Abstract
Context:
Fatigue in overhead athletes reduces shoulder muscular contraction and proprioception. These deficits may lead to alterations in scapular upward rotation, which is associated with multiple chronic shoulder conditions prevalent in tennis players.
Objective:
To identify the effect of a functional fatigue protocol on scapular upward rotation in collegiate male tennis players.
Design:
Randomized controlled clinical trial.
Setting:
Research laboratory.
Patients or Other Participants:
Twenty healthy male tennis players with no history of shoulder injury completed this study. Participants were divided into 2 groups, experimental (age = 19.4 ± 1.1 years, height = 180.1 ± 8.9 cm, weight = 72.7 ± 11.6 kg) and control (age = 19.6 ± 1.2 years, height = 181.1 ± 6.6 cm, weight = 81.6 ± 13.5 kg).
Intervention(s):
Participants in the experimental group performed a tennis-serving protocol until the onset of fatigue. Fatigue was defined as a participant reporting a rating of 15 on the Borg Scale of Perceived Exertion and reaching a heart rate of 70% of maximum. Instead of completing the fatigue protocol, control participants rested for an interval time matched to the experimental group.
Main Outcome Measure(s):
Scapular upward rotation of the dominant arm was measured at rest and at 60°, 90°, and 120° of glenohumeral elevation in the scapular plane. Upward-rotation measurements were taken prefatigue, postfatigue, and at 24, 48, and 72 hours postexercise. Scapular upward-rotation values were calculated as change scores from baseline and analyzed using a 2 × 4 mixed-model analysis of variance.
Results:
Significant group-by-time interaction effects were found in postfatigue change scores. The experimental group displayed scapular upward-rotation deficits at all testing positions postfatigue (rest: −2.1° ± 1.4°, 60°: −2.2° ± 2.2°, 90°: −3.2° ± 2.1°, 120°: −4.0° ± 1.3°). No differences were observed at 24, 48, or 72 hours after the fatigue protocol.
Conclusions:
Fatigue impaired scapular upward rotation in male tennis players, but values returned to baseline within 24 hours. Clinicians should monitor scapular upward rotation in tennis players returning to competition within a day after heavy serving activity.
Key Words: scapular dyskinesis, functional fatigue, tennis serve, overhead athletes
Key Points
Male tennis players experienced acute deficits in scapular upward rotation after serving until fatigued.
Male tennis players who did not undergo the fatigue protocol exhibited no scapular upward-rotation differences across testing sessions.
Scapular upward rotation returned to normal 24 hours after a functional fatigue protocol.
Fatigue is a natural physiologic response to exercise that describes the decline in work output associated with repetitive or sustained activity.1 It can reduce muscular contraction by inhibiting neural conduction from the central nervous system (CNS) or by depleting key substrates such as glycogen and adenosine triphosphate.2 In overhead athletes, fatigue can also decrease proprioception in the musculature that creates scapulothoracic and glenohumeral joint motion.3 Although a decline in performance is an obvious indicator of these sensorimotor deficits in athletes, injury may also result because of an inability to maintain proper form or efficiently dissipate the forces placed on the shoulder during dynamic overhead activity.4,5
The sensorimotor deficits and improper activation of upper extremity musculature resulting from fatigue may lead to scapular dyskinesis, which describes abnormalities in scapular position or motion (or both) during glenohumeral elevation.6 Despite advances in motion-capture technology, abnormal scapulothoracic kinematics are difficult to quantify because of the scapula's complex movement under the skin. Therefore, single-plane measures have been developed to provide clinically applicable information.6−8 The prominence of the scapular spine allows for the direct measurement of upward rotation, and normative values have been established by previous researchers.9 During the first 0° to 30° of normal glenohumeral abduction, the scapula sets on the thorax and does not rotate.9 As the humerus abducts between 30° and 90°, the scapula rotates upward 1° for every 2° of glenohumeral elevation, with this ratio changing to 1:1 from 90° to full abduction.9 A normal ratio between glenohumeral elevation and scapular upward rotation helps maintain congruency between the glenoid and humeral head while allowing adequate space for tissue movement between the acromion and humerus.6,10 However, a deviation from that normal ratio has been linked to a diverse range of shoulder conditions that are commonly observed in overhead athletes, including rotator cuff tendon failure, impingement syndrome, and glenohumeral instability.11−13
