Abstract
Background
Acute kidney injury (AKI) is a common complication following cardiac surgery. While AKI severity is associated with increased risk of short-term outcomes, its long-term impact is less well understood.
Methods
Adult patients undergoing isolated coronary artery bypass graft surgery at eight centers were enrolled into the Northern New England biomarker registry (n=1,610). Patients were excluded if they had renal failure (n=15) or died during index admission (n =38). AKI severity was defined using the AKI Network (AKIN). We linked our cohort to national Medicare and state all-payer claims to ascertain readmissions and to the National Death Index to ascertain survival. Kaplan-Meier and multivariate Cox’s proportional hazard modeling were conducted for time to readmission and death over 5 years.
Results
Within 5 years, 513 patients (33.8%) developed AKI with AKIN stage 1 (29.9%) and stage 2–3 (3.9%). There were 620 (39.9%) readmissions and 370 (23.8%) deaths. After adjustment, Stage 1 AKI patients had a 31% increased risk of readmission (95%CI: 1.10–1.57), while Stage 2–3 patients had a 98% increased risk (1.41–2.78) compared to those with no AKI. Relative to those without AKI, Stage 1 patients had a 56% increased risk of mortality (1.14–2.13) while those Stage 2–3 patients had a 3.5-times higher risk (2.16–5.60).
Conclusions
AKI severity using the AKIN stage criteria is associated with a significantly increased risk of 5-year readmission and mortality. Our findings suggest efforts to reduce AKI in the perioperative period may have significant long-term impact for patients and payers in reducing mortality and healthcare utilization.
Keywords: Coronary artery bypass graft, kidney, renal function, surgery, readmission, mortality
Readmissions account for significant increase in morbidity, mortality, costs and are potentially preventable.(1–3) Since the Hospital Readmission Reduction Program (HRRP), hospitals are facing the rapid onset of the readmission- and value-based purchasing penalties, resulting in reductions in reimbursement from the Center for Medicaid and Medicare Services (CMS, Section 3025 PPACT).(4, 5) Approximately two-thirds of the United States (US) hospitals have higher than expected readmission rates for patient populations of interest, including cardiac surgery.
Acute kidney injury (AKI) is a common complication occurring after cardiac surgery.(6) AKI has been shown to be associated with short- and long-term mortality after cardiac surgery.(7, 8) More recently, AKI has also been shown to be associated with hospital readmissions following cardiac surgery, hospitalization for heart failure, or acute myocardial infarction.(9–12) Moreover, recent evidence suggests that the severity of AKI might be an easily identifiable marker of the risk of 30-day readmission.(10) However, the long-term impacts of severity of AKI on readmission or mortality are less well understood.
Some studies have reported post-procedure AKI or renal failure as a significant risk factor for 30-day readmissions.(12–14) One study identified AKI severity as an ordinal risk factor for 30-day readmission after cardiac surgery.(10) While 30-day endpoints only provide a small window in evaluating morbidity and mortality, no report has evaluated a severity index for AKI, using the Acute Kidney Injury Network (AKIN)(15) staging criteria as a risk factor, for determining long-term risk of readmission or mortality after cardiac surgery.
Based on the evidence, we hypothesized that the severity of AKI, using the AKIN staging criteria, could serve as a risk factor for long-term readmission and mortality. Therefore, we examined whether post-cardiac surgery AKI stage (no AKI, AKI stage 1, stage 2, and stage 3) is associated with 5-year readmission and/or 5-year mortality.
Patients and Methods
Cohort: NNE Biomarker Study
Patients undergoing coronary artery bypass graft (CABG) surgery and/or valve surgery at any of 8 hospitals participating in the Northern New England Cardiovascular Disease Study Group (NNE) were prospectively enrolled into the NNE Biomarker Study from 2004 to 2007 (n = 1,690). For the present study, the sample was restricted to only those patients for whom CABG was the primary procedure (n=1610). Patients were excluded from the analysis if they had a history of renal failure (n = 15) or died during the index admission (n=38). Patients were also dropped if their recorded date of discharge occurred after their recorded date last known alive (n=1). The Committee for the Protection of Human Subjects at Dartmouth College (IRB) approved this study for both the prospective cohort with patient consent and the linkage of readmission and mortality events.
Primary Outcomes: 5-Year Readmission and Mortality
The cohort was linked to Medicare in-patient claims (completed by ResDAC) and state all-payer in-patient claims using name, gender, social security number, date of birth, and zip-code of residence at the time of surgery. Maine and Vermont completed links internally. We used probabilistic linking for New Hampshire all-payer in-patient claims. We achieved complete ascertainment for Medicare, VT, and ME. Five percent of NH patients were not matched in the NH in-patient claims. Reasons for readmission were determined using the principal diagnosis upon first readmission. Five-year mortality was ascertained by linking to the National Death Index.
Primary Exposure: AKIN Staging Criteria
The last serum creatinine prior to cardiac surgery and highest post-operative serum creatinine prior to discharge were used to classify the stage of AKI. AKI stages were defined by the AKIN definitions as follows: AKIN Stage 1: 0.3 or 50% increase in serum creatinine from baseline; AKIN Stage 2: a 2-fold increase in serum creatinine; and AKIN Stage 3: a 3-fold or 0.5 increase if the baseline serum creatinine was at least 4.0 (mg/dL), or new dialysis-dependent renal failure.(15) Due to the small proportion of patients in AKIN stage 2 and 3, we bundled stage 2 or 3 patients’ outcomes in this report.
Statistical Methods
Baseline, operative, and postoperative outcomes were compared using chi-square tests, and continuous data were compared between groups using the student’s t-test or Wilcoxon Rank-Sum tests, where appropriate. Kaplan-Meier time-to-event methods and log-rank tests were conducted to compare 5-year readmission (first readmission) and 5-year mortality across AKIN stages. Univariate and multivariate Cox’s proportional hazard models were constructed to compare hazard ratios across AKIN stages, adjusting for age, sex, body surface area, and presence of any vascular disease for readmission and the combined readmission and mortality endpoint. Mortality models were adjusted for age and sex. Multivariate cox’s proportional hazard models for 5-year readmission and mortality were repeated using multiple imputation methods to account for variables with missing values. We then conducted time-competing event analyses. All analyses were performed using Stata 13.1 (College Station, TX).
