. Studies in percutaneous liver biopsies and post-mortem tissue specimens. N Engl J Med. 1981;305:1067–1073. doi: 10.1056/NEJM198110293051807. [DOI] [PubMed] [Google Scholar]
- 148.Paterlini P, Driss F, Nalpas B, Pisi E, Franco D, Berthelot P, Bréchot C. Persistence of hepatitis B and hepatitis C viral genomes in primary liver cancers from HBsAg-negative patients: a study of a low-endemic area. Hepatology. 1993;17:20–29. [PubMed] [Google Scholar]
- 149.Paterlini P, Poussin K, Kew M, Franco D, Brechot C. Selective accumulation of the X transcript of hepatitis B virus in patients negative for hepatitis B surface antigen with hepatocellular carcinoma. Hepatology. 1995;21:313–321. [PubMed] [Google Scholar]
- 150.Poussin K, Dienes H, Sirma H, Urban S, Beaugrand M, Franco D, Schirmacher P, Bréchot C, Paterlini Bréchot P. Expression of mutated hepatitis B virus X genes in human hepatocellular carcinomas. Int J Cancer. 1999;80:497–505. doi: 10.1002/(sici)1097-0215(19990209)80:4<497::aid-ijc3>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 151.Bläckberg J, Kidd-Ljunggren K. Occult hepatitis B virus after acute self-limited infection persisting for 30 years without sequence variation. J Hepatol. 2000;33:992–997. doi: 10.1016/s0168-8278(00)80134-8. [DOI] [PubMed] [Google Scholar]
- 152.Mulrooney-Cousins PM, Chauhan R, Churchill ND, Michalak TI. Primary seronegative but molecularly evident hepadnaviral infection engages liver and induces hepatocarcinoma in the woodchuck model of hepatitis B. PLoS Pathog. 2014;10:e1004332. doi: 10.1371/journal.ppat.1004332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Pollicino T, Vegetti A, Saitta C, Ferrara F, Corradini E, Raffa G, Pietrangelo A, Raimondo G. Hepatitis B virus DNA integration in tumour tissue of a non-cirrhotic HFE-haemochromatosis patient with hepatocellular carcinoma. J Hepatol. 2013;58:190–193. doi: 10.1016/j.jhep.2012.09.005. [DOI] [PubMed] [Google Scholar]
- 154.Tamori A, Nishiguchi S, Kubo S, Koh N, Moriyama Y, Fujimoto S, Takeda T, Shiomi S, Hirohashi K, Kinoshita H, et al. Possible contribution to hepatocarcinogenesis of X transcript of hepatitis B virus in Japanese patients with hepatitis C virus. Hepatology. 1999;29:1429–1434. doi: 10.1002/hep.510290520. [DOI] [PubMed] [Google Scholar]
- 155.Squadrito G, Pollicino T, Cacciola I, Caccamo G, Villari D, La Masa T, Restuccia T, Cucinotta E, Scisca C, Magazzu D, et al. Occult hepatitis B virus infection is associated with the development of hepatocellular carcinoma in chronic hepatitis C patients. Cancer. 2006;106:1326–1330. doi: 10.1002/cncr.21702. [DOI] [PubMed] [Google Scholar]
- 156.Ikeda K, Marusawa H, Osaki Y, Nakamura T, Kitajima N, Yamashita Y, Kudo M, Sato T, Chiba T. Antibody to hepatitis B core antigen and risk for hepatitis C-related hepatocellular carcinoma: a prospective study. Ann Intern Med. 2007;146:649–656. doi: 10.7326/0003-4819-146-9-200705010-00008. [DOI] [PubMed] [Google Scholar]
- 157.Kitab B, Ezzikouri S, Alaoui R, Nadir S, Badre W, Trepo C, Chemin I, Benjelloun S. Occult HBV infection in Morocco: from chronic hepatitis to hepatocellular carcinoma. Liver Int. 2014;34:e144–e150. doi: 10.1111/liv.12482. [DOI] [PubMed] [Google Scholar]
