Abstract
For diagnosis and follow up, it is important to be able to quantify limp in an objective, and precise way adapted to daily clinical consultation. The purpose of this exploratory study was to determine if an inertial sensor-based method could provide simple features that correlate with the severity of lower limb osteoarthritis evaluated by the WOMAC index without the use of step detection in the signal processing. Forty-eight patients with lower limb osteoarthritis formed two severity groups separated by the median of the WOMAC index (G1, G2). Twelve asymptomatic age-matched control subjects formed the control group (G0). Subjects were asked to walk straight 10 meters forward and 10 meters back at self-selected walking speeds with inertial measurement units (IMU) (3-D accelerometers, 3-D gyroscopes and 3-D magnetometers) attached on the head, the lower back (L3-L4) and both feet. Sixty parameters corresponding to the mean and the root mean square (RMS) of the recorded signals on the various sensors (head, lower back and feet), in the various axes, in the various frames were computed. Parameters were defined as discriminating when they showed statistical differences between the three groups. In total, four parameters were found discriminating: mean and RMS of the norm of the acceleration in the horizontal plane for contralateral and ipsilateral foot in the doctor’s office frame. No discriminating parameter was found on the head or the lower back. No discriminating parameter was found in the sensor linked frames. This study showed that two IMUs placed on both feet and a step detection free signal processing method could be an objective and quantitative complement to the clinical examination of the physician in everyday practice. Our method provides new automatically computed parameters that could be used for the comprehension of lower limb osteoarthritis. It may not only be used in medical consultation to score patients but also to monitor the evolution of their clinical syndrome during and after rehabilitation. Finally, it paves the way for the quantification of gait in other fields such as neurology and for monitoring the gait at a patient’s home.
Introduction
Gait analysis plays an important role in the study of lower limb osteoarthritis on two grounds: first, osteoarthritis has important repercussions on gait biomechanics [1–4]. It rapidly worsen the prognosis for the affected joints, and on the long term affect the intact ones, which further compromises the mobility of the patients. Second, the functional syndrome, ie the limp evaluated with infrared markers, is well correlated with the severity of the pathology [5]. By using stereophotogrammetry and force plates in gait laboratories, compared to matched controls, knee osteoarthritis patients had reductions in walking speed [6–8], lower cadence [9,10], longer double support time [9,11] and a smaller stride length [12]. That is, gait analysis would be useful to quantify precisely the severity of osteoarthritis in a given patient. However, until recently, gait laboratories were too expensive and complex to be utilized in daily practice. This explains that clinical scores remains the gold standard to evaluate the severity of the pathology up to these days [13–15]. The Western Ontario and MACmaster Universities osteoarthritis index (WOMAC) is actually the most largely used of these scores in rheumatology for lower limb osteoarthritis to assess pain, stiffness, and physical function in patients. WOMAC is considered to be reliable, sensitive and adapted to clinical practice [16–18] and therefore, it is used in most osteoarthritis clinical studies [19,20]. It remains that clinical scores are inherently subjective, as they are based on the patient’s verbal reports and on the clinician’s visual skills and interpretations. For instance, the WOMAC index does not accurately reflect walking performances [21,22] and clinical scores have a lack of sensitivity for identifying changes of balance and walking in mild to moderate disease severity [23].
In that context, skin-mounted accelerometers seem to be well-suited for investigating gait kinematics in osteoarthritis patients [24]. They are inexpensive and non-invasive devices and, more importantly, they are suited for routine clinical practice. In particular, they can be used to evaluate gait using a standard protocol, which involves walking ten meters forward and ten meters back on a level surface at a self-selected walking speed [25–31]. An essential point using gait analysis in the everyday consultation is to extract from the raw data, automatically and in real time, useful parameters for the clinician. To begin, step detection and gait cycle identification are critical for computing gait parameters. By hand, it is time consuming and unfit for clinical practice [3,13,32,33]. On the other hand, the automated routines available for step detection are not robust because they are based on a priori predetermined threshold values [34,35]. In addition, step detection automated routines are based on the assumption that steps have stable kinematics, which is not the case in pathological conditions [34,36–40].
Inertial sensors are suitable for quantifying gait performance directly at the routine consultation level. For this use, the quantification can be driven by real-time and low-powered software. Advanced trunk accelerometric parameters have been found useful for detecting pathological gait [41]. Nevertheless, complex gait parameters often require previous step detection, which requires extensive and time-consuming computation for sufficient robustness. As well, the clinical meaning of complex gait parameters is not always clear, although recent papers have made substantial efforts to clarify this point [42]. Still, this situation is unfortunate because straight-forward gait parameters (mean or root mean square [RMS]) for the signals often reveal clinically interpretable results [41,43]. Therefore, simple parameters such as the RMS remain commonly used but often only for the lower back sensor [28,41,44–48]. They often show differences between the pathological and healthy gait. These simple parameters have not been explored at other key anatomical landmarks of the body.
Finally, the gait parameters have widely been developed in complex neurological limping models such as Parkinson disease, cerebral palsy or peripheral neuropathy and not in osteoarthritis, in which pain is believed to be the major limping cause and for which the simple gait parameters could have a direct, understandable clinical meaning [41].
Hence, we have tried to revisit the problem of gait analysis in osteoarthritis patients in daily practice using four inertial motion units (IMU) strapped to the head, lower back (L3-L4) and feet. We have also designed a new automated and online method of gait analysis. This method was then evaluated by comparing its outcome to the severity of the lower limb osteoarthritis evaluated with the WOMAC index in a cohort of 48 patients and 12 control subjects.
Methods
Subjects
All subjects (patients and control subjects) were coming for a clinical consultation at the orthopedic surgeon’s office (ThG) during three consecutive months. All consecutive patients or control subjects reaching the inclusion criteria during the inclusion period were included in the study.
All patients had hip or knee osteoarthritis diagnosed by an orthopedic surgeon (ThG) and graded with the WOMAC index (0 to 96). Patients had neither vestibular, neurological, or musculoskeletal disorders, nor any fractures of the lower extremity, nor rheumatoid arthritis or generalized osteoarthritis. Forty-eight patients with lower limb osteoarthritis were included (43 to 90 years, mean 70.9 years). Patients were divided into 2 severity groups of equal size separated by the median of the WOMAC index: the moderately impaired group (G 1) and the severely impaired group (G 2). The median value of the WOMAC index was 45/96. This median-based repartition was chosen in order to maximize the power of the statistical analysis.
