Abstract
Study Design Retrospective case series.
Objective To describe the perioperative complications (0 to 90 days) associated with pedicle subtraction osteotomies (PSOs) performed at a tertiary spine center by two experienced spine surgeons who recently adopted the technique.
Methods We reviewed all 65 patients (47 women and 18 men; mean age 60 years, range 24 to 80) who underwent a PSO at our institution. Descriptive data and analysis of complications were limited to the perioperative time (within 90 days of surgery). Data analyzed included operative time, length of stay (LOS), estimated blood loss (EBL), blood products, comorbidities, neurologic complications, and medical complications. Complications were rated as major and minor. Radiographic data was also analyzed.
Results Ten patients (15.4%) had a major complication, and 15 (23%) had a minor complication. There were three perioperative deaths. The most common major complication was neurologic deficit (6.2%, 4/65), three with a permanent foot drop, and one with paraplegia secondary to postoperative hematoma. There were no differences between patients with and without a major complication in regard to age, gender, comorbidities, operative time, number of levels fused, and EBL (p > 0.05). Patients with a major complication had a longer intensive care unit stay (p = 0.04). There was no difference in the rate of major complications between the initial and later cases performed.
Conclusion The major complication rate for pedicle subtraction osteotomy was 15% and the minor complication rate was 23%. The most common major complication was neurologic deficit in 6.2%. The complication rate did not change with increased surgeon experience.
Keywords: pedicle subtraction osteotomy, perioperative complications, adult spinal deformity, early complications
Introduction
Several studies over the last decade have reported on the use of the pedicle subtraction osteotomy (PSO) to correct sagittal and coronal deformity.1 2 3 4 5 6 7 8 9 10 Few studies specifically evaluate the perioperative complications related to this procedure.5 8 11 12 13 The reports that detail the complications of PSO originate out of a few major centers that were instrumental in perfecting and teaching the technique. As the use of this technique disseminates from the originators to other tertiary spine centers, the rate of complications may change. It is important to evaluate the complications of a newer surgical technique as its use spreads to those with less experience in the specific technique. The purpose of our study was to describe the perioperative complications (0 to 90 days) associated with PSOs performed at a tertiary spine center by two experienced spine surgeons who have more recently adopted the technique.
Methods
After International Review Board approval was obtained, we retrospectively reviewed our spine database for all patients who had undergone a PSO of the lumbar spine at our institution from 1999 to 2011 (Fig. 1). All procedures were performed by the two senior authors (M.D.D., D.S.B.) at one institution. Our surgical technique followed the description by Bridwell et al utilizing a standard Jackson frame, a high-speed drill, curettes and osteotomes for creation of the osteotomy, and thrombin-soaked collagen sponge as a hemostatic agent.14 The PSO was closed using a combination of compression and sagittal in situ bending of two rods across the osteotomy. Additional rod fixation (i.e., two additional rods across the PSO) was added at the surgeon's discretion but not routinely used in this series of patients. The PSOs were performed at T12 (2), L1 (2), L2 (17), L3 (33), L4 (9), and L5 (2). All patients who underwent a PSO at our institution were included in the study, and none were excluded. Both senior authors had greater than 10 years of experience as spine surgeons before performing their first PSO procedure. We recorded patient demographics, diagnosis, comorbidities, complications, estimated blood loss (EBL), blood products received, operative time, intensive care unit (ICU) stay, hospital stay, number of levels fused, number of prior surgeries, and radiographic cervical C7 plumb line (sagittal vertical axis) as well as pre- and postoperative pelvic parameters (Tables 1, 2, 3).
Fig. 1.
