SUMMARY
Sepsis and the acute respiratory distress syndrome (ARDS) are major causes of mortality without targeted therapies. Although many experimental and clinical observations have implicated gut microbiota in the pathogenesis of these diseases, culture-based studies have failed to demonstrate translocation of bacteria to the lungs in critically ill patients. Here we report culture-independent evidence that the lung microbiome is enriched with gut bacteria both in a murine model of sepsis and in humans with established ARDS. Following experimental sepsis, lung communities were dominated by viable gut-associated bacteria. Ecologic analysis identified the lower gastrointestinal tract, rather than the upper respiratory tract, as the likely source community of post-sepsis lung bacteria. In bronchoalveolar lavage fluid from humans with ARDS, gut-specific bacteria (Bacteroides spp.) were common and abundant, undetected by culture, and correlated with the intensity of systemic inflammation. Alveolar TNF-α, a key mediator of alveolar inflammation in ARDS, was significantly correlated with altered lung microbiota. Our results demonstrate that the lung microbiome is enriched with gut-associated bacteria in sepsis and ARDS, potentially representing a shared mechanism of pathogenesis in these common and lethal diseases.
INTRODUCTION
Sepsis and the acute respiratory distress syndrome (ARDS) are common, costly diseases with high mortality and no targeted therapies1,2. Sepsis is the most common cause of ARDS2,3, and sepsis-related ARDS is more severe and lethal than non-sepsis-related ARDS4. Numerous experimental and clinical observations over decades of study have demonstrated that the gut microbiome plays a key role in the pathogenesis of sepsis and ARDS5: antibiotic-suppressed and germ-free animals are protected from the lung injury and mortality of experimental sepsis6–8, and numerous clinical trials have demonstrated that prophylactic suppression of gut microbiota with antibiotics is protective against multiorgan failure and mortality in patients with critical illness5,9. Yet the mechanism of the gut microbiome’s role in sepsis and ARDS is undetermined5,10,11, and prior studies have been limited by dependence upon culture-based techniques of microbial identification12.
We here report that the lung microbiome is enriched with gut bacteria in experimental sepsis and human ARDS. Enrichment of the lung microbiome by gut-associated bacteria occurs independent of the upper respiratory tract, correlates with severity of systemic inflammation, and results in the persistence of viable bacteria within the lung microbiome. Alveolar TNF-α, a key mediator of alveolar inflammation in ARDS, is significantly correlated with alterations in lung microbiota. Our results suggest a potential common mechanism behind the gut microbiome’s established role in these common diseases of critical illness.
RESULTS
Lung microbiota are altered after experimental sepsis
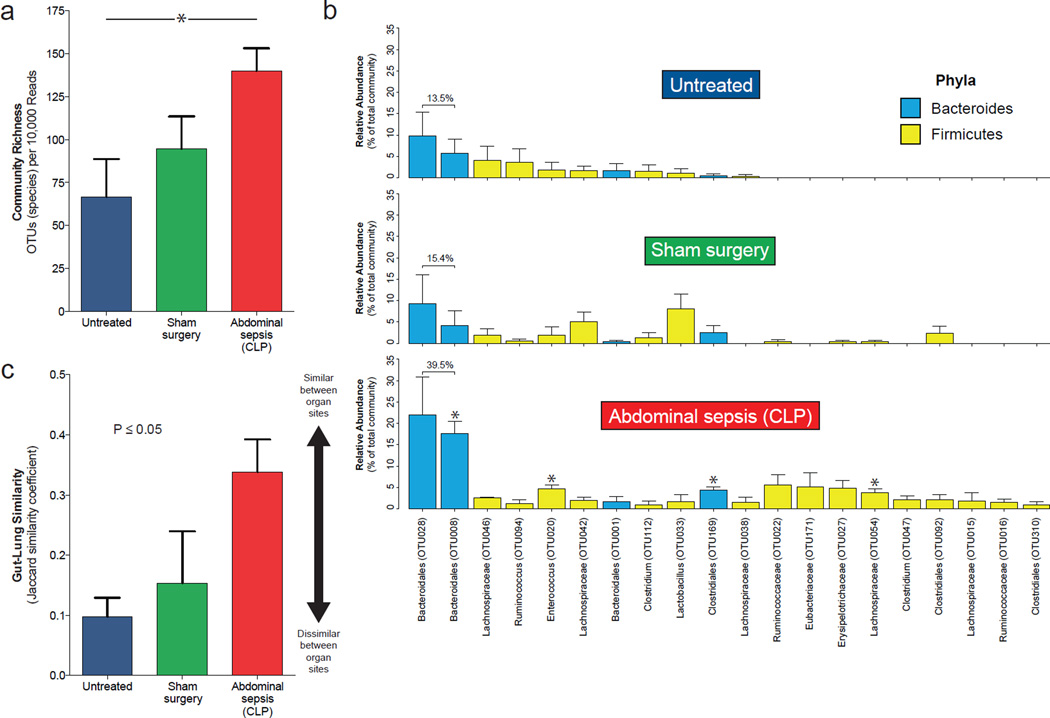
To determine whether sepsis results in altered lung microbiota, we used a well-established model of abdominal sepsis, cecal ligation and puncture (CLP). As previously described, this survivable model provokes transient systemic inflammation that mirrors the human septic response13. We studied the microbiota of the gastrointestinal and respiratory tracts via sequencing of bacterial 16S ribosomal RNA-encoding genes. Compared to the lungs of untreated mice, lungs of post-sepsis mice had greater community richness (number of detectable species) (Fig. 1a), consistent with immigration of new species. Bacterial communities in post-sepsis lungs were significantly distinct from those of untreated mice and mice that underwent sham surgery (P=0.02 for both). Lung communities of post-sepsis mice were significantly enriched with numerous bacteria found in the murine gut, including members of the Bacteroidales order, Enterococcus species (sp.), and Lachnospiraceae sp. (Fig. 1b). The two most abundant taxonomic groups, comprising nearly 40% of community members, were members of the Bacteroidales order, an abundant member of the murine gut microbiome. Abundant taxa in lungs of untreated mice are shown in Supplemental Figure 1. We then directly compared the bacterial community membership of colon and lung communities within each mouse to determine if post-sepsis lung communities more closely resembled those of the gut. Gut-lung similarity was significantly associated with experimental intervention (P≤0.05); gut and lung communities were most similar in post-sepsis lungs and most dissimilar in untreated mice (Fig. 1c).
Figure 1.
Altered lung microbiota 24 hours after experimental sepsis. Abdominal sepsis was induced in mice via cecal ligation and puncture, and lung bacterial communities were sequenced and analyzed after 24 hours. (a) The lungs of post-sepsis mice contained increased species richness compared to untreated mice, consistent with immigration of new species. (b) Relative abundance of bacteria in the lung microbiome following sepsis. The 20 most abundant operational taxonomic units detected in post-sepsis lungs are shown across experimental arms. Asterisks indicate OTUs significantly enriched in post-sepsis lungs compared to control groups. (c) Gut-lung community similarity after sepsis. For each mouse, the community similarity was calculated for paired lung and colon communities. Four mice were used in each intervention group. Group means and standard errors of the mean are depicted. Statistical significance was determined with two-way analysis of variation (ANOVA) with Tukey’s multiple comparisons test. * P ≤ 0.05. Values presented as means ± standard error of the mean. Significance in 1c reflects overall effect of intervention on community richness; between-group differences were not significant after controlling for multiple comparisons.