The control subjects had no orthopedic nor neurological problem that could affect their gait pattern. Twelve control subjects were included (40 to 87 years, mean 60.8). They formed the age-matched control group (G 0). The mean and standard deviation (SD) of the age, body mass index (BMI) and WOMAC index of each group are shown in Table 1.
Table 1. Age body mass index (BMI) and WOMAC index mean (upper case) and standard deviation (lower case) of group 1 and group 2 patients with symptomatic lower limb osteoarthritis and age matched controls.
| Group | Number | Age | BMI | WOMAC |
|---|---|---|---|---|
| 0 | 12 | 63,2 | 25,2 | 0,0 |
| 17,1 | 4,6 | 0,0 | ||
| 1 | 24 | 70.5 | 26.8 | 14,1 |
| 9.5 | 5,7 | 10,0 | ||
| 2 | 24 | 70,5 | 28,2 | 62,58 |
| 14,9 | 5,5 | 14,0 |
To assess the test–retest validity of the discriminating parameters, we checked their variability with IMU placement. For the sensor-placement control experiment 1, 2 healthy controls (age 22 and 23 years) performed 5 walking trials with sensors placed by 2 different operators at each trial. For the sensor-placement control experiment 2, these 2 subjects also performed 9 walking trials with displacement of the sensor along the antero-posterior (AP) axis and the medio-lateral (ML) axis in terms of the reference position (from -20 to +20 mm in 5-mm increments). Coefficients of variation () were evaluated for these 2 experiments, where μ is the mean and σ the standard deviation of the parameters over all trials for each sensor control experiment. A CV < 5% was considered correct and < 10% acceptable.
The study was validated by a local ethic comity (Comité de Protection des Personnes Ile de France II, n°CPP 2014-10-04 RNI) and both patients and control subjects gave their written consent to participate.
Instrumentation
Linear accelerations and angular velocities of the head, lower back (L4-L5 vertebra) and feet were collected using four IMUs including triaxial accelerometers, gyroscopes and magnetometers (XSens®, Culver City, CA, USA, MTw Measurement Units, 3,5h LiPo battery, 27g, 3,5x5,8x1,0cm^3, +/-16g, +/-1200deg/s, 100Hz, errors 0,003m/s2 and 0,05deg/s), fixed with manufacturer-designed adhesive straps and connected through WiFi with a computer.
Defining the sensor linked frame and the doctor’s office linked frame
The accelerations and the angular velocities of the four IMUs can be expressed in the sensor linked frame and in the doctor’s office linked frame.
The IMUs were fixed and aligned with respect to the body in the following way. The head sensor was positioned on the center of the forehead. The antero-posterior (AP) axis of the frame linked to the head sensor was the normal to the forehead surface. The medio-lateral (ML) axis was set parallel to the line joining the left temple and the right temple. The vertical (V) axis completed the orthonormal frame. The lumbar sensor was positioned at L4-L5 level. The AP axis of the frame linked to the lumbar sensor was normal to the back surface. The ML axis was set parallel to the line joining the right anterior superior iliac spine and left anterior superior iliac spine. The V axis completed the orthonormal frame. Each foot sensor was positioned at the center of the dorsal face of each foot. The V axes of each frame linked to each foot sensor were the normals to the dorsal surfaces of each foot. The AP axis was set parallel to the longitudinal direction of the foot. The ML axis completed the orthonormal frame. Positive directions for the axes were not defined because all computed gait parameters are independent of this orientation.
The doctor’s office frame was the fix frame linked to the doctor’s office. The V axis of the doctor’s office linked frame was aligned with the gravity. The horizontal plane (H) was the plane normal to the V axis. AP and ML axes were not defined in the doctor’s office linked frame. The change of frame from the sensor linked frames to the doctor’s office linked frame was done with an algorithm [49,50] based on the XSens® 3D magnetometer measurement. We used the manufacturer’s rotation matrix as described and validated by Cognolato [50].
Experimental design and data acquisition
The WOMAC index was evaluated and recorded by the same experimented orthopedic surgeon (ThG). The questions were always asked in the same order with the validated text. After the sensor fixation, the participant was instructed to execute the following steps: stand quiet for six seconds, walk ten meters at a preferred walking speed, make a U-turn, walk the ten meters back and stand quiet for two seconds.
Participants could keep their clothes and their shoes on. Participants with high heels (>2 cm) were asked to do the exercise without their shoes. Each participant completed two trials of this exercise to improve the reliability of the measure.
Data processing
Each phase of the exercise (quiet standing, walking and U-turn) was manually annotated without any step detection (RB). All parameters were computed on the concatenated signal of the walk phases of the exercise (Fig 1). One given parameter p is defined by a sensor = {head, lower back, ipsilateral foot, contralateral foot}, a frame = {sensor, office}, an axis = {AP,ML,V} if the frame is the sensor-linked frame or an axis = {H, V} if the frame is the doctor’s office-linked frame (H for horizontal plane), a signal sig = {acceleration, angular velocity} and a statistical tool stat = {mean, RMS}. Thus we computed the following:
where |.| is the absolute value and where in the case of n values x = {x1,x2,…,xn}:
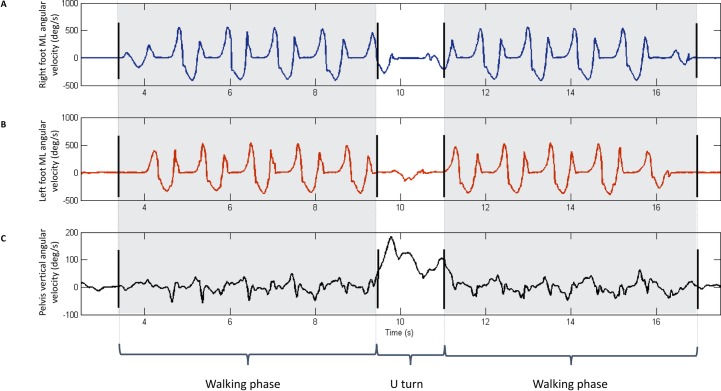
Fig 1. Representative data and manual phase annotation result for one healthy participant performing a 10 meters go and 10 meters back walking exercise at self-selected walking speed.
Black bars stand for manual annotation. Dashed zone corresponds to the walking phases. The walking parts of the signal were taken for parameter computation. (A)–Representative ML lateral angular velocity in the sensor linked frame for right foot. (B)—Representative ML lateral angular velocity in the sensor linked frame for left foot. (C)–Representative V angular velocity in the sensor linked frame for L3-L4.
the mean is defined by
the RMS is defined by
For each parameter, the mean of the two trials was taken. Sixty parameters were computed, fifteen for each sensor (Table 2).
