Abstract
Introduction
Patient-care workers are frequently exposed to sharps injuries, which can involve the risk of serious illness. Underreporting of these injuries can compromise prevention efforts.
Materials and Methods
We linked survey responses of 1572 non-physician patient-care workers with the Occupational Health Services (OHS) database at two academic hospitals. We determined whether survey respondents who said they had sharps injuries indicated that they had reported them and whether reported injuries were recorded in the OHS database.
Results
Respondents said that they reported 62 of 78 sharps injuries occurring over a 12-month period. Only 28 appeared in the OHS data. Safety practices were positively associated with respondents’ saying they reported sharps injuries but not with whether reported injuries appeared in the OHS data.
Conclusions
Administrators should consider creating reporting mechanisms that are simpler and more direct. Administrators and researchers should attempt to understand how incidents might be lost before they are recorded.
Keywords: surveillance, occupational injuries, sharps injuries, hospital incident reporting, underreporting
INTRODUCTION
Hospitals are known to have high injury rates [Bureau of Labor Statistics 2012], with direct patient-care workers having high injury rates in general [Boden, et al. 2012, d'Errico, et al. 2007, Rodríguez-Acosta, et al. 2009] and high sharps (sharp medical devices such as needles) injury rates in specific [Laramie, et al. 2011, Quinn, et al. 2009]. Sharps injuries are preventable, and elimination of consequent bloodborne pathogen exposures is an important public health goal.
Questions have been raised about whether reported injury rates reflect actual injury experience. Underreporting of workplace injuries in the U.S. is well documented [Azaroff, et al. 2002, Boden and Ozonoff 2008, Rosenman, et al. 2006]. This is seen among health care workers in particular [Galizzi, et al. 2010] and specifically for musculoskeletal [Menzel 2008, Siddharthan, et al. 2006] and sharps injuries [Alvarado-Ramy, et al. 2003, Cutter and Jordan 2013, Doebbeling, et al. 2003, Elder and Paterson 2006, Osborne 2003, Panlilio, et al. 2004, Tandberg, et al. 1991, Voide, et al. 2012]. The published rates for underreporting sharps injuries vary substantially and are not based on directly comparing survey data with administrative data containing the same group of subjects. Examples of studies based on survey data alone include a study of emergency health care workers that concluded that only 35% of sharps exposures were reported [Tandberg, et al. 1991] and a Swiss study that determined that 73.1% of health care workers reported their sharps exposures [Voide, et al. 2012]. British studies showed that there was as much as a ten-fold difference between injuries reported by survey compared to those based on standard reporting systems [Elder and Paterson 2006]. Factors associated with underreporting may include job insecurity [Azaroff, et al. 2002, Pransky, et al. 1999, Probst, et al. 2013], peer pressure not to report [Azaroff, et al. 2002], frustration with workers’ compensation procedures [Menzel 2008, Siddharthan, et al. 2006], and time pressure at work [Galizzi, et al. 2010, Probst and Graso 2013]. Underreporting has also been shown to be negatively associated with measures of safety climate [Probst, et al. 2008, Probst and Estrada 2010].
We surveyed non-physician patient-care workers including nurses and patient-care associates (aides) at two large academic hospitals in the metropolitan Boston area. We included questions asking them to tell us if they had experienced sharps injuries in the 12 months before they completed the survey and, if so, whether they had reported these injuries. Because we had access to hospitals’ electronic injury and illness database, we could then compare workers’ reports of these injuries with the administrative injury data. To our surprise, many of the injuries that workers said they reported were not included in the administrative data. This is the first study that we are aware of that examines whether workplace injuries that survey respondents indicated they reported could be found in their employer’s injury data.
Other survey questions provided measures of safety practices, staffing adequacy, and co-worker support. We examined whether these measures were related to injury reporting.
Reporting procedures
Both hospitals have standard policies and procedures requiring workers to report all work-related injuries and illnesses to their supervisors and to fill out a formal incident report by the day after the injury using a paper form or an electronic reporting system. This requirement is explained at new employee orientation. It covers both incidents considered recordable and non-recordable by the Occupational Safety and Health Administration (OSHA). Occupational Health Services (OHS) then enters this report into its database. Like OSHA, the Massachusetts Department of Public Health sharps surveillance program requires reporting of sharps-related incidents involving exposure to blood or other potentially infectious materials [Laramie, et al. 2011]. Incidents reported in this system are checked against the OHS data and added if missing from the latter.
If a worker is seen at the OHS and has not yet filled out an incident report, a nurse at the OHS will fill out a report at that time. In addition, the hospitals have backup procedures for directly calling OHS when standard procedures would be challenging, for example when an injury occurs in the operating room or during very busy times in the emergency room.
We note that injury reporting generally requires action by several people. First, the injured worker must report the injury, then the report must be forwarded to the people responsible for recordkeeping, and then the injury must be recorded. If anybody in this sequence of events does not move the process forward, the injury is not recorded.
