Abstract
Background
Co-occurrence of depression, anxiety, and hazardous drinking is high in clinical samples. Hazardous drinking can worsen depression and anxiety symptoms (and vice versa), yet less is known about whether reductions in hazardous drinking improve symptom outcomes.
Methods
Three hundred and seven psychiatry outpatients were interviewed (baseline, 3-, 6-months) for hazardous drinking (drinking over recommended daily limits), depression (PHQ-9), and anxiety (GAD-7) as part of a hazardous drinking intervention trial. Longitudinal growth models tested associations between hazardous drinking and symptoms (and reciprocal effects between symptoms and hazardous drinking), adjusting for treatment effects.
Results
At baseline, participants had moderate anxiety (M=10.81; SD=10.82) and depressive symptoms (M=13.91; SD=5.58); 60.0% consumed alcohol at hazardous drinking levels. Over 6-months, participants’ anxiety (B=−3.03, p<.001) and depressive symptoms (B=−5.39, p<.001) improved. Continued hazardous drinking led to slower anxiety (B=0.09, p=.005) and depressive symptom (B=0.10, p=.004) improvement; reductions in hazardous drinking led to faster anxiety (B=−0.09, p=.010) and depressive (B=−0.10, p=.015) symptom improvement. Neither anxiety (B=0.07, p=.066) nor depressive (B=0.05, p=.071) symptoms were associated with hazardous drinking outcomes.
Limitations
Participants were psychiatry outpatients, limiting generalizability.
Conclusions
Reducing hazardous drinking can improve depression and anxiety symptoms but continued hazardous use slows recovery for psychiatry patients. Hazardous drinking-focused interventions may be helpful in promoting symptom improvement in clinical populations.
Keywords: Depression, Alcohol, Hazardous drinking, Anxiety
1. Introduction
Co-occurrence of depression, anxiety, and hazardous drinking (drinking over recommended daily limits) is prevalent in the general population (Grant et al., 2004), and even more common among psychiatry patients (Sullivan et al., 2005). Hazardous drinking is problematic because it can impede treatment, raise the risk of escalation for alcohol problems, and lead to poor mental health outcomes (Kuo et al., 2006; Mills et al., 2009). To date, considerable work has examined relations between hazardous drinking, anxiety, and depression, and document findings important to symptom recovery. Hazardous drinking can interfere with psychosocial functioning and precipitates stressful interpersonal problems (Kung, 2000), which can in turn worsen mental health outcomes (Bell et al., 2015). Clinical investigations also report hazardous drinking as a risk factor for depression (Boschloo et al., 2012), and that continued alcohol consumption worsens anxiety and depressive symptoms (Schuckit and Hesselbrook, 1994). One study found patients treated for alcohol use disorder showed improvement (decreases) in symptoms following abstinence (Brown and Schuckit, 1988), indicating a potential association between reductions in alcohol consumption to symptom improvement. Such findings suggest that while hazardous drinking exacerbates symptoms, reductions in hazardous drinking may contribute to symptom improvement.
Studies report that anxiety and depressive symptoms can lead to higher alcohol intake, potentially consumed to reduce psychological distress or ‘self-medicate’ (Conner et al., 2009). Supporting the ‘self-medication’ model, a recent general population study tested bi-directional effects (alcohol consumption drives changes in general mental health and vice versa) of relations between mental health and heavy drinking, and found that mental health was the leading indicator of change (Bell et al., 2015). Whether similar findings would emerge in a clinical sample of psychiatry patients is largely unknown.
Studies have identified several ways alcohol intake potentially influences symptoms (and vice versa) in clinical samples, yet few have examined whether reduction in hazardous drinking contributes to improvement in anxiety and depression symptoms over time. Evidence to this in a clinical sample would signal a need for symptom stabilization efforts on alcohol screening and intervention when needed, which may accelerate recovery. As a primary study aim we examined associations between hazardous drinking and consumption reduction on anxiety and depression symptoms over 6-months in 307 psychiatric outpatients. Given the potential for bidirectional effects, we also explored associations between anxiety, depression, and hazardous drinking outcomes. Such findings would indicate that symptoms worsen hazardous drinking outcomes; and thus slow the rate of reduction in drinking days over time.
