Abstract
Study Design Survey study.
Objective To determine the global perspective on controversial aspects of sacral fracture classifications.
Methods While developing the AOSpine Sacral Injury Classification System, a survey was sent to all members of AOSpine and AOTrauma. The survey asked four yes-or-no questions to help determine the best way to handle controversial aspects of sacral fractures in future classifications. Chi-square tests were initially used to compare surgeons' answers to the four key questions of the survey, and then the data was modeled through multivariable logistic regression analysis.
Results A total of 474 surgeons answered all questions in the survey. Overall 86.9% of respondents felt that the proposed hierarchical nature of injuries was appropriate, and 77.8% of respondents agreed that that the risk of neurologic injury is highest in a vertical fracture through the foramen. Almost 80% of respondents felt that the separation of injuries based on the integrity of L5–S1 facet was appropriate, and 83.8% of surgeons agreed that a nondisplaced sacral U fracture is a clinically relevant entity.
Conclusion This study determines the global perspective on controversial areas in the injury patterns of sacral fractures and demonstrates that the development of a comprehensive and universally accepted sacral classification is possible.
Keywords: sacral fracture, sacral injury, AOSpine, AOTrauma, sacral classification, pelvis trauma
Introduction
Sacral fractures are complex injuries that rarely occur in isolation,1 2 3 and therefore they often require a multidisciplinary treatment approach including orthopedic trauma surgeons and spine surgeons (either orthopedic surgeons or neurosurgeons). Many classifications have been proposed for sacral fractures, but none are comprehensive or universally accepted.4 5 6 7 8 9 The development of a comprehensive, reliable, and universally accepted classification of these fractures is critical to allow for effective communication between treating physicians and trainees as well as researchers; furthermore, a well-designed classification may lead to the development of an optimal treatment algorithm for these challenging injuries.
The existing sacral injury classifications are based on either fracture morphology or an inferred mechanism of injury. The existing systems are either very broad and simplistic, such as the commonly used Denis classification that separates fractures broadly based on the location of the fracture with respect to the foramen, or they are exceedingly specific so that they can only be applied to a very select type of sacral fracture, such as the Isler classification, which is only relevant for a vertical fracture through the foramen. Alternatively, sacral fractures may be incorporated into pelvic injury classifications, but despite being one of the critical structures involved in posterior pelvic ring stability,10 only a rudimentary evaluation of sacral injuries is considered in pelvic fracture classifications.8 Finally, despite the fact that the treatment decisions are often affected by the neurologic status of the patient and associated soft tissue injuries, none of the existing classifications formally consider these variables.4 5 6 7 8 9
Recognizing the limitations of the existing classifications, the AOSpine Trauma Knowledge Forum is partnering with pelvic trauma experts from AOTrauma to develop a comprehensive sacral fracture classification similar to the AOSpine Thoracolumbar Injury Classification System and the AOSpine Subaxial Cervical Spine Injury Classification System.11 12 13 14 Importantly, one of the main goals of this project is to develop a classification system that will achieve global acceptance from both spine surgeons and orthopedic traumatologists. However, given the complexity of sacral fractures, multiple controversial areas will have to be addressed. In an effort to develop a classification that will be able to obtain global acceptance, a survey was sent to all AOSpine and AOTrauma members and their input was sought on controversial aspects of sacral fracture classification. The goal of this study is to determine the global perspective on controversial aspects of sacral fractures.
Methods
In July 2015, a survey (see Appendix A in online supplementary material) was sent to all members of AOSpine and AOTrauma. The survey was only sent out a single time, and each e-mail address was only permitted to answer the survey once. The survey included four simple yes-or-no questions. Along with demographic information including region, experience, and specialty, the following four questions were asked:
Do you think that the appropriate order for sacral fracture severity from least to most severe is transverse fractures, unilateral vertical fractures, and fractures that lead to spinopelvic instability?
In an isolated vertical fracture of the sacrum, do you agree that the risk of neurologic injury is highest in a vertical fracture through the foramen and lowest in a vertical fracture medial to the foramen?
Do you think the integrity of the L5–S1 facet is adequately considered if a unilateral vertical fracture where the ipsilateral superior S1 facet is discontinuous with the medial portion of the sacrum is considered differently from a fracture where the ipsilateral superior S1 facet is in continuity with the medial portion of the sacrum? (See Fig. 1.)