MATERIALS AND METHODS
This study was conducted as part of the program of research of the Harvard School of Public Health Center for Work, Health and Wellbeing described in detail elsewhere [Hopcia, et al. 2012, Sorensen, et al. 2011]. The goal of these studies is to identify the relationships among worksite policies, programs and practices and worker health and economic outcomes. To this end, cross-sectional administrative and survey data from patient-care units of the two hospitals were collected. This study was approved by the Harvard School of Public Health Institutional Review Board. All subjects provided signed informed consent,
Data
This study used data from the OHS injury and illness database, linked by a unique employee identifier with a survey of patient-care workers in the study hospitals. The study cohort of direct patient-care workers was identified using payroll data from 106 units at the two hospitals (55 at one and 51 at the other). Eligible staff worked at least 20 hours per week between October 1, 2008, and September 30, 2009. Additionally, temporary and agency staff were excluded due to the short-term nature of their work on specific units and their small numbers. The final cohort was coded with study identification numbers, and all personal identifying information was removed.
Administrative data
We extracted age, gender, race/ethnicity reported on the initial employment interview; date of hire of individual patient-care workers from the human resources database; and information on the number and types of jobs, job role and title, unit, and hours worked from the staffing database. We calculated job tenure (employment duration) as the study year (2009) minus the year of hire. We categorized tenure into two categories, 0–5 years (43% of the sample) and greater than 5 years.
We linked these data with the OHS database containing incident reports and workers’ compensation claims for the hospitals. Injury descriptors include employee identifier (the linking variable), date of injury, body parts affected, nature of injury, cause of injury, workers’ compensation medical, indemnity, administrative and legal costs, and whether OSHA regulations required reporting.
Survey data
The survey of patient-care workers was conducted between October 2009 and February 2010. We randomly selected 2000 of the 7019 eligible workers and invited them via e-mail to participate in the survey online. Subsequent invitations were conducted via email and postal mail with a survey and a return postage-paid envelope included. The 1572 surveys with at least 50% of the questions completed were included in the analysis for a response rate of 78.6%. Mean age was 41.7 for respondents and 41.8 for non-respondents. Response rates were 79.4% for females and 71.3% for males. They were 81.9% for white, non-Hispanic workers and 70.0% for others.
This study is based on sharps injuries described by the survey respondents as having occurred during the 12 months preceding the survey. For respondents who said they had experienced a sharps injury, we also asked whether they had reported the injury and, if not, why not. If injuries were reported by workers and recorded by OHS according to hospital policies, all sharps injuries should have been captured by the OHS database.
We examined the effects of worker perceptions of three organizational policies and practices on reporting: safety practices, co-worker support, and staffing adequacy. Each of these was measured by a scale derived from the survey of patient-care workers. These three measures are conceptually related to three factors that have been shown to be related to injury reporting: safety climate [Probst, et al. 2008, Probst and Estrada 2010], peer pressure not to report [Azaroff, et al. 2002], and time pressure at work [Galizzi, et al. 2010, Probst and Graso 2013]. The response scale for all items was a five-point scale. Final scales summed the scores for each item and divided by the number of items, so all scales ranged from 1 to 5.
The safety practices scale combined five items the Organizational Policies and Practices questionnaire [Amick III, et al. 2000] measuring safety diligence and safety training. These included: the identification and improvement of unsafe work conditions, housekeeping, action when safety rules are broken, whether supervisors confront and correct unsafe behaviors or hazards, and safety training of supervisors.
Perceived staffing adequacy was measured using four questions from the staffing adequacy subscale of the Nursing Work Index-Revised questionnaire [Aiken and Patrician 2000, Kim, et al. 2014]. The chosen items asked how often there had been enough patient-care workers, enough registered nurses, adequate support services, and enough time to discuss patient care workers with other staff.
Co-worker support was assessed using two items: “If needed, I can get support and help with my work from my co-workers,” and “The people I work with are helpful in getting the job done.” Both questions were adapted from the Job Content Questionnaire [Karasek, et al. 1998].
Data Analysis
We first identified sharps injuries recalled by survey respondents. Next, we identified those that respondents indicated that they had reported. For all survey respondents, we then examined the OHS data for the 12 months before they completed the survey to see if their sharps injuries were recorded in that database.
Other studies have noted that apparent underreporting may be the result of differential classification of injuries among data sources [Davis, et al. 2014, Wuellner and Bonauto 2014]. For workers with sharps injuries reported during the survey but apparently absent from the OHS database, we looked for cases in the OHS data that occurred up to 15 months before the survey that involved a cut or puncture or involved exposure to blood or other bodily fluids.
Finally, using logistic regression, we estimated associations between reporting and perceptions of safety practices, co-worker support, and staffing adequacy. All analyses were carried out using SAS Statistical software, version 9.2 (SAS Institute, Cary, NC).