2. Method
2.1. Participants
The 307 participants were selected from a randomized controlled trial of motivational interviewing (MI) in alcohol/drug use treatment for depression (Satre et al., 2016). Patients were recruited from: Kaiser Permanente Southern Alameda Medical Center Department of Psychiatry in Union City and Fremont, California. Inclusion criteria required: age ≥18; ≥5 Patient Health Questionnaire (PHQ-9) (Kroenke et al., 2001); absence of mania/psychosis; drug use (illicit/non-prescribed use) or hazardous drinking ≥3/≥4 drinks/day for women/men within 30 days. These participants were recruited at more conservative hazardous drinking levels than used in general population studies, as psychiatry patients often have medication interactions with alcohol; data were collected at the more widely used ≥4/≥5 drinks/day for women/men (Satre et al., 2016).
These 307 patients comprised our study sample, and we examined hazardous drinking patterns and hazardous drinking reductions on symptom recovery at the more widely used ≥4/≥5 drinks/day levels for women/men, adjusting for treatment effects. We also explored the effect of symptoms on hazardous drinking outcomes.
2.2. Measures
2.2.1. Hazardous drinking and hazardous drinking reductions
Consistent with NIAAA guidelines (NIAAA, 2005), hazardous drinking cut-offs were defined as ≥4/≥5 drinks in a day for women/men. A single-item hazardous drinking screener determined patients’ number of hazardous drinking days in the month before study interviews (baseline, 3-, 6-months); higher values indicated more drinking days at the hazardous drinking level. This screener has been validated as a predictor as substance use disorder risk (Dawson, 2010). Using original values of hazardous drinking days determined at study interviews, a time-varying reduction in hazardous drinking (Δ – hazardous drinking) variable was computed by subtracting hazardous drinking levels in subsequent study periods from levels in prior periods (hazardous drinking at 3 months – hazardous drinking at baseline =Δin hazardous drinking at three months, etc.).
2.2.2. Symptoms
PHQ-9 measured depression 2 weeks prior to each interview; higher scores indicate greater depression (9-items, range 0–27; score >5= at least mild depression) (Kroenke et al., 2001). Generalized Anxiety Disorder (GAD-7) scale measured anxiety in the 2 weeks prior to each interview; higher scores indicate greater anxiety (7-items, range 0–21; score >5= at least mild anxiety) (Spitzer et al., 2006).
2.3. Procedures
Data were collected for a randomized controlled trial of MI in alcohol/drug use treatment for depression. The methods and outcomes of the parent study have been reported (Satre et al., 2016). Eligibility was determined by baseline alcohol/drug use and PHQ-9 score. Demographics were collected at baseline and patients were randomized (MI: 45-min in-person session followed by two 15-min booster sessions; Control: 2-page brochure on substance use risks). Patients were offered $50 gift cards for completing the interviews. Of the 307 participants, 296 (96%) completed the 3-month telephone follow up, 302 (98%) completed the 6-month follow up. The University of California, San Francisco (UCSF) Committee on Human Subjects and the Kaiser Permanente Institutional Review Board approved the procedures. Patients were provided with written informed consent prior to participation.
2.4. Data analysis
We examined: (1) longitudinal associations of participants’ symptoms with time; (2) associations between hazardous drinking, reduction in hazardous drinking and symptoms; and (3) longitudinal associations between symptoms and hazardous drinking. As we are interested in examining change over time for symptom and hazardous drinking outcomes and then identifying differences in rates of change (Raudenbush and Bryk, 2009), we constructed a series of mixed-effects growth models employing restricted maximum likelihood estimation for estimating the parameters of continuous outcomes. This approach to longitudinal data analysis is a form of hierarchical linear modeling for repeated measures data where multiple measurement occasions are nested within persons (Raudenbush and Bryk, 2009). We first constructed unconditional models predicting depression/anxiety measures from time (coded: 0=baseline; 1=3-months; 2=6-months) to examine the overall trajectory of participants’ symptom levels over the follow-up. Subsequently, conditional growth models were constructed predicting symptom outcomes from time and time-varying hazardous drinking. To examine reduction in hazardous drinking on symptom outcomes, we computed growth models predicting symptom outcomes from time and time-varying Δ-hazardous drinking. Finally, to examine associations between symptoms and hazardous drinking outcome, conditional growth models were constructed predicting hazardous drinking from time and time-varying symptoms. Hazardous drinking was examined across all interviews as time-varying predictor and outcome. Conditional growth models included age, gender, MI as time-invariant covariates and psychiatry visits (medication management and/or psychotherapy visits) as a time-varying covariate. Rather than discard partial completers (~4.0% of the sample), the expectation maximization approach was used to handle missing data at the time of analysis. All variables were kept in their original distributions. Analyses were carried out in R version 2.14.2 (R Development Core Team, 2015) and HLM7 (Raudenbush et al., 2005). Statistical significance was defined at p<.05.