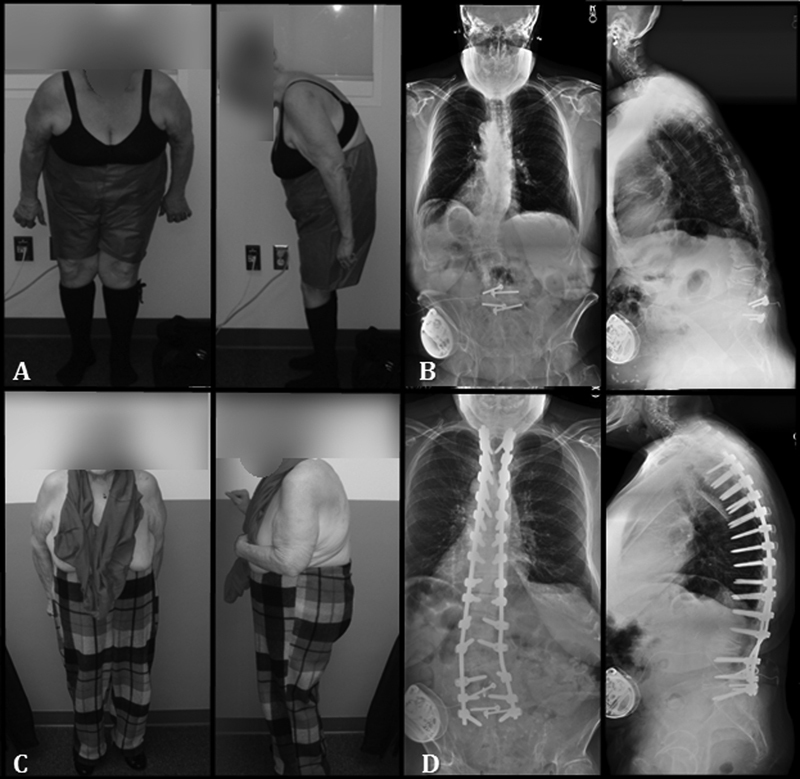
(A) Preoperative clinical images and (B) posteroanterior and lateral 36-inch standing radiographs of a 64-year-old woman with a previous L4–S1 fusion who presented with severe lumbar stenosis, neurogenic claudication, and inability to stand upright. (C, D) Post–pedicle subtraction osteotomy clinical and radiographic images showing improvement of both coronal and sagittal alignment.
Table 1. Sample statistics.
| Variable | n (%) | Range | Mean |
|---|---|---|---|
| Male | 12 (18) | ||
| Female | 53 (82) | ||
| Age at surgery (y) | 24–80 | 60 | |
| Follow up (mo) | 2–133 | 26 | |
| Duration of surgery (min) | 256–768 | 438 | |
| No. of levels fused | 3–16 | 8 | |
| ICU stay | 0–5 | 1 | |
| Hospital stay (d) | 3–24 | 7.6 | |
| Estimated blood loss (mL) | 450–9,000 | 2,371 | |
| Intraoperative (U) | 0–14 | 2 | |
| Perioperative (U) | 0–59 | 3 | |
| Intraoperative blood salvage (mL) | 250–4,000 | 1,130 | |
| Preoperative C7 plumb line | −44–293 | 118 | |
| Postoperative C7 plumb line | −44–175 | 53 | |
| Preoperative lumbar lordosis | 28 to −59 | −16 | |
| Postoperative lumbar lordosis | −15 to −73 | −41 | |
| Perioperative deaths | 3 (4.6) | ||
| Prior surgeries | 55 (84.6) | ||
| 1 | 16 (24.6) | ||
| 2 | 12 (18.4) | ||
| 3 | 6 (9.2) | ||
| 4 | 21 (32.3) | ||
| Comorbidities | 56 (86.1) | 1.78 | |
| 1 | 21 (32.3) | ||
| 2 | 17 (26.1) | ||
| 3 | 12 (18.4) | ||
| 4 | 5 (6) | ||
| 5 | 1 (1) | ||
| Minor complications | 15 (23) | ||
| 1 | 12 (18.4) | ||
| 2 | 1 (1.5) | ||
| 3 | 2 (3) | ||
| Major complications | 10 (15.4) | ||
| 1 | 8 (12.3) | ||
| 2 | 1 (1.5) | ||
| 4 | 1 (1.5) | ||
| Postoperative complications (major + minor) | 20 (30.8) | ||
| 1 | 12 (18.4) | ||
| 2 | 5 (7.7) | ||
| 3 | 1 (1.5) | ||
| 4 | 1 (1.5) | ||
| 5 | 1 (1.5) | ||
| Revision surgeries | 22 (33.8) | ||
| <3 mo | 11 (16.9) | ||
| >3 mo | 11 (16.9) |
Abbreviation: ICU, intensive care unit.
