Abstract
Study Design Retrospective comparative study.
Objective To compare strict Biffl criteria to more-liberal criteria for computed tomography angiography (CTA) when screening for blunt cerebrovascular injury (BCVI).
Methods All CTAs performed for blunt injury between 2009 and 2011 at our institution were reviewed. All patients with cervical spine fractures who were evaluated with CTA were included; patients with penetrating trauma and atraumatic reasons for imaging were excluded. We then categorized the patients' fractures based on the indications for CTA as either within or outside Biffl criteria. For included subjects, the percentage of studies ordered for loose versus strict Biffl criteria and the resulting incidences of BCVI were determined.
Results During our study period, 1,000 CTAs were performed, of which 251 met inclusion criteria. Of the injuries, 192 met Biffl criteria (76%). Forty-nine were found to have BCVIs (19.5%). Forty-one injuries were related to fractures meeting Biffl criteria (21.4%), and 8 were related to fractures not meeting those criteria (13.6%). The relative risk of a patient with a Biffl criteria cervical spine injury having a vascular injury compared with those imaged outside of Biffl criteria was 1.57 (p = 0.19).
Conclusions Our data demonstrates that although cervical spine injuries identified by the Biffl criteria trend toward a higher likelihood of concomitant BCVI (21.4%), a significant incidence of 13.6% also exists within the non-Biffl fracture cohort. As a result, a more-liberal screening than proposed by Biffl may be warranted.
Keywords: cervical spine trauma, cervical injury, blunt trauma, blunt cerebrovascular injury, vertebral artery injury, Biffl criteria
Introduction
Recent publications have found that blunt cerebrovascular injuries (BCVIs) are more common than previously thought.1 2 3 4 5 6 7 8 9 10 Once believed to be as infrequent as 0.1% of all blunt trauma cases, recent literature has shown an incidence of 0.24 to 3%.1 2 3 6 7 10 11 12 BCVIs are defined as injures to the carotid or vertebral arteries. Although these injuries are often asymptomatic, symptomatic injuries can be devastating, with reported mortality rates of 21 to 31% and permanent neurologic morbidity rates of 37 to 58%.1 3 6 Various groups found stroke rates of 21 to 64% if BCVIs are left untreated.2 3 4 5 10 13 14 Increased awareness of this potentially devastating problem has led to attempts to identify and treat these injuries earlier.
Four-vessel cerebral angiography (FVCA) has long been the gold standard for BCVI screening. However, computed tomography angiography (CTA) has mostly replaced FVCA due to its lower cost, fewer complications, and reduced resource requirements. The increased availability of this noninvasive screening tool has led to the clinical question, which blunt trauma patients should be screened? Many current screening guidelines are based on the criteria created by Biffl et al,3 4 5 13 who recommended screening of midface fractures, basilar skull fractures, diffuse axonal injury, cervical hematoma or abrasion, lateralizing neurologic changes, Glasgow comma scale (GCS) scores less than 6 to 8, and specific cervical spine fractures (C1–C3 fractures, vertebral body fractures, fractures through the transverse foramen, or fractures resulting in ligamentous injury or facet subluxation). At our institution, we have adopted more-liberal screening criteria to include all cervical spine fractures including those considered low risk by Biffl and coworkers.
We sought to compare the rates of BCVI detected by CTA of the cervical spine based on cervical spine fractures in patients who meet Biffl criteria and those who did not.
Materials and Methods
This study was approved by our institutional review board (no. 0006635) We retrospectively reviewed all cervical CTAs performed at our institution between December 2009 and December 2011. Patients who did not have any trauma and those who had a penetrating trauma were excluded. Patient charts were reviewed for sex, age, cervical spine injuries, CTA findings including Biffl grade (Table 1), and treatment(s) provided. We then categorized those patients' fractures according to the criteria by Biffl et al into a Biffl criteria fracture group and a non-Biffl fracture group.3 4 5 These groups were then compared for incidence and type of BCVI. We also went back and reviewed those non-Biffl fractures and determined if they met Biffl criteria for other reasons and evaluated those groups separately. The one exception was that at our institution we do not use GCS alone as an indication for BCVI workup, and we did not separate non-Biffl criteria fractures back into Biffl criteria solely on GCS because there are frequent trauma patients with low scores who do not receive CTAs at our institution.
