Abstract
Background: Familismo or familism is a cultural value frequently seen in Hispanic cultures, in which a higher emphasis is placed on the family unit in terms of respect, support, obligation, and reference. Familism has been implicated as a protective factor against mental health problems and may foster the growth and development of children. This study aims at measuring the size of the relationship between familism and mental health outcomes of depression, suicide, substance abuse, internalizing, and externalizing behaviors.
Methods: Thirty-nine studies were systematically reviewed to assess the relationship between familism and mental health outcomes. Data from the studies were comprised and organized into five categories: depression, suicide, internalizing symptoms, externalizing symptoms, and substance use. The Cohen's d of each value (dependent variable in comparison to familism) was calculated. Results were weighted based on sample sizes (n) and total effect sizes were then calculated. It was hypothesized that there would be a large effect size in the relationship between familism and depression, suicide, internalizing, and externalizing symptoms and substance use in Hispanics.
Results: The meta-analysis showed small effect sizes in the relationship between familism and depression, suicide and internalizing behaviors. And no significant effects for substance abuse and externalizing behaviors.
Discussion: The small effects found in this study may be explained by the presence of moderator variables between familism and mental health outcomes (e.g., communication within the family). In addition, variability in the Latino samples and in the measurements used might explain the small and non-significant effects found.
Keywords: familism, depression, suicide, substance abuse, internalizing, externalizing, Latino
According to the U.S. Census Bureau (2011), the Latino population has increased by almost 43% in 10 years (2000–2010) within the U.S. This growth accounts for over half of the increase in the total U.S. population (U.S. Census Bureau, 2011). Along with the rapid increase of this population, the magnitude of their socio-economic and health indicators have become public interest: 22% of Latino adults live below the poverty level (U.S. Census Bureau, 2013); 37% of Latinos are uninsured (Brown et al., 2000), only 1 out of 11 Latino-Americans with mental disorders contact a mental health care specialist (U.S. Department of Health and Human Services, 2001), and Latino adolescents have high rates of major depressive episodes and a low percentage is receiving treatment [Substance Abuse and Mental Health Services Administration (SAMHSA), 2015]. Nevertheless, conflicting evidence in mental health outcomes is found when the adult Latino population is analyzed. Alegría et al. (2008) found that Latino adults have lower prevalence of several mental health disorders compared to non-Latino whites. This type of evidence gives support to the Hispanic or Immigrant Paradox that has become a matter of interest in the past 10 years. This paradox establishes that Latinos or Hispanics sustain a health advantage over non-Hispanic whites (Elo et al., 2004; see Blanco et al., 2013). In this study, we considered Latinos or Hispanic as exchangeable words, although they do not refer to the same concept (see Gonzalez, 1992, November 15).
Even though the Hispanic paradox places immigrant Hispanics in a healthier position than non-Hispanic whites and Hispanic-Americans, the mental health outcomes reported by the American Psychiatric Association (APA, 2014); Substance Abuse and Mental Health Services Administration (SAMHSA, 2015), and the National Alliance for Mental Illnesses (NAMI, 2002) indicate that Latinos in general are at risk for several conditions. Both evidences for and against the Hispanic Paradox have placed a demand for research, to understand the factors associated with the health outcomes of Latinos. Hispanic cultural values have become an area of interest due to the suggested protective factor that they may serve (Smokowski et al., 2009; Calzada et al., 2012). One of the most studied Hispanic core cultural values is familismo or familism in which a higher emphasis is placed on the family unit in terms of respect, support, obligation, and reference (Calzada et al., 2012). It is of interest in this systematic review to analyze the relationship between familism and mental health outcomes in Latino populations.
Familism
Familism refers to the cultural value that one's family is expected to provide necessary emotional and instrumental social support when needed (Sabogal et al., 1987; Calzada et al., 2012). At the same time, familism creates a sense of obligation to take care of one's family, and to take one's family into consideration when making decisions. In this sense, family becomes a source of information for behaviors and attitudes (Parsai et al., 2009; Davila et al., 2011). There are three measures (structural, behavioral, and attitudinal) that can be used to assess levels of familism. Structural familism is the physical proximity to family members, behavioral is the behavior in relation to their family's values and expectations and lastly is attitudinal familism. Attitudinal familism measures an individual's thoughts and feelings on the three different aspects of familism: (a) supportive familism signifies the level to which the individual feels supported by his or her family and the degree of closeness in their family; (b) obligatory familism is the extent to which an individual believes the family has a responsibility to provide support (economic, social, or emotional) to other family members; and (c) referent familism is the extent to which one maintains behaviors that are consistent with the family values and expectations (Sabogal et al., 1987; Marsiglia et al., 2009). It is frequently specified that involvement in Latino culture is critical for high familism attitudes and that greater acculturation to American culture and more time spent in the United States is linked to lower levels of familism (Smokowski et al., 2009). Studies included in this meta-analysis measured attitudinal familism, through a series of questions or familistic statements based on a Likert scale.
Familism and mental health outcomes
Attitudinal familism has been implicated by many as a protective variable against mental health problems and fosters the growth and development of children (Zeiders et al., 2013). There is substantial literature to suggest this is a protective factor particularly among Latinos and also among Asians (Calzada et al., 2012).
It has been found that the high levels of family supportiveness among Mexican American families serve as a protective factor during times of crises and psychological distress (Umaña-Taylor et al., 2011). Furthermore, poor mental health has been linked to low levels of familism (Ornelas and Perreira, 2011). In a 2011 study, familism was found to moderate some variables of stress (i.e., acculturative stress) but was found insignificant in others (i.e., discrimination, economic hardship; Umaña-Taylor et al., 2011). The relationship between familism and depression and other internalizing symptoms varies throughout the literature with some studies showing no interaction between the two, others showing more depressive symptoms with higher familism levels (Zeiders et al., 2013) and some displaying familism as a protective buffer against depression (Ornelas and Perreira, 2011). These inconsistencies require further research between familism and depression.
Research investigating the association between familism and suicidal attempts has suggested familism as a protective factor because the greater sense of loyalty to the family offers a reason to live (Garza and Pettit, 2010). However, there is contradicting literature; some researchers have found that many adolescent Latina suicide attempters take on blame and guilt for family problems suggesting that perhaps familism could create an additional responsibility upon young Latinas (Kuhlberg et al., 2010). This is a very under researched area that necessitates more attention.
There is a plethora of consistent research on lower substance use, binge drinking, and smoking in Hispanics implying that cultural values play a significant role. A study done at the Institute for Health Promotion and Disease Prevention stated that perhaps the relationship that continues to appear between lower levels of substance use and Hispanics is due to familism by enhancing the responsibilities of the individual to positively represent their family (Soto et al., 2011). Many studies strictly look at drinking while others look at illicit drug use or marijuana, causing a need for more comprehensive research.
As previously stated, the relationship between familism and internalizing symptoms is inconsistent throughout the literature. There have been studies showing that familism moderates the relationship between risk factors (i.e., parent adolescent conflict) and outcome (i.e., internalizing symptoms), while others show contradicting evidence (Vargas et al., 2013). One study by Smokowski and colleagues in 2009 supports familism as a protective cultural factor against internalizing symptoms, noting that higher familism is related to lower internalizing symptoms (Smokowski et al., 2010). Other studies claim the protection of familism is mediated by parent-adolescent conflict (Smokowski and Bacallao, 2007; Smokowski et al., 2007). While there is much literature in support of familism as a protective factor, there is still inconsistency, demanding more research before conclusions can be confidently drawn.