Results
Overall, 513 patients (33.8%) developed AKI with AKIN stage 1 (29.9%) and stage 2–3 (3.9%). There were 620 (39.9%) readmissions and 370 (23.8%) deaths overall, and 620 (39.9%) readmissions and 192 (12.3%) deaths within 5 years. Patient characteristics and comorbidities are summarized in Table 1.
Table 1.
Patient Characteristics
| Total N = 1,690 | Percent/Mean ± SD | |
|---|---|---|
| AKIN | ||
| No AKIN | 66.25% | |
| Stage 1 | 29.87% | |
| Stage 2 | 2.30% | |
| Stage 3 | 1.58% | |
| Age (mean, SD) | 65.18 ± 10.06 | |
| Female | 22.37% | |
| BMI (mean, SD) | 29.72 ± 5.50 | |
| BSA (mean, SD) | 2.04 ± 0.24 | |
| Smoker | 23.23% | |
| Atrial fibrillation | 6.75% | |
| CHF | 9.46% | |
| Last pre-op serum creatinine (mean, SD) | 1.11 ± 0.90 | |
| Diabetes | 37.72% | |
| Ejection fraction <40% | 10.85% | |
| Hypertension | 80.89% | |
| IABP pre-op | 4.63% | |
| Prior MI | ||
| No | 55.85% | |
| < 24 hours pre-op | 1.74% | |
| > 24 hours & < 7 days pre-op | 18.57% | |
| > 7 days & < 365 days pre-op | 9.96% | |
| > 365 days pre-op | 13.88% | |
| Vascular disease | 27.12% | |
| Unstable angina | 54.34% | |
| COPD | 13.11% | |
| Left main, ≥50% stenosis | 34.19% | |
| Prior CABG | 2.08% | |
| Prior PCI | 20.50% | |
| Priority | ||
| Emergent | 1.93% | |
| Urgent | 67.42% | |
| Non-urgent | 30.66% | |
| Received pRBC units | 36.21% | |
| Number of pRBC units given pre-op | ||
| 0 | 97.81% | |
| 1 | 0.64% | |
| 2 | 0.97% | |
| 3 or more | 0.58% | |
AKI=acute kidney injury, AKIN=Acute Kidney Injury Network, BMI=body mass index (kg/m2), BSA=body surface area (m2), CABG=coronary artery bypass graft, CHF=congestive heart failure, COPD=chronic obstructive pulmonary disease, IABP=intra-operative balloon pump, MI=myocardial infarction, PCI=percutaneous coronary intervention, pRBC=packed red blood cell
We stratified intra- and post-operative variables by AKIN stage in Table 2. Intra-operative factors differed by AKIN stage for intra-aortic balloon pump (IABP), number of packed red blood cells (pRBC), and lowest hematocrit on bypass. Post-operative factors differed by AKIN stage for all outcomes, except for returning to bypass, returning to the operating room for bleeding, and a new Q-wave myocardial infarction (Table 2).
Table 2.
Procedural Characteristics by AKI Status
| No AKI | AKIN Stage 1 | AKIN Stage 2 or 3 | p-value | |
|---|---|---|---|---|
| Percent/Mean ± SD | Percent/Mean ± SD | Percent/Mean ± SD | ||
| Pump time (minutes; mean, SD) | 98.86±28.71 | 105.60±30.54 | 115.46±37.16 | <0.001 |
| Intra- or post-operative IABP | 1.39% | 1.76% | 8.47% | <0.001 |
| Total Number of pRBC units given during admission |
||||
| 0 | 71.04% | 50.11% | 30.51% | <0.001 |
| 1 | 6.17% | 10.15% | 13.56% | |
| 2 | 12.14% | 17.66% | 15.25% | |
| 3 or more | 10.65% | 22.08% | 40.68% | |
| Number of pRBC units given intra-op | ||||
| 0 | 87.48% | 77.53% | 62.71% | <0.001 |
| 1 | 3.98% | 7.05% | 11.86% | |
| 2 | 6.56% | 10.13% | 5.08% | |
| 3 or more | 1.99% | 5.29% | 20.34% | |
| Low hematocrit <20% | 13.28% | 21.45% | 25.93% | <0.001 |
| Number of pRBC units given post-op | ||||
| 0 | 77.73% | 62.69% | 44.07% | <0.001 |
| 1 | 6.06% | 9.71% | 16.95% | |
| 2 | 10.83% | 16.11% | 15.25% | |
| 3 or more | 5.37% | 11.48% | 23.73% | |
| Renal failure outcome | 0.00% | 0.00% | 13.56% | <0.001 |
| Atrial fibrillation, new post-op | 16.29% | 27.53% | 52.54% | <0.001 |
| Low output | 3.54% | 5.15% | 15.79% | <0.001 |
| Any Mediastinitis/sternal discharge req. re-op |
0.30% | 1.10% | 6.78% | <0.001 |
| Return to OR for bleeding | 1.09% | 1.76% | 1.69% | 0.563 |
| Q wave post-op | 0.44% | 1.23% | 1.85% | 0.180 |
| Pneumonia post-op | 0.70% | 2.20% | 13.56% | <0.001 |
| Return to bypass | 2.32% | 2.89% | 1.69% | 0.751 |
| Outcomes | ||||
| Dead at 30 days | 0.30% | 1.54% | 3.39% | 0.003 |
| Dead at 1 year | 1.19% | 3.96% | 10.17% | <0.001 |
| Dead at 5 years | 9.14% | 16.08% | 37.29% | <0.001 |