3. Results
3.1. Baseline characteristics, levels of hazardous drinking, and symptoms
Seventy percent were women and the average age was 37 (SD=13.18). Sixty percent reported hazardous drinking during baseline interviews and displayed a median of 1 (IQR: 0–4) hazardous drinking days in the prior month. Participants had moderate levels of anxiety (M=10.81; SD=5.16) and depression (M=13.85; SD=5.58). Further information on participants’ characteristics can be found in supplementary Table S1.
3.2. Longitudinal associations between hazardous drinking, reduction in hazardous drinking, and symptoms
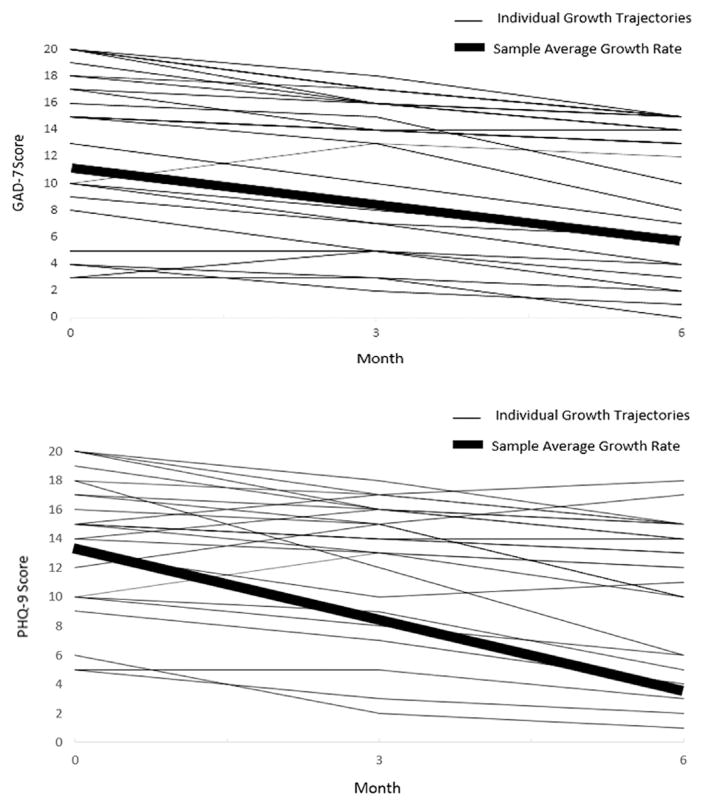
After finding relatively high anxiety and depressive symptom levels among the sample at baseline, we examined the longitudinal trajectories of these symptoms. Unconditional growth model results showed participants’ anxiety (B=−3.03, p<.001) and depressive symptoms (B=−5.39, p<.001) improved (Table 1; Fig. 1). Hazardous drinking was associated with slower anxiety (B=0.09, p=.005) and depressive symptom (B=0.10, p=.004) improvement, whereas reductions in hazardous drinking was associated with faster improvement in anxiety (B=−0.09, p=.010) and depressive (B=−0.10, p=.015) symptoms. Neither the average effect of anxiety (B=0.07, p=.066) nor depressive (B=0.05, p=.071) symptoms were associated with hazardous drinking outcomes (not shown).
Table 1.
