Abstract
Background:
Traffic and residential heating are the main sources of particulate matter (PM) in Northern Europe. Wood is widely used for residential heating and vehicle numbers are increasing. Besides traffic exhaust, studded tires produce road dust that is the main source of traffic-related PM10. Several studies have associated total PM mass with health symptoms; however there has been little research on the effects of PM from specific sources.
Objective:
To study the health effects resulting from traffic and local heating PM.
Methods:
Data on respiratory and cardiac diseases were collected within the framework of RHINE III (2011/2012) in Tartu, Estonia. Respondents’ geocoded home addresses were mapped in ArcGIS and linked with local heating-related PM2.5, traffic-related PM10 and total PM2.5 concentrations. Association between self-reported health and PM was assessed using multiple logistic regression analysis.
Results:
The annual mean modelled exposure for local heating PM2.5 was 2.3 μg/m3, for traffic PM10 3.3 μg/m3 and for all sources PM2.5 5.6 μg/m3. We found relationship between traffic induced PM10 as well as all sources induced PM2.5 with cardiac disease, OR=1.45 (95% CI 1.06−1.93) and 1.42 (95% CI 1.02−1.95), respectively. However, we did not find any significant association between residential heating induced particles and self-reported health symptoms. People with longer and better confirmed exposure period were also significantly associated with traffic induced PM10, all sources induced PM2.5 and cardiac diseases.
Conclusion:
Traffic-related PM10 and all sources induced PM2.5 associated with cardiac disease; whereas residential heating induced particles did not.
Keywords: Air pollution, Cardiac disease, Particulate matter, Residential heating, Respiratory disease, RHINE, Traffic
1. INTRODUCTION
There are two main sources of particulate matter (PM10) in Northern Europe cities: residential heating and traffic. Residential heating comprises a variety of small-scale wood or coal combustion appliances, such as wood stoves, open fireplaces, masonry heaters and central heating boilers fuelled by wood, coal and wood chips or pellets. Wood and biomass combustion particles may play a dominant role in peoples’ exposure to PM [1, 2]. Biomass burning contributes up to 40% of total particle mass in urban background regions where local heating is common [3-6]. Orru et al. (2010) found that combustion from biomass accounts for up to 40% of fine particles (PM2.5) in city of Tartu [6] and concentrations of fine particles PM2.5 and organic carbon in PM10 are usually highest in winter, when residential heating is used continuously [3, 5].
Due to insufficient air flow and relatively low combustion temperatures, several pollutants are produced from log burning in residential wood stoves [7]. According to the combustion conditions in such appliances (low/high temperatures, complete/incomplete combustion), different particles with different chemical compositions and of different sizes are formed: organic carbon particles, soot, inorganic ash particles and polycyclic aromatic hydrocarbons (PAHs) [8, 9].
In addition to traffic exhaust, the use of studded tyres in Northern Europe during winter results in higher rates of road abrasion and tyre and brake wear, which increases dust emissions [10]. Orru et al. (2010) have shown that at urban background site in Tartu, traffic and crustal dust are the second most important source of PM2.5 (up to 13% of total fine particle mass) [6]. There have been no traffic exhaust particle composition studies done in Tartu; however, as in most other cities we expect vehicle emissions to consist mainly of exhaust particles (PMexhaust), nitrogen oxides and black smoke [11]. Since the 1990s, levels of exhaust particles and PM10 have changed in Tartu; while in Estonia the mean age of cars has reduced and newer vehicles emit relatively less pollutants per unit, the total number of vehicles has increased 3-6 times depending on the Tartu region [12].
Both short- and long-term exposure to fine as well as coarse particles (PM2.5-10) are associated with cardiovascular and respiratory morbidity or mortality [13-18]. Associations to health symptoms have been found when analysing one region [19] or different regions within studies [20, 21], mass concentration and particle size are probably not the only factors in PM-related health effects. Some epidemiological or experimental studies have also tried to find evidence regarding what particle components are most harmful to human health [21-23].
There are several studies that linked traffic pollution and health [11, 14, 24], but the number of studies where the potential health effects of wood smoke exposure were investigated is relatively small. In addition, for studies where the effects of particles from different sources were compared, the focus was mainly on short-term health effects [25-28]. Some recent reviewers have concluded that in developed countries the adverse health effects associated with wood smoke exposure do not seem to be weaker than that of ambient particles from other sources [29, 30]. Despite great uncertainty regarding the health risks of primary anthropogenic fine particles from different sources, some experts consider traffic induced particles to be more toxic than most others [31].
