Abstract
Concerns about body shape and weight are core diagnostic criteria for eating disorders although intensity varies between patients. Few studies have focused on the clinical differences relative to the intensity of these concerns. Nonetheless, they might have a prognostic value. This study was aimed at identifying the characteristics associated with marked body shape concerns in patients with an eating disorder. Data was collected from a systematic and standardized clinical assessment of outpatients seeking treatment in our department for eating disorders. Only female patients, suffering from anorexia nervosa or bulimia nervosa, and with “no / mild” or “marked” body shape concerns according to the Body Shape Questionnaire, were included for the present study. We focused on sociodemographic characteristics, eating disorder characteristics, axis 1 disorders, types of attachment, self-esteem and dissociation. A multiple logistic regression was performed to identify factors related to “marked” body shape concerns. In our sample (123 participants, with a mean age of 24.3 years [range 16–61]), 56.9% had marked concerns with body shape. Marked body shape concerns were associated with a major depressive episode (OR = 100.3), the use of laxatives (OR = 49.8), a high score on the item “body dissatisfaction” of the Eating Disorders Inventory scale (OR = 1.7), a higher minimum body mass index (OR = 1.73), and a high score on the item “loss of control over behavior, thoughts and emotions” from the dissociation questionnaire (OR = 10.74). These results are consistent with previous studies, and highlight the importance of denial.
Introduction
Eating Disorders (ED), which include in particular Anorexia Nervosa (AN), Bulimia Nervosa (BN), Binge Eating Disorder (BED) and Other Specified / Unspecified Feeding and Eating Disorders are frequent pathologies which mainly affect young women and for whom the prognosis remains guarded. According to the American Psychiatric Association [1], prevalence of AN is 0.4% and that of BN is between 0.5% and 1.5%. A study by Zipfel et al. [2] found that only half of the patients suffering from AN had recovered after 21 years. About 10% of these AN patients met all the diagnostic criteria and more than 15% had died from an ED related cause (infectious cause, hydroelectrolytic disorders, suicide). Indeed, numerous studies mention the high mortality, between 5% and 10%, associated with AN [3]. The DSM-5 maintains a 5% mortality per decade for AN and a 2% mortality per decade for BN [1].
Patients with an ED are much more concerned with their body image and weight than the rest of the population. Body image is based on two key elements: a mental picture of one’s physical body (including size, shape, and appearance), and one’s attitude toward the physical self (such as thoughts, feelings and beliefs about one’s body). It is a part of body representation, involved in conscious body-related perception and cognition. ED are usually associated with disturbances of self-perception and body size estimation [4]. Having distorted oversized body image leads the patients with an ED to body dissatisfaction, resulting in negative thoughts and feelings about their own body, and reinforces the fear of gaining weight or becoming fat. These concerns usually are intrusive and pervasive in patients with an ED. As a rule, they occupy a significant space in the clinical symptoms of ED [5], whether it be AN or BN [6]. Indeed, the DSM-5 allocates a pivotal place to concerns related to body shape and weight in the diagnosis of AN, which appear also in the definition of BN [1] (S1 Table).
Marked concerns about weight and shape are a risk factor in developing an ED [7–10]. Moreover, body image disturbances have also been shown to be a recurrent factor in the persistence of ED [11] and in relapses [12], and could thus also have a prognostic value [6]. The mechanisms underlying a distorted body image remain unclear [13]. The development of neurocognitive sciences, with an increasing number of studies assessing cognitive functioning in ED, may help to better understand the distortion of body image. To date, studies have evoked a primary impairment in the processing of spatial reference frames along with an inability to update stored representations of body shape in ED patients. These deficiencies could be related to a distortion in body image [14].
Clinical experience shows that there are various intensities of body shape concerns among patients with ED, with different evolutions. Assessing body shape concerns is a challenge, as sometimes, they are not expressed consciously [15]. This explains the change in criterion B of AN diagnosis in the firth version of DSM [1]. To the best of our knowledge, no study has yet been conducted to determine the level of body shape concerns and their correlates among patients with an ED.
The aim of our study is thus to determine whether or not the intensity of body shape concerns in ED patients is associated with specific psychopathological profiles.
Materials and Methods
Procedure and Ethics
Our unit is specialized in ED management and is recognized as a Reference Centre for the Region of Western France. To receive treatment in our unit, patients must be referred to us by a medical professional. We provide physical, psychological and social care in accordance with guidelines for ED management [16–18]. The care objectives of our unit are; (i) to restore patients to a healthy weight, (ii) to change core dysfunctional symptoms and attitudes related to ED (excessive concerns about body shape and weight, dietary restriction, purge and binge symptoms, etc.) and (iii) to manage all other negative features of ED. Treatment is primarily in an outpatient format, with inpatient treatment provided only if necessary.
Since September 2012, an in depth clinical assessment is carried out systematically for all new ED patients referred to our unit for treatment. The aforementioned assessment, which forms the EVALADD cohort, takes place prior to the first medical consultation and aims at highlighting the risk factors involved in ED initiation and persistence. The main criteria for inclusion in the EVALADD cohort are; an age of 16 years or older and an ED as defined by the DSM-IV (but excluding amenorrhea for AN). Patients with a cognitive impairment or with difficulties in reading and writing French are not included. All patients have a face-to-face semi-structured interview and complete self-report questionnaires. Qualified and experienced staff members performe the assessments.
The EVALADD cohort was approved by the local Research Ethics Committee (Groupe Nantais d’Ethique dans le Domaine de la Santé), by the CCTIRS (Comité Consultatif sur le Traitement de l'Information en matière de Recherche dans le domaine de la Santé) and by the CNIL (Commission Nationale de l'Informatique et des Libertés). All participants provided written informed consent (for under 18 year olds written informed consent was provided by a legal representative), in accordance with the Helsinki declaration.