Do you think a nondisplaced sacral U fracture that may be seen in low-energy insufficiency fractures is a clinically relevant entity that deserves its own spot in a classification?
Fig. 1.
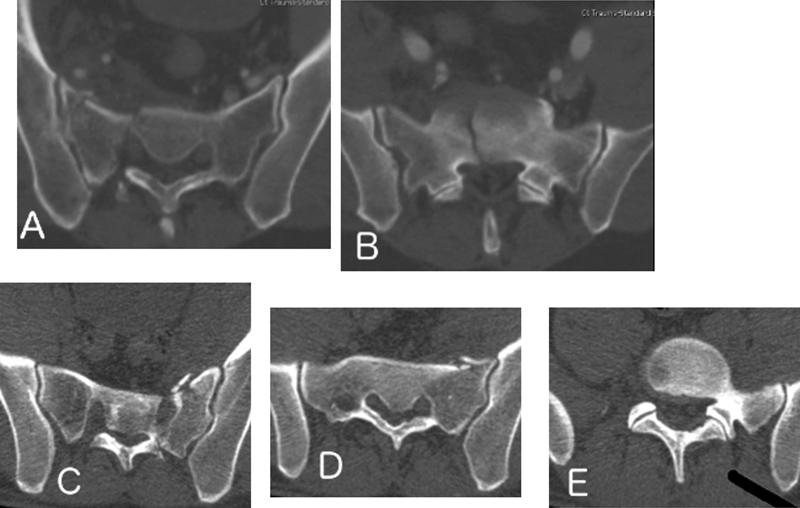
(A) Axial computed tomography (CT) image displaying a vertical fracture through the foramen. (B) Axial CT image of the same fracture at the cephalad aspect of the sacrum, demonstrating that the fracture exits medial to the L5–S1 facet. (C) Axial CT image of the sacrum demonstrating a vertical fracture through the sacral foramen. (D) Fracture exiting the sacrum into the sacroiliac joint. (E) Intact L5–S1 facet that is in continuity with the sacrum.
Chi-square tests were initially used to compare the surgeons' answers to the four key questions of the survey. Further on, the data was modeled through multivariable logistic regression analysis. Specifically, four logistic regression models were performed, with AO Region, specialization, years of clinical practice, and number of traumatic sacral fractures treated by the surgeon in the previous year considered as independent variables, whereas each one of the four key questions was used as the dependent variable. The statistical significance was determined by p ≤ 0.05. All statistical analyses were performed using SAS version 9.2 (SAS Institute Inc., Cary, North Carolina, United States).
Results
The survey was sent to 15,229 AOSpine and AOTrauma members; 671 surgeons (4.4%) from all six AO regions of the world responded to the survey, and 474 surgeons (3.1%) answered every question. The analysis of the results is based on respondents who answered all the questions. Respondents had varying experience and specialties. Table 1 presents the complete demographic data of the respondents. Overall, 86.9% of respondents felt that there was an increase in severity as fractures moved from a transverse fracture to a unilateral vertical fracture, and finally to a fracture that results in spinopelvic instability; 77.8% of respondents thought that in an isolated vertical fracture of the sacrum, the risk of neurologic injury is highest in a vertical fracture through the foramen and lowest in a vertical fracture medial to the foramen. Almost 4/5 of the respondents felt that it was appropriate to consider a unilateral vertical fracture where the ipsilateral superior S1 facet is discontinuous with the medial portion of the sacrum differently from a fracture where the ipsilateral superior S1 facet is in continuity with the medial portion of the sacrum, and 83.8% of surgeons agreed that a nondisplaced sacral U fracture is a clinically relevant entity that deserves its own spot in the classification (Fig. 2).
Table 1. Demographics of survey respondents.
| Characteristic | n (%) |
|---|---|
| Specialty | 474 |
| Orthopedic trauma surgeon | 350 (73.8) |
| Orthopedic spine surgeon | 95 (20.0) |
| Neurosurgeon | 29 (6.1) |
| Specialization (orthopedic spine surgeon and neurosurgeon combined) | 474 |
| Trauma surgeon | 350 (73.8) |
| Spine surgeon | 124 (26.2) |
| Years of clinical practice | 474 |
| 0–10 | 200 (42.2) |
| 11–20 | 149 (31.4) |
| > 20 | 125 (26.4) |
| AO region | 474 |
| Africa | 4 (0.8) |
| Asia Pacific | 77 (16.2) |
| Europe | 197 (41.6) |
| Latin/South America | 89 (18.8) |
| Middle East | 49 (10.3) |
| North America | 58 (12.2) |
| Number of traumatic sacral fractures the surgeon treated last year (four categories) | 474 |
| 0–5 | 256 (54.0) |
| 6–10 | 86 (18.1) |
| 11–20 | 62 (13.1) |
| > 20 | 70 (14.8) |
Fig. 2.
