Abstract
Background
Little is known about the course of depression in midlife women. This study aims to identify factors that distinguish risk factors for persistent or recurrent depression from those of a milder course across 13-years of follow-up.
Methods
297 Black and White premenopausal women aged 42-52 were enrolled at the Study of Women's Health Across the Nation Pittsburgh site. Psychiatric interviews obtained information on lifetime psychiatric diagnoses at baseline and occurrences of depression annually. We identified four depression patterns: 91(31%) had Persistent/recurrent major depressive disorder (MDD), 27(9%) Single Episode MDD, 35(12%) Minor Depression (minD) only, 144(48%) No Depression. We compared baseline risk factors for the Persistent/recurrent MDD group with each of the other three.
Results
A lifetime history of major or minor depression (p-values =.001-.08) and 2+ very upsetting life events in the previous year (p-values=.003-.04) were more likely to be reported by women in the Persistent/recurrent group than in the other three. The Persistent/recurrent group was more likely to report a family history of depression (p=.03) than the MinD group, and to report current sleep problems (p=.002) at baseline than the Single Episode MDD group.
Limitations
Small numbers of women with minD or a Single Episode MDD. Childhood maltreatment and family depression history were retrospectively reported.
Conclusions
A Persistent/recurrent depression course is common during midlife. In addition to personal and family histories of depression, providers of midlife health care should recognize that current sleep problems and recent very upsetting events are strong risk factors for a pernicious depression course.
Keywords: longitudinal, depressive disorders, midlife women, risk factors
1. Introduction
Clinical depression (major and minor) is a prevalent disorder with lifetime rates for women 1.5 to 2 times higher than for men. Lifetime prevalence of major depression is 22.9% for all women and 24.6% for women 50-64 years (Kessler et al., 2010). Depression is a complex disorder of multifactorial origin (Belmaker & Agam, 2008) associated with emotional, physical and functional morbidity (Blanco et al., 2010; Rubio et al., 2011). Social, biological, and psychological factors influence the development of depressive disorders (Colman & Ataullahjan, 2010). Importantly, clinical depressive disorders usually involve recurrent illness episodes. About 50-80% of those who experience a depressive episode will suffer from one or more additional episodes in their lifetime (Hardeveld et al., 2010; Kessler et al., 1997) with women more likely than men to experience recurrence (Eaton et al., 2008). However, published information about the longitudinal patterns of depression, particularly about persistent or recurrent course and their determinants in midlife women is limited.
Large population based studies have increased our understanding of the significance and consequences of depression, identifying a broad range of risk factors for its development but have typically assessed depressive symptoms or disorders at one cross-sectional or longitudinal time point. Limitations of previous studies include use of selected populations such as the elderly (Byers et al., 2012), short periods of follow-up (2-3 years) (Spijker et al., 2004), or lack of data on prior psychiatric history, childhood experiences or family history of depression. Few general population studies of women address the development and determinants of the course of depression throughout the lifecycle in general or midlife specifically.
Several longitudinal studies have focused on depression during midlife and reported that the menopausal transition (MT) is a period of increased risk for depressive symptoms (Cohen et al., 2006; Freeman et al., 2006; Freeman et al., 2004a; Woods et al., 2008). In our Study of Women's Health Across the Nation (SWAN) we found that MDD was more likely to occur during the MT (Bromberger et al., 2007; 2010), whereas Freeman et al., (2004) found no increased risk for MDD but had few women with a depressive disorder diagnosis. Studies of the MT have found that risk factors for depression during this time are similar to those for depression at other times in the lifecourse (see below). However, no study of midlife or the MT has examined risk factors for patterns of depressive disorders or their course over time. Such information is particularly relevant for aiding health care providers of midlife women in identifying and preventing an incident major (MDD) or minor (minD) depressive episode or its recurrence.
As noted above, a wide range of risk factors for depressive disorders have been identified (Dobson and Dozois, 2008). These include demographic characteristics, somatic symptoms (e.g., vasomotor symptoms, sleep problems), health-related factors (e.g., history of anxiety or substance use disorder, chronic medical condition), psychosocial/lifestyle factors (e.g., very stressful life event, low social support, low levels of physical activity). Multiple and varying exposures increase risk for depression during the MT. In this study we focused on health, functioning and psychosocial factors as risk factors because midlife and the MT is a time when health and social circumstances become more salient.
The current study aims to expand knowledge of current, recent, and distal risk factors for depression to those associated with a persistent or recurrent course of MDD during midlife among a community sample of midlife women. Women were initially assessed during the late reproductive period or early in the MT and followed annually for 13 years. In previous work we have shown that there is variation in risk factors for MDD during midlife in women with and without lifetime MDD prior to early perimenopause (Bromberger et al., 2015). Herein we ascertained patterns of MDD and minD over 13 years as women transitioned from premenopause and early perimenopause through postmenopause and evaluated factors associated with each pattern. Because a persistent or recurrent MDD illness is cumulatively more debilitating, affecting many aspects of functioning and quality of life than a single episode, we examined whether risk factors for this pernicious course of MDD could be identified and distinguished from those associated with episode(s) of minD or a single episode of MDD. Additionally, because one of the strongest risk factor for depression is a past history of depression (Kendler et al., 2010; Bromberger et al., 2011a), we were particularly interested in identifying factors that increased risk for persistent or recurrent MDD independent of a past lifetime history of minD or MDD. We hypothesized that women who went on to develop persistent or recurrent MDD over the 13 years of assessments would be more likely at baseline to report poorer health and functioning, more sleep problems, more recent stressful events, as well as a greater likelihood of a history of minD or MDD, anxiety disorder, childhood/adolescent maltreatment, and a family history of depression compared to women with only minD or a single episode of MDD.
2. Methods
2.1 Participants and procedures
The current report is based on data collected at the Pittsburgh site of a large multi-site, multiracial/ethnic community based study of the MT and aging, the Study of Women's Health Across the Nation (SWAN), and an ancillary study, the Mental Health Study (MHS). In SWAN, each site recruited White women and a predetermined minority group (Black at the Pittsburgh site). Eligibility criteria included being aged 42-52 years, having an intact uterus and at least one ovary, having had at least one menstrual period and no use of reproductive hormones in the previous three months, not pregnant and not breastfeeding. Approximately 50% of those eligible to participate in Pittsburgh entered the SWAN study. The SWAN study design and sampling procedures have been described previously (Sowers et al., 2000; Bromberger et al., 2011b). Participants and those who were eligible but did not participate did not vary by ethnicity, marital status, parity, quality of life, social support, perceived stress or reports of feeling ‘blue or depressed’ in the prior 2 weeks measured during the screener. The Pittsburgh site enrolled 162 Black and 301 White women using random digit dialing and a voter's registration list. Of these 463 women enrolled, 443 participated in the SWAN ancillary MHS, which began concurrent with the SWAN parent study in 1996. The 443 MHS participants (95.7%) and the 20 non-participants (4.3%) did not differ significantly on sociodemographic variables or percentage with Center for Epidemiologic Studies Depression (CES-D) scale (Radloff, 1977) scores ≥16. At the beginning of the baseline and follow-up core and MHS assessments, written informed consent was obtained from all participants in accordance with the University of Pittsburgh Institutional Review Board guidelines.
Women were evaluated at study entry and annually with similar protocols. Women provided extensive health, psychosocial, lifestyle, physical and psychological symptom and biologic data. As part of the MHS, the Structured Clinical Interview for the Diagnosis of DSM-IV Axis I Disorders (SCID) was conducted 2 to 9 months after the SWAN baseline assessment and within three months of each follow-up core SWAN visit. The current analysis used the psychiatric diagnostic data collected at baseline and at annual follow-up assessments. With the exception of information about family history and childhood/adolescent maltreatment (obtained at follow-up 8, 9 or 10), we used the data for predictor variables collected at baseline. For inclusion in the current analyses, participants had to meet the following three criteria: completed at least one follow-up assessment (n=425), the Family History of Depression interview (n=303), and the Childhood Trauma Questionnaire-short form (CTQ) (n=311).