Protective effects of familism on externalizing behaviors have been theorized to be because adolescents with higher familism attitudes feel more obligation toward the family unit and see acting out as disgracing their family (Germán et al., 2008). In particular, studies have found familism to be protective against deviant behavior despite being exposed to deviant peers (Germán et al., 2008). Another study found that in addition to mediating the risk factor of deviant peer association, higher familism values resulted in lower associations with deviant peers (Roosa et al., 2011). While the literature is fairly consistent, it is also highly restricted to child participants requiring more research across a larger age span (Roosa et al., 2011).
Aims and hypothesis
The familism component has been implicated as a potential protective factor within these mental health outcomes, nevertheless the empirical evidence is somewhat conflicting. To solve this, the present systematic revision aims at assessing the relationship between familism and five mental health outcomes: depression, suicide, substance abuse, internalizing, and externalizing behaviors. The methodology selected to pursue this aim is a meta-analysis, which is a type of research conducted in order to piece together various published studies and pieces of literature in an attempt to find patterns and implications that may otherwise go overlooked. We hypothesize that there will be a large effect size in the relationship between familism and depression, suicide, substance abuse, internalizing, and externalizing behaviors in the Latino or Hispanic population within the United States. A large effect size would suggest that familism serves as a protective factor for the mental health outcomes of interest in this study.
Methods
PsycINFO database was systematically searched to identify the research articles used in this systematic review. The article selection process was conducted using the four-step process suggested by the PRISMA group (Moher et al., 2009) for systematic reviews. From the original search, 141 articles were identified (see Table 1). Researchers reviewed titles and abstracts of the articles to determine if the studies were conducted with Latino population. During the screening step, those articles that were (a) duplicated records, (b) expert opinion, (c) literature reviews, and (d) qualitative studies were excluded. The result was 54 potential articles to be examined further for eligibility and inclusion. The criteria used for review of articles in the two final steps are described in Table 1. The number of studies included in the analysis was of 39 published articles and dissertations.
Table 1.
Article selection process using PRISMA (2009) Steps.
| Step | Criteria | No. of studies that fulfilled criteria |
|---|---|---|
| Identification | 1. Terms included in search: | 141 |
| (a) familism and depression, (b) familism and suicide, (c) familism and internalizing, (d) familism and substance, and (e) familism and externalizing. |
||
| 2. Publication year range: 2005–2015. | ||
| Screening | Titles and abstracts contained participants from Latino or Hispanic populations, born in or outside the U.S. Duplicated records, expert opinions, literature review, and qualitative studies were removed. |
54 |
| Eligibility | Full-text articles were quantitative studies with a measure of attitudinal familism and one of the mental health outcome variables of interest. | 50 |
| Included | Full-text articles had: | 39 |
| 1. Defined sample size of Latino or Hispanic population. 2. Clearly indicated the instrument used to measure familism and the mental health outcome variable of interest; 3. Reported statistics of the direct relationship between familism and, at least, one of the other mental health outcome variables of interest; and 4. Based the analysis on original data collection, not replicated data. |
Researchers examined each study for the following: (a) population, (b) sample size, (c) sample characteristics, (d) measure of familism used, (e) mental health outcome analyzed, (f) measure of mental health outcome used, and (g) type of statistical analysis used. This information is presented in Table 2 for each of the 39 articles.
Table 2.
Studies included in meta-analysis.
| Study | Sample | Familism measure | Mental health outcome | Instrument used | Statistics for analysis | Cohen's d |
|---|---|---|---|---|---|---|
| Baham, 2009 | 119 Mexican-American Adolescents, Age range: 15–17 years | MACVS | Substance abuse | YRBS | Correlation coefficients | 0.1202 |
| Internalizing | RCMAS and CDI | 0.1605 | ||||
| Externalizing | BPI | 0.1403 | ||||
| Baumann et al., 2010 | 169 Latina adolescents, Mean age: 15.19 years Women only, 73% born in the U.S. | AFS | Suicide | YSR | M and SD | 0.2453 |
| Internalizing | YSR | Correlation coefficients | 0.7903 | |||
| Externalizing | YSR | 0.1909 | ||||
| Burrow-Sanchez et al., 2014 | 106 Latino adolescents, Mean age: 15.30 years, Male: 91.5% | AFS | Depression | BDI-II | Correlation coefficient | 0.6198 |
| Born in the U.S.: 63.2% | ||||||
| Campos et al., 2014 | 173 Latino, Mean age: 19.93 years, Born in the U.S.: 80% | AFS | Depression | CES-D | Means and standard deviationsa | 0.1202 Obligational |
| 0.0801 Supportive | ||||||
| 0.0600 Reference | ||||||
| Cavanaugh, 2015 | 133 Latino adolescents, Mean age: 12.88 years, Female: 51% | MACVS | Internalizing | YSR | Correlation coefficients for both variables with each form of familism | 0.2213 Obligational |
| 0.2828 Supportive | ||||||
| 0.2828 Reference | ||||||
| Externalizing | 0.4727 Obligational | |||||
| 0.4082 Supportive | ||||||
| 0.3242 Reference | ||||||
| Chavez-Korell et al., 2014 | 98 Latino older adults, Mean age: 71.04 years, Female: 66% | PHFS | Depression | PHQ-9 | Correlation coefficient | 0.4945 |
| Cupito et al., 2015 | 179 Latino adolescents, Mean age: 14 years, Female: 52% | AFS | Depression | MFQ | Correlation coefficients for males and females, separately | 0.6060 Females |
| 0.4727 Males | ||||||
| De Santis et al., 2012 | 46 Hispanic male with HIV infection, Mean age: 44.2 years, Male only | AFS | Depression | CES-D | Correlation coefficient | 0.2173 |
| Diaz, 2011 | 194 Mexican-American adolescents, Mean age: 12.88 years, Female: 52.6% | MACVS | Internalizing | RCMAS and CDI | Correlation coefficients | 0.4511 |
| Externalizing | BPI | 0.020 | ||||
| Substance abuse | YRBS | 0.2213 | ||||
| Fallah, 2014 | 170 Latino adolescents, Mean age: 14.06 years, Female: 55%, Born outside the U.S.: 67% | AFS | Depression | MFQ | Correlation coefficient | 0.4727 |
| Garza and Pettit, 2010 | 61 Mexican or Mexican-American, Mean age: 34.55 years, Women only, All born outside the U.S. | AFS | Depression | BDI-II | Correlation coefficients | 0.3450 |
| Suicide | INQ | 0.0400 | ||||
