Abstract
Lately, much effort has been made to find mRNA biomarkers for tuberculosis (TB) disease/infection with microarray-based approaches. In a pilot investigation, through RNA sequencing technology, we observed a prominent modulation of DOCK9, EPHA4, and NPC2 mRNA abundance in the blood of TB patients. To corroborate these findings, independent validations were performed in cohorts from different areas. Gene expression levels in blood were evaluated by quantitative real-time PCR (Brazil, n = 129) or reanalysis of public microarray data (UK: n = 96; South Africa: n = 51; Germany: n = 26; and UK/France: n = 63). In the Brazilian cohort, significant modulation of all target-genes was observed comparing TB vs. healthy recent close TB contacts (rCt). With a 92% specificity, NPC2 mRNA high expression (NPC2high) showed the highest sensitivity (85%, 95% CI 65%–96%; area under the ROC curve [AUROC] = 0.88), followed by EPHA4 (53%, 95% CI 33%–73%, AUROC = 0.73) and DOCK9 (19%, 95% CI 7%–40%; AUROC = 0.66). All the other reanalyzed cohorts corroborated the potential of NPC2high as a biomarker for TB (sensitivity: 82–100%; specificity: 94–97%). An NPC2high profile was also observed in 60% (29/48) of the tuberculin skin test positive rCt, and additional follow-up evaluation revealed changes in the expression levels of NPC2 during the different stages of Mycobacterium tuberculosis infection, suggesting that further studies are needed to evaluate modulation of this gene during latent TB and/or progression to active disease. Considering its high specificity, our data indicate, for the first time, that NPC2high might serve as an accurate single-gene biomarker for TB.
Keywords: M. tuberculosis, LTBI, tuberculosis, messenger RNA, biomarkers
Introduction
Mycobacterium tuberculosis bacilli spread through the air, and the lung parenchyma is the main site of infection. Despite the availability of effective treatment, new tuberculosis (TB) cases are commonly mis- or under-diagnosed, leading to delayed initiation of chemotherapy and, consequently, to high morbidity and mortality (Golub et al., 2005; Belay et al., 2012). The diagnosis of pulmonary TB relies on the combination of clinical and epidemiological features associated with chest radiographic changes and microbiological findings (detection of acid-fast bacilli, culture growth or nucleic acid detection; Sia and Wieland, 2011). Nevertheless, the sputum smear lacks in sensitivity (50–70%), and the more sensitive culture (80–89% sensitivity), the gold-standard method, is time consuming as 4–8 weeks is required for visible colonies to appear (Reichman and Hersfield, 1993; Sia and Wieland, 2011). The availability of commercial automated rapid molecular tests (Xpert® MTB/RIF) has overcome this problem, providing results within 2 h and showing moderate to high accuracy (61.1–100% sensitivity; 90.9–100% specificity; Rachow et al., 2011). However, the use of any of these tests to investigate suspected cases of pulmonary TB is more complicated if sputum is of low quality or quantity, routinely requiring a bronchoscopy with bronchoalveolar lavage (Khalil and Butt, 2015). Thus, the global search for fast, more accurate and non-invasive diagnostic biomarkers for TB continues.
As the transcription of genes is a very dynamic process, modulation of their expression is the first major regulatory change in many biological processes (Riedmaier and Pfaffl, 2013). Correspondingly, prominent gene expression regulation has been found in blood cells of patients with pulmonary TB or LTBI (Berry et al., 2010; Lu et al., 2011; Maertzdorf et al., 2011, 2012; Bloom et al., 2013; Anderson et al., 2014; Esterhuyse et al., 2015; Laux da Costa et al., 2015; Zak et al., 2016). The potential applications of biomarkers for TB include not only the improvement of the current diagnostic tests, but also the possibility of assessing the response to drug therapy and targeted screening of eligible subjects for new TB vaccines and therapeutic trials. However, most previous exploratory attempts are based on array techniques for mRNA expression, which may have contributed to a high redundancy among studies, usually revealing mRNAs whose products correlate with the human immune response to TB: type-I and type-II interferon signaling, Toll-like receptors, T- and B-cell functions, and neutrophil influx (Blankley et al., 2014; Deffur et al., 2015). Moreover, even though some of the presented biomarkers/biosignatures showed high accuracy for TB detection, the lack of validations in cohorts from different geographical areas and/or the proposed use of combinations of a number of genes (from sets of 3 to 100s), hinder their use in clinical routine.
The advent of RNA sequencing (RNAseq) technology allowed the simultaneous measurement and profiling of the transcriptome of a biosample, avoiding biases introduced during microarray hybridization (Zhao et al., 2014). The aim of the present study therefore was to identify new mRNA biomarkers for TB in whole blood specimens. For this purpose, in an exploratory investigation, a small set of recent close TB contacts (rCt) exposed to a bacillary index case, and TB patients, were submitted to whole blood transcriptomic profiling via RNAseq (unpublished data); the raw transcriptome data can be found at the NCBI Gene Expression Omnibus (GEO) under the accession code GSE84076. Mining these data, highly prominent regulation of DOCK9, EPHA4, and NPC2 mRNA expression was observed in the TB samples. Following a first validation by quantitative real-time PCR (RT-qPCR) in a cohort of rCt and TB cases from Rio de Janeiro/Brazil, expression data from previous microarray studies (Berry et al., 2010; Maertzdorf et al., 2012; Bloom et al., 2013) were also used for an independent validation of these potential mRNA biomarkers in populations with different levels of TB incidence and diverse genetic backgrounds.
Materials and Methods
Ethics Statements
The study protocol was approved under the registration codes 560-10, 183-10, and 190/12, by the Ethics Committee of the Oswaldo Cruz Foundation, Clementino Fraga Filho University Hospital (CFFUH) and Polyclinic Augusto do Amaral Peixoto (PAAP), respectively. Participation in this study was voluntary and only subjects ≥18 years of age who gave informed written consent were eligible.
Participants
All participants were recruited from March 2010 to November 2013 at CFFUH and PAAP, both located in Rio de Janeiro state, Brazil, a TB endemic area with an incidence rate of 60.9/100,000 inhabitants (Equipe Gerência de Pneumologia Sanitária SES/RJ, 2014). Demographic characteristics were gathered via a structured questionnaire.
According to the Brazilian Ministry of Health policy recommendations for TB/LTBI screening, all rCt recruited underwent a clinical exam, the Mendel-Mantoux tuberculin skin test (TST), and chest X-ray examination at enrollment (T0). Besides clinical and epidemiological data, the diagnostic criteria for TB among rCt or index cases were at least one acid-fast bacilli-positive sputum sample for M. tuberculosis and/or positive sputum culture.