Participants
Data for our study was collected between September 2012 and June 2014, we only included patients that respected the following criteria (i) female patients, (ii) diagnosed with AN or BN and (iii) with a Body Shape Questionnaire (BSQ) score lower than or equal to 110, or above 140.
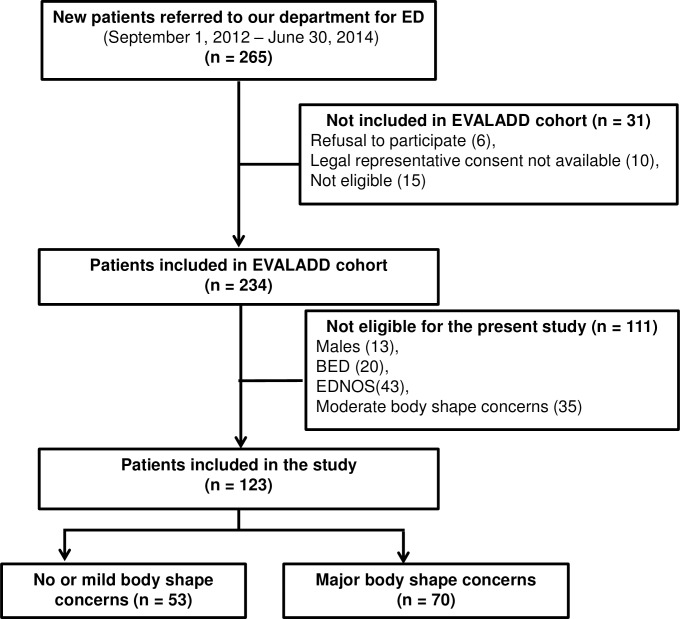
A total of 123 patients out of 234 recruits were included in the study. Fifty-three (53) had a score on the BSQ lower than or equal to 110, whereas 70 had a score on the BSQ above 140. The flow chart of patient selection is presented in Fig 1.
Fig 1. Flow chart of patient selection.
(n) Number of patients included or excluded at each step of the inclusion process. (BED) Binge Eating Disorder. (EDNOS) Eating Disorders Not Otherwise Specified.
Measures
Since this study was preliminary and exploratory in nature, a large range of variables was retained, all were useful in characterizing an ED and the psychopathology of the patients.
Socio-demographic data
The data collected concerned age, sex, marital status and professional status.
Eating disorder characteristics
Structured clinical interview: A standardized assessment of ED, specifically developed for our cohort, was performed by qualified and experienced staff members. Patients were asked about the history of their EDs (duration of ED, lowest body mass index (BMI), current ED (type of ED, current BMI), presence of associated behavior (vomiting, use of laxatives or appetite suppressants, problematic exercise, potomania, self-mutilation), personal history of physical and/or sexual abuse and family history of addictive behavior.
Body Shape Questionnaire (BSQ): The BSQ was conceived by Cooper et al. in 1987 [19] and the French version was validated in 2005 [20]. This self-assessment questionnaire is unidimensional and, through thirty-four items, investigates body dissatisfaction, i.e. concerns regarding weight, body shape, public embarrassment, feeling fat after eating, the banning of certain activities and the avoidance of showing one’s own body. The items reflect upon the last four weeks and answers are given on a 6-point Likert type scale ranging from “Never” to “Always”. The BSQ score provides a classification according to the intensity of body shape concerns (< 80: “no concern”; 80 to 110: “mild concerns”; 111 to 140: “moderate concerns”; > 140: “marked concerns”). The reliability of the BSQ has been reported as high (α = 0.96).
Morgan and Russel Scale: This structured interview examines the various ED characteristics and their repercussions during the previous six months, by way of five subscales exploring diet, menstruation, mental state, psycho-sexual functioning and socioeconomic status [21]. The average of these five scores was used as an average outcome score (Morgan and Russel total score) between 0 and 12, with 12 indicating normal functioning.
Eating Disorder Inventory-2 (EDI-2): This ninety-one (91) item self-assessment questionnaire evaluates the symptomatology and the behavior associated with ED [22]. It examines 11 dimensions: “Drive for thinness”, “Bulimia”, “Body dissatisfaction”, “Ineffectiveness”, “Perfectionism”, “Interpersonal distrust”, “Interoceptive awareness”, “Maturity fears”, “Asceticism”, “Impulse regulation” and “Social insecurity”. Answers are given on a 6-point Likert type scale ranging from “Never” to “Always”. Each of these dimensions can be analyzed independently and a score is calculated for each item. Internal consistency factors for the EDI-2 dimensions are between 0.44 and 0.93.
Contour Drawing Rating Scale (CDRS): This scale examines nine body shapes to which each is assigned a number, from 1 for the thinnest to 9 for the largest [23]. Patients must choose their current body shape and ideal body shape. The discrepancy between the ideal and current body shape scores is equal to the index of the body dissatisfaction score. If the resulting score is positive, body dissatisfaction is linked to a feeling of being overweight and if the score is negative, body dissatisfaction is linked to a feeling of being underweight. In the validation study, the CDRS showed a good level of reliability (r = 0.78) and validity (95.2% patients were positioned correctly).
Clinical characteristics
Mini International Neuropsychiatric Interview (MINI): The fifth version of this structured diagnostic interview allows for the main axis-I psychiatric disorders of the DSM-IV to be explored in a quick and standardized manner [24]. For the aim of this study, a French version was used [25] and only major depressive episodes and risk of suicide were considered. For major depressive episodes, the kappa coefficient (0.73), sensitivity (0.94) and specificity (0.78) were all good.