- 158.Chen CH, Changchien CS, Lee CM, Tung WC, Hung CH, Hu TH, Wang JH, Wang JC, Lu SN. A study on sequence variations in pre-S/surface, X and enhancer II/core promoter/precore regions of occult hepatitis B virus in non-B, non-C hepatocellular carcinoma patients in Taiwan. Int J Cancer. 2009;125:621–629. doi: 10.1002/ijc.24416. [DOI] [PubMed] [Google Scholar]
- 159.Lee SB, Kim KM, An J, Lee D, Shim JH, Lim YS, Lee HC, Chung YH, Lee YS. Clinical characteristics and potential aetiologies of non-B non-C hepatocellular carcinoma in hepatitis B virus endemic area. Liver Int. 2016;36:1351–1361. doi: 10.1111/liv.13099. [DOI] [PubMed] [Google Scholar]
- 160.Kondo R, Nakashima O, Sata M, Imazeki F, Yokosuka O, Tanikawa K, Kage M, Yano H. Pathological characteristics of patients who develop hepatocellular carcinoma with negative results of both serous hepatitis B surface antigen and hepatitis C virus antibody. Hepatol Res. 2014;44:1039–1046. doi: 10.1111/hepr.12219. [DOI] [PubMed] [Google Scholar]
- 161.Pollicino T, Saitta C, Raimondo G. Hepatocellular carcinoma: the point of view of the hepatitis B virus. Carcinogenesis. 2011;32:1122–1132. doi: 10.1093/carcin/bgr108. [DOI] [PubMed] [Google Scholar]
- 162.Pan J, Clayton M, Feitelson MA. Hepatitis B virus X antigen promotes transforming growth factor-beta1 (TGF-beta1) activity by up-regulation of TGF-beta1 and down-regulation of alpha2-macroglobulin. J Gen Virol. 2004;85:275–282. doi: 10.1099/vir.0.19650-0. [DOI] [PubMed] [Google Scholar]
- 163.Fallot G, Neuveut C, Buendia MA. Diverse roles of hepatitis B virus in liver cancer. Curr Opin Virol. 2012;2:467–473. doi: 10.1016/j.coviro.2012.05.008. [DOI] [PubMed] [Google Scholar]
- 164.Wong DK, Huang FY, Lai CL, Poon RT, Seto WK, Fung J, Hung IF, Yuen MF. Occult hepatitis B infection and HBV replicative activity in patients with cryptogenic cause of hepatocellular carcinoma. Hepatology. 2011;54:829–836. doi: 10.1002/hep.24551. [DOI] [PubMed] [Google Scholar]
- 165.Gozuacik D, Murakami Y, Saigo K, Chami M, Mugnier C, Lagorce D, Okanoue T, Urashima T, Bréchot C, Paterlini-Bréchot P. Identification of human cancer-related genes by naturally occurring Hepatitis B Virus DNA tagging. Oncogene. 2001;20:6233–6240. doi: 10.1038/sj.onc.1204835. [DOI] [PubMed] [Google Scholar]
- 166.García-Fulgueiras A, García-Pina R, Morant C, García-Ortuzar V, Génova R, Alvarez E. Hepatitis C and hepatitis B-related mortality in Spain. Eur J Gastroenterol Hepatol. 2009;21:895–901. doi: 10.1097/MEG.0b013e328313139d. [DOI] [PubMed] [Google Scholar]
- 167.Marcellin P, Pequignot F, Delarocque-Astagneau E, Zarski JP, Ganne N, Hillon P, Antona D, Bovet M, Mechain M, Asselah T, et al. Mortality related to chronic hepatitis B and chronic hepatitis C in France: evidence for the role of HIV coinfection and alcohol consumption. J Hepatol. 2008;48:200–207. doi: 10.1016/j.jhep.2007.09.010. [DOI] [PubMed] [Google Scholar]
- 168.Xie M, Rao W, Yang T, Deng Y, Zheng H, Pan C, Liu Y, Shen Z, Jia J. Occult hepatitis B virus infection predicts de novo hepatitis B infection in patients with alcoholic cirrhosis after liver transplantation. Liver Int. 2015;35:897–904. doi: 10.1111/liv.12567. [DOI] [PubMed] [Google Scholar]
- 169.Cholongitas E, Papatheodoridis GV, Burroughs AK. Liver grafts from anti-hepatitis B core positive donors: a systematic review. J Hepatol. 2010;52:272–279. doi: 10.1016/j.jhep.2009.11.009. [DOI] [PubMed] [Google Scholar]