Longitudinal predictors of anxiety and depression symptoms for substance misusing psychiatry patients.
| Variable | Depressiona
|
Anxietyb
|
||||||
|---|---|---|---|---|---|---|---|---|
| B | SE | t | p | B | SE | t | p | |
| Unconditional growth model | ||||||||
| Time | −5.39 | 0.34 | −15.70 | <.001 | −3.03 | 0.27 | −10.92 | <.001 |
| Δ – Hazardous drinking conditional growth modelc | ||||||||
| Age | −0.01 | 0.02 | −0.43 | .666 | −0.00 | 0.02 | 0.00 | .998 |
| Female | 2.20 | 0.68 | 3.20 | <.001 | 1.15 | 0.65 | 1.76 | .079 |
| MI treatment | −0.27 | 0.63 | −0.43 | .663 | −0.04 | 0.59 | −0.06 | .945 |
| Time | −4.23 | 1.79 | −2.35 | .019 | −2.92 | 1.50 | −1.94 | .053 |
| Time×age | 0.02 | 0.02 | 1.02 | .305 | −0.02 | 0.02 | −1.16 | .243 |
| Time×female | −1.03 | 0.74 | −1.39 | .164 | 0.07 | 0.62 | 0.12 | .903 |
| Time × MI treatment | 0.47 | 0.70 | 0.67 | .501 | −0.08 | 0.55 | −0.15 | .881 |
| Psychiatry visitsd | 0.17 | 0.08 | 2.13 | .033 | 0.06 | 0.07 | 0.91 | .361 |
| Δ – Hazardous drinkinge | −0.10 | 0.04 | −2.44 | .015 | −0.09 | 0.03 | −2.56 | .010 |
| Hazardous drinking conditional growth modelc | ||||||||
| Age | 0.01 | 0.60 | 0.23 | .816 | −0.00 | 0.02 | −2.22 | .026 |
| Female | 2.43 | 0.66 | 3.67 | <.001 | 1.27 | 0.63 | −0.23 | .810 |
| MI treatment | 0.26 | 0.60 | 0.43 | .663 | 0.26 | 0.57 | 0.45 | .648 |
| Time | −1.88 | 0.60 | −3.10 | .002 | −1.24 | 0.57 | −2.22 | <.001 |
| Time×age | −0.01 | 0.01 | −1.01 | .986 | −0.01 | 0.02 | −0.22 | .824 |
| Time×female | −1.00 | 0.01 | −2.67 | <.001 | −0.00 | 0.01 | −0.12 | .903 |
| Time×MI treatment | −0.40 | 0.33 | 1.18 | .237 | −0.08 | 0.55 | −0.50 | .615 |
| Psychiatry visitsd | −0.07 | 0.05 | −1.30 | .193 | 0.03 | 0.04 | −0.71 | .475 |
| Hazardous drinkingf | 0.10 | 0.03 | 2.84 | .004 | 0.09 | 0.03 | 2.79 | .005 |
B=beta coefficient; SE=standard error; t=t-ratio; p=p-values <.05 are presented in boldface; MI Treatment=motivation interviewing treatment condition.
PHQ-9 total score; higher scores indicate greater depression severity.
GAD-7 total score; higher scores indicate greater anxiety severity.
Conditional growth models were fit using restricted maximum likelihood estimation.
Psychiatry visits=time-varying covariate estimating the number of psychiatry visits prior to each interview.
Δ–Hazardous drinking=time-varying independent variable estimating average reductions in patient hazardous drinking (≥4/≥5 drinks in a day for women/men) days.
Hazardous drinking=time-varying independent variable estimating patient hazardous drinking (≥4/≥5 drinks in a day for women/men) days.
Fig. 1.
Unconditional growth models showing the average improvement in symptoms for the sample (N=307) over 6-months, derived from individual growth trajectories (n=25 displayed) of participant’s symptoms scores over the study duration.
Post-hoc moderator analyses employing mixed-effects growth models explored if the described associations between hazardous drinking and symptoms varied in magnitude by the quantity of drinks patients consumed per occasion. Results showed no significant interactions between hazardous drinking and drinking quantity on anxiety (B=0.01, p=.972) or depression (B=0.01, p=.489). Similarly, we found no significant interactions between hazardous drinking reduction and drinking quantity reduction on anxiety (B=−0.02, p=.111) or depressive (B=−0.03, p=.264) symptoms (not shown).