| Germán et al., 2008 | 598 Mexican-origin adolescents, Born in the U.S.: 79.1% | MACVS | Externalizing | CBCL TRF | Correlation coefficients | 0.1001 (Mother report) |
| 0.0200 (Father report) | ||||||
| 0.1403 (Teacher 1 report) | ||||||
| 0.2213 (Teacher 2 report) | ||||||
| Howarter, 2014 | 1386 Latino adolescents from project RED, Age range: 12–16 years, Female: 53.5% | Four-item scale | Depression | CES-D | Correlation coefficients | 0.1807 Females |
| Substance abuse | YRBS | for women and men separately, of depression, smoking and alcohol | ||||
| 0.3871 Males | ||||||
| 0.1605 Smoking females | ||||||
| 0.1403 Smoking males | ||||||
| 0.1001 Alcohol females | ||||||
| 0.1403 Alcohol males | ||||||
| Keeler et al., 2014 | 84 Mexican-American, Mean age: 30 years, Female: 48%, Born in the U.S.: 36% | Six-item scale | Depression | BDI-II | Correlation coefficients | 0.7473 |
| Kissinger et al., 2013 | 91 Latino migrant workers, Male only | AFS | Substance abuse | NSDUH tool, AUDIT | M and SD for each group | 0.4145 NSDUH |
| 0.1440 AUDIT | ||||||
| Kuhlberg et al., 2010 | 226 Latina adolescents, Mean age: 15.47 years, Women only | AFS | Suicide | Suicide Attempt | Mean and standard deviation Correlation coefficient | 0.2168 |
| Internalizing | YSR | 0.1403 | ||||
| Kuo et al., 2015 | 246 Latino adolescents, Mean age: 17.72 years, Female: 51% | MACVS | Depression | CED-S | Correlation coefficients for time 1 | 0.0801 (Mothers) |
| 0.1001 (Fathers) | ||||||
| Lac et al., 2011 | 1369 Latino adolescents, Mean age: 13.99 years, Female: 54.3% | Four-item scale | Substance abuse | One-item scale on marijuana use | Correlation for time 1 only | 0.1605 |
| Lin, 2007 | 596 Mexican-American adolescents, Mean age: 12.31 years, Female: 51% | MACVS | Substance abuse | YRBS | Correlation coefficient | 1.2904 |
| Losada et al., 2006 | 48 Adult caregivers, Mean age: 58.0 years, Female: 79.2%, Born in US: 54% | AFS | Depression | CES-D | Correlation coefficient | 0.3871 |
| Muñoz-Laboy et al., 2014 | 259 Formerly incarcerated Latino Men | AFS | Depression | BSI | Odds ratio | 0.0168 |
| Ocegueda, 2009 | 95 Mexican-American adolescents, Age range: 18–19 years, Female: 63.2% | Seven-item scale | Externalizing | Self-Report Delinquency Scale | Correlation | 1.0276 |
| Ornelas and Perreira, 2011 | 281 First-generation Latino youth parents, Mean age: 40 years, Female: 84% | Seven-item scale | Depression | PHQ-9 | Odds ratio of familism and each depression measurement | 0.0342 |
| CES-D | 0.1096 | |||||
| Peña et al., 2011 | 216 Adolescent Latinas reporting (suicide attempt vs. no suicide attempt), Mean age: 15.5 years, Women only | AFS | Suicide | Suicidal attempt | Mean and standard deviations of familism for each group (attempters vs. non-attempters) | 0.1219 |
| Reid-Quiñones, 2011 | 222 Latino emerging adults, Age range: 18–25 years, 61.7% Female, 72.5% born in the U.S. | MACVS | Substance abuse | CADS | Odds ratio for cigarette, marijuana and alcohol consumption | 0.000 Cigarette |
| DAST-20 | 0.0217 Alcohol | |||||
| 0.0109 Marijuana | ||||||
| Roosa et al., 2011 | 750 Mexican-origin adolescents, Mean age: 10.4 years, Female: 48.7% | MACVS | Externalizing | DISC | Correlation coefficient | 0.1403 |
| Soto et al., 2011 | 1616 Hispanic students, Age range: 13–15 years, Female: 54%, 88% born in the U.S. | Five-item scale | Substance abuse | YRBS | Odds ratio for marijuana, alcohol and cigarette use | 0.0476 Cigarette |
| 0.0527 Alcohol | ||||||
| 0.0724 Marijuana | ||||||
| Smokowski and Bacallao, 2007 | 323 Latino adolescents, Mean age: 15 years, Female: 51%, 97% born outside the U.S. | Six-item scale | Internalizing | YSR | Correlation coefficient | 0.7791 |
| Smokowski et al., 2007 | 100 Latino adolescents, Mean age: 15 years, Female: 54%, All born outside the U.S. | Seven-item scale | Internalizing Externalizing | YSR | Correlation coefficient | 0.6190 0.3367 |
| Smokowski et al., 2009 | 288, Latinos adolescents, Mean age: 15 years, Female: 54.5%, 67% born outside the U.S. | Seven-item scale | Internalizing | YSR | Correlation coefficient | 0.6755 |
| Smokowski et al., 2010 | 349 Latinos adolescents, Mean age, not reported, 66% born outside the U.S. | Seven-item scale | Internalizing | CBCL, YSR | Correlation coefficient | 0.5833 |
| Stein et al., 2015 | 173 Latino adolescents, Mean age: 14.08 years, Female: 53.8%, Mexican origin: 78% | AFS | Depression | MFQ | Correlation coefficient | 0.4082 |
| Telzer, 2012 | 385 Latino adolescents, Mean age: 15.01 years, Female: 51% | Twelve-item scale | Substance abuse | YRBS | Correlation coefficients | 0.3660 |
| Umaña-Taylor et al., 2011 | 207 Mexican-origin adolescents mothers, Mean age: 16.23 years, 64.6% born in the U.S. | MACVS | Depression | CES-D | Correlation between familism and depression | 0.1605 |
| Vargas et al., 2013 | 750 Mexican-American, Age range: 10–12 years, Female: 49%, 70% born in the U.S. | MACVS | Internalizing | DISC-IV | Correlation coefficients | 0.0200 |
| Externalizing | 0.0400 | |||||
| Venegas et al., 2012 | 160 Hispanics, Mean age: 19.9 years, Female: 50% | AFS | Substance abuse | DDQ | Mean and standard deviations | 0.0446 |
| Zapata et al., 2016 | 102 Latino adolescents, Mean age: 13.8 years, Male: 52.9%, Born in the U.S.: 51% | Seven-item scale | Substance abuse | Use of alcohol, cigarette and marijuana in the last 30 days | Correlation coefficients | 0.5608 Cigarette |
| 0.3450 Alcohol | ||||||
| 0.5833 Marijuana | ||||||
| Zayas et al., 2009 | 140 Latinas adolescents, Mean age: 15.21 years, Women only, 72.14% born in the U.S. | AFS | Suicide | Suicidal attempt | Means and standard deviations | 0.3106 |
| Zeiders et al., 2013 | 492 Latino adolescents, Age range: 13–23 years, Born in the US: 58% | MACVS | Depression | CES-D | Regression coefficients for each type of familism subscale | 0.1106 Obligational |
| 0.1711 Supportive | ||||||
| 0.1675 Reference |
AFS, Attitudinal Familism Scale; MACVS, Mexican-American Cultural Values Scale; CES-D, Center for Epidemiological Studies Depression Scale; PHQ-9, Patient Health Questionnaire-9; YSR, Youth Self-Report; CBCL, Child Behavior Check List; BDI-II, Beck Depression Inventory-II; INQ, Interpersonal Needs Questionnaire; DISC-IV, Diagnostic Interview Schedule for Children; YRBS, Youth Risk Behavior Survey; RCMAS, Revised Children's Manifest Anxiety Scale; CDI, Children Depression Inventory; DDQ, Daily Drinking Questionnaire; BPI, Behavior Problems Index; NSDUSH tool, National Survey on Drug Use and Health tool; AUDIT, Alcohol Use Disorders Identification Test; CADS, Core Alcohol and Drug Survey; DAST-20, Drug Use Screening Test-20; TRF, Teacher Report Form; MFQ, Mood and Feelings Questionnaire; BSI, Brief Symptoms Inventory for Depression.
With the provided data from the SEM we simulated data a 1000 times and estimated the correlations between the variables of interest. We used the mean and 95% CI correlations for the simulations.