After TB was excluded, TST results were read after 72 h, and any rCt showing an induration ≥5 mm were considered as LTBI. The rCt TST negative individuals (TSTneg) were followed up and retested after 12 months (T12). For those rCt showing a positive TST (TSTpos) or conversion (increase in induration of the TST reaction of at least 10 mm) at any time-point, a free-of-cost prophylactic treatment for LTBI (tLTBI) was offered, as well as the appropriate treatment for individuals who developed TB (TB progressors).
For the pilot RNAseq investigation a group of rCt from the Brazilian cohort was stratified according to the response to both TST and in house interferon-gamma release assays (IGRAs) under ESAT6:CFP10 stimulation (Araujo et al., 2014). Control and LTBI groups comprised 12 and 16 participants with TSTneg/IGRAneg or TSTpos/IGRApos, respectively. Six confirmed TB cases were also included.
The validation by RT-qPCR was performed using a larger cohort of rCt where IGRA results were not available. As the participants presented different baseline and follow-up responses to TST, they were allocated into groups according to the probability of having LTBI: (i) G.I (n = 12), very low: no TST reaction (0 mm) at baseline and at any of the follow up retests; (ii) G.II (n = 24), low to moderate: baseline TSTneg (0–4 mm) who did not return for skin test re-evaluation (16/24, 67%) or converted to TSTpos (8/24, 33%); and (iii) G.III (n = 48), high: baseline TSTpos (TST > 5 mm). The majority of TB samples (26/45, 58%) were from treatment-naive participants, and together with those treated ≤2 days comprise the group G.IV (n = 29). G.V (n = 12) comprises samples from TB cases with 3–6 days of anti-TB treatment, and G.VI consists of samples from TB cases with 7 days (n = 2) or 6 months (n = 2) of anti-TB treatment. Characteristics of all study participants are summarized in Table 1.
Table 1.
Clinical and demographic characteristics of the study population.
| Groups | n | Age1 (SD) | Males (%) | TST (T0)2 | TST (T4 or T12)2 | Abnormal Chest X-ray | Symptoms of TB | Sputum-smear/(and/or) culture positive cases |
|---|---|---|---|---|---|---|---|---|
| Probability of LTBI | ||||||||
| G.I Very low | 12 | 38.3 (16.2) | 1 (8.3) | 0 | 0 | 0 | 0 | 0/0 |
| G.II Low/moderate | 24 | 40.1 (15.5) | 6 (25) | 0–4 | ND or ≥5 mm | 0 | 2 | 0/0 |
| G.III High | 48 | 41.9 (14.9) | 14 (29) | ≥5 | – | 6 | 12 | 0/0 |
| TB (days after treatment onset) | ||||||||
| G.IV 0–2 | 29 | 39.4 (14.9) | 14 (48) | – | – | 29 | 29 | 18/18 |
| G.V 3–6 | 12 | 43.6 (13.1) | 8 (67) | – | – | 12 | 12 | 10/6 |
| G.VI ≥ 7 | 4 | 47.5 (20.1) | 3 (75) | – | – | 2 | 4 | 4/03 |
| Total | 129 | 41.1 (14.9) | 46 (36) | – | – | 49 | 59 | – |
The recent close tuberculosis (TB) contacts (rCt) and pulmonary TB patients were stratified according to the probability of latent TB infection (LTBI), via tuberculin skin test (TST) response at enrollment (T0) and follow up (T4 or T12), or the time (days) relapsed between the anti-tuberculosis treatment onset and the blood collection for this study, respectively.
1Mean age and standard deviation (SD), in years. 2TST in millimeters; Follow up TST in the 4th or 12th consecutive month. 3At the time of diagnostic. ND, not done.
Specimen Collection and RNA Isolation
Peripheral whole blood was collected in Paxgene RNA tubes (PreAnalytiX, SWZ) and stored at -70°C until processing. Total RNA was isolated using the PAXgene Blood miRNA Kit (PreAnalytiX, SWZ), which is indicated for the isolation and purification of total RNA longer than 18 nucleotides. The manufacturer’s instructions were followed at both stages. Total RNA was quantified with a Nanodrop ND-1000 spectrophotometer (Thermo Scientific, EUA) and RNA integrity was assessed via agarose gel electrophoresis.
cDNA Synthesis and RT-qPCR
DOCK9. EPHA4, and NPC2 mRNAs were selected for further validations. Total RNA (100 ng) was reverse transcribed into complementary DNA (cDNA) using the oligo (dT) primer and Superscript III kits (Invitrogen, Life Technologies, USA), according to the manufacturer’s protocol. RT-qPCR was performed as previously reported (Guerreiro et al., 2013), with minor modifications in the master mix preparation: 0.4 μL (250 nM) of gene-specific primers (Supplementary Table S1); 10 μL of Fast SYBR green (Applied Biosystems, Molecular Probes, Inc.); 2 μL of cDNA; and 7.6 μL of sterile DNase-, RNase-, and DNA-free water. All RT-qPCR tests were performed in duplicate, assayed and analyzed in a blind manner.
RT-qPCR Relative Expression Analysis
Individual expression of DOCK9. EPHA4, and NPC2 mRNAs was obtained as crossing point (Cp) values (Guerreiro et al., 2013), which were subsequently normalized to RPL13A mRNA expression, using the qPCR library (Ritz and Spiess, 2008) for the R statistical package 3.2.3 (R Development Core Team, 2014), resulting in relative expression data for the three target genes.
Microarray Reanalysis
Whole blood normalized microarray expression data from HD, LTBI and pulmonary TB adults (≥18 years of age) available at the GEO under accession number GSE19491 (Berry et al., 2010), GSE34608 (Maertzdorf et al., 2012), and GSE42826 (Bloom et al., 2013) were exported to Prism 6 (GraphPad Software) using the GEO2R (Barrett et al., 2013) web tool. Follow up data during anti-TB treatment were also available in Berry et al. (2010).
Statistical Analysis
Differences among biological groups were assessed with the Mann–Whitney (two groups) or Kruskal–Wallis (more than two groups) tests followed by Dunn’s multiple comparison tests correction, when applicable. The Friedman test was applied to analyze follow up data. p-values ≤ 0.05 and q-values < 0.01 were considered as significant. Mean, median, standard deviation (SD), dispersion plots, AUROC (area under the receiver operating characteristics curve) values and 95% confidence intervals (CI) were computed using Prism 6 (GraphPad Software); while the R statistical package 3.2.3 (R Development Core Team, 2014) was used for the ROC (receiver operating characteristics) curves (Robin et al., 2011), classification tree analysis (Therneau et al., 2015), and Venn diagrams (Chen and Boutros, 2011). Cut-off points were selected by fixing specificities ≥90%, after which relative expression of each gene was classified as low (below the cut-off) or high (above the cut-off).