4. Discussion
Studies have found that hazardous drinking leads to worse symptoms and vice versa, yet few conducted with clinical samples have investigated the association of reduction in hazardous consumption and symptoms over time. Therefore, we studied 307 psychiatric outpatients on their hazardous drinking patterns and reductions in hazardous consumption on anxiety and depression symptom recovery; and also explored the effect of symptoms on hazardous drinking outcomes over 6-months.
Results showed patients’ symptoms were the highest at baseline, and then continued to improve (on average, symptoms decreased in severity) over time. Patients who consumed alcohol at hazardous levels experienced slower symptom recovery; those reducing hazardous drinking experienced faster symptom improvement. We found no evidence of a longitudinal relationship between symptoms and hazardous drinking outcomes.
4.1. Clinical implications
These findings have clinical implications. Our results confirm that hazardous drinking is a prevalent and symptom-destabilizing problem for psychiatry patients, and also indicate that reductions in hazardous consumption can help improve symptoms. It can be inferred that delivering evidence-based brief alcohol interventions (Baker et al., 2012; Satre et al., 2016) to psychiatry patients who consume alcohol at hazardous levels (and introducing alcohol screening measures to ensure hazardous drinking is detected) would have a beneficial effect in terms of accelerating symptom improvement beyond usual psychiatric care alone. Our findings may inform the development of interventions to reduce the health impact of co-occurring hazardous drinking, anxiety, and depression.
This work also provides further support that on-going efforts to improve education for psychiatry patients around alcohol use and hazardous drinking are important (Edlund et al., 2012). Educating patients with hazardous drinking, anxiety, and depression that cutting back on drinking may be useful to help alleviate symptom distress. Perhaps if patients with these co-occurring conditions were aware that ongoing psychiatric distress could be linked to alcohol consumption levels, they would be more likely to consider treatment options to reduce drinking.
4.2. Study limitations
Limitations should be noted. Because our sample was selected from an outpatient psychiatry setting, findings are not directly comparable to recent general population studies that have examined relationships between sub-syndromal symptoms and alcohol use (not problem level consumption) (Bell et al., 2015). Participants were in a randomized controlled trial of MI and had PHQ-9 depression ≥5; potentially further limiting generalizability. We adjusted for treatment effects and psychiatry visits, yet patients could have been participating in treatments we did not account for analytically; and thus, cause-and-effect determinations cannot be made. Hazardous drinking was skewed and may have biased the findings; however, robust methods were used and provide more sensitive tests under these conditions (Raudenbush and Bryk, 2009). We did not have a large enough sample to examine risky substance use other than alcohol. We used standardized measures and general population hazardous drinking levels; yet, further research will be needed to test effects in more generalizable samples to the recent literature on co-occurring hazardous drinking, anxiety, and depression.
5. Conclusions
We found that reducing hazardous drinking can improve symptoms but continued alcohol consumption at hazardous levels slows symptom recovery for psychiatry patients. Our findings suggest that it would be useful for psychiatry service providers to deliver alcohol screening and hazardous-drinking focused interventions when needed to patients with co-occurring anxiety, depression, and hazardous drinking.
Supplementary Material
Acknowledgments
Role of funding source
This study was supported by the National Institute on Alcohol Abuse and Alcoholism (NIAAA: R01 AA020463) and the National Institute on Drug Abuse (NIDA: T32DA007250). The funding sources provided no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
We thank Georgina Berrios for assistance in conducting the study.
Appendix A. Supporting information
Supplementary data associated with this article can be found in the online version at http://dx.doi.org/10.1016/j.jad.2016.07.039.
Footnotes
Contributors
Drs. Bahorik and Satre formulated the research questions and constructed the study design. Dr. Bahorik wrote the first draft of the manuscript and all authors provided critical revisions. All authors contributed to and approved the final manuscript.
Conflict of interest
None.