Table 2. Patient comorbidities.
| Patient comorbidity | n (%) |
|---|---|
| Hypertension | 35 (53.8) |
| Peptic ulcer disease | 14 (21.5) |
| Hypothyroid disease | 18 (27.7) |
| Carcinoma in remission | 8 (12.3) |
| Asthma/COPD | 12 (18.5) |
| Coronary artery disease | 4 (6.2) |
| Diabetes | 5 (7.7) |
| Obesity | 8 (12.3) |
| Renal disease | 1 (1.5) |
| Substance abuse | 3 (4.6) |
| Coagulopathy | 5 (7.7) |
| Hepatitis | 3 (4.6) |
Abbreviation: COPD, chronic obstructive pulmonary disease.
Table 3. Diagnoses.
| Diagnosis | n |
|---|---|
| Acquired kyphosis | 17 |
| Fixed sagittal imbalance | 23 |
| Fixed sagittal imbalance + degenerative scoliosis | 12 |
| Fixed sagittal imbalance +adult idiopathic scoliosis | 13 |
| Total | 65 |
We categorized the complications as major and minor. The major complications included neurologic deficit, deep wound infection, myocardial infarct, pneumonia, respiratory distress, deep vein thrombosis, pulmonary embolus, and death. Minor complications included ileus, superficial infection, urinary tract infection, arrhythmias, epidural hematoma, and superficial deep vein thrombosis. Intraoperative complications included excessive blood loss (>3,000 mL), dural tear, and vascular injury. We analyzed the data for relationships between the presence of a major complication and patient and clinical variables and surgeon experience with performing PSOs between 1999 and 2011.
Our analysis included 65 patients (53 women and 12 men), with a mean age of 60 years (range 24 to 80) and mean follow-up of 41 months (range 2 to 166). The diagnosis included acquired kyphosis (17), fixed sagittal imbalance (FSI) (23), FSI and degenerative scoliosis (12), and FSI and adult idiopathic scoliosis (13; Table 3). Patient comorbidities are listed in Table 2.
Student t test was used to analyze the radiographic C7 plumb line lumbar sagittal alignment data and pelvic parameters data. Wilcoxon rank sum was utilized to analyze data that was not normally distributed.
Results
Sample statistics including the number of minor and major complications are listed in Table 1. The mean duration of surgery was 438 minutes (range 256 to 768), the mean ICU stay was 1 day (range 0 to 5), and the mean hospital stay was 7.6 days (range 3 to 24). The mean EBL was 2,371 mL (range 450 to 9,000). A mean of 2 U of packed red blood cells was given during surgery, and a mean of 3 U of packed red blood cells was given in the perioperative period. A mean of 1,130 mL of salvaged red blood cells was given (range 250 to 4,000). The mean value of pelvic incidence was 59 degrees. The mean values of sacral slope were 24 degrees preoperatively and 32 degrees postoperatively (p < 0.001), and the values of pelvic tilt were 35 degrees preoperatively and 27 degrees postoperatively (p < 0.001). The mean C7 plumb line preoperatively was 118 mm and postoperatively was 53 mm (p < 0.001). The mean lumbar lordosis was −16 degrees preoperatively and −41 degrees postoperatively (p < 0.001), for a mean correction of 25 degrees.
Eighty-four percent (55/65) of our patients had at least 1 prior surgery, and 60% (39/65) had 2 or more prior surgeries (Table 1). Eighty-six percent (56/65) had at least 1 comorbidity, and 51% (35/65) had 2 or more comorbidities present at the time of surgery.