| Readmitted at 30 days | 9.54% | 13.59% | 15.52% | 0.039 |
| Readmitted at 1 year | 24.05% | 36.10% | 50.00% | <0.001 |
| Readmitted at 5 years | 35.79% | 49.20% | 68.42% | <0.001 |
| Readmitted or dead at 30 days | 9.63% | 14.54% | 16.95% | 0.009 |
| Readmitted or dead at 1 year | 24.43% | 37.22% | 50.85% | <0.001 |
| Readmitted or dead at 5 years | 37.84% | 51.32% | 69.49% | <0.001 |
AKI=acute kidney injury, AKIN=Acute Kidney Injury Network, IABP=intra-operative balloon pump, OR=operating room, pRBC=packed red blood cell
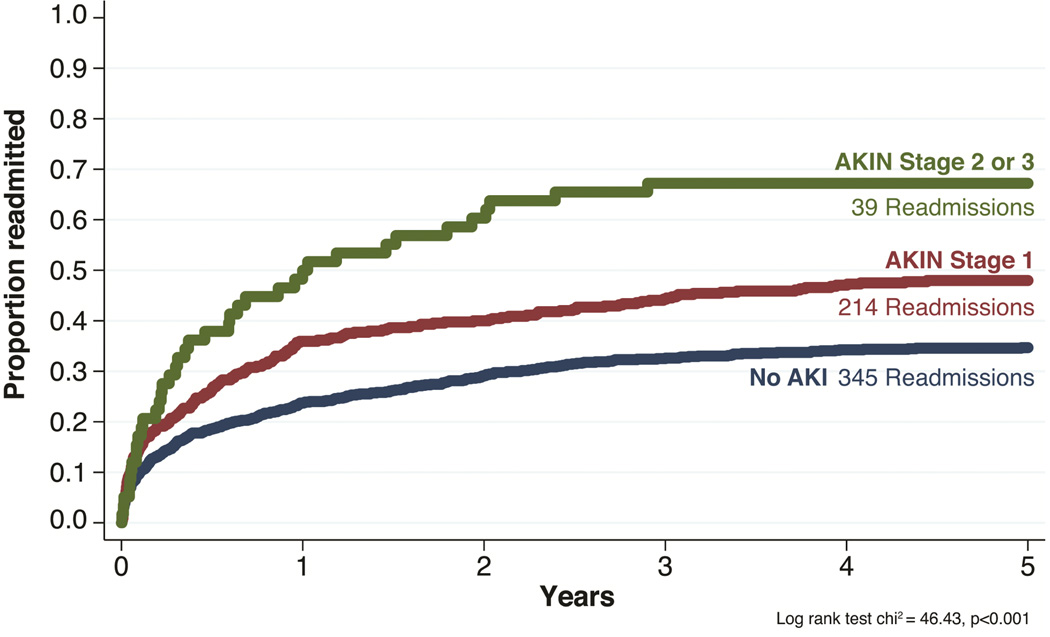
5-Year Readmission
The overall incidence of readmission was 12.1 per 100 person years, while highest among those with Stage 2–3 AKI (no AKI: 9.8, Stage 1: 16.2, Stages 2–3: 32.4 per 100 person years, p<0.001, Figure 1). After adjustment, patients in AKIN Stage 1 had a 31% increased risk of 5-year readmission (95%CI: 1.10, 1.57), while those in AKIN Stage 2–3 had a 98% increased risk (95%CI: 1.41, 2.78, Table 3). Multiple imputation methods confirmed our results with AKIN stage 1 (HR: 1.32; 95%CI: 1.10, 1.57) and AKIN stage 2–3 (HR: 1.94; 95%CI: 1.39, 2.73). Accounting for death as a time competing event, results were the same for AKIN stage 1 (HR:1.29; 95%CI: 1.08, 1.55) and AKIN stage 2–3 (HR: 1.96; 95%CI: 1.42, 2.71).
Figure 1. 5-Year Readmission.
We plot time from alive cardiac surgery discharge to the first readmission to any hospital stratified by AKIN stage: No AKI (blue line), AKIN Stage 1 (red line), and AKIN Stages 2–3 (green line). Log-rank test chi2 46.43, p-value <0.001. AKI= acute kidney injury. AKIN= Acute Kidney Injury Network.
Table 3.
Unadjusted and adjusted hazard ratios for 5-year readmission, 5-year mortality, and 5-year readmission or mortality.
| Unadjusted | Adjusted | |||||
|---|---|---|---|---|---|---|
| Hazard Ratio |
Confidence Interval |
p-value | Hazard Ratio |
Confidence Interval |
p-value | |
| 5-year Readmissiona | ||||||
| No AKI | 1.00 | (1.00–1.00) | -- | 1.00 | (1.00–1.00) | -- |
| AKIN Stage 1 | 1.53 | (1.29–1.81) | <0.001 | 1.31 | (1.10–1.57) | 0.002 |
| AKIN Stage 2 or 3 | 2.51 | (1.80–3.50) | <0.001 | 1.98 | (1.41–2.78) | <0.001 |
|
5-year Readmissiona (with death as a competing risk) |
||||||
| No AKI | 1.00 | (1.00–1.00) | -- | 1.00 | (1.00–1.00) | -- |
| AKIN Stage 1 | 1.51 | (1.27–1.79) | <0.001 | 1.29 | (1.08–1.55) | 0.004 |
| AKIN Stage 2 or 3 | 2.46 | (1.79–3.38) | <0.001 | 1.96 | (1.42–2.71) | <0.001 |
|
5-year Readmissiona (with missing observations imputed) |
||||||
| No AKI | 1.00 | (1.00–1.00) | -- | 1.00 | (1.00–1.00) | -- |
| AKIN Stage 1 | 1.53 | (1.29–1.82) | <0.001 | 1.32 | (1.10–1.57) | 0.002 |
| AKIN Stage 2 or 3 | 2.49 | (1.79–3.47) | <0.001 | 1.94 | (1.39–2.73) | <0.001 |
| 5-year Mortalityb | ||||||
| No AKI | 1.00 | (1.00–1.00) | -- | 1.00 | (1.00–1.00) | -- |
| AKIN Stage 1 | 1.85 | (1.36–2.51) | <0.001 | 1.56 | (1.14–2.13) | 0.005 |
| AKIN Stage 2 or 3 | 4.89 | (3.07–7.79) | <0.001 | 3.48 | (2.16–5.60) | <0.001 |
|
5-year Mortalityb (with missing observations imputed) |
||||||
| No AKI | 1.00 | (1.00–1.00) | -- | 1.00 | (1.00–1.00) | -- |
| AKIN Stage 1 | 1.82 | (1.34–2.48) | <0.001 | 1.56 | (1.14–2.12) | 0.005 |
| AKIN Stage 2 or 3 | 4.79 | (3.01–7.62) | <0.001 | 3.48 | (2.16–5.61) | <0.001 |
| 5-year Readmission or Mortalitya | ||||||
| No AKI | 1.00 | (1.00–1.00) | -- | 1.00 | (1.00–1.00) | -- |
| AKIN Stage 1 | 1.53 | (1.30–1.80) | <0.001 | 1.32 | (1.11–1.56) | 0.001 |
| AKIN Stage 2 or 3 | 2.46 | (1.78–3.39) | <0.001 | 1.93 | (1.39–2.69) | <0.001 |
|
5-year Readmission or Mortalitya (with missing observations imputed) |
||||||
| No AKI | 1.00 | (1.00–1.00) | -- | 1.00 | (1.00–1.00) | -- |
| AKIN Stage 1 | 1.53 | (1.30–1.81) | <0.001 | 1.32 | (1.12–1.56) | 0.001 |
| AKIN Stage 2 or 3 | 2.44 | (1.77–3.37) | <0.001 | 1.90 | (1.37–2.64) | <0.001 |
Adjusted for age, sex, body surface area, and vascular disease diagnosis.