Studies samples
All studies contained a sample of Latinos or Hispanics living in the United States. The studies required participants to self-identify as Hispanic or Latino. Participants were either foreign born or U.S. born. Those participants who were born in the U.S. had a Latin American background (e.g., one or both parents were born in Mexico, Central, or South America). As presented in Table 2, many of the studies contained samples of strictly adolescents. Only seven studies had adult participants (e.g., mean age higher than 18 years old). In terms of gender distribution, three studies were conducted with only a male population, and six studies with a female population exclusively. The rest of studies had both male and female Latinos in their samples. Most participants belonged to middle-, and high-school communities. Other participants were defined by one of the following different characteristics: adult caregivers, adolescent mothers, persons with HIV infections, formerly incarcerated Latinos, specific intervention-group participants (e.g., suicide attempter), or prevention/research group participants (e.g., RED, CAMINOS).
Measures
Familism
A variety of scales were used to determine familism scores for the participants in each study. The most widely used was the Attitudinal Familism Scale (AFS) generated by Lugo Steidel and Contreras (2003), which was used in 17 out of 39 studies. The following most used scale was the Mexican American Cultural Values Scale (MACVS; Knight et al., 2009), which was used in 11 out of the 39 studies. The rest of the studies used a scale from the University of California—San Francisco (Marin et al., 1987; Sabogal et al., 1987) or generated their own individual 3–7 item Likert scales.
Depression
The most used measure was the Center for Epidemiologic Studies Depression Scale, CES-D (Radloff, 1977; Santor and Coyne, 1997), utilized in eight studies. The Beck Depression Inventory II (Beck and Steer, 1991; Steer et al., 1998) was the second most used instrument for depression, present in three studies. Other studies used the Mood and Feelings Questionnaire by Angold et al. (1995), the Patient Health Quesitonnaire-9 (Kroenke and Spitzer, 2002), the Depression Brief Symptom Inventory, BSI (Derogatis, 1993), and the Child Depression Inventory (Kovacs, 1992).
Suicide
Suicidal attempts in each study were defined as any act of self-harm or intention of hurting or killing oneself. There was no scale to measure suicide; in each of the four suicidal studies, the participants were chosen for each condition based on medical records and/or reports by the school or family. Suicidal attempts, regardless of the level of lethality, were considered under the “suicide” condition while suicidal ideation was considered under internalizing.
Substance use
Substance use was self-reported by the participants. A variety of substances were encompassed in the studies including marijuana, alcohol, illicit drugs, and cigarettes. The most used instrument for self-reporting substance was the Youth Risk Behavior Survey (Centers for Disease Control and Prevention (CDC), 2000) in six of the studies. Other studies administered the Daily Drinking Questionnaire (Venegas et al., 2012), Alcohol Use Disorders Identification Test AUDIT (Cherpitel and Bazargan, 2003), the Core Alcohol and Drug Survey CADS (Presley et al., 1998), the Drug Abuse Screening Test DAST-20 (Skinner, 1982), and a self-generated report of substance abuse in the last 30 days.
Internalizing and externalizing symptoms
The most frequently used scale to measure internalizing and externalizing symptoms in participants was the Youth Self Report Scale YSRS (Baham, 2009), in six out of 39 studies. Also used was the Child Behavior Checklist (Achenbach, 1991), Revised Adolescent's Manifest Anxiety Scale RCAMS (Reynolds and Paget, 1981), the Diagnostic Interview Schedule for Children DISC-IV (Shaffer et al., 2000), Behavior Problems Index (adapted from the YSRS; Baham, 2009), Teacher's Report Form (Achenbach and Rescorla, 2001), and a Self-Report Delinquency Scale.
Data analysis
The studies included in this review contained various types of analyses, yielding to numerically different values. Studies presented one of the following data: Pearson's r correlation coefficient, odds ratios, hierarchical, standardized and unstandardized regression coefficients, or means and standard deviations for group comparisons (e.g., suicide attempter vs. non-attempter). In order to calculate a summarized effect of these studies, the data extracted from the articles were converted to standardized effect size measures. For each study, an effect size was calculated with Cohen's d (see Borenstein et al., 2009). The following formula was used for calculating Cohen's d of Pearson's r correlation coefficient:
| (1) |
For mean scores:
| (2) |
For odds ratios:
| (3) |
And, for regression coefficients:
| (4) |
Total effect sizes were calculated for each mental health outcome variable (e.g., depression, suicide, internalizing behaviors, substance abuse, externalizing behaviors). Results were weighted based on sample sizes (n):
| (5) |
The results presented in the following section are organized into five categories: depression, suicide, substance abuse, internalizing and externalizing behaviors.
Results
Effect sizes for Cohen's d were categorized as small, medium, or large, using the 0.2, 0.5, and 0.8 benchmarks, respectively (Borenstein et al., 2009). As Figure 1 shows, of the five dependent variables, internalizing behaviors (d = 0.33), suicide (d = 0.20), and depression (d = 0.21) showed a small effect with familism. The remaining two variables did not display a significant relationship.
Figure 1.
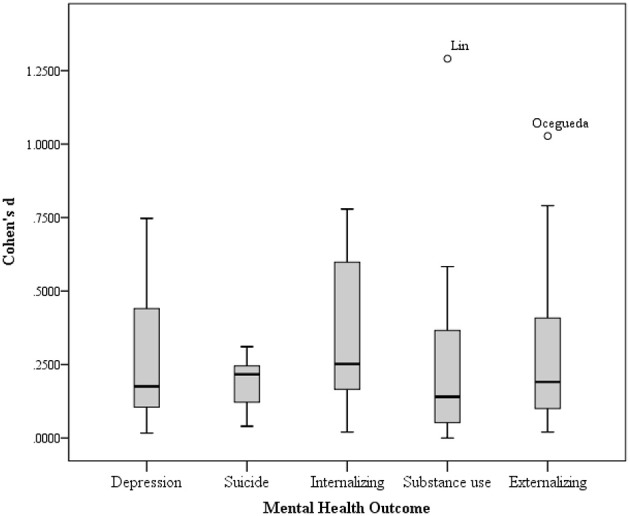
Effect sizes (Cohen's d) per mental health outcome variable.
As Table 2 indicates, individual studies showed stronger associations between familism and the mental health outcomes analyzed than the overall effect sizes reported above. The effect sizes for depression ranged from d = 0.02 to d = 0.75. Out of 24 studies on depression, 13 showed no significant effect (54.2%), 8 showed a small effect (33.3%), and 3 had moderate effect sizes (12.5%).
Substance use analysis included 21 studies, with effect sizes ranging from d = 0.00 to d = 1.29. Fourteen studies showed no significant effect sizes (66.7%); 4 studies had a small effect (19.0%) and 3 showed moderate effect sizes (14.3%).
The range of effect sizes for suicide was narrower, suggesting less variability within the relationship of familism and suicide (range of d [0.04, 0.31]). Out of 5 studies on suicide, 3 had small effect sizes and the rest no significant effects.
For the internalizing behaviors analysis, the effect sizes were distributed similarly. With a range of d = 0.02 to d = 0.78, there were 4 internalizing studies in each category: moderate, small and non-significant effect (33.3% each). With a very different distribution of effect sizes, the externalizing behaviors analysis showed a range of d = 0.02 to d = 1.03. Half of the studies showed no significant effects (7 out of 14 studies), 5 had small effect sizes, and only 2 reached moderate sizes for the effect.
Discussion
The results of this meta-analysis showed a small effect of familism on depression, suicide, and internalizing behaviors, and no effect for substance use and externalizing symptoms.