Either a major or a minor complication occurred in 31% (20/65) of patients. Major complications occurred in 15% (10/65) of patients, and minor complications occurred in 23% (15/65). There were 3 perioperative deaths: 1 patient died secondary to a pedicle screw placed in the L1 vertebral body where an aberrant aortic artery had eroded into the vertebral body and 2 patients died postdischarge secondary to narcotic pain medication overdose. The most common major complication was neurologic deficit in 6.2% (4/65): 3 had a permanent foot drop, and 1 had paraplegia secondary to postoperative hematoma. The incidence of each major, minor, and intraoperative complication is listed in Table 4. Overall, there were 11 reoperations: 3 patients with deep postoperative wound infections with 2 of them requiring 2 irrigations and debridements (5), 2 patients requiring hardware revision, 2 patients with acute proximal functional failure, 1 patient with a epidural hematoma, and 1 patient with acute postoperative hemorrhage secondary to a screw placed in the aberrant aortic artery (who later died). There was no significant relationship between any of the patient and clinical variables and the presence of a major complication, except for the length of ICU stay (p = 0.04; Table 5). The incidence of major complications collected from 1999 to 2011 was evaluated, and no temporal correlations were noted between the PSOs that were performed early versus those performed late in our study period.
Table 4. Complications.
| Complications | n (%) |
|---|---|
| Major (<3 mo) | 14 (21.5) |
| Neurologic deficit | 4 (6.2) |
| Deep wound infection | 3 (4.6) |
| Myocardial infarction | 1 (1.5) |
| Pneumonia | 2 (3) |
| Respiratory distress syndrome | 1 (1.5) |
| Perioperative death | 3 (4.6) |
| Minor complications (<3 mo) | 20 (30.8) |
| Ileus | 6 (9.2) |
| Superficial infection | 4 (6.2) |
| UTI | 5 (7.7) |
| Arrhythmias | 3 (4.6) |
| Superficial DVT | 1 (1.5) |
| Epidural hematoma | 1 (1.5) |
| Intraoperative complications | 15 (23) |
| Excessive blood loss | 4 (6.1) |
| Dural tears | 12 (18.4) |
| Vascular injury | 1 (1.5) |
Abbreviations: DVT, deep vein thrombosis; UTI, urinary tract infection.
Table 5. Relationship of patient and clinical variables to the presence of a major complication.
| Variable | 95% CI | p Value |
|---|---|---|
| EBL | 1544.34–2,995.66 | 0.7328b |
| Age | 52.52–66.28 | 0.3801b |
| Operative time | 378.31–559.29 | 0.3827b |
| Follow-up | 224.07–620.37 | 0.1156b |
| No. levels fused | 1.1–3.9 | 0.0860b |
| No. comorbidities | 1–2.2 | 0.9035b |
| Previous surgeries | −1.58–11.58 | 0.7669b |
| ICU stay | 0.62–1.19 | 0.0438b |
| Pre C7 plumb line | 29.29–287.91 | 0.2025a |
| Pre lumbar lordosis | −35.08–2.79 | 0.8885a |
| Coronal curve | −2.66 to −0.61 | 0.5540b |
t test.
Wilcoxon rank sum.
Abbreviations: EBL, estimated blood loss; ICU, intensive care unit; Pre, preoperative.
Discussion
The reporting of results and complications with the technique of PSO has come primarily from centers that originated and perfected this complex procedure.4 5 6 12 As with many surgical techniques, the results and complications of PSO may differ between surgeons and centers that have varying degrees of experience with the technique. The purpose of our study was to evaluate the perioperative complications associated with PSO at a tertiary spine center in which the technique was recently adopted.