Aim of the current study was to investigate potential effects of traffic and residential heating induced particles on respiratory and cardiac health.
2. METHODS
2.1. Study Site and Data
The study site Tartu is the second largest city in Estonia with a population 97,000. RHINE III (Respiratory Health in Northern Europe, www.rhine.nu) was a follow-up after 20 years of the respondents of the postal questionnaire survey ECRHS (European Community Respiratory Health Survey, www.ecrhs.org) conducted in 1993-1994. The original sample for Tartu comprised 3,000 people aged 20-44. In 1999-2001 the RHINE II postal questionnaire was sent to 2,459 (aged 25-49) and the more recent 2011-2012 RHINE III questionnaire to 2,130 Tartu residents aged between 39-63 (in both cases participants comprised those people who had answered the ECRHS questionnaire in 1993, minus citizens who had died or left Estonia).
For the current study we selected only 905 people from total 1369 RHINE III respondents who wrote their current address as Tartu in the questionnaire. We believe this is more accurate than the address in Population register, where the questionnaire was sent (residents don’t often update their current address). A separate analysis was done with those respondents who had been living at the same address since 2001 (623 inhabitants) (Table 3).
Table 3. Association between health symptoms and 2009-2012 particle exposure among respondents who had lived at the same address in Tartu since 2001.
| OR (95% CI) per increase in interquartile range exposure | ||||||||
|---|---|---|---|---|---|---|---|---|
| Traffic induced PM10 | Residential heating induced PM2.5 | Total all sources induced PM2.5 | ||||||
| Crude model | Adjusted model1 | Multi–source model2 | Crude model | Adjusted model1 | Multi–source model2 | Crude model | Adjusted model1 | |
| Attack of cough | 1.00 (0.81–1.21) | 1.06 (0.83–1.36) | 1.07 (0.83–1.37) |
1.01 (0.74–1.39) | 1.04 (0.71–1.52) | 1.02 (0.70–1.50) |
1.00 (0.81–1.23) | 1.06 (0.82–1.36) |
| Wheeze without cold | 1.05 (0.80–1.40) | 1.00 (0.70–1.44) | 0.98 (0.68–1.42) |
1.03 (0.66–1.61) | 1.33 (0.76–2.33) | 1.33 (0.76–2.38) |
1.06 (0.80–1.42) | 1.11 (0.77–1.60) |
| Ever had asthma | 0.97 (0.64–1.48) | 0.91 (0.53–1.58) | 0.91 (0.51–1.59) |
1.22 (0.63–2.35) | 1.10 (0.47–2.56) | 1.12 (0.48–2.65) |
1.04 (0.68–1.59) | 0.97 (0.56–1.69) |
| Allergic rhinitis | 1.17 (0.89–1.54) | 1.16 (0.83–1.62) | 1.21 (0.87–1.70) |
0.74 (0.49–1.13) | 0.66 (0.39–1.12) | 0.63 (0.37–1.10) |
1.02 (0.77–1.35) | 0.98 (0.69–1.41) |
| Attack of breathlessness | 1.01 (0.76–1.34) | 1.10 (0.78–1.55) | 1.07 (0.75–1.53) |
1.04 (0.66–1.64) | 1.31 (0.75–2.30) | 1.30 (0.74–2.30) |
1.02 (0.76–1.37) | 1.19 (0.83–1.69) |
| Chest tightness | 1.03 (0.79–1.34) | 1.09 (0.80–1.50) | 1.09 (0.79–1.50) |
0.93 (0.61–1.40) | 1.03 (0.62–1.72) | 1.02 (0.59–1.68) |
0.99 (0.76–1.30) | 1.08 (0.78–1.51) |
| Cardiac disease | 1.25 (0.98–1.60) | 1.39 (1.02–1.88)* | 1.37 (0.99–1.86) |
1.23 (0.82–1.87) | 1.38 (0.82–2.34) | 1.28 (0.74–2.19) |
1.29 (0.99–1.67) | 1.44 (1.04–1.97)* |
| Hypertension | 0.99 (0.79–1.24) | 0.92 (0.68–1.24) | 0.96 (0.71–1.29) |
0.79 (0.58–1.07) | 0.71 (0.45–1.13) | 0.72 (0.45–1.15) |
0.89 (0.70–1.12) | 0.84 (0.62–1.13) |
| Stroke | 1.07 (0.49–2.29) | 1.12 (0.43–2.82) | 1.14 (0.44–2.94) |
0.72 (0.21–2.49) | 0.84 (0.18–3.88) | 0.80 (0.16–3.88) |
0.93 (0.41–2.14) | 1.00 (0.38–2.72) |
| Heart infarction or angina pectoris | 1.13 (0.69–1.84) | 1.29 (0.68–2.42) | 1.37 (0.71–2.58) |
0.53 (0.23–1.18) | 0.70 (0.24–2.01) | 0.63 (0.21–1.91) |
0.87 (0.51–1.50) | 1.07 (0.55–2.14) |
1Logistic regression model adjusted for gender, age, BMI, education, smoking history in the last 10 years (current, ex–, never) and ETS; * p < 0.05
2Logistic regression model also adjusted for residential heating PM2.5 or traffic PM10 respectively; * p < 0.05
2.2. Questionnaire on Respiratory Health and Cardiac Diseases in RHINE III
The health symptoms were defined based on the following questions:
Attack of cough: “Have you been woken by an attack of coughing at any time in the last 12 months?”
