Abstract
Purpose:
The purpose of this study was to present the outcome and discuss the feasibility of rib composite flap with intercostal nerve and internal thoracic vessels for reconstructing mandibular defect.
Methods:
Rib composite flaps have been used in 82 patients for reconstructing benign tumor-caused large mandibular defects: 66 of the 82 patients were reconstructed using rib composite flap with intercostal nerve and internal thoracic vessels, whereas the other 16 patients were reconstructed using rib composite flap with internal thoracic vessels, without intercostal nerve. After operation, clinical observation, imageological examination, and sensory detection were used to evaluate the effect of reconstruction.
Results:
All rib composite flaps with intercostal nerve and internal thoracic vessels were successfully harvested and transplanted. Both immediate and long-term examination showed good appearance reconstruction. All followed-up patients conveyed good satisfaction degree with function and appearance reconstruction. Postoperative panoramic x-ray examination showed new bone formation between the transplanted rib and mandibular stump. Good recoveries of mandibular nerve sensory were observed when followed up after reconstruction surgery.
Conclusions:
Rib composite flap with intercostal nerve and internal thoracic vessels could be a promising method for reconstruction of mandibular defects.
Keywords: Internal thoracic artery, Mandible defect, nerve anastomosis, reconstruction, rib composite flap
Mandible is the only movable craniofacial bone and very important to facial aesthetics and masticatory function. Mandibular defects can be caused by traumas, dysplastic pathologies, atrophy, osteoradionecrosis, and benign or malignant neoplasm.1 Considering the esthetic and functional importance of the mandible, its reconstruction is a major objective in the treatment of mandibular bone defects.2 The reconstruction should provide both functional and cosmetic rehabilitation,3 whereas, how to get an ideal reconstruction of aesthetics, masticatory function and sensation has still been one of the most common surgical challenges for reconstructive surgeons.4
Multiple modalities have been used for mandibular reconstruction including reconstruction plates,5 nonvascularized bone graft,6,7 distraction osteogenesis,8 vascularized bone graft,9,10 and free vascularized bone flap.9,11 Nowadays, because of the the computer-assisted surgery technique, accurate mandibular reconstruction has been available.9,10 The vascularized fibula bone flap and iliac flap with vascular pedicle are generally accepted as the mainstay of large mandibular defects reconstruction. However, the optimal reconstruction of mandibular defects is still debated. Other reconstructive options are also done for mandibular reconstruction with good results.
The inferior alveolar nerve and mental nerve are important for the most basic functions in a human life, that is, feeling of lower lip, eating, and swallowing. Adequate nerve reconstruction is equally important for mandibular reconstruction. Cosmetic restoration should not be the only standard for evaluating mandibular reconstruction, but also the function and sensory of the recipient area must be taken into account.
In fact, the superiority of the vascularized rib graft over the nonvascularized rib graft has been well established in mandibular reconstruction.12 Based on anatomic dissections of vessels and nerves of the internal thoracic system, we developed a new reconstructive approach for mandibular defect—rib composite flap with internal thoracic vessels and intercostal nerve (RVN composite flap). Ten years of clinical studies in our hospital revealed several advantages of RVN flap: easy to master the operation; donor site not exposed; thin skin of the flap suitable for repairing oral mucosa to get a good cosmetic restoration; adequate blood supply of the flap for survival; good functional and sensory restoration, indicating that the RVN flap could be considered as a promising donor for the reconstruction of oral mandibular defects. In this study, we presented the method and also discussed the outcomes and feasibility of this composite flap for reconstructing mandibular defect.
MATERIALS AND METHODS
Clinical Data
This work has been approved by the ethical committees of Liaocheng people's hospital. And we also got the approval of all the patients. Eight-two patients (male 53, female 29), from 22 to 55 years old, with mandibular defect up to 11 cm with body and lift branch (60 patients) or angle (22 patients) involvement were included in this study. The 5th rib was selected as the donor bone for reconstructing the mandibular defect. Sixty-eight of the defects were reconstructed by grafting the 5th rib composite tissue flap with the internal thoracic artery and vein, and 14 by grafting the 5th rib with internal thoracic artery and vein. Sixty-six of the 82 patients were reconstructed with rib composite flap or rib with internal thoracic vessels and intercostal nerve (RVN composite flap), whereas the other 16 were reconstructed with rib composite flap or rib with internal thoracic vessels, without intercostal nerve (RV composite flap). Facial artery and vein (71 patients), thyroid artery and vein (8 patients), or superficial temporal artery and vein (3 patients) were selected for anastomosing rib flap vessels. After operation, clinical observation, imageological examination, and sensory detection were used to evaluate the effects of reconstruction.