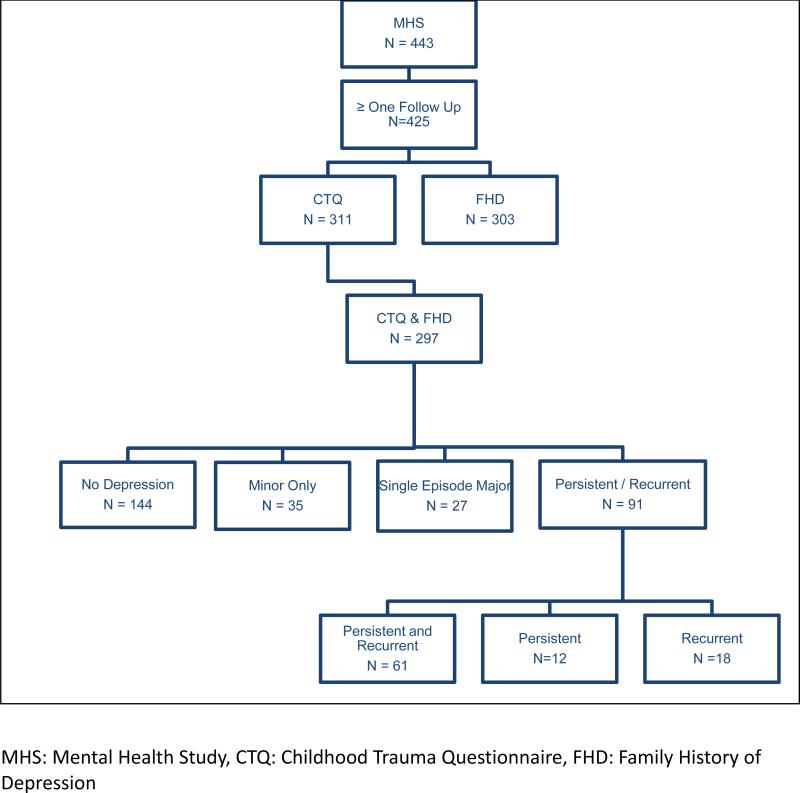
The current report focuses on the 297 women who met these criteria (See Figure 1). Compared to women who met the three criteria, those who did not had a higher mean Center for Epidemiologic Studies Depression (CES-D) scale score at baseline (p=.002), were younger (p=.005), more likely to be Black (p=.006), experience financial strain (p<.001), and to have a lifetime anxiety disorder (p=.02), and were less likely to be married (p=.02). Participants and nonparticipants had similar rates of lifetime depressive disorder, education, and recent very upsetting events. See Table 1. To evaluate the robustness of the results from the reduced sample, we removed family history of depression from the multivariable analysis in the 297 women in our current sample and compared these results to those from an analysis of the 425 women (had at least one follow-up). Results from these two analyses were consistent.
Figure 1.
Description of Study Groups
Table 1.
Compare Subjects in Study (N=297) to Those Not in Study (N=146)
| From N=443 | |||
|---|---|---|---|
| Characteristic | In Study N=297 (met 3 criteria*) | Not in Study, but in MHS N=146 | |
| Mean (sd) | Mean (sd) | p | |
| Baseline age | 45.7 (2.6) | 45.0 (2.3) | .005 |
| CESD score | 9.8 (8.4) | 13.0 (10.9) | .002 |
| N (%) | N (%) | p | |
|---|---|---|---|
| Married | 204 (69) | 84 (58) | .02 |
| Black | 91 (31) | 64 (44) | .006 |
| Some college or more | 227 (76) | 112 (77) | .95 |
| Not very hard paying for basics | 213 (72) | 81 (55) | .001 |
| Two or more very upsetting events | 86 (29) | 48 (33) | .41 |
| High CESD | 70 (24) | 48 (33) | .04 |
| Lifetime anxiety disorders | 64 (22) | 47 (32) | .02 |
| Lifetime MDD | 102 (34) | 56 (38) | .41 |
| Lifetime depression disorders | 140 (47) | 81 (55) | .10 |
Abbreviations: CES-D, Center for Epidemiologic Studies Depression scale; MDD, major depressive disorder; MHS, Mental Health Study; sd, standard deviation
Three criteria included completion of at least one follow-up MHS assessment, the Family History of Depression interview, and the Childhood Trauma Questionnaire-short form.
2.2 Measures
Assessment of Psychiatric Disorders
The SCID (Spitzer et al., 1992) is a semi-structured psychiatric interview for which we (Bromberger et al., 2011a) and others (Williams et al., 1992) have found substantial reliability for depressive and anxiety disorders (kappa=.81-.82). SCID interviews for diagnoses of lifetime MDD, minD (APA, DSM-IV, 2005), and other psychiatric disorders were conducted at study entry by trained mental health clinicians. Current/past year disorders occurring in the intervening year were diagnosed at each follow-up assessment. MinD was defined consistent with the research criteria provided for further study in DSM-IV as having at least two but fewer than five MDD symptoms (one of which was low mood or anhedonia) and impairment in functioning. We included minor depression as a form of ‘clinical depression’ because it is highly prevalent and is associated with impairment and significant decrements in health despite not meeting the symptom number criterion for major depression (Ayuso-Mateos,J.L.; Nuevo,R.; Verdes,E.; Naidoo,N.; Chatterji,S. 2010). In DSM 5, characteristics of a depressive disorder with insufficient symptoms, is called “Other Specified Depressive Disorder” (APA, DSM 5. 2013).
Because the prevalence of individual lifetime anxiety disorders was low, we defined lifetime anxiety disorder as present if any one disorder was diagnosed (Joffe et al., 2012). Similarly, we combined lifetime alcohol and non-alcohol substance use disorders into any substance use disorder.
Longitudinal Patterns of Clinical Depression
Based on the annual psychiatric data and irrespective of depression history prior to study entry, the course of clinical depression across the thirteen years was categorized as follows: No Depressive episode, minD only, Single Episode MDD, Persistent/recurrent MDD. The Persistent/recurrent MDD group included those with either a persistent course, a recurrent course, or both. Persistent MDD was defined as at least one episode of MDD that continued over two or more consecutive follow-up visits, and recurrent MDD as at least two non-consecutive follow-up visits with an MDD diagnosis or at least one MDD episode and one minD episode. Because small numbers had only a persistent (n=12) or recurrent (n=18) course, and the majority had both patterns (n=61), these groups were combined (See Figure 1).
Baseline characteristics
The predictors in the current analyses were those measured at baseline because we were interested in focusing on potential predictors of depression course as factors that a physician might use to inform risk for subsequent depression and its course.
Depressive symptoms were assessed at baseline with the CES-D scale, a 20-item scale measuring frequency of depressive symptoms during the previous week (Radloff, 1977). This scale has been used in many epidemiological studies with various race/ethnic groups, including Blacks (Jones-Webb & Snowden, 1993; Potter et al., 1995) and has well-established reliability (Matthews et al., 2010).
Demographic Factors
Race/ethnicity was self-identified as White or Black. Educational attainment was classified as some college or more (yes/no). Marital status was defined as married/living as married versus unpartnered (i.e., never married, separated/divorced, widowed). Difficulty paying for basics was defined as very or somewhat hard versus not very hard, indicating the presence/absence of financial strain.
Health Related Factors
Menopausal status
To be eligible for SWAN enrollment, women had to be pre- or early perimenopausal. Similar to World Health Organization recommended classifications (World Health Organization, 1996), menopausal status was based on menstrual bleeding patterns in the previous 12 months: Premenopausal was defined as no change in menstrual bleeding regularity and early perimenopausal as menses in the preceding 3 months with an increase in bleeding irregularity. Baseline menopausal status is included as a covariate because early perimenopause has been associated with a higher risk of depression episodes compared to premenopause (Bromberger et al, 2011a).
Lifetime medical conditions were self-reported. Participants were asked if they had ever been told by a health care provider that they had any of 12 pre-specified medical conditions: anemia, diabetes, high blood pressure/hypertension, arthritis/osteoarthritis, thyroid disease, heart attack, angina, fibroids, cancer (other than skin cancer), migraines, hypercholesterolemia, and osteoporosis. This variable was dichotomized as two or more versus one or none because most women had one or no conditions.