Wheeze without cold: “Have you had wheezing or whistling when you did not have a cold?”
Ever had asthma: “Do you have or have you ever had asthma?”
Allergic rhinitis: affirmative answer to questions “Do you have any nasal allergies including hay fever?” and “Have you ever experienced nasal symptoms such as nasal congestion, rhinorrhoea (runny nose) and/or sneezing attacks without having a cold?”
Attack of breathlessness: “Have you been woken by an attack of shortness of breath at any time during in the last 12 months?”
Chest tightness: “Have you woken up with a feeling of tightness in your chest at any time in the last 12 months?”
Cardiac disease: “Do you have any cardiac diseases?”
Hypertension: “Do you have high blood pressure?”
Stroke: “Have you ever had stroke?”
Heart infarction or angina pectoris: “Have you even been treated in hospital because of heart infarction or angina pectoris?”
The following confounding variables were used: gender, age, body mass index (BMI), education level, smoking habits, and environmental tobacco smoke (ETS) at home. Age was used as continuous variable and body mass index (BMI) was categorized into four groups: underweight (<18.5 kg/m2), normal weight (18.5-24.9 kg/m2), overweight (25.0-29.9 kg/m2) and obese (>30.0 kg/m2). Smoking habits were assessed for the preceding 10 years (current, ex-smoker and never smoked).
2.3. Exposure to Air Pollution
Mean annual pollution exposures for different sources (local heating induced PM2.5, traffic induced PM10 and total PM2.5) were modelled separately. Concentrations of PM2.5 and PM10 for the years 2009-2012 were calculated for grid size of 100x100 m across Tartu using an Eulerian air quality dispersion model part of the AirViro Air Quality Management System. AirViro is a web-based air pollution data management tool that uses measured levels of air pollution from monitoring stations and meteorological variables from meteorological stations. It is used in HIA and epidemiologic studies for air pollution exposure modelling [32, 33]. The local heating emissions data was based on a residential wood combustion (RWC) database that consisted of data from buildings (heating system and heated area in m2) and cadastral (cadastral coordinates) registries, which allowed us locate every household that used wood for heating. Household PM2.5 emissions (g/s) were calculated according to the size (m2) of each’s heated area. The RWC emission database was based on emission factors that have been measured in the Estonian Environmental Research Centre’s stove testing laboratory [34] and wood usage was acquired from the earlier questionnaire study in Tartu [35]. The traffic emission database was based on traffic counts conducted in 2011 and EEA/Corinair emission factors [36].
Modelled PM results for the years 2009-2012 were compared and validated with data of PM2.5 and PM10 at the Kalevi monitoring station in Tartu, where also aerosol chemical composition is measured in PM1 using the Aerodyne Aerosol Chemical Speciation Monitor (ACSM). The Kalevi station is located near the city centre in area with a relatively high percentage of wood burning heating systems. The ACSM is based on the widely used Aerodyne Aerosol Mass Spectrometer and combines an aerodynamic lens for particle focusing with high-vacuum particle thermal vaporization, electron impact ionization, and mass spectrometry [37]. The ACSM measures non-refractory PM1 composition (organics, SO4, NO3, NH4 and Chl) with a time resolution of 30 minutes.
