Abstract
AIM
To collect the evidence to estimate the correlation between smoking and the incidence of dry eye.
METHODS
The PubMed, EMBASE, the Cochrane Central Register of Controlled Trials (CENTRAL, last issue), CBM (Chinese BioMedical Literature Database), and CNKI (China National Knowledge Infrastructure/Chinese Academic Journals full-text Database) were searched for eligible studies published from January 1964 to December 2015 to investigate the association of smoking with the risk of dry eye. The odds ratio (OR) and 95% confidence interval (CI) were summarized and calculated. The extracted studies were pooled by the fixed-effects model or a random-effects model.
RESULTS
Two cohort studies and eight cross-sectional surveys were included in our Meta-analysis. There was no statistically significant relationship between current (OR=1.32; 95% CI: 0.99-1.76; P=0.055) or ever smoking (OR=1.12; 95% CI: 0.98-1.28; P=0.107) and the risk of dry eye among the studies, even when age and gender were adjusted (OR=1.16; 95% CI: 0.83-1.64; P=0.383). In the sensitivity analysis in which only general population were included, the association was significant between smoking and dry eye (OR=1.50; 95% CI: 1.08-2.09; P=0.016).
CONCLUSION
This Meta-analysis suggests that smoking may associate with the risk of dry eye in general population.
Keywords: dry eye, smoking, Meta-analysis
INTRODUCTION
Dry eye is a multifactorial disease characterized by ocular surface changes which result in tear film impairment, eye itchiness, redness, light hypersensitivity, blurred vision, and other symptoms and/or discomforts[1]–[2]. Dry eye is estimated to affect 5%-35% of worldwide population at various ages with increasing frequency[3]. In the United States, moderate and/or severe dry eye affected more than 3.2 million of female and 1.6 million of male population at the age of above 50 years old[4]–[5]. In China, the incidence of dry eye is also increasing because of air pollution, the popularization of computer and mobile phone, and rapid aging of the population, which is becoming an increasingly significant public health problem.
Dry eye is associated with many risk factors such as environment, lifestyle, age, sex, drug history, and systemic diseases, among which the lifestyle factors may play an important role[3]. Smoking is already known as an important risk factor for many chronic diseases and however is still an unclear risk factor of dry eye[3]. A number of studies evaluated the association between smoking and dry eye risk[6]–[19], which show that smoking could increase the risk of dry eye[12]–[13],[17]–[18]. However, other researches showed disputed results[7]–[8],[10]–[11],[14]–[15],[19]. The definition of dry eye was suggested according to tear break-up time (TBUT) and Schirmer score[2], and smoking was found to decrease TBUT in some of the studies[6],[9],[16], in which Sayin et al[9] found the decreasing of Schirmer score in smokers. Among the analyses, most of them showed their investigations were performed in specific populations. However, these results may not be representative of the larger population. Therefore, this Meta-analysis aims to summarize the association between smoking and the risk of dry eye, and to provide useful evidence for this association.
MATERIALS AND METHODS
Literature Search
The PubMed, EMBASE, The Cochrane Central Register of Controlled Trials (CENTRAL, last issue), CBM (Chinese BioMedical Literature Database) and CNKI (China National Knowledge Infrastructure/Chinese Academic Journals full-text Database) were searched for relevant articles published from January 1964 to December 2015. Our search strategies of PubMed and EMBASE are provided by Tables 1 and 2. We also searched the references which listed in the retrieved studies to find additional related articles.
Table 1. PubMed search strategy.
| No. | Search strategy1 |
| 1 | “Tobacco”[Mesh] OR “Smoking”[Mesh] |
| 2 | Smok*[tiab] OR tobacco[tiab] OR cigarette[tiab] OR nicotiana*[tiab] OR lifestyle*[tiab] |
| 3 | 1 OR 2 |
| 4 | “Dry Eye Syndromes”[Mesh] OR “Meibomian Glands”[Mesh] |
| 5 | dry eye*[tiab] OR xerophthalmi*[tiab] OR meibomian gland dysfunction[tiab] OR MGD[tiab] |
| 6 | 4 OR 5 |
| 7 | “Case-Control Studies”[Mesh] OR “Cohort Studies”[Mesh] OR “Cross-Sectional Studies”[Mesh] |
| 8 | Case control [tiab] OR case comparison[tiab] OR case compeer[tiab] OR case referrent*[tiab] OR case base [tiab] OR retrospective stud*[tiab] OR cohort[tiab] OR concurrent stud*[tiab] OR incidence[tiab] OR longitudinal stud*[tiab] OR follow up[tiab] OR prospective stud*[tiab] OR cross sectional[tiab] OR disease frequency[tiab] OR prevalence[tiab] |
| 9 | 7 OR 8 |
| 10 | 3 AND 6 AND 9 |
1Database: PubMed (inception to December 2015).