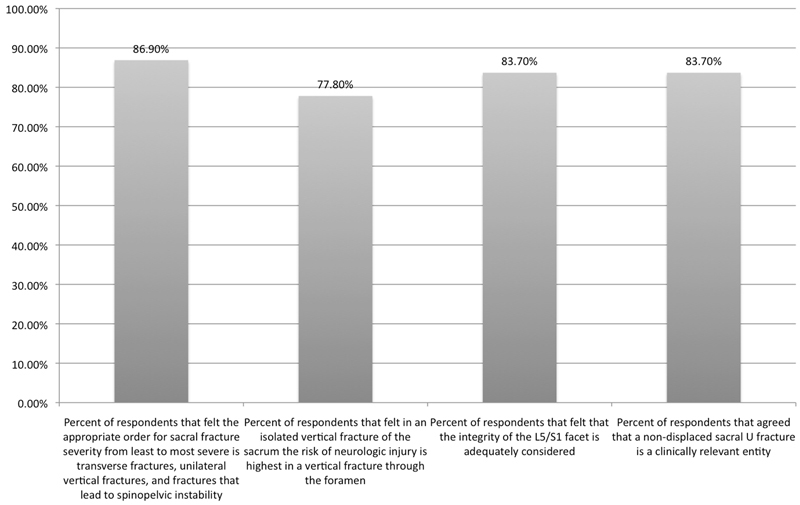
Overall results of the survey suggest that there is widespread agreement with the proposed morphologic classification of sacral fractures.
When the results were stratified by region (Table 2), the regional differences were seen in the responses to the question concerning the risk to neurologic injury with vertical sacral fractures (p = 0.014) and the question concerning the integrity of the L5–S1 facet (p = 0.039). Specifically, only 62.1% of surgeons from North America agreed that the risk of neurologic injury is highest in a vertical fracture through the foramen and lowest in a vertical fracture medial to the foramen, and although this number represents almost two thirds of all North American surgeons, it is substantially lower than the rest of the world. Additionally, although 69.4% of the surgeons from the Middle East felt that the integrity of the L5–S1 facet was adequately considered if a unilateral vertical fracture where the ipsilateral superior S1 facet is discontinuous with the medial portion of the sacrum is considered differently from a fracture where the ipsilateral superior S1 facet is in continuity with the medial portion of the sacrum, this number was substantially less than surgeons from every other region in the world.
Table 2. Regional analysis of the survey results.
| Yes responses, n (%) | ||||||
|---|---|---|---|---|---|---|
| Characteristics | Asia Pacific (n = 77) | Europe (n = 197) | Latin/South America (n = 89) | Middle East (n = 49) | North America (n = 58) | p Valuea |
| Do you think that the appropriate order for sacral fracture severity from least to most severe is transverse fractures, unilateral vertical fractures, and fractures that lead to spinopelvic instability? | 66 (85.7) | 173 (87.8) | 77 (86.5) | 38 (77.6) | 54 (93.1) | 0.204 |
| In an isolated vertical fracture of the sacrum, do you agree that the risk of neurologic injury is highest in a vertical fracture through the foramen and lowest in a vertical fracture medial to the foramen? | 63 (81.8) | 162 (82.2) | 70 (78.7) | 35 (71.4) | 36 (62.1) | 0.014 |
| Do you think the integrity of the L5–S1 facet is adequately considered if a unilateral vertical fracture where the ipsilateral superior S1 facet is discontinuous with the medial portion of the sacrum is considered differently from a fracture where the ipsilateral superior S1 facet is in continuity with the medial portion of the sacrum? | 67 (87.0) | 164 (83.2) | 77 (86.5) | 34 (69.4) | 52 (89.7) | 0.039 |
| Do you think a nondisplaced sacral U fracture that may be seen in low-energy insufficiency fractures is a clinically relevant entity that deserves its own spot in the classification? | 66 (85.7) | 162 (82.2) | 72 (80.9) | 40 (81.6) | 53 (91.4) | 0.449 |
Note: Due to extremely low frequencies, Africa was not included in the comparison.