The small effects on depression, suicide and internalizing behaviors are coherent since depression and suicidal behavior are frequently associated with internalizing symptoms (depression, anxiety, mood disorders; Bridge et al., 2005). An important part of the etiology of mood disorders and other internalizing disorders, involve reduced or inadequate family support (Sheeber et al., 1997; Fristad et al., 2003). Therefore, it would make sense that attitudinal familism, which includes the feeling of support by one's family, would be related with lower rates of internalizing symptoms and consequently, lower suicide rates and depression symptoms. Family support reflects a positive family functioning which serves as a buffer effect for stressful life experiences in childhood, adolescence, and adulthood (Tubman and Windle, 1995). Since Latino adolescents are considered at a higher risk of suicide [Substance Abuse and Mental Health Services Administration (SAMHSA), 2015], the summary effect found in the present study is suggesting that many adolescents refrain from turning to extreme acts such as suicide, by reaching out to family members when support is needed (Dunham, 2004). With low levels of familism values it is likely that an adolescent struggling with stressful life events or internalizing symptoms would be hesitant to turn to parents and family members for support, subsequently increasing the risk and result of depression and suicidal behaviors. Nevertheless, the effect sizes for depression, suicide and internalizing behaviors should be interpreted with caution. The effect sizes for the three variables were small. That is, the results are suggesting that attitudinal familism has a real effect on these variables, but it can only account for a small proportion of variance for depression, suicide and internalizing symptoms. Potential reasons for the small effect are address at the end of this section.
The results of the present study showed no significant effect sizes of familism on substance use and externalizing behaviors. Although the magnitude of the effects is indicating that family factors alone play only a minimal role in causing or predicting externalizing symptoms and substance abuse, one's perception of familial support is critical in the causes of substance use and externalizing psychopathologies (Beitchman et al., 2005). Then, how can the non-significant effect size be explained in Latino population? Maybe, attitudinal familism as a cultural value is not as important as behavioral familism. That is, manifest behaviors of support and good communication. Kam and Yang (2014) found that attitudinal familism was not significantly related to personal substance-abuse norms in adolescents Latinos, but targeted mother-child communication was. This finding could be particularly relevant for Latino adolescents born in the U.S., whose levels of acculturation may be higher and cultural familism lower in comparison to those born and raised outside the U.S. (see Cervantes, 2002). Recent findings support that both U.S.-born and foreign-born Latinos experience acculturation stress, even when they are completely bilingual and bicultural (Cervantes et al., 2013). Acculturation stress has been found positively associated with externalizing problems or conduct problems in both populations. Such relationship is moderated by parental monitoring (i.e., behavioral familism), which provides a protective effect against externalizing problems (Hurwich-Reiss and Gudiño, 2015).
The small and non-significant effects found in this meta-analysis could be the result of limitations from the studies included in this meta-analysis, as well as from our methods. Limitations on measurement variability and sample variability should be noted and improved upon in future research.
The first concern arises from the measurements used in the studies included in the meta-analysis. As reported on Table 2, studies measured familism with the MACVS, the Familism Scale of Sabogal, and the Familism Scale of Lugo. Other studies just built their own Likert scale for familism, using 4–7 items. Not all of the studies differentiated the subscales scores of familism (supportive, obligatory, and referent familism). And those studies which built their own instruments did not mention a particular type of attitudinal familism, addressing the variable in general terms. The differences in the measurement raises concern because there is evidence that supportive and referent familism is a protective factor for mental health outcomes, while obligatory familism is not (Zeiders et al., 2013). Therefore, those studies measuring the subtypes of familism that averaged across the scale could have larger effect sizes if they were analyzed separately. And, the rest of studies that did not differentiate between the subtypes may have somewhat ambiguous conclusions.
In terms of sample variability, it is important to address differences within Latino population. Social psychology has explained in a simple and easy way how humans use heuristics for categorizing persons in groups and assigning equal values and characteristics to them. A phenomenon called the out-group homogeneity effect, which simplifies our thinking processes (Quattrone and Jones, 1980). This effect is relevant to interpret the meta-analysis because the studies included had relevant within-group differences in terms of how their samples were conceptualized and characterized. From those studies that reported specific information of their sample, most had Latino participants who were born in the U.S. (ranging from 36 to 100% participants born in the U.S., see Table 2). Few studies just requested participants to self-identify as Latino or Hispanic. No information of country of origin or numbers of years in the U.S. was reported. Although, all participants had a Latin American background, they all cannot be considered equal or homogenous. That is, the out-group homogeneity effect should be avoided for two reasons. In the first place, the Hispanic paradox evidences differences between Hispanic immigrants and U.S. born persons of Hispanic origin, in terms of health (Blanco et al., 2013), which suggests a cultural protective factor that is diminished by acculturation (Calzada et al., 2012). In addition, when analyzing results from Substance Abuse and Mental Health Services Administration (SAMHSA, 2015) and Alegría et al. (2008), differences between adults and adolescents Latinos arise, with adolescents being at greater risk of mental health disorders. The difference between age groups could be explained using the “dual frame of reference” by Suárez-Orozco and Suárez-Orozco (1995), which explains how Latino immigrants use their families back home as a reference when reflecting about their lives in the U.S. while U.S. born Latinos could be comparing themselves to American peers. Since social and economic conditions of the families back home are often worse, the U.S. immigrants are less likely to experience distress, in comparison to U.S. born Latinos (U.S. Department of Health and Human Services, 2001). And in second place, and equally important, Latinos are usually defined as individuals who speak Spanish and have a Latin American background; and in consequence persons from more than 15 different countries are grouped into one sole category (using again the out-group homogeneity effect). Within-group variability in Latino population is particularly important when studying immigrants to the U.S. The U.S. Department of Health and Human Services (2001) gives reasons to care about the differences within Latino population. The reasons that motivate a Mexican origin person to migrate to the U.S. is different to those that motivate a Central American or a South American. According to the report, Mexicans are pushed by the economic hardship, while Central American were mostly driven by the civil wars and violent conflicts. South Americans who have better economic conditions and less violence, are probably motivated to migrate for other reasons. This difference within group should be addressed in future studies, because depression, alcoholism, and PTSD may be at higher risk in Central American immigrants than in other immigrants of the region.
Therefore, studies including all U.S.-born and foreign-born Latinos in one group are not attending important within group differences. Berdahl and Torres Stone (2009) conducted a study that enlightens such differences. They compared Mexicans, Cubans, and Puerto Ricans to non-Latino whites and found that Mexicans were less likely to use mental health services, compared to all previous groups. The researchers discuss their findings by addressing the diverse sociopolitical relationships of these countries with the U.S.
Future meta-analysis on familism and mental health outcomes should take into account the limitations in the present study. First, this study was limited to attitudinal familism. Therefore, the current results cannot be generalized to all types of familism. We consider that separate analysis should be conducted for each type of familism, including behavioral or manifest acts of familism. Separate analysis would help understand the differential effect of each type of familism on each type of mental health outcomes in Latinos. Second, the measure of each construct widely varied between studies. To protect against potential method variability affecting the results, future meta-analysis should consider including studies with similar measurement scales. Third, the study did not limit the sample by age, country of origin, time in the U.S. or socioeconomic status. With a larger body of publications on this topic a more stringent inclusion criteria should be used. To reduce sample variability, future researchers should to opt for a specific age range, geographical area (e.g., Mexican, Central American, Caribbean, or South American origin) and time in the U.S. The concerns about sample variability have been exposed above.
The interest of familism in Hispanic or Latino cultures is a relatively new but quickly growing field of interest. Further research and evidence proving the effects of familism on mental health could give a greater grasp on etiology and treatment options for psychopathologies. The aspects discussed in this section in terms of sample characteristics and measurement should be taken into consideration for future studies.
Author contributions
EV and CP conducted the literature research and conducted the statistical analysis. CP wrote most of the Introduction and EV wrote most of the Methods, Results and Discussion sections. MG helped with data analysis and interpretation. MS and DJ supervised the study and gave feedback, made corrections and contributed with important ideas for the introduction and discussion.