Table 2. Acceleration and angular velocity parameters in the sensor linked frames and the doctor’s office linked frame.
RMS for root mean square.
| Sensor linked frame | ||
| Axis and plane | Acceleration | Angular velocity |
| Meadial lateral (ML) | - | Mean |
| RMS | RMS | |
| Anterior posterior (AP) | - | Mean |
| RMS | RMS | |
| Vertical (V) | - | Mean |
| RMS | RMS | |
| Doctor’s office linked frame | ||
| Axis and plane | Acceleration | Angular velocity |
| Horizontal (H) plane | Mean | - |
| RMS | - | |
| Vertical (V) axis | Mean | Mean |
| RMS | RMS | |
The parameters were also computed by sliding the manually-annotated computation window one second earlier and one second later to take the error of the manual phase annotation into consideration (see Results section). The parameters affected by the gravity component were not studied because they were too sensor’s positioning dependent. These parameters were: the mean of the norm of the acceleration in the sensor linked frames in the AP, ML and V directions on the four markers i.e.:
Gravity component of the acceleration was not removed. The angular velocities in the horizontal plane in the doctor’s office frame was not studied because of the absence of clinical meaning of this parameter i.e.:
Mean walking velocity was computed by dividing the walking distance (20 m) by the duration of the walking phases.
Statistical analysis
A one-way analysis of variance (ANOVA) with Tukey pairwise comparison test and a one-way analysis of covariance (ANCOVA) with age and BMI as covariate with Tukey pairwise comparison were performed on all three groups on all the 61 parameters. Mean walking velocity was not taken as covariate because it is known to decrease with lower limb osteoarthritis severity [25]. We defined a discriminating parameter as a parameter that showed statistical differences using an ANOVA analysis with a Tukey pairwise comparison test (p-value set under 0, 05) between all three groups (G1vsG2, G2vsG3 and G1vsG3).
Results
Data processing
We could manually annotate the initial quiet-standing phase, the go-walking phase, the U-turn and the back-walking phase for all 48 lower limb osteoarthritis patients and the 12 control subjects. Representative data and manual phase annotation results for one control subject performing a 10 meters forward and 10 meters back walking task at a self-selected walking speed are shown in Fig 1. The cumulative error for the manual exercise phase annotation was 1 second. The relative errors due to the manual annotation error on the parameters were 5% on average for the mean of the acceleration in the horizontal plane on the ipsilateral foot. The errors did not change the statistical significance of the in-between group differences shown by the discriminating parameters.
Parameters and statistical analysis
Looking at the 60 IMU-based parameters we found (S1 Table):
in the sensor linked frames: no discriminating parameters (results not shown).
in the doctor’s office linked frame: the mean and the RMS of the norm of the acceleration in the horizontal plane for the contralateral (p-values respectively G0vsG1 = 0.011; G1vsG2 = 0.013; G0vsG2<0.0001 for mean and G0vsG1 = 0.010 G1vsG2 = 0.026; G0vsG2<0.0001 for RMS) and the ipsilateral (p-values respectively G0vsG1 = 0.002; G1vsG2 = 0.0004; G0vsG2<0.0001 for mean and; G0vsG1 = 0.001; G1vsG2 = 0.001; G2vsG0<0.0001 for RMS) foot were discriminating parameters (Fig 2). In our predefined formalism these parameters are p{ipsilateral foot,controlateral foot},office,H,acceleration,{mean,RMS}.
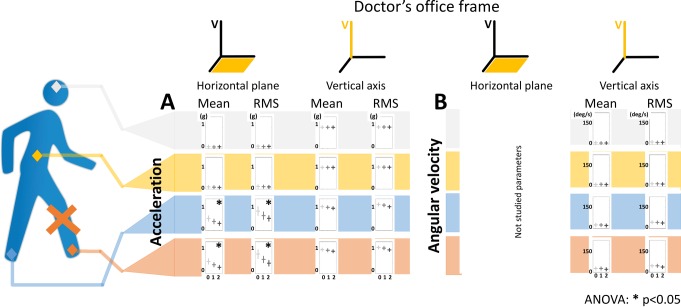
Fig 2. Selected 24 parameters out of the 60 IMU based parameters computed in the doctor’s office linked frame obtained from 4 IMUs on 12 control subjects and 48 patients during a 10 meters go and 10 meters back walking task.
Sensor location are shown on the walking silhouette by colored diamonds: grey for the head, yellow for the sacrum, blue for the contralateral foot and red for the ipsilateral foot. The red cross of the walking silhouette indicates the ipsilateral foot to the lesion defined by the side where the patient is the more symptomatic. Each parameter is represented by a bar diagram. The row indicate the location of the sensor and whether the parameters is computed on an acceleration (A) or an angular velocity signal (B). The columns indicate whether the parameter is computed on the horizontal plane or on the vertical axis and whether the parameter is a mean or a RMS of the norm of the walking signal. In each bar diagram, the parameter is represented as a function of the severity. The results are shown by a modulated grey cross: horizontal bar stands for mean and vertical bar stands for the standard deviation. Light grey represents the healthy group (G0), medium grey the moderately impaired group (G1) and dark grey the severely impaired group (G2). The parameters marked by a star (*) are the discriminating parameters (parameters that show significant difference between the three WOMAC index defined severity groups). The statistical analysis was performed with an ANOVA analysis and a Tukey pairwise comparison test (p-value set at 0.05). RMS stands for root mean square and V for vertical axis.
These parameters can be
In the sensor linked frame, angular velocities around the ML axis on the ipsilateral and contralateral feet didn’t appear to be discriminating parameters, but showed statistical significant differences between the group of control subjects and the two groups of patients (results not shown).
No parameters from the lower back and no parameter from the head were discriminating parameters.
We found that the mean and RMS of the norm of the acceleration in the horizontal plane in the doctor’s office linked frame for contralateral and ipsilateral feet still met our definition of discriminating parameters with age and BMI as covariate.