Chi-square test.
Next, the results were stratified by experience. Experience was accounted for in two ways: first respondents were stratified by years in practice, and additionally they were stratified by the number of traumatic sacral fractures they treated in the previous year (Table 3). No significant variability was found in the responses based on years in practice, but as surgeons treated more sacral fractures, they were less likely to agree that the risk of neurologic injury is highest in a vertical fracture through the foramen and lowest in a vertical fracture medial to the foramen (p = 0.003). However, despite this variability, more than two out of three surgeons who treat more than 10 sacral fractures a year agree that that the risk of neurologic injury is highest in a vertical fracture through the foramen and lowest in a vertical fracture medial to the foramen. Finally, the results were compared between spine surgeons (orthopedic or neurosurgeon) and orthopedic trauma surgeons. Significantly more spine surgeons than trauma surgeons agreed that the risk of neurologic injury is highest in a vertical fracture through the foramen (84.7 versus 75.4%, respectively, p = 0.033); however, still more than three in four trauma surgeons agreed that fractures through the foramen have the highest rate of neurologic injuries. No other significant difference was identified by specialty (Fig. 3).
Table 3. Experiential analysis in responses based upon years in practice or the number of traumatic sacral fractures treated in the last year.
| Yes responses, n (%) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Years of clinical practice | Number of traumatic sacral fractures the surgeon treated last year | |||||||
| Characteristics | 0–10 (n = 200) | 11–20 (n = 149) | >20 (n = 125) | p Valuea | 0–5 (n = 256) | 6–10 (n = 86) | >10 (n = 132) | p Valuea |
| Do you think that the appropriate order for sacral fracture severity from least to most severe is transverse fractures, unilateral vertical fractures, and fractures that lead to spinopelvic instability? | 178 (89.0) | 127 (85.2) | 107 (85.6) | 0.516 | 222 (86.7) | 79 (91.9) | 111 (84.1) | 0.248 |
| In an isolated vertical fracture of the sacrum, do you agree that the risk of neurologic injury is highest in a vertical fracture through the foramen and lowest in a vertical fracture medial to the foramen? | 155 (77.5) | 121 (81.2) | 93 (74.4) | 0.396 | 211 (82.4) | 69 (80.2) | 89 (67.4) | 0.003 |
| Do you think the integrity of the L5–S1 facet is adequately considered if a unilateral vertical fracture where the ipsilateral superior S1 facet is discontinuous with the medial portion of the sacrum is considered differently from a fracture where the ipsilateral superior S1 facet is in continuity with the medial portion of the sacrum? | 166 (83.0) | 128 (85.9) | 103 (82.4) | 0.684 | 214 (83.6) | 77 (89.5) | 106 (80.3) | 0.195 |
| Do you think a nondisplaced sacral U fracture that may be seen in low-energy insufficiency fractures is a clinically relevant entity that deserves its own spot in the classification? | 171 (85.5) | 126 (84.6) | 100 (80.0) | 0.404 | 216 (84.4) | 75 (87.2) | 106 (80.3) | 0.371 |
Chi-square test.
Fig. 3.
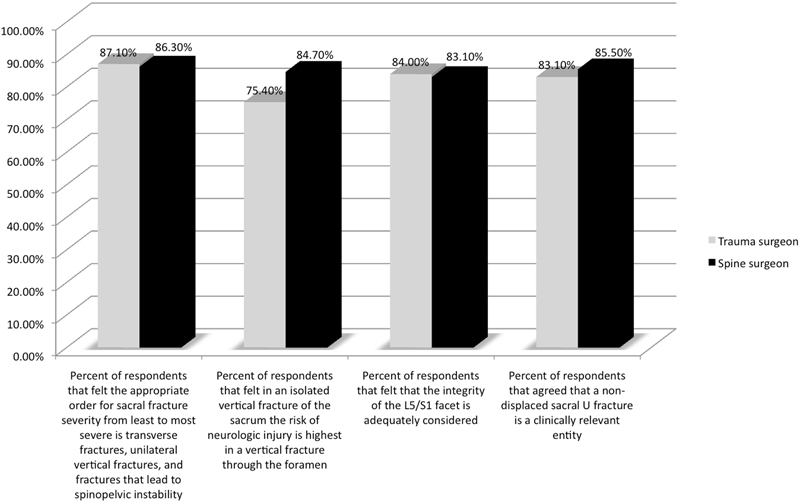
Results of the survey comparing spine surgeons and trauma surgeons. More spine surgeons than trauma surgeons agreed with the organization of B-type injuries (84.7% versus 75.4%, respectively, p = 0.03); however, still more than three in four trauma surgeons agreed with the organization of B-type injuries.