RESULTS
Population characteristics and reported injuries
The average age of patient care workers among survey respondents was more than 40 years, and they were predominantly white and female. Of the survey respondents, 8.1 percent were patient care associates (PCAs) and 70.5 percent were nurses (Table I). During the study period, the 1572 surveyed workers indicated they had experienced 78 sharps injuries. According to the OHS database, however, these workers experienced only 32 sharps injuries.
Table I.
Sample Statistics (N=1572)
| Individual and Job Characteristics | N | Frequency (%) or Mean (SD) |
|---|---|---|
| Gender | ||
| Male | 1572 | 144 (9.2%) |
| Female | 1572 | 1428 (90.8%) |
| Race/Ethnicity | ||
| Other | 1572 | 367 (23.3%) |
| White, non-Hispanic | 1572 | 1205 (76.7%) |
| Age category | ||
| < 30 | 1572 | 324 (20.6%) |
| 30–39 | 1572 | 372 (23.7%) |
| 40–49 | 1572 | 393 (25.0%) |
| 50+ | 1572 | 483 (30.7%) |
| Age, years | 1572 | 41.7 (± 11.75) |
| Tenure | ||
| 0–5 years | 1572 | 674 (42.9%) |
| >5 years | 1572 | 898 (57.1%) |
| Occupation | ||
| Staff nurse | 1565 | 1103 (70.5%) |
| Patient care associate | 1565 | 127 (8.1%) |
| Other | 1565 | 335 (21.4%) |
| Perceived adequate staffing | 1522 | 3.7 (± 0.70) |
| Coworker Support | 1563 | 4.0 (± 0.75) |
| Safety practices scale | 1542 | 3.7 (± 0.66) |
| Injury Counts | ||
| Number of sharps injuries in OHS data | 28 | |
| Number of sharps injuries in Survey | 78 |
Relationship between survey and OHS sharps injuries
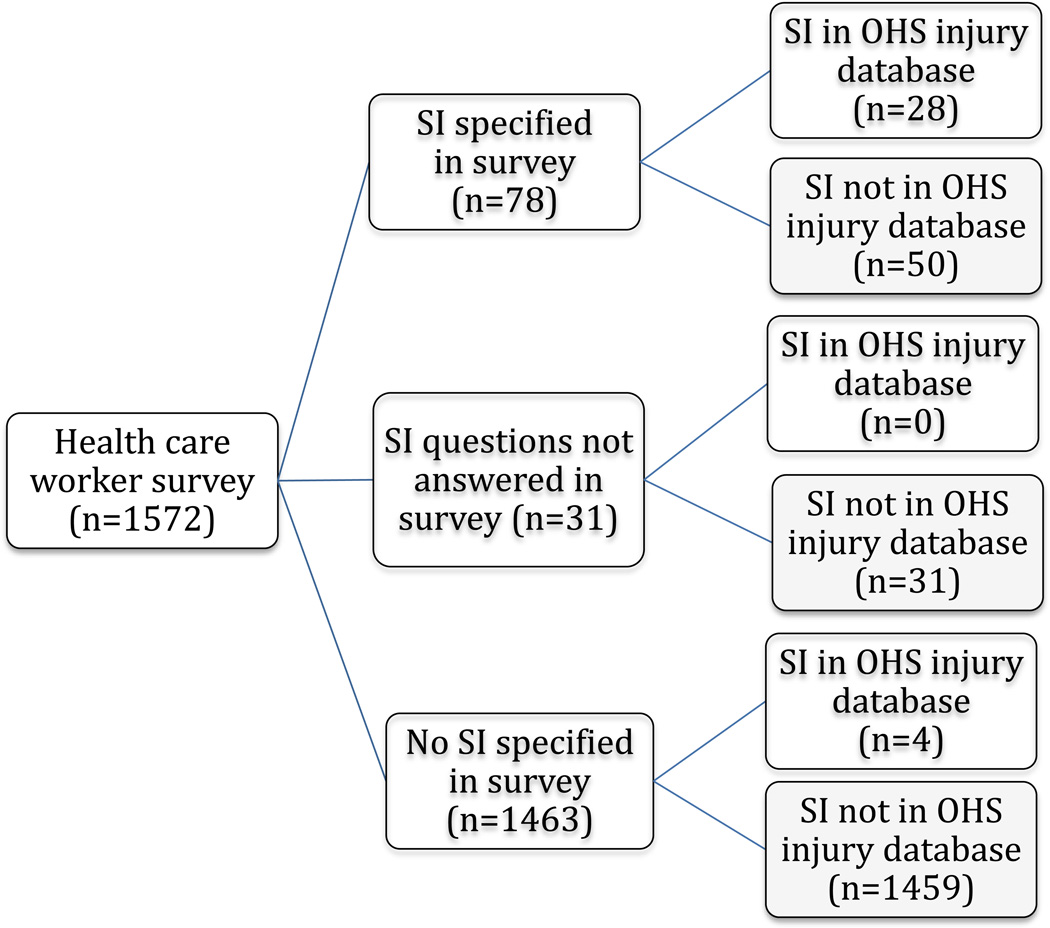
Figure 1 illustrates the relationship between sharps injuries reported in the survey and in the OHS data. Survey respondents said that they had reported 62 of the 78 sharps injuries they had experienced. Of these, we found only 28 in the OHS data. Four sharps injuries in the OHS data were not reported in the survey. One of these four was almost 11 months before the survey and may have been remembered by the respondent as outside the reporting frame, but the other three were within 6 months of the survey. Overall, there were 82 sharps injuries included in one or both sources. Of these, 32 (39%) were in the OHS data and 78 (95%) were in the survey.