Results
Target-Genes Screening via RNAseq
The proposed groups for this pilot investigation did not differ significantly in age (mean age [SD], in years: control: 42.1 [14.4]; LTBI: 45.5 [12.7]; and TB: 44.9 [13.2], p = 0.202). A predominance of women among control (10/12, 83%) and LTBI (10/16, 63%) groups compared to the active TB cases (2/6, 33%) was observed.
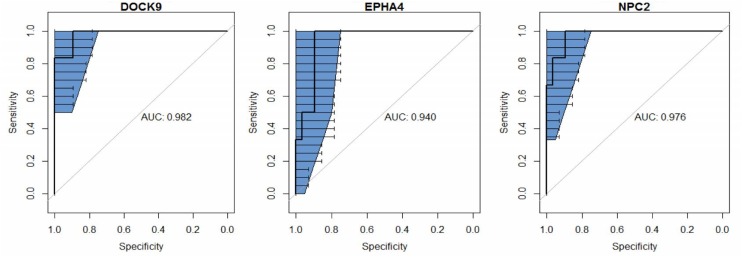
The group with active pulmonary TB was used as reference of infection for biomarker screening. Compared to control and LTBI groups, 120 and and 52 genes, respectively, were differentially expressed in the TB cases. From these sets of genes, 13 mRNAs (ANKRD22. APOL4. BANK1. BATF2. DHRS9. DOCK9. EPHA4. ETV7. FAM26. FMN1. NPC2. NT5E, and WARS) were found in both comparisons (TB vs. LTBI or controls). Then, as the highest AUROC (≥0.94) were observed for DOCK9. EPHA4, and NPC2 (Figure 1), these three genes were selected for further validations.
FIGURE 1.
Receiver operating characteristic (ROC) curve analysis and the respective areas under the curve (AUC) with 95% confidence intervals (blue), comparing peripheral blood DOCK9. EPHA4, and NPC2 gene expression profiles, obtained via RNA sequencing, between recent close tuberculosis (TB) contacts (rCt, n = 28) and patients with pulmonary TB (n = 6) for the screening of target genes for Mycobacterium tuberculosis infection.
Gene Expression Profiling via RT-qPCR: The Brazilian Cohort
The assay was performed in 129 participants comprising 45 TB patients and 84 rCt. The majority of the TB cases were confirmed by a positive sputum smear and/or culture (G.IV = 27/29 [93%]; G.V = 10/12 [83%]; G.VI = 3/4 [75%]). Clinical examination and free-of-cost treatment for LTBI/TB was offered at baseline and during follow up, but 35% (29/84) of the rCt did not return for re-evaluation. The mean age [SD] of the recruited rCt (41 [15.1] years) and TB (41 [14.9] years) participants was not significantly different (p = 0.787). Most of the TB patients were males (rCt: 21/84, 25%; TB: 25/45, 56%) with abnormal findings on chest x-ray (rCt: 6/84, 7%; TB: 45/45, 100%) and clinical symptoms of TB (rCt: 14/84, 17%; TB: 43/45, 96%; Table 1).
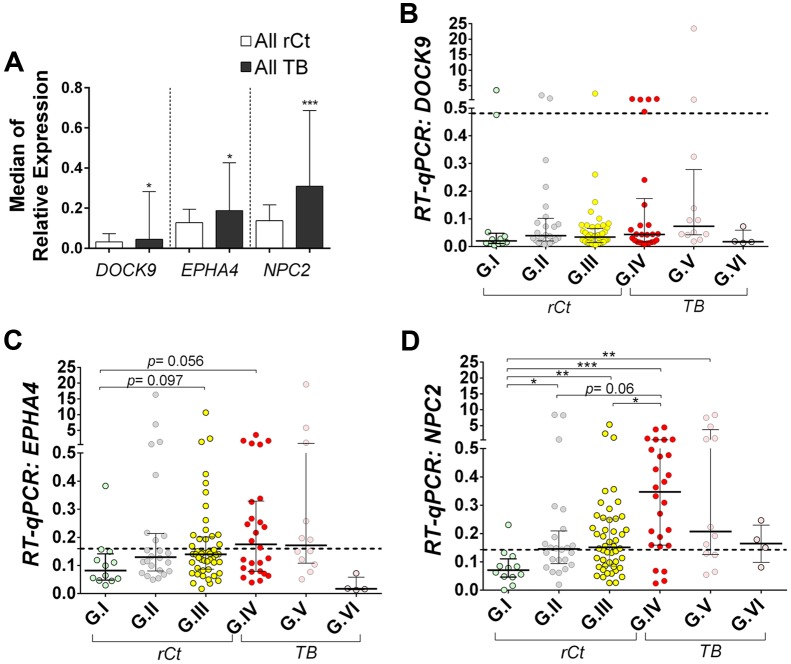
Gene expression profiling of EPHA4 and NPC2 showed a tendency of gradual median increment from G.I to G.IV, decreasing toward G.V and G.VI (Supplementary Table S2). Hence, in multiple group comparisons, only EPHA4 and NPC2 offered significant, or borderline, differences between controls (G.I) and latently (G.III) or actively infected groups (G.IV) (Figures 2B–D). Interestingly, a bimodal expression profile was observed for DOCK9 and EPHA4 especially in group G.IV (Figures 1 and 2B).
FIGURE 2.
Relative expression of DOCK9, EPHA4, and NPC2 mRNAs in whole blood, as obtained with quantitative real-time PCR (RT-qPCR). RPL13A mRNA was used as reference (housekeeping) gene. All participants were recruited from the broad population of routine clinical practice at public hospitals in Rio de Janeiro/Brazil. Data are shown as median ± interquartile range. (A) Comparison between all healthy recent close TB contacts (rCt) and patients with pulmonary tuberculosis (TB). Mann–Whitney U-test; ∗p < 0.05 and ∗∗∗p < 0.001. (B–D) Comparison between healthy recent close TB contacts (rCt) stratified in three groups according to probability of latent tuberculosis infection: (G.I, n = 12) very low, (G.II, n = 24) low to moderate, and (G.III, n = 48) moderate to high; and tuberculosis (TB) cases grouped by the time elapsed between the anti-TB treatment onset and the blood collection for this study (G.IV: 0–2 days, n = 29; G.V: 3–6 days, n = 12; and G.VI: ≥7 days, n = 4). (B) DOCK9, (C) EPHA4, and (D) NPC2 gene expression. The Kruskal–Wallis test was used to access significance of global differences across groups (DOCK9 p = 0.039, EPHA4 p = 0.059 and NPC2 p < 0.0001), among rCt (DOCK9 p = 0.276, EPHA4 p = 0.079 and NPC2 p = 0.005) or TB (DOCK9: p = 0.18; EPHA4: p = 0.38; and NPC2: p = 0.28), followed by Dunn’s Multiple Comparison test (∗p < 0.05, ∗∗p ≤0.005, and ∗∗∗p ≤ 0.001).