Tennis players are at particular risk for these chronic upper extremity injuries because the serving stroke is performed at shoulder rotational velocities of up to 1500°/s several hundred times per match, with numerous repetitions also occurring during practice.14,15 To reduce the injury risk, tennis athletes experience a natural shift toward more upward rotation in the dominant arm.16 This positive adaptation may be counteracted by fatigue, which limits the ability of the rotator cuff and scapular stabilizers to dissipate excessive forces, instigating a cascade effect of muscular compensation, scapular malposition, and eventual injury.17 If scapular movement in tennis players does not return to prefatigue values after an intense bout of overhead activity, as observed in baseball players,18 repetitive microtrauma to the shoulder may occur. This microtrauma may then place a tennis athlete at higher risk for chronic injury days after the match or practice because of increased cumulative stress to the shoulder resulting from poor biomechanics.11,12 However, to our knowledge, the effects of fatigue on scapular upward rotation in tennis players have not been investigated. Therefore, the purpose of our study was to determine whether a functional fatigue protocol (FFP) affected scapular upward-rotation values in collegiate male tennis players. A secondary purpose was to determine the length of time for scapular upward rotation to return to prefatigue values. We hypothesized that an FFP would impair scapular upward rotation.
METHODS
Participants
Twenty collegiate men's tennis players participated in this research study (Table 1). Each participant was an active member of an intercollegiate or club tennis team during the semester in which he was tested. Volunteers with a previous history of shoulder surgery, dislocation, fracture, or altered upper extremity sensation were excluded. Volunteers were also excluded if they had experienced injury within the 6 months before testing. All participants provided written informed consent as approved by the university's institutional review board, which also approved the study.
Table 1. .
Demographic Data
| Variable |
Group |
|
| Experimental (n = 10) |
Control (n = 10) |
|
| Age, y | 19.4 ± 1.1 | 19.6 ± 1.2 |
| Height, cm | 180.1 ± 8.9 | 181.1 ± 6.6 |
| Weight, kg | 72.7 ± 11.6 | 81.6 ± 13.5 |
Instrumentation
We recorded each participant's height and weight using a calibrated eye-level physician scale (Detecto Inc, Webb City, MO). A manual, handheld 12-in (30.48-cm) goniometer (model J00240; Bionetics, St Laurent, Quebec, Canada) modified with a bubble level was used to ensure proper arm position in all testing positions.
Scapular upward rotation was measured with a modified digital protractor (model Pro 360; Macklanburg Duncan, Oklahoma City, OK) that has been shown to be valid compared with an electrogoniometer on the dominant arm (r > 0.989) and reliable (intraclass correlation coefficient [ICC] = 0.89−0.96) in previous literature.7,8 To modify the protractor, we placed 2 adjustable 10-cm locator rods on the side of the instrument. The locator rods contacted 2 landmarks on the scapular spine, the root of the scapular spine and the posterolateral acromion. Moleskin was placed at the end of each rod for patient comfort. A bubble level was also placed on the digital protractor to prevent anterior tilting of the instrument (Figure 1). The primary investigator (R.L.R.), who has previous experience measuring scapular upward rotation, obtained all measurements.
Figure 1. .

Digital protractor modification.
A standard tennis ball (Wilson Sports, Chicago, IL) and each participant's personal racquet were used to complete the FFP. Maximum serve velocity was recorded by a radar gun (Stalker Sports Radar, Plano, TX) with a measurement accuracy of ±0.16 km/h. The Borg rating of perceived exertion (RPE; 6 to 20 scale) and heart rate, as measured by a wrist monitor (model FT1; Polar Electro Inc, Lake Success, NY), were used to assess fatigue level.