Figure 1.
Sharps Injury (SI) Reporting in Survey and Occupational Health Service (OHS) Database
Figure 1 reveals an important inconsistency between the survey and OHS data. Survey respondents indicated that they reported 62 of 78 sharps injuries. However, only 28 of those actually appeared in the OHS data.
We attempted to see if sharps injuries respondents identified as occurring in the 12 months preceding the survey could be linked to earlier injuries or injuries classified as non-sharps in the OHS data. Among people who indicated they had sharps injuries in the survey, we found two OHS sharps injuries that occurred about 13 months before the survey date. For this group, three non-sharps cases in the OHS data involved exposure to bodily fluids (blood or urine splashes). The two OHS-reported injuries that occurred just outside the study period were not included in our data and thus might have been misclassified as unreported.
Impact of safety practices and other organizational factors on reporting
We next examined workplace characteristics that may influence the probability that an injury specified in the survey was reported. We hypothesized that positive perceptions of safety practices, staffing adequacy, and co-worker support would be associated with more complete reporting.
Using bivariate logistic regression, we examined associations between individual and organizational characteristics and whether survey respondents who said that they had sharps injuries also said that they reported them. We found that reporting a sharps injury was significantly associated with the safety practices measure and gender (Table II). Confidence intervals for the staffing adequacy and co-worker support measures included 1.0.
Table II.
Bivariate Logistic Estimates of Odds that Respondents said they Reported Sharps Injuries (n=78)
| Odds Ratio |
95% Confidence Interval |
|
|---|---|---|
| Gender female (vs. male) | 6.54 | 1.26 – 34.5 |
| Race/ethnicity white non-Hispanic (vs. Other) | 1.07 | 0.25 – 4.50 |
| Age category | ||
| 30–39 (vs. < 30) | 1.30 | 0.27 – 6.30 |
| 40–49 (vs. < 30) | 1.28 | 0.30 – 5.41 |
| 50+ (vs. < 30) | 1.20 | 0.25 – 5.86 |
| Tenure >5 years (vs. 0–5 years) | 2.64 | 0.75 – 9.26 |
| Occupation | ||
| Staff nurse (vs. other) | 1.00 | 0.23 – 4.27 |
| Patient-care associate (vs. other) | 0.75 | 0.09 – 5.96 |
| Safety practices scale | 2.82 | 1.19 – 6.72 |
| Coworker support | 1.67 | 0.76 – 3.69 |
| Perceived adequate staffing | 1.92 | 0.87 – 4.24 |
Number of subjects with missing data: 2 for safety practices, 5 for staffing adequacy, none for other variables.
There were too few sharps injuries to support stable multivariable estimates of reporting. However, to see whether confounding appeared to affect the bivariate results, we estimated multivariable logistic regressions, including race, gender, and the three organizational characteristics of interest. Confidence intervals became wider, as would be expected. The estimated odds ratios for safety practices (3.11) and co-worker support (1.75) exhibited little change. On the other hand, the estimated effect of staffing adequacy almost disappeared. (See Supplemental Table SI.)
We next used bivariate logistic regression to examine the association between individual and organizational characteristics and whether a sharps injury that respondents said they reported appeared in the OHS data. We found that presence of survey-reported sharps injuries in the OHS data had virtually no association with our safety practices measure (Table III). Both the co-worker support and adequate staffing measures had estimated odds ratios around 2.0, but confidence intervals included 1.0. Only race/ethnicity had a substantial and statistically significant odds ratio, with white, non-Hispanic workers indicating much more often that they reported their injuries. Estimates using multivariable logistic regression were similar. (See Supplemental Table SII.)
Table III.
Bivariate Logistic Estimates of Odds that Sharps Injuries that Respondents said they Reported Appear in OHS Data (n=62)*
| Odds Ratio |
95% Confidence Interval |
|
|---|---|---|
| Gender Male (vs. female)** | - | - |
| Race/Ethnicity White non-Hispanic (vs. Other) | 11.2 | 1.28 – 98.7 |
| Age Category | ||
| 30–39 (vs. < 30) | 0.94 | 0.27 – 4.04 |
| 40–49 (vs. < 30) | 1.05 | 0.27 – 4.03 |
| 50+ (vs. < 30) | 3.00 | 0.65 – 13.8 |
| Tenure >5 years (vs. 0–5 years) | 0.97 | 0.93 – 1.01 |
| Occupation | ||
| Staff Nurse (vs. Other) | 1.40 | 0.38 – 5.23 |
| Patient-care Associate (vs. Other) | 0.28 | 0.02 – 3.36 |
| Safety Practices Scale | 1.15 | 0.54 – 2.42 |
| Coworker Support | 2.18 | 0.92 – 5.17 |
| Perceived Adequate Staffing | 1.73 | 0.80 – 3.74 |
Number of subjects with missing data: 2 for safety practices, 5 for staffing adequacy, none for other variables.