Surgical Methods
The RVN composite flap was designed according to the defect size of mandibular and adjacent soft tissue. Briefly, skin and soft tissue of the RVN composite flap was harvested according to the blood supply of the rib region with a size 10% larger than the recipient area and with a width not covering the 4th and 6th rib; the size of rib was harvested as the defect size of mandibular. Figure 1A shows the incision design of the RVN composite flap. The largest RVN composite flap in our study was up to 11 cm × 6 cm, and the smallest one was 8 cm × 6 cm.
FIGURE 1.
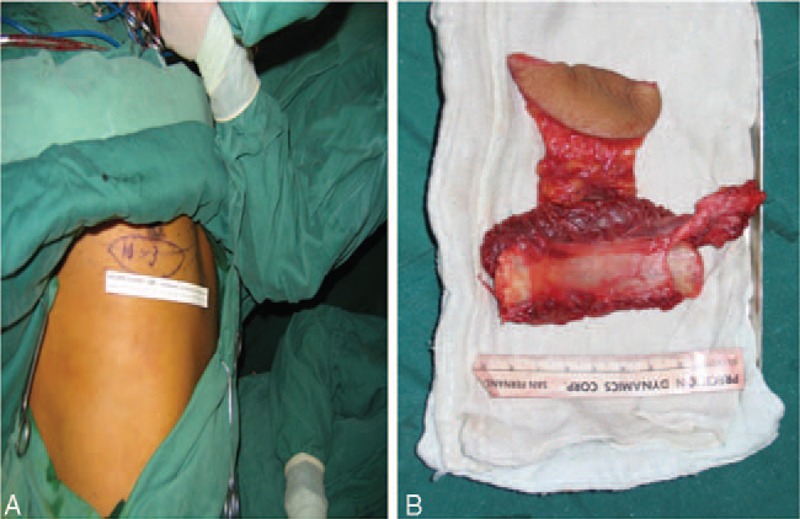
The rib composite flap was designed according to the mandibular defect and blood supply of the rib region. A, The flap was outlined. B, Prepared flap.
According to the designed incision, the skin and subcutaneous tissue was incised and separated from fascia layer, and the 5th rib was correspondingly fully exposed. After the perichondrium was incised, a segment of the 5th costicartilage was removed, and then internal thoracic vessels together with the anterior intercostal branches to the adjacent 5th rib were exposed. The internal thoracic vessels were separated from pleura. The rib was transected, and the free composite graft was removed from the underlying parietal pleura by blunt dissection. Then the intercostales interni and externi muscle were cut off. When the recipient area was prepared, the intercostal nerve and internal thoracic artery and vein were incised. The proximal end of the nerve and vessels were ligatured while the distal nerve and vessels attached to the flap were kept free. Active bleeding of bone marrow cavity and intercostal muscles indicated a good blood supply. Figure 1B shows the prepared flap.
The free margins of the 2 remnants of the mandibular rami were dissected free. The left facial, thyroid or superficial temporal artery, and vein were dissected, isolated, and transected for anastomosing to the vessel of the RVN flap. The inferior alveolar nerve and mental nerve were also dissected free and prepared for anastomosing to the nerve of the RVN flap. After shaping the rib according to the outline of the defected mandible, the rib composite flap was put in and fixed to the mandibular defect site. Under operating microscope, vascular anastomosis and nerve anastomosis were performed.
Outcome Assessment
Flap evaluating: flap color, temperature, texture and capillary refilling were used to evaluate condition of the flap. Good flap must be with color similar to the donor site, with temperature difference between flap and adjacent tissue less than 2°C, with slight swelling but subside about 3 days after surgery, and with capillary refilling time about 1 to 2 seconds.