Adjusted for age and sex.
The TRIBE consortium, which represents cardiac surgery data from across the United States and Canada, provided unpublished external validation of our findings, where patients with stage 1 or 2 AKI are significantly more likely to be readmitted within one year (Stage 1 adjusted OR=1.55, 95%CI: 1.13, 2.13; Stage 2 adjusted OR=3.02, 95%CI: 1.29, 7.07) compared to patients with no AKI.
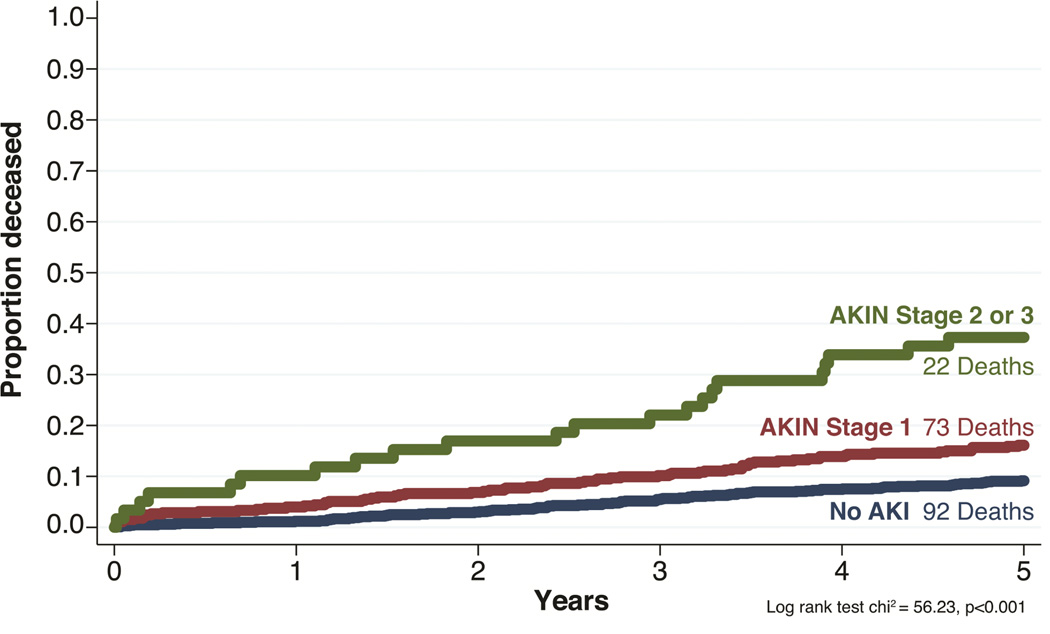
5-Year Mortality
The incidence of 5-year mortality was 2.6 per 100 person-years. The rate increased across AKI severity (no AKI: 1.9, AKIN Stage 1: 3.5, AKIN Stages 2–3: 9.4 per 100 person years, p<0.001, Figure 2). After adjustment, relative to those without AKI, patients in AKIN Stage 1 had a 56% increased risk of mortality (95%CI: 1.14, 2.13) while those in Stage 2 or 3 had a 348% higher risk (95%CI: 2.16, 5.60). Multiple imputation confirmed our results with AKIN stage 1 (HR: 1.56; 95%CI: 1.14, 2.12) and AKIN stage 2–3 (HR: 3.48; 95%CI: 2.16, 5.61).
Figure 2. 5-Year Mortality.
We plot time from alive cardiac surgery discharge to all-cause death stratified by AKIN stage: No AKI (blue line), AKIN Stage 1 (red line), and AKIN Stages 2–3 (green line). Log-rank test chi2 56.23, p-value <0.001. AKI= acute kidney injury. AKIN= Acute Kidney Injury Network.