Table 2. EMBASE search strategy.
| No. | Search strategy1 |
| 1 | exp tobacco/ OR exp smoking/ |
| 2 | (smok* OR tobacco OR cigarette OR nicotiana* OR lifestyle*).mp |
| 3 | 1 OR 2 |
| 4 | Exp dry eye/ OR exp xerophthalmia/ OR exp meibomian gland/ |
| 5 | (Dry eye* OR xerophthalmi* OR meibomian gland dysfunction OR MGD).mp |
| 6 | 4 OR 5 |
| 7 | Exp case control study/ OR exp cohort analysis/ OR exp cross-sectional study/ |
| 8 | (Case control OR case comparison OR case compeer OR case referrent* OR case base OR retrospective stud* OR cohort OR concurrent stud* OR incidence OR longitudinal stud* OR follow up OR prospective stud* OR cross sectional OR disease frequency OR prevalence).mp |
| 9 | 7 OR 8 |
| 10 | 3 AND 6 AND 9 |
1Database: EMBASE (OvidSP) (1974 to 2015 December).
Study Selection
For our Meta-analysis, articles fulfilled these inclusion criteria were selected: 1) cross-sectional, case-control or cohort study design; 2) estimation of the association between smoking and dry eye risk; 3) reporting of data adequate to estimate relative risk (RR) and/or odds ratio (OR) with a 95% confidence interval (95% CI). And the exclusion criteria were as follows: 1) repeated publications; 2) non-original literature (e.g. comment, letter, review, etc.). In cases of the publication overlapped, we only used the studies with the largest sample size. And it had no language limitations for the publications.
Data Extraction
The following information from each included studies were extracted: first author, publication year, country, years of follow-up or the study period, study design, age range, the sample size, smoking exposure status, the ORs with corresponding 95% CIs, and the adjusted variables. The status of smoking exposure (i.e. current and/or ever smoking) was taken from each of the articles directly.
The data extraction was performed independently by two authors (Xu L and Zhu XY) who resolved the disagreements by discussions between them. The final decision was made by a third investigator (Zhang W) if no consensus could be achieved.
Statistical Analysis
In our Meta-analysis, the association of smoking with dry eye was investigated, with or without the adjustment of age and gender. Then, to pool a risk estimate, we extracted the ORs of dry eye related to smoking from individual studies and weighted log risk estimates by the inverse of their variances. Among the included studies, heterogeneity was detected using Q-test. Studies were pooled using a Mantel-Haenszel fixed-effects model or a DerSimonian and Laird random-effects model depending on the heterogeneity[20]. In addition, for the control of potential bias, sensitivity analysis was performed. Egger's regression asymmetry test was performed to examine the possible publication bias with a funnel plot of log [OR] against its standard error (SE) visually.
All statistical analyses were completed by the statistical analysis software STATA 11.2 (Stata Corporation, College Station, TX, USA). A P value less than 0.05 was defined as statistically significance for the pooled ORs, while the significance level was 0.10 for the test of heterogeneity and publication bias. All the tests were two sided.
RESULTS
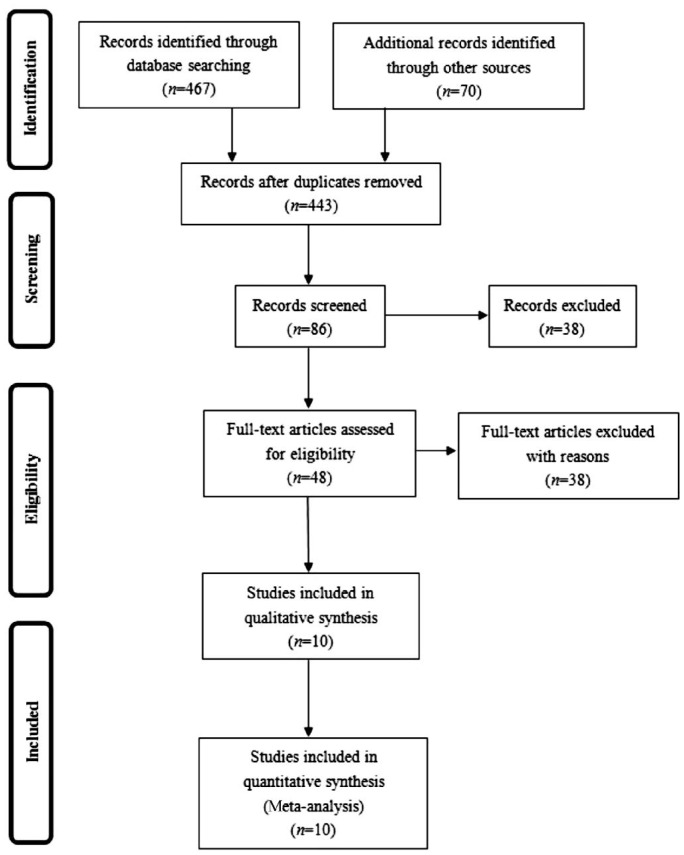
Ten studies[7]–[8],[10]–[14],[17]–[18],[21] which fulfilled the inclusion criteria were identified (refer to the flow diagram in Figure 1), including two cohort studies[10],[13] and eight cross-sectional surveys[7]–[8],[11]–[12],[14],[17]–[18],[21]. Two cohort studies[10],[13] were both from the United States. Three of the eight cross-sectional surveys included[17]–[18],[21] were from China, two[7],[14] from Japan, one[8] from India, one[11] from Australia, and one[12] from Indonesia. The study samples included in the Meta-analysis were summarized in Table 3.