- 170.Dickson RC, Everhart JE, Lake JR, Wei Y, Seaberg EC, Wiesner RH, Zetterman RK, Pruett TL, Ishitani MB, Hoofnagle JH. Transmission of hepatitis B by transplantation of livers from donors positive for antibody to hepatitis B core antigen. The National Institute of Diabetes and Digestive and Kidney Diseases Liver Transplantation Database. Gastroenterology. 1997;113:1668–1674. doi: 10.1053/gast.1997.v113.pm9352871. [DOI] [PubMed] [Google Scholar]
- 171.Franz C, Perez Rde M, Zalis MG, Zalona AC, Rocha PT, Gonçalves RT, Nabuco LC, Villela-Nogueira CA. Prevalence of occult hepatitis B virus infection in kidney transplant recipients. Mem Inst Oswaldo Cruz. 2013;108:657–660. doi: 10.1590/0074-0276108052013019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Zhang YJ, Li H, Wu HC, Shen J, Wang L, Yu MW, Lee PH, Bernard Weinstein I, Santella RM. Silencing of Hint1, a novel tumor suppressor gene, by promoter hypermethylation in hepatocellular carcinoma. Cancer Lett. 2009;275:277–284. doi: 10.1016/j.canlet.2008.10.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Samal J, Kandpal M, Vivekanandan P. Molecular mechanisms underlying occult hepatitis B virus infection. Clin Microbiol Rev. 2012;25:142–163. doi: 10.1128/CMR.00018-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Fang S, Huang SF, Cao J, Wen YA, Zhang LP, Ren GS. Silencing of PCDH10 in hepatocellular carcinoma via de novo DNA methylation independent of HBV infection or HBX expression. Clin Exp Med. 2013;13:127–134. doi: 10.1007/s10238-012-0182-9. [DOI] [PubMed] [Google Scholar]
- 175.Vivekanandan P, Thomas D, Torbenson M. Methylation regulates hepatitis B viral protein expression. J Infect Dis. 2009;199:1286–1291. doi: 10.1086/597614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Han YF, Zhao J, Ma LY, Yin JH, Chang WJ, Zhang HW, Cao GW. Factors predicting occurrence and prognosis of hepatitis-B-virus-related hepatocellular carcinoma. World J Gastroenterol. 2011;17:4258–4270. doi: 10.3748/wjg.v17.i38.4258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Johnstone RW, Licht JD. Histone deacetylase inhibitors in cancer therapy: is transcription the primary target? Cancer Cell. 2003;4:13–18. doi: 10.1016/s1535-6108(03)00165-x. [DOI] [PubMed] [Google Scholar]
- 178.Pontisso P, Vidalino L, Quarta S, Gatta A. Biological and clinical implications of HBV infection in peripheral blood mononuclear cells. Autoimmun Rev. 2008;8:13–17. doi: 10.1016/j.autrev.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 179.Wang F, Yuan S, Teng KY, Garcia-Prieto C, Luo HY, Zeng MS, Rao HL, Xia Y, Jiang WQ, Huang HQ, et al. High hepatitis B virus infection in B-cell lymphoma tissue and its potential clinical relevance. Eur J Cancer Prev. 2012;21:261–267. doi: 10.1097/CEJ.0b013e3283498e87. [DOI] [PubMed] [Google Scholar]
- 180.Engels EA, Cho ER, Jee SH. Hepatitis B virus infection and risk of non-Hodgkin lymphoma in South Korea: a cohort study. Lancet Oncol. 2010;11:827–834. doi: 10.1016/S1470-2045(10)70167-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Ulcickas Yood M, Quesenberry CP, Guo D, Caldwell C, Wells K, Shan J, Sanders L, Skovron ML, Iloeje U, Manos MM. Incidence of non-Hodgkin’s lymphoma among individuals with chronic hepatitis B virus infection. Hepatology. 2007;46:107–112. doi: 10.1002/hep.21642. [DOI] [PubMed] [Google Scholar]