Procedures
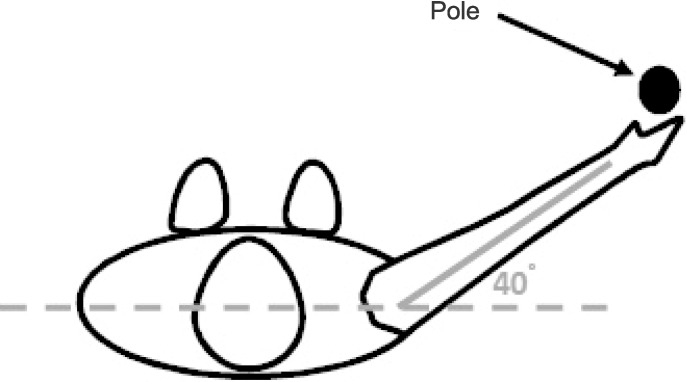
After completing a health history questionnaire ensuring that all inclusion and no exclusion criteria were met, participants were divided into the experimental and control groups by block randomization from a random number generator, and anthropometric data were obtained. Participants were asked to refrain from any strenuous shoulder activity (eg, tennis play, weight lifting, throwing) 3 days before and 3 days after prefatigue testing. To assess scapular upward rotation, we had participants stand on a line of tape placed on the floor so their feet were perpendicular to the tape. Another tape line was placed to intersect the initial line at a 40° angle on the participant's dominant side. This line indicated the scapular plane. A guide pole was placed on the line to indicate the scapular plane and ensure proper position of the participant's arm during glenohumeral elevation (Figure 2). Each participant actively moved his dominant arm to 60°, 90°, and 120° of elevation in the scapular plane, as measured by a manual handheld goniometer, while an investigator assisted with arm placement. At each position, a piece of tape was applied to the guide pole, and the participant was instructed as to which angle corresponded to each mark. The guide pole and its markings were used to ensure consistency of arm angles among testing trials.
Figure 2. .
Guide pole setup.
Scapular Upward-Rotation Measurement
Scapular upward rotation was measured using the digital protractor at 3 testing positions consistent with previous reports of scapular positioning.7,8 Each participant's scapular rotation was assessed 3 times at rest, 60°, 90°, and 120° of active glenohumeral elevation in the scapular plane. This initial measurement served as a baseline for each participant. The testing order was randomized using a random number generator. For each measurement, the participant elevated his arm to the appropriate angle in the scapular plane, as marked on the guide pole. Once the degree of elevation was reached, the investigator palpated and marked the root of the scapular spine and posterolateral acromion. After these 2 marks were made, the adjustable locator rods of the digital protractor were placed in line with the marks. Using the bubble level as a guide, the digital protractor was held in place on the skin. When the value on the digital protractor screen reached equilibrium, the investigator recorded the value. After each measurement, the participant moved the arm back to neutral and was allowed up to a 30-second rest period before the next trial began. The mean value of the 3 trials for each glenohumeral-elevation position was used for analysis.
Functional Fatigue Protocol
Immediately after the prefatigue testing, the participants in the experimental group moved to the tennis court and performed a 3-minute, self-selected serving warmup to mimic normal activity before a match. After the warmup, participants served 5 times at maximum velocity from the service side with which they were most comfortable. The velocities of these serves were averaged to determine the participant's mean peak velocity. After a 3-minute rest period, participants were asked to serve 1 ball every 10 seconds at a speed greater than 90% of their mean peak velocity. If maximum velocity fell below 90%, the participants were orally prompted to “try harder.” The participants were orally prompted with “out” if the ball did not land within the service court. Fatigue level on the Borg RPE scale and heart rate were recorded each minute. Fatigue was considered to have been reached when the participant reported an exertion level of 15 or more on the Borg RPE scale and had a heart rate of more than 70% of his maximum (206.3 − [0.711 × age]).19 We chose these values because of their high correlation with the metabolic responses of fatigue.20
Posttesting
Once participants in the experimental group fatigued, they immediately returned to the biomechanics laboratory, where measurements of scapular upward rotation were repeated at each of the 3 glenohumeral-elevation angles using the same methods described for the prefatigue testing. All posttesting started within 5 minutes of the participant's completing the FFP. The testing measurements were repeated on each participant for the 3 days after the FFP at approximately the same time of day. Therefore, 5 measurements were taken for each participant (pre-FFP, post-FFP, and days 1, 2, and 3).