Figure 1. PRISMA flow diagram.
Table 3. Summary of the ten studies included in this Meta-analysis with regard to the smoking status and dry eye risk.
| First author | Year | Country | Population | Study design | Age range (a) | n | Smoking exposure status | OR (95% CI) | Adjusted age and gender |
| Uchino[7] | 2009 | Japan | Office workers who use visual display terminals | Cross-sectional survey | 22-60 | 3549 | Current | 0.77 (0.53-1.12) | Y |
| Sahai[8] | 2005 | India | Hospital-based population | Cross-sectional survey | >20 | 500 | Current | 1.42 (0.89-2.27) | - |
| Moss[10] | 2008 | USA | Population-based | Cohort study | 43-86 | 2414 | Current | 0.89 (0.65-1.20) | - |
| Ever | 1.06 (0.86-1.30) | - | |||||||
| Chia[11] | 2003 | Australia | Population-based | Cross-sectional survey | ≥49 | 1075 | Current | 0.70 (0.40-1.10) | Y |
| Lee[12] | 2002 | Indonesia | Households | Cross-sectional survey | ≥21 | 1058 | Current | 1.50 (1.00-2.20) | Y |
| Ever | 1.20 (0.60-2.40) | - | |||||||
| Moss[13] | 2000 | USA | Population-based | Cohort study | 43-84 | 3703 | Current | 1.44 (1.13-1.83) | Y |
| Ever | 1.16 (0.96-1.39) | - | |||||||
| Uchino[14] | 2013 | Japan | Office workers who use visual display terminals | Cross-sectional survey | 22-65 | 561 | Current | 0.86 (0.54-1.35) | Y |
| Xiao[17] | 2011 | China | Smoker and non-smoker (man) | Cross-sectional survey | 25-75 | 2385 | Current | 2.24 (1.78-2.81) | - |
| Su[18] | 2012 | China | Students | Cross-sectional survey | 19-26 | 1168 | Current | 2.57 (1.41-4.67) | - |
| Hua[21] | 2014 | China | Population-based | Cross-sectional survey | 12-88 | 2600 | Current | 2.26 (1.50-3.40) | Y |
Current Smokers
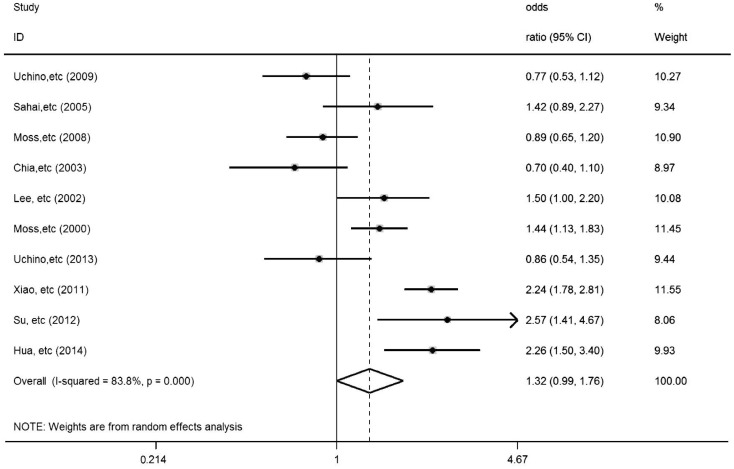
All ten studies[7]–[8],[10]–[14],[17]–[18],[21] in which two cohort studies[10],[13] and eight cross-sectional surveys[7]–[8],[11]–[12],[14],[17]–[18],[21] were included in the analysis of the relationship between current smoking and the risk of dry eye, among which six studies[7],[11]–[14],[21] adjusted variables including age and gender, and seven studies[10]–[13],[17]–[18],[21] were population-based studies (Table 4). It was found that the association between current smoking (OR=1.32; 95% CI: 0.99-1.76; P=0.055) and increased risk of dry eye was not statistically significant (Figure 2). Statistically significant heterogeneity (Q=55.42, P=0.000) was found across the studies.