Imageological examination: postoperative panoramic x-ray examinations were detected 7 to 10 days and 3 months after operation to evaluate the bone union and osteogenesis. Seven to ten days after operation, emission computed tomography was performed to detect the blood supply as described previously.13 Briefly, the radionuclides were extracted from 99mTc generators (Mon-Tek, Eczaciba i/Monrol), and MDP (Mon. MDP, Eczaciba i, Monrol) was labeled and characterized according to the manufacturer's recommendations. Three to four hours after the injection of 740 MBq (20 mCi) of 99m Tc MDP, images of uptake in grafted rib were acquired.
Sensory testing: to evaluate the restoration of the grafted nerve, the sensory of lower lip was examined using the Neurometer current perception threshold/unmyelinated (CPT/C). The Neurometer CPT/C produces constant-current sine wave stimulation at 2000, 250, and 5 Hz with corresponding depolarization periods of 0.25, 2, and 100 ms, respectively. Large myelinated A (Aβ), small myelinated A (Aδ), and unmyelinated C (C) nerve fibers are evaluated with a series of 2000-, 250-, and 5-Hz electrical stimuli, respectively.14,15 Sensory testing in our study referred to a previous study on intercostal nerve damage after video-assisted thoracic surgery.16 Briefly, a pair of gold-plated surface electrodes was placed just on the lower lip. At each frequency (2000, 250, and 5 Hz), the current was slowly increased until the subject reported sensation. The stimulus was then turned off, the intensity was decreased by 0.1 mA, and the stimulus was turned back on. This procedure was repeated until a range of 0.1 mA was established at which level the patient reported feeling the high intensity but could not detect the lower intensity. Using a double-blind methodology, in an isolated room, the patient was then presented with 6 to 20 cycles of randomly selected real and false stimuli above and below the perception threshold level until the exact CPT value could be determined within a 0.02 mA range.
Statistical Analysis
Statistical analysis was calculated using chi-square test and paired t test by SPSS10.0 software. P values ≤0.05 were considered as statistically significant.
RESULTS
All the flaps survived without infection or necrosis, although vascular crisis emerged in 1 patient with diabetes but was immediately treated and rescued. The donor sites healed without any sequelae after operation, although 2 patients have once suffered pleural tear which was recovered after immediately treatment. Figure 2A and B showed that there was no significant change of facial appearance 7 months after operation compared with preoperation. All patients receiving nerve anastomosis got good sensory recovery.
FIGURE 2.
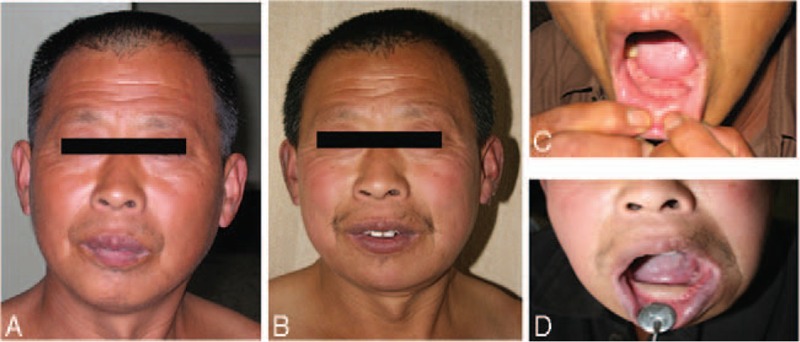
A, Frontal view of a patient before operation. B, Frontal view of a patient before operation. C, Intraoral view of the lesion area. D, Intraoral view of the flap.
Seven to ten days after graft, emission computed tomography radionuclide imaging was performed. The grafted rib showed a high uptake of radioactive substance, indicating adequate blood supply and survival of the rib flap (Fig. 3). Six months after graft, panoramic radiographs showed alignment between the rib and the mandibular stump (Fig. 4), suggesting a good heeling between grafted rib and mandible.
FIGURE 3.