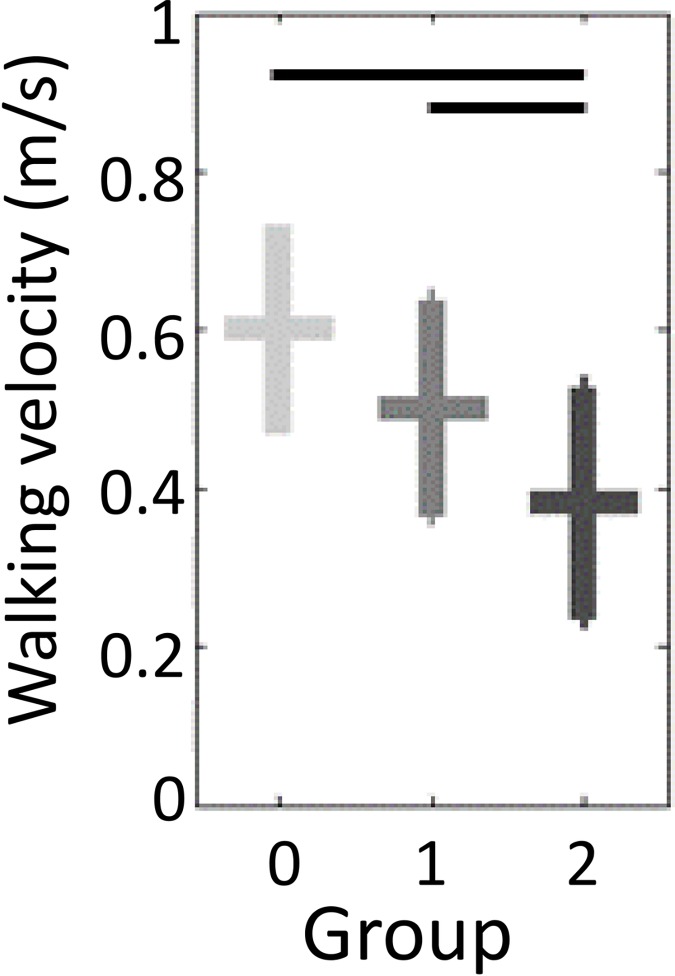
For walking velocity, differences were significant between G0 and G2, G1 and G2. No significant difference in walking velocity was found between G0 and G1 (Fig 3). Thus, walking velocity was not a discriminating parameter.
Fig 3. Mean walking velocity as a function of the WOMAC index based osteoarthritis severity groups.
The results are shown by a modulated grey cross: horizontal bar stands for mean and vertical bar stands for the standard deviation. Light grey represents the healthy participants, medium grey the moderately impaired group and dark grey the severely impaired group. Black horizontal bars show the statistical differences between the groups computed with an ANOVA analysis and a Tukey pairwise comparison test (p-value set at 0.05).
Sensor-placement control experiment 1 gave a CV < 5% and experiment 2 a CV < 10% for the mean of the norm of the acceleration in the horizontal plane and the RMS of the norm of the acceleration in the horizontal plane (Table 3).
Table 3. Sensor-placement control experiment 1 (Exp. 1): coefficient of variation (CV; mean/SD) of the mean and root mean square (RMS) of the norm for acceleration in the horizontal plane in the right foot for 2 subjects over 5 walking trials with renewal of the sensor placement at each trial.
Sensor-placement control experiment 2 (Exp. 2): CV over 9 walking trials (-20; -15; -10; -5; 0; 5; 10; 15; 20 mm) with displacement of the sensor in increments of 5 mm along the antero-posterior axis and medio-lateral axis in terms of the reference position. Values are in percentages.
| Mean | RMS | ||
|---|---|---|---|
| Exp. 1 | Subject 1 | 3.5* | 4.3* |
| Subject 2 | 0.9* | 2.1* | |
| Exp. 2 | Subject 1 | 7.4 | 8.9 |
| Subject 2 | 2.9* | 4.0* | |
* CV < 5%.
Discussion
The correlation between lower limb osteoarthritis severity and stereophotogrammetry is well established [5,26,27,51–57]. In contrast, only two studies retrieved the same correlation using inertial sensors [52,54]. We confirm that result here. In addition, to the best of our knowledge, it is the first lower limb osteoarthritis study where the IMU-based gait parameters were extracted without step detection, which is important for daily clinical use. Finally, our results suggest that two IMUs placed on the feet are sufficient to quantify the severity of inferior limb osteoarthritis, which further improves the use of the method in daily practice.
We compared 48 patients and 12 control subjects walking 10 meters forward and 10 meters back under clinical consultation conditions. The four-IMUs-based method showed a discrimination capacity of clinical severity groups for 4 of the 60 parameters tested. These discriminating parameters were: mean and RMS of the norm of the acceleration in the horizontal plane in the doctor’s office linked frame for the contralateral and the ipsilateral feet. The results remained statistically significant with BMI and age as covariate. The absence of clinical correlation with parameters in the head and lower back reflected that lower limb osteoarthritis impacted the kinematics of the painful segment more than the upper body, which, to the best of our knowledge, has not been specifically shown previously [1,12,56,58–61]. However, it cannot be excluded that a more precise method of measurement, such as stereophotogrammetry, could reveal subtle differences. It remains that one important conclusion would be that two sensors placed at the feet, would be sufficient in daily practice to rate osteoarthritis severity.
Walking speed is known to influence gait parameters [62] and osteoarthritis reduces walking speed. Hence, the question is whether the influence of osteoarthritis severity on the gait parameters was solely caused by the reduction of walking speed, or if osteoarthritis per se led to a change of gait pattern. To analyze the change of walking pattern independently from the walking speed, a first method is to walk at a predetermined walking speed [1,3,12,33,56,58,63–65]. It requires dedicated material (treadmill), which is not suited in daily clinical practice and it does not allow to capture natural and repeatable walking patterns [25]. A second method is to select subgroups of participants walking at their preferred walking speed matched in walking speed [66]. But, the subgroups do not reflect the general populations of the whole severity groups [25]. A third method would be to set walking speed as covariate [63,67,68]. As walking speed is inherently linked to disease progress, and its mean value tends to decrease with increasing levels of disease severity, this technique is inappropriate [25]. Therefore, we chose to have participant walking at preferred walking speeds. Using that method, we showed on our dataset that walking velocity was not a discriminating parameter when comparing G0 and G1. Altogether, this negative result suggests that osteoarthritis per se caused a change of gait pattern, independent from the walking velocity. Pain could likely be a factor.
Our method gave a global view of the gait kinematics, which summed up the impacts of ostheoarthritis at the hip, knee and ankle joints levels. Also, ipsilateral and contralateral sides were defined with respect to the more symptomatic side of the patient. Therefore, our approach may help to objectively rate lower limb osteoarthritis severity in daily clinical practice but it is not suited to gain a detailed insight in the walking pattern of these patients [52].
The manual phase annotation of the walking exercise we used saved time but could have lowered the robustness of our method. However, we showed that the errors due to manual annotation didn’t change the statistical validity of the discriminating parameters in our study. Computation of gait parameters in the sensor-linked frame is prone to lower the reproducibility of the parameters because it is biased by the inherent variability of the positions of the sensors [44,69]. This explains why in our study, robust discriminating accelerometric parameters for lower limb osteoarthritis severity were all found in the doctor’s office linked frame.