Table 4. Statistical results of the included studies.
| Groups | Reference No. | OR (95% CI) | P | Heterogeneity test |
|
| Q | P | ||||
| Current smoking | 7-8,10-14,17-18,21 | 1.32 (0.99-1.76) | 0.055 | 55.42 | 0.000 |
| Sensitivity analysis (1) | 7,11-14,21 | 1.16 (0.83-1.64) | 0.383 | 23.24 | 0.000 |
| Sensitivity analysis (2) | 6,10-13 | 1.50 (1.08-2.09) | 0.016 | 38.45 | 0.000 |
| Ever smoking | 9,11-12 | 1.12 (0.98-1.28) | 0.107 | 0.45 | 0.800 |
Sensitivity analysis (1): Only the studies which adjusted age and gender were included; Sensitivity analysis (2): Only general population were included.
Figure 2. In ten included studies (two cohort studies and eight cross-sectional surveys), risk estimates of dry eye associated with current cigarette smoking.
Squares indicate study-specific risk estimates (size of square reflects study-specific statistical weight, i.e. inverse of the variance); horizontal lines indicate 95% CIs; diamonds indicate summary risk estimates with its corresponding 95% CI.
Ever Smokers
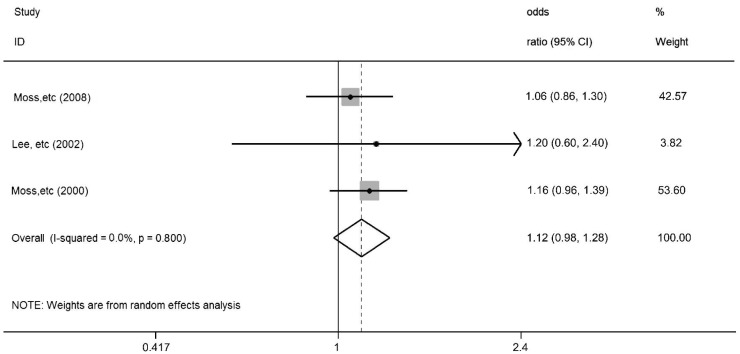
Three studies[10],[12]–[13] in which two cohort studies and one cross-sectional survey was included in the analysis of the relationship between ever smoking and dry eye risk (Table 4). It was found that the association between ever smoking (OR=1.12; 95% CI: 0.98-1.28; P=0.107) and increased risk of dry eye was also not statistically significant (Figure 3). Statistically significant heterogeneity (Q=0.45, P=0.800) was not found across the studies.
Figure 3. In three included studies (two cohort studies and one cross-sectional survey), risk estimates of dry eye associated with ever cigarette smoking.
Squares indicate study-specific risk estimates (size of square reflects study-specific statistical weight, i.e. inverse of the variance); horizontal lines indicate 95% CIs; diamonds indicate summary risk estimates with its corresponding 95% CI.
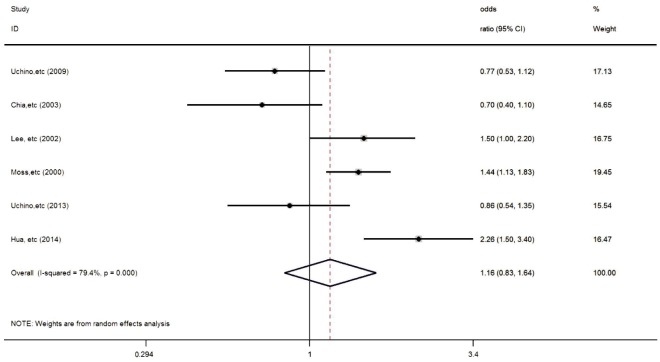
Adjusted Age and Gender
When only the studies which adjusted age and gender were included[7],[11]–[14],[21], the result showed no statistically significant relationship between current smoking and dry eye (OR=1.16; 95% CI: 0.83-1.64; P=0.383) (Figure 4). The heterogeneity across the studies was not significantly changed by Q test (Q=24.23, P=0.000).
Figure 4. In six included studies (one cohort study and five cross-sectional surveys), risk estimates of dry eye associated with current cigarette smoking which adjusted age and gender.
Squares indicate study-specific risk estimates (size of square reflects study-specific statistical weight, i.e. inverse of the variance); horizontal lines indicate 95% CIs; diamonds indicate summary risk estimates with its corresponding 95% CI.
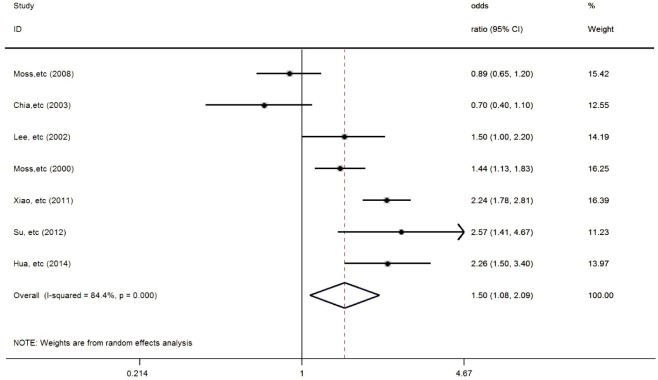
General Population
In the sensitivity analysis in which only general population were included[10]–[13],[17]–[18],[21], the result showed statistically significant relationship between current smoking and dry eye (OR=1.50; 95% CI: 1.08-2.09; P=0.016) (Figure 5). The heterogeneity across the studies was not significantly changed by Q test (Q=38.45, P=0.000).
