Abstract
Sprint interval training (SIT) elicits comparable long-term adaptations versus continuous exercise training (CEX) including increased maximal oxygen uptake (VO2max) and fat utilization. However, there is limited research examining acute hemodynamic responses to SIT. The aim of this study was to examine hemodynamic responses to low-volume SIT. Active men (n=6, VO2max = 39.8 ± 1.7 mL/kg/min) and women (n=7, VO2max = 37.3 ± 5.7 mL/kg/min) performed a ramp-based VO2max test (RAMP) to determine workload for the SIT session. Subjects returned within 1 wk and completed a session of SIT consisting of six 30-s bouts of “all-out” cycling at 130% maximal workload (Wmax) interspersed with 120 s of active recovery. Continuously during RAMP and exercise and recovery in SIT, VO2 was obtained and thoracic impedance was used to estimate heart rate (HR), stroke volume (SV), and cardiac output (CO). Results revealed no significant differences in COmax (p = 0.12, 19.7 ± 2.4 L/min vs. 20.3 ± 1.8 L/min) but lower SVmax (p = 0.004, 110.4 ± 15.7 mL vs. 119.4 ± 15.5 mL) in RAMP versus SIT. HRmax from SIT (179.0 ± 11.8 b/min) was lower (p = 0.008) versus RAMP (184.4 ± 7.9 b/min). Peak VO2 (L/min) was lower (p < 0.001) in response to SIT (2.43 ± 0.82 L/min) compared to RAMP (2.84 ± 0.82 L/min). Hemodynamic variables increased linearly across SIT bouts and remained significantly elevated in recovery. Sprint interval training consisting of 3 min of supramaximal exercise elicits similar CO yet lower VO2 compared to RAMP.
Keywords: VO2max, cycle ergometer, cardiac output, stroke volume, interval training
Introduction
According to the Centers for Disease Control and Prevention (CDC), more than one-third of adults in the United States are obese. Obesity contributes to disease onset such as type 2 diabetes, cancer, heart disease, and stroke, all of which may be prevented through proper nutrition and exercise [1]. Modern exercise guidelines suggest 150 minutes of continuous exercise training (CEX) per week to mitigate health risks [2]; however, as this recommendation is relatively time-consuming, it is not feasible for all individuals considering that lack of time is a significant barrier to regular exercise [3]. As a result, exercise scientists have studied alternatives to CEX such as high intensity interval training (HIIT) consisting of repeated, intense brief bursts of exercise interspersed with recovery. One paradigm of HIIT is sprint interval training (SIT), which has been shown to elicit comparable long-term metabolic and cardiovascular adaptations versus CEX despite a much lower training volume and training time [4]. For example, in response to 6 wk of treadmill-based SIT, there were similar increases in maximal oxygen uptake (VO2max) compared with CEX [5]. In overweight/obese subjects, Gillen et al. [6] showed significant increases in VO2max and oxidative capacity in response to 3 min/wk of SIT which was performed at 170% maximal workload (Wmax). The mean improvement in VO2max reported in response to 2-8 wk of SIT is 4-13% in healthy individuals [7], which is an important outcome considering the effect of VO2max on mortality risk [8].
Despite the clear evidence that chronic SIT enhances VO2max, the mechanism responsible for this adaptation remains undetermined. In the MacPherson et al. [5] study, maximal cardiac output (COmax) did not change after 6 wk of SIT, which suggests that peripheral adaptations led to the increase in VO2max. In another study in obese women [9] in which a 12% increase in VO2max was exhibited, stroke volume (SV) at 50% VO2max was increased in response to 12 sessions of SIT, although no maximal values were determined. Matsuo et al. [10] documented that 8 wk of SIT led to improved resting SV and left ventricular mass, although similar to the Trilk et al. [9] study, measures were not acquired at VO2max.