Our technical results were similar to prior studies as evidenced by our radiographic and sagittal correction data. Our mean improvement in lumbar lordosis was 25 degrees, compared with 30 degrees reported by Berven et al,4 33 degrees by Bridwell et al,5 and 24 degrees by Ahn et al.6
Our perioperative data is comparable to previous reports on PSO. If we compare the operative time, EBL, blood products transfused, and hospital stay, our mean operative time (7.3 hours) was less than that reported by Bridwell et al (12.2 hours)5; however, they included total operative time, which included patients who underwent combined anteroposterior fusion. Our mean EBL (2,371 mL) was similar to that reported by Bridwell et al (2,386 mL)5 but less than that reported by Ahn et al (3,520 mL).6 Our mean hospital stay (7.6 days) was lower than that in previous studies.6 Operative and perioperative blood transfusions were similar across studies.5
Comprehensive data including the perioperative complications has been rarely reported in prior studies. Ahn et al reported 28 intraoperative complications in 25 patients.6 The highest reported complication was dural tear (17 patients). Two patients had nerve root injuries. Our rate of dural tear was 18.4%. Overall, they reported 55 complications in 38 patients. The most common complications were instrumentation-related, followed by pseudarthrosis and pneumonia. Five patients had neurologic deficits (6%), which was similar to our rate of neurologic deficits of 6.2%, but higher than the 2.8% reported at long-term follow-up by Buchowski et al.12
PSOs are performed most commonly as revision procedures in middle-aged and older women. The mean age of the patients in our study was 60 years; in the study by Bridwell et al, 53.4 years; and in the study by Ahn et al, 54.4 years. In our study, 85% of our patients had at least one prior spine surgery, which was similar to other reports.4 5 6 When we analyzed patients with major complications, age and revision were not significant factors (Table 5). However, this data may be impacted by the fact that most of our patients were over 50 years of age and most had prior surgery. If we compare our data with that reported for longer fusions in the older population, the complication rates are similar.15 The only correlation of a major complication in our study that was significant was length of ICU stay, which was not surprising as the major complication likely resulted in an increase of ICU days required.
Our perioperative death rate was higher than that reported in other studies and highlights the psychosocial and technical complexity of patients undergoing multiple-revision spine surgery due to deformity. We had three deaths within the 90-day postoperative period. One was surgically related to an aberrant aortic artery that had eroded into the L1 vertebral body after multiple-revision spine surgery. This complication occurred prior to the initiation of the PSO during routine placement of an L1 pedicle screw that violated the aberrant aortic artery. The other two were due to narcotic pain medication overdose in the postdischarge period.
Overall, our complication rates are similar to that reported out of centers with the initial experience in performing PSOs. The senior surgeons in our study were both experienced (>10 years) spine surgeons prior to performing their first PSOs, and the complication profiles were not temporally correlated with increased experience in performing this procedure. Inexperienced spine surgeons may have different results when initially performing this complex procedure.
Our study is limited because it was retrospective and did not have controls for potential confounding factors. One strength of our study is that we included all patients who underwent a PSO at our institution and we captured all perioperative complications.
Conclusion
Our perioperative complication rates were similar to those previously reported from the initial centers with experience performing PSOs. The complications were not related to age, operative time, number of levels fused, prior surgeries, presence of comorbidities, or increased surgeon experience in performing this procedure.
Footnotes
