Abstract
AIM
To quantify the association between alcohol consumption and dry eye syndrome (DES) with Meta-analysis of published case-control and cross-sectional studies.
METHODS
Three databases were screened for potentially eligible studies through Nov. 30, 2015, PubMed, Web of Science, and the Cochrane Library. Odds ratios (ORs) were pooled with 95% confidence intervals (CIs) to evaluate the relationship between alcohol consumption and DES risk. Subgroup analyses were performed according to diagnostic criteria, publication year, sample size, alcohol intake and adjusted factors.
RESULTS
A total of 10 (9 case-control and 1 cross-sectional) studies from 8 articles were included in this Meta-analysis. The pooled results showed that alcohol consumption would significantly increase the risk of DES (OR 1.15, 95% CI: 1.02-1.30), and the results were independent of smoking, hypertension, diabetes and thyroid disease history. And the results of subgroup analyses indicated an increased incidence of DES diagnosed by typical DES symptoms and positive objective tests together (OR 1.18, 95% CI: 1.01-1.39) among drinkers, but not by typical DES symptoms alone (OR 1.11, 95% CI: 0.94-1.32). What's more, any drinkers were at higher risk of suffering from DES (OR 1.33, 95% CI: 1.31-1.34), while heavy drinkers not (OR 1.01, 95% CI: 0.86-1.18).
CONCLUSION
The present Meta-analysis suggests that alcohol consumption may be a significant risk factor for DES. Alcohol-induced peripheral neuropathymay falsely reduce the prevalence of DES among heavy drinkers. Future prospective studies of alcohol consumption and DES risk are needed to confirm our results.
Keywords: dry eye syndrome, alcohol consumption, Meta-analysis
INTRODUCTION
Dry eye syndrome (DES) is an ocular surface disorder characterized by eye discomfort, visual disturbance, tear film instability, destruction and inflammation of the ocular surface, and high tears osmolarity[1]. The prevalence of DES ranges from 7.8% to 33.7%, as documented in large etiological research studies[2]. In addition to physical comfortableness, patients also suffer from significant socioeconomic factors, such as increased healthcare costs and impaired vision-related quality-of-life issues[3]. In the past few decades, various population-based studies have been designed to explore the potential risk factors of DES[4]–[10], many of which indicated that alcohol consumption may play an important role in DES development[7],[9].
In addition to the significant cost burden and impaired social ability, alcohol consumption has been proven to be significantly related to a variety of diseases[10]–[11], while the association between alcohol and the risk of DES still remains unclear. For the past few decades, researchers have held controversial opinions about this topic: Chia et al[10] argued that drinking may play a protective role in the development of DES; on the contrary, Galor et al[7] showed that drinking was related to an increased risk of DES; others held the opinion that DES may have nothing to do with alcohol consumption[3]–[6],[8]. Given the fact that individual studies may be limited because of sample size, we therefore conducted this Meta-analysis to quantitively describe the relationship between alcohol consumption and DES.
MATERIALS AND METHODS
This Meta-analysis was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement checklist[11].
Search Strategy and Study Selection
Primary systemic literature searches were performed using the following three databases: PubMed, Web of Science, and the Cochrane Library, covering studies published until Nov. 30, 2015. The primary search strategy included DES (“dry eye”, “xerophthalmia” and “keratoconjunctivitissicca”), alcohol (“alcohol” and “drinking”), and humanstudies. Taking the PubMed database as a sample, the primary search item was “alcohol consumption [Title/Abstract]” OR “alcohol abuse [Title/Abstract]” OR “drinking [Title/Abstract]” AND “dry eye [Title/Abstract]” OR “xerophthalmia [Title/Abstract]” OR “keratoconjunctivitissicca [Title/Abstract]” AND “Human [Mesh]”. Considering that some epidemiologic studies on risk factors of DES may not include alcohol in their titles and abstracts, even though they have evaluated the relationship in their text, we took risk factors (“risk factors”), DES (“dry eye”, “xerophthalmia” and “keratoconjunctivitissicca”), and human studies as our secondary search strategy to avoid omission. Taking the PubMed database as a sample, the secondary search item was “risk factors [Title/Abstract]” AND “dry eye [Title/Abstract]” OR “exophthalmia [Title/Abstract]” OR “keratoconjunctivitissicca [Title/Abstract]” AND “Human [Mesh]”. The reference lists of selected papers were manually screened for potential papers missed in the primary and secondary search.