Two aspects of the positioning of the sensors may affect gait parameters by using IMUs: the orientation and position of the sensor on the measured body segment [70–73]. In the present study, all discriminating parameters were computed from the laboratory frame (i.e. the frame in which the vertical axis and horizontal plane are independent of the initial orientation of the sensor). Nevertheless, with the effect of the position of the sensor on the body segment, the CV was < 5% for our discriminating parameters, for realistic placement errors (we estimated our error as routine to be about 10 mm), and < 10% for extreme placement errors. Indeed, special care is needed for placement of the sensor, but this positioning had moderate impact on the parameters we propose.
We compared the IMU-based gait parameters and lower limb osteoarthritis assessed by the WOMAC index, which is a purely clinical score. Classically, inertial sensor based studies use the Kellgren and Lawrence radiographic score to rate knee osteoarthritis [5,26,27,53–57]. Radiographic knee osteoarthritis severity is known to have poor correlation with the clinic namely gait disturbance [74,75]. Radiographic osteoarthritis can be clinically silent [26], which could explain the inconsistent correlation between gait analysis and radiographic-based lower limb osteoarthritis severity [59]. Again, it can be hypothesized that pain commands walking strategies.
Finally, beyond the fact that we designed an automated method of gait quantification, adapted to daily practice, our results gave some insight in the impact of lower limb osteoarthritis on locomotion. The most relevant results of our study are the decrease of the mean and RMS of norm of the acceleration in the horizontal plane on both feet with disease severity. It could result from a diminution of movement in the AP direction due to pain. This interpretation had been suggested in studies relying on local peak amplitudes [13,54,76,77]. Liikavainio et al. (2010) have also hypothesized that patients use a different strategy to brake the forward movement of the swinging leg before floor contact. This strategy could explain both the reduction of our global parameters and the increase of the local peaks in patients reported by others.
Conclusion
Our study showed that by using two IMUs placed on both feet and a signal processing method without step detection, we could objectively quantify limp in lower-limb osteoarthritis. This finding underlines the importance of measuring key anatomical landmarks and accessible gait parameters in exploring limp by using IMUs and severity grading. Although the proposed method still had some limitations, it provided new, automatically computed parameters that could be used for the comprehension of lower limb osteoarthritis in current medical practice. It may not only be used in medical consultation to score patients, but also to monitor the evolution of their clinical syndrome during and after rehabilitation. Finally, it paves the way for the quantification of gait in other fields such as neurology and for home monitoring.
Supporting Information
Each parameter is defined by: a sensor = {head, lower back, ipsilateral foot, contralateral foot}; a frame = {sensor, office}; an axis = {AP,ML,V} if the frame is the sensor-linked frame or an axis = {H, V} if the frame is the doctor’s office-linked frame (H for horizontal plane); a signal sig = {acceleration, angular velocity} and a statistical tool stat = {mean, RMS}. The parameter ipsilateral foot-office-H-acceleration-mean-modified corresponds to the parameter ipsilateral foot-office-H-acceleration-mean computed with the cumulative error for the manual exercise phase annotation that was estimated at 1 second. Accelerations are given in g and angular velocities in deg/s. AP antero-posterior, ML medio-lateral, V vertical, H horizontal plane, RMS root mean square, BMI body mass index.
(XLSX)
Acknowledgments
Blynn Shideler for writing assistance.
SATT Ile-de-France Innov for funding.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
SATT Innov Ile de France. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Childs JD, Sparto PJ, Fitzgerald GK, Bizzini M, Irrgang JJ. Alterations in lower extremity movement and muscle activation patterns in individuals with knee osteoarthritis. Clin Biomech 2004;19:44–9. [DOI] [PubMed] [Google Scholar]
- 2.McKean KA, Landry SC, Hubley-Kozey CL, Dunbar MJ, Stanish WD, Deluzio KJ. Gender differences exist in osteoarthritic gait. Clin Biomech 2007;22:400–9. 10.1016/j.clinbiomech.2006.11.006 [DOI] [PubMed] [Google Scholar]
- 3.Astephen JL, Deluzio KJ, Caldwell GE, Dunbar MJ, Hubley-kozey CL. Gait and neuromuscular pattern changes are associated with differences in knee osteoarthritis severity levels. J Biomech 2008;41:868–76. 10.1016/j.jbiomech.2007.10.016 [DOI] [PubMed] [Google Scholar]
- 4.Andriacchi TP, Hurwitz DE. Gait biomechanics and the evolution of total joint replacement. Gait Posture 1997;5:256–64. 10.1016/S0966-6362(97)00013-1 [DOI] [Google Scholar]
- 5.Tas S. Effects of severity of osteoarthritis on the temporospatial gait parameters in patients with knee osteoarthritis. ACTA Orthop Traumatol Turc 2014;48:635–41. 10.3944/AOTT.2014.13.0071 [DOI] [PubMed] [Google Scholar]
- 6.Astephen JL, Deluzio KJ. Changes in frontal plane dynamics and the loading response phase of the gait cycle are characteristic of severe knee osteoarthritis application of a multidimensional analysis technique. Clin Biomech 2005;20:209–17. [DOI] [PubMed] [Google Scholar]
- 7.Brinkmann JR, Perry J. Rate and range of knee motion during ambulation in healthy and arthritic subjects. Phys Ther 1985;65:1055–60. [DOI] [PubMed] [Google Scholar]
- 8.Hanlon M, Anderson R. Prediction methods to account for the effect of gait speed on lower limb angular kinematics. Gait Posture 2006;24:280–7. 10.1016/j.gaitpost.2005.10.007 [DOI] [PubMed] [Google Scholar]
- 9.Chen CPC, Chen MJL, Pei Y-C, Lew HL, Wong P-Y, Tang SFT. Sagittal plane loading response during gait in different age groups and in people with knee osteoarthritis. Am J Phys Med Rehabil 2003;82:307–12. 10.1097/01.PHM.0000056987.33630.56 [DOI] [PubMed] [Google Scholar]
- 10.Stauffer RN, Chao EYS, Györy AN. Biomechanical gait analysis of the diseased knee joint. Clin Orthop Relat Res 1977;126:246–55. [PubMed] [Google Scholar]