Lifetime history of treatment for emotional problems (coded as yes/no) was determined by self-report at the baseline SCID interview.
Functional Health and Well-Being were assessed with four subscales from the MOS 36-item Short Form (SF-36, a widely used self-administered instrument with good reliability (Ware and Sherbourne, 1992; McHorney et al., 1994). Role and social function were assessed using three SF-36 subscales: role limitations related to physical health or emotional problems, and effect of problems on social function. Each scale was dichotomized using the 25th percentile of the sample as the cut point for impaired functioning as previously established (Rose et al., 1999). The 25th percentiles reflect impaired health in the general population according to age and gender norms (Ware et al, 1993). Bodily pain was assessed with the 2-item subscale from the SF-36 which was summed and dichotomized at the 25th percentile to indicate high body pain (Rose et al. 1999).
Sleep problems were determined based on self-reported number of nights of difficulty falling asleep, staying asleep or early morning awakening during the previous 2 weeks. A sleep problem was defined if at least one of these three sleep symptoms was reported at least three times per week (Kravitz et al., 2008).
Psychosocial and Lifestyle Factors
Physical activity was measured with a composite continuous measure (range 3–15) adapted from the Kaiser Physical Activity Survey and the Baecke physical activity questionnaire (Baecke et al., 1982; Sternfeld et al., 1999). Information on the intensity, duration, and frequency of activity related to the domains of daily living, exercise/sports, and home/child care was obtained, and a total physical activity score reflected activity across all three domains.
Stressful events experienced in the previous 12 months were assessed with a checklist of 18 life events and then rated according to how upsetting they were (Bromberger et al., 2011a). The number of very upsetting life events a participant reported was dichotomized as none or one versus 2 or more. In simple exploratory analyses, we examined the prevalence of type(s) of very upsetting events by depression group that were salient for midlife women.
Family and Childhood Exposures
Data on family history of depression and childhood maltreatment were collected at follow-up visit 8, 9, or 10 from women still actively participating in the SWAN MHS (n=335).
Family History of Depression
Trained interviewers obtained information on family history of depression in first degree relatives using the family history method and a modified version of the depression module from the Family Interview for Genetic Studies (FIGS) (Maxwell 1992; Nurnberger et al., 1994). The family history method, in which an informant is queried about the history of mental illness in relatives, has been used in numerous studies of psychiatric disorder, and data from prior research indicate the family history method has acceptable reliability and validity (Andreasen et al., 1977; Weissman et al., 2000).
Childhood Maltreatment
History of childhood abuse or neglect was determined from the 28-item short form of the Childhood Trauma Questionnaire (CTQ: Bernstein et al., 2003). Participants rate items from each of five subscales (emotional abuse, physical abuse, emotional neglect, physical neglect, and sexual abuse) from 1 (never) to 5 (very often true); subscale scores range from 5-25. Validated clinical cutoff points have sensitivity and specificity at 0.85 relative to clinical interview (therapists’ ratings of childhood maltreatment) (Bernstein et al., 2003; Walker et al., 1999). Scores for each scale that were at or above these thresholds were classified as positive for abuse or neglect. If scoring was below all clinical cutoff points, an individual was classified as not exposed to abuse or neglect. The CTQ has strong test-retest reliability and convergent validity with clinical interview and therapist ratings (Bernstein et al., 1994).
2.3 Statistical Analyses
We assessed a woman's depression profile over the 13 follow-up visits and categorized each woman into one of four depression groups as described above. After determining depression group membership, bivariate analyses were performed using univariate multinomial logistic regression models to determine whether demographic or baseline clinical covariates were associated with depression group. Because the primary goal was to identify factors that were associated with higher risk for long term Persistent/recurrent MDD in particular, the Persistent/recurrent MDD group was compared to each group. Candidate predictors for the multivariable multinomial logistic regression model were factors that differed between the Persistent/recurrent MDD group and the minD or Single Episode MDD in the univariate models with a p-value <0.10. We did not adjust for multiple comparisons because the purpose of the separate univariate analyses was to identify candidates for inclusion in the multivariable multinomial analysis and we wanted to be as inclusive as possible. Age and race were also included in this final model. Regression analyses were performed using STATA (version 13.0; StataCorp, College Station, TX).
3. Results
After 13 years, 144 (48%) of 297 women developed no episodes of major or minor depression, 35 (12%) experienced episodes of minD only, 27 (9%) developed one episode of MDD, and 91 (31%) developed a Persistent/recurrent MDD course during the follow-up. On average, women completed 11 of 13 follow up visits (range=8 - 13, mean=12.5, sd=1). Table 2 shows the distribution of characteristics at baseline for the four depression groups. Among the four groups, about 75% had attained some college or more, 22% - 37% were Black, and more than half were premenopausal at study entry. Almost all women (98%) had become postmenopausal by their last annual visit.
Table 2.
Baseline Demographic and Clinical Characteristics of Depression Groups and Full Sample, n (%)a
| Baseline Characteristic | No Depression | Minor Depression | Single Episode Major Depression | Persistent / Recurrent Major Depression | All |
|---|---|---|---|---|---|
| N | 144 | 35 | 27 | 91 | 297 |
| Age, mean (sd) | 46.0 (2.7) | 45.3 (2.2) | 45.7 (2.7) | 45.3 (2.3) | 45.7 (2.6) |
| Race, n (%) | |||||
| White | 106 (74) | 22 (63) | 21 (78) | 57 (63) | 206 (69) |
| Black | 38 (26) | 13 (37) | 6 (22) | 34 (37) | 91 (31) |
| Marital status, n (%) | |||||
| Not married / not partnered | 34 (24) | 13 (37) | 7 (26) | 37 (41) | 91 (31) |
| Married / living as married | 109 (76) | 22 (63) | 20 (74) | 53 (59) | 204 (69) |
| Paying for basics, n (%) | |||||
| Very / somewhat hard | 34 (24) | 9 (26) | 6 (22) | 34 (38) | 83 (28) |
| Not very hard | 110 (76) | 26 (74) | 21 (78) | 56 (62) | 213 (72) |
| Education, n (%) | |||||
| High school or less | 39 (27) | 7 (20) | 6 (22) | 18 (20) | 70 (24) |
| Some college or more | 105 (73) | 28 (80) | 21 (78) | 73 (80) | 227 (76) |
| Overall health, n (%) | |||||
| Excellent / very good | 108 (76) | 24 (68) | 19 (70) | 54 (60) | 205 (69) |
| Good / fair / poor | 35 (24) | 11 (31) | 8 (30) | 36 (40) | 90 (31) |
| Menopausal status, n (%) | |||||
| Perimenopausal | 64 (45) | 15 (43) | 12 (46) | 43 (48) | 134 (46) |
| Premenopausal | 79 (55) | 20 (57) | 14 (54) | 47 (52) | 160 (54) |
| Low role physical, n (%) | 30 (21) | 7 (20) | 8 (30) | 38 (42) | 83 (28) |
| High bodily pain, n (%) | 24 (17) | 7 (20) | 8 (30) | 34 (37) | 73 (25) |
| Low social function, n (%) | 15 (10) | 10 (29) | 7 (26) | 30 (33) | 62 (21) |
| Low role emotional, n (%) | 14 (10) | 5 (14) | 7 (26) | 32 (35) | 58 (20) |
| CES-D, mean (sd) | 7.2 (6.9) | 8.4 (6.8) | 10.7 (7.3) | 14.1 (9.5) | 9.8 (8.4) |
| BMI category, n (%) | |||||
| Normal / underweight(<25) | 52 (36) | 12 (34) | 12 (44) | 26 (29) | 102 (34) |
| Overweight (25 - 29) | 44 (31) | 10 (29) | 8 (30) | 32 (35) | 94 (32) |
| Obese (30 +) | 48 (33) | 13 (37) | 7 (26) | 33 (36) | 101 (34) |
| Physical activity, mean (sd) | 8.1 (1.6) | 7.8 (1.7) | 7.9 (1.7) | 7.7 (1.7) | 7.9 (1.7) |
| Sleep problems, n (%) | 36 (25) | 8 (23) | 3 (11) | 42 (46) | 89 (30) |
| Very upsetting life events, n (%) | |||||
| None - one | 114 (80) | 28 (80) | 23 (85) | 45 (50) | 210 (71) |
| Two or more | 29 (20) | 7 (20) | 4 (15) | 46 (51) | 86 (29) |
| Number of lifetime medical conditions, n (%)b | |||||
| None - one | 98 (68) | 19 (54) | 16 (59) | 36 (40) | 169 (57) |
| Two or more | 45 (31) | 16 (46) | 11 (41) | 54 (60) | 126 (43) |
| Lifetime treatment for emotional problems, n (%) | 39 (28) | 16 (46) | 13 (48) | 54 (61) | 122 (42) |
| Lifetime major depression, n (%) | 28 (19) | 9 (26) | 9 (33) | 56 (62) | 102 (34) |
| Lifetime minor depression, n (%) | 18 (13) | 6 (17) | 1 (4) | 13 (14) | 38 (13) |
| Lifetime major / minor depression, n (%) | 46 (32) | 15 (43) | 10 (37) | 69 (76) | 140 (47) |
| Lifetime anxiety disorder, n (%)c | 17 (12) | 11 (31) | 6 (22) | 30 (33) | 64 (22) |
| Lifetime substance use disorder, n (%)d | 14 (10) | 5 (14) | 4 (15) | 17 (19) | 40 (13) |
| Lifetime alcohol use disorder, n (%) | 12 (8) | 3 (9) | 34 (11) | 15 (16) | 33 (11) |
| Lifetime non-alcohol use disorder, n (%) | 4 (3) | 4 (11) | 1 (4) | 7 (8) | 16 (5) |
| Any childhood / adolescent abuse and / or neglect, n (%)e | 34 (24) | 13 (37) | 13 (48) | 48 (53) | 108 (37) |
| Family history depression, n (%)e | 33 (23) | 9 (26) | 11 (41) | 49 (54) | 102 (34) |
Abbreviations: BMI, Body mass index; CES-D, Center for Epidemiologic Studies Depression scale; sd, standard deviation.