It is evident that chronic adaptations to exercise training such as increases in VO2max occur due to the repeated stimulation of daily bouts of training. One study examining acute physiological adaptations during a single session of Wingate-based SIT found that oxygen uptake and heart rate surpassed 80% of estimated maximal values [11]. In another study [12], a single Wingate test elicited similar values of cardiac output (CO) versus ramp exercise to VO2max (RAMP). This would suggest that despite its brief duration, SIT places a tremendous stress upon the cardiovascular system. In active young men (VO2max = 49 mL/kg/min), Zafeiridis et al. [13] compared changes in CO and peripheral O2 utilization between acute SIT (29 repeats of 30 s bouts at 110% Wmax with 30 s passive recovery), HIIT (nine 2 min bouts at 95% Wmax with 2 min passive recovery), and CEX at 70% Wmax which were matched for duration (29 min). Results showed comparable peak values of SV, arteriovenous oxygen difference, and blood pressure between bouts, although peak heart rate (HR), CO, and VO2 were higher in response to HIIT and continuous exercise versus SIT. These data suggest that SIT elicits lower maximal CO and thus VO2 compared to high volume HIIT or CEX. Nevertheless, this study is limited by lack of RAMP-derived values for CO and a relatively prolonged session of SIT which would be impractical for most exercisers who lack the fitness, time, or motivation to perform. A shorter SIT regimen would be advantageous considering that minimal volumes of SIT have been shown to improve VO2max [6,14].
Numerous studies demonstrate the beneficial effects of chronic SIT [4-6], while no study has elucidated the acute hemodynamic responses during a single session of low-volume SIT. Findings from the current study could help clarify long-term hemodynamic adaptations to SIT. Moreover, changes in SV and CO during recovery are poorly understood and if they remain significantly elevated, may contribute to the training effect seen with SIT. The primary aim of this study was to examine hemodynamic responses to a brief session of SIT in habitually-active men and women. It was hypothesized that there would be no differences in hemodynamic responses between SIT and RAMP, and that HR, SV, and thus CO would be sustained at high levels during active recovery.
Materials and methods
Participants
Thirteen habitually active men (n=6) and women (n=7) participated in the study. Demographics of the subjects are depicted in Table 1. Habitually active was defined as meeting the current American College of Sports Medicine recommendation [2] of at least 150 min/wk of physical activity in the preceding year. Subjects completed activities such as resistance training, aerobic exercise, and non-competitive sports. Participants were free of knee ailments and other pre-existing health conditions that would inhibit their ability to participate in intense cycling. Participants were not obese (BMI < 30 kg/m2) and had a BMI equal to 24.9 ± 3.5 kg/m2. Men were older and heavier than women yet showed similar VO2max (p = 0.08). Each participant filled out a health history questionnaire to confirm study eligibility and provided written informed consent. The procedures completed in this study were approved by the University Institutional Review Board.
Table 1.
Participant demographic data (mean ± SD)
| Parameter | Men (n=6) | Women (n=7) |
|---|---|---|
| Age (yr) | 29.5 ± 7.6 | 22.9 ± 1.7* |
| Height (cm) | 179.0 ± 11.2 | 165.6 ± 7.2* |
| Body mass (kg) | 87.3 ± 16.3 | 61.9 ± 8.0* |
| Body mass index (kg/m2) | 27.1 ± 2.7 | 22.6 ± 2.8* |
| VO2max (mL/kg/min) | 39.8 ± 1.7 | 37.3 ± 5.7 |
p < 0.05 versus men.
Study design
Subjects completed two visits to the laboratory in a one week period. Exercise sessions were conducted at the same time of day within subjects, and were held approximately three hours after a light meal. Prior to each visit, participants abstained from strenuous exercise for 24 hr and alcohol for 48 hr. On day 1, a ramp protocol to volitional fatigue was performed to determine VO2max and maximal workload (Wmax) followed by a single session of SIT 3-7 d later.
Assessment of maximal oxygen uptake (VO2max)
Initially, participants’ height and body mass were measured using a calibrated scale (Healthometer, Model 402KL, Jarden, Wilmington, DE, USA), from which body mass index was determined. Subsequently, ramp exercise was performed on an electrically-braked cycle ergometer (RacerMate Dynafit Pro, Seattle, WA, USA). Participants completed a 2 min warm-up at 50-60 W followed by 25-30 W/min increments in work rate until volitional exhaustion (cadence < 50 rev/min). VO2max attainment was verified by incidence of a plateau in VO2 at VO2max, a respiratory exchange ratio (RER) > 1.10, and HRmax ± 10 b/min within 220-age [15]. At volitional exhaustion, VO2max was determined as the mean of the two preceding 15 s values, and Wmax was noted and used to determine intensities for the SIT protocol. During exercise, expired air was measured by a metabolic cart (Parvomedics True One, Sandy, Utah, USA). Prior to exercise, the metabolic cart was calibrated to room air (temperature = 21-23°C, relative humidity = 40-60%) and to gases of known concentration (16.00% O2 and 3.99% CO2). A 3-L calibration syringe (Hans Rudolph, Kansas City, MO, USA) was used for volume calibration. Values for the following variables were obtained every 15 s during exercise: VO2 (L/min and mL/kg/min), carbon dioxide output (VCO2), ventilation (VE), and RER.