Figure 5. In seven included studies (two cohort studies and five cross-sectional surveys), risk estimates of dry eye associated with current cigarette smoking.
Squares indicate study-specific risk estimates (size of square reflects study-specific statistical weight, i.e. inverse of the variance); horizontal lines indicate 95% CIs; diamonds indicate summary risk estimates with its corresponding 95% CI.
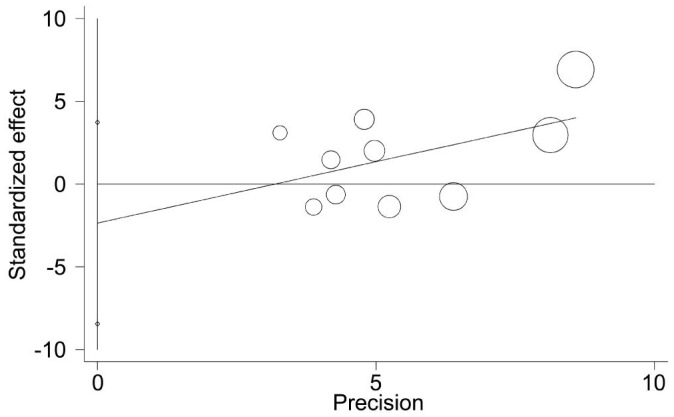
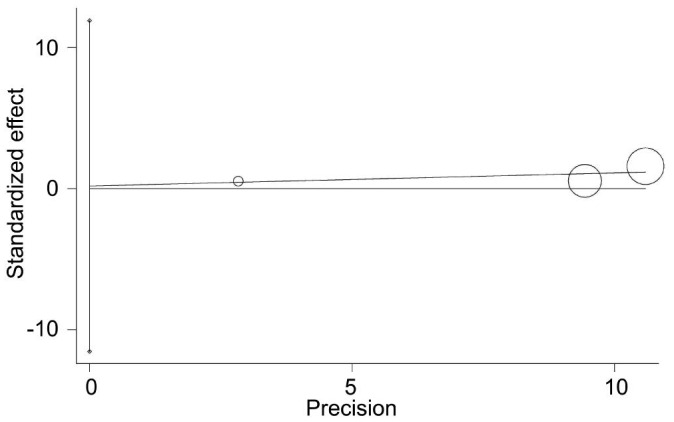
Furthermore, Egger's regression asymmetry test was performed to detect the possible publication bias. It revealed no statistically significant publication bias for the association between current smoking and dry eye (P=0.397) (Figure 6), even when only the studies which adjusted age and gender (P=0.383) or in the sensitivity analysis in which only general population were included (P=0.706). No statistically significant asymmetry was also not detected for association between ever smoking and dry eye (P=0.875) which indicating an absence of substantial publication bias (Figure 7).
Figure 6. A funnel plot, showing no publication bias of ten included studies (two cohort studies and eight cross-sectional surveys) as assessed by Egger's test in this Meta-analysis.
Figure 7. A funnel plot, showing no publication bias of three included studies (two cohort studies and one cross-sectional survey) as assessed by Egger's test in this Meta-analysis.
DISCUSSION
In our primary Meta-analysis, the effect of smoking on dry dye was evaluated. Our results showed no significant association between current smoking and increased risk of dry eye, but the P value was close to 0.05 (P=0.055). We also found no significant association in the analyses on ever smoking (P=0.107).
Several pathogenesis of dry eye including chronic inflammation of the ocular surface, decreased sensitivity of cornea and conjunctiva, reduction of production and/or stability of tears, and epithelial damage have been suggested[1]–[2]. As mentioned, smoking is a well-known risk factor for many chronic diseases, which also affects the eyes. The health of the eye could be affected by smoking toxins which decrease blood flow and/or accelerate thrombus formation in ocular capillaries[22]. Cigarette smoking may also cause a higher risk of many eye diseases such as cataracts, age-related macular degeneration, glaucoma, diabetic retinopathy, and optic neuritis[22], but the relationship between smoking and the risk of dry eye was still unclear. The pooled analysis by Thomas et al[16]. and some other studies[6],[9] found that the tear stability and the sensitivity of cornea and conjunctiva could be decreased by smoking which also showed the decreased TBUT. Also, for dry eye patients, smoking had been reported to induce discomforts including burning and foreign body sensation of the eyes[23]–[24]. But for the results of Schirmer score, it showed no significant change[6],[16]. On the International Dry Eye Workshop 2007, the diagnostic criteria of dry eye were suggested to be TBUT ≤10s and Schirmer score performed without anesthesia ≤5 mm in 5min[2]. The possible explanation is that there were no clear diagnostic criteria of dry eye in the studies or just using questionnaire. It may affect the association between dry eye and smoking of some studies, thus cause the bias.