Table 1. Denver Grading Scale for blunt cerebrovascular injuries.
| Grade | Scale |
|---|---|
| I | Irregularity of the vessel wall or dissection/intramural hematoma with <25% luminal stenosis |
| II | Intraluminal thrombus or raised intimal flap, or dissection/intramural hematoma with ≥25% luminal stenosis |
| III | Pseudoaneurysms |
| IV | Vessel occlusion |
| V | Vessel transection |
Imaging
All patients were imaged for cervical spine injuries under the trauma algorithm with computed tomography on a Seimens Emotion 8 slice, a Seimens Emotion 16 slice, or a Seimens High Definition Dual Source 64/128 slice scanner (Siemens Medical Solutions USA, Inc., Malvern, Pennsylvania, United States) or patients had an outside scan that was confirmed to have a cervical spine fracture by a board-certified attending radiologist. If they were found to meet BCVI screening criteria, patients subsequently underwent a CTA on either the Seimens Emotion 16 slice or Seimens High Definition Dual Source 64/128 scanner and again their imaging was reviewed by a board-certified attending radiologist to confirm a BCVI.
Data Analysis
Data was stored and managed with Microsoft Excel 2011 (Microsoft, Redmond, Washington, United States), and statistical analysis was performed using R statistical software (R Foundation for Statistical Computing, Vienna, Austria) to calculate the incidences of the vascular injuries and the relative risks (prevalence risk ratios). The 95% confidence intervals with mid p values were determined using bootstrap.
Results
From December 2009 through December 2011, 1,000 CTAs were performed at our institution. Of these imaging studies, 749 were excluded for penetrating trauma or no cervical spine fractures, leaving 251 CTAs of the cervical spine after blunt trauma for evaluation. The cohort contained 174 males and 77 females with an average age of 46.9 years (range 6.7 to 94.7 years) (Table 2). Of these 251 patients, 192 patients' cervical spine injuries met Biffl criteria (76%). Of those screened, 49 were found to have BCVIs (49/251, screening yield 19.5%; Fig. 1). Forty-one injuries were related to fractures meeting Biffl criteria (41/192, screening yield 21.4%), and 8 were related to fractures not meeting those criteria (8/59, screening yield 13.6%; Figs. 2 and 3, Table 3). The relative risk of a patient with a Biffl criteria cervical spine injury having a vascular injury compared with those imaged under more-liberal criteria was 1.57 (95% confidence interval 0.67 to 4.68, p = 0.19). After isolating those fractures that did not meet Biffl fracture criteria, we re-evaluated to see if they met other Biffl criteria for BCVI workup despite CTAs being ordered for non-Biffl cervical spine fractures. In doing so, we isolated 8 additional Biffl workups and 1 injury to give us 202 patients meeting Biffl criteria with 44 injuries (44/202, screening yield 21.8%), which left us with 7 injuries related to non-Biffl criteria that were imaged for cervical spine fractures (7/51, screening yield 13.7%). After regrouping, the relative risk of having a BCVI in the Biffl group was 1.52 (95% confidence interval 0.81 to 4.44), but this result was not significant (p = 0.25).
Table 2. Patient demographics.
| Demographic | n |
|---|---|
| Male | 174 (69%) |
| Female | 77 (31%) |
| Age (y) | |
| Average | 47.0 |
| Minimum | 6.7 |
| Maximum | 94.7 |
| Mechanism of injury | |
| MVC | 163 (126 B, 37 NB) |
| Fall | 37 (31 B, 6 NB) |
| MCC | 27 (17 B, 10 NB) |
| Pedestrian versus car | 9 (8 B, 1 NB) |
| Moped | 5 (2 B, 3 NB) |
| Diving injury | 2 (1 B, 1 NB) |
| Bicycle | 2 (1 B, 1 NB) |
| Crush | 1 (1 B, 0 NB) |
| Horse | 1 (1 B, 0 NB) |
| Bull-related injury | 1 (1 B, 0 NB) |
| Assault | 1 (1 B, 0 NB) |
| Football injury | 1 (1 B, 0 NB) |
| Pedestrian versus train | 1 (1 B, 0 NB) |
Abbreviations: B, Biffl criteria fracture; MCC, motorcycle collision; MVC, motor vehicle collision; NB, non-Biffl criteria cervical fracture.