Relationship Scales Questionnaire (RS-Q): This 30 item self-assessment questionnaire was developed in 1991 [26] and validated in French in 2010 [27]. This questionnaire is based on the theoretical principles of Bowlby and, more specifically, on the concept of an Internal Working Model to examine four different types of attachments: “secure”, “fearful”, “preoccupied” and “dismissing”. For all items, answers were given on a 5-point Likert type scale ranging from “Not at all like me” to “just like me”. In the French translation study, cronbach’s alpha coefficient was moderate (α > 0.60) and the Intraclass Coefficients were good (> 0.75).
Self-Esteem Scale (SES)
This self-assessment questionnaire enables a global evaluation of self-esteem based on ten items [28]. For all items, answers are given on a 4-point Likert type scale ranging from “Strongly disagree” to “Strongly agree”. Cronbach's alpha coefficient ranges from 0.77 to 0.88 and correlations from the test-retest reliability range from between 0.82 to 0.88. The global score indicates a “low self-esteem” (score <30) or a “high self-esteem” (score ≥ 30). The validation of a French version was obtained in 1990 [29].
Dissociation Questionnaire (DIS-Q)
This 63-item questionnaire assists in the assessment of dissociative experiences according to four sub-scales: “identity confusion”, “loss of control over behavior, thoughts and emotions”, “amnesia” and “absorption” [30]. Answers are given on 5-point Likert type scale ranging from “Not at all” to “Extremely”. For each subscale an average score is calculated. Cronbach's alpha ranges from 0.69 to 0.94. The validation of a French version was obtained in 1998 [31].
Statistical analysis
We established two groups of patients according to BSQ scale scores: a group “no or mild concerns with body shape” (BSQ ≤ 110) and a group “marked concerns with body shape” (BSQ > 140).
A descriptive statistical analysis of the socio-demographic, clinical and ED characteristics was carried out in order to obtain means, medians and standard deviations for continuous variables, and numbers of patients, for categorical variables. An univariate analysis was performed in the following way. The links, between the socio-demographic, clinical and ED characteristics on the one hand, and the BSQ status (“low” vs “marked” concerns with body shape) on the other hand, were studied using Student tests for the quantitative variables and Chi-2 or Fisher tests for the qualitative variables [32].
Thereafter multivariate analyses (multiple logistic regression) were performed using an iterative selection procedure to select the variables that were significantly associated with the BSQ status, as assessed by the likelihood ratio test. Variables were considered as candidates for the model if they were associated to “marked concerns with body shape” in a univariate analysis with a p < 0.20. In this step, non-significant variables at 5% were removed one at a time, starting with the least significant variable (backward procedure), in order to select only the variables which provided significant information. Variables to be included in the final models were selected using a p < 0.05 criterion. The corresponding odds ratio and associated 95% confidence interval were estimated. Discrimination of the final logistic models, which describes the models ability to differentiate between “low” versus “high” BSQ scores, was assessed using the area under the Receiver Operating Characteristic (ROC) curve and the goodness-of-fit of the model was assessed using the Hosmer–Lemeshow test. The statistical analysis was carried out with SAS 9.1 and R statistical software (SAS Institute, Inc.). The conditions of validity were verified for all of the tests and models.
Results
Description of the complete sample
The study sample included a total of 123 patients of whom 121 had complete data.
Socio-demographic Data
Only women aged between 16 and 61, with a mean of 24.3 years old (SD = 9.3) were included in our sample. Most patients were single (83.7%) and unemployed (72.4%).
Eating Disorder Characteristics
Of the 123 patients, 46 (37.4%) had a restricting type of AN (AN-R), 28 (22.8%) had a binge eating/purging type of AN (AN-B/P) and 49 (39.8%) displayed BN. The ED had on average started 8 years before (SD = 9.15). The clinical characteristics associated with ED are detailed in Table 1.
Table 1. Characteristics (current or past) associated with ED (N = 123).
| Characteristics | Percentages |
|---|---|
| Vomiting | 61.8% |
| Laxatives | 24.4% |
| Appetite suppressants | 13.8% |
| Problematic exercise | 63.3% |
| Potomania | 25.2% |
| Self-mutilation | 25.2% |
N, number of patients; %, percentage.
The average BMI across the sample was 17.6 kg/m2 (SD = 3.18). Most of the patients (87) expressed body dissatisfaction due to a feeling of being overweight (62.6% with a positive CDRS score), while 34 expressed body dissatisfaction due to a feeling of being underweight (27.6% with a negative CDRS score) and 12 stated that their current body shape matched their ideal body shape (9.8% with neutral CDRS score). Amongst the 123 patients, 53 had a BSQ score below or equal to 110, and made up the first group (“no or mild body shape concerns”), whereas 70 patients had a BSQ score greater than or equal to 140, and made up the second group (“marked body shape concerns”). The highest positive scores of the EDI-2 sub-items concerned “Body dissatisfaction”, “Drive for thinness”, “Interoceptive awareness” and “Ineffectiveness”. Amongst other characteristics, physical or sexual abuse was associated with ED in respectively 6.5% and 13% of cases. Overall, 87% of patients acknowledged some prior family history of addiction (taking into account all types of addictive disorders). ED made up half (50.5%) of this type of family history.
Clinical Characteristics
Amongst the 123 patients, the vast majority (75.6%) reported a major depressive episode either current (30.1%) or past (45.5%). A current suicide risk was displayed in 60.2% of the sample. The psychological characteristics, as evaluated by the self-assessment questionnaires are listed in Table 2.