Male respondents had no reported injuries in the OHS data.
We asked about reasons for not reporting sharps injuries (Table IV). Of the 16 people who said that they did not report a sharps injury, 15 responded to this question. The most common reasons for not reporting fell into two categories: the perception that the injury was not high risk and thinking that reporting took too much time (likely because taking the time to report conflicted with their patient care responsibilities). These are similar to reasons for not reporting reported for construction workers in Moore, et al. [2013]. Of course, these responses did not address why injuries that survey respondents said they reported did not appear in the OHS data.
Table IV.
Reasons for not Reporting Sharps Injuries (n=16)
| Reason | No | Yes | Total |
|---|---|---|---|
| I didn’t feel the patient and/or sharps injury was high risk | 6 | 8 | 14 |
| The reporting of sharps injuries takes too long | 8 | 7 | 15 |
| I was embarrassed that I had an injury | 11 | 4 | 15 |
| I didn’t want to disclose that I had the injury to my manager or peers | 11 | 3 | 14 |
| Nurse manager reprimands nurses who don’t use sharps devices correctly | 13 | 1 | 14 |
| I didn’t want to disclose that I didn’t use the safety devices | 14 | 0 | 14 |
Note: Totals not equal to 16 because of missing responses.
CONCLUSIONS
Injury reporting
This is the first study that we are aware of that examined whether workplace injuries that survey respondents indicated they reported could be found in employers’ injury data. It examined sharps injury reporting among patient care workers in two academic acute-care hospitals. We found that the hospitals’ administrative data captured only 36 percent of sharps injuries that survey respondents said they had experienced.
When we examined the relationship between survey responses and employer injury records, we found substantial disparities. Our results appear to confirm other studies’ findings that substantial numbers of injuries are not included in employer records. More than half of the sharps injuries that workers said they had reported did not appear in the OHS data. Moreover, the data reveal two sources of attrition: workers did not report some injuries, and some injuries that were reported were not recorded.
This study has several limitations. First, this is a study that is based on fewer than 100 sharps injuries in two academic hospitals. As such, it has limited power to support stable multivariable estimates of reporting behavior and possibly limited generalizability. Also, because it is cross-sectional, it is not possible to determine the direction of causality in the relationship between safety practices and reporting. However, the case for better organizational safety practices leading to more complete reporting seems more compelling than the converse. Finally, although the survey response rate was 79%, response rates differed between women and men and between white non-Hispanic workers and others.
There are a number of potential explanations for the reporting and reporting discrepancy that do not involve underreporting. First, people may have verbally reported an injury but incorrectly believed that completing an incident report was unnecessary unless they were at substantial risk. We note that 8 of 14 people who indicated why they didn’t report sharps injuries said that they didn’t think the injury was high risk (Table IV). Others who considered their injuries to be low risk may have verbally reported them but not completed the formal incident report.
Another possibility is that sharps injuries that occurred more than12 months before the survey were reported. We found two such cases that occurred between 12 and 15 months before the survey date.
A third possible explanation is that some respondents reported as sharps injuries exposures to bodily fluids that did not involve sharps. Among the 34 survey respondents lacking sharps injuries in the OHS data but who indicated that they had reported sharps injuries, three had non-sharps incidents involving exposure to bodily fluids (blood or urine splashes) in the OHS data. We think it is unlikely that these exposures would have been reported as sharps injuries on the survey but leave this as a possibility.
On the other hand, people may have reported sharps injuries that were not entered in the OHS data. They may have gone to the emergency room instead of OHS, believing that emergency room personnel would report the injury. However, by policy, reporting is the responsibility of the injured employee or that person’s supervisor, so no incident report would have been created. Alternatively, some may have reported the injury to their supervisors who failed to report the injury to OHS. A third possibility is that some employees called the OHS for advice and were advised to follow up by opening an incident report, but did not do so.
Organizational policies and practices and injury reporting
Safety climate has been shown in survey studies to be positively associated with injury reporting [Probst, et al. 2008, Probst and Estrada 2010]. When we used the survey data to indicate whether injured workers said they reported their sharps injuries, the estimated impact of safety practices on reporting was positive and statistically significant (Table II). However, we did not find an association between the safety practices measure and whether sharps injuries that respondents said they reported appeared in the OHS data (Table III). Instead, co-worker support and perceived staffing adequacy had substantial associations, although confidence intervals included 1.0. This suggests different processes are in play in the two stages of injury reporting and that different factors affect each.