- 11.Smith AJ, Lloyd DG, Wood DJ. Pre-surgery knee joint loading patterns during walking predict the presence and severity of anterior knee pain after total knee arthroplasty. J Orthop Res 2004;22:260–6. 10.1016/S0736-0266(03)00184-0 [DOI] [PubMed] [Google Scholar]
- 12.Baliunas AJ, Hurwitz DE, Ryals AB, Karrar A, Case JP, Block JA, et al. Increased knee joint loads during walking are present in subjects with knee osteoarthritis. Osteoarthr Cartil 2002;10:573–9. [DOI] [PubMed] [Google Scholar]
- 13.Turcot K, Aissaoui R, Boivin K, Pelletier M, Hagemeister N, de Guise JA. New accelerometric method to discriminate between asymptomatic subjects and patients with medial knee osteoarthritis during 3-D gait. Biomed Eng IEEE Trans 2008;55:1415–22. [DOI] [PubMed] [Google Scholar]
- 14.Sharma L, Kapoor D, Issa S. Epidemiology of osteoarthritis: an update. Curr Opin Rheumatol 2006;18:147–56. 10.1097/01.bor.0000209426.84775.f8 [DOI] [PubMed] [Google Scholar]
- 15.Herzog W, Federico S. Considerations on joint and articular cartilage mechanics. Biomech Model Mechanobiol 2006;5:64–81. 10.1007/s10237-006-0029-y [DOI] [PubMed] [Google Scholar]
- 16.McConnell S, Kolopack P, Davis AM. The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC): A Review of Its Utility and Measurement Properties. Arthritis Care Res (Hoboken) 2001:453–61. [DOI] [PubMed] [Google Scholar]
- 17.Roos EM, Klässbo M, Lohmander LS. WOMAC Osteoarthritis Index: Reliability, validity, and responsiveness in patients with arthroscopically assessed osteoarthritis. Scand J Rheumatol 1999;28:210–5. [DOI] [PubMed] [Google Scholar]
- 18.Bellamy N. Pain assessment in osteoarthritis: experience with the WOMAC osteoarthritis index. Semin Arthritis Rheum 1989;18:14–7. [DOI] [PubMed] [Google Scholar]
- 19.Angst F, Aeschlimann A, Steiner W, Stucki G. Responsiveness of the WOMAC osteoarthritis index as compared with the SF-36 in patients with osteoarthritis of the legs undergoing a comprehensive rehabilitation intervention. Ann Rheumatolgic Disord 2001:834–40. [PMC free article] [PubMed] [Google Scholar]
- 20.Theiler R, Sangha O, Schaeren S, Michel BA, Tyndall A, Dick W, et al. Superior responsiveness of the pain and function sections of WOMAC Index as compared to the Lequesne-algofunctional Index in patients with osteoarthritis of the lower extremities. Osteoarthr Cartil 1999:515–9. 10.1053/joca.1999.0262 [DOI] [PubMed] [Google Scholar]
- 21.Witvrouw E, Victor J, Bellemans J, Rock B, Van Lummel R, Van Der Slikke R, et al. A correlation study of objective functionality and WOMAC in total knee arthroplasty. Knee Surgery, Sport Traumatol Arthrosc 2002;10:347–51. 10.1007/s00167-002-0302-2 [DOI] [PubMed] [Google Scholar]
- 22.Lindemann U, Becker C, Muche R, Aminian K, Dejnabadi H, Nikolaus T, et al. Gait analysis and WOMAC are complementary in assessing functional outcome in total hip replacement. Clin Rehabil 2006;20:413–20. [DOI] [PubMed] [Google Scholar]
- 23.Hubble RP, Naughton G a., Silburn P a., Cole MH. Wearable Sensor Use for Assessing Standing Balance and Walking Stability in People with Parkinson’s Disease: A Systematic Review. PLoS One 2015;10:e0123705 10.1371/journal.pone.0123705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Auvinet B, Berrut G, Touzard C, Moutel L, Collet N, Chaleil D, et al. Reference data for normal subjects obtained with an accelerometric device. Gait Posture 2002;16:124–34. [DOI] [PubMed] [Google Scholar]
- 25.Astephen Wilson JL. Challenges in dealing with walking speed in knee osteoarthritis gait analyses. Clin Biomech 2012;27:210–2. 10.1016/j.clinbiomech.2011.09.009 [DOI] [PubMed] [Google Scholar]
- 26.Nagano Y, Naito K, Saho Y, Torii S, Ogata T, Nakazawa K, et al. Association between in vivo knee kinematics during gait and the severity of knee osteoarthritis. Knee 2012;19:628–32. 10.1016/j.knee.2011.11.002 [DOI] [PubMed] [Google Scholar]
- 27.Kiss RM. Effect of severity of knee osteoarthritis on the variability of gait parameters. J Electromyogr Kinesiol 2011;21:695–703. 10.1016/j.jelekin.2011.07.011 [DOI] [PubMed] [Google Scholar]
- 28.Mizuike C, Ohgi S, Morita S. Analysis of stroke patient walking dynamics using a tri-axial accelerometer. Gait Posture 2009;30:60–4. 10.1016/j.gaitpost.2009.02.017 [DOI] [PubMed] [Google Scholar]
- 29.Van Den Noort JC, Van Der Esch M, Steultjens MPM, Dekker J, Schepers HM, Veltink PH, et al. The knee adduction moment measured with an instrumented force shoe in patients with knee osteoarthritis. J Biomech 2012;45:281–8. 10.1016/j.jbiomech.2011.10.027 [DOI] [PubMed] [Google Scholar]
- 30.Freedman Silvernail J, Milner CE, Thompson D, Zhang S, Zhao X. The influence of body mass index and velocity on knee biomechanics during walking. Gait Posture 2013;37:575–9. 10.1016/j.gaitpost.2012.09.016 [DOI] [PubMed] [Google Scholar]
- 31.Heiden TL, Lloyd DG, Ackland TR. Knee joint kinematics, kinetics and muscle co-contraction in knee osteoarthritis patient gait. Clin Biomech 2009;24:833–41. [DOI] [PubMed] [Google Scholar]
- 32.Jordan K, Challis JH, Newell KM. Walking speed influences on gait cycle variability. Gait Posture 2007;26:128–34. 10.1016/j.gaitpost.2006.08.010 [DOI] [PubMed] [Google Scholar]
- 33.Landry SC, McKean KA, Hubley-Kozey CL, Stanish WD, Deluzio KJ. Knee biomechanics of moderate OA patients measured during gait at a self-selected and fast walking speed. J Biomech 2007;40:1754–61. 10.1016/j.jbiomech.2006.08.010 [DOI] [PubMed] [Google Scholar]
- 34.Ying H, Silex C, Schnitzer a, Leonhardt S, Schiek M. Automatic Step Detection in the Accelerometer Signal. 4th Int Work Wearable Implant Body Sens Networks (BSN 2007) 2007;13:80–5. 10.1007/978-3-540-70994-7_14 [DOI] [Google Scholar]
- 35.Pan J, Tompkins WJ. A real-time QRS detection algorithm. IEEE Trans Biomed Eng 1985;32:230–6. 10.1109/TBME.1985.325532 [DOI] [PubMed] [Google Scholar]
- 36.Marschollek M, Goevercin M, Wolf K-H, Song B, Gietzelt M, Haux R, et al. A performance comparison of accelerometry-based step detection algorithms on a large, non-laboratory sample of healthy and mobility-impaired persons. Eng. Med. Biol. Soc. 2008. EMBS 2008. 30th Annu. Int. Conf. IEEE, 2008, p. 1319–22. [DOI] [PubMed] [Google Scholar]
- 37.Dijkstra B, Zijlstra W, Scherder E, Kamsma Y. Detection of walking periods and number of steps in older adults and patients with Parkinson’s disease: Accuracy of a pedometer and an accelerometry-based method. Age Ageing 2008;37:436–41. 10.1093/ageing/afn097 [DOI] [PubMed] [Google Scholar]
- 38.Fortune E, Lugade V, Morrow M, Kaufman K. Step Counts Using a Tri-Axial Accelerometer During Activity. AsbwebOrg n.d.:1–2.