Table 2. Clinical Characteristics associated with ED (N = 123).
| Variables | Mean (SD) |
|---|---|
| SES Total score | 22.05 (6.05) |
| RSQ Secure attachment score | 2.69 (0.64) |
| RSQ Fearful attachment score | 3.39 (0.87) |
| RSQ Preoccupied attachment score | 3.39 (0.75) |
| RSQ Dismissing attachment score | 3.21 (0.81) |
| DIS-Q Total score | 2.59 (0.59) |
| DIS-Q Confusion score | 2.64 (0.84) |
| DIS-Q Amnesia score | 1.86 (0.66) |
| DIS-Q Loss of control score | 2.82 (0.77) |
| DIS-Q Absorption score | 2.97 (0.73) |
N, Number of patients; SD, Standard deviation; DIS-Q, Dissociation Questionnaire; RSQ, Relationship Scale Questionnaire; SES, Self-Esteem Scale.
Comparison of the two groups of patients: univariate analysis and multiple logistic regression
Fifty-three (53) patients had a BSQ score lower than or equal to 110 and were classified in the group “no or mild concerns with body shape”. Whereas, 70 patients had a BSQ score higher than 140 and were classified in the group “marked concerns with body shape”. As shown in Table 3, an univariate analysis was performed in order to identify variables associated with marked body shape concerns.
Table 3. Univariate comparison of patients according to the intensity of body shape concerns (N = 123).
| Variables | No or mild body shape concerns n = 53% or m (sd) | Marked body shape concerns n = 70% or m (sd) | p | Statistical tests |
|---|---|---|---|---|
| Age (years) | 25.2 (10.7) | 23.6 (8.1) | 0.37 | Student test |
| Marital status: single | 83.0% | 84.3% | 0.45 | Fischer test |
| Professional status: unemployed | 75.5% | 70.0% | 0.50 | Chi2 test |
| Duration of ED (years) | 8.0 (10.7) | 7.9 (7.8) | 0.96 | Student test |
| Type of ED: anorexia nervosa | 84.9% | 41.4% | < 0.01 | Chi2 test |
| Current BMI (kg/m2) | 15.9 (2.0) | 18.3 (3.3) | < 0.01 | Student test |
| Minimum BMI (kg/m2) | 14.4 (2.0) | 16.0 (2.2) | < 0.01 | Student test |
| Vomiting (current and past) | 39.6% | 78.6% | < 0.01 | Chi2 test |
| Use of laxatives (current and past) | 7.6% | 37.1% | < 0.01 | Fischer test |
| Use of appetite suppressants (current and past) | 1.9% | 22.9% | < 0.01 | Fischer test |
| Problematic exercise (current and past) | 51.9% | 72.1% | 0.02 | Chi2 test |
| Potomania (current and past) | 15.1% | 32.9% | 0.02 | Chi2 test |
| Self-mutilation (current and past) | 9.4% | 37.1% | <0.01 | Chi2 test |
| Family history of addictive behavior | 81.1% | 91.4% | 0.09 | Chi2 test |
| Morgan & Russel total score | 6.2 (1.9) | 5.9 (1.7) | 0.38 | Student test |
| EDI -Drive for thinness | 10.8 (5.4) | 17.6 (2.3) | <0.01 | Student test |
| EDI- Bulimia | 3.4 (4.4) | 12.0 (6.1) | 0.02 | Student test |
| EDI- Body dissatisfaction | 8.9 (4.7) | 20.7 (6.2) | <0.01 | Student test |
| EDI- Ineffectiveness | 8.7 (5.4) | 16.2 (7.5) | <0.01 | Student test |
| EDI- Perfectionism | 5.6 (3.5) | 7.4 (4.3) | 0.01 | Student test |
| EDI- Interpersonal distrust | 5.2 (3.7) | 8.6 (4.6) | <0.01 | Student test |
| EDI- Interceptive awareness | 8.5 (4.6) | 16.5 (6.5) | <0.01 | Student test |
| EDI- Maturity fears | 6.3 (4.5) | 7.4 (6.0) | 0.23 | Student test |
| EDI- Asceticism | 5.2 (3.2) | 9.8 (9.8) | <0.01 | Student test |
| EDI- Impulse regulation | 3.4 (3.8) | 10.3 (7.1) | <0.01 | Student test |
| EDI -Social insecurity | 6.6 (3.6) | 11.1 (4.8) | <0.01 | Student test |
| CDRS- Body dissatisfaction | -0.51 (1.5) | 3.5 (2.2) | <0.01 | Student test |
| Major depressive episode (current and past) | 52.8% | 93.0% | <0.01 | Chi2 test |
| Current risk of suicide | 39.6% | 75.7% | <0.01 | Fischer test |
| History of physical and /or sexual abuse | 5.7% | 18.6% | 0.06 | Fischer test |
| RSQ -Secure attachment | 14.7 (3.0) | 12.5 (3.0) | <0.01 | Student test |
| RSQ- Fearful attachment | 12.5 (3.5) | 14.4 (3.3) | <0.01 | Student test |
| RSQ- Preoccupied attachment | 13.4 (2.9) | 13.7 (3.1) | 0.63 | Student test |
| RSQ—Dismissing attachment | 15.6 (3.8) | 16.4 (4.2) | 0.28 | Student test |
| SES total score | 25.5 (5.2) | 19.4 (5.3) | <0.01 | Student test |
| DIS-Q Confusion | 2.3 (0.7) | 2.9 (0.8) | <0.01 | Student test |
| DIS-Q Loss of control | 2.4 (0.6) | 3.2 (0.7) | <0.01 | Student test |
| DIS-Q Amnesia | 1.6 (0.4) | 2.1 (0.7) | <0.01 | Student test |
| DIS-Q Absorption | 2.8 (0.8) | 3.1 (0.7) | 0.04 | Student test |
%, percentage; m, mean; sd, standard deviation; BMI, Body Mass Index; CDRS, Contour Drawing Rating Scale; DIS-Q, Dissociation Questionnaire; ED, Eating Disorder; EDI, Eating Disorder Inventory; RSQ, Relationship Scales Questionnaire; SES, Self-Esteem Scale.