- 182.Elbedewy TA, Elashtokhy HE, Rabee ES, Kheder GE. Prevalence and chemotherapy-induced reactivation of occult hepatitis B virus among hepatitis B surface antigen negative patients with diffuse large B-cell lymphoma: significance of hepatitis B core antibodies screening. J Egypt Natl Canc Inst. 2015;27:11–18. doi: 10.1016/j.jnci.2015.01.004. [DOI] [PubMed] [Google Scholar]
- 183.Makvandi K, Ranjbari N, Makvandi M, Ashraf Teimori A, Neisi N, Rasti M, Alipour V, Albokord M, Kanani M, Ahadi R, et al. Study of the Association of Mutant HBsAg Gene and Hodgkin and Non-Hodgkin Lymphoma. Jundishapur J Microbiol. 2015;8:e25726. doi: 10.5812/jjm.25726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Cheung WI, Lin SY, Leung VK, Fung KS, Lam YK, Lo FH, Chau TN. Prospective evaluation of seropositive occult hepatitis B viral infection in lymphoma patients receiving chemotherapy. Hong Kong Med J. 2011;17:376–380. [PubMed] [Google Scholar]
- 185.Slusarczyk J, Małkowski P, Bobilewicz D, Juszczyk G. Cross-sectional, anonymous screening for asymptomatic HCV infection, immunity to HBV, and occult HBV infection among health care workers in Warsaw, Poland. Przegl Epidemiol. 2012;66:445–451. [PubMed] [Google Scholar]
- 186.US Public Health Service. Updated U.S. Public Health Service Guidelines for the Management of Occupational Exposures to HBV, HCV, and HIV and Recommendations for Postexposure Prophylaxis. MMWR Recomm Rep. 2001;50:1–52. [PubMed] [Google Scholar]
- 187.Squadrito G, Spinella R, Raimondo G. The clinical significance of occult HBV infection. Ann Gastroenterol. 2014;27:15–19. [PMC free article] [PubMed] [Google Scholar]
- 188.Borzooy Z, Jazayeri SM, Mirshafiey A, Khamseh A, Mahmoudie MK, Azimzadeh P, Geravand B, Boroumand MA, Afshar M, Poortahmasebi V, et al. Identification of occult hepatitis B virus (HBV) infection and viral antigens in healthcare workers who presented low to moderate levels of anti-HBs after HBV vaccination. Germs. 2015;5:134–140. doi: 10.11599/germs.2015.1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Chiarakul S, Eunumjitkul K, Vorapimol AR, Kaewkungwal J, Chimparlee N, Poovorawan Y. Response of health care workers with isolated antibody to hepatitis B core antigen to hepatitis B vaccine. Southeast Asian J Trop Med Public Health. 2011;42:831–838. [PubMed] [Google Scholar]
- 190.Shim J, Kim KY, Kim BH, Chun H, Lee MS, Hwangbo Y, Jang JY, Dong SH, Kim HJ, Chang YW, et al. Anti-hepatitis B core antibody is not required for prevaccination screening in healthcare workers. Vaccine. 2011;29:1721–1726. doi: 10.1016/j.vaccine.2010.11.044. [DOI] [PubMed] [Google Scholar]
- 191.Sukriti NT, Sethi A, Agrawal K, Agrawal K, Kumar GT, Kumar M, Kaanan AT, Sarin SK. Low levels of awareness, vaccine coverage, and the need for boosters among health care workers in tertiary care hospitals in India. J Gastroenterol Hepatol. 2008;23:1710–1715. doi: 10.1111/j.1440-1746.2008.05483.x. [DOI] [PubMed] [Google Scholar]
- 192.Yen YH, Chen CH, Wang JH, Lee CM, Changchien CS, Lu SN. Study of hepatitis B (HB) vaccine non-responsiveness among health care workers from an endemic area (Taiwan) Liver Int. 2005;25:1162–1168. doi: 10.1111/j.1478-3231.2005.01157.x. [DOI] [PubMed] [Google Scholar]
- 193.Yeo W, Chan TC, Leung NW, Lam WY, Mo FK, Chu MT, Chan HL, Hui EP, Lei KI, Mok TS, et al. Hepatitis B virus reactivation in lymphoma patients with prior resolved hepatitis B undergoing anticancer therapy with or without rituximab. J Clin Oncol. 2009;27:605–611. doi: 10.1200/JCO.2008.18.0182. [DOI] [PubMed] [Google Scholar]