Assessment of hemodynamic function
An impedance cardiograph device (Physioflow Enduro, Manatec, Strasbourg, France) was used to evaluate hemodynamic function. This method has been described in detail elsewhere [16] and been found valid and reliable at rest and during exercise up to VO2max. This method detects changes in transthoracic impedance during phases of the cardiac cycle to calculate SV, which is multiplied by HR to estimate CO. Participants entered the laboratory and were required to sit quietly for approximately 5 min. An alcohol swab was used to clean the neck, right chest, trunk at V6, and spine, and then an electrode gel (NuPrep, Weaver and Company, Aurora, CO) was rubbed into these areas and the skin was further cleaned with a paper towel. Two sets of electrodes (Skintact ECG electrodes, Leonhard Lang GmbH, Innsbruck, Austria), one electrode transmitting and the other sensing, were applied above the supraclavicular fossa at the left base of the neck and at the height of the xiphoid on the spine. Another pair of electrodes (one placed on the right chest and another at V6) was used to monitor the ECG trace. Once applied, these leads were taped to the skin to minimize movement. The participant was seated on the cycle ergometer for 2 min, blood pressure (BP) was recorded at the antecubital space, and they were told not to talk and remain motionless. Then, the device was calibrated following a 30-beat procedure using the baseline BP value, which was averaged.
Once calibration was completed, resting values for HR, SV, and CO were obtained after which the warm-up began. During exercise, HR, SV, and CO values were determined every 10 s. Maximal values of HR, SV, and CO were identified as the highest values at any point during exercise. To represent hemodynamic responses for each SIT bout, the last two values of each bout and the first value in the recovery period were averaged, and values from the last 1 min of the cool-down period (six consecutive values) were averaged to indicate recovery values. Peak arteriovenous oxygen difference (a-vO2diff) was calculated as the quotient of VO2max (mL/min)/COmax (L/min) and expressed in mL/dL.
Completion of sprint interval training (SIT)
On the second visit, participants completed a SIT session on the identical electrically-braked cycle ergometer that consisted of six 30 s “all-out” sprints at 130% Wmax. Bouts were interspersed with 2 min active recovery at 20% Wmax. All SIT sessions were preceded by a 4 min warm-up at 20% Wmax. Occasionally, participants required additional recovery time when they were unable to initiate the subsequent sprint bout. Strong verbal encouragement was provided to subjects during SIT. Gas exchange data and thoracic impedance data were continuously obtained during this session.
Data analysis
Data are expressed as mean ± standard deviation and were analyzed with SPSS (version 22.0; IBM Corp., Armonk, N.Y., USA). Dependent t-test was used to examine differences in peak values between RAMP and SIT. One-way repeated measures ANOVA was used to identify potential differences in variables between RAMP and SIT. Gender was labeled as the between subjects variable. If a significant F value was detected, Bonferroni’s post hoc test was used to determine which comparisons were significantly different. Effect size was expressed as partial eta-squared (η2 p). Statistical significance was equal to p < 0.05.
Results
All participants completed all sessions. Data were combined across men and women as there were no gender differences in hemodynamic responses during SIT (p > 0.05), although SVmax (p = 0.009, 119.9 ± 12.9 mL vs. 100.2 ± 13.0 mL) and COmax (p = 0.02, 21.1 ± 1.9 L/min vs. 18.3 ± 2.4 L/min) were higher in men versus women as previously reported [17].