Subsequently, four multivariable logistic regression models were performed to identify demographic variables that were independent predictors of the survey responses. The full results of this analysis are presented in Table 4. Surgeons from the Middle East were more likely than European participants to disagree with the statement that the appropriate order for sacral fracture severity from least to most severe is transverse fractures, unilateral vertical fractures, and fractures that lead to spinopelvic instability (odds ratio = 0.36; 95% confidence interval [CI] 0.16 to 0.86; p = 0.020). Surgeons from either the Middle East (odds ratio = 0.42; 95% CI 0.20 to 0.91; p = 0.028) or North America (odds ratio = 0.43; 95% CI 0.21 to 0.87; p = 0.019) were less likely than those from Europe to agree that in an isolated vertical fracture of the sacrum, the risk of neurologic injury is highest in a vertical fracture through the foramen and lowest in a vertical fracture medial to the foramen, as were surgeons who treated >10 sacral fractures the last year (odds ratio = 0.51; 95% CI 0.29 to 0.90; p = 0.020). Being from the Middle East (p = 0.023) was the only variable found to affect the response to the question regarding the integrity of the L5–S1, and no variables independently affected the surgeons' response to the question pertaining to nondisplaced U-type fractures.
Table 4. Multivariable logistic regression models designed to identify variables that were independently associated with the four responses of the surveya .
| Agree with the hierarchical nature of the classification? | Agree with the risk of neurologic injury in vertical sacral fractures? | Is L5–S1 adequately considered? | Is a nondisplaced sacral U fracture a distinct entity that should be in the classification? | |||||
|---|---|---|---|---|---|---|---|---|
| Variable and category | Odds ratio (95% CI) | p Value | Odds ratio (95% CI) | p Value | Odds ratio (95% CI) | p Value | Odds ratio (95% CI) | p Value |
| AO region | ||||||||
| Europe | Baseline | – | Baseline | – | Baseline | – | Baseline | – |
| Asia Pacific | 0.75 (0.34–1.66) | 0.481 | 0.85 (0.42–1.72) | 0.646 | 1.22 (0.56–2.66) | 0.616 | 1.16 (0.55–2.46) | 0.696 |
| Latin/South America | 0.70 (0.32–1.55) | 0.383 | 0.60 (0.31–1.17) | 0.133 | 1.16 (0.55–2.46) | 0.699 | 0.75 (0.38–1.48) | 0.407 |
| Middle East | 0.36 (0.16–0.86) | 0.020b | 0.42 (0.20–0.91) | 0.028b | 0.42 (0.19–0.89) | 0.023b | 0.80 (0.34–1.87) | 0.605 |
| North America | 2.09 (0.66–6.60) | 0.210 | 0.43 (0.21–0.87) | 0.019b | 2.29 (0.86–6.09) | 0.098 | 2.78 (0.99–7.86) | 0.053 |
| Specialty | ||||||||
| Trauma surgeon | Baseline | – | Baseline | – | Baseline | – | Baseline | – |
| Spine surgeon | 0.91 (0.48–1.71) | 0.761 | 1.62 (0.91–2.89) | 0.098 | 0.94 (0.52–1.70) | 0.847 | 1.17 (0.64–2.13) | 0.605 |
| Years of clinical practice | ||||||||
| 0–10 | Baseline | – | Baseline | – | Baseline | – | Baseline | – |
| 11–20 | 0.67 (0.34–1.34) | 0.262 | 1.00 (0.56–1.78) | 0.998 | 1.19 (0.62–2.26) | 0.601 | 0.99 (0.52–1.86) | 0.970 |
| >20 | 0.66 (0.32–1.35) | 0.255 | 0.70 (0.40–1.23) | 0.213 | 0.90 (0.47–1.70) | 0.743 | 0.68 (0.37–1.28) | 0.237 |
| Number of traumatic sacral fractures treated the last year | ||||||||
| 0–5 | Baseline | – | Baseline | – | Baseline | – | Baseline | – |
| 6–10 | 1.77 (0.74–4.23) | 0.200 | 0.87 (0.46–1.66) | 0.680 | 1.63 (0.74–3.59) | 0.222 | 1.29 (0.62–2.69) | 0.494 |
| >10 | 0.62 (0.31–1.20) | 0.156 | 0.51 (0.29–0.90) | 0.020b | 0.62 (0.33–1.15) | 0.131 | 0.62 (0.33–1.14) | 0.124 |
AO region, specialty, years of clinical practice, and number of traumatic sacral fractures treated in the previous year were regarded as independent variables, and each response to the survey questions was the dependent variable.