The initial selection of studies was based on titles and abstracts. Secondly, the full text of each selected study was screened by two independent investigators (You YS and Yu XN) according to the following inclusion criteria: 1) original research studies reporting independent data on the association between alcohol consumption and risk of DES; 2) studies with age and gender adjusted odds ratios (ORs) and 95% confidence interval (CI), or sufficient data to evaluate the ORs and 95% CI. Studies meeting any of the following criteria would be excluded: 1) review or case-report papers; 2) not published original full-text articles; 3) duplication of previously published studies. No specific language restriction was imposed on the selection of studies.
Data Extraction and Study Quality Assessment
Two investigators (You YS and Yu XN) independently extracted the data using a standardized data extraction format, including the following data: first author's name, publication year, country, study design, sample size, alcohol consumption status, diagnostic criteria of DES, adjusted variables, and OR values with corresponding 95% CIs. Studies involving two independent sets of data were considered to be two separate studies. Only the most recent or most informative studies were included in the present Meta-analysis to avoid double publication. For the studies involving varying degree of DES, only the most serious were included.
The qualities of all selected studies were evaluated based on the Newcastle-Ottawa scale (NOS)[12], and studies scoring five or more points were considered to be of high quality.
DES patients were divided into two groups in terms of diagnostic criteria: patients with symptomatic DES and patients with diagnosed DES. Symptomatic DES were defined through a questionnaire or an interview containing at least the following DES symptoms: dryness, foreign body sensation, burning, scratchiness, and discomfort[4]–[8]. Diagnosed DES were defined as the simultaneous presence of symptoms and at least one positive sign (Schirmer test score ≤5 mm, Tear breakup time ≤10s, fluorescein staining score ≥1, and rose bengal score ≥3), or receiving some form of dry eye therapy [3]–[4],[8]–[10].
Subjects involved in this Meta-analysis were divided into three groups in terms of daily alcohol intake: heavy drinkers, any drinkers and non-drinkers. Currently, There are no universally accepted definitions of heavy drinkers[13]. In this study, heavy drinkers were defined as males who consumed more than 7 drinks on a single occasion or females who consumed more than 5 drinks on a single occasion at least once per month, or people who drink more than 14 units a week[4],[8],[10].
Statistical Analysis
All statistical analyses were performed using Stata version 12.0 software. The statistical significance level was set to P<0.05, except in the case of heterogeneity.
The OR values with corresponding 95% CIs were used as the valid estimates for all involved studies to calculate a pooled OR with 95% CI. Potential heterogeneity among the included studies was assessed based on Cochran's Q statistic and an I2 index score,with the significance level set at a P-value less than 0.10 or an I2 score greater than 50%[14]. When high heterogeneity was detected, the random effects model based on the DerSimonian and Laird[15] method was used; otherwise, the fixed-effects model based on the inverse variance method was performed. Subgroup analyses were conducted according to diagnostic criteria and alcohol intake. The sensitivity analysis was used to assess the robustness of the main Meta-analysis results by sequentially omitting individual studies. Egger's linear regression and Begg's linear regression were used to assess the potential publication bias[16].