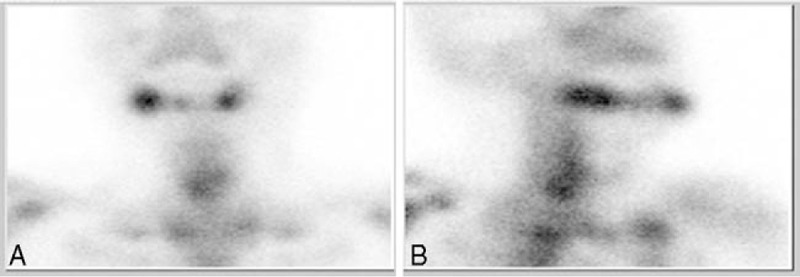
Seven to ten days after operation. Emission computed tomography image: increased uptake at the grafted rib (A, frontal view; B, lateral view).
FIGURE 4.
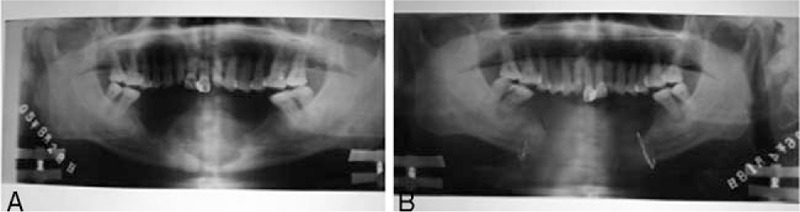
Panoramic radiographs image. A, Image of the lesion area. B, Good alignment between the rib and the mandibular stump 6 months after operation.
After operation, mandibular midline shift occurred in 2 patients, nevertheless, by wearing inclined bite plane and functional exercise the occlusal relationship gradually restored.
Following mandibular reconstruction, 60 of the 66 patients received sensory reconstruction of lower lip, including touch, algesthesia, temperature, and two-point discrimination; however, none of the 16 patients received mandibular reconstruction with non-nervalized rib composite flap got sensory restoration of lower lip (Table 1).
TABLE 1.
Lower Lip (At Least 3/4 Area) Restored Sensory Function
| Feeling Restoration | No Feeling Restoration | P | |
| With nerve anastomoses | 60 | 6 | |
| Without nerve anastomoses | 0 | 16 | <0.001* |
*Significantly different by the Fisher exact test.
Neurometer CPT/C test was performed to test the sensory recovery of the lower lip. When stimulated with 5 Hz current, the affected side sensory threshold of the patients with RVN flaps were nearly paralleled to that of the unaffected side, whereas the affected side of the patients with RV flaps showed a much higher sensory threshold than that of the unaffected side (Fig. 5A), indicating that RVN composite flap could result a good sensory recovery of unmyelinated C (C) fibers. Similar results were shown when detected with 250 Hz and 2000 Hz current (Fig. 5B and C), indicating that RVN composite flap could result a good sensory recovery Aδ and Aβ nerve fibrosis.