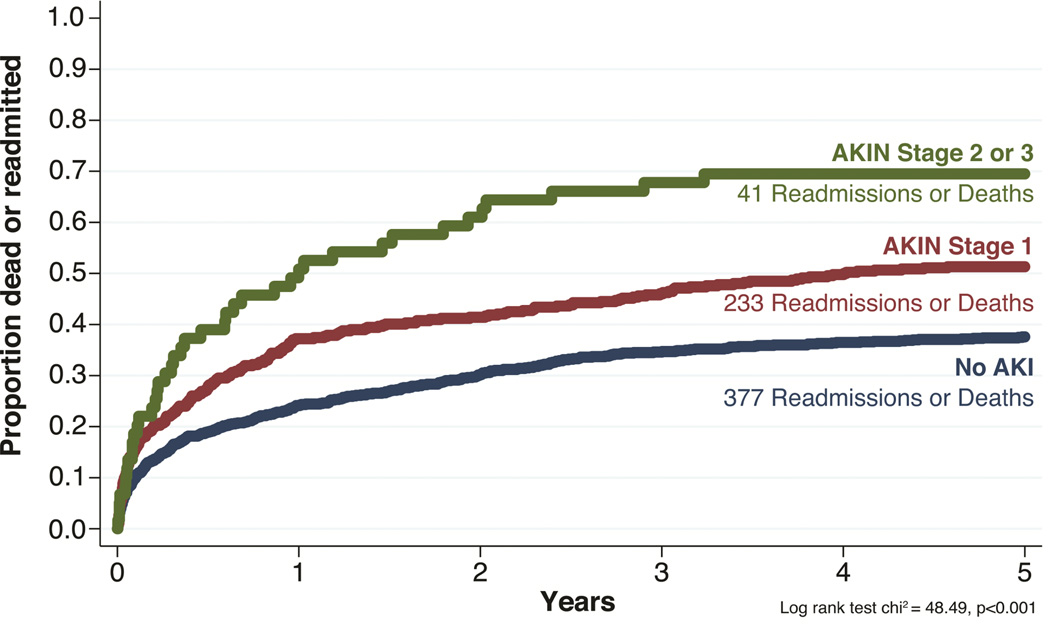
5-Year Readmission or Mortality
The overall incidence of 5-year combined readmission or mortality was 13.1 per 100 person-years. Incidence rates increased across AKI severity (no AKI: 10.7, AKIN Stage 1: 17.6, AKIN Stages 2–3: 34.0 per 100 person years, p<0.001, Figure 3). After adjustment, patients in AKIN Stage 1 had a 32% increased risk of mortality (95%CI: 1.11, 1.56) relative to those without AKI, while those in Stage 2 or 3 had a 93% higher risk (95%CI: 1.39, 2.69). Multiple imputation methods confirmed our results for AKIN stage 1 (HR: 1.32; 95%CI: 1.12, 1.56) and AKIN stage 2–3 (HR: 1.90; 95%CI: 1.37, 2.64).
Figure 3. 5-Year Readmission or Mortality.
We plot time from alive cardiac surgery discharge to readmission or all-cause death stratified by AKIN stage: No AKI (blue line), AKIN Stage 1 (red line), and AKIN Stages 2–3 (green line). Log-rank test chi2 48.49, pvalue <0.001. AKI= acute kidney injury. AKIN= Acute Kidney Injury Network.
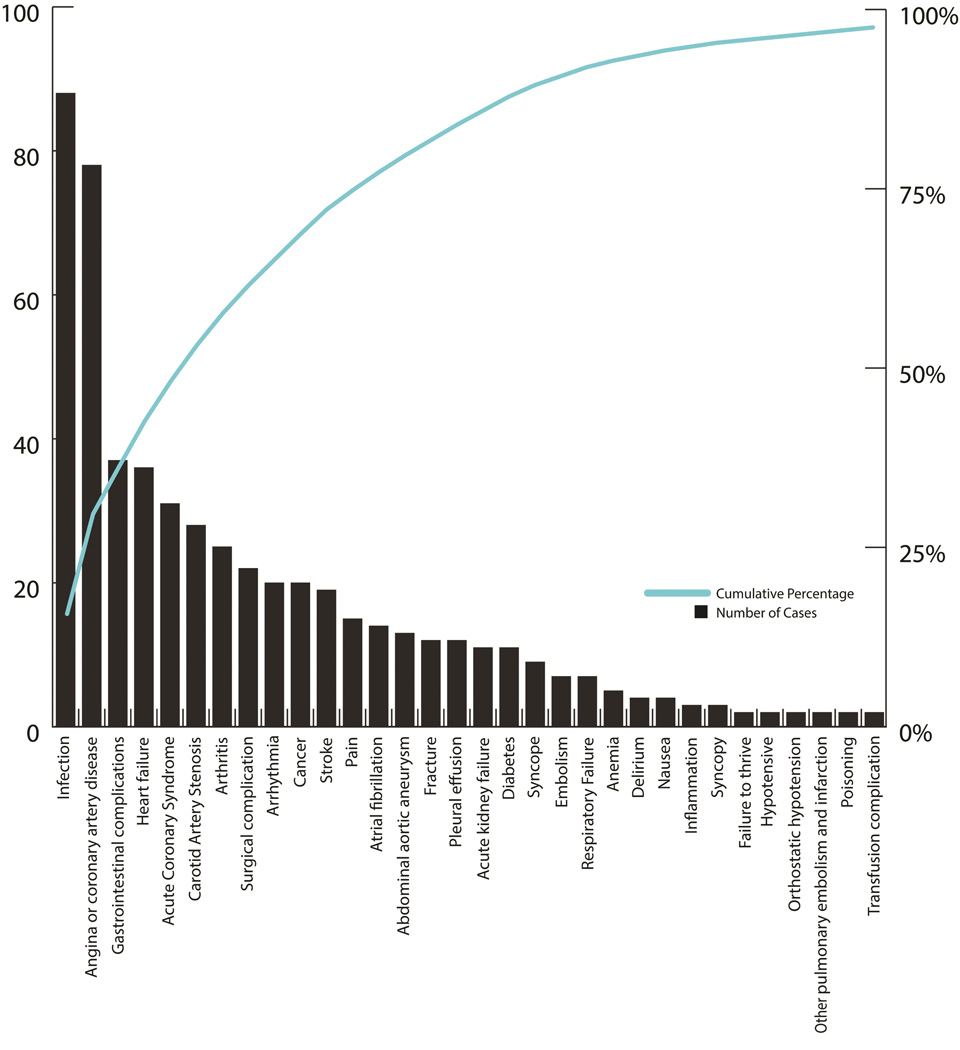
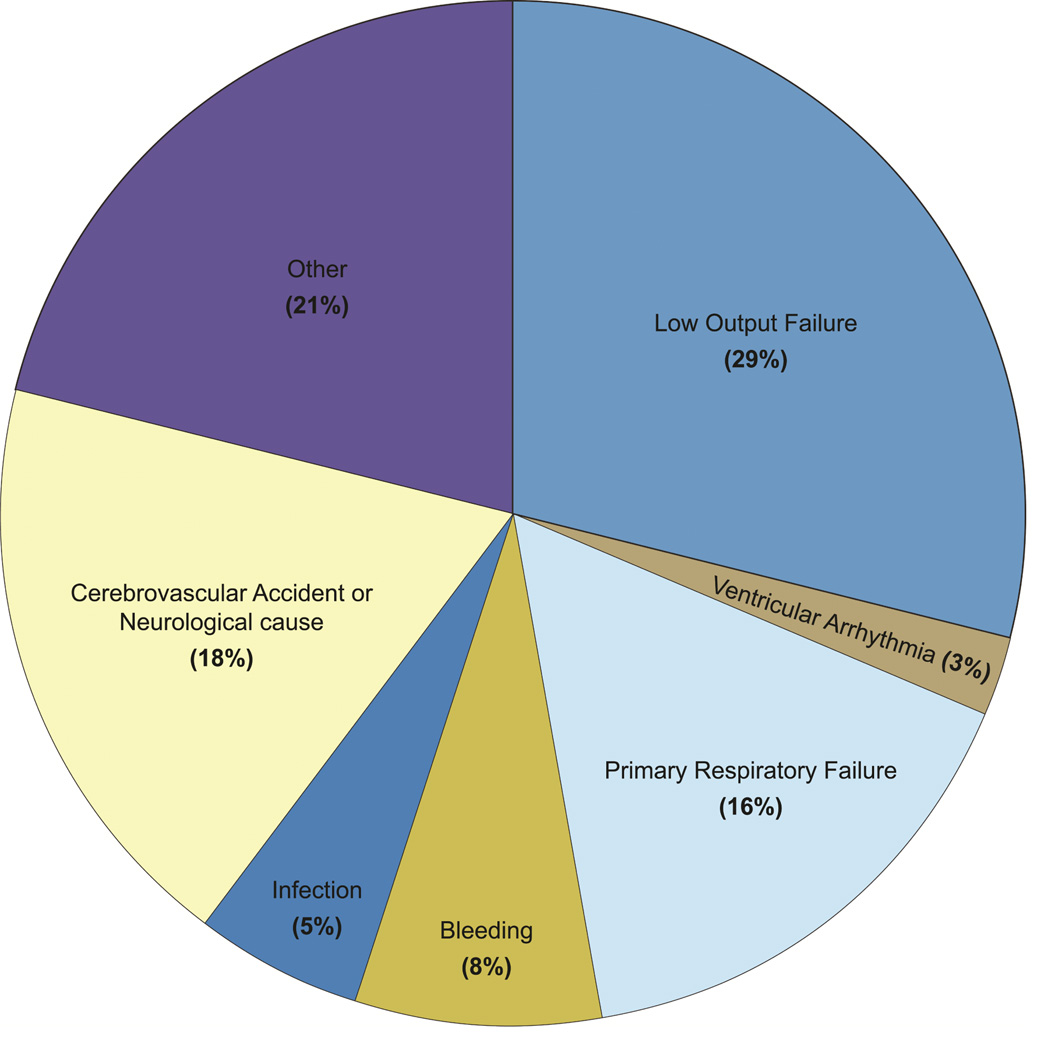
Reasons for readmission and death
The reasons for hospital readmission are shown in Figure 4. The primary causes of death are illustrated in Figure 5. The most common causes of readmission were infection and angina or coronary artery disease. The most common cause of death was low output heart failure.
Figure 4. Reasons for Hospital Readmission.
This Pareto chart depicts the reasons for readmission in our cohort. The category “Other” is not included in this chart accounting for 2.5% of readmissions. Blue line shows the cumulative percentage of readmissions, and the black bars indicate the number of readmissions in this cohort.
Figure 5. Primary Causes of Death.
Pie chart illustrates the most frequent causes of death and their percentages of occurrence in the study cohort.
Comment