Following to multiple logistic regression, only five variables remained independently associated with “marked concerns with body shape” (BSQ score > 140): a history of major depressive episodes (OR = 100.3); a high minimum BMI (OR = 1.7); a high score on the EDI-2 “body dissatisfaction” (OR = 1.7); the use of laxatives (OR = 49.8) and a high score on the DIS-Q “loss of control” (OR = 10.7). The results of the multiple logistic regression are detailed in Table 4.
Table 4. Multiple logistic regression analysis (final model): factors associated with “marked concerns with body shape” (N = 121).
| Variables | OR | CI95% (OR) | p-value |
|---|---|---|---|
| Major depression (current or past) | 100.28 | [4.36; >999.99] | 0.004 |
| Minimum BMI | 1.73 | [1.14; 2.46] | 0.0087 |
| Laxatives use (current or past) | 49.81 | [2.16; >999.99] | 0.0147 |
| EDI- Body dissatisfaction | 1.68 | [1.28; 2.2] | 0.0002 |
| DIS-Q—Loss of control | 10.74 | [2.24; 51.43] | 0.003 |
OR, Odds ratio; CI95%, 95% confidence interval; BMI, Body Mass Index; DIS-Q, Dissociation Questionnaire; EDI, Eating Disorder Inventory.
The Hosmer-Lemeshow goodness-of-fit test shows that the final model is well calibrated with p = 0.96 (a high p-value indicating a good fit) [32]. The area under the ROC curve is 0.98 showing that the model discriminated well [32] between patients who had “marked concerns with body shape” (N = 70) and those who had “no or mild concerns with body shape” (N = 53).
Discussion
Our study confirms the hypothesis of a link between the intensity of body shape concerns and specific clinical variables.
Firstly, we showed that a significant proportion of patients seeking treatment for ED had no or only mild concerns with body shape. This could be of surprise as body shape concerns are core symptoms of ED. However, this situation is not unusual and several explanations can be considered. Patients with low or normal BMI could have self-reported that they were satisfied with their current body shape whereas the interviewer could have detected that the self-evaluation was unduly influenced by body shape and weight. This raises the question of the truthfulness of patients’ responses as a whole (body shape concerns, laxative use, etc.) when using self-questionnaires. This response bias associated with the self-assessment tools could be explained by the socially desirable responses observed in adolescents and young adults with ED [33]. Furthermore, patients could admit that they are thin, while they still focus on certain body parts, especially the abdomen, buttocks or thighs [1], leading to under-evaluating the importance of body shape concerns assessed by a self-questionnaire. A recent literature review has concluded that patients with AN tend to focus on symptom-specific details, like body parts [34]. Another reason is a state of denial of any illness. Individuals with ED, in particular those suffering from AN, frequently either lack insight into or deny the problem [1]. A previous study [15] has shown that patients in a state of denial, suffering from ED, were more likely to have lower scores of body and weight concerns in self-reported measures. In our study, patients with no or mild body shape concerns were more likely to have a lower minimum BMI, fewer major depressive episodes and less laxatives use. Thus, we can presume that a part of these patients were in a more engrained state of denial of any illness and consequently had more difficulty admitting to characteristics in relation to their body shape or to the negative effects of illness (depression, loss of control). They seemingly also had more difficulty in recognizing the limits of physical health (resulting in a lower minimum BMI).
Secondly, we showed that a larger part of our sample had marked concerns with body shape, and our regression model indicated that a history of major depression, the use of laxatives, a higher minimum BMI, a high score on the “body dissatisfaction” item of the EDI scale and a high score on the “loss of control over behavior, thoughts and emotions” item on the DIS-Q were predictors of marked body shape concerns.
Indeed, we demonstrate a strong correlation between body shape concerns and major depressive episodes (current or past). These results are consistent with those available in scientific literature. For example, Hartmann et al. concluded that there is a relationship between ED and major depression [35] and Hepworth et al. concluded that a negative mood has been shown to increase body size perception [36]. Tuschen-Caffier et al. conducted an experiment, via eye-tracking, and concluded that patients with severe depression were more focused on negatively valenced body parts [37].
We also show that the use of laxatives (current or past) is closely linked to marked body shape concerns. The varying type of ED between the two groups may well have influenced our results since the use of laxatives cannot be associated with AN-R because of its very nature. One could also take a similar line with respect to the “vomiting” symptom. However, our study did not reveal any link between vomiting and marked body shape concerns, this provides material in favor of a specific and real link between marked body shape concerns and the use of laxatives. Furthermore, the association between body shape concerns and laxatives use has already been pointed out by Bryant-Waugh et al. [38]. Another study has shown that some patients with ED may abuse laxatives for different reasons or as manifestations of different forms of psychopathology [39]. Personality dimensions were not assessed in the present study, although it could be argued that our patients with marked body shape concerns displayed personality characteristics that could explain the use of laxatives.
In addition, “Body dissatisfaction” in the EDI-2 was the only EDI-2 subscale associated with marked body shape concerns. The BSQ and the EDI-2 “Body dissatisfaction” subscale investigate very similar fields relating to body shape concerns. The validation study of the BSQ showed significant correlation between the EDI-2 and the BSQ measures for this item [19]. Another study also showed a significant correlation between the BSQ and the EDI-2 “Body dissatisfaction” and the EDI-2 “Drive for thinness” subscales [40].
Moreover, the minimum BMI since the onset of illness were higher in patients with marked body shape concerns. The type of ED could also have influenced the minimum BMI, although we can also suppose that as a general rule, patients with a lower body weight exhibit a more acute state of denial and alexithymia and are therefore less in touch with their body shape concerns. To the best of our knowledge, we did not find studies about the specific influence of BMI on body concerns in a population suffering from ED. However, several studies based on adolescents and adults in the general population indicate that satisfaction with body shape and weight decreases as BMI increases, especially among females [41–45].