All prefatigue and postfatigue measurements were obtained in the control group with the same method at all 5 time periods. Control participants were also randomly matched to those in the experimental group so that postfatigue measurements were taken at an interval that corresponded to the time that the matched participant took to complete the FFP and posttest measurements.
Statistical Analysis
Raw data are presented in Table 2, but data were analyzed using the change score from the prefatigue trials. We calculated these values by subtracting data taken from the postfatigue sessions (post-FFP and days 1, 2, and 3) from the prefatigue values. Therefore, four 2 × 4 analyses of variance (group × change score from prefatigue) were used to examine the dependent variable of mean upward rotation at rest and at the 3 positions of humeral elevation (60°, 90°, and 120°). Data were analyzed using SPSS statistical software (version 22.0; IBM Corporation, Armonk, NY) with an a priori α level set at P < .05. The assumption of sphericity was violated in all analyses, so we adjusted the significance of F ratios according to the Greenhouse-Geisser correction. Tukey honestly significant difference post hoc testing was used to evaluate significant analysis-of-variance models.
Table 2. .
Raw Scapular Upward-Rotation Values, ° (Mean ± SD)
| Condition |
Group |
Time |
||||
| Prefatigue |
Postfatigue |
Day 2 |
Day 3 |
Day 4 |
||
| Rest | Experimental | 1.5 ± 2.7 | −0.7 ± 2.8 | 1.2 ± 3.0 | 1.5 ± 2.5 | 1.2 ± 2.5 |
| Control | 2.7 ± 5.3 | 2.8 ± 5.2 | 2.7 ± 5.4 | 2.8 ± 5.3 | 2.9 ± 5.3 | |
| 60° | Experimental | 7.9 ± 4.5 | 5.7 ± 4.7 | 7.8 ± 4.8 | 7.9 ± 4.6 | 7.7 ± 4.6 |
| Control | 9.1 ± 7.3 | 9.3 ± 7.3 | 9.4 ± 7.3 | 9.6 ± 7.6 | 9.4 ± 7.3 | |
| 90° | Experimental | 22.5 ± 5.4 | 19.3 ± 5.2 | 22.4 ± 5.4 | 22.4 ± 5.4 | 22.5 ± 5.4 |
| Control | 25.7 ± 9.5 | 25.8 ± 9.5 | 25.8 ± 9.6 | 25.1 ± 9.0 | 26.0 ± 9.2 | |
| 120° | Experimental | 37.3 ± 6.9 | 33.4 ± 6.5 | 36.7 ± 7.0 | 36.8 ± 7.0 | 37.2 ± 6.8 |
| Control | 38.0 ± 9.1 | 38.0 ± 9.2 | 38.2 ± 9.3 | 38.2 ± 9.1 | 38.2 ± 9.0 | |
RESULTS
Twenty participants were recruited, but 1 withdrew from the experimental group because of noncompliance with the FFP. The experimental-group participants completed the FFP, reaching or exceeding 15 on the RPE scale and 70% of maximum heart rate after 10.1 ± 7.1 minutes, which equaled 58.2 ± 41.7 serves. All participants consistently served above 90% of their maximum speed and to the correct location on the court. When fatigue was reached, the experimental-group participants' mean RPE was 16.0 ± 1.6, and the average heart rate was 152.5 ± 26.6 beats/min.