RESULTS
Literature Search Results and Characteristics of Included Studies
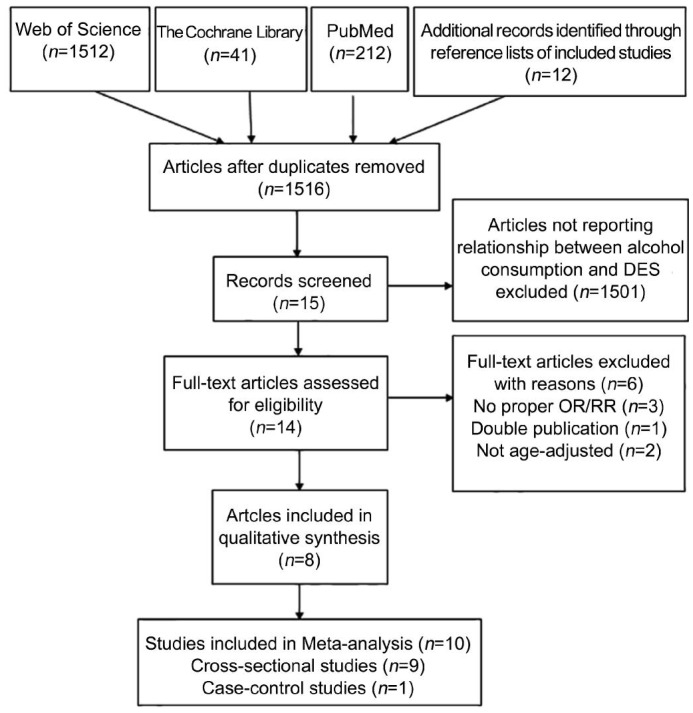
Of the 1516 potentially relevant articles identified by searching electronic databases and reference lists of the selected articles (Figure 1). After excluding 1 article that was not available in full text[17], 14 articles were retrieved for final review following the primary selection based on titles and abstracts. Six articles were excluded for the following reasons: 3 articles did not provide proper OR values and 95% CIs[18]–[20], 2 articles were not age adjusted[21]–[22], and 1 article provided data that had been used in another study[23]. Ultimately, 9 cross-sectional studies and 1 case-control study from 8 articles meeting all predefined inclusion criteria were included in the present Meta-analysis[3]–[10], and all are considered to be of high quality according to the NOS scores. The characteristics of the involved studies are summarized in Table 1, and a total of 2 477 343 subjects were included in the present Meta-analysis.
Figure 1. Flow diagram of study selection process.
Table 1. Characteristics of 8 case-control/cross-sectional articles included into the present Meta-analysis.
| Source (published year, country) | Study design | Sample size | Age (a) | Diagnostic criteria | Adjusted factors | NOS scores |
| Ahn et al (2014, Korea) | Cross-sectional | 11666 | 19-95 | Both | Age, gender, education, etc. | 6 |
| Galor et al (2012, USA) | Case-control | 2454458 | 21-100 | Clinical diagnose | Age, gender | 7 |
| Viso et al (2009, Spain) | Cross-sectional | 654 | 40-96 | Both | Age, sex, computer use, etc. | 6 |
| Moss et al (2000, USA) | Cross-sectional | 3722 | 48-91 | Typicalsymptoms | Age, sex, smoking status, etc. | 7 |
| Chia et al (2003, Australia) | Cross-sectional | 1174 | 50-90 | Typical symptoms | Age, sex | 7 |
| Tan et al (2015, Singapore) | Cross-sectional | 1004 | 15-83 | Typical symptoms | Age, gender, contact lens wear, etc. | 7 |
| Guo et al (2010, China) | Cross-sectional | 2486 | 40-91 | Clinical diagnose | Age, gender, education, etc. | 7 |
| Lu et al (2008, China) | Cross-sectional | 2229 | ≥40 | Clinical diagnose | Age, gender, education, etc. | 7 |
Association Between Dry Eye Syndrome and Alcohol Consumption
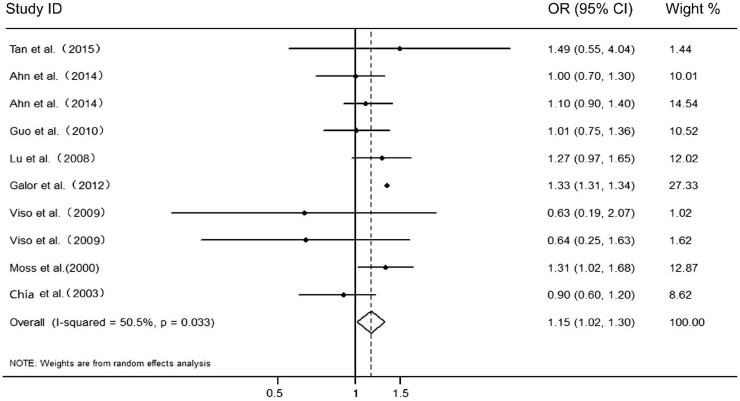
The pooled results of the 10 studies from 8 included articles indicated that alcohol consumption was a significant risk factor of DES (Figure 2; OR 1.15, 95% CI: 1.02-1.30; I2=50.5%, Pheterogeneity=0.033; Begg's: P=0.54, Z=0.592, Egger's: P=0.004). And the results were independent of smoking, hypertension, diabetes and thyroid disease history, which were also risk factors of DES (Table 2).