Finally, we have shown a link between marked body shape concerns and a high score on the DIS-Q “loss of control” subscale. The latter focuses on analyzing the loss of control over one’s own behavior, thoughts and emotions and it includes some items on controlling one’s eating habits. Thus, it would seem that feeling loss of control over one’s behavior, thoughts and emotions would rather be linked to high body shape concerns. One can presume that the type of ED does have a minimal influence on this feeling, since loss of control is more often felt with BN or AN-B/P than with AN-R, the latter being on the contrary an exercise of excessive control. As a general rule, one can also speculate that when patients are able to voice their body shape concerns, they have in fact already let go and have somewhat abandoned controlling their symptoms, at least to the point of trusting their interviewer enough to talk about them. These patients display clinical signs and behavior different from those who show no or mild body shape concerns.
An important point to highlight is that our study did not show any link between the type of ED and the intensity of body shape concerns; although the distribution of ED types was seemingly not homogeneous between the two groups of patients. Indeed, we found that a higher proportion of patients with AN-R were in the “no or mild body shape concerns” group. Conversely a higher proportion of patients with BN were in the “marked body shape concerns” group. Possibly, the sample size for each ED sub-type is insufficient to provide evidence of a link between the type of ED and the intensity of body shape concerns. Equally likely, there might not be any link between the type of ED and the intensity of body shape concerns. Other authors have used the BSQ to evaluate body shape concerns between groups of patients suffering from ED (one having only AN-R and the other a mix of BN and AN-B/P). No significant difference between the two groups of patients was reported, although they too had small samples [40].
Finally, we have not found a link between a history of sexual abuse and the intensity of body shape concerns. A history of sexual abuse during childhood is, however, a risk factor for developing body dissatisfaction [46]. Our sample was probably too small to reveal such a link since only 16 patients included had a history of sexual abuse. The prevalence of sexual abuse in the general population varies widely, according to authors, ranging from 18% [46] to 33.8% [47]. Data collection for our study began before patients were admitted into our ward. In this context, it is therefore possible that patients under-reported a history of sexual abuse.
The results must be viewed in the context of several limitations. As already partly mentioned, it is very difficult to measure a state of denial, which probably represents the major bias of this type of study and more specifically in patients suffering from AN-R. As a matter of fact, the DSM-5 recommends including the inability to gain weight as a diagnosis criterion, because many patients insist that they have no body shape concerns, yet they are paradoxically unable to reach normal weight. This item may be considered as a state of denial or as a form of disconnection. Furthermore, we have included all patients seeking treatment for their ED, whatever the duration of their disorder. Since our study is a transversal and exploratory work, these results do not enable us to qualify a scale of severity, to predict how clinical signs will evolve, nor to provide prognostic factors. However, this study did include 123 patients, and such a large number allows for a good representativity of patients seeking treatment for ED. The refusal rate in our cohort was also very low and both the interview and the self-assessment questionnaire allowed for investigating body concerns in a complementary manner.
Conclusion
Our study confirms that it is relevant in clinical practice to investigate the intensity of body shape concerns. We show a link to the specific clinical picture and, in particular, major depressive episodes and the use of laxatives. These results should encourage clinicians to systematically evaluate body shape concerns. Furthermore, clinicians should not always be reassured by a low level of body shape concerns, that could in fact reflect a state of denial and a potentially more severe ED. We could go further by doing a longitudinal study and evaluate how patients evolve according to the intensity of their body shape concerns in order to determine whether or not they are indeed a prognostic factor. Therefore, body shape concerns can be considered as a legitimate potential therapeutic target. To this end, body dissatisfaction seems to be improved by conditioning exercises, using repeated mirror exposure focusing on attractive and unattractive body parts [48] or a brief intervention involving photographs of bodies paired with positive social feedback [49]. Furthermore, cognitive remediation could modify the impairment in body image perception.
Supporting Information
Diagnostic and statistical manual of mental health disorders: DSM-5 5th ed. Washington DC: American Psychiatric Publishing; 2013.
(DOC)
Acknowledgments
We would like to thank warmly other staff members (Charlotte Bregeau and Juliette Leboucher) who performed the assessment of the EVALADD cohort.