NPC2 presented the most significant differential expression, as mRNA levels in controls (G.I) were significantly lower than in the other groups (p < 0.05), except for TB with >7 days of specific treatment (G.VI, p > 0.999). Moreover, up-regulation of NPC2, with consistent changes in median expression, was observed in active disease (G.IV, p ≤ 0.001) compared to rCt with high (G.III, p < 0.05) or low-to-moderate (G.II, p = 0.06) probability of infection (Figure 2D).
RT-qPCR: ROC Curve Analysis
Receiver operating characteristic curve analysis demonstrated that relative expression of NPC2 mRNA had the highest discriminatory power for detection of LTBI (G.III, AUROC = 0.79, 95% CI = 0.65–0.92), TB (G.IV, AUROC = 0.88, 95% CI = 0.77–0.99), or both active and latent infections (G.III + G.IV, AUROC = 0.82, 95% CI = 0.72–0.93), followed by EPHA4 (LTBI, G.III: AUROC = 0.70, 95% CI = 0.53–0.87; TB, G.IV: AUROC = 0.73, 95% CI = 0.56–0.90; and both G.III + G.IV: AUROC = 0.720, 95% CI = 0.56–0.88) and last by DOCK9 (LTBI, G.III: AUROC = 0.59, 95% CI = 0.40–0.79; TB, G.IV: AUROC = 0.66, 95% CI = 0.46–0.86; and both G.III + G.IV: AUROC = 0.63, 95% CI = 0.43–0.82) (Supplementary Figure S1).
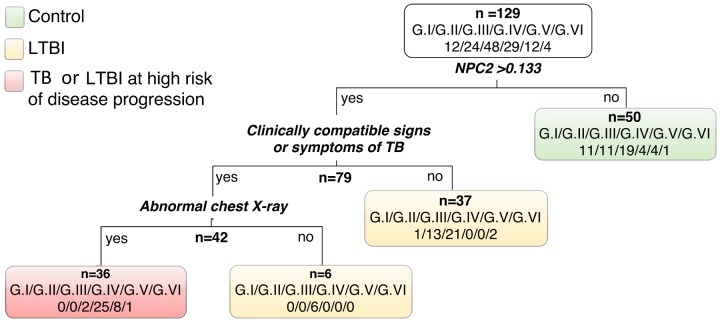
Remarkably, in single gene analysis NPC2 mRNA expression levels showed the highest discrimination, detecting 86% (25/29) of the TB (G.IV) patients and only one control (1/12), corresponding to 92% specificity (Table 2). Therefore, using NPC2high expression for screening, in conjunction with the available clinical/radiological findings, allowed to differentiate latent and active forms of infections: G.I = 0/12 (0%), G.II = 0/24 (0%), G.III = 2/48 (4%), G.IV = 25/29 (86%), G.V = 8/12 (67%), G.VI = 1/4 (25%) (Figure 3). The use of combinations of the three mRNAs and/or other available epidemiological data did not improve classifying capability any further.
Table 2.
Receiver operating characteristic (ROC) analysis of normalized expression values, via quantitative real-time PCR, to classify recent close TB contacts from G.I (low probability of latent tuberculosis infection) and patients with tuberculosis (G.IV) in the Brazilian cohort.
| Gene | AUC | Sensitivity (%) | Specificity (%) | Cut-off point¥ |
|---|---|---|---|---|
| [95% CI] | ||||
| DOCK9 | 0.66 [0.46–0.86] | 19 [7–39] | 91.7 [62–100] | >0.481 |
| EPHA4 | 0.73 [0.56–0.90] | 53.4 [33–73] | 91.7 [62–100] | >0.160 |
| NPC2 | 0.88 [0.77–0.99] | 84.6 [65–96] | 91.7 [62–100] | >0.133 |
¥normalized expression values.
FIGURE 3.
Classification tree using relative expression of NPC2 mRNA by RT-qPCR (cut-off 0.133) in conjunction with clinical and radiological information. Latent TB infection probability groups: G.I very low, G.II low to moderate, and G.III moderate to high; and patients with active pulmonary tuberculosis (TB) grouped by the time (days) elapsed between the anti-TB treatment onset and the blood collection for this study (G.IV: 0–2 days; G.V: 3–6 days; and G.VI: ≥7 days).
RT-qPCR: Follow up Analysis
Among all rCt showing an NPC2high expression profile (NPC2high/total: G.I = 1/12 [8.3%], G.II = 13/24 [54.2%], and G.III = 29/48 [60.4%]; total = 43/84 [51%]), the majority accepted the prophylactic treatment for LTBI (tLTBI/NPC2high: G.I = 0/1 [0%]; G.II = 4/13 [31%]; G.III = 25/29 [86%]; total = 29/43 [67%]). Of note, among all untreated rCt (n = 41), a single subject in G.III progressed to active TB during follow up (Supplementary Table S3). The mRNA expression profile of this participant was high only for NPC2 at T0 (DOCK9: 0.070, EPHA4: 0.121 and NPC2: 0.248), which was even higher upon diagnosis of TB (DOCK9: 0.076, EPHA4: 0.247 and NPC2: 0.309) and decreased after the anti-TB treatment (DOCK9: 0.019, EPHA4: 0.065 and NPC2: 0.152) (Supplementary Figure S2). None of the NPC2low participants progressed to active TB during the period of this study.