Figure 2. The relationship between alcohol consumption and DES.
Table 2. Results of subgroup analysis.
| Subgroups | No. of studies | Pooled OR (95% CI) | Pheterogeneity |
| Diagnostic criteria | |||
| Symptomatic DES | 5 | 1.18 (1.01-1.39) | 0.08 |
| Diagnostic DES | 5 | 1.11 (0.94-1.32) | 0.313 |
| Alcohol intake | |||
| Any drinker vs non-drinkers | 5 | 1.33 (1.31-1.34) | 0.484 |
| Heavy drinker vs non-drinkers | 5 | 1.01 (0.86-1.18) | 0.643 |
| Study design | |||
| Case-control | 1 | 1.33 (1.31-1.34) | 1 |
| Cross-sectional | 9 | 1.11 (0.99-1.23) | 0.49 |
| Sample size | |||
| ≤3000 | 6 | 1.06 (0.90-1.25) | 0.413 |
| >3000 | 4 | 1.23 (1.08-1.40) | 0.107 |
| Publication year | |||
| <2010 | 6 | 1.33 (1.31-1.34) | 0.116 |
| ≥2010 | 4 | 1.06 (0.91-1.23) | 0.851 |
| Adjustment for confounders | |||
| Smoking | 8 | 1.10 (1.00-1.23) | 0.419 |
| No smoking | 2 | 1.33 (1.32-1.35) | 0.823 |
| Hypertension | 6 | 1.33 (1.31-1.34) | 0.14 |
| No hypertension | 4 | 1.03 (0.87-1.23) | 0.57 |
| Diabetes | 3 | 1.22 (0.96-1.54) | 0.191 |
| No diabetes | 7 | 1.15 (1.00-1.32) | 0.026 |
| Thyroid disease | 4 | 1.15 (1.00-1.33) | 0.523 |
| No thyroid disease | 6 | 1.12 (0.92-1.35) | 0.034 |
Results of Subgroup Analysis
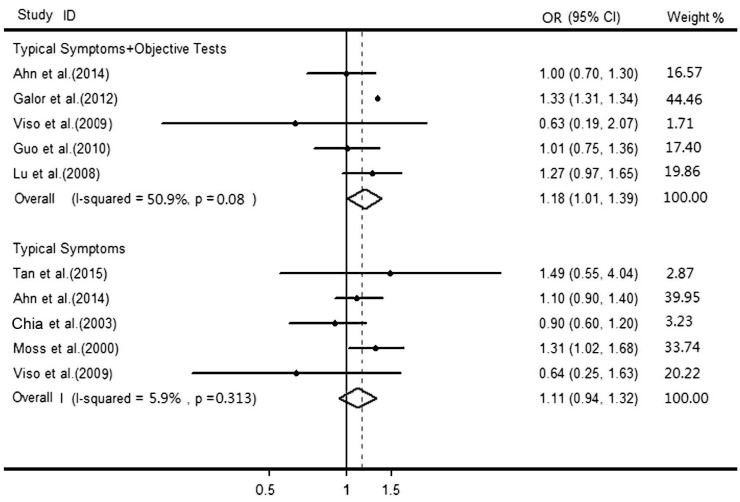
To further explore the influence of diagnostic criteria, subgroup analyses were conducted. A total of 5 studies included DES patients with typical DES symptoms alone[3]–[4],[8]–[10], and 5 studies included DES patients with both typical dry eye symptoms and positive objective tests[4]–[8]. Alcohol consumption could significantly increase the risk of DES among patients with both typical dry eye symptoms and positive objective tests (Figure 3; OR 1.18, 95% CI: 1.01-1.39; I2=50.9%, Pheterogeneity=0.087; Begg's: P=0.462, Z=0.73, Egger's: P=0.033), but no significant effect of alcohol consumption was detected on DES risk among patients with only typical symptoms (Figure 3; OR 1.11, 95% CI: 0.94-1.32; I2=5.9%, Pheterogeneity=0.313; Begg's: P=1.00, Z=0.00, Egger's: P=0.589).