Data Availability
All relevant data are within the paper and its supporting information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1.American Psychiatric Association. Diagnostic and statistical manual of mental health disorders: DSM-5 5th ed. Washington DC: American Psychiatric Publishing; 2013. [Google Scholar]
- 2.Zipfel S, Lowe B, Reas DL, Deter HC, Herzog W. Long-term prognosis in anorexia nervosa: lessons from a 21-year follow-up study. Lancet. 2000. February 26;355(9205):721–2. 10.1016/S0140-6736(99)05363-5 [DOI] [PubMed] [Google Scholar]
- 3.Treasure J, Schmidt U. Anorexia nervosa. BMJ Clin Evid. 2008;01(1011):2–14. [Google Scholar]
- 4.Esposito R, Cieri F, di Giannantonio M, Tartaro A. The role of body image and self-perception in anorexia nervosa: the neuroimaging perspective. J Neuropsychol. May 25. [DOI] [PubMed] [Google Scholar]
- 5.Treasure J, Claudino AM, Zucker N. Eating disorders. Lancet. 2010. February 13;375(9714):583–93. 10.1016/S0140-6736(09)61748-7 [DOI] [PubMed] [Google Scholar]
- 6.Casper RC, Halmi KA, Goldberg SC, Eckert ED, Davis JM. Disturbances in body image estimation as related to other characteristics and outcome in anorexia nervosa. Br J Psychiatry. 1979. January;134:60–6. [DOI] [PubMed] [Google Scholar]
- 7.Killen JD, Taylor CB, Hayward C, Haydel KF, Wilson DM, Hammer L, et al. Weight concerns influence the development of eating disorders: a 4-year prospective study. J Consult Clin Psychol. 1996. October;64(5):936–40. [DOI] [PubMed] [Google Scholar]
- 8.Stice E, Hayward C, Cameron RP, Killen JD, Taylor CB. Body-image and eating disturbances predict onset of depression among female adolescents: a longitudinal study. J Abnorm Psychol. 2000. August;109(3):438–44. [PubMed] [Google Scholar]
- 9.Jacobi C, Hayward C, de Zwaan M, Kraemer HC, Agras WS. Coming to terms with risk factors for eating disorders: application of risk terminology and suggestions for a general taxonomy. Psychol Bull. 2004. January;130(1):19–65. 10.1037/0033-2909.130.1.19 [DOI] [PubMed] [Google Scholar]
- 10.Stice E, Marti CN, Durant S. Risk factors for onset of eating disorders: evidence of multiple risk pathways from an 8-year prospective study. Behav Res Ther. 2011. October;49(10):622–7. 10.1016/j.brat.2011.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fairburn CG, Stice E, Cooper Z, Doll HA, Norman PA, O'Connor ME. Understanding persistence in bulimia nervosa: a 5-year naturalistic study. J Consult Clin Psychol. 2003. February;71(1):103–9. [PubMed] [Google Scholar]
- 12.Fairburn CG, Peveler RC, Jones R, Hope RA, Doll HA. Predictors of 12-month outcome in bulimia nervosa and the influence of attitudes to shape and weight. J Consult Clin Psychol. 1993. August;61(4):696–8. [DOI] [PubMed] [Google Scholar]
- 13.Riva G, Gaudio S, Dakanalis A. I'm in a virtual body: a locked allocentric memory may impair the experience of the body in both obesity and anorexia nervosa. Eat Weight Disord. 2014. March;19(1):133–4. 10.1007/s40519-013-0066-3 [DOI] [PubMed] [Google Scholar]
- 14.Serino S, Dakanalis A, Gaudio S, Carra G, Cipresso P, Clerici M, et al. Out of body, out of space: Impaired reference frame processing in eating disorders. Psychiatry Res. 2015. December 15;230(2):732–4. 10.1016/j.psychres.2015.10.025 [DOI] [PubMed] [Google Scholar]
- 15.Couturier JL, Lock J. Denial and minimization in adolescents with anorexia nervosa. Int J Eat Disord. 2006. April;39(3):212–6. 10.1002/eat.20241 [DOI] [PubMed] [Google Scholar]
- 16.Haute Autorité de Santé (HAS). Recommandations de bonne pratique: Anorexie mentale: prise en charge: argumentaire: HAS—Haute Autorité de santé AFDAS-TSA—Association française pour le développement des approches spécialisées des troubles du comportement alimentaire Inserm—Institut national de la santé et de la recherche médicale 2010 Juin 2010.
- 17.American Psychiatric Association (APA). Treatment of patients with eating disorders,third edition. American Psychiatric Association. Am J Psychiatry. 2006. July;163(7 Suppl):4–54. [PubMed] [Google Scholar]
- 18.National Institute for health and Care Excellence (NICE). Eating Disorders Core interventions in the treatment and management of anorexia nervosa, bulimia nervosa and related eating disorders. The British Pyschological Society & The Royal College of Psychiatrists; 2004. [PubMed] [Google Scholar]
- 19.Cooper PJ, Taylor MJ, Cooper Z, Fairburn CG. The development and validation of the body shape questionnaire. Int J Eat Disord. 1987;6:485–94. [Google Scholar]
- 20.Rousseau A, Knotter A, Barbe P, Raich R, Chabrol H. [Validation of the French version of the Body Shape Questionnaire]. Encephale. 2005. Mar-Apr;31(2):162–73. [DOI] [PubMed] [Google Scholar]
- 21.Morgan HG, Hayward AE. Clinical assessment of anorexia nervosa. The Morgan-Russell outcome assessment schedule. Br J Psychiatry. 1988. March;152:367–71. [DOI] [PubMed] [Google Scholar]
- 22.Garner DM. Eating Disorder Inventory 2—Professional manual: Psychological Assessment Ressources; 1991.