- 39.Libby R. A simple method for reliable footstep detection on embedded sensor platforms. Sensors Peterbrgh NH 2008:1–16. [Google Scholar]
- 40.Thuer G, Verwimp T. Step Detection Algorithms for Accelerometers. E-Lab Master’s Thesis, from Artesis Univ Coll Antwerp, Antwerp, Belgium 2009;2009:1–8.
- 41.Sejdić Ervin, Lowry KA, Bellanca J, Redfern MS, Brach JS. A comprehensive assessment of gait accelerometry signals in time, frequency and time-frequency domains. IEEE Trans Neural Syst Rehabil Eng 2015;22:603–12. 10.1109/TNSRE.2013.2265887.A [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Din S Del, Godfrey A, Galna B, Lord S, Rochester L. Free-living gait characteristics in ageing and Parkinson ‘ s disease: impact of environment and ambulatory bout length. J Neuroeng Rehabil 2016:1–12. 10.1186/s12984-016-0154-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Barrois R, Oudre L, Moreau T, Truong C, Vayatis N, Buffat S, et al. Quantify osteoarthritis gait at the doctor ‘ s office: A simple pelvis accelerometer based method independent from footwear and aging. Comput Methods Biomech Biomed Engin 2015:1880–1. 10.1080/10255842.2015.1072414 [DOI] [PubMed] [Google Scholar]
- 44.Moe-Nilssen R. A new method for evaluating motor control in gait under real-life environmental conditions. Part 1: The instrument. Clin Biomech 1998;13:320–7. [DOI] [PubMed] [Google Scholar]
- 45.Bolink SAAN, Lenguerrand E, Brunton LR, Wylde V, Gooberman-hill R, Heyligers IC, et al. Clinical Biomechanics Assessment of physical function following total hip arthroplasty: Inertial sensor based gait analysis is supplementary to patient-reported outcome measures. JCLB 2016;32:171–9. 10.1016/j.clinbiomech.2015.11.014 [DOI] [PubMed] [Google Scholar]
- 46.Bolink SAAN, Brunton LR, Laarhoven S van, Lipperts M, Heyligers IC, Blom AW, et al. Frontal plane pelvic motion during gait captures hip osteoarthritis related disability. Hip Int 2016;0:0–0. 10.5301/hipint.5000282 [DOI] [PubMed] [Google Scholar]
- 47.Bolink SAAN, Grimm B, Heyligers IC. The Knee Patient-reported outcome measures versus inertial performance-based outcome measures: A prospective study in patients undergoing primary total knee arthroplasty. Knee 2015;22:618–23. 10.1016/j.knee.2015.04.002 [DOI] [PubMed] [Google Scholar]
- 48.Staab W, Hottowitz R, Sohns C, Sohns JM, Gilbert F, Menke J, et al. Accelerometer and Gyroscope Based Gait Analysis Using Spectral Analysis of Patients with Osteoarthritis of the Knee. J Phys Ther Sci 2014;26:997–1002. 10.1589/jpts.26.997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Madgwick SOH. An efficient orientation filter for inertial and inertial/magnetic sensor arrays. Rep X-Io Univ Bristol 2010:32. doi: 10.1109/ICORR.2011.5975346 [DOI] [Google Scholar]
- 50.Cognolato M. Experimental validation of XSens inertial sensor during clinical and sport motion capture. 2012.