FIGURE 5.
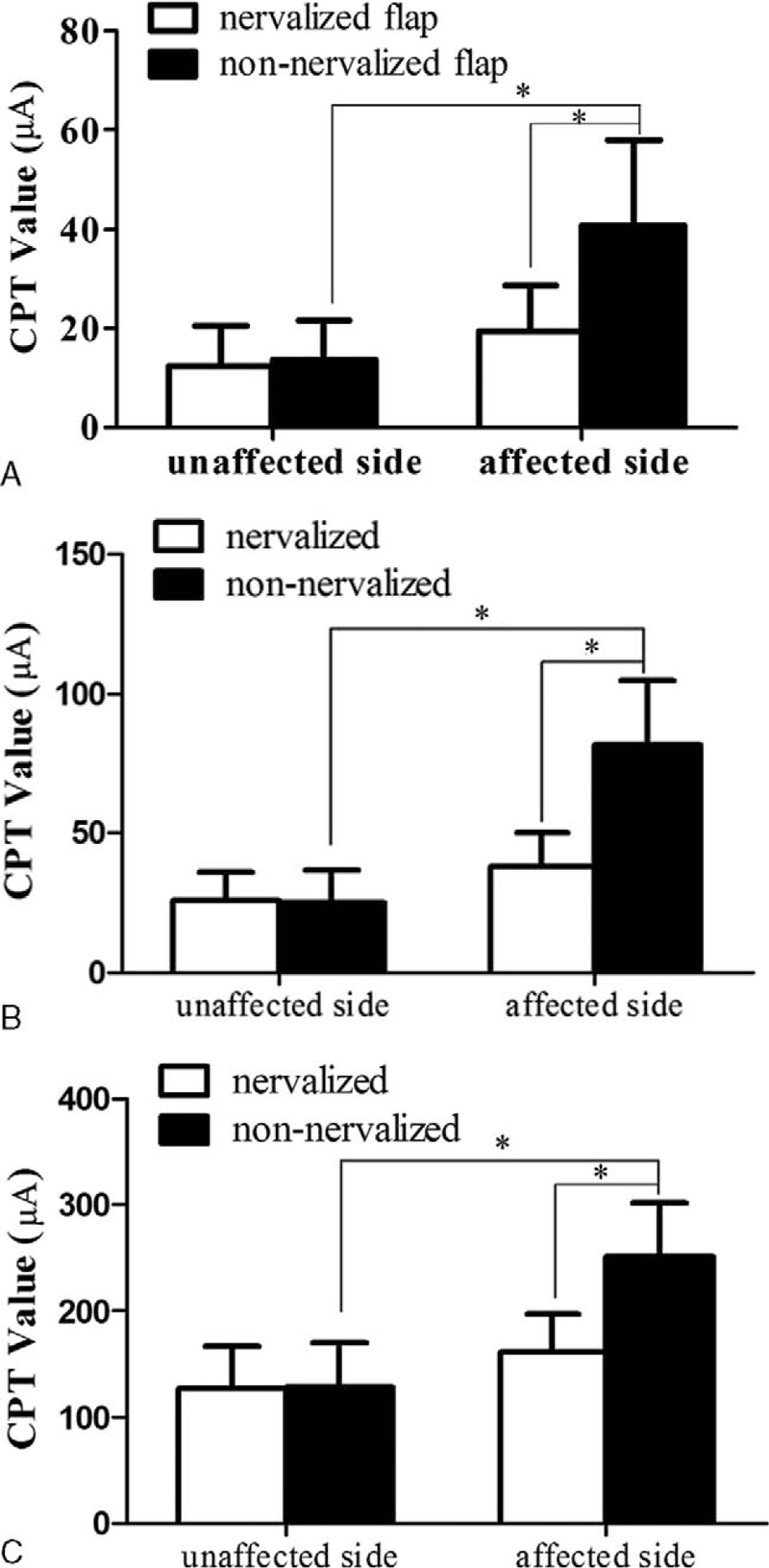
Threshold of sensory detected by Neurometer CPT/C test. A, Threshold of sensory was detected under a current frequency of 5 Hz to evaluate the recovery of unmyelinated C (C) fibers. B, Threshold of sensory was detected under a current frequency of 250 Hz to evaluate the recovery of small myelinated A (Aδ) fibers. C, Threshold of sensory was detected under a current frequency of 2000 Hz to evaluate the recovery of large myelinated A (Aβ) fibers. (∗P < 0.05). CPT/C, current perception threshold/unmyelinated.
DISCUSSION
In 2012 and 2013, different methods of mandible reconstruction were used, including nonvascularized bone grafts,6,7 pedicle flaps,9,10 and titanium reconstruction plates,5 distraction osteogenesis,8 but the gold standard for reconstruction of the mandible is the free osteocutaneous flap.17 The fibula osteocutaneous free flap is the most common approach to mandibular reconstruction, but other osteocutaneous flaps are still widely used for some advantage. In our study, we demonstrate that rib composite flaps with internal thoracic vessels and nerve (RVN composite flaps) could be considered as a promising donor for the reconstruction of mandibular defects, considering several advantages of the RVN composite flap for maxillofacial reconstruction: easy to master the operation, donor site not exposed, thin skin of the flap suitable for repairing oral mucosa to get a good cosmetic restoration, adequate blood supply of the flap for survive, and good functional and sensory restoration.