Implications
Examining only survey responses or only administrative sources may not provide a good measure of reporting and may not tell the whole reporting story. In addition, for sharps injuries that workers say they reported, those of white non-Hispanic workers appear more likely than those of other workers to be recorded in hospitals’ administrative data. Thus, because of the loss of this information, surveillance-based prevention activities may pay inadequate attention to specific hazards faced disproportionately by non-white and Hispanic workers.
We have seen that, even in a setting with clear reporting roles and responsibilities, where workers receive training on injury reporting, reported injuries may not make it into the employer’s injury database. Administrators designing reporting systems should consider creating reporting mechanisms that are simpler and more direct. Initial reporting should be as easy, fast, and automatic as feasible. Effective reporting systems should make it difficult for information to be lost or misdirected. For example, an anonymous reviewer suggested providing a “single button” to push when a sharps injury occurs. This could provide time and location of injury and potentially provide employee identification. Follow-up for additional details could occur later.
Administrators and researchers analyzing reporting should attempt to understand each step in the reporting pathway and the ways in which incidents might be lost before they are recorded. Without more attention to the injury reporting pathway, too much may be left to chance.
Supplementary Material
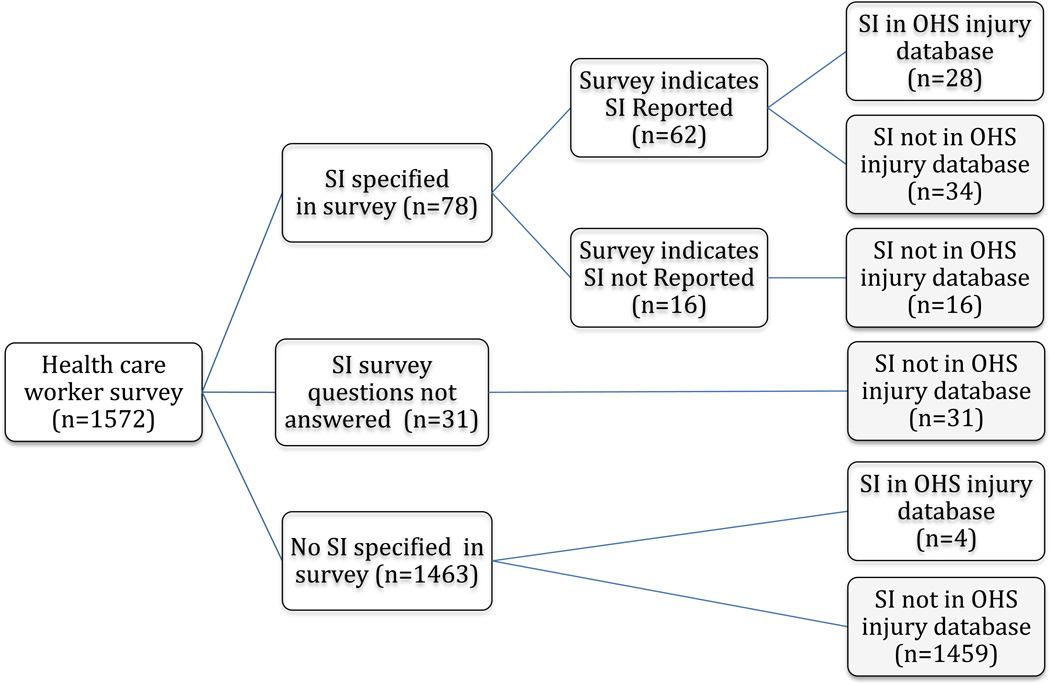
Figure 2.
Sharps Injury (SI) Reporting in Survey of Health Care Workers and Occupational Health Service (OHS) Database
Acknowledgments
The research was funded by the National Institute for Occupational Safety and Health, Grant 5U19 OH008861, the National Institute for Occupational Safety and Health Education and Research Center Grant T42 OH 008416-03, and the Occupational Physicians Scholarship Fund (American College of Occupational & Environmental Medicine). The views expressed here are not necessarily the views of either organization. This study was approved by the Harvard School of Public Health Institutional Review Board for protection of human subjects. All subjects provided written informed consent.
Contributor Information
Leslie I. Boden, Email: lboden@bu.edu, Boston University School of Public Health, Boston, Massachusetts.
Yolanta V. Petrofsky, Email: Yolanta.V.Petrofsky@kp.org, The Permanente Medical Group, Sacramento, California.
Karen Hopcia, Email: khopcia@uic.edu, University of Illinois at Chicago College of Nursing, Chicago, Illinois.
Gregory R. Wagner, Email: gwagner@cdc.gov, National Institute for Occupational Safety and Health, Washington, DC and Harvard School of Public Health, Boston, Massachusetts.
Dean Hashimoto, Email: dhashimoto@mgh.harvard.edu, Partners HealthCare System, Occupational Health Services, Boston, Massachusetts and Boston College Law School, Newton, Massachusetts.