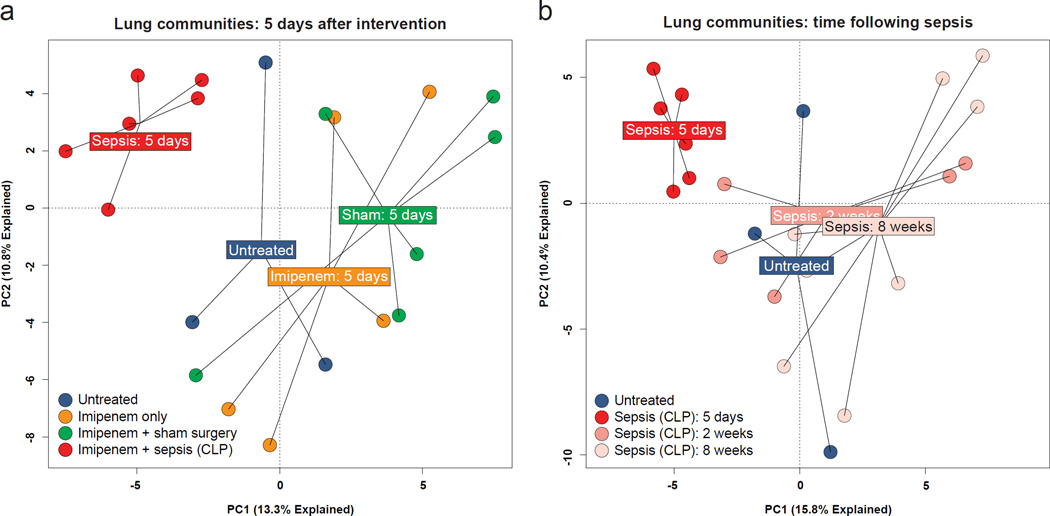
Given this evidence of gut-associated bacteria in the lungs 24 hours after experimental sepsis, we performed an experiment with additional experimental controls and extended timepoints to determine the duration of altered lung microbiota after sepsis. We compared mice exposed to experimental sepsis (CLP and concurrent imipenem) with mice exposed to sham surgery plus imipenem, mice exposed to imipenem only, and mice that received no intervention. We studied their lung communities at five days, two weeks and eight weeks following intervention. Lung communities significantly differed collectively according to intervention at five days (P=0.003). This collective difference in lung microbiota across intervention arms had resolved at two weeks and eight weeks (P>0.05, Supplemental Figure 2). Five days post-sepsis, bacterial communities from lungs of post-sepsis mice were distinct from those of all control groups: sham-surgery-plus-imipenem (P=0.001), imipenem-only (P=0.004), and untreated (P=0.02)(Fig. 2a). By contrast, two weeks and eight weeks following exposure, lung communities from post-sepsis mice were indistinguishable from those of untreated mice (P>0.05, Fig. 2b). Thus the lung microbiome is altered following experimental sepsis, remains altered for at least five days, and normalizes by two weeks.
Figure 2.
Transient alteration of the lung microbiome after experimental sepsis. Mice were exposed to abdominal sepsis (cecal ligation and puncture and imipenem) and compared at multiple timepoints to three experimental control groups: untreated, imipenem only, and imipenem with sham surgery. (a) Five days after exposure, bacterial communities in the lungs of post-sepsis mice were distinct from those of all control groups. (b) Lung communities of post-sepsis mice were distinct from untreated mice after five days but indistinguishable at 2 and 8 weeks following injury.
The post-sepsis lung microbiome is enriched with gut-associated bacteria
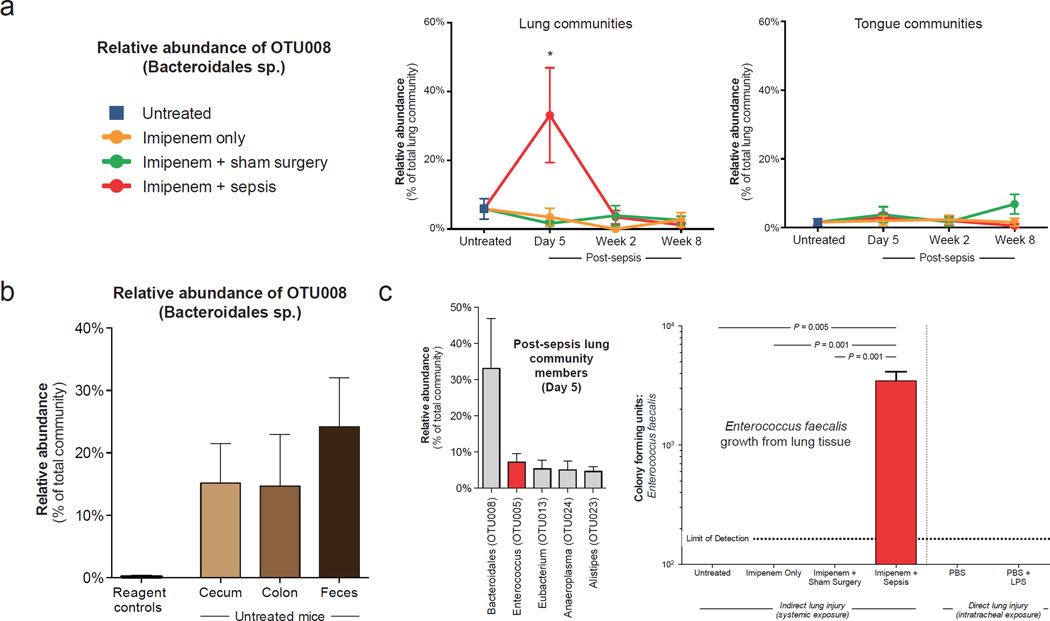
We then performed ecologic analysis to identify the source of altered lung microbiota after sepsis. To determine which bacteria were responsible for the altered communities in post-sepsis lungs, we used biplot analysis of principal component analysis (vegan14) as well as model-based analysis of multivariate abundance data (mvabund15) to identify key microbial drivers of altered communities. Both techniques identified a member of the Bacteroidales order (OTU008) as enriched within the post-sepsis lung community (Supplemental Figure 3a). Alignment searches of sequence databases revealed that while this taxonomic group (sequences with 100% coverage and 100% alignment) has been detected frequently in the murine gut16–18, no cultured specimen has been reported (Supplemental Figure 4). This Bacteroidales OTU comprised one third (33.1%) of total community membership in post-sepsis lungs at five days, and was not enriched in the lungs of any control group (Fig. 3a). Its abundance normalized at two weeks. We analyzed oral bacterial communities to determine if enrichment of the lungs with this Bacteroidales OTU was secondary to altered upper respiratory tract microbiota. This Bacteroidales OTU was not abundant in bacterial communities of the tongues of mice following sepsis at any timepoint (Fig. 3a), indicating that the upper respiratory tract was not the source of altered lung microbiota in the post-sepsis period.
Figure 3.
Evidence suggesting gut-lung translocation after experimental sepsis. (a) The bacterial communities of post-sepsis lungs were dominated by an uncultured bacterium, OTU008 (Bacteroidales sp.) that normalized after 2 weeks. This bacterium did not dominate the bacterial communities detected in simultaneously collected tongue specimens. (b) This Bacteroidales sp. was of minimal abundance in reagent control specimens, but was the most abundant community member in all lower gastrointestinal sites of mice before injury. (c) This Bacteroidales sp. was not detected by culture, but Enterococcus faecalis (the second most abundant species detected in the lungs of mice 5 days after sepsis) was isolated via aerobic culture from the lungs of all post-sepsis mice 5 days after injury. It was not isolated from the lungs of any control group, including mice exposed to direct lung injury via intratracheal LPS instillation. Statistical significance was determined by Kruskal–Wallis one-way analysis of variance with Dunn’s multiple comparisons test (a, c). Values presented as means ± standard error of the mean. Six mice were used in each intervention arm and timepoint. PBS: phosphate-buffered saline. LPS: lipopolysaccharide.
We then compared other potential source communities to determine the origin of this Bacteroidales OTU. This sequence was detected in only one of 14 procedural and reagent control specimens, and comprised only 0.11% of bacterial sequences in these controls (Fig. 3b). By contrast, this Bacteroidales OTU was the most abundant taxonomic group detected in specimens from the gut (cecum, colon and feces) of untreated mice (Fig. 3b), comprising 18% of all sequences. The time course of gut-lung similarity in paired specimens from mice following experimental sepsis is shown in Supplemental Figure 5. This Bacteroidales OTU was detected inconsistently in blood specimens taken from post-sepsis mice (3 of 6 mice at five days post-sepsis). By contrast it was uniformly present in the lungs of post-sepsis mice (6 of 6 mice). Supplemental Figure 6 shows the relative abundance of this Bacteroidales OTU in gut specimens from post-sepsis mice following injury. Taken together, these results indicate that the lower gastrointestinal tract is the most likely source community of bacteria in the post-sepsis lung microbiome. The route of translocation (via portal circulation, systemic circulation or mesenteric lymphatics), if present, remains undetermined.