Using AKIN stage criteria, our study confirms similar findings from past literature that AKI severity is associated with increased hospital readmission and mortality.(16, 17) We discovered AKIN stage 1 and stages 2–3 were associated with a significant 31% to 98% increased hazard of 5-year readmission. In addition, AKIN stage 1 and stages 2–3 were associated with a significant 56% to 3.5-fold increased hazard of 5-year mortality. Our findings suggest that current and novel therapeutic interventions to reduce AKI may have a significant long-term impact for patients and payers in reducing readmission and mortality up to five years.
The effects of creatinine elevation on long-term patient readmission and mortality are significant, even when the creatinine returns to baseline before the patient is discharged from the hospital.(7) We evaluated the association of an AKI severity index (AKIN staging criteria) and risk of patients dying or being readmitted up to five years after cardiac surgery. We found AKIN stage to be a simple risk factor for risk of long-term readmission or mortality. Although we are the first to report on the predictive ability of AKIN stage as a severity index for mortality and readmission out to five years among patients alive at discharge, recent studies have supported the association between AKI and readmission, predominately in patients hospitalized for heart failure. These reports have identified that worsening renal function, among patients hospitalized for heart failure, has been predictive of mortality and 30-day heart failure readmissions.(18, 19) Others have investigated AKI or the RIFLE (Risk, Injury, Failure, Loss of function, End-stage renal disease) criteria and their association with mortality and readmission. Among patients hospitalized for heart failure, those that developed AKI were at a significant increased risk of readmission within 30 days (9.2% versus 6.0%, p=0.0003).(12) In another investigation, the RIFLE criteria was used as a significant independent risk factor for mortality or heart failure readmissions up to one year.(20) However, when heart failure readmissions were abstracted from the one-year events, the RIFLE criteria did not demonstrate a trend in rates of one-year heart failure readmissions. Contrary to this report, our research supports the use of the AKIN staging criteria for prediction of 5-year readmissions or five-year mortality after live discharge from cardiac surgery in a multi-center regional collaborative.