Gas exchange data
Table 2 reports peak values for VO2 (L/min), VCO2, VE, and RER for both RAMP and SIT. Change in VO2 during the entire session of SIT is reported in Figure 1. Mean VO2 steadily increased (p < 0.001) from rest (0.34 ± 0.10 L/min) to 2.14 ± 0.59 L/min at bout 1 to 2.43 ± 0.63 L/min at bout 6, with all values lower than RAMP. All exercise VO2 values were significantly different from each other (p < 0.05). The greatest value for VO2 (L/min) during SIT was from bout 5 (2.46 ± 0.65 L/min), which was significantly lower (p = 0.002) than RAMP-derived VO2max (2.84 ± 0.82 L/min) and equal to 85.6% of the RAMP value. Recovery VO2 values increased from after bout 1 (1.52 ± 0.48 L/min) to post-bout 5 (1.61 ± 0.49 L/min) which equals 53.1-55.6% VO2max from RAMP. Post hoc analyses showed no difference (p > 0.75) in recovery VO2 across bouts. Bonferroni’s post hoc test showed that VO2 was significantly lower during all recovery periods compared to all exercise values in RAMP and SIT.
Table 2.
Comparison of peak responses between SIT and RAMP (mean ± SD)
| Parameter | SIT | RAMP |
|---|---|---|
| VO2 (L/min) | 2.46 ± 0.65 | 2.84 ± 0.82* |
| VCO2 (L/min) | 2.71 ± 0.81 | 3.60 ± 0.98* |
| Ventilation (L/min) | 101.6 ± 30.6 | 111.2 ± 28.0 |
| RER | 1.14 ± 0.09 | 1.27 ± 0.06* |
| Heart rate (b/min) | 178.2 ± 11.8 | 184.4 ± 7.9* |
| Stroke volume (mL) | 117.2 ± 12.4 | 110.9 ± 15.4* |
| Cardiac output (L/min) | 20.3 ± 1.8 | 19.7 ± 2.4 |
| Arteriovenous O2 difference (mL/dL) | 13.6 ± 3.2 | 14.2 ± 2.7 |
p < 0.05 versus SIT.
Figure 1.
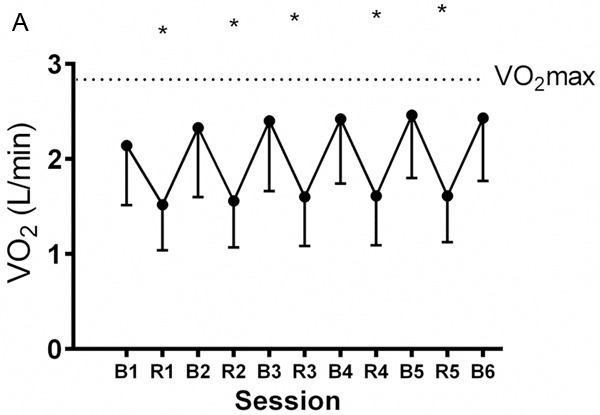
Mean ± SD change in VO2 during a single session of SIT (B= bout, R= rest); * = p < 0.05 for recovery versus exercise values. The dashed line represents maximal oxygen uptake from RAMP.
Hemodynamic responses
Maximal hemodynamic variables are shown in Table 2. Peak HR during RAMP (Table 2) was significantly higher (p = 0.008, η2 p = 0.86) than HR from SIT. Heart rate increased from rest (82.2 ± 10.1 b/min) during SIT (p < 0.001) with all exercise values different from each other (Figure 2A) with exception of bouts 3-6. HR was equal to 161.8 ± 14.2 b/min after bout 1 and peaked at 178.2 ± 11.8 b/min at bout 6 of SIT. During recovery, HR post-bout 1 differed from all other values. Mean HR in recovery was equal to 154.0 ± 21.3 b/min which is 83.2% of the RAMP value. Peak SV from RAMP was lower (p = 0.034, η2 p = 0.38) than SV in SIT; however, during SIT, there no change (p = 0.12) in SV throughout the entire session (Figure 2B) although it did increase from rest (82.9 ± 14.7 mL), and small declines in SV were exhibited in active recovery. Maximal CO during RAMP was similar versus SIT (p = 0.12). During SIT, CO increased from rest (6.7 ± 1.1 L/min) and was equal to 18.3 ± 2.9 L/min at bout 1, which is 93% of the RAMP value, and peaked at 20.3 ± 1.8 L/min at bout 6 (Figure 2C). All exercise values were not different (p > 0.05) from each other. Recovery CO was equal to 15.0 ± 2.6 L/min after bout 1 and gradually increased to 16.7 ± 3.1 L/min after bout 5, although no significant differences in recovery CO were seen throughout SIT. Mean CO during recovery was equal to 15.9 ± 2.8 L/min which is 81% of the RAMP derived maximal value. Post hoc analyses revealed significantly lower CO during recovery versus exercise values.