Disclosures Michael D. Daubs: none Darrel S. Brodke: none Prokopis Annis: none Brandon D. Lawrence: none
References
- 1.Kim K T, Park D H, Lee S H, Suk K S, Lee J H, Park K J. Partial pedicle subtraction osteotomy as an alternative option for spinal sagittal deformity correction. Spine (Phila Pa 1976) 2013;38(14):1238–1243. doi: 10.1097/BRS.0b013e31828e0e56. [DOI] [PubMed] [Google Scholar]
- 2.Cho K J, Kim K T, Kim W J. et al. Pedicle subtraction osteotomy in elderly patients with degenerative sagittal imbalance. Spine (Phila Pa 1976) 2013;38(24):E1561–E1566. doi: 10.1097/BRS.0b013e3182a63c29. [DOI] [PubMed] [Google Scholar]
- 3.Scheer J K, Lafage V, Smith J S. et al. Maintenance of radiographic correction at 2 years following lumbar pedicle subtraction osteotomy is superior with upper thoracic compared with thoracolumbar junction upper instrumented vertebra. Eur Spine J. 2015;24(1) 01:S121–S130. doi: 10.1007/s00586-014-3391-y. [DOI] [PubMed] [Google Scholar]
- 4.Berven S H, Deviren V, Smith J A, Emami A, Hu S S, Bradford D S. Management of fixed sagittal plane deformity: results of the transpedicular wedge resection osteotomy. Spine (Phila Pa 1976) 2001;26(18):2036–2043. doi: 10.1097/00007632-200109150-00020. [DOI] [PubMed] [Google Scholar]
- 5.Bridwell K H, Lewis S J, Edwards C. et al. Complications and outcomes of pedicle subtraction osteotomies for fixed sagittal imbalance. Spine (Phila Pa 1976) 2003;28(18):2093–2101. doi: 10.1097/01.BRS.0000090891.60232.70. [DOI] [PubMed] [Google Scholar]
- 6.Ahn U M, Ahn N U, Buchowski J M. et al. Functional outcome and radiographic correction after spinal osteotomy. Spine (Phila Pa 1976) 2002;27(12):1303–1311. doi: 10.1097/00007632-200206150-00011. [DOI] [PubMed] [Google Scholar]
- 7.Chen I H, Chien J T, Yu T C. Transpedicular wedge osteotomy for correction of thoracolumbar kyphosis in ankylosing spondylitis: experience with 78 patients. Spine (Phila Pa 1976) 2001;26(16):E354–E360. doi: 10.1097/00007632-200108150-00010. [DOI] [PubMed] [Google Scholar]
- 8.Hyun S J, Rhim S C. Clinical outcomes and complications after pedicle subtraction osteotomy for fixed sagittal imbalance patients: a long-term follow-up data. J Korean Neurosurg Soc. 2010;47(2):95–101. doi: 10.3340/jkns.2010.47.2.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim K T, Lee S H, Suk K S, Lee J H, Jeong B O. Outcome of pedicle subtraction osteotomies for fixed sagittal imbalance of multiple etiologies: a retrospective review of 140 patients. Spine (Phila Pa 1976) 2012;37(19):1667–1675. doi: 10.1097/BRS.0b013e3182552fd0. [DOI] [PubMed] [Google Scholar]
- 10.Yang B P, Ondra S L, Chen L A, Jung H S, Koski T R, Salehi S A. Clinical and radiographic outcomes of thoracic and lumbar pedicle subtraction osteotomy for fixed sagittal imbalance. J Neurosurg Spine. 2006;5(1):9–17. doi: 10.3171/spi.2006.5.1.9. [DOI] [PubMed] [Google Scholar]
- 11.Ikenaga M, Shikata J, Takemoto M, Tanaka C. Clinical outcomes and complications after pedicle subtraction osteotomy for correction of thoracolumbar kyphosis. J Neurosurg Spine. 2007;6(4):330–336. doi: 10.3171/spi.2007.6.4.8. [DOI] [PubMed] [Google Scholar]
- 12.Buchowski J M, Bridwell K H, Lenke L G. et al. Neurologic complications of lumbar pedicle subtraction osteotomy: a 10-year assessment. Spine (Phila Pa 1976) 2007;32(20):2245–2252. doi: 10.1097/BRS.0b013e31814b2d52. [DOI] [PubMed] [Google Scholar]
- 13.Barrey C, Perrin G, Michel F, Vital J M, Obeid I. Pedicle subtraction osteotomy in the lumbar spine: indications, technical aspects, results and complications. Eur J Orthop Surg Traumatol. 2014;24(1) 01:S21–S30. doi: 10.1007/s00590-014-1470-8. [DOI] [PubMed] [Google Scholar]
- 14.Bridwell K H, Lewis S J, Rinella A, Lenke L G, Baldus C, Blanke K. Pedicle subtraction osteotomy for the treatment of fixed sagittal imbalance. Surgical technique. J Bone Joint Surg Am. 2004;86-A 01:44–50. doi: 10.2106/00004623-200403001-00007. [DOI] [PubMed] [Google Scholar]
- 15.Daubs M D, Lenke L G, Cheh G, Stobbs G, Bridwell K H. Adult spinal deformity surgery: complications and outcomes in patients over age 60. Spine (Phila Pa 1976) 2007;32(20):2238–2244. doi: 10.1097/BRS.0b013e31814cf24a. [DOI] [PubMed] [Google Scholar]