Fig. 1.
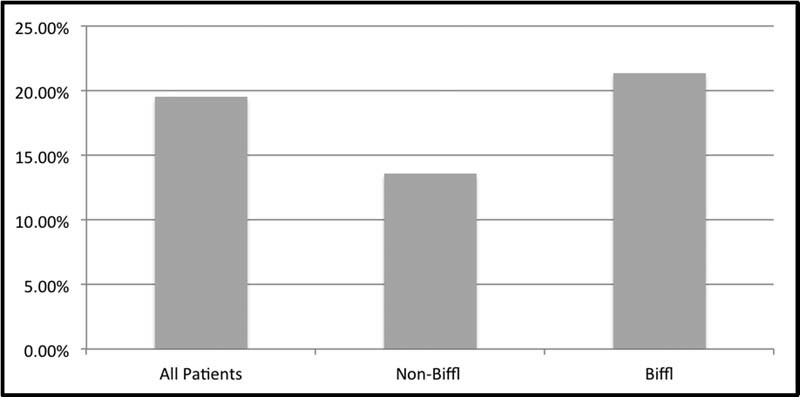
Blunt cerebrovascular injury incidences for computed tomography angiography screening from December 2009 through December 2011.
Fig. 2.
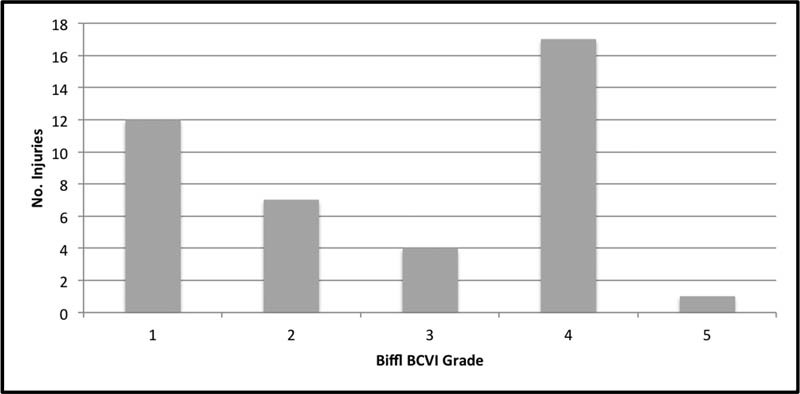
Blunt cerebrovascular injury (BCVI) grades for Biffl criteria cervical spine fractures determined by computed tomography angiography from December 2009 through December 2011.
Fig. 3.
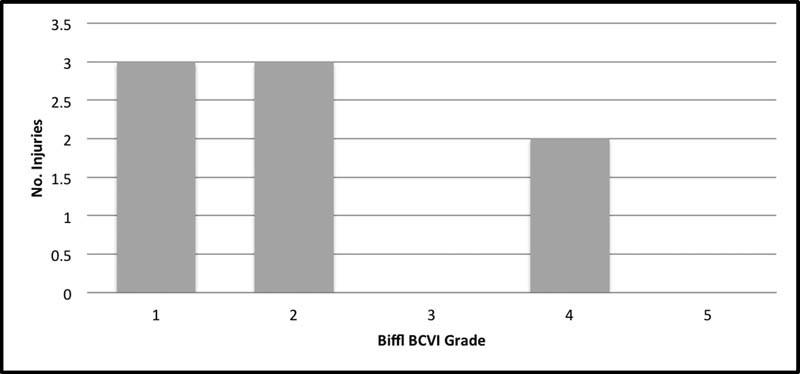
Blunt cerebrovascular injury (BCVI) grades for non-Biffl criteria cervical spine fractures determined by computed tomography angiography from December 2009 through December 2011.