- 23.Thompson MA, Gray JJ. Development and validation of a new body-image assessment scale. J Pers Assess. 1995. April;64(2):258–69. 10.1207/s15327752jpa6402_6 [DOI] [PubMed] [Google Scholar]
- 24.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59 Suppl 20:22–33;quiz 4–57. [PubMed] [Google Scholar]
- 25.Lecrubier Y, Sheehan DV, Weiller E, Amorim P, Bonora I, Harnett Sheehan K, et al. The Mini International Neuropsychiatric Interview (MINI). A short diagnostic structured interview: reliability and validity according to the CIDI. European Psychiatry. 1997;12(5):224–31. [Google Scholar]
- 26.Bartholomew K, Horowitz LM. Attachment Styles Among \bung Adults: A Test of a Four-Category Model. Journal of Personality and Social Psychology. 1991. August;61(2):226–44. [DOI] [PubMed] [Google Scholar]
- 27.Guédeney N, Fermanian J, Bifulco A. La version française du Relationship Scales Questionnaire de Bartholomew (RSQ, Questionnaire des échelles de relation): étude de validation du construit. L'Encéphale. 2010;36(1):69–76. [DOI] [PubMed] [Google Scholar]
- 28.Rosenberg M. Society and the Adolescent Self-image. Princeton: Princeton University Press; 1965. [Google Scholar]
- 29.Vallieres EF, Vallerand RJ. Traduction et validation canadienne-française de l'échelle de l'estime de soi de Rosenberg. International Journal of Psychology. 1990;25(2):305–3016. [Google Scholar]
- 30.Vanderlinden J, Van Dyck R, Vandereycken W, Vertommen H, Verkes RJ. The dissociation questionnaire (DIS-Q): Development and characteristics of a new self-report questionnaire. Clin Psychol Psychother. 1993;1(21–27). [Google Scholar]
- 31.Mihaescu G, Vanderlinden J, Séchaud M, Heize X, Baettig D. le questionnaire de dissociation DIS-Q: résultats préliminaires dans une population Suisse Francophone. Encephale. 1998;24(4):337–46. [PubMed] [Google Scholar]
- 32.Bouyer J. méthodes statistiques: médecine- biologie Paris: Broché; 1997. [Google Scholar]
- 33.Johnson ME, Brems C, Fischer P. Sex role conflict, social desirability, and eating-disorder attitudes and behaviors. J Gen Psychol. 1996. January;123(1):75–87. 10.1080/00221309.1996.9921261 [DOI] [PubMed] [Google Scholar]
- 34.Madsen SK, Bohon C, Feusner JD. Visual processing in anorexia nervosa and body dysmorphic disorder: similarities, differences, and future research directions. J Psychiatr Res. 2013. October;47(10):1483–91. 10.1016/j.jpsychires.2013.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hartmann AS, Greenberg JL, Wilhelm S. The relationship between anorexia nervosa and body dysmorphic disorder. Clin Psychol Rev. July;33(5):675–85. 10.1016/j.cpr.2013.04.002 [DOI] [PubMed] [Google Scholar]
- 36.Hepworth R, Mogg K, Brignell C, Bradley BP. Negative mood increases selective attention to food cues and subjective appetite. Appetite. 2010. February;54(1):134–42. 10.1016/j.appet.2009.09.019 [DOI] [PubMed] [Google Scholar]
- 37.Tuschen-Caffier B, Bender C, Caffier D, Klenner K, Braks K, Svaldi J. Selective Visual Attention during Mirror Exposure in Anorexia and Bulimia Nervosa. PLoS One. 2015;10(12):e0145886 10.1371/journal.pone.0145886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bryant-Waugh R, Turner H, East P, Gamble C, Mehta R. Misuse of laxatives among adult outpatients with eating disorders: prevalence and profiles. Int J Eat Disord. 2006. July;39(5):404–9. 10.1002/eat.20267 [DOI] [PubMed] [Google Scholar]
- 39.Pryor T, Wiederman MW, McGilley B. Laxative abuse among women with eating disorders: an indication of psychopathology? Int J Eat Disord. 1996. July;20(1):13–8. [DOI] [PubMed] [Google Scholar]
- 40.Lavoisy G, Guelfi JD, Vera L, Dardennes R, Rouillon F. [Evaluation of perturbed body image in eating disorders using the Body Shape Questionnaire]. Encephale. 2008. December;34(6):570–6. 10.1016/j.encep.2007.11.005 [DOI] [PubMed] [Google Scholar]
- 41.Fan Y, Li Y, Liu A, Hu X, Ma G, Xu G. Associations between body mass index, weight control concerns and behaviors, and eating disorder symptoms among non-clinical Chinese adolescents. BMC Public Health. 2010;10:314 10.1186/1471-2458-10-314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kaminsky LA, Dewey D. The association between body mass index and physical activity, and body image, self esteem and social support in adolescents with type 1 diabetes. Can J Diabetes. 2014. August;38(4):244–9. 10.1016/j.jcjd.2014.04.005 [DOI] [PubMed] [Google Scholar]
- 43.Mendonca KL, Sousa AL, Carneiro CS, Nascente FM, Povoa TI, Souza WK, et al. Does nutritional status interfere with adolescents' body image perception? Eat Behav. 2014. August;15(3):509–12. 10.1016/j.eatbeh.2014.06.011 [DOI] [PubMed] [Google Scholar]
- 44.Pingitore R, Spring B, Garfield D. Gender differences in body satisfaction. Obes Res. 1997. September;5(5):402–9. [DOI] [PubMed] [Google Scholar]
- 45.Calzo JP, Sonneville KR, Haines J, Blood EA, Field AE, Austin SB. The development of associations among body mass index, body dissatisfaction, and weight and shape concern in adolescent boys and girls. J Adolesc Health. 2012. November;51(5):517–23. 10.1016/j.jadohealth.2012.02.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Preti A, Incani E, Camboni MV, Petretto DR, Masala C. Sexual abuse and eating disorder symptoms: the mediator role of bodily dissatisfaction. Compr Psychiatry. 2006. Nov-Dec;47(6):475–81. 10.1016/j.comppsych.2006.03.004 [DOI] [PubMed] [Google Scholar]
- 47.Halperin DS, Bouvier P, Jaffe PD, Mounoud RL, Pawlak CH, Laederach J, et al. Prevalence of child sexual abuse among adolescents in Geneva: results of a cross sectional survey. BMJ. 1996. May 25;312(7042):1326–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jansen A, Voorwinde V, Hoebink Y, Rekkers M, Martijn C, Mulkens S. Mirror exposure to increase body satisfaction: Should we guide the focus of attention towards positively or negatively evaluated body parts? J Behav Ther Exp Psychiatry. 2016. March;50:90–6. 10.1016/j.jbtep.2015.06.002 [DOI] [PubMed] [Google Scholar]
- 49.Aspen V, Martijn C, Alleva JM, Nagel J, Perret C, Purvis C, et al. Decreasing body dissatisfaction using a brief conditioning intervention. Behav Res Ther. 2015. June;69:93–9. 10.1016/j.brat.2015.04.003 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Diagnostic and statistical manual of mental health disorders: DSM-5 5th ed. Washington DC: American Psychiatric Publishing; 2013.
(DOC)
Data Availability Statement
All relevant data are within the paper and its supporting information files.