Column percentages may not sum to 100% due to rounding; percentages are calculated after excluding participants with missing data.
Medical conditions included anemia, diabetes, high blood pressure / hypertension, arthritis / osteoarthritis, thyroid disease, heart attack, angina, fibroids, cancer (other than skin cancer), migraines, hypercholesterolemia, and osteoporosis.
Lifetime history of anxiety disorder included panic, agoraphobia without panic, social phobia, specific phobia, obsessive-compulsive disorder, generalized anxiety disorder, anxiety disorder not otherwise specified.
Numbers for lifetime substance use disorder reflect at least one alcohol or non-alcohol abuse or dependence disorder. Therefore, numbers of total alcohol and non-alcohol disorder listed separately do not add up to numbers in lifetime substance use disorder.
Childhood abuse / trauma and family history questionnaires were administered at follow-up visits 08 - 10 and follow-up visits 09 - 10, respectively.
Women in the Persistent/recurrent group met SCID criteria for a depressive episode during the month before the assessment or during the previous 12 months an average of 5 of 13 visits (38%) and reported experiencing high depressive symptom (CES-D >16 in the past week) on average at 25% of visits. Because we evaluated past year and current depression together, a woman could have had a depressive episode in the past year that was not current and thus could have a low CES-D at study visit. In contrast, women with No Depression, minD only, or Single Episode MDD reported having high levels of depressive symptoms on average at 4%, 6%, and 17% of their visits, respectively. (See Table 3) Nearly half of the sample had a history of lifetime MDD (34%) or minD (13%) prior to study enrollment with either an MDD or minD history in 32% of the No Depression, 43% of the Minor depression, 37% of the Single Episode MDD, and 76% of the Persistent/recurrent MDD. Median (IQR) number of lifetime MDD episodes was different only for the Persistent/recurrent MDD group, median=2 (1, 4) whereas the median (IQR) was the same for the other three groups, median=1 (1, 2). For 19.9% (n=59) of all women, this was their first episode [12.7% had minD, 24.8% had at least one MDD episode]. Importantly, among women with a first episode of MDD, 56% (n=39) went on to have a persistent or recurrent course whereas 56% of those with a history of depression had at least one MDD episode and 87% (n=79) went on to have a persistent or recurrent course.
Table 3.
Percent of Follow-Up Visits with High CESD and Clinical Depression by Depression Group
| No Depression | Minor Depression | Single Episode Major Depression | Persistent/Recurrent Major Depression | All | |
|---|---|---|---|---|---|
| Percent of follow-up visits with high CESD | |||||
| Mean (sd) | 4 (10) | 6 (11) | 17 (22) | 25 (24) | 12 (19) |
| Median (IQR) | 0 (0, 4) | 0 (0, 9) | 8 (0, 31) | 17 (8, 38) | 0 (0, 15) |
| Minimum, Maximum | 0, 69 | 0, 54 | 0, 69 | 0, 100 | 0, 100 |
| Percent of follow-up visits with major/minor | |||||
| Mean (sd) | 0 (0) | 14 (9) | 8 (1) | 40 (22) | 15 (22) |
| Median (IQR) | 0 (0,0) | 15 (8,15) | 8 (8,8) | 31 (23,54) | 8 (0,23) |
| Minimum, Maximum | 0,0 | 8,56 | 8,11 | 15,100 | 0,100 |
Abbreviations: CES-D, Center for Epidemiologic Studies Depression scale; sd, standard deviation; IQR, interquartile range.
At baseline, the number of distal risk factors (lifetime history of major/minor depression episodes, anxiety disorder, alcohol and substance use disorders, childhood abuse or neglect and family history of depression), as well as current sleep problems, two or more medical conditions, and recent upsetting life events were all most prevalent in the Persistent/recurrent MDD group. Low functioning on all of the SF-36 subscales was more prevalent and the mean CES-D was highest in the Persistent/recurrent group compared to the other groups. Obesity was more prevalent in the minD and Persistent/recurrent groups.
3.1 Univariate Analyses
The results of univariate analyses are shown in Table 3. Baseline characteristics that differed between the Persistent/recurrent MDD group and the minD or Single Episode MDD at a p-value <0.10 included: lifetime major/minor depression and family history of depression, low role physical, low role emotional, high bodily pain, mean CES-D score, current sleep problems, two or more medical conditions, two or more very upsetting life events. See Supplementary Table for frequencies of specific upsetting events by depression group.
3.2 Multivariable Multinomial Regression Model
In the multivariable model, each individual characteristic was simultaneously adjusted for lifetime MDD or minD and every other characteristic. Results are shown in Table 4.
Table 4.