Table 3. Subjects with non-Biffl criteria cervical spine fracture with blunt cerebrovascular injuries.
| Age (y) | Sex | Mechanism of injury | Cervical spine fracture | Blunt cerebrovascular injury | Biffl grade | Treatment |
|---|---|---|---|---|---|---|
| 27.3 | M | Fall | Left C5 inferior articular facet and lamina fractures with associated fractures of the left superior articular facet of C6 and T1 | Left vertebral artery dissection with thrombus resulting in occlusion of the left vertebral artery from thoracic inlet to C2 level | 4 | Heparin drip to aspirin |
| 55.8 | M | MVC | Left C5 inferior articular facet and left C6 superior articular facet fractures | Bilateral vertebral artery narrowing focally at the C5 level bilaterally without evidence of occlusion | 2 | Heparin drip to clopidogrel |
| 29.6 | M | MCC | Right C5 lateral mass fracture | Left proximal vertebral artery high-grade narrowing likely on the basis of dissection along the C5–C7 levels | 2 | Heparin drip to aspirin |
| 50.9 | M | Fall | Right C6 lamina fracture with extension into right facet joint | Right vertebral artery narrowing of 25% narrowing at the C4–C5 level | 1 | Heparin drip to nothing on discharge |
| 34.9a | M | MCC | Left C6 and C7 transverse process fractures | Left internal carotid artery focal dissection at the C1 level without high-grade stenosis and long-segment luminal irregularity of the right internal carotid artery without high-grade stenosis | 2 | None secondary to intracranial hemorrhage |
| 36.2 | M | MVC | Left C6 nondisplaced lamina fracture with extension into facet joint | Left vertebral artery luminal irregularity at level of C6 level | 1 | Clopidogrel |
| 78.8 | M | Fall | Right C7 lamina fracture with extension into articular facet and C6 anterior listhesis | Right vertebral artery dissection with less than 25% narrowing at C6–C7 level | 1 | Heparin drip to aspirin |
| 59.2 | M | MVC | Left C6 and C7 nondisplaced transverse processes fractures | Left vertebral artery occlusion just distal to origin of artery | 4 | Aspirin |
Abbreviations: MCC, motorcycle collision; MVC, motor vehicle collision.
Only non-Biffl criteria cervical spine fracture that met screening criteria based on other factors for midface fractures.
Of the fractures meeting Biffl criteria, 26 (53%) involved the C1–C3, 15 (31%) involved the vertebral body, 24 (49%) involved the transverse foramen, 11 (22%) involved facet subluxation, and 5 (10%) were ligamentous injuries of the spine. Of those patients, 21 patients met 2 criteria (51.2%), 9 patients met 3 criteria (12.2%), and 3 patients met 4 criteria (9.8%) (Fig. 4). For the non-Biffl cervical spine fractures, all 8 that resulted in vascular injury involved the C5, C6, and/or C7 lamina, facets, or posterior elements. The one patient with a non-Biffl criteria cervical fracture with a vascular injury, which met other Biffl criteria, had C6 and C7 transverse process fractures but extensive facial fractures (Table 3).
Fig. 4.
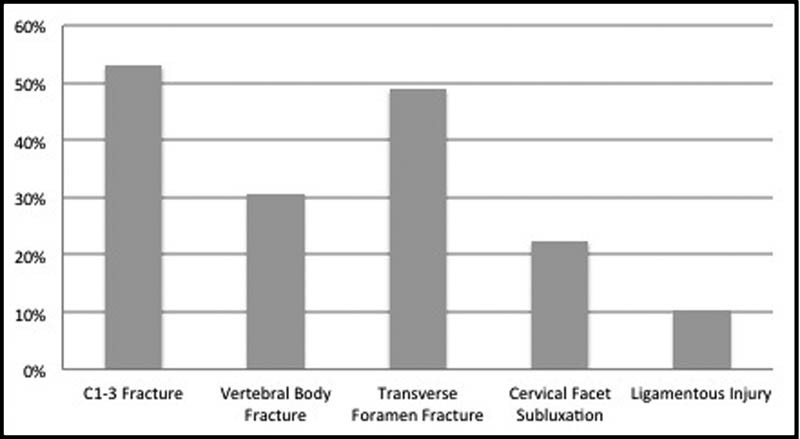
Biffl criteria cervical spine fracture breakdown for those patients who met Biffl Criteria and were found to have a blunt cerebrovascular injury from December 2009 through December 2011.