Statistical significance.
Discussion
The results of this study demonstrate that even in the controversial aspects of sacral fractures, there is a broad global consensus on how a classification should approach these topics. Although there was some variability in response based on region, experience, and specialty, the vast majority of all groups of surgeons agreed that there is an increase in severity as fractures move from transverse to vertical to fractures that result in spinopelvic instability. Interestingly, surgeons from North America were most likely to disagree with the statement that the risk of neurologic injury is highest in a vertical fracture through the foramen and lowest in a vertical fracture medial to the foramen despite the fact that the seminal study identifying the low risk of neurologic injuries with isolated vertical fractures medial to the foramen was performed in North America.15 Additionally, although the majority of surgeons from the Middle East agreed with all of the questions asked, they had a significantly different response to all of the questions except the question pertaining to U-type sacral fractures. Finally, although surgeon specialty did appear to significantly affect the results in the univariable analysis, this variability was not significant in the multivariable regression analysis. The results of this survey suggest that the development of a comprehensive sacral injury classification system that may be acceptable to surgeons worldwide is possible.
The controversies investigated in this study are in large part a result of the inadequacy of the current classifications. Currently, the most commonly used sacral classification is the Denis classification, which divides factures of the sacrum based on their location, irrespective of their orientation. Zone 1 injuries are lateral to the foramen, and they account for ∼50% of all sacral fractures. Because an isolated zone 1 injury is completely lateral to the foramen, the rate of neurologic injury is low (∼6%). Zone 2 injuries are fractures that involve the sacral foramen but do not extend medial to the foramen; they account for approximately one third of all sacral fractures and are associated with a neurologic injury (most commonly an L5, S1, or S2 nerve root injury) in ∼28% of cases; finally, zone 3 injuries are all sacral fractures that have extension medial to the foramen (regardless of orientation), and therefore these fractures involve the spinal canal. These injuries are the most rare, but may result in a neurologic injury in more than 50% of cases.4
Although the Denis classification is commonly used, it drastically oversimplifies sacral fractures, which has made meaningful interpretation of the existing literature on sacral fractures difficult. This difficulty is most clearly seen in Denis zone 3 injuries, as these injuries may be relatively benign isolated vertical fractures or highly unstable U-type fractures. Bellabarba et al reported on 10 vertical fractures medial to the foramen without a transverse component, and none of the patients in this case series had an associated neurologic injury.15 Comparatively, Roy-Camille et al,6 with further modifications proposed by Strange-Vognsen and Lebech,7 proposed a separate classification for zone 3 U-type fractures. These injuries are highly unstable injuries that are associated with bilateral spinopelvic instability, and they have a high rate of neurologic injury. Despite the differences in presentation and appropriate treatment between the injuries described by Bellabarba et al and Roy-Camille et al, all of these injuries are still classified as zone 3 injuries in the Denis classification.4 6 7 15 The failure of the existing classifications to clearly differentiate sacral fractures has made an evidence-based algorithm for the treatment of these injuries challenging. The results of the current study suggest that there is a broad global consensus among trauma and spine surgeons on how controversial aspects of sacral fractures should be classified. Only with a comprehensive and reproducible sacral fracture classification can a cogent treatment algorithm be developed.
One of the most important findings of this study is that 77.8% of respondents agree that the risk of neurologic injury is highest in a vertical fracture through the foramen and lowest in a vertical fracture medial to the foramen. Because the Denis classification is widely used, the authors of the current study did not anticipate such an overwhelming percent of the global community would agree that the risk of neurologic injury is highest in a vertical fracture through the foramen and lowest in a vertical fracture medial to the foramen. These findings suggest that changing the order of vertical sacral fractures in a new classification will likely be met with broad acceptance.
