Abstract
The Children's Cancer Survivorship Study reports more chronic illnesses in sarcoma survivors than other pediatric cancers. Chemotherapy and radiation put survivors at risk for developing chronic illnesses, including heart disease, diabetes, hypertension, and kidney failure. Sarcoma survivors may have a reduced life expectancy and signs of heart disease in their 30s and 40s. Since these medical problems occur much later in the general population, they often go undetected or misdiagnosed in sarcoma survivors, creating delays in intervention and treatment. The good news is that these chronic illnesses can often be prevented or minimized. The most common adverse effect of chemotherapy and radiation is coronary artery disease (CAD). CAD has a number of risk factors, including hypertension, diabetes, obesity, and dyslipidemia. These risk factors are modifiable with lifestyle changes, including diet and exercise, and/or pharmacological intervention. By identifying and managing risk factors like hypertension early, we in turn reduce the risk for CAD and prolong survival. This is well established in the general population; there is no reason a priori not to apply it to sarcoma survivors. Sarcoma survivors should be followed by physicians who understand the late effects and outcomes of sarcoma treatment. The University of Michigan Sarcoma Survivorship Clinic provides long-term care for sarcoma survivors by preventing, diagnosing, and treating the adverse long-term physical and psychological effects associated with sarcoma survivorship.
Sarcoma Survivors: A Unique At-Risk Population
Bone and soft tissue sarcomas are rare cancers, but represent a significant proportion of cancers diagnosed in adolescents and young adults. The majority of patients diagnosed with sarcoma will be cured of their disease and live cancer free. Diagnosed as children, adolescents, or adults, sarcoma survivors are at a great risk of developing a severe or life-threatening chronic medical condition1,2 related to their sarcoma treatment as they age. Survivors face issues specific to their surgeries, radiation treatment, systemic chemotherapy, and psychosocial issues that can have a major impact on long-term health.
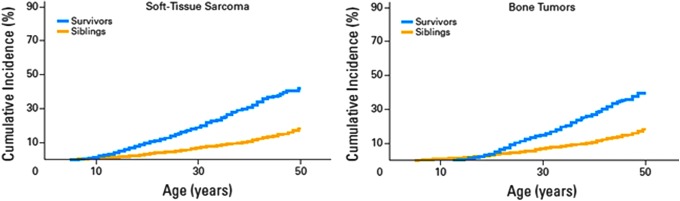
The Children's Cancer Survivorship Study3 Report reveals rates of severe chronic illnesses in sarcoma survivors much higher than those found in other pediatric cancers. Sarcoma survivors, despite being cured, may have a reduced life expectancy and sometimes show signs in their 30s and 40s of heart disease seen in older adults. Acquired heart disease in a 30-year-old is rare; heart disease in a 30-year-old sarcoma survivor is not. In fact, heart disease is the main issue facing sarcoma survivors.4 Doxorubicin is the most common chemotherapy given to sarcoma patients that causes cardiac toxicity, much of which is irreversible. The progression to heart failure may be prevented with early intervention if screened for early. Other potential conditions include type 2 diabetes, high blood pressure, lipid disorders, kidney failure, anxiety, depression and other mental health problems, sarcoma recurrence, and new secondary cancer(s).3 These illnesses can occur as soon as 2 years after completing sarcoma treatment (Fig. 1).
FIG. 1.
Cumulative incidence of severe, disabling, life-threatening, or fatal chronic health conditions among 2124 sarcoma survivors diagnosed in 1970–1986.3,8
Since these medical problems occur much later in the general population, they often go undetected or misdiagnosed in sarcoma survivors,5 creating delays in intervention and treatment. The good news is that these chronic illnesses can often be prevented or minimized. The most common adverse effect of chemotherapy and radiation is coronary artery disease (CAD). CAD has a number of risk factors, including hypertension, diabetes, obesity, and dyslipidemia. These risk factors are modifiable with lifestyle changes, including diet and exercise, and/or pharmacological intervention. By identifying and managing risk factors like hypertension early, we in turn reduce the risk for CAD and prolong survival. This is well established in the general population; there is no reason a priori not to apply it to sarcoma survivors (Fig. 2).
FIG. 2.
Cardiovascular risk factors and major cardiac events.4
The Institute of Medicine and the American Society of Clinical Oncology (ASCO)'s shared care model6 for breast cancer, prostate cancer, and colon cancer survivors between the medical oncologist and the primary care physician are unlikely to meet the needs of a sarcoma survivor. In January 2014, the Annals of Internal Medicine7 reported that on average, internists were “somewhat uncomfortable” caring for survivors of Hodgkin lymphoma, acute lymphoblastic leukemia, and osteosarcoma. Sarcoma survivors are best followed by physicians familiar with the chronic effects of sarcoma treatment especially systemic therapies as well as the local/regional therapies of surgery and radiation therapy.