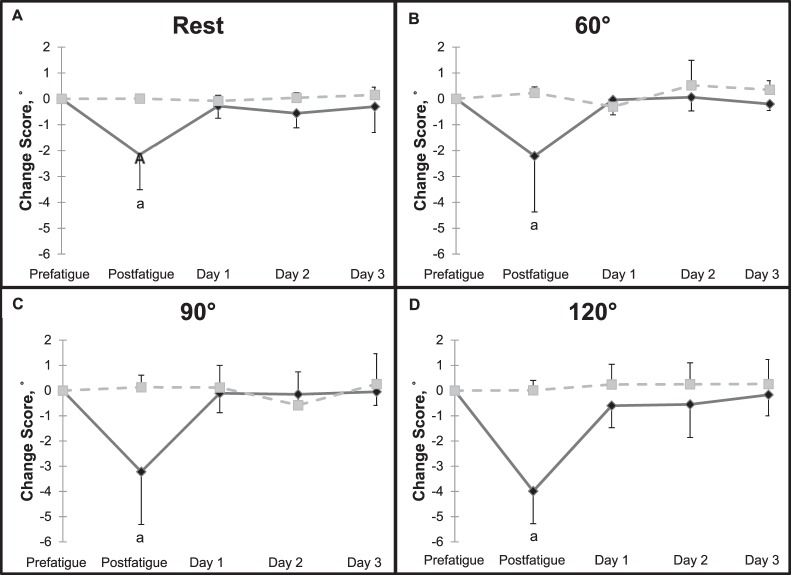
Change scores for both groups are presented in Figure 3. At rest, a significant group-by-time interaction effect was present (F3,54 = 13.19, P < .001). Post hoc testing identified a significant difference between change scores post-FFP in the experimental group (−2.16° ± 1.35°) and the values observed in subsequent testing sessions. Participants in the experimental group had a significant decrease in scapular upward rotation immediately after fatigue that returned to baseline the next day, whereas participants in the control group did not experience this change. A similar interaction effect was noted immediately post-FFP at 60° (−2.21° ± 2.16°, F3,54 = 6.72, P = .007), 90° (−3.22° ± 2.09°, F3,54 = 13.60, P < .001), and 120° (−3.99° ± 1.29°, F3,54 = 18.21, P < .001) of glenohumeral elevation in the experimental group, with values again returning to baseline 24 hours postfatigue.
Figure 3. .
Scapular upward-rotation change scores compared with prefatigue (baseline) value. A, Arm by the side. B, Arm at 60° of glenohumeral elevation in the scapular plane. C, Arm at 90° of glenohumeral elevation in the scapular plane. D, Arm at 120° of glenohumeral elevation in the scapular plane. a Indicates a difference from all other change-score values at the same humeral elevation, P < .05.
DISCUSSION
The ability to maintain scapular upward rotation during serving is important in limiting the chronic injury risk in tennis players. The main finding of our study was a decrease in scapular upward rotation immediately after a sport-specific FFP in collegiate male tennis players. As hypothesized, participants who underwent the fatigue protocol presented with a decrease in scapular upward rotation at rest and at all 3 testing positions (60°, 90°, and 120°) immediately post-FFP, whereas participants who were not fatigued exhibited no differences across testing sessions. However, this change in the fatigued participants was noted only immediately after activity, and scapular upward rotation returned to prefatigue values before the 24-hour postfatigue test. Although our scapular upward-rotation values indicate a ratio greater than the traditional 2° of glenohumeral elevation for every 1° of scapular upward rotation,9 they are similar to the results of another study that suggested a 3.8 : 1 relationship.21
Limited literature describes the effects of an FFP on scapular kinematics, but our findings agree with those from an earlier study of baseball players,18 which showed that 61.5% of athletes experienced scapular upward-rotation decreases immediately after throwing 60 pitches. Even though only some of these athletes presented with scapular malposition after pitching, scapular upward rotation across all participants decreased by about 2°, which was similar to our results at rest (−2.16° ± 1.35°) and 60° (−2.21° ± 2.16°).18 Conversely, some authors21,22 have shown an increase in upward rotation after an FFP, typically when resistance was added to the overhead task during glenohumeral elevation. This type of protocol fatigues the infraspinatus muscle and could lead to superior translation of the humeral head in the glenoid.23 The scapula may then have compensated for this superior translation by increasing upward rotation to avoid compression of the structures in the subacromial space.24 This pattern appears to have superseded the fatigue of the scapular upward rotators, such as the upper trapezius and serratus anterior, that also occurred after the glenohumeral-elevation fatigue protocol.22 Although we did not collect electromyographic data, an examination of previous normative muscle-activation levels during the tennis serve may give some insight into the postfatigue differences between our participants and those of previous studies. Our FFP may not have created the same response because the infraspinatus, which is active only to about half of its maximum voluntary isometric contraction during the serve,25 likely does not fatigue enough to create humeral head translation. Therefore, a compensatory movement pattern, such as that seen in the glenohumeral-elevation resistance protocols, may not occur from fatigue induced by tennis serving. Instead, the downward rotation of the scapular kinematic changes immediately postfatigue observed in our study may result from an imbalance in the scapular musculature. The serratus anterior is active to a greater extent than the latissimus dorsi in all phases of the tennis serve,25 suggesting that the scapular upward rotators were more fatigued than the downward rotators after our FFP. This asymmetry could have led to the scapular kinematic changes immediately post-FFP observed in this study. Because our purpose was to understand the effects of functional fatigue on scapular kinematics in tennis players, we designed an ecologically valid protocol to meet this purpose.