Univariate Multinomial Regression Models for Each Baseline Characteristic
| Baseline Characteristic | Persistent / Recurrent Major vs. No Depression | Persistent / Recurrent Major vs. Minor Depression | Persistent / Recurrent Major vs. Single Episode Major Depression | |||
|---|---|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | |
| Age (per 1 unit increase) | 0.89 (0.81, 1.00) | .04 | 1.00 (0.85, 1.18) | 1.00 | 0.93 (0.79, 1.11) | .44 |
| Black vs. White | 1.67 (0.94, 2.94) | .08 | 1.01 (0.45, 2.27) | .98 | 2.08 (0.77, 5.56) | .15 |
| Married vs. Not | 0.45 (0.25, 0.79) | .006 | 0.85 (0.38, 1.89) | .68 | 0.50 (0.19, 1.30) | 16 |
| Paying for basics, not very vs. very / some hard | 0.51 (0.29, 0.90) | .02 | 0.57 (0.24, 1.35) | .21 | 0.47 (0.17, 1.28) | .14 |
| Education, some college+ vs. high school or less | 1.52 (0.80, 2.86) | .20 | 1.01 (0.38, 2.70) | .98 | 1.16 (0.41, 3.33) | .78 |
| Overall Health, good / fair / poor vs. excellent / very good | 2.04 (1.16, 3.57) | .01 | 1.45 (0.64, 3.33) | .38 | 1.59 (0.63, 4.00) | .33 |
| Menopausal Status, premenopausal vs. perimenopausal | 0.88 (0.52, 1.49) | .65 | 0.82 (0.37, 1.79) | .62 | 0.93 (0.39, 2.27) | .88 |
| Low role physical | 2.70 (1.54, 4.76) | .001 | 2.86 (1.14, 7.14) | .03 | 1.69 (0.68, 4.35) | .26 |
| High bodily pain | 2.94 (1.61, 5.56) | <.001 | 2.38 (0.94, 5.88) | .07 | 1.41 (0.56, 3.57) | .46 |
| Low social function | 4.17 (2.13, 8.33) | <.001 | 1.23 (0.52, 2.86) | .64 | 1.41 (0.53, 3.70) | .49 |
| Low role emotional | 5.00 (2.50, 10.00) | <.001 | 2.23 (1.15, 9.04) | .03 | 1.54 (0.59, 4.00) | .37 |
| CES-D (per 1 unit increase) | 1.11 (1.08, 1.15) | <.001 | 1.09 (1.03, 1.14) | .002 | 1.04 (0.94, 1.10) | .10 |
| BMI Category | ||||||
| Overweight vs. normal / underweight | 1.45 (0.76, 2.78) | .26 | 1.47 (0.55, 4.00) | .45 | 1.85 (0.66, 5.26) | .25 |
| Obese vs. normal / underweight | 1.37 (0.72, 2.63) | .33 | 1.18 (0.46, 3.03) | .74 | 2.17 (0.75, 6.25) | .15 |
| Physical activity | 0.85 (0.72, 1.00) | .049 | 0.95 (0.75, 1.20) | .70 | 0.92 (0.71, 1.19) | .54 |
| Sleep problems | 2.56 (1.47, 4.55) | .001 | 2.86 (1.19, 7.14) | .02 | 6.67 (1.92, 25.00) | .003 |
| Very upsetting life events | ||||||
| Two or more vs. none - one | 4.00 (2.27, 7.14) | <.001 | 4.00 (1.61, 10.00) | .003 | 5.88 (1.89, 20.00) | .002 |
| Lifetime medical conditions a | ||||||
| Two or more vs. none - one | 3.23 (1.89, 5.56) | <.001 | 1.79 (0.81, 3.85) | .15 | 2.22 (0.91, 5.26) | .08 |
| Lifetime treatment for emotional problems | 4.00 (2.33, 7.14) | <.001 | 1.89 (0.85, 4.17) | .12 | 1.72 (0.72, 4.00) | .23 |
| Lifetime major / minor depression | 6.67 (3.70, 12.50) | <.001 | 4.17 (1.85, 10.00) | .001 | 5.26 (2.30, 14.29) | <.001 |
| Lifetime anxiety disorder b | 3.70 (1.85, 7.14) | <.001 | 1.08 (0.47, 2.50) | .87 | 1.72 (0.63, 4.76) | .29 |
| Lifetime substance use disorder, n (%) | 2.13 (0.99, 4.57) | .05 | 1.38 (0.47, 4.07) | .56 | 1.32 (0.40, 4.32) | .65 |
| Any child / adolescent abuse and / or neglect | 3.57 (2.04, 6.25) | <.001 | 1.89 (0.85, 4.17) | .12 | 1.20 (0.51, 2.86) | .68 |
| Family history depression | 4.00 (2.22, 7.14) | <.001 | 3.33 (1.43, 7.69) | .006 | 1.69 (0.71, 4.00) | .23 |
Abbreviations: CES-D, Center for Epidemiologic Studies Depression scale; CI, confidence interval; OR, odds ratio; p, p-value.
Medical conditions included anemia, diabetes, high blood pressure / hypertension, arthritis / osteoarthritis, thyroid disease, heart attack, angina, fibroids, cancer (other than skin cancer), migraines, hypercholesterolemia, and osteoporosis.
Lifetime history of anxiety disorder included panic, agoraphobia without panic, social phobia, specific phobia, obsessive-compulsive disorder, generalized anxiety disorder, anxiety disorder not otherwise specified.
Comparison of the Persistent/recurrent Group with Each Group
Relative to the No Depression group, the Persistent/recurrent group at baseline was more likely to be younger (p=.04), 2.5 times more likely to have ever had two or more medical conditions (p=.006), and three times more likely to have a lifetime history of major/minor depression (p=.001) and a family history of depression (p=.001). The Persistent/recurrent group was also more than twice as likely to report two or more very upsetting events in the past year (p=.02).
When compared with the Minor depression group, the Persistent/recurrent group was nearly three times more likely to report both a family history of depression (p=.03) and experiencing two or more very upsetting events in the past year (p=.04). They were also nearly twice as likely to have a lifetime history of major/minor depression but this did not reach statistical significance (p=.08).
Compared with the Single Episode MDD group, the Persistent/recurrent group, was four times more likely to have a lifetime history of major/minor depression (p=.009) and seven to eight times more likely to report current sleep problems (p=.002), and two or more very upsetting events in the past year (p=.003). Follow-up analyses indicated that current sleep problems at baseline were equally prevalent in the Persistent/recurrent MDD whether or not they were depressed at baseline (41.7% and 47.8%, respectively). Among the Single Episode MDD group, only one woman was depressed at baseline and she reported no sleep problems.
Race, impaired role function due to physical or emotional problems, high bodily pain, and mean CES-D at study entry did not vary significantly between the Persistent/recurrent group and each of the other three groups (p-values >.10).
4. Discussion
In this community sample of midlife White and Black women aged 42 - 52 and premenopausal or early perimenopausal at study entry, one-half developed at least one depressive episode, either minD (11.8%) or MDD (39.7%) during 13 years of annual follow-up assessments. Among those who developed at least one MDD episode, the majority (77.1%) went on to experience a persistent or recurrent course of MDD during follow-up. In the entire sample, 30.6% experienced a Persistent/recurrent course.. Of the women with a first lifetime MDD episode, more than half developed a persistent or recurrent course. Taken together, among those who developed an MDD episode during midlife, the majority experienced a pernicious depression course. Furthermore, while experiencing a first episode of MDD or minD at midlife is less common than before midlife, a substantial minority develop a persistent or recurrent course of MDD. This finding emphasizes the utility of examining longitudinal patterns of clinical depression as this highlights the importance of preventing early episodes of depression and interrupting the potential for a deleterious course in midlife.
Our results also highlight other important risk factors for Persistent/recurrent MDD, both for those with and without a history of clinical depression prior to midlife that should be considered in monitoring risk for MDD. As expected, most were more prevalent in women with Persistent/recurrent MDD than in those with No Depression. Importantly, women in the Persistent/recurrent MDD group were more likely to have had two or more very upsetting life events in the year prior to study enrollment than women with minD or Single MDD episode as well as those with No Depression. Stressful events are known to predict subsequent depression (Harkness, 2008). However, to the best of our knowledge, it is unknown whether more events pose an increased risk for a poor depression course in midlife women than does a single episode.
Sleep problems at study entry were more likely to be reported by the group that developed a Persistent/recurrent course than by each of the other three groups although the difference remained statistically significant in the multivariable comparison only with the Single Episode MDD group. This association was found even among those who reported sleep problems when they were not experiencing an episode of depression. Disturbed sleep is ubiquitous in women with clinical depression and is a cardinal criterion of depression (DSM-5). Symptoms of sleep disturbance may also predict subsequent depression (Baglioni et al., 2011) but study results have been inconsistent, in part because of confounding with depressive disorder itself as sleep problems may be a prodromal, residual or concurrent depressive symptom. Our data add importantly to these observations by showing that midlife women with sleep problems who are on the verge of or early in the MT are at a greater risk for a Persistent/recurrent depressive course than for a Single Episode MDD during and after the MT. These findings highlight the importance of treating sleep disturbance in this population as a possible strategy to reduce the likelihood that midlife women will develop a persistent or recurrent depression course.