The anatomic characteristics of the intercostal vessels and intercostal nerve make the operation easy to master. The anatomic position of the intercostal artery supplying the rib flap is generally constant. Intercostal artery supplying the 5th rib and flap is originated from the internal thoracic vessel. The diameter of intercostal artery is about 2.1 mm, although smaller than that of fibular artery supplying fibular flap but still enough for vessel anastomosis and blood circulation reconstruction. The diameter of intercostal nerve is about 1.2 mm, making the nerve anastomosis an easy job.
The rib composite flap showed a high survival rate. In our study, all the grafted ribs were survived. We speculated that this higher survival rate of rib flaps may partially be due to the adequate blood supply. The periosteal blood supply from the internal thoracic artery would be sufficient to support the bone and overlying skin.18 There are a plenty of nutrient foramens in the surface of ribs, ensuring adequate blood supply from periosteal to the rib flaps.19 Our speculation agreed well with Bhathena18 who reported that survival of the anterior rib segment grafts based on internal thoracic artery depends on the periosteal blood supply, and that the periosteal circulation alone can provide adequate nutrition for bone viability and bone healing.
The RVN composite flap made a satisfactory recovery of the lower lip sensory. In our study, the inferior alveolar nerve and mental nerve were also dissected free and anastomosed with the intercostal nerve. The nerve anastomosis led to an excellent recovery of lower lip sensory. In fact, the notion of nerve restoration in the same period with mandibular reconstruction has already been put forward and sural nerve has been clinically used composite with fibular flap.20 The distribution of cutaneous branch of intercostal nerves is segmental and overlapping, and 1 nerve dysfunction could be compensated by its adjacent nerves, therefore the RVN flap will not result in sensory loss of the donor site. Moreover, the diameter of intercostal nerve is enough for end-to-end anastomosis. As the above advantage, intercostal nerve has already been widely used in reconstruction of nerves.21,22
Although the RVN flap could be suitable for functional and aesthetic reconstruction of mandible, there are still some drawbacks. First, as to the limited length of rib, it is difficult to harvest enough rib bone for large defect of mandible. Fibular could provide bone length up to 25 cm, which is adequate for large defect, even full-length defect of mandible. Although for rib, the largest bone length used in our study is about 11 cm. But for defects not so large, rib flap may be an available choice. Second, compared with fibular and ilium flap, the cortical of rib is thinner and more fragile, making it less suitable for teeth implantation.
Despite some drawbacks, the RVN flap possesses several unique advantages, leading it a promising choice for mandibular reconstruction.
Footnotes
B.Z., K-Y.L., and L-C.J. contributed equally to this work.
This study is supported by Projects of medical and health technology development program in Shandong province (No. 2013WS0085), the Foundation for Outstanding Young Scientist in Shandong Province (No. BS2014YY054), and the National Natural Science Foundation of China funded project (No. 81272958 and No. 81472530).
The authors report no conflicts of interest.
REFERENCES
- 1.Torroni A, Marianetti TM, Romandini M, et al. Mandibular reconstruction with different techniques. J Craniofac Surg 2015; 26:885–890. [DOI] [PubMed] [Google Scholar]
- 2.Omeje K, Efunkoya A, Amole I, et al. A two-year audit of non-vascularized iliac crest bone graft for mandibular reconstruction: technique, experience and challenges. J Korean Assoc Oral Maxillofac Surg 2014; 40:272–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goh BT, Lee S, Tideman H, et al. Mandibular reconstruction in adults: a review. Int J Oral Maxillofac Surg 2008; 37:597–605. [DOI] [PubMed] [Google Scholar]