References
- Baker AL, Thornton KL, Hides L, Lubman DI. Psychological interventions for alcohol misuse among people with co-occurring depression or anxiety disorders: a systematic review. J Affect Disord. 2012;139(3):217–229. doi: 10.1016/j.jad.2011.08.004. [DOI] [PubMed] [Google Scholar]
- Bell S, Orford J, Britton A. Heavy drinking and mental health: an exploration of the dynamic 10-year longitudinal relationship in a prospective cohort of untreated heavy drinkers. Alcohol Clin Exp Res. 2015;39:688–696. doi: 10.1111/acer.12681. [DOI] [PubMed] [Google Scholar]
- Boschloo L, van den Brink W, Penninx BW, Wall MM, Hasin DS. Alcohol-use disorder severity predicts first-incidence of depressive disorders. Psychol Med. 2012;42:695–703. doi: 10.1017/S0033291711001681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown SA, Schuckit MA. Changes in depression among abstinent alcoholics. J Stud Alcohol Drugs. 1988;49:412. doi: 10.15288/jsa.1988.49.412. [DOI] [PubMed] [Google Scholar]
- Conner KR, Pinquart M, Gamble SA. Meta-analysis of depression and substance use among individuals with alcohol use disorders. J Subst Abuse Treat. 2009;37:127–137. doi: 10.1016/j.jsat.2008.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DA, Pulay AJ, Grant BF. A comparison of two single-item screeners for hazardous drinking and alcohol use disorder. Alcohol Clin Exp Res. 2010;34:364–374. doi: 10.1111/j.1530-0277.2009.01098.x. [DOI] [PubMed] [Google Scholar]
- Edlund MJ, Booth BM, Han X. Who seeks care where? Utilization of mental health and substance use disorder treatment in two national samples of individuals with alcohol use disorders. J Stud Alcohol Drugs. 2012;73(4):635–646. doi: 10.15288/jsad.2012.73.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. 2004;61(8):807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kung WW. The intertwined relationship between depression and marital distress: elements of marital therapy conducive to effect treatment outcome. J Marital Fam Ther. 2000;26:51–63. doi: 10.1111/j.1752-0606.2000.tb00276.x. [DOI] [PubMed] [Google Scholar]
- Kuo PH, Gardner CO, Kendler KS, Prescott CA. The temporal relationship of the onsets of alcohol dependence and major depression: using a genetically informative study design. Psychol Med. 2006;36:1153–1162. doi: 10.1017/S0033291706007860. [DOI] [PubMed] [Google Scholar]
- Mills KL, Deady M, Proudfoot H, Sannibale C, Teesson M, Mattick R, Burns L. Guidelines on the Management of Co-occurring Alcohol and Other Drug and Mental Health Conditions in Alcohol and Other Drug Treatment Settings. National Drug and Alcohol Research Centre, University of Sydney; Sydney: 2009. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. Helping patients who drink too much: a clinician’s guide. National Institute on Alcohol Abuse and Alcoholism; Rockville, MD: 2005. updated 2005 edition, NIH Publication No. 04-3769. [Google Scholar]
- R Development Core Team. R Foundation for Statistical Computing (Version 2.14.2) Vienna, Austria: 2015. R: a language and environment for statistical computing. Computer Software. [Google Scholar]
- Raudenbush S, Bryk A, Congdon R. HLM 7 for Windows [Computer Software] Skokie, IL: Scientific Software International, Inc; 2005. [Google Scholar]
- Raudenbush DSW, Bryk DAS. Applications and Data Analysis Methods. 2. Sage; Thousand Oaks, CA: 2009. Hierarchical linear models. [Google Scholar]
- Satre DD, Leibowitz A, Sterling SA, Lu Y, Travis A, Weisner C. A randomized clinical trial of motivational interviewing to reduce alcohol and drug use among patients with depression. J Consult Clin Psychol. 2016;84:510–513. doi: 10.1037/ccp0000096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuckit MA, Hesselbrook V. Alcohol dependence and anxiety disorders: what is the relationship? Am J Psychiatry. 1994;151:1723–1734. doi: 10.1176/ajp.151.12.1723. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JBW, Lowe B. A brief measure for assessing generalized anxiety disorder. Arch Int Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Sullivan LE, Fiellin DA, O’Connor PG. The prevalence and impact of alcohol problems in major depression: a systematic review. Am J Med. 2005;118:330–341. doi: 10.1016/j.amjmed.2005.01.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.