Unlike bacterial culture, sequencing-based approaches depend only on the presence of bacterial DNA and do not reflect bacterial viability. To determine if the post-sepsis lung microbiome contains viable gut-associated bacteria, we cultured homogenized lung specimens of post-sepsis mice. Enterococcus faecalis was cultured from the lungs of all post-sepsis mice five days after exposure, and was not cultured from the lungs of mice in any control group (Fig. 3c). No bacterial growth, E. faecalis or otherwise, was observed from concurrent blood cultures. E. faecalis corresponded genetically to the second most abundant OTU in lungs of post-sepsis mice (Fig. 3c) and was identified by mvabund as relatively enriched within lungs of post-sepsis mice. As it has previously been reported that lung injury alone, in the absence of sepsis, is sufficient to alter the lung microbiome of mice19, we used a model of direct lung injury (intratracheal lipopolysaccharide [LPS] instillation) to test whether direct lung injury could provoke the outgrowth of gut-associated bacteria. No bacterial growth, E. faecalis or otherwise, was observed from the lungs of either the LPS-instilled mice or those of controls (Fig. 3c). These data demonstrate that the gut-associated bacteria present in the post-sepsis lung microbiome are viable, and are not attributable to local inflammation alone.
To determine if enrichment of lung microbiota with gut-associated bacteria was specific to the CLP model, we employed a systemic LPS model of sepsis for validation. One day after LPS-induced shock, lung communities were significantly distinct from those of untreated mice (P=0.004, Supplemental Figure 7a), a difference that resolved by 4 days. This was driven by an Enterobacteriaceae-classified OTU that was enriched in post-sepsis lungs compared to those of untreated mice (P<0.01, Supplemental Figure 7b–c). A database alignment search determined that this OTU shares 100% genomic identity with gut-associated members of the Enterobacteriaceae family such as Enterobacter cloacae and Klebsiella pneumoniae (Supplemental Figure 7d). We concluded that enrichment of the lung microbiome with gut-associated bacteria is not specific to the CLP model of sepsis.
The lung microbiome of humans with ARDS is enriched with uncultured gut bacteria
Given this experimental evidence suggesting translocation of gut bacteria to the lungs in sepsis, we asked if gut-associated bacteria are present in the lung microbiota of humans with ARDS. We sequenced bacterial communities in 100 specimens of bronchoalveolar lavage (BAL) fluid collected from 68 patients with ARDS, and compared these communities to those of seven healthy volunteers. Demographics and clinical features of ARDS patients are presented in Supplemental Table 1. We employed analysis of multivariate abundance (mvabund) to identify taxa enriched in BAL specimens from patients with ARDS relative to healthy subjects (Supplemental Figure 3b); of these, we focused on a prominent member of the Bacteroides genus (OTU009) that was classified to the same order (Bacteroidales) as the OTUs enriched in the post-sepsis lungs in our murine experiments. Alignment searches of databases revealed perfect alignment (100% coverage, 100% alignment) between this Bacteroides sp. and four anaerobic species abundant in the human gut20–22: B. fragilis, B. thetaiotaomicron, B. faecichinchillae and B. salyersiae (Supplemental Figure 4). Of the 24 BAL specimens in this cohort studied by aerobic culture at the University of Michigan Clinical Microbiology Laboratory, none grew Bacteroides sp., despite culture-independent identification of this organism in eight (33%), confirming the limited sensitivity of aerobic culture-based techniques in identifying gut-associated anaerobes in respiratory specimens.
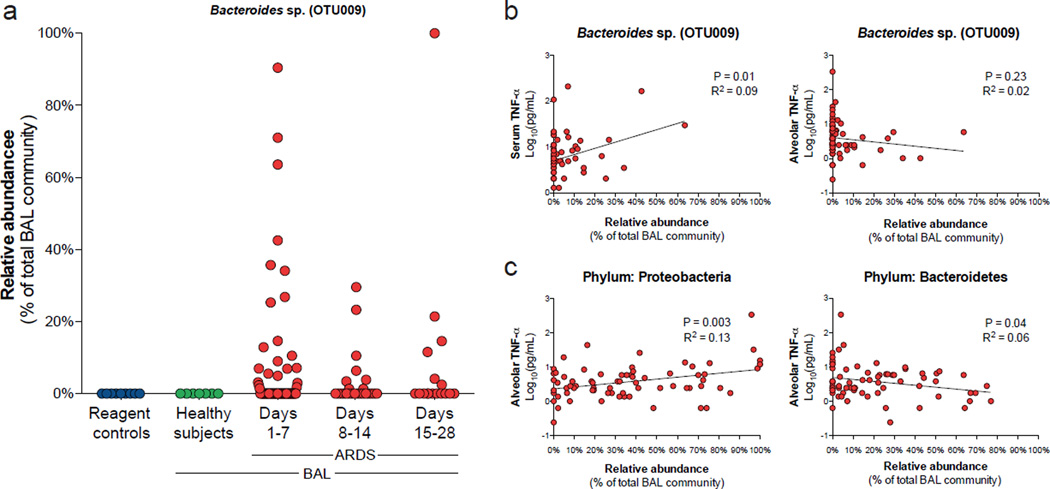
This gut-associated Bacteroides OTU was common and abundant in the BAL fluid of patients with ARDS, and was not detected in reagent control specimens nor in the BAL fluid of healthy subjects (Fig. 4a). It was detected in 33% (33) of ARDS BAL specimens, representing 41% (28) of all unique ARDS patients. This Bacteroides OTU comprised 5.7% of all sequences detected in ARDS BAL specimens. Supplemental Figure 8 shows the relative stability of this OTU in BAL communities of patients for whom serial BAL specimens were available. No association was detected between relative abundance of this Bacteroidales OTU and time since onset of ARDS, predisposing factor for ARDS, or severity of illness at diagnosis (P>0.05 for all). In a validation analysis using a previously published data set of bacterial communities sequenced from BAL from healthy subjects23, we identified a representative sequence corresponding to this Bacteroides OTU (100% alignment). This Bacteroides OTU was detected in the BAL of only one of twenty-six healthy subjects. Thus collectively this gut-associated Bacteroides sp. was detected in the lungs of only one of thirty-three (3.0%) healthy subjects, confirming it is not a normal community member in the healthy lung microbiome.
Figure 4.
Evidence suggesting gut-lung translocation of bacteria in humans with the acute respiratory distress syndrome (ARDS). A Bacteroides sp. (OTU009), a representative of most abundant bacterial genus in the human gut microbiome, was absent from reagent control specimens and the lungs of healthy subjects, but common (33% of specimens) in the lungs of patients with ARDS (a). The relative abundance of this Bacteroides sp. was positively correlated with serum TNF-α but not associated with alveolar TNF-α (b). By contrast, alveolar TNF-α was positively correlated with relative abundance of the Proteobacteria phylum and negatively correlated with the Bacteroidetes phylum (c). 100 bronchoalveolar lavage specimens from 68 unique patients were studied. Statistical significance was determined by linear regression using logarithmically-transformed cytokine data (b, c).
We then asked if enrichment of lung microbiota with gut bacteria was associated with systemic and alveolar inflammation, both as measured on the day of bronchoscopy. We compared alveolar microbiota with concentrations of TNF-α in serum (which is correlated with the diagnosis and severity of sepsis24,25) and BAL fluid (which is correlated with the diagnosis, severity and mortality of ARDS26,27). Among patients with ARDS, we observed a significant association between relative abundance of this gut-associated Bacteroides OTU and patients’ concurrent serum TNF-α concentration (P=0.01, Fig. 4b). This finding indicates that enrichment of gut bacteria in the lung microbiome is correlated with severity of acute systemic inflammation. By contrast, no association was found between relative abundance of this Bacteroides OTU and alveolar TNF-α concentration (P>0.05, Fig. 4b), suggesting that gut-lung bacterial translocation, if present, correlates with systemic, but not alveolar, inflammation. Relative enrichment of lung microbiota with the Proteobacteria phylum has been repeatedly associated with inflammatory lung disease28–30, as compared to enrichment with Bacteroidetes (e.g. Prevotella genus), the most abundant phylum in the healthy respiratory tract27,28. We hypothesized that relative abundance of Proteobacteria in the lungs of patients with ARDS would be correlated with alveolar inflammation. A significant positive correlation was observed between relative abundance of Proteobacteria and alveolar TNF-α (P=0.003, Fig. 4c). This relationship remained significant when we excluded specimens from subjects with a predisposing condition of pneumonia (P=0.02). By contrast, relative abundance of the usually prominent Bacteroidetes phylum was negatively correlated with alveolar TNF-α (P=0.04, Fig. 4c). These data confirm that key features of alveolar inflammation in ARDS are associated with alterations in lung microbiota.