- 4.Pirgousis P, Eberle N, Fernandes R. Reoperative mandibular reconstruction. Oral Maxillofac Surg Clin North Am 2011; 23:153–160. [DOI] [PubMed] [Google Scholar]
- 5.Wilde F, Hanken H, Probst F, et al. Multicenter study on the use of patient-specific CAD/CAM reconstruction plates for mandibular reconstruction. Int J Comput Assist Radiol Surg 2015; 10:2035–2051. [DOI] [PubMed] [Google Scholar]
- 6.Mensink G, Verweij JP, Gooris PJ, et al. Bilateral sagittal split osteotomy in a mandible previously reconstructed with a non-vascularized bone graft. Int J Oral Maxillofac Surg 2013; 42:830–834. [DOI] [PubMed] [Google Scholar]
- 7.Agrawal A, Mehrotra D, Mohammad S, et al. Randomized control trial of non-vascularized fibular and iliac crest graft for mandibular reconstruction. J Oral Biol Craniofac Res 2012; 2:90–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang X, Lin Y, Yi B, et al. Distraction osteogenesis in functional reconstruction of mandible—report of 6 cases. Chin J Dent Res 2000; 3:16–25. [PubMed] [Google Scholar]
- 9.Modabber A, Mohlhenrich SC, Ayoub N, et al. Computer-aided mandibular reconstruction with vascularized iliac crest bone flap and simultaneous implant surgery. J Oral Implantol 2015; 41:e189–e194. [DOI] [PubMed] [Google Scholar]
- 10.Modabber A, Ayoub N, Mohlhenrich SC, et al. The accuracy of computer-assisted primary mandibular reconstruction with vascularized bone flaps: iliac crest bone flap versus osteomyocutaneous fibula flap. Med Devices (Auckl) 2014; 7:211–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen SH, Chen HC, Horng SY, et al. Reconstruction for osteoradionecrosis of the mandible: superiority of free iliac bone flap to fibula flap in postoperative infection and healing. Ann Plast Surg 2014; 73 suppl 1:S18–S26. [DOI] [PubMed] [Google Scholar]
- 12.Trignano E, Fallico N, Nitto A, et al. The treatment of composite defect of bone and soft tissues with a combined latissimus dorsi and serratus anterior and rib free flap. Microsurgery 2013; 33:173–183. [DOI] [PubMed] [Google Scholar]
- 13.Aydogan F, Akbay E, Cevik C, et al. Blood-pool SPECT in addition to bone SPECT in the viability assessment in mandibular reconstruction. Eur Rev Med Pharmacol Sci 2014; 18:587–592. [PubMed] [Google Scholar]
- 14.Katims JJ, Naviasky EH, Ng LK, et al. New screening device for assessment of peripheral neuropathy. J Occup Med 1986; 28:1219–1221. [PubMed] [Google Scholar]
- 15.Katims JJ, Naviasky EH, Rendell MS, et al. Constant current sine wave transcutaneous nerve stimulation for the evaluation of peripheral neuropathy. Arch Phys Med Rehabil 1987; 68:210–213. [PubMed] [Google Scholar]
- 16.Miyazaki T, Sakai T, Tsuchiya T, et al. Assessment and follow-up of intercostal nerve damage after video-assisted thoracic surgery. Eur J Cardiothorac Surg 2011; 39:1033–1039. [DOI] [PubMed] [Google Scholar]
- 17.Ferreira JJ, Zagalo CM, Oliveira ML, et al. Mandible reconstruction: history, state of the art and persistent problems. Prosthet Orthot Int 2015; 39:182–189. [DOI] [PubMed] [Google Scholar]
- 18.Bhathena HM, Kavarana NM. Primary reconstruction of head and neck cancer with anterior rib, osteomyocutaneous composite flap. Head Neck 1992; 14:183–187. [DOI] [PubMed] [Google Scholar]
- 19.Ariyan S. The viability of rib grafts transplanted with the periosteal blood supply. Plast Reconstr Surg 1980; 65:140–151. [DOI] [PubMed] [Google Scholar]
- 20.Tanaka K, Okazaki M, Homma T, et al. Bilateral inferior alveolar nerve reconstruction with a vascularized sural nerve graft included in a free fibular osteocutaneous flap after segmental mandibulectomy. Head Neck 2015; 38:E111–E114. [DOI] [PubMed] [Google Scholar]
- 21.Lykissas MG, Kostas-Agnantis IP, Korompilias AV, et al. Use of intercostal nerves for different target neurotization in brachial plexus reconstruction. World J Orthop 2013; 4:107–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nishimura Y, Mizushima T, Tajima F, et al. Cardiovascular responses to static muscle contraction in patients with brachial plexus injury treated with intercostal nerve transfer. J Neurotrauma 2011; 28:1289–1294. [DOI] [PubMed] [Google Scholar]