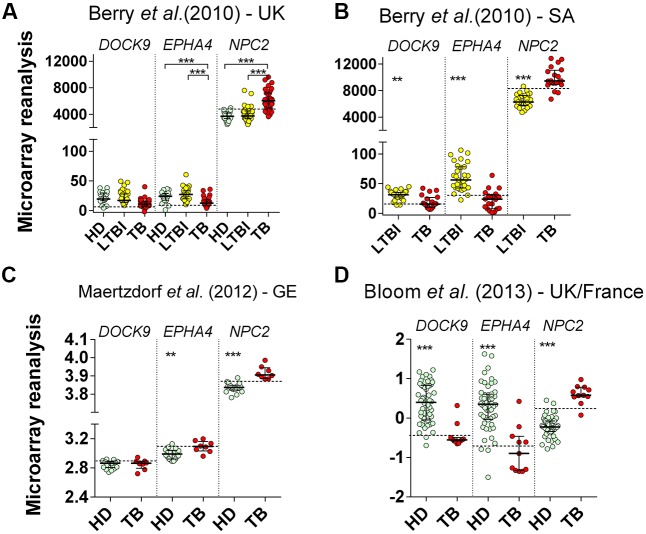
Microarray Reanalysis: Cross-Sectional Studies
All reanalyzed cohorts showed significant (p < 0.001) differential expression of EPHA4 and NPC2 mRNAs in whole blood of TB patients (Figures 4A–D). Specificities were high (≥94%) for all selected genes. In ROC curve analysis, again, the highest AUROC values (≥0.95) were observed for NPC2 mRNA, corresponding to sensitivities between 82% (95% CI 66%–93%) and 100% (95% CI 63%–100%), followed by EPHA4, AUROC from 0.79% (95% CI 0.66%–0.91%) to 0.92% (95% CI 0.85%–1.0%), with poor-to-moderate sensitivities: 23.5% (95% CI 11%–41%) to 75% (95% CI 51%–91%) (Table 3). On the other hand, DOCK9 mRNA, AUROC from 0.53% (95% CI 0.28%–0.82%) to 0.93% (95% CI 0.84%–1.0%), usually showed low sensitivities, from 13% (95% CI 3%–57%) to 35% (95% CI 15%–59%), except for the Bloom et al. (Bloom et al., 2013) study (82%, 95% CI 48%–98%) (Table 3).
FIGURE 4.
Reanalysis of DOCK9, EPHA4, and NPC2 expression in whole blood from healthy donors (HD), latently infected subjects (LTBI) and patients with pulmonary tuberculosis (TB) based on the data published by Berry et al. (2010), Maertzdorf et al. (2012), and Bloom et al. (2013). The previous microarrays studies were performed in cohorts from: (A) UK (HD = 24, LTBI = 38, TB = 24), (B) South Africa (LTBI = 31, TB = 20), (C) Germany (HD = 18, TB = 8), and (D) UK/France (HD = 52, TB = 11), respectively. Mann–Whitney U or Kruskal–Wallis tests were performed for two or >2 groups comparisons, respectively (∗∗p ≤ 0.005 and ∗∗∗p < 0.001). Small lines, dotted lines and bars represent the median, cut-off and ±interquartile range, respectively.
Table 3.
Receiver operating characteristic curve reanalysis of deposited microarray expression data for DOCK9. EPHA4, and NPC2, to classify healthy donors (HD) and tuberculosis (TB) cases in cohorts from the UK, South Africa, Germany, and France.
| Study site (reference) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| UK† (2) | South Africa¥ (2) | Germany (5) | UK/France (6) | ||||||
| Gene | n | Value [95% CI] | n | Value [95% CI] | n | Value [95% CI] | n | Value [95% CI] | |
| DOCK9 | AUC (HD vs. TB) | 0.79 [0.66–0.92] | 0.80 [0.66–0.95] | 0.53 [0.28–0.82] | 0.93 [0.84–1.0] | ||||
| Specificity (%) | 24 | 96 [79–100] | 31 | 97 [83–100] | 18 | 94 [73–100] | 52 | 96. [87–100] | |
| Sensitivity (%) | 34 | 15 [5–31] | 20 | 35 [15–59] | 8 | 13 [0.3–53] | 11 | 82 [48–98] | |
| EPHA4 | AUC (HD vs. TB) | 0.79 [0.66–0.91] | 0.92 [0.85–1.0] | 0.85 [0.69–1.0] | 0.90 [0.79–1.0] | ||||
| Specificity (%) | 24 | 96 [79–100] | 31 | 97 [83–100] | 18 | 94 [73–100] | 52 | 962 [87–100] | |
| Sensitivity (%) | 34 | 24 [11–41] | 20 | 75 [51–91] | 8 | 63 [25–92] | 11 | 55[23–83] | |
| NPC2 | AUC (HD vs. TB) | 0.95 [0.91–1.0] | 0.97 [0.93–1.0] | 0.99 [0.95–1.0] | 0.99 [0.97–1.0] | ||||
| Specificity (%) | 24 | 96 [79–100] | 31 | 97 [83–100] | 18 | 94 [73–100] | 52 | 96 [87–100] | |
| Sensitivity (%) | 34 | 82 [66–93] | 20 | 85 [66–97] | 8 | 100 [63–100] | 11 | 91 [58–100] | |
†Study population composed of immigrants from endemic countries or household contacts.
¥HD samples were not available; therefore, ROC analysis was performed comparing latently infected subjects and TB patients.
Microarray Reanalysis: TB Treatment follow up
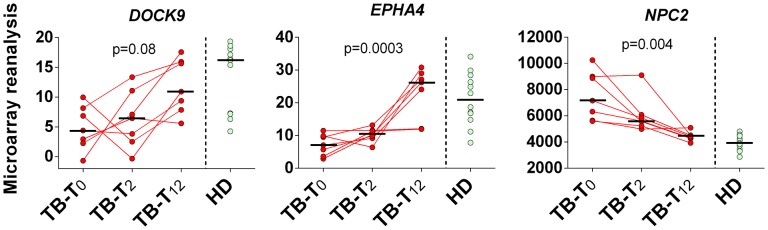
Reanalyzing microarray blood expression data from TB patients (n = 7) at enrollment (T0), and at T2 and T12 (elapsed time in months) after initiation of antimycobacterial treatment, we noticed a gradual trend of up-regulation of DOCK9 (p = 0.08) and EPHA4 mRNA (p = 0.0003), and down-regulation of NPC2 (p = 0.004), during follow up (Figure 5). Even though DOCK9 and EPHA4 showed bimodal gene expression profiles among HD (n = 12) and TB-T12 groups, no statistical differences were observed between these groups for all target genes (Mann–Whitney U-test, p ≥ 0.415) and, notably, the NPC2high biomarker was the only one that normalized completely 12 months after the onset of anti-TB treatment.
FIGURE 5.
Twelve months follow up of DOCK9, EPHA4, and NPC2 expression after initiation of anti-TB treatment. Pulmonary tuberculosis (TB, n = 7) was confirmed by isolation of M. tuberculosis upon culture of sputum or bronchoalvelolar lavage fluid. Samples from healthy donors (HD, n = 12) without known exposure to TB who were negative by both tuberculin skin test and interferon-gamma release assay were also included in the analysis. Whole blood samples from TB patients were collected prior to the initiation of the anti-mycobacterial therapy (TB-T0), in the second (TB-T2) and twelfth (TB-T12) consecutive months. Short bars represent medians. Reanalyzed data from Berry et al. (2010).