Figure 2.
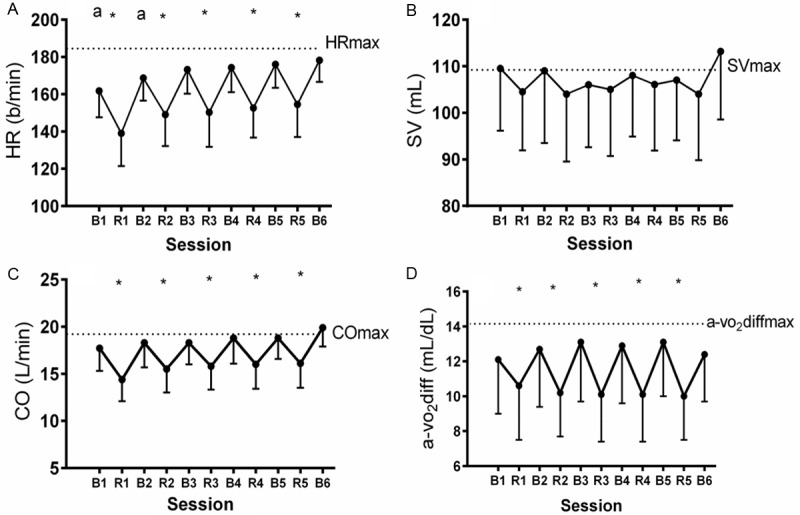
Mean ± SD change in (A) HR; a = p < 0.05 versus peak values, * = p < 0.05 for recovery versus exercise values, (B) SV, (C) CO; * = p < 0.05 for recovery versus exercise values, and (D) a-vO2difference; * = p < 0.05 for recovery versus exercise values, during a single session of SIT (B= bout, R= rest). In all figures, the dashed line represents maximal values from RAMP.
Results showed that a-vO2diff increased from rest (5.1 ± 1.6 mL/dL) and peaked at bout 3 of SIT (13.6 ± 3.2 mL/dL), which was similar (p = 0.38) to the peak RAMP value equal to 14.2 ± 2.7 mL/dL (Table 2). Arteriovenous O2 difference did not change across SIT bouts, although recovery values were lower (p < 0.05) than those recorded at the end of each bout (Figure 2D).
Discussion
Although VO2max is significantly increased in response to low-volume SIT [7], the mechanism explaining this finding is unknown. The primary aim of this study was to compare acute hemodynamic responses between a brief session of SIT and a ramp-based VO2max test. The results of the present study oppose the hypothesis as SIT elicits lower HRmax, higher SVmax, but similar COmax compared to RAMP, although VO2 was lower versus RAMP. The second part of the hypothesis was also supported, showing elevated levels of cardiac work during active recovery at intensities equal to 20% Wmax. Despite the intermittent nature of SIT, it exerts a substantial and sustained load on the cardiovascular system which may explain a portion of the increase in VO2max seen with chronic interval training.