REFERENCES
- Aiken LH, Patrician PA. Measuring organizational traits of hospitals: the Revised Nursing Work Index. Nurs Res. 2000;49:146–153. doi: 10.1097/00006199-200005000-00006. [DOI] [PubMed] [Google Scholar]
- Alvarado-Ramy F, Beltrami EM, Short LJ, Srivastava PU, Henry K, Mendelson M, Gerberding JL, Delclos GL, Campbell S, Solomon R. A comprehensive approach to percutaneous injury prevention during phlebotomy: results of a multicenter study, 1993–1995. Infect Control Hosp Epidemiol. 2003;24:97–104. doi: 10.1086/502179. [DOI] [PubMed] [Google Scholar]
- Amick BC, III, Habeck RV, Hunt A, Fossel AH, Chapin A, Keller RB, Katz JN. Measuring the impact of organizational behaviors on work disability prevention and management. J Occup Rehabil. 2000;10:21–38. [Google Scholar]
- Azaroff LS, Levenstein C, Wegman DH. Occupational injury and illness surveillance: Conceptual filters explain underreporting. American Journal of Public Health. 2002;92:1421–1429. doi: 10.2105/ajph.92.9.1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boden LI, Ozonoff A. Capture-recapture estimates of nonfatal workplace injuries and illnesses. Annals of Epidemiology. 2008;18:500–506. doi: 10.1016/j.annepidem.2007.11.003. [DOI] [PubMed] [Google Scholar]
- Boden LI, Sembajwe G, Tveito TH, Hashimoto D, Hopcia K, Kenwood C, Stoddard AM, Sorensen G. Occupational injuries among nurses and aides in a hospital setting. Am J Ind Med. 2012;55:117–126. doi: 10.1002/ajim.21018. [DOI] [PubMed] [Google Scholar]
- Bureau of Labor Statistics USDoL. Workplace Injuries and Illnesses -- 2011. Washington, DC: 2012. [Google Scholar]
- Cutter J, Jordan S. The systems approach to error reduction: factors influencing inoculation injury reporting in the operating theatre. Journal of nursing management. 2013;21:989–1000. doi: 10.1111/j.1365-2834.2012.01435.x. [DOI] [PubMed] [Google Scholar]
- d'Errico A, Punnett L, Cifuentes M, Boyer J, Tessler J, Gore R, Scollin P, Slatin C, Promoting H Safe Employment In Healthcare Research T. Hospital injury rates in relation to socioeconomic status and working conditions. Occup Environ Med. 2007;64:325–333. doi: 10.1136/oem.2006.027839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis LK, Grattan KM, Tak S, Bullock LF, Ozonoff A, Boden LI. Use of multiple data sources for surveillance of work-related amputations in Massachusetts, comparison with official estimates and implications for national surveillance. Am J Ind Med. 2014 doi: 10.1002/ajim.22327. [DOI] [PubMed] [Google Scholar]
- Doebbeling BN, Vaughn TE, McCoy KD, Beekmann SE, Woolson RF, Ferguson KJ, Torner JC. Percutaneous injury, blood exposure, and adherence to standard precautions: are hospital-based health care providers still at risk? Clin Infect Dis. 2003;37:1006–1013. doi: 10.1086/377535. [DOI] [PubMed] [Google Scholar]
- Elder A, Paterson C. Sharps injuries in UK health care: a review of injury rates, viral transmission and potential efficacy of safety devices. Occup Med (Lond) 2006;56:566–574. doi: 10.1093/occmed/kql122. [DOI] [PubMed] [Google Scholar]
- Galizzi M, Miesmaa P, Punnett L, Slatin C. Injured Workers’ Underreporting in the Health Care Industry: An Analysis Using Quantitative, Qualitative, and Observational Data. Ind Relat. 2010;49:22–43. doi: 10.1111/j.1468-232X.2009.00585.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopcia K, Dennerlein JT, Hashimoto D, Orechia MT, Sorensen G. A Case-Control Study of Occupational Injuries for Consecutive and Cumulative Shifts Among Hospital Registered Nurses and Patient Care Associates. Workplace Health Saf. 2012;60:437. doi: 10.3928/21650799-20120917-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karasek R, Brisson C, Kawakami N, Houtman I, Bongers P, Amick B. The Job Content Questionnaire (JCQ): an instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol. 1998;3:322. doi: 10.1037//1076-8998.3.4.322. [DOI] [PubMed] [Google Scholar]
- Kim S-S, Okechukwu CA, Dennerlein JT, Boden LI, Hopcia K, Hashimoto DM, Sorensen G. Association between perceived inadequate staffing and musculoskeletal pain among hospital patient care workers. International archives of occupational and environmental health. 2014;87:323–330. doi: 10.1007/s00420-013-0864-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laramie AK, Pun VC, Fang SC, Kriebel D, Davis L. Sharps Injuries among Employees of Acute Care Hospitals in Massachusetts, 2002–2007. Infect Control Hosp Epidemiol. 2011;32:538–544. doi: 10.1086/660012. [DOI] [PubMed] [Google Scholar]