Discussion
Previous whole blood genomic-scale studies pointed to a 144 (Bloom et al., 2013) or 393 (Berry et al., 2010) gene-transcript signature (including DOCK9 and EPHA4) for TB, showing 61.7–94.1% sensitivities and 93.8–97% specificities (Berry et al., 2010; Bloom et al., 2013). Nevertheless, the use of 100s of genes for transcriptional profiling in clinical practice is currently impractical. Lu et al. (2011) proposed a smaller combination of genes, CXCL10. ATP10A and TLR6, which showed 71% sensitivity and 89% specificity to discriminate between latent and active TB. Lee et al. (2016) with a similar objective showed excellent AUROC ( = 1.0) for the comparisons between LTBI (n = 7) or active TB (n = 7) vs. HD (n = 7) using peripheral blood ASUN or PTPRC mRNA levels. Even though this accuracy was independently validated (AUROC ≥ 0.94), the assayed cohort had a small sample size (15 TB, 17 LTBI, and 15 HD; Lee et al., 2016). In a separate study, gene expression differentiation between TB and other pulmonary diseases was also described, which was based on another set of three genes (GBP5. GZMA, and CD64) and had a 93% sensitivity and 95% specificity; Laux da Costa et al., 2015). More recently, Zak et al. (2016), in a prospective African contact tracing study that featured a study design similar to ours (RNAseq for target-gene screening and RT-qPCR for biomarker validation), proposed a 16 gene-based transcriptional biosignature for risk of disease progression with 80.6% specificity, but with low sensitivity (66.1%) in the 12 months preceding TB diagnosis.
In the present study, we describe, for the first time, an up-regulation of NPC2 mRNA levels in the blood of tuberculous subjects, as well as the transcription profiles of DOCK9. EPHA4 and NPC2 among Brazilians recently exposed to a TB index case. As 25% (1/4) of the untreated subjects from G.III progressed to active TB during the 1-year follow up period (Supplementary Table S3), the prophylactic treatment might have compromised the evaluation of the proposed biomarker in the early detection of TB. Another limitation of this study is the lack of an unexposed control group among the Brazilian donors. However, in high TB-burden scenarios, as Rio de Janeiro/Brazil, it is difficult to rule out a previous exposure to M. tuberculosis, even in subjects with no reported contact with a TB index case. To overcome this, we opted to group the enrolled participants according to baseline and follow up response to TST, a highly sensitive LTBI test (Schluger and Burzynski, 2010), and evaluated HD expression profiles in other cohorts. Notably, a one-gene biosignature, NPC2high, showed high sensitivity (85%) and specificity (92%), via RT-qPCR, for TB detection. In addition, a reanalysis of expression data from public repositories showed a similar sensitivity (82–100%) and specificity (94–97%) in populations with different genetic backgrounds (Berry et al., 2010; Maertzdorf et al., 2012; Bloom et al., 2013).
Here, the monitoring of NPC2 mRNA levels in blood could be used as a screening tool for the detection of active TB. On the other hand, by RT-qPCR or microarray reanalysis, DOCK9 (13–82%) and EPHA4 (24–75%) usually showed poor-to-moderate sensitivities but, interestingly, they exhibited a dichotomous median expression profile among the different TB groups in comparison to the respective control: down-modulation in populations from the UK and South Africa (Figure 4), but the contrary among Brazilians (Figures 2B,C) and Germans (Figure 4C). A bimodal DOCK9 and EPHA4 mRNA expression profile was also observed, principally in the TB groups from Brazil (G.IV and G.V, Figures 2B,C), UK cross-sectional (Figure 4D) and the follow up cohorts (Figure 4). This bimodal transcription, in response to physiological disturbances, was previously described for other genes (Bessarabova et al., 2010). Furthermore, according to Bessarabova et al. (2010) the presence of a bimodal gene expression profile could correspond to different disease subtypes. Thus, further studies are needed to assess whether different M. tuberculosis strains, infection sites, previous infections, host genetic background or co-morbidities can affect DOCK9 and EPHA4 mRNA expression profiles. Interestingly, this bimodal behavior was not observed for NPC2.
Anti-TB chemotherapy usually requires a 6-months standard regimen to eradicate the infection (Jindani et al., 2004). The observed change trend in the median expression levels for all target genes toward an uninfected control-like transcriptional profile, in the beginning of treatment (G.VI, Figure 2), and more pronounced in the TB-T12 group (Figure 3), is an indication that these modulations are dependent on the presence of viable bacilli in the host system.
The exact physiological role of the dedicator of cytokinesis 9 (Dock9) protein has not been totally defined yet. According to Gadea and Blangy (2014), it is possible that Dock9 plays a role in the activation of Cdc42, a Rho GTPase that can affect TGF-beta1-mediated transcriptional responses. Dock9 has also been implicated in the epithelial to mesenchymal cell transition through the reorganization of the actin cytoskeleton and the regulation of cell polarity (Brown et al., 2008; Gadea and Blangy, 2014). Previous studies have pointed to the role of Epha4 and its receptor, Ephrin A1, in the process of lymphocyte and monocyte adhesion (Poitz et al., 2015). The Eph/Ephrin-system, among others, was described to influence Rho GTPases, such as Cdc42 (Singh et al., 2012). Taken together, these observations suggest that these proteins have a common pathway in the recruitment of immune cells to M. tuberculosis infection sites.
NPC2 plays roles in cholesterol and glycolipid trafficking and/or transport, and mutations in it are causally related to Niemann-Pick disease, a life-threatening lysosomal storage disease (Park et al., 2003), but studies on its role in M. tuberculosis pathogenesis are scarce. Recently, knockdown experiments demonstrated that adding all-trans retinoic acid (ATRA), the biologically active form of vitamin A, to M. tuberculosis-infected human monocyte cultures resulted in an NPC2-dependent decrease in total cellular cholesterol, associated with a consequent increase in antimicrobial activity through lysosomal acidification (Wheelwright et al., 2014). The authors postulated that decreasing levels of NPC2 expression might favor M. tuberculosis persistence. In contrast, we observed an up-regulation of NPC2 mRNA in whole blood from patients with active TB and LTBI subjects, indicating that increased NPC2 expression is part of the host response to TB infection but does not confer protection in all cases. As we could observe in the incident case (Supplementary Figure S2), and in the subcohort of NPC2high TB patients in whom disease progression could not be prevented, expression of this gene was still high. Our data indirectly demonstrate that upon the persistence of M. tuberculosis, systemic modulation of gene expression may occur even in asymptomatic, but latently infected subjects. Nonetheless, it is still necessary to investigate which genotypic or phenotypic features could be responsible for the NPC2low expression profile in a few TB patients. Moreover, it is also necessary to clarify whether NPC2 up-regulation is specific for TB infection among patients with respiratory symptoms. In two of the reanalyzed studies (Maertzdorf et al., 2012; Bloom et al., 2013) samples from other pulmonary diseases were also included (data not shown). The NPC2high blood expression profile was detected in only 1/6 (17%) pneumonia patients and 1/8 (13%) lung cancer patients (Bloom et al., 2013) but, in 50% (n = 9/18) (Maertzdorf et al., 2012) and 56% (n = 9/16) (Bloom et al., 2013) of patients with active sarcoidosis. As sarcoidosis is a low incidence disease (Nunes et al., 2007), of which M. tuberculosis is a possible aetiological agent (van Enschot and van Balkom, 2013), the observed relatively frequent detection of the NPC2high biomarker should not compromise the application of this marker for the screening of active TB cases.