Dry eye is associated with many risk factors such as environment as mentioned. Among the risk factor of dry eye, older age and female sex were two of the most aconsistent ones[3],[25]. The effect of sex hormones on the homeostasis of ocular surface had been acknowledged. It was reported by Sullivan et al. that androgen levels decrease with advancing age in both males and females[26]. Clinically, patients suffering from sex hormone deficiency including congenital androgen insufficiency syndrome[27]–[28], Sjogren's syndrome[29], premature ovarian failure[30], and those receiving anti-androgen medications[31]–[33] usually had higher risk of dry eye. Also, it is known that smoking is more prevalent in male population than female. Five studies in which adjusted age and gender were included in the analysis[7],[11]–[14]. When age and gender were adjusted, it also showed no statistically significant relationship between current smoking and dry eye (OR=1.16; 95% CI: 0.83-1.64; P=0.383).
Apart from age and sex, environment may also affect the incidence of dry eye. For example, the office workers who use visual display terminals (VDTs)[34] and glaucoma patient who use anti-glaucoma medication[35] were found to have higher risk of dry eye. In this Meta-analysis, the result of no significant association was changed between current smoking and dry eye when only the studies which sample is general population were included. The possible explanation for the inconsistency of the result is that some of the studies included in our primary Meta-analysis were related to the populations exposed to other risk factors of dry eye such as the use of VDTs, or the studies were related to specific population such as hospital-based population.
Several strengths and limitations of this Meta-analysis should be understood for proper interpretation of the results and findings. For the strengths, the first is this Meta-analysis included the studies in several important English databases published from January 1964 to December 2015. Second, the adjustment of age and gender and the subgroup analysis of general population were performed to avoid the bias of different age and sex, and to reduce the influence of different population including the patients of other eye diseases and/or visual display terminal users, and positive results was found in the analysis of general population. The most important is that the result of this Meta-analysis may be helpful to the ophthalmologists' suggestion of lifestyle on dry eye patients. For the limitations, the first is that most of the articles included are cross-sectional surveys which may affect the quality of this analysis. Second, our results were probably be affected by misclassification of smoking, and we did not include the studies related to passive smoking. And our results may be affected by different factors although we did sensitivity analysis of general populations and adjusted age and gender. Third, among the studies included, some of them showed different or unclear diagnostic criteria and/or types of dry eye, which may also affect our results. The statistically significant heterogeneity showed by our result could not be avoided. In addition, present data were inadequate to carry out dose-dependent risk estimation.
In summary, this Meta-analysis of all ten studies shows negative association between current and/or ever smoking and increasing risk of dry eye. But when only the studies which sample is general population were included, it showed statistically significant relationship between current smoking and dry eye. The findings would be possible to indicate that smoking may associate with the risk of dry eye in general population which may be helpful to the ophthalmologists' suggestion on dry eye patients. This Meta-analysis cannot explore the association between different types of dry eye and smoking due to the limitation of data in this study. Therefore, further investigations and Meta-analysis are needed to validate the role for smoking in the incidence of dry eye.
Acknowledgments
Foundations: Supported by National Natural Science Foundation (No.81370992; No.81570812); Research Foundation of Shanghai Science and Technology Committee (No.14411960600).
Conflicts of Interest: Xu L, None; Zhang W, None; Zhu XY, None; Suo T, None; Fan XQ, None; Fu Y, None.