Figure 3. The relationship between DES based on two different diagnostic criteria and alcohol consumption.
Subgroup analyses were also conducted according to study design, sample size, and publication year (Table 2), and the results indicated that the significance did not alter among cross-sectional studies that were conducted after 2010 and contained more than 3000 subjects. Besides, we also performed subgroup analysis in terms of daily alcohol intake, and given the fact that there are no universally accepted definitions of heavy drinkers, we put this part in supporting information.
Meta-regression Analysis
A Meta-regression analysis was conducted to explore the influence of sample size, publication year, and study area on the heterogeneity of the included studies, but none of the factors were proven to be a main source of heterogeneity (P>0.05).
Sensitivity Analysis
Individual studies were sequentially omitted, and all the pooled results fell in the range of the confidence interval with all the included studies, which indicated robust main Meta-analysis results.
DISCUSSION
The results of the present Meta-analysis involving 9 cross-sectional and 1 case-control studies indicated that alcohol consumption can increase the risk of DES, especially for patients based on typical symptoms and positive objective examinations. It was worth noting that heavy drinkers did not have a higher risk of suffering from DES, but any drinkers did. All the relationships were independent of age and gender.
Some researchers have reported the presence of ethanol in tears after alcohol consumption[24], which was significantly related to decreased tear-film volume, disturbed tear-film structure, facilitated aqueous layer, and deteriorated tearfilm[24]–[26]. Tear hyperosmolarity, which is highly related to the increased prevalence of DES, was also detected after heavy drinking[25]–[26]. Besides, ethanol in tears could also induce the increased expression of proinflammatory cytokines (e.g. IL-1β, IL-6, and IL-8) in corneal stromal cells and epithelial cells[27]. And according to precious studies, ocular surface inflammation is a main pathogenic factor for DES[28]–[29]. Given this fact, increased levels of ethanol in tears after alcohol consumption could directly trigger the development of DES. Besides, chronic alcoholism could induce vitamin A deficiency by influencing the storage of retinol in the liver[30]–[31]. And an absence of vitamin A would cause significant loss of goblet cells and lead to increased epidermal keratinization and squamous metaplasia of the mucous membranes in the cornea and conjunctiva, which is an important pathogenesis of DES[32]–[33]. Thus, vitamin A deficiency secondary to alcohol malnutritionis another main cause of DES for drinkers.
In this Meta-analysis, we noticed that DES patients based on typical symptoms and positive objective tests showed a significant relationship with alcohol consumption, while patients with typical DES symptoms did not. This maybe attributed to the decreased corneal sensitivity caused by alcohol-induced peripheral neuropathy[34], which results in an under estimation of DES incidence. As a consequence, the OR values for patients with typical DES symptoms were reduced. There markable results of subgroup analyses according to alcohol intake can also be explained by the above mentioned mechanism. Compared to any drinkers, heavy drinkers are at higher risk of suffering from alcohol-induced peripheral neuropathy[34], and therefore have a reduced chance of visiting eye clinics for dry eye symptoms.