Strengths and Limitations
There are limitations to consider for our investigation of AKIN staging criteria and the association with 5-year readmission and mortality. First, our prospective cohort was developed to enroll patients into a biomarker cohort. While enrollment was consistent at all medical centers, this investigation is limited to patients consented into the NNE biomarker cohort and does not reflect consecutive patients. However, Table 4 demonstrates patients enrolled were comparable to non-enrolled patients in the NNE. External validation from the TRIBE consortium supports generalizability of our findings to other centers.
Table 4.
Patient Characteristics by NNE Biomarker Cohort status
| Not in biomarker cohort | In biomarker cohort | ||
|---|---|---|---|
| Percent/Mean ± SD | Percent/Mean ± SD | p-value | |
| Age (mean, SD) | 65.37 ± 10.56 | 65.18 ± 10.06 | 0.528 |
| Female | 24.66% | 22.37% | 0.053 |
| BMI (mean, SD) | 29.68 ± 5.90 | 29.72 ± 5.50 | 0.789 |
| BSA (mean, SD) | 2.03 ± 0.25 | 2.04 ± 0.24 | 0.206 |
| Smoker | 24.71% | 23.23% | 0.214 |
| CHF | 11.93% | 9.46% | 0005 |
| Last pre-op serum creatinine (mean, SD) | 1.10 ± 0.88 | 1.11 ± 0.90 | 0.678 |
| Diabetes | 35.54% | 37.72% | 0.107 |
| Vascular disease | 25.26% | 27.12% | 0.131 |
| Unstable angina | 55.45% | 54.34% | 0.290 |
| COPD | 12.28% | 13.11% | 0.374 |
| Left main, ≥50% stenosis | 34.94% | 34.19% | 0.593 |
| Prior CABG | 3.56% | 2.08% | 0.003 |
| Priority | |||
| Emergent | 8.70% | 1.93% | <0.001 |
| Urgent | 63.96% | 67.42% | |
| Non-urgent | 27.34% | 30.66% | |
BMI=body mass index (kg/m2), BSA=body surface area (m2), CABG=coronary artery bypass graft, CHF=congestive heart failure, COPD=chronic obstructive pulmonary disease, MI=myocardial infarction, pRBC=packed red blood cell
Second, serum creatinine used to define AKI and AKIN staging criteria were measured daily postoperatively at each medical center, rather than at a single laboratory. Therefore, there may be variability in the measurement of AKI. However, we have no reason to believe there was differential ascertainment of creatinine data between patients with AKI versus those without AKI.
Third, as with any observational trial, the issue of unmeasured confounding is a concern. We did not capture post-hospitalization risk factors for readmission or mortality. However, the NNE registry has some of the most extensive patient and procedural data for cardiac surgery, and we are confident we have thoroughly evaluated patient, procedural, and perfusion risk factors for readmission. In addition, we adjusted for variables used in the age, sex, body surface area, and vascular disease in our models.(21)
Currently, we have a limited understanding on the causal relationship between AKI and long-term readmission or mortality. It is likely that AKIN stage is acting as a severity index for risk of near-term adverse events, such as readmissions and mortality, and acting as a surrogate for the physiologic vulnerability of patients. In our previous research, we identified that AKI duration, after cardiac surgery, impacts 5-year survival.(16) This effect on survival may not be directly related to the kidney injury. AKI may be a surrogate for other undetected organ injuries, an epiphenomenon, thereby being useful as a signal for increased likelihood of readmission and long-term survival. While the renal injury may not be substantial enough to significantly impair toxin excretion and electrolyte balance, AKI, as an epiphenomenon, may be contributing to adverse outcomes by virtue of other affected organ systems.(10, 16) It is unknown whether this notion is valid. However, it is also likely that injuring the kidney during or after cardiac surgery may cause more rapid progression of kidney disease(22) and result in injury to other organs, therefore supporting the need of biomarker evaluation in readmission.(23, 24)
Our study also has notable strengths. Ascertainment of readmission is commonly a problem in epidemiological investigations, often limited to readmission occurring to the same site. Readmission to other facilities is often missing in most analyses.(3) We, however, linked our cohort with both Medicare in-patient claims and state all-payer in-patient claims to provide the most complete ascertainment of readmission possible. We also report on the association of AKI severity and long-term outcomes using a multi-centered regional collaborative. We identified and evaluated the association of AKIN stage as a severity index for 5-year readmission and 5-year mortality following adult cardiac surgery. These efforts provide the cardiac surgical community with a simple tool for pre-discharge screening of long-term risk of readmission and mortality. Further research is needed in this area to understand the pathophysiology of decompensated renal function and long-term events, such as readmission and mortality occurring well after the index cardiac surgery. In addition, novel approaches to prevent renal injury in the peri- and post-operative setting must continue to be developed and evaluated in cardiac surgery.
Conclusions
We discovered that AKI severity, using the AKIN stage criteria, is associated with a significantly increased risk of 5-year readmission and 5-year mortality following cardiac surgery. Our findings suggest that efforts to reduce AKI may have significant long-term impact for patients and payers on survival and health care utilization.
Acknowledgments
Research was supported by the National Heart Lung and Blood Institute R01HL119664 (PI:Brown).