- Menzel NN. Underreporting of musculoskeletal disorders among health care workers: research needs. AAOHN journal. 2008;56:487. doi: 10.3928/08910162-20081201-06. [DOI] [PubMed] [Google Scholar]
- Moore JT, Cigularov KP, Sampson JM, Rosecrance JC, Chen PY. Construction workers' reasons for not reporting work-related injuries: an exploratory study. International journal of occupational safety and ergonomics (Poland) 2013;19:97–105. doi: 10.1080/10803548.2013.11076969. [DOI] [PubMed] [Google Scholar]
- Osborne S. Perceptions that influence occupational exposure reporting. AORN journal. 2003;78:262–272. doi: 10.1016/s0001-2092(06)60776-x. [DOI] [PubMed] [Google Scholar]
- Panlilio AL, Orelien JG, Srivastava PU, Jagger J, Cohn RD, Cardo DM. Estimate of the annual number of percutaneous injuries among hospital-based healthcare workers in the United States, 1997–1998. Infect Control Hosp Epidemiol. 2004;25:556–562. doi: 10.1086/502439. [DOI] [PubMed] [Google Scholar]
- Pransky G, Snyder T, Dembe A, Himmelstein J. Under-reporting of work-related disorders in the workplace: a case study and review of the literature. Ergonomics. 1999;42:171–182. doi: 10.1080/001401399185874. [DOI] [PubMed] [Google Scholar]
- Probst TM, Barbaranelli C, Petitta L. The relationship between job insecurity and accident under-reporting: A test in two countries. Work Stress. 2013;27:383–402. [Google Scholar]
- Probst TM, Brubaker TL, Barsotti A. Organizational injury rate underreporting: The moderating effect of organizational safety climate. J Appl Psychol. 2008;93:1147. doi: 10.1037/0021-9010.93.5.1147. [DOI] [PubMed] [Google Scholar]
- Probst TM, Estrada AX. Accident under-reporting among employees: Testing the moderating influence of psychological safety climate and supervisor enforcement of safety practices. Accid Anal Prev. 2010;42:1438–1444. doi: 10.1016/j.aap.2009.06.027. [DOI] [PubMed] [Google Scholar]
- Probst TM, Graso M. Pressure to produce=pressure to reduce accident reporting? Accid Anal Prev. 2013;59:580–587. doi: 10.1016/j.aap.2013.07.020. [DOI] [PubMed] [Google Scholar]
- Quinn MM, Markkanen PK, Galligan CJ, Kriebel D, Chalupka SM, Kim H, Gore RJ, Sama SR, Laramie AK, Davis L. Sharps injuries and other blood and body fluid exposures among home health care nurses and aides. Am J Public Health. 2009;99:S710–S717. doi: 10.2105/AJPH.2008.150169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodríguez-Acosta R, Richardson D, Lipscomb H, Chen J, Dement J, Myers DJ, Loomis D. Occupational injuries among aides and nurses in acute care. Am J Ind Med. 2009;52:953–964. doi: 10.1002/ajim.20762. [DOI] [PubMed] [Google Scholar]
- Rosenman KD, Kalush A, Reilly MJ, Gardiner JC, Reeves M, Luo ZW. How much work-related injury and illness is missed by the current national surveillance system? J Occup Environ Med. 2006;48:357–365. doi: 10.1097/01.jom.0000205864.81970.63. [DOI] [PubMed] [Google Scholar]
- Siddharthan K, Hodgson M, Rosenberg D, Haiduven D, Nelson A. Under-reporting of work-related musculoskeletal disorders in the Veterans Administration. Int J Health Care Qual Assur. 2006;19:463–476. doi: 10.1108/09526860610686971. [DOI] [PubMed] [Google Scholar]
- Sorensen G, Stoddard AM, Stoffel S, Buxton O, Sembajwe G, Hashimoto D, Dennerlein JT, Hopcia K. The role of the work context in multiple wellness outcomes for hospital patient care workers. J Occup Environ Med. 2011;53:899. doi: 10.1097/JOM.0b013e318226a74a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tandberg D, Stewart KK, Doezema D. Under-reporting of contaminated needlestick injuries in emergency health care workers. Ann Emerg Med. 1991;20:66–70. doi: 10.1016/s0196-0644(05)81122-9. [DOI] [PubMed] [Google Scholar]
- Voide C, Darling K, Kenfak-Foguena A, Erard V, Cavassini M, Lazor-Blanchet C. Underreporting of needlestick and sharps injuries among healthcare workers in a Swiss University Hospital. Swiss Med Wkly. 2012;142 doi: 10.4414/smw.2012.13523. [DOI] [PubMed] [Google Scholar]
- Wuellner SE, Bonauto DK. Injury classification agreement in linked Bureau of Labor Statistics and Workers' Compensation data. Am J Ind Med. 2014 doi: 10.1002/ajim.22289. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.