- 194.Coppola N, Tonziello G, Pisaturo M, Messina V, Guastafierro S, Fiore M, Iodice V, Sagnelli C, Stanzione M, Capoluongo N, et al. Reactivation of overt and occult hepatitis B infection in various immunosuppressive settings. J Med Virol. 2011;83:1909–1916. doi: 10.1002/jmv.22199. [DOI] [PubMed] [Google Scholar]
- 195.Pei SN, Chen CH, Lee CM, Wang MC, Ma MC, Hu TH, Kuo CY. Reactivation of hepatitis B virus following rituximab-based regimens: a serious complication in both HBsAg-positive and HBsAg-negative patients. Ann Hematol. 2010;89:255–262. doi: 10.1007/s00277-009-0806-7. [DOI] [PubMed] [Google Scholar]
- 196.Palmore TN, Shah NL, Loomba R, Borg BB, Lopatin U, Feld JJ, Khokhar F, Lutchman G, Kleiner DE, Young NS, et al. Reactivation of hepatitis B with reappearance of hepatitis B surface antigen after chemotherapy and immunosuppression. Clin Gastroenterol Hepatol. 2009;7:1130–1137. doi: 10.1016/j.cgh.2009.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Talotta R, Atzeni F, Sarzi Puttini P. Reactivation of occult hepatitis B virus infection under treatment with abatacept: a case report. BMC Pharmacol Toxicol. 2016;17:17. doi: 10.1186/s40360-016-0060-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Chaulet P. Tuberculosis: a six-month cure. World Health Forum. 1989;10:116–122. [PubMed] [Google Scholar]
- 199.Filippini P, Coppola N, Pisapia R, Scolastico C, Marrocco C, Zaccariello A, Nacca C, Sagnelli C, De Stefano G, Ferraro T, et al. Impact of occult hepatitis B virus infection in HIV patients naive for antiretroviral therapy. AIDS. 2006;20:1253–1260. doi: 10.1097/01.aids.0000232232.41877.2a. [DOI] [PubMed] [Google Scholar]
- 200.Kubo S, Tamori A, Ohba K, Shuto T, Yamamoto T, Tanaka H, Nishiguchi S, Wakasa K, Hirohashi K, Kinoshita H. Previous or occult hepatitis B virus infection in hepatitis C virus-associated hepatocellular carcinoma without hepatic fibrosis. Dig Dis Sci. 2001;46:2408–2414. doi: 10.1023/a:1012359400193. [DOI] [PubMed] [Google Scholar]
- 201.Lalazar G, Rund D, Shouval D. Screening, prevention and treatment of viral hepatitis B reactivation in patients with haematological malignancies. Br J Haematol. 2007;136:699–712. doi: 10.1111/j.1365-2141.2006.06465.x. [DOI] [PubMed] [Google Scholar]
- 202.Kusumoto S, Tanaka Y, Mizokami M, Ueda R. Reactivation of hepatitis B virus following systemic chemotherapy for malignant lymphoma. Int J Hematol. 2009;90:13–23. doi: 10.1007/s12185-009-0359-5. [DOI] [PubMed] [Google Scholar]
- 203.Liang R. How I treat and monitor viral hepatitis B infection in patients receiving intensive immunosuppressive therapies or undergoing hematopoietic stem cell transplantation. Blood. 2009;113:3147–3153. doi: 10.1182/blood-2008-10-163493. [DOI] [PubMed] [Google Scholar]
- 204.Lau GK, Leung YH, Fong DY, Au WY, Kwong YL, Lie A, Hou JL, Wen YM, Nanj A, Liang R. High hepatitis B virus (HBV) DNA viral load as the most important risk factor for HBV reactivation in patients positive for HBV surface antigen undergoing autologous hematopoietic cell transplantation. Blood. 2002;99:2324–2330. doi: 10.1182/blood.v99.7.2324. [DOI] [PubMed] [Google Scholar]
- 205.Ma SY, Lau GK, Cheng VC, Liang R. Hepatitis B reactivation in patients positive for hepatitis B surface antigen undergoing autologous hematopoietic cell transplantation. Leuk Lymphoma. 2003;44:1281–1285. doi: 10.1080/1042819031000083343. [DOI] [PubMed] [Google Scholar]