DISCUSSION
The core finding of our study is that gut-associated bacteria, undetectable via conventional culture techniques, enrich the lung microbiome in experimental sepsis and human ARDS. Microbial evidence suggesting gut-lung translocation and disorder of the lung microbiome are respectively correlated with indices of systemic and alveolar inflammation. Our results suggest a potential common mechanism behind the gut microbiome’s established role in these common and lethal diseases.
The importance of the gut microbiome in the pathogenesis of critical illness has been established for more than sixty years6, though to date the mechanism of its role has been undetermined5,10,11. Suppression of gut bacteria, either via enteric antibiotics or use of germ-free animals, is protective against the lung injury and mortality of critical illness, a robust observation described widely across species (mice8,31, rats32, rabbits7 and dogs6) and models of shock (hemorrhage6, sepsis7 and ischemia/reperfusion8). Dozens of clinical trials have demonstrated that suppression of the gut microbiome (selective decontamination of the digestive tract) is protective against multiorgan failure and mortality in patients with critical illness5,9. Permeability of the intestinal wall is increased in critical illness and predictive of clinical outcome33, and culture-identified translocation of gut bacteria to mesenteric lymphatics is observed in experimental shock34 and predictive of subsequent sepsis in postoperative patients35. In a recent culture-independent study of patients undergoing hematopoietic stem cell transplant, features of the gut microbiome were predictive of pulmonary infiltrates (as observed in ARDS) and mortality36. Yet prior studies have failed to find evidence of bacterial translocation via sampling of the systemic, portal and lymphatic circulations12,37. Two potential explanations may explain the discrepancy between our findings and those of previous studies. Firstly, our culture-independent methodology is far more sensitive than prior culture-based approaches, as many bacteria in the human gut are undetectable via conventional culture38. The dominant lung bacteria in our experimental sepsis model is an as-of-yet uncultured Bacteroidales sp., and the most prominent gut-associated bacteria in our human ARDS specimens were of the Bacteroides genus; neither grow in the standard conditions of clinical microbiology laboratories. Secondly, our results demonstrate the persistence of viable gut bacteria in the lungs days after sepsis, even in the absence of persistent bacteremia. This indicates that even a brief, transient immigration of gut bacteria may alter the lung microbiome. Gut permeability and the toxicity of mesenteric lymph peak in the immediate hours following experimental shock39,40, so subsequent assessment of blood or mesenteric lymph may fail to detect the presence of bacteria.
Our study is the first culture-independent analysis of the human lung microbiome in ARDS. Previous culture-dependent studies have suggested a relationship between bacteria of the respiratory tract and the pathophysiology of ARDS5. Pneumonia occurs far more frequently in patients with ARDS than in other mechanically ventilated patients41, and pulmonary exposure to bacterial factors (e.g. LPS and flagellin) provokes inflammation and injury characteristic of ARDS. Culture-independent studies of mechanically ventilated patients have demonstrated a previously unappreciated complexity to the respiratory microbiome5,42, and animal experimentation has recently shown that direct lung injury alters the lung microbiome19. In our study, disorder of the lung microbiome, characterized by enrichment with the Proteobacteria phylum (commonly enriched in the lung microbiota of patients with inflammatory lung conditions28–30) was significantly associated with elevated alveolar concentrations of TNF-α, a key mediator of pulmonary inflammation in ARDS that is independently predictive of mortality27. By contrast, decreased alveolar concentrations of TNF-α were associated with enrichment of the lung microbiome with Bacteroidetes, the most abundant phylum in the lung microbiome of healthy subjects23,28. Our results do not imply that bacterial translocation and dysbiosis are the sole or primary cause of ARDS, as numerous non-bacterial exposures (e.g. oleic acid, hydrochloric acid and gut ischemia factors40) can initiate alveolar injury, and the complex clinical syndromes of sepsis and ARDS each encompass multiple pathophysiological pathways. Sepsis and ARDS both have dynamic and temporally heterogeneous clinical and biological courses; our study of BAL specimens from patients with established ARDS may not reflect the microbiology of early and developing ARDS. Though we could control for antibiotic exposure in our murine model of sepsis, the effects of ubiquitous antibiotic exposure on lung microbiota in humans with ARDS is unknown. Additionally, though TNF-α is a key mediator in these conditions (systemically in sepsis28,29, in the alveolar space in ARDS30,31), it alone cannot represent the complexity of the dysregulated host response of critical illness. Further study will be needed to determine the role of lung microbiota in the initiation, augmentation and perpetuation of ARDS.
In both our animal model of sepsis and our human study of ARDS, we identified prominent anaerobic gut-associated bacteria not previously implicated in sepsis or ARDS. The Bacteroidales OTU that dominated post-sepsis lungs has previously been identified molecularly, but not cultured, in the murine gut16–18. Separately, a distinct OTU of the Bacteroides genus was common and abundant in lungs of humans with ARDS but absent from those of healthy subjects. This genus is the most abundant taxonomic group in the human gut microbiome43, and this OTU was absent from lung specimens both in our study’s healthy subjects and from previously published reports of the normal lung microbiome23,44,45. Within the field of environmental microbiology, molecular detection of the Bacteroides genus is used as an indicator of human fecal contamination in watersheds46. Our results suggest it may serve a similar role within the respiratory ecosystem. The relative abundance of this Bacteroides OTU in the lung microbiome, plausibly reflecting the degree of gut-lung translocation, was significantly associated with serum concentrations of TNF-α, a key mediator of the septic stress response that is predictive of patient mortality24,25. In an innovative recent study of patients with established ARDS, latent class analysis identified a subphenotype of ARDS patients characterized by high systemic inflammation, associated with worse prognosis and distinct response to therapy47. Our finding that systemic TNF-α correlates with enrichment of gut bacteria in BAL fluid suggests that this subphenotype may be characterized by differences in lung microbiota. Importantly, the Bacteroides genus is highly variable in its abundance, is dominant in only a subset of healthy adults43, and is diminished in patients with established critical illness48. It is thus not a universal marker of human gut microbiota. Further longitudinal study of paired stool and lung specimens will be needed to determine the true prevalence of gut-lung translocation in sepsis and ARDS.
The lung microbiome is determined by the balance of three ecological factors: immigration, elimination and the relative growth rates of resident microbiota49. Our experimental results demonstrate that the upper respiratory tract, the lung microbiome’s primary source community in health, is not the source of altered lung microbiota after sepsis. Though our findings suggest a mechanism of immigration via translocation of gut microbiota, a competing explanation is relative outgrowth of bacteria present in low abundance before injury. Indeed, the Bacteroidales OTU enriched after CLP-induced sepsis was detectable in low levels in lung communities of untreated mice. Yet E. faecalis, detected via culture in all post-sepsis lung specimens, was not cultured from the lungs of any control animal. Thus if this gut-associated bacteria is present in lung communities before injury, its abundance is less than our assay’s very low limit of detection (100 CFUs per lung). Analogously, if the Bacteroides OTU that was abundant in our human ARDS specimens is present in the healthy lung microbiome, it is present but below the highly sensitive limit of detection of 16S sequencing. Further, our model of direct lung injury (intratracheal LPS) resulted in no detectable outgrowth of gut-associated bacteria, a finding consistent with previously published studies19. Definitive proof of gut-lung translocation will require additional study, including techniques such as paired metagenomic comparisons of gut and lung microbiota and use of labeled “tracer” bacteria in gnotobiotic animals. We have recently posited a conceptual model of how alveolar inflammation and injury can both perpetuate - and be perpetuated by - disordered bacterial communities in the respiratory tract5,50. The significant positive correlation we report between alveolar TNF-α and enrichment with the Proteobacteria phylum is evidence that even in the absence of gut-lung translocation, the microbiome may play an important role in ARDS.
In summary, these data demonstrate that the lung microbiome is enriched with gut bacteria in experimental sepsis and human ARDS. Enrichment with gut bacteria is significantly associated with key features of systemic inflammation. Alveolar TNF-α, a key mediator of the alveolar inflammation of ARDS, is significantly correlated with disorder of the lung microbiome. Our findings suggest that gut-lung translocation and alteration of the lung microbiome may represent a common mechanism of pathogenesis in sepsis and ARDS, and suggest potential therapeutic targets for the prevention and treatment of these common and lethal diseases.