Funding
Support from NIA Developmental Grant R21TW009665 and the University of Kansas Open Access Author Fund.
Conflict of interest statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- Achenbach T. M. (1991). Manual for the Child Behavior Checklist/4–18 and 1991 Profile. University of Vermont, Department of Psychology, Burlington. [Google Scholar]
- Achenbach T. M., Rescorla L. A. (2001). Manual for the ASEBA School-Age Forms & Profiles. University of Vermont, Research Center for Children, Youth & Families, Burlington. [Google Scholar]
- Alegría M., Canino G., Shrout P. E., Woo M., Duan N., Vila D., et al. (2008). Prevalence of mental illness in immigrant and non-immigrant U.S. Latino groups. Am. J. Psychiatry 165, 359–369. 10.1176/appi.ajp.2007.07040704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association (APA) (2014). Mental Health Disparities: Hispanics/Latinos. APA Fact Sheet: Division of Diversity and Health Equity; Available online at: www.psychiatry.org [Google Scholar]
- Angold A., Costello E., Messer S., Pickles A., Winder F., Silver D. (1995). Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. Int. J. Methods Psychiatr. Res. 5, 237–249. [Google Scholar]
- Baham M. E. (2009). Sibling Relationship Quality and Psychosocial Outcomes in European-and Mexican-American Adolescents: The Moderating Role of Familism. Arizona State University. Retrieved from ProCite.
- Baumann A. A., Kuhlberg J. A., Zayas L. H. (2010). Familism, mother-daughter mutuality, and suicide attempts of adolescent Latinas. J. Fam. Psychol. 24, 616–624. 10.1037/a0020584 [DOI] [PubMed] [Google Scholar]
- Beck A. T., Steer R. (1991). Manual for the Beck Scale for Suicidal Ideation. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Beitchman J. H., Adlaf E. M., Atkinson L., Douglas L., Beitchman J. H., Adlaf E. M., et al. (2005). Psychiatric and substance use disorders in late adolescence: the role of risk and perceived social support. Am. J. Addict. 14, 124–138. 10.1080/10550490590924755 [DOI] [PubMed] [Google Scholar]
- Berdahl T. A., Torres Stone R. A. (2009). Examining Latino differences in mental healthcare use: the roles of acculturation and attitude towards healthcare. Community Ment. Health J. 45, 393–403. 10.1007/s10597-009-9231-6 [DOI] [PubMed] [Google Scholar]
- Blanco C., Morcillo C., Alegría M., Dedios M. C., Fernández -Navarro P., Regincos R., et al. (2013). Acculturation and drug use disorders among Hispanics in the U.S. J. Psychiatr. Res. 47, 226–232. 10.1016/j.jpsychires.2012.09.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borenstein M., Hedges L. V., Higgins J. P. T., Rothstein H. R. (2009). Introduction to Meta-Analysis. West Sussex: John Wiley & Sons. [Google Scholar]
- Bridge J. A., Barbe R. P., Birmaher B., Kolko D. J., Brent D. A. (2005). Emergent suicidality in a clinical psychotherapy trial for adolescent depression. Am. J. Psychiatry 162, 2173–2175. 10.1176/appi.ajp.162.11.2173 [DOI] [PubMed] [Google Scholar]
- Brown E. R., Ojeda V. D., Wyn R., Levan R. (2000). Racial and Ethnic Disparities in Access to Health Insurance and Health Care. Los Angeles, CA: UCLA Center for Health Policy Research and The Henry J. Kaiser Family Foundation. [Google Scholar]
- Burrow-Sanchez J. J., Ortiz-Jensen C., Corrales C., Meyers K. (2014). Acculturation in a pretreatment simple of Latino adolescents: a confirmatory factor analytic study. Hisp. J. Behav. Sci. 37, 103–117. 10.1177/0739986314560148 [DOI] [Google Scholar]
- Calzada E. J., Tamis-LeMonda C. S., Yoshikawa H. (2012). Familismo in mexican and dominican families from low-income, Urban communities. J. Fam. Issues 34, 1696–1724. 10.1177/0192513X12460218 [DOI] [Google Scholar]
- Campos B., Ullman J. B., Aguilera A., Dunkel C. (2014). Familism and psychological health: the intervening role of closeness and social support. Cultur. Divers. Ethnic Minor. Psychol. 20, 191–201. 10.1037/a0034094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavanaugh A. M. (2015). Examining Linkages among Sources of Racial-Ethnic Discrimination and Latino Adolescents' Psychological and Academic Outcomes: Are Culturally-Relevant Factors Protective? University of North Carolina, Greensboro, NC. [Google Scholar]
- Centers for Disease Control Prevention (CDC) (2000). Youth Risk Behavior Survey. Available online at: www.cdc.gov/yrbss
- Cervantes C. A. (2002). Explanatory emotion talk in Mexican immigrant and Mexican American families. Latino J. Behav. Sci. 24, 138–164. 10.1177/0739986302024002003 [DOI] [Google Scholar]
- Cervantes R. C., Padilla A. M., Napper L. E., Goldbach J. T. (2013). Acculturation-related stress and mental health outcomes among three generations of Hispanic adolescents. Hisp. J. Behav. Sci. 35, 451–468. 10.1177/0739986313500924 [DOI] [Google Scholar]
- Chavez-Korell S., Benson-Florez G., Delgado Rendon A., Farias R. (2014). Examining the relationships between physical functioning, ethnic identity, acculturation, familismo, and depressive symptoms for Latino older adults. Couns. Psychol. 42, 255–277. 10.1177/0011000013477906 [DOI] [Google Scholar]
- Cherpitel C. J., Bazargan S. (2003). Screening for alcohol problems: comparison of theaudit, RAPS4 and RAPS4-QF among African American and Hispanic patients in an inner city emergency department. Drug Alcohol Depend. 71, 275–280. 10.1016/S0376-8716(03)00140-6 [DOI] [PubMed] [Google Scholar]
- Cupito A. M., Stein G. L., Gonzalez L. M. (2015). Familial cultural values, depressive symptoms, school belonging and grades in Latino adolescents: does gender matter? J. Child Fam. Stud. 24, 1638–1649. 10.1007/s10826-014-9967-7 [DOI] [Google Scholar]
- Davila Y. R., Reifsnider E., Pecina I. (2011). Familismo: influence on Hispanic health behaviors. Appl. Nurs. Res. 24, e67–e72. 10.1016/j.apnr.2009.12.003 [DOI] [PubMed] [Google Scholar]
- Derogatis L. R. (1993). BSI Brief Symptom Inventory. Administration, Scoring, and Procedures Manual, 4th Edn. Minneapolis, MN: National Computer Systems. [Google Scholar]
- De Santis J. P., Gonzalez-Guarda R. M., Vasquez E. P. (2012). Psychosocial and cultural correlates of depression among Hispanic men with HIV infection: a pilot study: depression and HIV. J. Psychiatr. Ment. Health Nurs. 19, 860–869. 10.1111/j.1365-2850.2011.01865.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diaz P. (2011). Perceived Group Discrimination and Problem Behavior: The Moderating Role of Traditional Cultural Values and Familial Relationships in Mexican American Adolescents. Arizona State University. Available online at: http://repository.asu.edu/attachments/56914/content/Diaz_asu_0010E_10815.pdf
- Dunham K. (2004). Young adults' support strategies when peers disclose suicidal intent. Suicide Life-Threat. Behav. 34, 56–65. 10.1521/suli.34.1.56.27773 [DOI] [PubMed] [Google Scholar]
- Elo I. T., Turra C. M., Kestenbaum B., Ferguson B. R. (2004). Mortality among elderly Hispanics in the United States: past evidence and new results. Demography 41, 109–128. 10.1353/dem.2004.0001 [DOI] [PubMed] [Google Scholar]
- Fallah N. (2014). Familial, Academic, and Interpersonal Predictors of Attributional Style in Latino Youth. University of North Carolina, Greensboro, NC. [Google Scholar]
- Fristad M. A., Gavazzi S. M., Mackinaw-Koons B. (2003). Family psychoeducation. Biol. Psychiatry 53, 1000–1008. 10.1016/S0006-3223(03)00186-0 [DOI] [PubMed] [Google Scholar]
- Garza M. J., Pettit J. W. (2010). Perceived burdensomeness, familism, and suicidal ideation among Mexican women: enhancing understanding of risk and protective factors. Suicide Life-Threat. Behav. 40, 561–573. 10.1521/suli.2010.40.6.561 [DOI] [PubMed] [Google Scholar]
- Germán M., Gonzales N. A., Dumka L. (2008). Familism values as a protective factor for mexican-origin adolescents exposed to deviant peers. J. Early Adolesc. 29, 16–42. 10.1177/0272431608324475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez D. (1992, November 15). What's the problem with ‘Hispanic’? Just ask a ‘Latino’. The New York Times. Available online at: http://www.nytimes.com.