Considering the limitations of available routine methods for screening of M. tuberculosis infection among respiratory symptomatic or asymptomatic individuals, which hamper the control of this important illness, the profiling of NPC2 mRNA expression in blood seems to be an attractive alternative, since it has demonstrated an excellent accuracy using a fast methodology such as RT-qPCR for single-gene quantification in blood specimens. The additional similar results, obtained with populations of various genetic backgrounds and from different TB-burden scenarios, encourage us to stress the need for further validations of this biomarker in new cohorts, evaluating its modulation during disease progression and treatment success. In the meantime, the roles of DOCK9. EPHA4, and NPC2 genes in TB pathogenesis also merit further investigations.
Author Contributions
LA, FP, and MS designed the study. LA and MS wrote the manuscript. LV, MR-A, FM, AA, AM, AK, JL, MM, and FP modified the manuscript. Human samples were obtained by LA, MR-A, FM, AA, AM, AK, JL, MM, and MS. LA and AA performed the RT-qPCR experiments. LA and MR-A performed the microarray reanalysis. LA, LV, and MR-A conducted statistical analysis. All authors reviewed the results, made substantial contributions and approved the final version of the manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank Nidai de Bárbara da Silva and Janaína Leung for technical support, Aravind Tallam for bioinformatics support, and Michael Jarek and Sabin Bhuju for RNA sequencing.
Footnotes
Funding. This work was supported by CNPq (Science and Technology Ministry, Brazil), CAPES (Education Ministry, Brazil); Research Program for the Unified Health System (PPSUS-FAPERJ, Brazil); Program for Excellence Research Support of the Institute Oswaldo Cruz (PAEF, Health Ministry, FIOCRUZ, and Brazil); and by the Helmholtz Association’s Initiative on Individualized Medicine (iMed).
Supplementary Material
The Supplementary Material for this article can be found online at: http://journal.frontiersin.org/article/10.3389/fmicb.2016.01586
References
- Anderson S. T., Kaforou M., Brent A. J., Wright V. J., Banwell C. M., Chagaluka G., et al. (2014). Diagnosis of childhood tuberculosis and host RNA expression in Africa. N. Engl. J. Med. 370 1712–1723. 10.1056/NEJMoa1303657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Araujo L. S., Mello F. C., Silva Nde B., Leung J. A., Machado S. M., Sardella I. G. (2014). Evaluation of gamma interferon immune response elicited by the newly constructed PstS-1(285-374):CFP10 fusion protein to detect Mycobacterium tuberculosis infection. Clin. Vaccine Immunol. 21 552–560. 10.1128/CVI.00726-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett T., Wilhite S. E., Ledoux P., Evangelista C., Kim I. F., Tomashevsky M., et al. (2013). NCBI GEO: archive for functional genomics data sets–update. Nucleic Acids Res. 41 D991–D995. 10.1093/nar/gks1193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belay M., Bjune G., Ameni G., Abebe F. (2012). Diagnostic and treatment delay among tuberculosis patients in afar region, Ethiopia: a cross-sectional study. BMC Public Health 12:369 10.1186/1471-2458-12-369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry M. P., Graham C. M., Mcnab F. W., Xu Z., Bloch S. A., Oni T., et al. (2010). An interferon-inducible neutrophil-driven blood transcriptional signature in human tuberculosis. Nature 466 973–977. 10.1038/nature09247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bessarabova M., Kirillov E., Shi W., Bugrim A., Nikolsky Y., Nikolskaya T. (2010). Bimodal gene expression patterns in breast cancer. BMC Genomics 11(Suppl. 1):S8 10.1186/1471-2164-11-S1-S8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blankley S., Berry M. P., Graham C. M., Bloom C. I., Lipman M., O’garra A. (2014). The application of transcriptional blood signatures to enhance our understanding of the host response to infection: the example of tuberculosis. Philos. Trans. R. Soc. Lond. B Biol. Sci. 369:20130427 10.1098/rstb.2013.0427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloom C. I., Graham C. M., Berry M. P., Rozakeas F., Redford P. S., Wang Y., et al. (2013). Transcriptional blood signatures distinguish pulmonary tuberculosis, pulmonary sarcoidosis, pneumonias and lung cancers. PLoS ONE 8:e70630 10.1371/journal.pone.0070630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown K. A., Ham A. J., Clark C. N., Meller N., Law B. K., Chytil A., et al. (2008). Identification of novel Smad2 and Smad3 associated proteins in response to TGF-beta1. J. Cell. Biochem. 105 596–611. 10.1002/jcb.21860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen H., Boutros P. C. (2011). VennDiagram: a package for the generation of highly-customizable Venn and Euler diagrams in R. BMC Bioinform. 12:35 10.1186/1471-2105-12-35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deffur A., Wilkinson R. J., Coussens A. K. (2015). Tricks to translating TB transcriptomics. Ann. Transl. Med. 3:s43 10.3978/j.issn.2305-5839.2015.04.12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Equipe Gerência de Pneumologia Sanitária SES/RJ (2014). Boletim Tuberculose 2014 [Online]. Available: http://riocomsaude.rj.gov.br/Publico/MostrarArquivo.aspx?C=wXJ%2BKouHyII%3D (accessed April 7, 2016). [Google Scholar]
- Esterhuyse M. M., Weiner J., III, Caron E., Loxton A. G., Iannaccone M., Wagman C., et al. (2015). Epigenetics and proteomics join transcriptomics in the quest for tuberculosis biomarkers. MBio 6 e1187–e1115. 10.1128/mBio.01187-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gadea G., Blangy A. (2014). Dock-family exchange factors in cell migration and disease. Eur. J. Cell Biol. 93 466–477. 10.1016/j.ejcb.2014.06.003 [DOI] [PubMed] [Google Scholar]
- Golub J. E., Bur S., Cronin W. A., Gange S., Baruch N., Comstock G. W., et al. (2005). Patient and health care system delays in pulmonary tuberculosis diagnosis in a low-incidence state. Int. J. Tuberc. Lung Dis. 9 992–998. [PubMed] [Google Scholar]