The University of Michigan Sarcoma Survivorship Clinic
Medical oncologist, Laurence H. Baker, DO has been treating sarcoma patients for more than 40 years and believes that sarcoma survivors should be appropriately followed by physicians who understand the late effects and outcomes of cancer treatment for sarcoma as well as the potential complications to look for in the future. In October 2014, he created the University of Michigan Sarcoma Survivorship Clinic.
The Clinic offers proactive lifelong care, including systematic planning for cancer prevention and patient-centered surveillance based on the survivor's personal risk, cancer therapy, genetic predispositions, lifestyle behaviors, and other comorbid health conditions. Regardless of where a patient was treated or lives in the country, the clinic is open to sarcoma survivors 16 years and older who have been off therapy for at least 2 years and to patients who are transitioning from pediatric to adult medical care. Survivor patients may self-refer or physicians may refer patients to the Sarcoma Survivorship Clinic.
Sarcoma survivors are unique individuals whose needs range from those with few long-term effects from their treatment to patients with chronic conditions or significant treatment-related health issues. Providing survivorship care requires a variety of approaches to meet their needs. All survivors require education regarding their individual health risks and screening needs. The Sarcoma Survivorship Clinic focuses on the survivor's total well-being, creating strategies to best manage any healthcare issues that may arise.
We provide a comprehensive health exam and determine a patient's risk of developing chronic illnesses based on their treatment and medical history. There is a strong focus on cardiovascular chronic illness. Signs of congestive heart failure are observed and screened with echocardiography. Patients who received Doxorubicin are screened annually for cardiomyopathy with an echocardiogram with strain. Preventive measures are available for those patients who received radiation to the chest. This includes cholesterol lowering and assessing obesity with functional status. We apply well-established criteria for cancer screening prospectively. Survivors are followed for skeletal-muscular dysfunction, metabolic syndrome, diabetes, hypertension, cardiac diseases, anxiety, depression, renal insufficiency (for more careful inspection of drug toxicity), and obesity. Visits typically include laboratory blood and urine tests, a 6-minute hall walk (to assess physical function), as well as a meeting with a dietician to assist with weight management.
Patients complete risk assessment questions for us to learn their perception of risk of their sarcoma returning, the possibility of a secondary cancer, and the possibility of developing chronic health condition(s) related to their sarcoma treatment. This assessment informs us how best to tailor the educational component of the appointment to teach the patient about their individual risks based on their prior treatment and medical and family history. Patients are also evaluated with questions from the National Institutes of Health's (NIH) Patient-Reported Outcome Measurement Information System (PROMIS), a system of highly reliable, precise measures of patient-reported health status. Our patients complete the PROMIS questionnaires on Anxiety, Depression, Mobility, Pain Interference, Sleep Disturbance, and Physical Function before their first clinic visit and then every 6 months thereafter. If the patient already has an early diagnosis of a chronic medical disease, we will consult and work closely with the appropriate specialist to formulate the best treatment plan. Based on the clinic visit, we may refer patients to a specialist on our team, which includes onco-cardiology, nephrology, pulmonary medicine, orthopedic surgery, radiation oncology, psychiatry, physical medicine and rehabilitation (PM&R), endocrinology, gynecology, and internal medicine. In addition to our individualized educational component, patients receive a Sarcoma Survivorship Care Plan to empower them with the knowledge of their treatment history, personalized risk assessment, monitoring recommendations, referrals to specialists, and recommendations for health-protective behaviors. For continuity of care, these plans are also shared with the patient's physicians. The patient's survivorship plan reflects the regular patient assessments to address the survivor's changing needs over time.
Unless presenting chronic or severe life-threatening issues, patients are seen annually and undergo a series of examinations to monitor for chronic illnesses and measure performance such as physical strength and cognitive function. The Program's regular clinic visits and the patient questionnaires will allow us to monitor and recognize potential physical and mental conditions over time. This regular contact will also allow us to diagnose and treat any conditions earlier, and with better outcomes.
The Long-Term Impact of Sarcoma Treatment
Our Sarcoma Survivorship Program database captures data on specific cancer(s), treatment regimen(s), chronic illness history, family health history, laboratory data, as well as the prospective data: the long-term and late physical and psychological effects of cancer and its treatment and any comorbid medical conditions. The Sarcoma Survivorship Program database was created to teach us about the potential of early recognition and intervention, and confirm that earlier identification improves long-term function, reduces debilitating symptoms, and potentially reduces mortality (Table 1). Without appropriate awareness of late effects by patients and/or providers, symptoms may be discounted and/or attributed to other causes, leading to misinformed evaluation and possibly delayed and/or inappropriate treatment. It is critical that we improve our knowledge of the long-term impact of cancer therapy to effectively counsel survivors and offer effective intervention strategies to prevent or minimize the impact of adverse late effects.
Table 1.