- Howarter A. D. (2014). Socioeconomic Status, Acculturation, Family Characteristics, and Health Behaviors: Testing the Reserve Capacity Model with Hispanic Adolescents. University of Missouri, Kansas City, MO. [Google Scholar]
- Hurwich-Reiss E., Gudiño O. G. (2015). Acculturation stress and conduct problems among Latino adolescents: the impact of family factors. J. Latina/o Psychol. 10.1037/lat0000052 [DOI] [Google Scholar]
- Kam J. A., Yang S. (2014). Explicating how parent-child communication increases Latino and European American early adolescents' intentions to intervene in a friend's substance abuse. Prevent. Sci. 15, 536–546. 10.1007/s11121-013-0404-8 [DOI] [PubMed] [Google Scholar]
- Keeler A. R., Sieger J. T., Alvaro E. M. (2014). Depression and help seeking among Mexican-Americans: the mediating role of familism. J. Immigr. Minor. Health 16, 1225–1231. 10.1007/s10903-013-9824-6 [DOI] [PubMed] [Google Scholar]
- Kissinger P., Althoff M., Burton N., Schmidt N., Hembling J., Salinas O., et al. (2013). Prevalence, patterns and predictors of substance use among Latino migrant men in a new receiving community. Drug Alcohol Depend. 133, 814–824. 10.1016/j.drugalcdep.2013.08.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knight G. P., Gonzales N. A., Saenz D. S., Bonds D. D., German M., Deardorff J., et al. (2009). The Mexican American cultural values scale for adolescents and adults. J. Early Adolesc. 30, 444–481. 10.1177/0272431609338178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacs M. (1992). Children's Depression Inventory. New York, NY: Multi-Health Systems Inc. [Google Scholar]
- Kroenke K., Spitzer R. L. (2002). The PHQ-9: a new depression and diagnostic severity measure. Psychiatr. Ann. 32, 509–521. 10.3928/0048-5713-20020901-06 [DOI] [Google Scholar]
- Kuhlberg J. A., Peña J. B., Zayas L. H. (2010). Familism, parent-adolescent conflict, self-esteem, internalizing behaviors and suicide attempts among adolescent Latinas. Child Psychiatry Hum. Dev. 41, 425–440. 10.1007/s10578-010-0179-0 [DOI] [PubMed] [Google Scholar]
- Kuo S. I., Updegraff K. A., Zeiders K. H., McHale S. M., Umana-Taylor A. J., Rodriguez De Jesus S. A. (2015). Mexican American adolescents' sleep patterns: contextual correlates and implications for health and adjustment in young adulthood. J. Youth Adolesc. 44, 346–361. 10.1007/s10964-014-0156-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lac A., Unger J. B., Basáñez T., Ritt-Olson A., Soto D. W., Baezconde-Garbanati L. (2011). Marijuana use among Latino adolescents: gender differences in protective familial factors. Subst. Use Misuse 46, 644–655. 10.3109/10826084.2010.528121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin C. V. (2007). Latino Adolescent Substance Use: Importance of Cultural Values and Peer Influence. Arizona State University. Available online at: http://gradworks.umi.com/32/58/3258118.html
- Losada A., Robinson Shurgot G., Knight B. G., Márquez M., Montorio I., Izal M., et al. (2006). Cross-cultural study comparing the association of familism with burden and depressive symptoms in two samples of Hispanic dementia caregivers. Aging Ment. Health 10, 69–76. 10.1080/13607860500307647 [DOI] [PubMed] [Google Scholar]
- Lugo Steidel A., Contreras J. M. (2003). A new familism scale for use with Latino populations. Hisp. J. Behav. Sci. 25, 312–330. 10.1177/0739986303256912 [DOI] [Google Scholar]
- Marin G., Sabogal F., Marin B. V., Otero-Sabogal R., Perez-Stable E. J. (1987). Development of a short acculturation scale for Hispanics. Hisp. J. Behav. Sci. 9, 183–205. 10.1177/07399863870092005 [DOI] [Google Scholar]
- Marsiglia F. F., Parsai M., Kulis S. (2009). Effects of familism and family cohesion on problem behaviors among adolescents in Mexican immigrant families in the Southwest U.S. J. Ethn. Cult. Divers. Soc. Work 18, 203–220. 10.1080/15313200903070965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D. G., The PRISMA Group (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. PLoS Med. 6:e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muñoz-Laboy M., Worthington N., Perry A., Guilamo-Ramos V., Cabassa L., Lee J., et al. (2014). Socio-environmental risks for untreated depression among formerly incarcerated Latino men. J. Immigr. Minor. Health 16, 1183–1192. 10.1007/s10903-013-9814-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Alliance for Mental Illnesses (NAMI) (2002). Latino Community Mental Health Fact Sheet. NAMI: Multicultural Action Center; Available onlie at: www.nami.org [Google Scholar]
- Ocegueda I. K. (2009). Predictors of Adolescent Delinquency in Mexican-Americans. Los Angeles, CA: Alliant International University. [Google Scholar]
- Ornelas I. J., Perreira K. M. (2011). The role of migration in the development of depressive symptoms among Latino immigrant parents in the USA. Soc. Sci. Med. 73, 1169–1177. 10.1016/j.socscimed.2011.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsai M., Voisine S., Marsiglia F. F., Kulis S., Nieri T. (2009). The protective and risk effects of parents and peers on substance use, attitudes, and behaviors of Mexican and Mexican American female and male adolescents. Youth Soc. 40, 353–376. 10.1177/0044118X08318117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peña J. B., Kuhlberg J. A., Zayas L. H., Baumann A. A., Gulbas L., Hausmann-Stabile C., et al. (2011). Familism, family environment, and suicide attempts among Latina youth. Suicide Life-Threat. Behav. 41, 330–341. 10.1111/j.1943-278X.2011.00032.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Presley C. A., Meilman P. W., Leichliter J. S. (1998). Core Alcohol and Drug Survey User's Manual, 6th Edn. Carbondale, IL: Southern Illinois University. [Google Scholar]
- Quattrone G. A., Jones E. E. (1980). The perception of variability within in-groups and out-groups: implications for the law of small numbers. J. Pers. Soc. Psychol. 38, 141–152. 10.1037/0022-3514.38.1.141 [DOI] [Google Scholar]
- Radloff L. S. (1977). The CES-D Scale: a self-report depression scale for research in the general population. Appl. Psychol. Meas. 1, 385–401. 10.1177/014662167700100306 [DOI] [Google Scholar]
- Reid-Quiñones K. (2011). Parent-Child Communication about Substance Use: Experiences of Latino Emerging Adults. Virginia Commonwealth University Richmond, Virginia. Available online at: https://dizzyg.library.vcu.edu/handle/10156/3539