Significant heterogeneity among the included studies was detected by means of Cochran's Q statistic and I2 score, and may be caused by various sample sizes, DES criteria, adjusted factors, the study population, and so on. We therefore performed sensitivity analysis to evaluate the influence of a single study on the pooled results, which indicated the robustness of our results. Additionally, we performed a Meta-regression analysis to assess the effects of sample size, publication year, and the study area on the heterogeneity of the included studies. And none of the factors were proven to be a main source of heterogeneity. The existence of significant heterogeneity indicates the need for uniform methodologies in future studies.
It was noteworthy that the sample size of one included study is larger than all the other studies combined[7], as the data included patients from 365 eye clinics across America. According to results of sensitivity analysis, omitting this study did not alter the significance of the pooled results.
The limitations of our Meta-analysis should be addressed. First of all, compared with the randomized controlled trial (RCT) design, the cross-sectional or case-control study design may increase the inevitable systemic errors. Secondly, due to the diversity of the involved subjects and study design, obvious heterogeneity was detected, which has nothing to do with sample size, publication year or the study area. Thirdly, none of the included studies provided data on the types of alcoholic drink, and it remains unclear if there is a difference among the different types of alcoholic drinks. Fourthly, too few studies were involved to promote the accuracy of the publication bias test. Fifthly, although we have performed subgroup analysis to eliminate the effects of other potential risk factors of DES (smoking, hypertension, diabetes, thyroid disease history), other known risk factors (such as contact lens uses, hormone replacement therapy) were not included in this Meta-analysis due to insufficient data.
Despite all the limitations, we did have some strengths. First of all, all the included articles are age and gender adjusted, which were well recognized as a risk factor for DES[3]–[5]. Secondly, we distinguished patients only with typical DES symptoms from patients with both typical symptoms and positive objective examinations, and separately analyzed the influence of alcohol consumption on them. Finally, the majority of the included studies were based on the general population for more generalizable results.
In conclusion, the pooled results of the 10 involved studies from 8 articles showed that alcohol consumption could increase the risk of DES. For heavy drinkers, peripheral neuropathy caused by alcohol consumption may decrease their corneal sensitivity, and the real severity of DES tends to be underestimated, which should draw the attention of ophthalmologists. For any disease, the key point is to cure the disease by understanding and addressing the underlying source. Our findings indicate that controlling alcohol consumption may help to reduce DES prevalence. To confirm these findings, further efforts should be made to make a better understanding of the potentialbiological mechanisms. Large-scale and long-term RCTs in various populations should be designed to provide more powerful epidemiological evidence.
Acknowledgments
Foundation: Supported by Zhejiang Key Laboratory Fund of China (No.2011E10006).
Conflicts of Interest: You YS, None; Qu NB, None; Yu XN, None.