Data for the First 30-Patient Cohort
| Patient reported | Sarcoma survivorship clinic | ||||
|---|---|---|---|---|---|
| Patients (n) | Patients (n) | ||||
| Received a survivorship plan when completed sarcoma treatment | 13% (4) | Age at diagnosis Range (8–61) | Before age 30 | 53% (16) | |
| Family history of cancer | First degree relative | 30% (9) | Mean | 32 years | |
| More than one | Median | 35 years | |||
| first degree relative | 23% (7) | ||||
| Second degree relative | 63% (19) | Mode | 19 years 17% (5) | ||
| Patient-reported diagnosis or treatment for | Second cancer (in addition to sarcoma) | 20% (6) | New findings | Hypertension | 33% (10) |
| Cardiomyopathy | 7% (2) | ||||
| Hypertension | 17% (5) | At risk of developing cardiac disease secondary to chemotherapy | 20% (6) | ||
| Cardiac issues (congestive heart failure and coronary artery disease) | 10% (3) | Diabetes | 3% (1) | ||
| Anxiety | 30% (9) | Hyperlipidemia | 20% (6) | ||
| Depression | 23% (7) | Renal insufficiency | 10% (3) | ||
| Osteopenia/osteoporosis | 20% (6) | Thyroid dysfunction | 10% (3) | ||
| Renal function issues/kidney disease | 3% (1) | Osteoporosis | 10% (3) | ||
| Concerns about fertility | 23% (7) | Osteoarthritis | 3% (1) | ||
| Concerns about sleep quality | 17% (5) | Thoracic aneurism | 3% (1) | ||
| Sinus tachycardia | 3% (1) | ||||
| Hearing loss | 7% (2) | ||||
| Fear | 27% (8) | ||||
| Depression | 13% (4) | ||||
| Recommendations | Recommended regular cancer screening | 20% (6) | |||
| Recommended weight loss | 50% (15) | ||||
| Recommended exercise | 50% (15) | ||||
Since opening the Survivorship Clinic in October 2014, our patients have confirmed they are deficient in health-related knowledge and are not engaged in consensus health promotion and screening practices that could improve their long-term outcomes. In fact, when asked questions such as “to what degree of certainty do you think you are cured of your sarcoma?” and “because of your sarcoma treatment, to what extent do you think that you are at risk of developing significant heart disease, hypertension, kidney failure, anxiety, depression and other mental health problems, the sarcoma returning, or developing a new cancer?,” only 40% were knowledgeable about some of the adverse effects. This may be because only 13% received a Survivorship Plan when they completed their treatment or the failure of the treating oncologist to discuss their risks.3 Our research addresses the specific gaps in knowledge such as the incidence of and risk factors for late and long-term effects of sarcoma and its treatment. Now that we have started seeing our patients again for their annual visit, we will be able to monitor adverse effects over time.
The purpose of the Sarcoma Survivorship Program is to provide patients with strategies to optimize their overall health and wellness, now and in the future. The program aims to provide excellent clinical care to patients while fostering clinical research that will lead to further advances in care for sarcoma survivors to prevent morbidity/lethality of chronic medical conditions and to improve the quality of life in sarcoma survivors of all ages. We are pursuing research to develop more effective strategies that can be developed to precisely identify sarcoma survivors at greatest risk for specific outcomes.
University of Michigan Sarcoma Survivorship Program: www.mcancer.org/sarcoma-survivorship
University of Michigan Sarcoma Survivorship Clinic: www.mcancer.org/sarcoma-survivorship/sarcoma-survivorship-clinic
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Nagarajan R, Kamruzzaman A, Ness KK, et al. Twenty years of follow-up of survivors of childhood osteosarcoma. Cancer. 2011;117(3):625–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ginsberg JP, Goodman P, Leisenring W, et al. Long-term survivors of childhood Ewing sarcoma: report from the childhood cancer survivor study. J Natl Cancer Inst. 2010;102(16):1272–83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Oeffinger KC, Mertens AC, Sklar CA, et al. Chronic health conditions in adult survivors of childhood cancer. N Engl J Med. 2006;355(15):1572–82 [DOI] [PubMed] [Google Scholar]
- 4.Armstrong GT, Oeffinger KC, Chen Y, et al. Modifiable risk factors and major cardiac events among adult survivors of childhood cancer. J Clin Oncol. 2013;31(29):3673–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Henderson TO, Rajaraman P, Stovall M, et al. Risk factors associated with secondary sarcomas in childhood cancer survivors: a report from the childhood cancer survivor study. Int J Radiat Oncol Biol Phys. 2012;84(1):224–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ganz PA, Kwan L, Some rfield MR, et al. The role of prevention in oncology practice: results from a 2004 survey of American Society of Clinical Oncology members. J Clin Oncol. 2006;24(18):2948–57 [DOI] [PubMed] [Google Scholar]
- 7.Suh E, Daugherty CK, Wroblewski K, et al. General internists' preferences and knowledge about the care of adult survivors of childhood cancer: a cross-sectional survey. Ann Intern Med. 2014;160(1):11–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Armstrong GT, Kawashima T, Leisenring W, et al. Aging and risk of severe, disabling, life-threatening, and fatal events in the childhood cancer survivor study. J Clin Oncol. 2014;32(12):1218–27 [DOI] [PMC free article] [PubMed] [Google Scholar]