Discussion
The screening for and management of patients with BCVIs has been a subject of interest over the last two decades. Injuries that were once thought to be very rare have been shown to be more common.1 2 3 4 5 6 7 8 9 10 Originally, patients were screened for injury only if they had neurologic symptoms. With the risk for severe neurologic morbidity or mortality after BCVI, attempts were made to diagnose and intervene before the onset of symptoms.1 3 6 BCVIs have a 10-hour to 72-hour asymptomatic period, during which neurologic sequelae can be prevented by systemic anticoagulation or surgical intervention.14
The symptom-free window along with the ability to prevent significant morbidity and mortality in patients with BCVI has led to significant study of this problem. Despite this attention in the literature, there is no one set of screening criteria, and those that exist have been in a process of refinement. The screening criteria set by Biffl and Cothren are generally accepted, though some authors support more-liberal screening guidelines and others like Mayberry et al support less-aggressive screening.6 9 More-liberal screening ensures fewer missed injuries; however, it comes at an increased cost both monetarily and in the form of radiation exposure.
Traditionally the FVCA was the gold standard for screening for BCVI. However, FVCA is resource intensive and has a 1 to 3% rate of complications, including arterial occlusion (0.2%), hematoma (0.5%), pseudoaneurysm (0.2%), contrast nephropathy (0.2 to 2%), infection, radiation exposure, transient ischemic attack (2.5%), or stroke (1%).3 7 10 11 14 To avoid these complications, other imaging modalities have been explored including duplex Doppler, magnetic resonance angiography, and CTA. To date, CTA has been the most widely accepted substitute due to its noninvasive nature, decreased cost, speed, three-dimensional analysis, and wide availability.1 11 12 13
Biffl et al originally found that CTA was of low yield in blunt trauma with a sensitivity of 47 to 68% and a specificity of 67%. This finding was supported by others, who found specific sensitivities of 44 to 47% and 50 to 53% for carotid and vertebral artery injures.10 14 15 However, this result has improved with the advent of multidetector CTA. More recent reports have found the sensitivity and specificity have improved to 40 to 96% and 90 to 97% for vertebral injury and 67 to 100% and 88 to 98% for carotid injury.12 14 15 With the newer technology, the tests require less time, contrast load, and radiation compared with angiography.14 Despite the improvement in technology, CTA still has a relatively high false-positive rate (43% in the study by Malhotra et al),12 so caution should be taken for overdiagnosis of injuries.3 12 14 Since the switch from FVCA to CTA as the first-line screening test, immediate complications have been drastically reduced. However, at this institution unpublished data has shown that the radiation exposure for a trauma patient who undergoes BCVI screening is increased by 31 to 57%.
Several studies have utilized the criteria proposed by Biffl et al, but there has been some debate about screening for cervical fractures.1 2 3 5 6 7 8 10 Initially, any patient with spinal fractures was screened for BCVI, because a 39 to 46% incidence of vertebral artery injury was associated with spinal fractures in general without a specific relationship between vertebral artery injury and any specific types or levels of fracture.10
Over time, the screening indications for vascular injury in patients with cervical spine trauma have been narrowed. Miller et al suggested a relationship of BCVI with fractures extending into the transverse foramen or with associated facet subluxation. Based on these findings, Miller et al suggested that all other fractures could be ignored for screening.10 Subsequently, Cothren et al in 2003 reported that fractures of the upper spine from C1 to C3 had an 87% rate of vertebral artery injury and should be added to the criteria for screening.4 5 They found those injuries comprised 73% of cervical spine fractures and had a 37% rate of BCVI. By limiting screening to just those three injury patterns, they would have been able to eliminate 77 angiograms (13%) from their study of 605 cases.4 5
Our study had an overall incidence of BCVI of 19.5% for all patients screened with cervical spine fractures, which is comparable to other studies.6 8 9 10 11 12 13 14 15 We additionally found a nonsignificant difference between those patients who had fractures that met Biffl criteria (21.4%) and those with fractions that did not meet Biffl criteria (13.6%, p = 0.19), which would suggest that screening based on a limited number of fracture morphologies is not appropriate and will lead to significant numbers of missed BCVIs.