List of Abbreviations
- AKI
Acute Kidney Injury
- AKIN
Acute Kidney Injury Network
- CABG
Coronary Artery Bypass Grafting
- CI
Confidence Interval
- CMS
Centers for Medicare & Medicaid Services
- HR
Hazard Ratio
- HRRP
Hospital Readmission Reduction Program
- IABP
Intra-Aortic Balloon Pump
- NNE
Northern New England Cardiovascular Disease Study Group
- OR
Odds Ratio
- pRBC
packed Red Blood Cells
- ResDAC
Research Data Assistance Center (at the Centers for Medicare & Medicaid Services)
- RIFLE
Risk, Injury, Failure, Loss of function, End-stage renal disease (criteria for classifying AKI)
- STS
Society of Thoracic Surgeons
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Brock J, Mitchell J, Irby K, et al. Association between quality improvement for care transitions in communities and rehospitalizations among medicare beneficiaries. JAMA : the journal of the American Medical Association. 2013;309(4):381–391. doi: 10.1001/jama.2012.216607. [DOI] [PubMed] [Google Scholar]
- 2.Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA : the journal of the American Medical Association. 2013;309(4):355–363. doi: 10.1001/jama.2012.216476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the medicare fee-forservice program. N Engl J Med. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 4.Litmathe J, Kurt M, Feindt P, Gams E, Boeken U. Predictors and outcome of icu readmission after cardiac surgery. Thorac Cardiovasc Surg. 2009;57(7):391–394. doi: 10.1055/s-0029-1185852. [DOI] [PubMed] [Google Scholar]
- 5.Angelelli J, Gifford D, Intrator O, Gozalo P, Laliberte L, Mor V. Access to postacute nursing home care before and after the bba. Balanced budget act. Health Aff (Millwood) 2002;21(5):254–264. doi: 10.1377/hlthaff.21.5.254. [DOI] [PubMed] [Google Scholar]
- 6.Vives M, Wijeysundera D, Marczin N, Monedero P, Rao V. Cardiac surgery-associated acute kidney injury. Interactive cardiovascular and thoracic surgery. 2014;18(5):637–645. doi: 10.1093/icvts/ivu014. [DOI] [PubMed] [Google Scholar]
- 7.Brown JR, Cochran RP, Dacey LJ, et al. Perioperative increases in serum creatinine are predictive of increased 90-day mortality after coronary artery bypass graft surgery. Circulation. 2006;114(1 Suppl):I409–I413. doi: 10.1161/CIRCULATIONAHA.105.000596. [DOI] [PubMed] [Google Scholar]
- 8.Brown JR, Cochran RP, MacKenzie TA, et al. Long-term survival after cardiac surgery is predicted by estimated glomerular filtration rate. The Annals of thoracic surgery. 2008;86(1):4–11. doi: 10.1016/j.athoracsur.2008.03.006. [DOI] [PubMed] [Google Scholar]
- 9.Brown JR, Malenka DJ, DeVries JT, et al. Transient and persistent renal dysfunction are predictors of survival after percutaneous coronary intervention: Insights from the dartmouth dynamic registry. Catheter Cardiovasc Interv. 2008;72(3):347–354. doi: 10.1002/ccd.21619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brown JR, Parikh CR, Ross CS, et al. Impact of perioperative acute kidney injury as a severity index for thirty-day readmission after cardiac surgery. The Annals of thoracic surgery. 2014;97(1):111–117. doi: 10.1016/j.athoracsur.2013.07.090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goldenberg I, Chonchol M, Guetta V. Reversible acute kidney injury following contrast exposure and the risk of long-term mortality. Am J Nephrol. 2009;29(2):136–144. doi: 10.1159/000151772. [DOI] [PubMed] [Google Scholar]
- 12.Thakar CV, Parikh PJ, Liu Y. Acute kidney injury (aki) and risk of readmissions in patients with heart failure. Am J Cardiol. 2012;109(10):1482–1486. doi: 10.1016/j.amjcard.2012.01.362. [DOI] [PubMed] [Google Scholar]
- 13.Magnus PC, Chaisson K, Kramer RS, et al. Causes of 30-day readmission after cardiac surgery in northern new england. Circulation. 2011;124(21):A13474. [Google Scholar]
- 14.Shehata N, Forster A, Li L, et al. Does anemia impact hospital readmissions after coronary artery bypass surgery? Transfusion. 2012 doi: 10.1111/trf.12007. [DOI] [PubMed] [Google Scholar]
- 15.Mehta RL, Kellum JA, Shah SV, et al. Acute kidney injury network: Report of an initiative to improve outcomes in acute kidney injury. Critical care (London, England) 2007;11(2):R31. doi: 10.1186/cc5713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brown JR, Kramer RS, Coca SG, Parikh CR. Duration of acute kidney injury impacts long-term survival after cardiac surgery. The Annals of thoracic surgery. 2010;90(4):1142–1148. doi: 10.1016/j.athoracsur.2010.04.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brown JR, Parikh CR, Ross CS, et al. Impact of perioperative acute kidney injury as a severity index for thirty-day readmission after cardiac surgery. The Annals of thoracic surgery. 2014;97(1):111–117. doi: 10.1016/j.athoracsur.2013.07.090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patel UD, Greiner MA, Fonarow GC, Phatak H, Hernandez AF, Curtis LH. Associations between worsening renal function and 30-day outcomes among medicare beneficiaries hospitalized with heart failure. American heart journal. 2010;160(1):132–138. e131. doi: 10.1016/j.ahj.2010.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Logeart D, Tabet JY, Hittinger L, et al. Transient worsening of renal function during hospitalization for acute heart failure alters outcome. International journal of cardiology. 2008;127(2):228–232. doi: 10.1016/j.ijcard.2007.06.007. [DOI] [PubMed] [Google Scholar]
- 20.Shirakabe A, Hata N, Kobayashi N, et al. Long-term prognostic impact after acute kidney injury in patients with acute heart failure. International heart journal. 2012;53(5):313–319. doi: 10.1536/ihj.53.313. [DOI] [PubMed] [Google Scholar]
- 21.Shahian DM, He X, O'Brien SM, et al. Development of a clinical registry-based 30-day readmission measure for coronary artery bypass grafting surgery. Circulation. 2014;130(5):399–409. doi: 10.1161/CIRCULATIONAHA.113.007541. [DOI] [PubMed] [Google Scholar]
- 22.Chawla LS, Amdur RL, Amodeo S, Kimmel PL, Palant CE. The severity of acute kidney injury predicts progression to chronic kidney disease. Kidney Int. 2011;79(12):1361–1369. doi: 10.1038/ki.2011.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ronco C, Haapio M, House AA, Anavekar N, Bellomo R. Cardiorenal syndrome. Journal of the American College of Cardiology. 2008;52(19):1527–1539. doi: 10.1016/j.jacc.2008.07.051. [DOI] [PubMed] [Google Scholar]
- 24.Scheel PJ, Liu M, Rabb H. Uremic lung: New insights into a forgotten condition. Kidney Int. 2008;74(7):849–851. doi: 10.1038/ki.2008.390. [DOI] [PubMed] [Google Scholar]