ONLINE METHODS
Ethics statement
The animal studies contained in this manuscript were approved by the University Committee on the Care and Use of Animals (UCUCA) at the University of Michigan. Laboratory animal care policies at the University of Michigan follow the Public Health Service policy on Humane Care and Use of Laboratory Animals. Animals were assessed twice daily for physical condition and behavior. Animals assessed as moribund were humanely euthanized by CO2 asphyxiation.
All clinical investigations were conducted according to the principles expressed in the Declaration of Helsinki. The human study protocol was approved by the institutional review board of the University of Michigan Healthcare System. All patients or their legal surrogates provided written informed consent. The institutional review boards have examined the protocols and certified that “The risks are reasonable in relation to benefits to subjects and the knowledge to be gained. The risks of the study have been minimized to the extent possible.”
Mice
8- to 12-week old male C57Bl/6 mice were purchased from Jackson Laboratories and housed under specific pathogen-free conditions. For safety, post-surgical (sham and CLP) mice were housed separately from untreated and antibiotic-only mice. Apart from this isolation of post-surgical mice, mice were not separately housed according to intervention arm or timepoint. Given the copraphagic behavior of co-housed mice, cage number was recorded for each mouse and incorporated as a potential confounder into multivariable microbiome analysis as reported in Results. Intervention group was determined for each mouse by random selection by investigators. In the initial (24 hour CLP) experiment, four mice were used per intervention arm. In the subsequent experiment (extended timepoint CLP), six mice were used per intervention arm per timepoint. These numbers were used based on prior experiments on antibiotic-treated mice that demonstrated appreciable microbial community effects comparing comparably sized groups. Except as where reported otherwise, all reported replicates were biological (distinct mice separately exposed to the same intervention) rather than technical (repeated measurement or analysis of the same sample).
Cecal ligation and puncture (CLP)
CLP was used as a model of systemic sepsis syndrome as previously described13,51. Mice were anesthetized with a mixture of intraperitoneal xylazine and ketamine. A 1-cm longitudinal incision was made to the lower-right quadrant of the abdomen and the cecum exposed. The distal one-third of the cecum was ligated with a 3-0 silk suture and punctured through with a 19-gauge needle. The cecum was then placed back in the peritoneal cavity, and the incision was closed with surgical staples. In sham surgical controls, the cecum was exposed but not ligated or punctured, then returned to the abdominal cavity. All mice were administered 1 ml of sterile saline subcutaneously for fluid resuscitation and 0.5 mg of subcutaneous imipenem during the immediate postoperative period. As described in Results, various control arms received no intervention, imipenem only, imipenem plus sham surgery, and imipenem plus CLP. Each experiment, as detailed in Results, was performed once. No unreported experiments have been omitted from Results.
Lipopolysaccharide models
Lipopolysaccharide (LPS) (derived from Escherechia coli 0111:B4, Sigma-Aldrich) was given systemically as a model of systemic shock and intratracheally as a model of direct lung injury. Systemic shock was induced using a single intraperitoneal injection of 5 mg/kg. Control mice received an intraperitoneal injection of phosphate buffer solution (PBS). Mice were harvested at 1 day and 4 days following exposure. Direct lung injury was induced via intratracheal instillation of 10 μg LPS; control mice received an intratracheal instillation of PBS. Mice were harvested 3 days following exposure.
Mouse tissue collection and processing
Mice were euthanized via CO2 asphyxiation. Low biomass specimens (tongue, lung) were removed prior to high biomass specimens (cecum, colon, feces). Blood was collected from mice during harvest using needle aspiration via the right ventricle. Instruments were rinsed with ethanol and flamed between each organ. Murine lungs were excised, placed in tubes containing 1 ml of sterile water and homogenized mechanically by using a Tissue-Tearor (Biospec Products, Bartlesville, Okla.). The tissue homogenizer was cleaned and rinsed in ethanol and water between each tissue. Water control specimens from homogenization, exposed to cleaned instruments, were included in sequencing as procedural controls.
Lung and blood CFU assay
Aliquots of lung homogenates and blood were plated onto LB media in 10-fold dilutions and incubated aerobically at 37°C. Colonies were counted after 24 hours of growth. In addition to the Enterococcus growth depicted in Figure 3, the lungs of two sham surgery animals and one post-sepsis animal grew Lactobacillus spp., and the lungs of one CLP mouse grew Staphylococcus sp. Overall CFU counts were significantly greater in post-sepsis lungs (P ≤ 0.01), and the specific growth of Lactobacillus spp. and Staphylocococcus sp. was not significantly different across intervention arms (P > 0.05). No growth was observed three days after intratracheal instillation of PBS or PBS and LPS. CFUs were plated and measured in duplicate for each mouse; values reported are means for each animal.
Subject enrollment
All human ARDS subjects were enrolled in a multicenter randomized trial of recombinant human granulocyte-macrophage colony stimulating factor for patients with ARDS (ClinicalTrials.gov number NCT00201409). Details of study sites and enrollment have previously been described52. ARDS was defined clinically as per the American-European Consensus Conference definition53. Patients were excluded if younger than 18 years, if 7 or more days had elapsed since onset of ARDS, if there was evidence of preexisting chronic respiratory failure, if the patient was neutropenic, if the patient had a history of hematologic malignancy or bone marrow transplantation, if the patient was already enrolled in other therapeutic trials or if the patient or his/her authorized decision maker or attending physician had decided to forego aggressive care. Patients were enrolled within 7 days of first meeting criteria for ARDS. Reported timepoints are relative to the time of randomization. Both pre-intervention and post-intervention BAL specimens were used from patients in both study arms. Randomization to the GM-CSF arm had no detectable effect on BAL microbiota (P > 0.05, PERMANOVA) or the abundance of the Bacteroidetes-classified OTU009, using either initial or post-intervention BAL specimens. Healthy control subjects were recruited from the southeast Michigan community. All control subjects were less than 55 years of age, were taking no medications, and were life-long nonsmokers. The validation cohort of BAL specimens from healthy subjects has previously been published and described in detail23. Specimens in this cohort were similarly sequenced using the 454 Pyrosequencing platform, though whole BAL specimens were used; the cell removal step does result in detection of a related but taxonomically distinct community in BAL fluid54.
Study population
We sequenced 100 specimens of BAL fluid collected from 68 unique patients with ARDS admitted to intensive care units in three academic medical centers: University of Michigan Medical Center, Emory University Hospitals, and the University of Colorado Denver. Mean time since study enrollment (which was within 7 days of meeting ARDS criteria) was 8.7 ± 6.2 days. 25 specimens were obtained within 3 days of enrollment, 61 within seven days, 84 within two weeks and 99 within 3 weeks; one specimen was obtained 28 days after study enrollment. Patients had a mean age of 47.4 ± 14.5 years and were predominantly male (67%) and Caucasian (66%). The most common ARDS risk factors were pneumonia (29.4%), sepsis (26.4%) and aspiration (20.6%). Other etiologies included pancreatitis, trauma and transfusion-related lung injury. Additional information including clinical microbiology results and antibiotic exposure was obtained from the electronic medical records of 18 subjects enrolled at the University of Michigan Medical Center representing 24 total BAL fluid specimens. Of these, at the time of bronchoscopy all specimens (100%) were obtained while the subject was receiving antibiotics, and most (83.3%) were obtained while subjects were receiving multiple antibiotics. The most common antibiotics used were vancomycin (50%), piperacillin-tazobactam (41.7%), levofloxacin (41.7%) and cefepime (16.7%). Relatively few specimens were obtained from subjects receiving antifungal therapy (12.5%) or macrolide antibiotics (8.3%). The most common clinical microbiology results were no growth (37.5%), “oral flora” (33.3%), Pseudomonas aeruginosa (8.3%), Burkholderia cepacia (8.3%) and Staphylococcus spp. (8.3%).
BAL collection and processing
BAL was performed using standard technique before randomization and at designated timepoints following enrollment (3 days, 7 days, 14 days, 21 days). One hundred sixty milliliters of sterile isotonic saline was instilled in 20-mL aliquots, with gentle suctioning after each aliquot. Bronchoscopy was not performed for research purposes if the P/F ratio was less than 100, the patient was deemed to be too unstable by the attending clinician, or the surrogate declined participation in this portion of the study. Cells were separated via centrifugation (11g for 10 minutes), and the cell-free supernatant was frozen at −80°C for subsequent assays. Cell-free supernatants were subsequently centrifuged (22,500g for 30 minutes) with the resulting pellet used for DNA isolation.