The fatigue induced by the FFP likely reduced proprioceptive feedback to the CNS via sensorimotor system deficits.3,26 When sensory feedback is altered, the CNS misjudges the motor commands needed to produce normal movement trajectories.27,28 Over the course of the FFP, the continued use of improper motor commands could have created a temporary new motor pattern for glenohumeral elevation, as has been previously observed in reaching tasks.28 This new pattern may have then limited scapular upward rotation immediately after fatigue. Tennis athletes amass numerous repetitions of glenohumeral-elevation tasks over the course of their careers, so these patterns likely reverted to normal within 24 hours of the FFP. Fatigue probably led to both muscular and proprioceptive deficits, which combined to decrease the scapular upward rotation we observed. However, we cannot speculate as to which system contributed most or whether the deficiencies were central or peripheral in nature.
Our finding that scapular upward-rotation deficits presented immediately after an FFP suggests that tennis players acutely develop abnormal scapular-movement patterns as a result of fatigue. This dyskinesis can be clinically meaningful for overhead athletes, as changes of approximately 3° are associated with the development of subacromial impingement.29 Therefore, the 2° to 4° deficits in scapular rotation noted in this study between the prefatigue and postfatigue conditions could increase the impingement risk over time in tennis players who continue to participate in repetitive, overhead activity while fatigued. Because upward rotation returns to prefatigue values within 24 hours of an intense bout of serving, there does not appear to be an increased risk during the next day's tennis activity. However, our study included only 1 bout of fatigue lasting approximately 10 minutes, so we cannot speculate on the cumulative effects of fatiguing overhead activity on scapular upward rotation.
Testing was performed only once every 24 hours. Therefore, the specific time frame for scapular recovery in tennis players within the first day after an FFP cannot be identified. Additionally, the upward-rotation measurements taken during this study were static in nature, and our results should be interpreted with caution because of the dynamic movement of the shoulder during tennis. However, the complex movement of the scapula creates inconsistencies in 3-dimensional motion capture, and measurement of dynamic movement is not clinically feasible. Finally, only collegiate male tennis players were included in the study, so extrapolations of these findings to other populations (eg, females, different ages) or overhead sports should be limited.
CONCLUSIONS
Our findings suggest that male tennis players experienced a decrease in scapular upward rotation immediately after an FFP at rest and at 60°, 90°, and 120° of glenohumeral abduction, potentially placing them at risk of subacromial impingement when they are fatigued. However, these altered scapular upward-rotation values returned to prefatigue levels within 24 hours after the FFP. Because they can be obtained quickly and easily, scapular upward-rotation measurements could be used by sports medicine professionals to identify athletes at risk of injury within 24 hours of heavy bouts of tennis serving. Our results may also help clinicians understand the influence of fatigue on scapular kinematics and potentially identify an underlying mechanism of chronic shoulder injury. Future researchers should identify alterations in scapular upward rotation within a 24-hour period after fatigue to determine suggested rest intervals between matches and practices in an attempt to decrease injury risk. The effects of shoulder fatigue on female tennis players and on repetitive bouts of serving are also areas that could be explored to enhance injury prevention in these athletes. Based on the results of this study, clinicians should monitor scapular upward rotation in fatigued tennis players who are returning to competition within a 24-hour period.