- Reynolds C. R., Paget K. D. (1981). Factor analysis of the Revised Children's Manifest Anxiety Scale for blacks, whites, males, and females with a national normative sample. J. Consult. Clin. Psychol. 49, 352–359. 10.1037/0022-006X.49.3.352 [DOI] [PubMed] [Google Scholar]
- Roosa M. W., Zeiders K. H., Knight G. P., Gonzales N. A., Tein J.-Y., Saenz D., et al. (2011). A test of the social development model during the transition to junior high with Mexican American adolescents. Dev. Psychol. 47, 527–537. 10.1037/a0021269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabogal F., Marin G., Otero-Sabogal R., Marin B. V., Perez-Stable E. J. (1987). Hispanic familism and acculturation: what changes and what doesn't? Hisp. J. Behav. Sci. 9, 397–412. 10.1177/07399863870094003 [DOI] [Google Scholar]
- Santor D. A., Coyne J. C. (1997). Shortening the CES-D to improve its ability to detect cases of depression. Psychol. Assess. 9, 233–243. 10.1037/1040-3590.9.3.233 [DOI] [Google Scholar]
- Shaffer D., Fisher P., Lucas C. P., Dulcan M. K., Schwab-Stone M. E. (2000). NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV) description, differences from previous versions, and reliability of some common diagnoses. J. Am. Acad. Child Adolesc. Psychiatry 39, 28–38. 10.1097/00004583-200001000-00014 [DOI] [PubMed] [Google Scholar]
- Sheeber L., Hops H., Alpert A., Davis B., Andrews J. (1997). Family support and conflict: prospective relations to adolescent depression. J. Abnorm. Child Psychol. 25, 333–344. 10.1023/A:1025768504415 [DOI] [PubMed] [Google Scholar]
- Skinner H. (1982). The drug abuse screening test. Addict. Behav. 7, 363–371. 10.1016/0306-4603(82)90005-3 [DOI] [PubMed] [Google Scholar]
- Smokowski P. R., Bacallao M., Buchanan R. L. (2009). Interpersonal mediators linking acculturation stressors to subsequent internalizing symptoms and self-esteem in Latino adolescents. J. Community Psychol. 37, 1024–1045. 10.1002/jcop.20346 [DOI] [Google Scholar]
- Smokowski P. R., Bacallao M. L. (2007). Acculturation, internalizing mental health symptoms, and self-esteem: cultural experiences of Latino adolescents in North Carolina. Child Psychiatry Hum. Dev. 37, 273–292. 10.1007/s10578-006-0035-4 [DOI] [PubMed] [Google Scholar]
- Smokowski P. R., Chapman M. V., Bacallao M. L. (2007). Acculturation risk and protective factors and mental health symptoms in immigrant Latino adolescents. J. Hum. Behav. Soc. Environ. 16, 33–55. 10.1300/10911350802107710 [DOI] [Google Scholar]
- Smokowski P. R., Rose R. A., Bacallao M. (2010). Influence of risk factors and cultural assets on Latino adolescents' trajectories of self-esteem and internalizing symptoms. Child Psychiatry Hum. Dev. 41, 133–155. 10.1007/s10578-009-0157-6 [DOI] [PubMed] [Google Scholar]
- Soto C., Unger J. B., Ritt-Olson A., Soto D. W., Black D. S., Baezconde-Garbanati L. (2011). Cultural values associated with substance use among Hispanic adolescents in southern California. Subst. Use Misuse 46, 1223–1233. 10.3109/10826084.2011.567366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steer R. A., Kumar G., Ranieri W. F., Beck A. T. (1998). Use of the beck depression inventory-II with adolescent psychiatric outpatients. J. Psychopathol. Behav. Assess. 20, 127–137. 10.1023/A:1023091529735 [DOI] [Google Scholar]
- Stein G. L., Gonzalez L. M., Cupito A. M., Kiang L., Supple A. J. (2015). The protective role of familism in the lives of Latino adolescents. J. Fam. Issues 36, 1255–1273. 10.1177/0192513X13502480 [DOI] [Google Scholar]
- Suárez-Orozco C., Suárez-Orozco M. (1995). Transformations: Immigration, Family Life, and Achievement Motivation among Latino Adolescents. Stanford, CA: Stanford University Press. [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) (2015). Behavioral Health Barometer: United States, 2014. HHS Publication No. SMA–15–4895. Rockville, MD: Substance Abuse and Mental Health Services Administration.
- Telzer E. H. (2012). Neurobehavioral Correlates of Familism and Adolescent Risk Taking. University of California, Los Angeles, CA. [Google Scholar]
- Tubman J. G., Windle M. (1995). Continuity of difficult temperament in adolescence: relations with depression, life events, family support, and substance use across a one year period. J. Youth Adolesc. 24, 133–153. 10.1007/BF01537146 [DOI] [Google Scholar]
- Umaña-Taylor A. J., Updegraff K. A., Gonzales-Backen M. A. (2011). Mexican-origin adolescent mothers' stressors and psychosocial functioning: examining ethnic identity affirmation and familism as moderators. J. Youth Adolesc. 40, 140–157. 10.1007/s10964-010-9511-z [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau (2011). The Hispanic Population: 2010. U.S. Department of Commerce: Economics and Statistics Administration. [Google Scholar]
- U.S. Census Bureau (2013). Poverty Rates for Selected Detailed Race and Hispanic Groups by State and Place: 2007–2011. U.S. Department of Commerce: Economics and Statistics Administration. [Google Scholar]
- U.S. Department of Health and Human Services (2001). Mental Health: Culture, Race, and Ethnicity—A Supplement to Mental Health: A Report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services. [Google Scholar]
- Vargas D. A., Roosa M. W., Knight G. P., O'Donnell M. (2013). Family and cultural processes linking family instability to Mexican American adolescent adjustment. J. Fam. Psychol. 27, 387–397. 10.1037/a0032863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venegas J., Cooper T. V., Naylor N., Hanson B. S., Blow J. A. (2012). Potential cultural predictors of heavy episodic drinking in Hispanic college students: heavy episodic drinking. Am. J. Addict. 21, 145–149. 10.1111/j.1521-0391.2011.00206.x [DOI] [PubMed] [Google Scholar]
- Zapata M. I., Grzywacz J. G., Cervantes R. C., Merten M. J. (2016). Stress and alcohol, cigarette, and marijuana use among Latino adolescents in families with undocumented immigrants. J. Child Fam. Stud. 25, 475–487. 10.1007/s10826-015-0249-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zayas L. H., Bright C. L., Álvarez-Sánchez T., Cabassa L. J. (2009). Acculturation, familism and mother–daughter relations among suicidal and non-suicidal adolescent Latinas. J. Prim. Prev. 30, 351–369. 10.1007/s10935-009-0181-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeiders K. H., Updegraff K. A., Umaña-Taylor A. J., Wheeler L. A., Perez-Brena N. J., Rodríguez S. A. (2013). Mexican-origin youths' trajectories of depressive symptoms: the role of familism values. J. Adolesc. Health 53, 648–654. 10.1016/j.jadohealth.2013.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]