REFERENCES
- 1.Mantelli F, Massaro-Giordano M, Macchi I, Lambiase A, Bonini S. The cellular mechanisms of dry eye: from pathogenesis to treatment. J Cell Physiol. 2013;228(12):2253–2256. doi: 10.1002/jcp.24398. [DOI] [PubMed] [Google Scholar]
- 2.The definition and classification of dry eye disease: report of the Definition and Classification Subcommittee of the International Dry Eye WorkShop (2007) Ocul Surf. 2007;5(2):75–92. doi: 10.1016/s1542-0124(12)70081-2. [DOI] [PubMed] [Google Scholar]
- 3.The epidemiology of dry eye disease: report of the Epidemiology Subcommittee of the International Dry Eye WorkShop (2007) Ocul Surf. 2007;5(2):93–107. doi: 10.1016/s1542-0124(12)70082-4. [DOI] [PubMed] [Google Scholar]
- 4.Schaumberg DA, Sullivan DA, Buring JE, Dana MR. Prevalence of dry eye syndrome among US women. Am J Ophthalmol. 2003;136(2):318–326. doi: 10.1016/s0002-9394(03)00218-6. [DOI] [PubMed] [Google Scholar]
- 5.Christen WG, Gaziano JM, Hennekens CH. Design of Physicians' Health Study II--a randomized trial of beta-carotene, vitamins E and C, and multivitamins, in prevention of cancer, cardiovascular disease, and eye disease, and review of results of completed trials. Ann Epidemiol. 2000;10(2):125–134. doi: 10.1016/s1047-2797(99)00042-3. [DOI] [PubMed] [Google Scholar]
- 6.Lee SY, Petznick A, Tong L. Associations of systemic diseases, smoking and contact lens wear with severity of dry eye. Ophthalmic Physiol Opt. 2012;32(6):518–526. doi: 10.1111/j.1475-1313.2012.00931.x. [DOI] [PubMed] [Google Scholar]
- 7.Uchino M, Uchino Y, Dogru M, Schaumberg DA, Tsubota K. Dry eye disease in Japan: an epidemiologic study. Cornea. 2009;28(11):S31–S34. [Google Scholar]
- 8.Sahai A, Malik P. Dry eye: prevalence and attributable risk factors in a hospital-based population. Indian J Ophthalmol. 2005;53(2):87–91. doi: 10.4103/0301-4738.16170. [DOI] [PubMed] [Google Scholar]
- 9.Sayin N, Kara N, Pekel G, Altinkaynak H. Effects of chronic smoking on central corneal thickness, endothelial cell, and dry eye parameters. Cutan Ocul Toxicol. 2014;33(3):201–205. doi: 10.3109/15569527.2013.832688. [DOI] [PubMed] [Google Scholar]
- 10.Moss SE, Klein R, Klein BE. Long-term incidence of dry eye in an older population. Optom Vis Sci. 2008;85(8):668–674. doi: 10.1097/OPX.0b013e318181a947. [DOI] [PubMed] [Google Scholar]
- 11.Chia EM, Mitchell P, Rochtchina E, Lee AJ, Maroun R, Wang JJ. Prevalence and associations of dry eye syndrome in an older population: the Blue Mountains Eye Study. Clin Experiment Ophthalmol. 2003;31(3):229–232. doi: 10.1046/j.1442-9071.2003.00634.x. [DOI] [PubMed] [Google Scholar]
- 12.Lee AJ, Lee J, Saw SM, Gazzard G, Koh D, Widjaja D, Tan DT. Prevalence and risk factors associated with dry eye symptoms: a population based study in Indonesia. Br J Ophthalmol. 2002;86(12):1347–1351. doi: 10.1136/bjo.86.12.1347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moss SE, Klein R, Klein BE. Prevalence of and risk factors for dry eye syndrome. Arch Ophthalmol. 2000;118(9):1264–1268. doi: 10.1001/archopht.118.9.1264. [DOI] [PubMed] [Google Scholar]
- 14.Uchino M, Yokoi N, Uchino Y, Dogru M, Kawashima M, Komuro A, Sonomura Y, Kato H, Kinoshita S, Schaumberg DA, Tsubota K. Prevalence of dry eye disease and its risk factors in visual display terminal users: The Osaka study. Am J Ophthalmol. 2013;156(4):759–766. doi: 10.1016/j.ajo.2013.05.040. [DOI] [PubMed] [Google Scholar]
- 15.Bukhari A, Ajlan R, Alsaggaf H. Prevalence of dry eye in the normal population in Jeddah, Saudi Arabia. Orbit. 2009;28(6):392–397. doi: 10.3109/01676830903074095. [DOI] [PubMed] [Google Scholar]
- 16.Thomas J, Jacob GP, Abraham L, Noushad B. The effect of smoking on the ocular surface and the precorneal tear film. Australas Med J. 2012;5(4):221–226. doi: 10.4066/AMJ.2012.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xiao XL, Ye JZ, Wei FB, Xu JZ. Prevalence of dry eye in the smoking population in Liuzhou, Guangxi Province. Guide of China Medicine. 2011;9(19):236–237. [Google Scholar]
- 18.Su DX, Ma LL, Zhang LS. The investigation and research of prevalence of xeroma in a certain school. Chinese Journal of Clinical Rational Drug Use. 2012;5(20):35–37. [Google Scholar]