ACKNOWLEDGMENTS
This study was funded by the National Athletic Trainers' Association Research & Education Foundation.
REFERENCES
- 1. Mannion AF, Dolan P. Relationship between myoelectric and mechanical manifestations of fatigue in the quadriceps femoris muscle group. Eur J Appl Physiol Occup Physiol. 1996; 74 5: 411– 419. [DOI] [PubMed] [Google Scholar]
- 2. Davis JM, Bailey SP. Possible mechanisms of central nervous system fatigue during exercise. Med Sci Sports Exerc. 1997; 29 1: 45– 57. [DOI] [PubMed] [Google Scholar]
- 3. Tripp BL, Yochem EM, Uhl TL. Functional fatigue and upper extremity sensorimotor system acuity in baseball athletes. J Athl Train. 2007; 42 1: 90– 98. [PMC free article] [PubMed] [Google Scholar]
- 4. Qin J, Lin JH, Faber GS, Buchholz B, Xu X. Upper extremity kinematic and kinetic adaptations during a fatiguing repetitive task. J Electromyogr Kinesiol. 2014; 24 3: 404– 411. [DOI] [PubMed] [Google Scholar]
- 5. Gescheit DT, Cormack SJ, Reid M, Duffield R. Consecutive days of prolonged tennis match play: performance, physical, and perceptual responses in trained players. Int J Sports Physiol Perform. 2015; 10 7: 913– 920. [DOI] [PubMed] [Google Scholar]
- 6. Kibler WB. The role of the scapula in athletic shoulder function. Am J Sports Med. 1998; 26 2: 325– 337. [DOI] [PubMed] [Google Scholar]
- 7. Tucker WS, Ingram RL. Reliability and validity of measuring scapular upward rotation using an electrical inclinometer. J Electromyogr Kinesiol. 2012; 22 3: 419– 423. [DOI] [PubMed] [Google Scholar]
- 8. Johnson MP, McClure PW, Karduna AR. New method to assess scapular upward rotation in subjects with shoulder pathology. J Orthop Sports Phys Ther. 2001; 31 2: 81– 89. [DOI] [PubMed] [Google Scholar]
- 9. Inman VT, Saunders JB, Abbott LC. Observations of the function of the shoulder joint. 1944. Clin Orthop Relat Res. 1996; 330: 3– 12. [DOI] [PubMed] [Google Scholar]
- 10. Kibler WB, Sciascia A. Current concepts: scapular dyskinesis. Br J Sports Med. 2010; 44 5: 300– 305. [DOI] [PubMed] [Google Scholar]
- 11. Warner JJ, Micheli LJ, Arslanian LE, Kennedy J, Kennedy R. Scapulothoracic motion in normal shoulders and shoulders with glenohumeral instability and impingement syndrome: a study using Moiré topographic analysis. Clin Orthop Relat Res. 1992; 285: 191– 199. [PubMed] [Google Scholar]
- 12. Paletta GA, Jr, , Warner JJ, Warren RF, Deutsch A, Altchek DW. Shoulder kinematics with two-plane x-ray evaluation in patients with anterior instability or rotator cuff tearing. J Shoulder Elbow Surg. 1997; 6 6: 516– 527. [DOI] [PubMed] [Google Scholar]
- 13. Solem-Bertoft E, Thuomas KA, Westerberg CE. The influence of scapular retraction and protraction on the width of the subacromial space: an MRI study. Clin Orthop Relat Res. 1993; 296: 99– 103. [PubMed] [Google Scholar]
- 14. Kibler WB. Biomechanical analysis of the shoulder during tennis activities. Clin Sports Med. 1995; 14 1: 79– 85. [PubMed] [Google Scholar]