It is noteworthy that with the exception of a lifetime history of depression at study entry, early exposures (two or more chronic medical conditions, a history of an anxiety disorder, childhood maltreatment, or a family history of MDD) posed similar risks for Persistent/recurrent and Single Episode MDD during midlife. Furthermore, while a family history of depression significantly increased risk for Persistent/recurrent MDD compared to minD, a history of child/adolescent abuse or neglect did not distinguish these groups. In contrast, recent difficulties (two or more very upsetting life events and current sleeping problems) increased the risk for Persistent/recurrent MDD compared to that for Single Episode MDD by 7-8 fold. Of further interest is that although a history of MDD was more prevalent in the Persistent/recurrent than the Single Episode MDD group, the number of past MDD episodes did not differ significantly among the groups. These results suggest that recent factors may be particularly important to evaluate during midlife and be more amenable to intervention than more distant ones. Cognitive - behavioral interventions have been shown to be efficacious for a variety of depression related factors, such as sleep problems and stress, (Edinger et al., 2003; Blumenthal et al., 1999; Ernst et al., 1998)
Numerous and varied pathways or intermediate factors may connect prior exposures such as family history of depression to depression episodes during midlife. Intermediary outcomes (such as elevated depression symptoms or disorder or stressful events) may pose an increased emotional vulnerability for later or persistent MDD. Biological factors such as inflammatory markers and changing hormonal dynamics may also link early exposures to subsequent depression (Nemeroff & Seligman, 2013).
5. Limitations and strengths
Several limitations need to be considered in interpreting these results, including small numbers of women with minD or a Single Episode MDD and the retrospective reporting of childhood maltreatment and family depression history. We did not include detailed data on total duration of time depressed or receiving treatment. Because the goal of the current report was to identify prospectively risk factors for a later deleterious course of depression that could be identified at an initial health care evaluation of women in midlife, we only examined data that were obtained at study entry. Results are limited to premenopausal or early perimenopausal midlife women who were not using reproductive hormones or pregnant in the 3 months prior to study entry and may not generalize to women in the MHS who dropped out of the study by visits 8 and 9 which reduced the MHS sample by one third. However, analyses conducted on the 425 MHS participants showed that other than not including family history of depression, the results were similar to those for the 297 women, suggesting that results generalize to the original MHS sample. Results do not generalize to men or to patterns/trajectories of depressive disorders earlier or later in life. Also, menopause status and hormonal factors at the time of each depression episode could not be examined given the study design.
Despite these limitations, the study has many strengths and is unique in prospectively evaluating the influence of a variety of distal and proximal factors to the course of clinical depression among a community sample of women during midlife, an important period of risk for depression. Women were followed longer and at more frequent intervals than in previous studies. Further, the use of the SCID, a semi-structured interview that has been considered the gold standard for obtaining diagnostic data, is a major strength. Although other studies of midlife and the MT (Freeman et al., 2004; 2006; Cohen et al., 2006) have reported on major depression, neither used the SCID or a similar diagnostic instrument.
6. Conclusions
The study results provide information on the natural course of clinical depression disorders in midlife women during a period of major endocrine, health and psychosocial changes. We identified four patterns of depressive disorders over 13 years indicating that depressive episodes are common during midlife, and their persistence and recurrence is the norm among those who experience an episode of MDD during midlife. This deleterious course was also observed among those who had never experienced depression prior to midlife.
Our findings are important for both future research and clinical care and prevention. We identified salient risk factors for Persistent/recurrent MDD, but because of design limitations, we were not able to move beyond these. Future research should consider more complex life course based models of depression pathways including those that take into account how factors interact, and the potential roles of moderator and mediator variables. With respect to clinical care, information about a patient's history of depression, her family history of depression, as well as her experience with recent upsetting events or sleep problems can help clinicians assess and address the potential risk factors for developing MDD and preventing a persistent or recurrent course during midlife.
Supplementary Material
Table 5.
Results from Multivariable Multinomial Regression Model a
| Baseline Characteristic | Persistent / Recurrent Major vs. No Depression | Persistent / Recurrent Major vs. Minor Depression | Persistent / Recurrent Major vs. Single Episode Major Depression | |||
|---|---|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | |
| Age (per 1 unit increase) | 0.87 (0.76, 0.99) | .04 | 0.96 (0.80, 1.15) | .65 | 0.89 (0.73, 1.09) | .28 |
| Black vs. White | 1.65 (0.80, 3.42) | .18 | 0.99 (0.40, 2.48) | .98 | 2.43 (0.80, 7.37) | .12 |
| Low role physical | 0.90 (0.40, 2.04) | .80 | 1.18 (0.38, 3.62) | .77 | 1.01 (0.31, 3.29) | .98 |
| High bodily pain | 1.40 (0.62, 3.17) | .42 | 1.20 (0.40, 3.60) | .75 | 0.62 (0.20, 1.96) | .42 |
| Low role emotional | 1.57 (0.60, 3.81) | .39 | 1.14 (0.33, 4.00) | .84 | 0.66 (0.18, 2.40) | .53 |
| CES-D (per 1 unit increase) | 1.04 (1.00, 1.09) | .07 | 1.00 (0.97, 1.10) | .30 | 0.97 (0.91, 1.04) | .41 |
| Sleep problems | 1.88 (0.93, 3.87) | .08 | 2.26 (0.85, 6.00) | .10 | 8.91 (2.16, 36.69) | .002 |
| Two or more very upsetting life events vs. none - one | 2.35 (1.15, 4.82) | .02 | 2.86 (1.03, 7.90) | .04 | 7.25 (1.94, 27.02) | .003 |
| Two or more medical conditions b vs. none - one | 2.56 (1.32, 5.30) | .006 | 1.48 (0.62, 3.54) | .37 | 2.00 (0.75, 5.31) | .17 |
| Lifetime major / minor depression | 3.78 (1.85, 7.70) | <.001 | 2.30 (0.91, 5.80) | .08 | 4.22 (1.43, 12.45) | .009 |
| Family history depression | 3.25 (1.64, 6.46) | .001 | 2.72 (1.08, 6.86) | .03 | 1.28 (0.49, 3.39) | .62 |
Abbreviations: CES-D, Center for Epidemiologic Studies Depression scale; CI, confidence interval; OR, odds ratio; p, p-value.
Results are from a single multivariable model. To facilitate interpretation, odds of a given risk factor for the persistent/recurrent group are compared to each group individually. Thus, no depression, minor depression and single episode major depression serve as their respective reference groups.
Medical conditions included anemia, diabetes, high blood pressure, arthritis / osteoarthritis, thyroid disease, heart attack / angina, fibroids, cancer (other than skin cancer), migraines, hypercholesterolemia, and osteoporosis.
Highlights.
We assessed risk factors for 4 patterns of clinical depression over 13 years.
Nearly half the women had no major or minor depression, 35 (12%) had minor only.
Persistent/recurrent MDD is common in midlife women independent of a lifetime MDD.
40% had at least 1 MDD episode; 77% of these had a persistent/recurrent course.
Major risk factors for persistence/recurrence are sleep problems, upsetting events.
Risk factors for poor MDD course should be assessed in midlife women.
Acknowledgements
Clinical Centers: University of Michigan, Ann Arbor – Siobán Harlow, PI 2011 – present, MaryFran Sowers, PI 1994-2011; Massachusetts General Hospital, Boston, MA – Joel Finkelstein, PI 1999 – present; Robert Neer, PI 1994 – 1999; Rush University, Rush University Medical Center, Chicago, IL – Howard Kravitz, PI 2009 – present; Lynda Powell, PI 1994 – 2009; University of California, Davis/Kaiser – Ellen Gold, PI; University of California, Los Angeles – Gail Greendale, PI; Albert Einstein College of Medicine, Bronx, NY – Carol Derby, PI 2011 – present, Rachel Wildman, PI 2010 – 2011; Nanette Santoro, PI 2004 – 2010; University of Medicine and Dentistry – New Jersey Medical School, Newark – Gerson Weiss, PI 1994 – 2004; and the University of Pittsburgh, Pittsburgh, PA – Karen Matthews, PI.