- 206.Knöll A, Boehm S, Hahn J, Holler E, Jilg W. Reactivation of resolved hepatitis B virus infection after allogeneic haematopoietic stem cell transplantation. Bone Marrow Transplant. 2004;33:925–929. doi: 10.1038/sj.bmt.1704457. [DOI] [PubMed] [Google Scholar]
- 207.Hui CK, Sun J, Au WY, Lie AK, Yueng YH, Zhang HY, Lee NP, Hou JL, Liang R, Lau GK. Occult hepatitis B virus infection in hematopoietic stem cell donors in a hepatitis B virus endemic area. J Hepatol. 2005;42:813–819. doi: 10.1016/j.jhep.2005.01.018. [DOI] [PubMed] [Google Scholar]
- 208.Onozawa M, Hashino S, Izumiyama K, Kahata K, Chuma M, Mori A, Kondo T, Toyoshima N, Ota S, Kobayashi S, et al. Progressive disappearance of anti-hepatitis B surface antigen antibody and reverse seroconversion after allogeneic hematopoietic stem cell transplantation in patients with previous hepatitis B virus infection. Transplantation. 2005;79:616–619. doi: 10.1097/01.tp.0000151661.52601.fb. [DOI] [PubMed] [Google Scholar]
- 209.Aksoy S, Harputluoglu H, Kilickap S, Dede DS, Dizdar O, Altundag K, Barista I. Rituximab-related viral infections in lymphoma patients. Leuk Lymphoma. 2007;48:1307–1312. doi: 10.1080/10428190701411441. [DOI] [PubMed] [Google Scholar]
- 210.Francisci D, Falcinelli F, Schiaroli E, Capponi M, Belfiori B, Flenghi L, Baldelli F. Management of hepatitis B virus reactivation in patients with hematological malignancies treated with chemotherapy. Infection. 2010;38:58–61. doi: 10.1007/s15010-009-9019-1. [DOI] [PubMed] [Google Scholar]
- 211.Seto WK, Chan TS, Hwang YY, Wong DK, Fung J, Liu KS, Gill H, Lam YF, Lie AK, Lai CL, et al. Hepatitis B reactivation in patients with previous hepatitis B virus exposure undergoing rituximab-containing chemotherapy for lymphoma: a prospective study. J Clin Oncol. 2014;32:3736–3743. doi: 10.1200/JCO.2014.56.7081. [DOI] [PubMed] [Google Scholar]
- 212.Hsu C, Tsou HH, Lin SJ, Wang MC, Yao M, Hwang WL, Kao WY, Chiu CF, Lin SF, Lin J, et al. Chemotherapy-induced hepatitis B reactivation in lymphoma patients with resolved HBV infection: a prospective study. Hepatology. 2014;59:2092–2100. doi: 10.1002/hep.26718. [DOI] [PubMed] [Google Scholar]
- 213.Dominguez N, Manzano ML, Muñoz R, Martin A, Fernandez I, Castellano G. Late reactivation of occult hepatitis B virus infection in a patient with chronic lymphocytic leukemia after rituximab and fludarabine-based regimen. Leuk Lymphoma. 2015;56:1160–1163. doi: 10.3109/10428194.2014.947978. [DOI] [PubMed] [Google Scholar]
- 214.Liu JY, Sheng YJ, Ding XC, Tang H, Tong SW, Zhang DZ, Zhou Z, Hu P, Liao Y, Ren H, et al. The efficacy of lamivudine prophylaxis against hepatitis B reactivation in breast cancer patients undergoing chemotherapy: a meta-analysis. J Formos Med Assoc. 2015;114:164–173. doi: 10.1016/j.jfma.2012.10.007. [DOI] [PubMed] [Google Scholar]
- 215.Madaliński K, Sylvan SP, Hellstrom U, Mikołajewicz J, Dzierzanowska-Fangrat K. Presence of anti-preS1, anti-preS2, and anti-HBs antibodies in newborns immunized with Bio-Hep-B vaccine. Med Sci Monit. 2004;10:PI10–PI17. [PubMed] [Google Scholar]
- 216.Ge G, Wang S, Han Y, Zhang C, Lu S, Huang Z. Removing N-terminal sequences in pre-S1 domain enhanced antibody and B-cell responses by an HBV large surface antigen DNA vaccine. PLoS One. 2012;7:e41573. doi: 10.1371/journal.pone.0041573. [DOI] [PMC free article] [PubMed] [Google Scholar]