- Guerreiro L. T., Robottom-Ferreira A. B., Ribeiro-Alves M., Toledo-Pinto T. G., Rosa Brito T., Rosa P. S., et al. (2013). Gene expression profiling specifies chemokine, mitochondrial and lipid metabolism signatures in leprosy. PLoS ONE 8:e64748 10.1371/journal.pone.0064748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jindani A., Nunn A. J., Enarson D. A. (2004). Two 8-month regimens of chemotherapy for treatment of newly diagnosed pulmonary tuberculosis: international multicentre randomised trial. Lancet 364 1244–1251. 10.1016/S0140-6736(04)17141-9 [DOI] [PubMed] [Google Scholar]
- Khalil K. F., Butt T. (2015). Diagnostic yield of bronchoalveolar lavage gene Xpert in smear-negative and sputum-scarce pulmonary tuberculosis. J. Coll. Physicians. Surg. Pak. 25 115–118. [PubMed] [Google Scholar]
- Laux da Costa L., Delcroix M., Dalla Costa E. R., Prestes I. V., Milano M., Francis S. S., et al. (2015). A real-time PCR signature to discriminate between tuberculosis and other pulmonary diseases. Tuberculosis (Edinb) 95 421–425. 10.1016/j.tube.2015.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S. W., Wu L. S., Huang G. M., Huang K. Y., Lee T. Y., Weng J. T. (2016). Gene expression profiling identifies candidate biomarkers for active and latent tuberculosis. BMC Bioinform. 17(Suppl. 1):3 10.1186/s12859-015-0848-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu C., Wu J., Wang H., Wang S., Diao N., Wang F., et al. (2011). Novel biomarkers distinguishing active tuberculosis from latent infection identified by gene expression profile of peripheral blood mononuclear cells. PLoS ONE 6:e24290 10.1371/journal.pone.0024290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maertzdorf J., Ota M., Repsilber D., Mollenkopf H. J., Weiner J., Hill P. C., et al. (2011). Functional correlations of pathogenesis-driven gene expression signatures in tuberculosis. PLoS ONE 6:e26938 10.1371/journal.pone.0026938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maertzdorf J., Weiner J., III, Mollenkopf H. J., Network T. B., Bauer T., Prasse A., et al. (2012). Common patterns and disease-related signatures in tuberculosis and sarcoidosis. Proc. Natl. Acad. Sci. U.S.A. 109 7853–7858. 10.1073/pnas.1121072109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nunes H., Bouvry D., Soler P., Valeyre D. (2007). Sarcoidosis. Orphanet J. Rare Dis. 2:46 10.1186/1750-1172-2-46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park W. D., O’brien J. F., Lundquist P. A., Kraft D. L., Vockley C. W., Karnes P. S., et al. (2003). Identification of 58 novel mutations in niemann-pick disease type C: correlation with biochemical phenotype and importance of PTC1-like domains in NPC1. Hum. Mutat. 22 313–325. 10.1002/humu.10255 [DOI] [PubMed] [Google Scholar]
- Poitz D. M., Ende G., Stutz B., Augstein A., Friedrichs J., Brunssen C., et al. (2015). EphrinB2/EphA4-mediated activation of endothelial cells increases monocyte adhesion. Mol. Immunol. 68 648–656. 10.1016/j.molimm.2015.10.009 [DOI] [PubMed] [Google Scholar]
- R Development Core Team (2014). R: A Language and Environment for Statistical Computing, 2 Edn Vienna: R Foundation for Statistical Computing. [Google Scholar]
- Rachow A., Zumla A., Heinrich N., Rojas-Ponce G., Mtafya B., Reither K., et al. (2011). Rapid and accurate detection of Mycobacterium tuberculosis in sputum samples by cepheid xpert MTB/RIF assay–a clinical validation study. PLoS ONE 6:e20458 10.1371/journal.pone.0020458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reichman L. B., Hersfield E. S. (1993). “Tuberculosis- a comprehensive international approach,” in Lung Biology in Health and Disease, eds Reichman L. B., Hersfield E. S. (New York, NY: Marcel Dekker Inc.), 149. [Google Scholar]
- Riedmaier I., Pfaffl M. W. (2013). Transcriptional biomarkers–high throughput screening, quantitative verification, and bioinformatical validation methods. Methods 59 3–9. 10.1016/j.ymeth.2012.08.012 [DOI] [PubMed] [Google Scholar]
- Ritz C., Spiess A. N. (2008). qpcR: an R package for sigmoidal model selection in quantitative real-time polymerase chain reaction analysis. Bioinformatics 24 1549–1551. 10.1093/bioinformatics/btn227 [DOI] [PubMed] [Google Scholar]
- Robin X., Turck N., Hainard A., Tiberti N., Lisacek F., Sanchez J. C., et al. (2011). pROC: an open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinformatics 12:77 10.1186/1471-2105-12-77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schluger N. W., Burzynski J. (2010). Recent advances in testing for latent TB. Chest 138 1456–1463. 10.1378/chest.10-0366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sia I. G., Wieland M. L. (2011). Current concepts in the management of tuberculosis. Mayo Clin. Proc. 86 348–361. 10.4065/mcp.2010.0820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh A., Winterbottom E., Daar I. O. (2012). Eph/ephrin signaling in cell-cell and cell-substrate adhesion. Front. Biosci. (Landmark Ed) 17:473–497. 10.2741/3939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Therneau T., Atkinson B., Ripley B. (2015). rpart: Recursive Partitioning and Regression Trees. R package version 4.1-10. Available at: http://CRAN.Rproject.org/package=rpart [Google Scholar]
- van Enschot J. W., van Balkom R. H. (2013). Sarcoidosis following Mycobacterium tuberculosis infection: coincidence or consequence. Respir. Med. Case Rep. 9 11–14. 10.1016/j.rmcr.2013.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wheelwright M., Kim E. W., Inkeles M. S., De Leon A., Pellegrini M., Krutzik S. R., et al. (2014). All-trans retinoic acid-triggered antimicrobial activity against Mycobacterium tuberculosis is dependent on NPC2. J. Immunol. 192 2280–2290. 10.4049/jimmunol.1301686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zak D. E., Penn-Nicholson A., Scriba T. J., Thompson E., Suliman S., Amon L. M., et al. (2016). A blood RNA signature for tuberculosis disease risk: a prospective cohort study. Lancet 387 2312–2322. 10.1016/S0140-6736(15)01316-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao S., Fung-Leung W. P., Bittner A., Ngo K., Liu X. (2014). Comparison of RNA-Seq and microarray in transcriptome profiling of activated T cells. PLoS ONE 9:e78644 10.1371/journal.pone.0078644 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.