The retrospective nature of this study was a limitation in that we only reviewed those patients who were screened and then determined if a cervical fracture was present, which did not always allow us to confirm the indication for ordering the CTA. When we went back and reincluded non-Biffl criteria fractures in the Biffl criteria group if they met other workup noncervical spine fracture criteria to include midface fractures, basilar skull fractures, diffuse axonal injury, cervical hematoma/ abrasion, or lateralizing neurologic changes, our data remained largely unchanged. This data again demonstrated a 21.0% rate of CTA-documented BCVI for patients meeting Biffl criteria and 13.7% for patients with no identifiable Biffl criteria, with the CTA likely ordered due to presence of non-Biffl criteria cervical spine fracture (p = 0.32).
In our study, our goal was to evaluate the specific incidence of missed injuries based on strict versus loose criteria pertaining to cervical spine fractures, and from our results we propose that even if a larger series made the screening criteria difference statistically significant, a 13.6 or 13.7% incidence of missed BCVIs is clinically significant. This recommendation for looser criteria for specifically cervical spine fractures has been more recently supported by Jacobson et al, who showed an incidence of missed BCVI of 37% when limiting to Denver criteria and instead screened all patients with blunt trauma already receiving at CT of the cervical spine and/or CTA of the chest with a CTA of the neck.16
Treatment was not a primary goal for this study, and for that reason, no recommendations based on this study can be made. In the literature, there is still significant controversy regarding treatment, with some advocating that antiplatelet medications are equivalent to anticoagulation,8 9 17 but others continue to support full anticoagulation as the first-line treatment when not contraindicated as they continue to believe and support the research that shows decreased rates of poor neurologic outcomes and associated morbidity/mortality.1 3 6 10 With there still being no clear answer, we at our institution based on these findings and our experience along with the above literature have sided with aggressive treatment with full anticoagulation in an attempt to decrease rates of secondary neurologic sequelae. However, there is always a balance for treatment in trauma patients. If a patient has an operative fracture, the treatment of the vascular injury has to be balanced with the risk of the surgical complications from anticoagulation. It has been the tradition at our institution to then defer anticoagulation to the surgeon's preference, letting the clinical situation dictate the algorithm based on fracture morphology and treatment plan weighed against the BCVI grade.
As listed above, our study was limited by its retrospective nature and the justification for screening. Another limitation of the study was that CTA was performed at the discretion of the ordering physician, which means that we cannot exclude the possibility that some patients with cervical spine fractures may not have been screened. This issue could be problematic for our data if the patient had minor non-Biffl cervical spine fractures that did not trigger the physician to order a CTA, which would have affected our results.
Conclusions
Though once believed to be rarely associated with vascular injury, blunt cervical trauma cases need to be considered for vascular injury because of the risk of neurologic sequelae. Early detection and intervention have been shown to decrease overall morbidity and mortality, making screening for BCVI important. Screening criteria for BCVI are still being debated. Our study suggests that a subset of patients not meeting Biffl criteria have BCVI. Widening the screening criteria to include all spine fractures may detect BCVI that may otherwise be missed and possibly lead to neurologic sequelae.
Future Directions
In an effort to minimize the number of patients with missed BCVIs, future prospective multicenter studies to better evaluate criteria for screening patients are needed. Prospective studies elucidating patients who are at higher risk will help to reduce the risks of screening with CTA and their increased cost while preventing significant morbidity and mortality in patients with missed BCVI.
Disclosures
Gregory Grabowski: Consultant (DePuy/Synthes)
Ryan N. Robertson: Travel expenses (Stryker)
Blair M. Barton: none
Mark A. Cairns: none
Sharon W. Webb: none
Note
This study has been presented as a paper presentation (paper# 692) at the 2014 AAOS Annual Meeting in New Orleans, Louisiana. No contributors to this paper have any conflicts of interest or received any funding for this project except for a scholarly grant after the completion of this study by Stryker to present this material at the AAOS Annual Meeting.