- 15. Johnson CD, McHugh MP, Wood T, Kibler B. Performance demands of professional male tennis players. Br J Sports Med. 2006; 40 8: 696– 699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Cools AM, Johansson FR, Cambier DC, Velde AV, Palmans T, Witvrouw EE. Descriptive profile of scapulothoracic position, strength and flexibility variables in adolescent elite tennis players. Br J Sports Med. 2010; 44 9: 678– 684. [DOI] [PubMed] [Google Scholar]
- 17. Altchek DW, Weiland DE. Tennis. : Krishnan SG, Hawkins RJ, Warren RF. . The Shoulder and the Overhead Athlete. Philadelphia, PA: Lippincott Williams & Wilkins; 2004: 340– 348. [Google Scholar]
- 18. Pellegrini A, Tonino P, Paladini P, Cutti A, Ceccarelli F, Porcellini G. Motion analysis assessment of alterations in the scapulo-humeral rhythm after throwing in baseball pitchers. Musculoskelet Surg. 2013; 97 suppl 1: 9– 13. [DOI] [PubMed] [Google Scholar]
- 19. Londeree BR, Moeschberger ML. Influence of age and other factors on maximal heart rate. J Cardiac Rehabil. 1984; 4 2: 44– 49. [Google Scholar]
- 20. Kang J, Chaloupka EC, Mastrangelo MA, Donnelly MS, Martz WP, Robertson RJ. Regulating exercise intensity using ratings of perceived exertion during arm and leg ergometry. Eur J Appl Physiol Occup Physiol. 1998; 78 3: 241– 246. [DOI] [PubMed] [Google Scholar]
- 21. McQuade KJ, Dawson J, Smidt GL. Scapulothoracic muscle fatigue associated with alterations in scapulohumeral rhythm kinematics during maximum resistive shoulder elevation. J Orthop Sports Phys Ther. 1998; 28 2: 74– 80. [DOI] [PubMed] [Google Scholar]
- 22. Ebaugh DD, McClure PW, Karduna AR. Effects of shoulder muscle fatigue caused by repetitive overhead activities on scapulothoracic and glenohumeral kinematics. J Electromyogr Kinesiol. 2006; 16 3: 224– 235. [DOI] [PubMed] [Google Scholar]
- 23. Halder AM, Zhao KD, Odriscoll SW, Morrey BF, An KN. Dynamic contributions to superior shoulder stability. J Orthop Res. 2001; 19 2: 206– 212. [DOI] [PubMed] [Google Scholar]
- 24. Wassinger CA, Sole G, Osborne H. Clinical measurement of scapular upward rotation in response to acute subacromial pain. J Orthop Sports Phys Ther. 2013; 43 4: 199– 203. [DOI] [PubMed] [Google Scholar]
- 25. Ryu RK, McCormick J, Jobe FW, Moynes DR, Antonelli DJ. An electromyographic analysis of shoulder function in tennis players. Am J Sports Med. 1988; 16 5: 481– 485. [DOI] [PubMed] [Google Scholar]
- 26. Bowman TG, Hart JM, McGuire BA, Palmieri RM, Ingersoll CD. A functional fatiguing protocol and deceleration time of the shoulder from an internal rotation perturbation. J Athl Train. 2006; 41 3: 275– 279. [PMC free article] [PubMed] [Google Scholar]
- 27. Kawato M. Internal models for motor control and trajectory planning. Curr Opin Neurobiol. 1999; 9 6: 718– 727. [DOI] [PubMed] [Google Scholar]
- 28. Takahashi CD, Nemet D, Rose-Gottron CM, Larson JK, Cooper DM, Reinkensmeyer DJ. Effect of muscle fatigue on internal model formation and retention during reaching with the arm. J Appl Physiol (1985). 2006; 100 2: 695– 706. [DOI] [PubMed] [Google Scholar]
- 29. Su KP, Johnson MP, Gracely EJ, Karduna AR. Scapular rotation in swimmers with and without impingement syndrome: practice effects. Med Sci Sports Exerc. 2004; 36 7: 1117– 1123. [DOI] [PubMed] [Google Scholar]