The major finding in this study was that each 30 s SIT bout elicits similar CO values exceeding 90% COmax, with all values comparable to RAMP. Similar CO was also demonstrated in active men completing 15 min of steady-state exercise at 65% Wmax and interval training at 85% Wmax [18]. In healthy men [19], no difference in CO was observed in response to a single Wingate test compared to RAMP, although SV was higher and HR was lower, as seen in the present study (Table 2). Data from Adami et al. [20] in well-trained men showed similar CO in response to cycling at 120% VO2max versus RAMP, which was consequent with faster CO kinetics during interval training despite slower VO2 kinetics. This was explained by the higher contribution of anaerobic metabolism towards ATP supply at 120% VO2max, leading to a smaller volume of O2 taken up at the alveolar level. This may partially explain why peak VO2 was lower in SIT versus RAMP despite the similar CO (Table 2). In young men and women with VO2max = 52.3 mL/kg/min [21], CO was significantly higher in response to 6 min versus 12 min of graded treadmill exercise, although VO2max was similar to the RAMP value. This was attributed to a higher temperature rise in the longer protocol which would lead to vasodilation of the cutaneous circulation, thus reducing central venous pressure and SV. It is plausible that brief bouts of SIT coupled with long periods of recovery do not allow body temperature to rise sufficiently to diminish CO. These data and ours show a disassociation between maximal CO and VO2max. Nevertheless, comparisons between these studies and ours should be cautioned considering that participant characteristics, exercise protocols, and methods for measuring CO differ across studies.
Our findings show significantly higher peak SV during SIT versus RAMP (Table 2), and moreover, that SV did not decline during recovery compared to values exhibited at the end of each SIT bout (Figure 2B). In trained cyclists completing interval training at 90% Wmax, SV attained 102% of RAMP derived values [22]. Supporting our data (Figure 2B), their recovery SV values were similar to those seen during interval training. In response to repeated 30 s bouts of interval training, mean SV was lower than values shown during CEX and 2 min interval bouts, although peak values did not differ [13]. This is due to the action of the muscle pump during active recovery, which influences peripheral resistance and venous return to maintain SV. Among the factors that may limit VO2max, SV appears to be paramount as it is significantly different between trained and untrained individuals [23]. Given this information, it is plausible that in order to attain the optimal cardiovascular benefits of exercise training, individuals should train at intensities maximizing SV, as exhibited in the entire session of SIT (Figure 2B), to achieve sufficient overload and greater training adaptation [23].
Our results show no difference in peak a-vO2diff between SIT and RAMP as well as no change in this variable from bouts 1-6 of SIT. These data are supported by previous findings showing similar mean and peak a-vO2diff between CEX, high-volume HIIT, and SIT [13]. Together, this would indicate that peripheral oxygen utilization as represented by the a-vO2diff does not change during bouts of cycling varying in intensity from submaximal to supramaximal. In a recent study [24], 11 men completed incremental exercise and a 30 s Wingate test during which oxygen delivery and hemodynamics were measured. Data showed that leg fractional oxygen extraction was similar between exercise modes despite lower whole-body and leg VO2 during the Wingate test versus RAMP. This led the authors to conclude that a single bout of supramaximal exercise such as the Wingate test has a mismatch between oxygen delivery and oxygen uptake in that the muscle is overperfused and unable to fully utilize the available oxygen. This may explain the similar CO but significantly lower VO2 between RAMP and SIT.
Compared to RAMP, our data showing lower oxygen uptake throughout SIT are supported by previous findings. In healthy adults, VO2 was lower in response to eight bouts of the identical SIT regime compared to eight 60 s bouts of HIIT at 85% Wmax or RAMP [25]. Tschakert et al. [26] demonstrated in cardiac patients that repeated 20 s bouts of SIT evokes lower VO2 and HR versus high volume HIIT or RAMP. Our data show that peak VO2 from SIT was equal to 84.6% VO2max, which is similar to values (> 80% VO2max) reported from a previous study [11] in which four Wingate tests were performed separated by 4 min recovery. Despite the submaximal VO2 values likely attributed to a lower contribution of oxidative metabolism to ATP supply versus RAMP, low volume SIT presents a significant cardiorespiratory stimulus that exceeds current intensity recommendations for CEX. Consequently, it is not surprising that chronic SIT increases VO2max in various populations [7].
One limitation of this study was the small sample size consisting of active young men and women, so data cannot be applied to older or less active populations. Another limitation of the study was the prolonged recovery time that was allocated between bouts, which ensured that all participants could complete the entire session. Shorter recovery would minimize the duration of the bout and potentially lead to lower decreases in hemodynamic responses, presenting even greater load on the cardiovascular system. This longer recovery likely contributed to the significant differences in HR between SIT bouts and periods of recovery. Previous data [12] from RAMP exercise show that day-to-day estimates of maximal CO determined from thoracic impedance are highly related (ICC = 0.95) and higher than those from the Wingate test (ICC = 0.90). To our knowledge, the reliability of CO measures during a session of interval training using thoracic impedance is unknown.