This study has significant limitations. First it is survey of surgeons, and the responses given to a survey are not always consistent with a surgeon's actual behavior. So despite the fact that there is a global consensus on how controversial areas of sacral injuries should be handled in a new classification system, this consensus does not ensure acceptance of a new classification. Additionally, although this survey had over 600 responses, the overall response rate was still very low (4.4%). This rate probably reflects also the low frequency of these injuries. Furthermore, this study only sought input on areas of sacral fractures that the AOSpine Trauma Knowledge forum thought were controversial, and undoubtedly there may be other controversial aspects of sacral injuries. Finally, as this survey was only sent to members of AOSpine and AOTrauma, the results are representative of the worldwide AO community.
Conclusion
Because sacral injuries are complex injuries that require a multidisciplinary treatment approach, a comprehensive and universally accepted classification system is critical to ensure accurate communication between the treating physicians. This study establishes the most accepted manner in which controversial areas in the injury patterns should be addressed in a new sacral fracture classification.
Support
AOSpine supported this manuscript.
AOSpine is a clinical division of the AO Foundation—an independent medically guided not for profit organization. The AO has a strong financial independence thanks to the foundations endowment. The annual operating activities are financed through three pillars: collaboration and support agreements with DePuy Synthes and other industrial partners, return on own financial assets, and other third-party income (e.g., participant fees, R&D projects, memberships).
The AOSpine Knowledge Forums are pathology-focused working groups acting on behalf of AOSpine in their domain of scientific expertise. Each forum consists of a steering committee of up to 10 international spine experts who meet biannually to discuss research, assess the best evidence for current practices, and formulate clinical trials to advance their field of spine expertise. Authors are compensated for their travel and accommodation costs. Study support is provided directly through AOSpine's Research Department and AO's Clinical Investigation and Documentation Unit. There are no other institutional subsidies, corporate affiliations, or funding sources supporting this work unless clearly documented and disclosed.
Footnotes
Disclosures Gregory D. Schroeder: Travel expenses (Medtronic, AOSpine) Mark F. Kurd: none Christopher K. Kepler: Personal fees (AOSpine, Healthgrades, Inc.) James C. Krieg: Consultant (Conventus, Synthes, Medtronic, Merk); Stocks (Conventus, Domain Surgical, MDLive, Trice Medical); Speaker (Synthes); Royalties (SAM Medical, Synthes CMF) Jefferson R. Wilson: Personal fees (AOSpine) Conor P. Kleweno: none Reza Firoozabadi: Consultant (Smith & Nephew) Carlo Bellabarba: Board member (Cervical Spine Research Society, North American Spine Society, Orthopedics Today); Grant (AOSpine North America, Depuy, Omega) Frank Kandizoria: Personal fees (AOSpine, ESJ-OOT); Consultant (DePuy, Siemens); Speakers' bureau (DePuy, Siemens, AOSpine); Board member (Eurospine, Dwg, DGOU, AOSpine) Klause J. Schnake: Personal fees (AOSpine, Medtronic, Expanding Orthopaedics, OttoBock Healthcare, DePuy); Grant (AOSpine) S. Rajesekaran: Personal fees (AOSpine) Marcel F. Dvorak: Personal fees (AOSpine) Jens R. Chapman: Personal fees (AOSpine, Renovis Medical); Board member (Global Spine Journal, Spine, The Spine Journal, AOSpine North America, AOSpine Foundation, Cervical Spine Research Society); Royalties (Global Spine Journal) Luiz R. Vialle: Personal fees (AOSpine); Board member (AO Foundation) F. C. Oner: Personal fees (AOSpine, Medtronic, Synthes); Grant (AOSpine, DePuy) Alexander R. Vaccaro: Personal fees (AOSpine); Grant (Cerapedics); Board membership (AOSpine, Innovative Surgical Design, Association of