References
- 1.Baker W E, Wassermann J. Unsuspected vascular trauma: blunt arterial injuries. Emerg Med Clin North Am. 2004;22(4):1081–1098. doi: 10.1016/j.emc.2004.05.009. [DOI] [PubMed] [Google Scholar]
- 2.Berne J D, Cook A, Rowe S A, Norwood S H. A multivariate logistic regression analysis of risk factors for blunt cerebrovascular injury. J Vasc Surg. 2010;51(1):57–64. doi: 10.1016/j.jvs.2009.08.071. [DOI] [PubMed] [Google Scholar]
- 3.Biffl W L, Cothren C C, Moore E E. et al. Western Trauma Association critical decisions in trauma: screening for and treatment of blunt cerebrovascular injuries. J Trauma. 2009;67(6):1150–1153. doi: 10.1097/TA.0b013e3181c1c1d6. [DOI] [PubMed] [Google Scholar]
- 4.Cothren C C, Moore E E, Biffl W L. et al. Cervical spine fracture patterns predictive of blunt vertebral artery injury. J Trauma. 2003;55(5):811–813. doi: 10.1097/01.TA.0000092700.92587.32. [DOI] [PubMed] [Google Scholar]
- 5.Cothren C C, Moore E E, Ray C E Jr, Johnson J L, Moore J B, Burch J M. Cervical spine fracture patterns mandating screening to rule out blunt cerebrovascular injury. Surgery. 2007;141(1):76–82. doi: 10.1016/j.surg.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 6.Kerwin A J, Bynoe R P, Murray J. et al. Liberalized screening for blunt carotid and vertebral artery injuries is justified. J Trauma. 2001;51(2):308–314. doi: 10.1097/00005373-200108000-00013. [DOI] [PubMed] [Google Scholar]
- 7.Fabian T C, Croce M A, Minard G. et al. Current issues in trauma. Curr Probl Surg. 2002;39(12):1160–1244. doi: 10.1067/msg.2002.128499. [DOI] [PubMed] [Google Scholar]
- 8.Lebl D R, Bono C M, Velmahos G, Metkar U, Nguyen J, Harris M B. Vertebral artery injury associated with blunt cervical spine trauma: a multivariate regression analysis. Spine (Phila Pa 1976) 2013;38(16):1352–1361. doi: 10.1097/BRS.0b013e318294bacb. [DOI] [PubMed] [Google Scholar]
- 9.Mayberry J C Brown C V Mullins R J Velmahos G C Blunt carotid artery injury: the futility of aggressive screening and diagnosis Arch Surg 20041396609–612., discussion 612–613 [DOI] [PubMed] [Google Scholar]
- 10.Miller P R Fabian T C Croce M A et al. Prospective screening for blunt cerebrovascular injuries: analysis of diagnostic modalities and outcomes Ann Surg 20022363386–393., discussion 393–395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Berne J D Reuland K S Villarreal D H McGovern T M Rowe S A Norwood S H Sixteen-slice multi-detector computed tomographic angiography improves the accuracy of screening for blunt cerebrovascular injury J Trauma 20066061204–1209., discussion 1209–1210 [DOI] [PubMed] [Google Scholar]
- 12.Malhotra A K Camacho M Ivatury R R et al. Computed tomographic angiography for the diagnosis of blunt carotid/vertebral artery injury: a note of caution Ann Surg 20072464632–642., discussion 642–643 [DOI] [PubMed] [Google Scholar]
- 13.Biffl W L Egglin T Benedetto B Gibbs F Cioffi W G Sixteen-slice computed tomographic angiography is a reliable noninvasive screening test for clinically significant blunt cerebrovascular injuries J Trauma 2006604745–751., discussion 751–752 [DOI] [PubMed] [Google Scholar]
- 14.Burlew C C, Biffl W L. Imaging for blunt carotid and vertebral artery injuries. Surg Clin North Am. 2011;91(1):217–231. doi: 10.1016/j.suc.2010.10.004. [DOI] [PubMed] [Google Scholar]
- 15.Bub L D, Hollingworth W, Jarvik J G, Hallam D K. Screening for blunt cerebrovascular injury: evaluating the accuracy of multidetector computed tomographic angiography. J Trauma. 2005;59(3):691–697. [PubMed] [Google Scholar]
- 16.Jacobson L E, Ziemba-Davis M, Herrera A J. The limitations of using risk factors to screen for blunt cerebrovascular injuries: the harder you look, the more you find. World J Emerg Surg. 2015;10:46. doi: 10.1186/s13017-015-0040-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alterman D M Heidel R E Daley B J et al. Contemporary outcomes of vertebral artery injury J Vasc Surg 2013573741–746., discussion 746 [DOI] [PubMed] [Google Scholar]