REFERENCES
- 1.The definition and classification of dry eye disease: report of the definition and classification subcommittee of the international dry eye workshop (2007) Ocul Surf. 2007;5(2):75–92. doi: 10.1016/s1542-0124(12)70081-2. [DOI] [PubMed] [Google Scholar]
- 2.Yang WJ, Yang YN, Cao J, Man ZH, Yuan J, Xiao X, Xing YQ. Risk factors for dry eye syndrome: a retrospective case-control study. Optom Vis Sci. 2015;92(9):e199–e205. doi: 10.1097/OPX.0000000000000541. [DOI] [PubMed] [Google Scholar]
- 3.Tan LL, Morgan P, Cai ZQ, Straughan RA. Prevalence of and risk factors for symptomatic dry eye disease in Singapore. Clin Exp Optom. 2015;98(1):45–53. doi: 10.1111/cxo.12210. [DOI] [PubMed] [Google Scholar]
- 4.Ahn JM, Lee SH, Rim TH, Park RJ, Yang HS, Kim TI, Yoon KC, Seo KY, Epidemiologic Survey Committee of the Korean Ophthalmological Society Prevalence of and risk factors associated with dry eye: the Korea National Health and Nutrition Examination Survey 2010–2011. Am J Ophthalmol. 2014;158(6):1205–1214.e7. doi: 10.1016/j.ajo.2014.08.021. [DOI] [PubMed] [Google Scholar]
- 5.Guo B, Lu P, Chen X, Zhang W, Chen R. Prevalence of dry eye disease in Mongolians at high altitude in China: the Henan eye study. Ophthalmic Epidemiol. 2010;17(4):234–241. doi: 10.3109/09286586.2010.498659. [DOI] [PubMed] [Google Scholar]
- 6.Lu P, Chen X, Liu X, Yu L, Kang Y, Xie Q, Ke L, Wei X. Dry eye syndrome in elderly Tibetans at high altitude: a population-based study in China. Cornea. 2008;27(5):545–551. doi: 10.1097/ICO.0b013e318165b1b7. [DOI] [PubMed] [Google Scholar]
- 7.Galor A, Feuer W, Lee DJ, Florez H, Faler AL, Zann KL, Perez VL. Depression, post-traumatic stress disorder, and dry eyesyndrome: a study utilizing the national United States Veterans Affairs administrative database. Am J Ophthalmol. 2012;154(2):340–346. doi: 10.1016/j.ajo.2012.02.009. [DOI] [PubMed] [Google Scholar]
- 8.Viso E, Rodriguez-Ares MT, Gude F. Prevalence of and associated factors for dry eye in a Spanish adult population (the Salnes Eye Study) Ophthalmic Epidemiol. 2009;16(1):15–21. doi: 10.1080/09286580802228509. [DOI] [PubMed] [Google Scholar]
- 9.Moss SE, Klein R, Klein BE. Prevalence of and risk factors for dry eye syndrome. Arch Opthalmol. 2000;118(9):1264–1268. doi: 10.1001/archopht.118.9.1264. [DOI] [PubMed] [Google Scholar]
- 10.Chia EM, Mitchell P, Rochtchina E, Lee AJ, Maroun R, Wang JJ. Prevalence and associations of dry eye syndrome in an older population: the Blue Mountains Eye Study. Clin Exp Ophthalmol. 2003;31(3):229–232. doi: 10.1046/j.1442-9071.2003.00634.x. [DOI] [PubMed] [Google Scholar]
- 11.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wells GA, Shea B, O'Conneel D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. 2014. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 11 Feb 2016.
- 13.Wang W, Zhang X. Alcohol intake and the risk of age-related cataracts: a meta-analysis of prospective cohort studies. PLoS One. 2014;9(9):e107820. doi: 10.1371/journal.pone.0107820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.DerSimonian R, Kacker R. Random-effects model for meta-analysis of clinical trials: an update. Contemp Clin Trials. 2007;28(2):105–114. doi: 10.1016/j.cct.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 16.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sendecka M, Baryluk A, Polz-Dacewicz M. Prevalence and risk factors of dry eye syndrome. Przegl Epidemiol. 2004;58(1):227–233. [PubMed] [Google Scholar]