Acknowledgements
The authors appreciate the dedication of the participants in completing the requirements of this study.
References
- 1.Ogden CL, Carroll MD, Fryar CD, Flegal KM. Prevalence of obesity among adults and youth: United States, 2011-2014. NCHS Data Brief. 2015:1–8. [PubMed] [Google Scholar]
- 2.Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee IM, Neiman DC, Swain DP. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43:1334–1359. doi: 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]
- 3.Trost SG, Owen N, Bauman AE, Sallis JF, Brown W. Correlates of adults’ participation in physical activity: review and update. Med Sci Sports Exerc. 2002;34:1996–2001. doi: 10.1097/00005768-200212000-00020. [DOI] [PubMed] [Google Scholar]
- 4.Burgomaster KA, Howarth KR, Phillips SM, Rakobowchuk M, Macdonald MJ, McGee SL, Gibala MJ. Similar metabolic adaptations during exercise after low volume sprint interval and traditional endurance training in humans. J Physiol. 2008;586:151–160. doi: 10.1113/jphysiol.2007.142109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Macpherson RE, Hazell TJ, Olver TD, Paterson DH, Lemon PWR. Run sprint interval training improves aerobic performance but not maximal cardiac output. Med Sci Sports Exerc. 2010;43:115–122. doi: 10.1249/MSS.0b013e3181e5eacd. [DOI] [PubMed] [Google Scholar]
- 6.Gillen JB, Percival ME, Skelly LE, Martin BJ, Tan RB, Tarnopolsky MA, Gibala MJ. Three minutes of all-out intermittent exercise per week increases skeletal muscle oxidative capacity and improves cardiometabolic health. PLoS One. 2014;9:e111489. doi: 10.1371/journal.pone.0111489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sloth M, Sloth D, Overgaard K, Dalgas U. Effects of sprint interval training on VO2max and aerobic exercise performance: A systematic review and meta-analysis. Scand J Med Sci Sports. 2013;23:e341–e352. doi: 10.1111/sms.12092. [DOI] [PubMed] [Google Scholar]
- 8.Myers J, Prakash M, Froelicher V, Do D, Partington S, Atwood JE. Exercise capacity and mortality among men referred for exercise testing. N Engl J Med. 2002;346:793–801. doi: 10.1056/NEJMoa011858. [DOI] [PubMed] [Google Scholar]
- 9.Trilk JL, Singhal A, Bigelman KA, Cureton KJ. Effect of sprint interval training on circulatory function during exercise in sedentary, overweight/obese women. Eur J Appl Physiol. 2010;111:1591–1597. doi: 10.1007/s00421-010-1777-z. [DOI] [PubMed] [Google Scholar]
- 10.Matsuo T, Saotome K, Seino S, Shimojo N, Matsushita A, Iemitsu M, Oshima H, Tanaka K, Mukai C. Effects of a low-volume aerobic-type interval exercise on VO2max and cardiac mass. Med Sci Sports Exerc. 2014;46:42–50. doi: 10.1249/MSS.0b013e3182a38da8. [DOI] [PubMed] [Google Scholar]
- 11.Freese EC, Gist NH, Cureton KJ. Physiological responses to an acute bout of sprint interval cycling. J Strength Cond Res. 2013;27:2768–2773. doi: 10.1519/JSC.0b013e318281575c. [DOI] [PubMed] [Google Scholar]
- 12.Astorino TA, Bovee C, DeBoe A. Estimating hemodynamic responses to the Wingate test using thoracic impedance. J Sports Sci Med. 2015;14:834–840. [PMC free article] [PubMed] [Google Scholar]
- 13.Zafeiridis A, Kounoupis A, Dipla K, Kyparos A, Nikolaidis MG, Smilios I, Vrabas IS. Oxygen delivery and muscle deoxygenation during continuous, long- and short-interval exercise. Int J Sports Med. 2015;36:872–880. doi: 10.1055/s-0035-1554634. [DOI] [PubMed] [Google Scholar]