Bacterial DNA isolation
Genomic DNA was extracted from mouse tissue and human acellular BAL pellets resuspended in 360μl ATL buffer (Qiagen DNeasy Blood & Tissue kit) and homogenized in UltraClean fecal DNA bead tubes (MO-BIO, Carlsbad, CA) using a modified protocol previously demonstrated to isolate bacterial DNA55. Sterile laboratory water and AE buffer used in DNA isolation were collected and analyzed as potential sources of contamination.
16S DNA sequencing
Mouse tissue specimens
The V4 region of the 16s rRNA gene was amplified using published primers56 and the dual-indexing sequencing strategy developed by the laboratory of Patrick D. Schloss57. Sequencing was performed using the Illumina MiSeq platform, using a MiSeq Reagent Kit V2 (500 cycles), according to the manufacturer’s instructions with modifications found in the Schloss SOP58. Accuprime High Fidelity Taq was used in place of Accuprime Pfx SuperMix. Primary PCR cycling conditions were 95°C for two minutes, followed by 20 cycles of touchdown PCR (95°C 20 seconds, 60°C 20 seconds and decreasing 0.3 degrees each cycle, 72°C 5 minutes), then 20 cycles of standard PCR (95°C for 20 seconds, 55°C for 15 seconds, and 72°C for 5 minutes), and finished with 72°C for 10 minutes.
Human BAL specimens
The V3-V5 hypervariable regions of the bacterial 16S rRNA gene were sequenced in the V5-V3 direction using barcoded primer sets corresponding to 357F and 926R59. These barcoded primers were originally developed by the Broad Institute. Primary PCR cycling conditions were 95°C for two minutes, followed by 20 cycles of touchdown PCR (95°C 20 seconds, followed by an annealing for 30 seconds beginning at 60°C and decreasing one degree every two cycles until 50°C, and an elongation of 72°C 45 seconds), then 20 cycles of standard PCR (95°C for 20 seconds, 50°C for 30 seconds, and 72°C for 45 seconds), and finished with 72°C for 5 minutes. Quality control and sequencing was carried out at the University of Michigan, using the Roche 454 GS Junior according to established protocols60.
Cytokine measurement in ARDS patients
TNF-α was measured in the 74 human BAL fluid specimens for which adequate fluid was available, acquired from 55 unique patients. TNF-α was also measured in 58 serum specimens collected from 46 unique patients. These serum specimens were collected on the same day as the bronchoscopy used for comparison. TNF-α was measured in serum and BAL fluid using enzyme-linked immunosorbent assay (R & D Systems) according to the manufacturer’s protocol. Samples were assayed in duplicate and individual data points analyzed and presented as mean values. Cytokine values were log-transformed to obtain a normal distribution prior to regression analysis.
Statistical analyses
Sequence data were processed and analyzed using the software mothur v.1.27.0 according to the Standard Operating Procedure for 454 and MiSeq sequence data using a minimum sequence length of 250 basepairs58,61,62. For each experiment and sequencing run, a shared community file and a phylotyped (genus-level grouping) file were generated using operational taxonomic units (OTUs) binned at 97% identity generated using the dist.seqs, cluster, make.shared and classify.otu commands in mothur. OTU numbers were arbitrarily assigned in the binning process and are referred to throughout the manuscript in association with their most specified level of taxonomy. Classification of OTUs was carried out using the mothur implementation of the Ribosomal Database Project (RDP) Classifier and the RDP taxonomy training set 9 (fasta reference = trainset9_032012.pds.fasta, taxonomy reference = trainset9_032012.pds.tax), available on the mothur website. Sequences are available via the NCBI Sequence Read Archive (accession numbers SRP067346 and SRP067513).
We performed microbial ecology analysis using the vegan package 2.0-4 and mvabund in R14,15,63. For relative abundance and ordination analysis, samples were normalized to the percent of total reads and we restricted analysis to OTUs that were present at greater than 1% of the sample population; all OTUs were included in diversity analysis. Direct community similarity comparisons were performed using the Jaccard similarity index. We performed ordinations using Principal Component Analysis on Hellinger-transformed normalized OTU tables generated using Euclidean distances64. We determined significance of differences in community composition using PERMANOVA (adonis) with 1000 permutations using Euclidean distance matrix. We performed all analyses in R and GraphPad Prism 6. We compared means via paired t-test and paired ANOVA with Tukey’s multiple comparisons test as appropriate. Linear regressions between relative abundances and cytokine concentrations were performed using log-transformed cytokine concentrations and adjusted for intrasubject correlations. Permutation analysis using serial exclusion of subjects was performed to confirm that significance did not depend on the inclusion of outliers. Investigators were not blinded to intervention status of specimens during analysis.
In the first sequencing run (454, ARDS BALs), we obtained 1587 ± 1085 reads per specimen and no specimens were excluded from analysis. In the second sequencing run (MiSeq, CLP, 24 hour time point), we obtained 26,440 ± 38,804 reads per specimen. Four specimens, all blood, had too few reads to interpret (range 5–19 reads) and were excluded from analysis. In the third sequencing run (MiSeq, CLP, extended time points), we obtained 23,725 ± 33,792 reads per specimen. Nine specimens were excluded from analysis because they had too few reads to interpret (range 16–237 reads): four blood specimens, two cecum specimens, two reagent control specimens, one feces specimen and two lung specimens.
Representative sequences of key microbiota
The representative sequence of the Bacteroidales OTU (OTU008) depicted in Figure 3 is: TACGGAGGATGCGAGCGTTATCCGGATTTATTGGGTTTAAAGGGTGCGTAGGCGGCCTGCCAAGTCAGCGGTAAAATTGCGGGGCTCAACCCCGTACAGCCGTTGAAACTGCCGGGCTCGAGTGGGCGAGAAGTATGCGGAATGCGTGGTGTAGCGGTGAAATGCATAGATATCACGCAGAACCCCGATTGCGAAGGCAGCATACCGGCGCCCGACTGACGCTGAGGCACGAAAGTGCGGGGATCAAACAGG.
The representative sequence of the Bacteroidetes OTU (OTU009) depicted in Figure 4 is: TCTTGAGTACAGTAGAGGTGGGCGGAATTCGTGGTGTAGCGGTGAAATGCTTAGATATCACGAAGAACTCCGATTGCGAAGGCAGCTCACTGGACTGCAACTGACACTGATGCTCGAAAGTGTGGGTATCAAACAGGATTAGATACCCTGGTAGTCCACACAGTAAACGATGAATACTCGCTGTTTGCGATATACAGTAAGCGGCCAAGCGAAAGCATTAAGTATTCCACCTGGGGAGTACGCCGGCAACGGTGAA.
Identification of procedural contaminants
Reagents used in DNA isolation and library preparation contain bacterial DNA that can contaminate sequence-based studies of microbial communities65. To identify potential sources of contamination in sequencing, we collected multiple procedural controls, including sterile water used in tissue collection (exposed to instruments used in harvesting and tissue homogenization), sterile water used in library preparation, and AE buffer used in DNA isolation. Procedural and environmental control specimens from the collection of human BAL specimens were not collected at the time of sampling and were not analyzed, including bronchoscope rinse specimens, endotracheal tube specimens, and sterile (pre-lavage) saline. These procedural controls and mock community standards were analyzed as quality controls in each sequencing run. Specimens were processed in a randomized order to minimize the risk of false pattern formation due to reagent contamination65. The presence of bacterial DNA in all procedural controls was confirmed in all three sequencing runs. In the first sequencing run (human ARDS BAL specimens), both sterile water used in specimen processing and AE buffer from the DNA isolation kit were sequenced. Sequences detected in procedural control specimens were significantly distinct from sequences detected in both ARDS BAL specimens and healthy subject BALs (P ≤ 0.001 for both). The dominant taxa in procedural control specimens were a Lachnospiraceae sp. (OTU036) and an unclassified OTU (OTU016), which comprised a mean of 22.1% of sequences in procedural controls but only 0.44% of sequences in BAL specimens. The Bacteroidetes sp. discussed in Results (OTU009) was not detected in any of the eight procedural control specimens (0% of total sequences). In the second experiment (CLP, 24-hour timepoint), procedural control specimen communities were distinct from all tissue communities (P < 0.05 for blood, P < 0.004 for all other organ sites). The most abundant OTUs in procedural controls (comprising a mean of 45.1% of sequences) were an Acinetobacter sp. (OTU030), a Pelomonas sp. (OTU023), an unclassified OTU (OTU100) and a Clostridium sp. (OTU009). These were common and abundant in blood specimens (comprising a mean of 19.0% of sequences) but infrequent and in low abundance in colon, tongue and lung specimens (comprising a mean of 1.6% of sequences). In the third experiment (CLP, extended timepoints), all types of procedural control specimen communities were distinct from the communities of all tissue types (P < 0.001 for all comparisons). All procedural control specimens were dominated by a single Pseudomonas sp. (OTU004) that comprised a mean of 46.7% of reads; its presence both in specimen collection water and in kit reagent specimens confirmed that it was introduced in sequencing preparation rather than upstream in the tissue collection step. It was excluded from analysis; this was the only OTU excluded from any analysis in this study. The Bacteroidales sp. (OTU008) discussed in Results was detected in only one of fourteen procedural control specimens, and comprised a mean of only 0.11% of all sequences.