- 18.Paulsen AJ, Cruickshanks KJ, Fischer ME, Huang GH, Klein BE, Klein R, Dalton DS. dry eye in the beaver dam offspring study: prevalence, risk factors, and health-related quality of life. Am J Ophthalmol. 2014;157(4):799–806. doi: 10.1016/j.ajo.2013.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moss SE, Klein R, Klein BE. Long-term incidence of dry eye in an older population. Optom Vis Sci. 2008;85(8):668–674. doi: 10.1097/OPX.0b013e318181a947. [DOI] [PubMed] [Google Scholar]
- 20.Moss SE, Klein R, Klein BE. Incidence of dry eye in an older population. Arch Ophthalmol. 2004;122(3):369–373. doi: 10.1001/archopht.122.3.369. [DOI] [PubMed] [Google Scholar]
- 21.Uchino M, Nishiwaki Y, Michikawa T, Shirakawa K, Kuwahara E, Yamada M, Dogru M, Schaumberg DA, Kawakita T, Takebayashi T, Tsubota K. Prevalence and risk factors of dry eyedisease in Japan: Koumi study. Ophthalmology. 2011;118(12):2361–2367. doi: 10.1016/j.ophtha.2011.05.029. [DOI] [PubMed] [Google Scholar]
- 22.Jie Y, Xu L, Wu YY, Jonas JB. Prevalence of dry eye among adult Chinese in the Beijing Eye Study. Eye(Lond) 2009;23(3):688–693. doi: 10.1038/sj.eye.6703101. [DOI] [PubMed] [Google Scholar]
- 23.Galor A, Feuer W, Lee DJ, Florez H, Carter D, Pouyeh B, Prunty WJ, Perez VL. Prevalence and risk factors of dry eye syndrome in a United States veterans affairs population. Am J Ophthalmol. 2011;152(3):377–384.e2. doi: 10.1016/j.ajo.2011.02.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Arora SS, Vatsa M, Singh R, Jain A. Iris recognition under alcohol influence: A preliminary study. 2012 5th IAPR International Conference on Biometrics (ICB); 2012. [Google Scholar]
- 25.Castro JJ, Pozo AM, Rubiño M, Anera RG, Jiménez Del Barco L. Retinal-image quality and night-vision performance after alcohol consumption. J Ophthalmol. 2014;2014:704823. doi: 10.1155/2014/704823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Oh JY, Yu JM, Ko JH. Analysis of ethanol effects on corneal epithelium. Invest Ophthalmol Vis Sci. 2013;54(6):3852–3856. doi: 10.1167/iovs.13-11717. [DOI] [PubMed] [Google Scholar]
- 27.Cumurcu T, Gunduz A, Cumurcu BE, Gül IG, Akpolat N, Karlidag R. The changes in tear film parameters and impression cytology in heavily drinking men. Cornea. 2013;32(3):237–241. doi: 10.1097/ICO.0b013e31825239d1. [DOI] [PubMed] [Google Scholar]
- 28.Calonge M, Enríquez-de-Salamanca A, Diebold Y, González-García MJ, Reinoso R, Herreras JM, Corell A. Dry eye disease as an inflammatory disorder. Ocul Immunol Inflamm. 2010;18(4):244–253. doi: 10.3109/09273941003721926. [DOI] [PubMed] [Google Scholar]
- 29.Stevenson W, Chauhan SK, Dana R. Dry eye disease: an immune-mediated ocular surface disorder. Arch Ophthalmol. 2012;130(1):90–100. doi: 10.1001/archophthalmol.2011.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fuchs J. Alcoholism, malnutrition, vitamin deficiencies, and the skin. Clin Dermatol. 1999;17(4):457–461. doi: 10.1016/s0738-081x(99)00032-2. [DOI] [PubMed] [Google Scholar]
- 31.Lieber CS. Alcohol, liver, and nutrition. J Am Coll Nutr. 1991;10(6):602–632. doi: 10.1080/07315724.1991.10718182. [DOI] [PubMed] [Google Scholar]
- 32.Hatchell DL, Sommer A. Detection of ocular surface abnormalities in experimental vitamin A deficiency. Arch Ophthalmol. 1984;102(9):1389–1393. doi: 10.1001/archopht.1984.01040031131040. [DOI] [PubMed] [Google Scholar]
- 33.Kim EC, Choi JS, Joo CK. A comparison of vitamin a and cyclosporine a 0.05% eye drops for treatment of dry eye syndrome. Am J Ophthalmol. 2009;147(2):206–213.e3. doi: 10.1016/j.ajo.2008.08.015. [DOI] [PubMed] [Google Scholar]
- 34.Ferdinandis TG, De Silva HJ. Illicit alcohol consumption and neuropathy-a preliminary study in Sri Lanka. Alcohol Alcohol. 2008;43(2):171–173. doi: 10.1093/alcalc/agm162. [DOI] [PubMed] [Google Scholar]