NIH Program Office: National Institute on Aging, Bethesda, MD – Winifred Rossi 2012 - present; Sherry Sherman 1994 – 2012; Marcia Ory 1994 – 2001; National Institute of Nursing Research, Bethesda, MD – Program Officers.
Central Laboratory: University of Michigan, Ann Arbor – Daniel McConnell (Central Ligand Assay Satellite Services).
Coordinating Center: University of Pittsburgh, Pittsburgh, PA – Maria Mori Brooks, PI 2012 - present; Kim Sutton-Tyrrell, PI 2001 – 2012; New England Research Institutes, Watertown, MASonja
McKinlay, PI 1995 – 2001.
Steering Committee: Susan Johnson, Current Chair
Chris Gallagher, Former Chair
We thank the study staff at each site and all the women who participated in SWAN.
Financial Support
The Study of Women's Health Across the Nation (SWAN) was supported by the National Institutes of Health (NIH), Department of Health and Human Services (HHS), through the National Institute on Aging (NIA), the National Institute of Nursing Research (NINR) and the NIH Office of Research on Women's Health (ORWH) (Grants U01NR004061, U01AG012505, U01AG012535, U01AG012531, U01AG012539, U01AG012546, U01AG012553, U01AG012554, and U01AG012495). The SWAN Mental Health Study has grant support from the National Institute of Mental Health (R01MH59689). The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the NIA, NIMH, ORWH or the NIH.
(HJ) This work was supported by Merck & Company.
Glossary
- MHS
Mental Health Study
- CTQ
Childhood Trauma Questionnaire
- FHD
Family History of Depression
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
1 Conflict of Interest
2 Joyce T. Bromberger: None
3 Howard M. Kravitz: None
4 Ada Youk: None
5 Laura L. Schott: None
6 Hadine Joffe: Consulting for Mitsubishi Tanabe Pharma, Merck & Company, NeRRRe
7 Therpeutics, Noven Pharmaceuticals, Inc., SAGE Therapeutics
8 Author Contributions:
Joyce Bromberger: Dr. Bromberger was responsible for the conception, design and interpretation of analyses, writing the first draft and giving final approval of the version submitted for publication.
Howard Kravitz: Dr. Kravitz coordinated data collection at the Chicago SWAN location, provided advice on all aspects of study design and interpretation of data and edited the article.
Ada Youk: Dr. Youk contributed to the design of the study and interpretation of data; conducted all analyses, and takes responsibility for the integrity of the data and the accuracy of the data analysis; reviewed the manuscript for accuracy and intellectual content.
Laura Schott: Dr. Schott was responsible for all analyses, interpretation of data, and the critical review and editing of the article for accuracy and important intellectual content.
Hadine Joffe: Dr. Joffe made substantive contributions to the design of the study, interpretation of data, and critical revisions of manuscript for important intellectual content.
REFERENCES
- American Psychiatric Association . Major Depressive Disorder and Dysthymic Disorder in Diagnostic and Statistical Manual of Mental Disorders. 4th Edition Washington, DC.: 2005. pp. 356pp. 380–381. [Google Scholar]
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 5th Edition. Arlington, VA.: 2013. [Google Scholar]
- Andreasen NC, Endicott J, Spitzer RL, Winokur G. The family history method using diagnostic criteria. Reliability and validity. Archives of General Psychiatry. 1977 Oct;34(10):1229–1235. doi: 10.1001/archpsyc.1977.01770220111013. [DOI] [PubMed] [Google Scholar]
- Ayuso-Mateos JL, Nuevo R, Verdes E, Naidoo N, Chatterji S. From depressive symptoms to depressive disorders: the relevance of thresholds. British Journal of Psychiatry. 2010;196(5):365–71. doi: 10.1192/bjp.bp.109.071191. [DOI] [PubMed] [Google Scholar]
- Baecke JAH, Burema J, Frijters ER. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. American Journal of Clinical Nutrition. 1982;36:936–942. doi: 10.1093/ajcn/36.5.936. [DOI] [PubMed] [Google Scholar]
- Baglioni C, Spiegelhalder K, Nissen C, Riemann D. Clinical implications of the causal relationship between insomnia and depression: how individually tailored treatment of sleeping difficulties could prevent the onset of depression. Journal of the European Association for Predictive, Preventive and Personalised Medicine. 2011 Sep;2(3):287–293. doi: 10.1007/s13167-011-0079-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belmaker RH, Agam G. Major Depressive Disorder. New England Journal of Medicine. 2008 Jan;358(1):55–68. doi: 10.1056/NEJMra073096. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Fink L, Handelsman L, Foote J, Lovejoy M, Wenzel K, Sapareto E, Ruggiero J. Initial reliability and validity of a new retrospective measure of child abuse and neglect. American Journal of Psychiatry. 1994;(151):1132–1136. doi: 10.1176/ajp.151.8.1132. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, Stokes J, Handelsman L, Medrano M, Desmond D, Zule W. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse and Neglect. 2003;(27):169–190. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- Bijl R, De Graaf R, Ravelli A, Smit F, Vollebergh WA. Gender and age-specific first incidence of DSM-III-R psychiatric disorders in the general populations. Results from the Netherlands Mental Health Survey and Incidence Study (NEMESIS). Social Psychiatry and Psychiatric Epidemiology. 2002;37:372–379. doi: 10.1007/s00127-002-0566-3. [DOI] [PubMed] [Google Scholar]
- Blanco C, Okuda M, Markowitz J, Shang-Min L, Grant B, Hasin D. The Epidemiology of Chronic Major Depressive Disorder and Dysthymic Disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2010 Dec;71(12):1645–1656. doi: 10.4088/JCP.09m05663gry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumenthal JA, Babyak MA, Moore KA, Craighead WE, Herman S, Khatri P, Waugh R, Napolitano MA, Forman LM, Appelbaum M, Doraiswamy PM, Krishnan KR. Effects of exercise training on older patients with major depression. Archives of Internal Medicine. 1999;159:2349–2356. doi: 10.1001/archinte.159.19.2349. [DOI] [PubMed] [Google Scholar]
- Bromberger JT, Kravitz HM. Mood and Menopause: Findings from the Study of Women's Health Across the Nation (SWAN) over 10 years. Obstetrics and Gynecology Clinics of North America. 2011b;38(3):609–625. doi: 10.1016/j.ogc.2011.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bromberger JT, Kravitz HM, Chang YF, Cyranowski JM, Brown C, Matthews KA. Major depression during and after the menopausal transition: Study of Women's Health Across the Nation (SWAN) Psychological Medicine. 2011a;(41):1879–1888. doi: 10.1017/S003329171100016X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bromberger JT, Schott L, Kravitz HM, Joffe H. Risk factors for major depression during midlife among a community sample of women with and without prior major depression: are they the same or different? Psychological Medicine. 2015 Jun;45(8):1653–1664. doi: 10.1017/S0033291714002773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byers AL, Vittinghoff E, Lui LY, Hoang T, Blazer DG, Covinsky KE, Ensrud KE, Cauley JA, Hillier TA, Fredman L, Yaffe K. Twenty-year depressive trajectories among older women. Archives of General Psychiatry. 2012;69(10):1703–1079. doi: 10.1001/archgenpsychiatry.2012.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colman I, Ataullahjan A. Life course perspectives on the epidemiology of depression. Canadian Journal of Psychiatry. 2010 Oct;55(10):622–632. doi: 10.1177/070674371005501002. [DOI] [PubMed] [Google Scholar]
- Dobson KS, Dozois JA. Introduction: assessing risk and resilience factors in models of depression. In: Dobson KS, Dozois DJA, editors. Risk factors in depression. xxv. Elsevier Academic Press; San Diego, CA, US: 2008. pp. 1–16.pp. 483 http://dx.doi.org/10.1016. [Google Scholar]