Supplementary Material
Acknowledgments
Funding provided by the National Institutes for Health (UL1TR000433 [RPD], K23HL130641 [RPD], T32HL00774921 [BHS], R01HL123515 [TJS], UO1HL123031 [TJS], U01HL098961 [GBH] and R01HL114447 [GBH]). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Support provided by the Michigan Institute for Clinical & Health Research [RPD], the Host Microbiome Initiative of the University of Michigan [RPD, BHS], and the University of Michigan Center for Integrative Research in Critical Care [RPD]. The authors thank the University of Michigan Multidisciplinary Intensive Care Research Workgroup for helpful discussions and Alexander Bredenkamp for bioinformatic assistance.
Footnotes
AUTHOR CONTRIBUTIONS
RPD and BHS conceived the experiment. RPD, BHS, TJS and GBH designed the study. RPD, BHS, MWN and NRF performed experiments. RPD analyzed data. RPD, BHS, JRE, TJS and GBH provided critical analysis and discussions. RPD wrote the first draft, and all authors participated in revision.
COMPETING FINANCIAL INTERESTS
The authors declare no competing financial interests.
References
- 1.Angus DC, et al. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit. Care Med. 2001;29:1303–1310. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Rubenfeld GD, et al. Incidence and outcomes of acute lung injury. N. Engl. J. Med. 2005;353:1685–1693. doi: 10.1056/NEJMoa050333. [DOI] [PubMed] [Google Scholar]
- 3.Hudson LD, Milberg JA, Anardi D, Maunder RJ. Clinical risks for development of the acute respiratory distress syndrome. Am. J. Respir. Crit. Care Med. 1995;151:293–301. doi: 10.1164/ajrccm.151.2.7842182. [DOI] [PubMed] [Google Scholar]
- 4.Sheu CC, et al. Clinical characteristics and outcomes of sepsis-related vs non-sepsis-related ARDS. Chest. 2010;138:559–567. doi: 10.1378/chest.09-2933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dickson RP. The microbiome and critical illness. Lancet Respir. Med. 2016;4:59–72. doi: 10.1016/S2213-2600(15)00427-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fine J, Frank H, Schweinburg F, Jacob S, Gordon T. The bacterial factor in traumatic shock. Ann. N. Y. Acad. Sci. 1952;55:429–445. doi: 10.1111/j.1749-6632.1952.tb26558.x. [DOI] [PubMed] [Google Scholar]
- 7.Cuevas P, De la Maza LM, Gilbert J, Fine J. The lung lesion in four different types of shock in rabbits. Arch. Surg. 1972;104:319–322. doi: 10.1001/archsurg.1972.04180030067015. [DOI] [PubMed] [Google Scholar]
- 8.Souza DG, et al. The essential role of the intestinal microbiota in facilitating acute inflammatory responses. J. Immunol. 2004;173:4137–4146. doi: 10.4049/jimmunol.173.6.4137. [DOI] [PubMed] [Google Scholar]
- 9.Silvestri L, de la Cal MA, van Saene HK. Selective decontamination of the digestive tract: the mechanism of action is control of gut overgrowth. Intensive Care Med. 2012;38:1738–1750. doi: 10.1007/s00134-012-2690-1. [DOI] [PubMed] [Google Scholar]
- 10.Alverdy JC, Laughlin RS, Wu L. Influence of the critically ill state on host-pathogen interactions within the intestine: gut-derived sepsis redefined. Crit. Care Med. 2003;31:598–607. doi: 10.1097/01.CCM.0000045576.55937.67. [DOI] [PubMed] [Google Scholar]
- 11.Deitch EA. Gut-origin sepsis: evolution of a concept. Surgeon. 2012;10:350–356. doi: 10.1016/j.surge.2012.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moore FA, et al. Gut bacterial translocation via the portal vein: a clinical perspective with major torso trauma. J. Trauma. 1991;31:629–636. doi: 10.1097/00005373-199105000-00006. discussion 636-628. [DOI] [PubMed] [Google Scholar]
- 13.Walley KR, Lukacs NW, Standiford TJ, Strieter RM, Kunkel SL. Balance of inflammatory cytokines related to severity and mortality of murine sepsis. Infect. Immun. 1996;64:4733–4738. doi: 10.1128/iai.64.11.4733-4738.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Oksanen JF, et al. vegan: Community Ecology Package. R package version 2.0-4. 2012 [Google Scholar]
- 15.Wang Y, Naumann U, Wright ST, Warton DI. mvabund- an R package for model-based analysis of multivariate abundance data. Methods Ecol. Evol. 2012;3:471–474. [Google Scholar]
- 16.Evans CC, et al. Exercise prevents weight gain and alters the gut microbiota in a mouse model of high fat diet-induced obesity. PLoS One. 2014;9:e92193. doi: 10.1371/journal.pone.0092193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Devkota S, et al. Dietary-fat-induced taurocholic acid promotes pathobiont expansion and colitis in Il10−/− mice. Nature. 2012;487:104–108. doi: 10.1038/nature11225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Musch MW, Wang Y, Claud EC, Chang EB. Lubiprostone decreases mouse colonic inner mucus layer thickness and alters intestinal microbiota. Dig. Dis. Sci. 2013;58:668–677. doi: 10.1007/s10620-012-2509-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Poroyko V, et al. Alterations of lung microbiota in a mouse model of LPS-induced lung injury. Am. J. Physiol. Lung Cell Mol. Physiol. 2015;309:L76–L83. doi: 10.1152/ajplung.00061.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xu J, et al. A genomic view of the human-Bacteroides thetaiotaomicron symbiosis. Science. 2003;299:2074–2076. doi: 10.1126/science.1080029. [DOI] [PubMed] [Google Scholar]
- 21.Kasai C, et al. Comparison of the gut microbiota composition between obese and non-obese individuals in a Japanese population, as analyzed by terminal restriction fragment length polymorphism and next-generation sequencing. BMC Gastroenterol. 2015;15:100. doi: 10.1186/s12876-015-0330-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eckburg PB, et al. Diversity of the human intestinal microbial flora. Science. 2005;308:1635–1638. doi: 10.1126/science.1110591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dickson RP, et al. Changes in the lung microbiome following lung transplantation include the emergence of two distinct Pseudomonas species with distinct clinical associations. PLoS One. 2014;9:e97214. doi: 10.1371/journal.pone.0097214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Osuchowski MF, Welch K, Siddiqui J, Remick DG. Circulating cytokine/inhibitor profiles reshape the understanding of the SIRS/CARS continuum in sepsis and predict mortality. J. Immunol. 2006;177:1967–1974. doi: 10.4049/jimmunol.177.3.1967. [DOI] [PubMed] [Google Scholar]
- 25.Damas P, et al. Tumor necrosis factor and interleukin-1 serum levels during severe sepsis in humans. Crit. Care Med. 1989;17:975–978. doi: 10.1097/00003246-198910000-00001. [DOI] [PubMed] [Google Scholar]
- 26.Suter PM, et al. High bronchoalveolar levels of tumor necrosis factor and its inhibitors, interleukin-1, interferon, and elastase, in patients with adult respiratory distress syndrome after trauma, shock, or sepsis. Am. Rev. Respir. Dis. 1992;145:1016–1022. doi: 10.1164/ajrccm/145.5.1016. [DOI] [PubMed] [Google Scholar]
- 27.Meduri GU, et al. Inflammatory cytokines in the BAL of patients with ARDS. Persistent elevation over time predicts poor outcome. Chest. 1995;108:1303–1314. doi: 10.1378/chest.108.5.1303. [DOI] [PubMed] [Google Scholar]