- 14.Metcalfe RS, Babraj JA, Fawkner SG, Vollaard NB. Towards the minimal amount of exercise for improving metabolic health: beneficial effects of reduced-exertion high-intensity interval training. Eur J Appl Physiol. 2012;112:2767–2775. doi: 10.1007/s00421-011-2254-z. [DOI] [PubMed] [Google Scholar]
- 15.Astorino TA. Alterations in VO2max and the VO2 plateau with manipulation of sampling interval. Clin Physiol Funct Imaging. 2009;29:60–67. doi: 10.1111/j.1475-097X.2008.00835.x. [DOI] [PubMed] [Google Scholar]
- 16.Charloux A, Lonsdorfer-Wolf E, Richard R, Lampert E, Oswald-Mammosser M, Bertrand M, Geny B, Lonsdorfer J. A new impedance cardiographic device for the non-invasive evaluation of cardiac output at rest and during exercise: a comparison with the “direct” Fick method. Eur J Appl Physiol. 2000;82:313–320. doi: 10.1007/s004210000226. [DOI] [PubMed] [Google Scholar]
- 17.Vella CA, Robergs RA. A review of the stroke volume response to upright exercise in healthy subjects. Br J Sports Med. 2005;39:190–195. doi: 10.1136/bjsm.2004.013037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Foster C, Meyer K, Georgakopoulos N, Ellestad AJ, Fitzgerald DJ, Tilman K, Weinstein H, Young H, Roskamm H. Left ventricular function during interval and steady state exercise. Med Sci Sports Exerc. 1999;31:1157–1162. doi: 10.1097/00005768-199908000-00012. [DOI] [PubMed] [Google Scholar]
- 19.Fontana P, Betschon K, Boutellier U, Toigo M. Cardiac output but not stroke volume is similar in a Wingate and VO2peak test in young men. Eur J Appl Physiol. 2011;111:155–158. doi: 10.1007/s00421-010-1645-x. [DOI] [PubMed] [Google Scholar]
- 20.Adami A, Pogliaghi S, De Roia G, Capelli C. Oxygen uptake, cardiac output, and muscle deoxygenation at the onset of moderate and supramaximal exercise in humans. Eur J Appl Physiol. 2011;111:1517–1527. doi: 10.1007/s00421-010-1786-y. [DOI] [PubMed] [Google Scholar]
- 21.McCole S, Davis A, Fueger P. Is there a disassociation of maximal oxygen consumptionand maximal cardiac output? Med Sci Sports Exerc. 2001;33:1265–1269. doi: 10.1097/00005768-200108000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Stanley J, Buchheit M. Moderate recovery unnecessary to sustain high stroke volume during interval training. A brief report. J Sports Sci Med. 2014;13:393–396. [PMC free article] [PubMed] [Google Scholar]
- 23.Wang E, Solli GS, Nyberg SK, Hoff J, Helgerud J. Stroke volume does not plateau in female endurance athletes. Int J Sports Med. 2012;33:734–739. doi: 10.1055/s-0031-1301315. [DOI] [PubMed] [Google Scholar]
- 24.Calbet JA, Losa-Reyna J, Torres-Peralta R, Rasmussen P, Ponce-González JG, Sheel AW, de la Calle-Herrero J, Guadalupe-Grau A, Morales-Alamo D, Fuentes T, Rodríguez-García L, Siebenmann C, Boushel R, Lundby C. Limitations to oxygen transport and utilization during sprint exercise in humans: evidence for a functional reserve in muscle oxygen diffusing capacity. J Physiol. 2015;593:4649–4664. doi: 10.1113/JP270408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wood KM, LaValle K, Greer K, Bales B, Thompson H, Astorino TA. Effects of two regimens of high intensity interval training (HIIT) on acute physiological and perceptual responses. J Str Cond Res. 2016;30:244–50. doi: 10.1519/JSC.0000000000001042. [DOI] [PubMed] [Google Scholar]
- 26.Tschakert G, Kroepfl JM, Mueller A, Harpf H, Harpf L, Traninger H, Wallner-Liebmann S, Stojakovic T, Scharnagl H, Meinitzer A, Pichlhoefer P, Hofmann P. Acute physiological responses to short- and long-stage high-intensity interval exercise in cardiac rehabilitation: A pilot study. J Sports Sci Med. 2016;15:80–91. [PMC free article] [PubMed] [Google Scholar]