Collaborative Spine Research, Spinicity); Consultant (DePuy, Medtronic, Stryker Spine, Globus, Stout Medical, Gerson Lehman Group, Medacorp, Innovative Surgical Design, Orthobullets, Ellipse, Vertex); Royalties (Medtronic, Stryker Spine, DePuy, Globus, Aesculap, Thieme, Jaypee, Elsevier, Taylor and Francis); Stock options (Replication Medica, Globus, Paradigm Spine, Stout Medical, Spine Medica, Computational Biodynamics, Progressive Spinal Technologies, Spinology, Small Bone Innovations, Cross Current, In Vivo, Flagship Surgical, Advanced Spinal Intellectual Properties, Cytonics, Bonovo Orthopaedics, Electrocore, Gamma Spine, Location Based Intelligence, Flow Pharma, RSI, Rothman Institute and Related Properties, Innovative Surgical Design, Spinicity)
Supplementary Material
References
- 1.Bonnin J G. Sacral fractures and injuries to the cauda equina. J Bone Joint Surg. 1945;27:113–127. [Google Scholar]
- 2.Lunsjo K, Tadros A, Hauggaard A, Blomgren R, Kopke J, Abu-Zidan F M. Associated injuries and not fracture instability predict mortality in pelvic fractures: a prospective study of 100 patients. J Trauma. 2007;62(3):687–691. doi: 10.1097/01.ta.0000203591.96003.ee. [DOI] [PubMed] [Google Scholar]
- 3.Vaccaro A R, Kim D H, Brodke D S. et al. Diagnosis and management of sacral spine fractures. Instr Course Lect. 2004;53:375–385. [PubMed] [Google Scholar]
- 4.Denis F, Davis S, Comfort T. Sacral fractures: an important problem. Retrospective analysis of 236 cases. Clin Orthop Relat Res. 1988;227(227):67–81. [PubMed] [Google Scholar]
- 5.Isler B. Lumbosacral lesions associated with pelvic ring injuries. J Orthop Trauma. 1990;4(1):1–6. doi: 10.1097/00005131-199003000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Roy-Camille R, Saillant G, Gagna G, Mazel C. Transverse fracture of the upper sacrum. Suicidal jumper's fracture. Spine (Phila Pa 1976) 1985;10(9):838–845. doi: 10.1097/00007632-198511000-00011. [DOI] [PubMed] [Google Scholar]
- 7.Strange-Vognsen H H, Lebech A. An unusual type of fracture in the upper sacrum. J Orthop Trauma. 1991;5(2):200–203. doi: 10.1097/00005131-199105020-00014. [DOI] [PubMed] [Google Scholar]
- 8.Burgess A R, Eastridge B J, Young J W. et al. Pelvic ring disruptions: effective classification system and treatment protocols. J Trauma. 1990;30(7):848–856. [PubMed] [Google Scholar]
- 9.Sabiston C P, Wing P C. Sacral fractures: classification and neurologic implications. J Trauma. 1986;26(12):1113–1115. doi: 10.1097/00005373-198612000-00010. [DOI] [PubMed] [Google Scholar]
- 10.Letournel E. [Surgical fixation of displaced pelvic fractures and dislocations of the symphysis pubis (excluding acetabular fractures) (author's transl)] Rev Chir Orthop Reparatrice Appar Mot. 1981;67(8):771–782. [PubMed] [Google Scholar]
- 11.Vaccaro A R Koerner J D Radcliff K E et al. AOSpine subaxial cervical spine injury classification system Eur Spine J 2015; February 26 (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 12.Schroeder G D, Vaccaro A R, Kepler C K. et al. Establishing the injury severity of thoracolumbar trauma: confirmation of the hierarchical structure of the AOSpine Thoracolumbar Spine Injury Classification System. Spine (Phila Pa 1976) 2015;40(8):E498–E503. doi: 10.1097/BRS.0000000000000824. [DOI] [PubMed] [Google Scholar]
- 13.Vaccaro A R Schroeder G D Kepler C K et al. The surgical algorithm for the AOSpine thoracolumbar spine injury classification system Eur Spine J 2015; June 26 (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 14.Vaccaro A R, Oner C, Kepler C K. et al. AOSpine thoracolumbar spine injury classification system: fracture description, neurological status, and key modifiers. Spine. 2013;38(23):2028–2037. doi: 10.1097/BRS.0b013e3182a8a381. [DOI] [PubMed] [Google Scholar]
- 15.Bellabarba C, Stewart J D, Ricci W M, DiPasquale T G, Bolhofner B R. Midline sagittal sacral fractures in anterior-posterior compression pelvic ring injuries. J Orthop Trauma. 2003;17(1):32–37. doi: 10.1097/00005131-200301000-00005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