- 19.Tian YJ, Liu Y, Zou HD, Fu J, Shen BJ, Wang WW, Xu X. The epidemiologic study of dry eye in Beixinjing district of Shanghai. Chinese Journal of Practical Ophthalmology. 2009;27(7):776–780. [Google Scholar]
- 20.DerSimonian R, Kacker R. Random-effects model for meta-analysis of clinical trials: an update. Contemp Clin Trials. 2007;28(2):105–114. doi: 10.1016/j.cct.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 21.Hua R, Yao K, Hu Y, Chen L. Discrepancy between subjectively reported symptoms and objectively measured clinical findings in dry eye: a population based analysis. BMJ Open. 2014;4(8):e005296. doi: 10.1136/bmjopen-2014-005296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Timothy CO, Nneli RO. The effects of cigarette smoking on intraocular pressure and arterial blood pressure of normotensive young Nigerian male adults. Niger J Physiol Sci. 2007;22(1–2):33–36. [PubMed] [Google Scholar]
- 23.Altinors DD, Akca S, Akova YA, Bilezikçi B, Goto E, Dogru M, Tsubota K. Smoking associated with damage to the lipid layer of the ocular surface. Am J Ophthalmol. 2006;141(6):1016–1021. doi: 10.1016/j.ajo.2005.12.047. [DOI] [PubMed] [Google Scholar]
- 24.Matsumoto Y, Dogru M, Goto E, Sasaki Y, Inoue H, Saito I, Shimazaki J, Tsubota K. Alterations of the tear film and ocular surface health in chronic smokers. Eye (Lond) 2008;22(7):961–968. doi: 10.1038/eye.2008.78. [DOI] [PubMed] [Google Scholar]
- 25.Schaumberg DA, Uchino M, Christen WG, Semba RD, Buring JE, Li JZ. Patient reported differences in dry eye disease between men and women: impact, management, and patient satisfaction. PLoS One. 2013;8(9):e76121. doi: 10.1371/journal.pone.0076121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sullivan BD, Evans JE, Dana MR, Sullivan DA. Influence of aging on the polar and neutral lipid profiles in human meibomian gland secretions. Arch Ophthalmol. 2006;124(9):1286–1292. doi: 10.1001/archopht.124.9.1286. [DOI] [PubMed] [Google Scholar]
- 27.Sullivan BD, Evans JE, Cermak JM, Krenzer KL, Dana MR, Sullivan DA. Complete androgen insensitivity syndrome: effect on human meibomian gland secretions. Arch Ophthalmol. 2002;120(12):1689–1699. doi: 10.1001/archopht.120.12.1689. [DOI] [PubMed] [Google Scholar]
- 28.Cermak JM, Krenzer KL, Sullivan RM, Dana MR, Sullivan DA. Is complete androgen insensitivity syndrome associated with alterations in the meibomian gland and ocular surface? Cornea. 2003;22(6):516–521. doi: 10.1097/00003226-200308000-00006. [DOI] [PubMed] [Google Scholar]
- 29.Sullivan DA, Belanger A, Cermak JM, Berube R, Papas AS, Sullivan RM, Yamagami H, Dana MR, Labrie F. Are women with Sjögren's syndrome androgen-deficient? J Rheumatol. 2003;30(11):2413–2419. [PubMed] [Google Scholar]
- 30.Smith JA, Vitale S, Reed GF, Grieshaber SA, Goodman LA, Vanderhoof VH, Calis KA, Nelson LM. Dry eye signs and symptoms in women with premature ovarian failure. Arch Ophthalmol. 2004;122(2):151–156. doi: 10.1001/archopht.122.2.151. [DOI] [PubMed] [Google Scholar]
- 31.Sullivan BD, Evans JE, Krenzer KL, Reza Dana M, Sullivan DA. Impact of antiandrogen treatment on the fatty acid profile of neutral lipids in human meibomian gland secretions. J Clin Endocrinol Metab. 2000;85(12):4866–4873. doi: 10.1210/jcem.85.12.7066. [DOI] [PubMed] [Google Scholar]
- 32.Krenzer KL, Dana MR, Ullman MD, Cermak JM, Tolls DB, Evans JE, Sullivan DA. Effect of androgen deficiency on the human meibomian gland and ocular surface. J Clin Endocrinol Metab. 2000;85(12):4874–4882. doi: 10.1210/jcem.85.12.7072. [DOI] [PubMed] [Google Scholar]
- 33.Sullivan DA. Androgen deficiency & dry eye syndromes. Arch Soc Esp Oftalmol. 2004;79(2):49–50. [PubMed] [Google Scholar]
- 34.Kawashima M, Yamatsuji M, Yokoi N, Fukui M, Ichihashi Y, Kato H, Nishida M, Uchino M, Kinoshita S, Tsubota K. Screening of dry eye disease in visual display terminal workers during occupational health examinations: The Moriguchi study. J Occup Health. 2015;57(3):253–258. doi: 10.1539/joh.14-0243-OA. [DOI] [PubMed] [Google Scholar]
- 35.Chen HY, Lin CL, Tsai YY, Kao CH. Association between Glaucoma Medication Usage and Dry Eye in Taiwan. Optom Vis Sci. 2015;92(9):e227–e232. doi: 10.1097/OPX.0000000000000667. [DOI] [PubMed] [Google Scholar]