- Eaton WW, Shao H, Nestadt G, Lee B, Bienvenu J, Zandi P. Population-based study of first onset and chronicity in major depressive disorder. Archives of General Psychiatry. 2008 May;65(5):513–520. doi: 10.1001/archpsyc.65.5.513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edinger JD, Sampson WS. A primary care “friendly” cognitive behavioral insomnia therapy. Sleep. 2003;26:177–182. doi: 10.1093/sleep/26.2.177. [DOI] [PubMed] [Google Scholar]
- Ernst E, Rand JI, Stevinson C. Complementary therapies for depression: an overview. Archives of General Psychiatry. 1998;55:1026–1032. doi: 10.1001/archpsyc.55.11.1026. [DOI] [PubMed] [Google Scholar]
- Freeman EW. Associations of depression with the transition to menopause. Menopause. 2010 Jul;17(4):823–827. doi: 10.1097/gme.0b013e3181db9f8b. [DOI] [PubMed] [Google Scholar]
- Hardeveld F, Spijker J, DeGraaf R, Nolen WA, Beekman ATF. Prevalence and predictors of recurrence of major depressive disorder in the adult population. Acta Psychiatrica Scandinavica. 2010;(122):184–191. doi: 10.1111/j.1600-0447.2009.01519.x. [DOI] [PubMed] [Google Scholar]
- Harkness KL. Life events and hassles. In: Dobson KS, Dozois DJA, editors. Risk Factors of Depression. Academic Press imprint of Elsevier. Inc.; Amsterdam: 2008. pp. 317–342. [Google Scholar]
- Joffe H, Chang Y, Dhaliwal S, Hess R, Thurston R, Gold E, Matthews K, Bromberger J. Lifetime history of depression and anxiety disorders as a predictor of quality of life in midlife women in the absence of current illness episodes. Archives of General Psychiatry. 2012;69(5):484–492. doi: 10.1001/archgenpsychiatry.2011.1578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones-Webb RJ, Snowden LR. Depression Symptoms among Black and Whites: Differential Patterns of Risk. American Journal of Public Health. 1993;(83):240–244. doi: 10.2105/ajph.83.2.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Gardner CO. Dependent stressful life events and prior depressive episodes in the prediction of major depression. Archives of General Psychiatry. 2010;67(11):1120–1127. doi: 10.1001/archgenpsychiatry.2010.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Birnbaum H, Bromet E, Hwang I, Sampson N, Shahly V. Age differences in major depression: Results from the National Comorbidity Surveys Replication (NCS-R). Psychological Medicine. 2010;40(2):225–237. doi: 10.1017/S0033291709990213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Nelson CB, Hughes M, Swartz M, Blazer DG. Sex and depression in the national comorbidity survey II: cohort effects. Journal of Affective Disorders. 1994;(30):15–26. doi: 10.1016/0165-0327(94)90147-3. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Zhao S, Blazer D, Swartz M. Prevalence, correlates, and course of minor depression and major depression in the national comorbidity survey. Journal of Affective Disorders. 1997;45(1-2):19–30. doi: 10.1016/s0165-0327(97)00056-6. [DOI] [PubMed] [Google Scholar]
- Kravitz HM, Zhao X, Bromberger JT, Gold EB, Hall MH, Matthews KA, Sowers MR. Sleep disturbance during the menopausal transition in a multi-ethnic community sample of women. Sleep. 2008;31(7):979–990. [PMC free article] [PubMed] [Google Scholar]
- Matthews KA, Schott LL, Bromberger JT, Cyranowski JM, Everson-Rose SA, Sowers MF. Are there bi-directional associations between depressive symptoms and C-Reactive protein in mid-life women? Brain, Behavior, and Immunity. 2010 Jan;24(1):96–101. doi: 10.1016/j.bbi.2009.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxwell M. A Manual for FIGS. National Institutes of Mental Health Clinical Neurogenetics Branch; Bethesda, MD.: 1992. Family Interview for Genetic Studies (FIGS). [Google Scholar]
- McHorney CA, Ware JE, Jr., Lu JF, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Medical Care. 1994;32(1):40–66. doi: 10.1097/00005650-199401000-00004. [DOI] [PubMed] [Google Scholar]
- Nemeroff CB, Seligman F. The pervasive and persistent neurobiological and clinical aftermath of child abuse and neglect. The Journal of Clinical Psychiatry. 2013;74(10):999–1001. doi: 10.4088/JCP.13com08633. [DOI] [PubMed] [Google Scholar]
- Nurnberger JI, Jr, Blehar MC, Kaufmann CA, York-Cooler C, Simpson SG, Harkavy-Friedman J, Severe JB, Malaspina D, Reich T. Diagnostic interview for genetic studies. Rationale, unique features, and training. NIMH Genetics Initiative. 1994 Nov;51(11):849–859. doi: 10.1001/archpsyc.1994.03950110009002. discussion 863-864. [DOI] [PubMed] [Google Scholar]
- Potter LB, Rogler LH, Moscicki EK. Depression among Puerto Ricans in New York City: the Hispanic Health and Nutrition Examination Survey. Social Psychiatry and Psychiatric Epidemiology. 1995;30(4):185–193. doi: 10.1007/BF00790657. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale, a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977 Jun;1(3):385–401. [Google Scholar]
- Rose MS, Koshman ML, Spreng S, Sheldon R. Statistical issues encountered in the comparison of health-related quality of life in diseased patients to published general population norms: problems and solutions. Journal of Clinical Epidemiology. 1999 May;52(5):405–412. doi: 10.1016/s0895-4356(99)00014-1. [DOI] [PubMed] [Google Scholar]
- Rubio JM, Markowitz JC, Alegria A, Perez-Fuentes G, Liu SM, Lin KH. Epidemiology of chronic and nonchronic major depressive disorder: results from the national epidemiologic survey on alcohol and related conditions. Depression and Anxiety. 2011 Aug;28(8):622–631. doi: 10.1002/da.20864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sowers MFR, Crawford SL, Sternfeld B, Morganstein D, Gold EB, Greendale GA, Evans DA, Neer R, Matthews KA, Sherman S, Lo A, Weiss G, Kelsey JL. SWAN: A multicenter, multiethnic, community-based cohort study of women and the menopausal transition. In: Lobo RA, Kelsey L, Marcus R, editors. In Menopause. Academic Press; San Diego, CA.: 2000. pp. 175–188. [Google Scholar]
- Spijker J, de Graaf R, Bijl RV, Beekman ATF, Ormel J, Nolen WA. Determinants of persistence of major depressive episodes in the general population. Results from the Netherlands Mental Health Survey and Incidence Study (NEMESIS). Journal of Affective Disorders. 2004;(81):231–240. doi: 10.1016/j.jad.2003.08.005. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JB, Gibbon M, First MB. The Structured Clinical Interview for DSM-III-R (SCID). I: History, rationale, and description. Archives of General Psychiatry. 1992 Aug;49(8):624–629. doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- Sternfeld B, Ainsworth BE, Quesenberry CP. Physical activity patterns in a diverse population of women. Preventive Medicine. 1999;28(3):313–323. doi: 10.1006/pmed.1998.0470. [DOI] [PubMed] [Google Scholar]
- Walker EA, Gelfand A, Katon WJ, Koss MP, Von Korff M, Bernstein D, Russo J. Adult health status of women with histories of childhood abuse and neglect. American Journal of Medicine. 1999;(107):332–339. doi: 10.1016/s0002-9343(99)00235-1. [DOI] [PubMed] [Google Scholar]
- Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- Weissman MM, Wickramaratne P, Adams P, Wolk S, Verdeli H, Olfson M. Brief screening for family psychiatric history: The family history screen. Archives of General Psychiatry. 2000 Jul;57(7):675–682. doi: 10.1001/archpsyc.57.7.675. [DOI] [PubMed] [Google Scholar]
- Williams JB, Gibbon M, First MB, Spitzer RL, Davies M, Borus J, Howes MJ, Kane J, Pope HG, Jr, Rounsaville B, Wittchen HU. The Structured Clinical Interview for DSM-III-R (SCID). II. Multisite test-retest reliability. Archives of General Psychiatry. 1992;(49):630–636. doi: 10.1001/archpsyc.1992.01820080038006. [DOI] [PubMed] [Google Scholar]
- World Health Organization Technical Report Service Research on the menopause in the 1990s. Report of a WHO Scientific Group. 1996;(866):1–107. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.