- 51.Astephen JL, Deluzio KJ, Caldwell GE, Dunbar MJ, Hubley-Kozey CL. Gait and neuromuscular pattern changes are associated with differences in knee osteoarthritis severity levels. J Biomech 2008;41:868–76. 10.1016/j.jbiomech.2007.10.016 [DOI] [PubMed] [Google Scholar]
- 52.Brandes M, Schomaker R, Molenhoff G, Rosenbaum D. Quantity versus quality of gait and quality of life in patients with osteoarthritis. Gait Posture 2008;28:74–9. 10.1016/j.gaitpost.2007.10.004 [DOI] [PubMed] [Google Scholar]
- 53.Huang SC, Wei IP, Chien HL, Wang TM, Liu YH, Chen HL, et al. Effects of severity of degeneration on gait patterns in patients with medial knee osteoarthritis. Med Eng Phys 2008;30:997–1003. 10.1016/j.medengphy.2008.02.006 [DOI] [PubMed] [Google Scholar]
- 54.Liikavainio T, Bragge T, Hakkarainen M, Karjalainen PA, Arokoski JP. Gait and muscle activation changes in men with knee osteoarthritis. Knee 2010;17:69–76. 10.1016/j.knee.2009.05.003 [DOI] [PubMed] [Google Scholar]
- 55.Mündermann A, Dyrby CO, Hurwitz DE, Sharma L, Andriacchi TP. Potential Strategies to Reduce Medial Compartment Loading in Patients With Knee Osteoarthritis of Varying Severity: Reduced Walking Speed. Arthritis Rheum 2004;50:1172–8. 10.1002/art.20132 [DOI] [PubMed] [Google Scholar]
- 56.Mündermann A, Dyrby CO, Andriacchi TP. Secondary gait changes in patients with medial compartment knee osteoarthritis: increased load at the ankle, knee, and hip during walking. Arthritis Rheum 2005;52:2835–44. 10.1002/art.21262 [DOI] [PubMed] [Google Scholar]
- 57.Zeni JA, Higginson JS. Differences in gait parameters between healthy subjects and persons with moderate and severe knee osteoarthritis: a result of altered walking speed? Clin Biomech 2009;24:372–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gök H, Ergin S, Yavuzer G. Kinetic and kinematic characteristics of gait in patients with medial knee arthrosis. Acta Orthop 2002;73:647–52. [DOI] [PubMed] [Google Scholar]
- 59.Heiden TL, Lloyd DG, Ackland TR. Knee joint kinematics, kinetics and muscle co-contraction in knee osteoarthritis patient gait. Clin Biomech 2009;24:833–41. 10.1016/j.clinbiomech.2009.08.005 [DOI] [PubMed] [Google Scholar]
- 60.Hinman RS, Bennell KL, Metcalf BR, Crossley KM. Delayed onset of quadriceps activity and altered knee joint kinematics during stair stepping in individuals with knee osteoarthritis. Arch Phys Med Rehabil 2002;83:1080–6. 10.1053/apmr.2002.33068 [DOI] [PubMed] [Google Scholar]
- 61.Turcot K, Aissaoui R, Boivin K, Hagemeister N, Pelletier M, de Guise JA. Test-Retest Reliability and Minimal Clinical Change Determination for 3-Dimensional Tibial and Femoral Accelerations During Treadmill Walking in Knee Osteoarthritis Patients. Arch Phys Med Rehabil 2008;89:732–7. 10.1016/j.apmr.2007.09.033 [DOI] [PubMed] [Google Scholar]
- 62.Hirasaki E, Moore ST, Raphan T, Cohen B. Effects of walking velocity on vertical head and body movements during locomotion. Exp Brain Res 1999;127:117–30. [DOI] [PubMed] [Google Scholar]
- 63.Kaufman KR, Hughes C, Morrey BF, Morrey M, An K-N. Gait characteristics of patients with knee osteoarthritis. J Biomech 2001;34:907–15. [DOI] [PubMed] [Google Scholar]
- 64.Al-Zahrani KS, Bakheit AMO. A study of the gait characteristics of patients with chronic osteoarthritis of the knee. Disabil Rehabil 2002;24:275–80. [DOI] [PubMed] [Google Scholar]
- 65.Hurwitz DE, Ryals AB, Case JP, Block JA, Andriacchi TP. The knee adduction moment during gait in subjects with knee osteoarthritis is more closely correlated with static alignment than radiographic disease severity, toe out angle and pain. J Orthop Res 2002;20:101–7. 10.1016/S0736-0266(01)00081-X [DOI] [PubMed] [Google Scholar]
- 66.Rutherford DJ, Hubley-Kozey CL, Stanish WD, Dunbar MJ. Neuromuscular alterations exist with knee osteoarthritis presence and severity despite walking velocity similarities. Clin Biomech 2011;26:377–83. 10.1016/j.clinbiomech.2010.11.018 [DOI] [PubMed] [Google Scholar]
- 67.Zeni JA, Richards JG, Higginson JS. Two simple methods for determining gait events during treadmill and overground walking using kinematic data. Gait Posture 2008;27:710–4. 10.1016/j.gaitpost.2007.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Lewek MD, Rudolph KS, Snyder-Mackler L. Control of frontal plane knee laxity during gait in patients with medial compartment knee osteoarthritis. Osteoarthr Cartil 2004;12:745–51. 10.1016/j.joca.2004.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kavanagh JJ, Menz HB. Accelerometry: a technique for quantifying movement patterns during walking. Gait Posture 2008;28:1–15. 10.1016/j.gaitpost.2007.10.010 [DOI] [PubMed] [Google Scholar]
- 70.Moe-Nilssen R. Test-retest reliability of trunk accelerometry during standing and walking. Arch Phys Med Rehabil 1998;79:1377–85. 10.1016/S0003-9993(98)90231-3 [DOI] [PubMed] [Google Scholar]
- 71.Sabatini AM. Wearable sensor systems in biomechanics: assessment of unrestrained walking features. Instrum. Meas. Technol. Conf. 2004. IMTC 04. Proc. 21st IEEE, vol. 2, 2004, p. 881–3.
- 72.Henriksen M, Lund H, Moe-Nilssen R, Bliddal H, Danneskiod-Samsøe B. Test—retest reliability of trunk accelerometric gait analysis. Gait Posture 2004;19:288–97. 10.1016/S0966-6362(03)00069-9 [DOI] [PubMed] [Google Scholar]
- 73.Kavanagh JJ, Menz HB. Accelerometry: A technique for quantifying movement patterns during walking. Gait Posture 2008;28:1–15. 10.1016/j.gaitpost.2007.10.010 [DOI] [PubMed] [Google Scholar]
- 74.Hannan MT, Felson DT, Pincus T. Analysis of the discordance between radiographic changes and knee pain in osteoarthritis of the knee. J Rheumatol 2000;27:1513–7. [PubMed] [Google Scholar]
- 75.Dieppe PA. Relationship between symptoms and structural change in osteoarthritis. what are the important targets for osteoarthritis therapy? J Rheumatol 2004:50–3. [PubMed] [Google Scholar]
- 76.Lafortune MA. Three-dimensional acceleration of the tibia during walking and running. J Biomech 1991;24:877–86. [DOI] [PubMed] [Google Scholar]
- 77.Liikavainio T, Isolehto J, Helminen HJ, Perttunen J, Lepola V, Kiviranta I, et al. Loading and gait symmetry during level and stair walking in asymptomatic subjects with knee osteoarthritis: importance of quadriceps femoris in reducing impact force during heel strike? Knee 2007;14:231–8. 10.1016/j.knee.2007.03.001 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Each parameter is defined by: a sensor = {head, lower back, ipsilateral foot, contralateral foot}; a frame = {sensor, office}; an axis = {AP,ML,V} if the frame is the sensor-linked frame or an axis = {H, V} if the frame is the doctor’s office-linked frame (H for horizontal plane); a signal sig = {acceleration, angular velocity} and a statistical tool stat = {mean, RMS}. The parameter ipsilateral foot-office-H-acceleration-mean-modified corresponds to the parameter ipsilateral foot-office-H-acceleration-mean computed with the cumulative error for the manual exercise phase annotation that was estimated at 1 second. Accelerations are given in g and angular velocities in deg/s. AP antero-posterior, ML medio-lateral, V vertical, H horizontal plane, RMS root mean square, BMI body mass index.
(XLSX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.