- 28.Hilty M, et al. Disordered microbial communities in asthmatic airways. PLoS One. 2010;5:e8578. doi: 10.1371/journal.pone.0008578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Huang YJ, et al. Airway microbiota and bronchial hyperresponsiveness in patients with suboptimally controlled asthma. J. Allergy Clin. Immunol. 2011;127:372–381. e371–e373. doi: 10.1016/j.jaci.2010.10.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sze MA, et al. Host response to the lung microbiome in chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 2015;192:438–445. doi: 10.1164/rccm.201502-0223OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang D, et al. Neutrophil ageing is regulated by the microbiome. Nature. 2015 doi: 10.1038/nature15367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rush BF, Jr, et al. Does the bacteremia observed in hemorrhagic shock have clinical significance? A study in germ-free animals. Ann. Surg. 1989;210:342–345. doi: 10.1097/00000658-198909000-00010. discussion 346-347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Doig CJ, et al. Increased intestinal permeability is associated with the development of multiple organ dysfunction syndrome in critically ill ICU patients. Am. J. Respir. Crit. Care Med. 1998;158:444–451. doi: 10.1164/ajrccm.158.2.9710092. [DOI] [PubMed] [Google Scholar]
- 34.Baker JW, Deitch EA, Li M, Berg RD, Specian RD. Hemorrhagic shock induces bacterial translocation from the gut. J. Trauma. 1988;28:896–906. doi: 10.1097/00005373-198807000-00002. [DOI] [PubMed] [Google Scholar]
- 35.O'Boyle CJ, et al. Microbiology of bacterial translocation in humans. Gut. 1998;42:29–35. doi: 10.1136/gut.42.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Harris B, et al. Gut Microbiota Predict Pulmonary Infiltrates After Allogeneic Hematopoietic Cell Transplantation. Am. J. Respir. Crit. Care Med. 2016 doi: 10.1164/rccm.201507-1491OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lemaire LC, et al. Thoracic duct in patients with multiple organ failure: no major route of bacterial translocation. Ann. Surg. 1999;229:128–136. doi: 10.1097/00000658-199901000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Suau A, et al. Direct analysis of genes encoding 16S rRNA from complex communities reveals many novel molecular species within the human gut. Appl. Environ. Microbiol. 1999;65:4799–4807. doi: 10.1128/aem.65.11.4799-4807.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Guo S, Al-Sadi R, Said HM, Ma TY. Lipopolysaccharide causes an increase in intestinal tight junction permeability in vitro and in vivo by inducing enterocyte membrane expression and localization of TLR-4 and CD14. Am. J. Pathol. 2013;182:375–387. doi: 10.1016/j.ajpath.2012.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Adams CA, Jr, Xu DZ, Lu Q, Deitch EA. Factors larger than 100 kd in post-hemorrhagic shock mesenteric lymph are toxic for endothelial cells. Surgery. 2001;129:351–363. doi: 10.1067/msy.2001.111698. [DOI] [PubMed] [Google Scholar]
- 41.Chastre J, et al. Nosocomial pneumonia in patients with acute respiratory distress syndrome. Am. J. Respir. Crit. Care Med. 1998;157:1165–1172. doi: 10.1164/ajrccm.157.4.9708057. [DOI] [PubMed] [Google Scholar]
- 42.Kelly BJ, et al. Composition and dynamics of the respiratory tract microbiome in intubated patients. Microbiome. 2016;4:7. doi: 10.1186/s40168-016-0151-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Arumugam M, et al. Enterotypes of the human gut microbiome. Nature. 2011;473:174–180. doi: 10.1038/nature09944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Morris A, et al. Comparison of the respiratory microbiome in healthy nonsmokers and smokers. Am. J. Respir. Crit. Care Med. 2013;187:1067–1075. doi: 10.1164/rccm.201210-1913OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Segal LN, et al. Enrichment of the lung microbiome with oral taxa is associated with lung inflammation of a Th17 phenotype. Nature Microbiology. 2016;1:16031. doi: 10.1038/nmicrobiol.2016.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Santoro AE, Boehm AB. Frequent occurrence of the human-specific Bacteroides fecal marker at an open coast marine beach: relationship to waves, tides and traditional indicators. Environ. Microbiol. 2007;9:2038–2049. doi: 10.1111/j.1462-2920.2007.01319.x. [DOI] [PubMed] [Google Scholar]
- 47.Calfee CS, et al. Subphenotypes in acute respiratory distress syndrome: latent class analysis of data from two randomised controlled trials. Lancet Respir. Med. 2014;2:611–620. doi: 10.1016/S2213-2600(14)70097-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zaborin A, et al. Membership and behavior of ultra-low-diversity pathogen communities present in the gut of humans during prolonged critical illness. mBio. 2014;5:e01361–e01314. doi: 10.1128/mBio.01361-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dickson RP, Martinez FJ, Huffnagle GB. The role of the microbiome in exacerbations of chronic lung diseases. Lancet. 2014;384:691–702. doi: 10.1016/S0140-6736(14)61136-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dickson RP, Erb-Downward JR, Huffnagle GB. Homeostasis and its disruption in the lung microbiome. Am. J. Physiol. Lung Cell Mol. Physiol. 2015;309:L1047–L1055. doi: 10.1152/ajplung.00279.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Steinhauser ML, et al. IL-10 is a major mediator of sepsis-induced impairment in lung antibacterial host defense. J. Immunol. 1999;162:392–399. [PubMed] [Google Scholar]
- 52.Paine R, 3rd, et al. A randomized trial of recombinant human granulocyte-macrophage colony stimulating factor for patients with acute lung injury. Crit. Care Med. 2012;40:90–97. doi: 10.1097/CCM.0b013e31822d7bf0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bernard GR, et al. The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am. J. Respir. Crit. Care Med. 1994;149:818–824. doi: 10.1164/ajrccm.149.3.7509706. [DOI] [PubMed] [Google Scholar]
- 54.Dickson RP, et al. Cell-associated bacteria in the human lung microbiome. Microbiome. 2014;2:28. doi: 10.1186/2049-2618-2-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mason KL, et al. Candida albicans and bacterial microbiota interactions in the cecum during recolonization following broad-spectrum antibiotic therapy. Infect. Immun. 2012;80:3371–3380. doi: 10.1128/IAI.00449-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Caporaso JG, et al. Global patterns of 16S rRNA diversity at a depth of millions of sequences per sample. Proc. Natl. Acad. Sci. U.S.A. 2011;108(Suppl 1):4516–4522. doi: 10.1073/pnas.1000080107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kozich JJ, Westcott SL, Baxter NT, Highlander SK, Schloss PD. Development of a dual-index sequencing strategy and curation pipeline for analyzing amplicon sequence data on the MiSeq Illumina sequencing platform. Appl. Environ. Microbiol. 2013;79:5112–5120. doi: 10.1128/AEM.01043-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Schloss PD. 454 SOP - mothur. 2015 [Google Scholar]
- 59.Jumpstart Consortium Human Microbiome Project Data Generation Working Group. Human Microbiome Consortium 16S 454 Sequencing Protocol. 2010 [Google Scholar]
- 60.Daigle D, Simen BB, Pochart P. High-throughput sequencing of PCR products tagged with universal primers using 454 life sciences systems. Chapter 7, Unit7 5. Curr. Protoc. Mol. Biol. 2011 doi: 10.1002/0471142727.mb0705s96. [DOI] [PubMed] [Google Scholar]
- 61.Schloss PD. MiSeq SOP - mothur. 2015 [Google Scholar]
- 62.Schloss PD, et al. Introducing mothur: open-source, platform-independent, community-supported software for describing and comparing microbial communities. Appl. Environ. Microbiol. 2009;75:7537–7541. doi: 10.1128/AEM.01541-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2013. [Google Scholar]
- 64.Legendre P, Gallagher ED. Ecologically meaningful transformations for ordination of species data. Oecologia. 129:271–280. doi: 10.1007/s004420100716. [DOI] [PubMed] [Google Scholar]
- 65.Salter SJ, et al. Reagent and laboratory contamination can critically impact sequence-based microbiome analyses. BMC Biol. 2014;12:87. doi: 10.1186/s12915-014-0087-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.