For investigating potential specific sources of the measured particles, positive matrix factorization (PMF) was performed using SoFi 5.3 software [38]. Three main factors were identified according to the mass-to-charge (m/z) ratio: biomass burning aerosol (BBOA, m/z 29, 60, 73); oxidized organic aerosol (OOA, m/z 43, 44); hydrocarbon-like organic aerosol (HOA, m/z 27, 41, 43, 44, 55, 57, 69, 71). BBOA (50.64% of the total concentration) had small peak in the morning and a much larger peak in the evening. This was most likely indicative of peoples’ heating habits in the nearby RWC area. HOA (28.02% of the total concentration), which is associated with sources such as traffic, had a minimum during the night and peaks during the morning and evening rush hours. OOA (21.34% of the total concentration) is associated with aged aerosols and is counted as background concentration [39].
Modelled PM concentrations were linked with respondents’ geocoded home addresses using ArcGIS 10.1 (ESRI, Redlands, CA, USA).
2.4. Statistical Analyses
For the analysis of the association between PM exposure at their home address and self-reported health problems, multiple logistic regression in Stata (StataCorp LP, College Station, TX, USA) was used. Odds ratios (OR) calculated per interquartile range (IQR) were used to describe between particle concentrations and health outcomes. All analyses (local heating PM2.5, traffic PM10 and total PM2.5) were adjusted for gender, age, body mass index (BMI), education level, smoking history and ETS (environmental tobacco smoke) at home.
3. RESULTS
3.1. Participants’ Demographics and Health Symptoms
The characteristics of the study participants are summarized in Table 1. The mean age of respondents was 50 years. There were slightly more women (60.0%) and almost half of all respondents (43.4%) had a higher education. The prevalence of current smokers was 28.2% and 18.4% of respondents had been exposed to environmental tobacco smoke (ETS) in their homes every day. Among the health symptoms, the highest prevalence was for coughing (46.4%) and allergic rhinitis (36.9%). One quarter (25.4%) of respondents were obese (BMI >30).
Table 1. Characteristics of the Tartu study populations.
| Variables | Respondents living in Tartu in 2012 (n=905) | Respondents living at the same address since 2001 (n=623) | ||
|---|---|---|---|---|
| n | % | n | % | |
| BMI (kg/m2) | ||||
| Underweight | 3 | 0.3 | 2 | 0.3 |
| Normal weight | 347 | 38.8 | 231 | 37.5 |
| Overweight | 318 | 35.5 | 212 | 34.4 |
| Obese | 227 | 25.4 | 171 | 27.8 |
| Gender | ||||
| Male | 362 | 40.0 | 246 | 39.5 |
| Female | 543 | 60.0 | 377 | 60.5 |
| Smoking history during the previous 10 years | ||||
| Current | 198 | 28.2 | 136 | 27.7 |
| Ex-smoker | 76 | 10.8 | 52 | 10.6 |
| Never smoked | 429 | 61.0 | 303 | 61.7 |
| Environmental Tobacco Smoke (ETS) at home | ||||
| Every day | 162 | 18.4 | 111 | 18.4 |
| 1-4 times a week | 26 | 3.0 | 22 | 3.6 |
| 1-3 times a month | 46 | 5.2 | 30 | 5.0 |
| Never | 646 | 73.4 | 441 | 73.0 |
| Education | ||||
| Basic | 46 | 5.2 | 35 | 5.8 |
| Secondary | 454 | 51.4 | 332 | 54.7 |
| Higher | 383 | 43.4 | 240 | 39.5 |
| Attack of cough | 414 | 46.4 | 276 | 45.0 |
| Wheeze without cold | 134 | 15.1 | 87 | 14.3 |
| Ever had asthma | 53 | 6.8 | 38 | 7.2 |
| Allergic rhinitis | 196 | 36.9 | 137 | 37.5 |
| Attack of breathlessness | 128 | 14.3 | 85 | 13.8 |
| Chest tightness | 168 | 18.9 | 105 | 17.2 |
| Cardiac disease | 140 | 15.9 | 109 | 18.0 |
| Hypertension | 230 | 25.7 | 170 | 27.5 |
| Stroke | 14 | 1.6 | 10 | 1.6 |
| Heart infarction or angina pectoris | 31 | 3.7 | 25 | 4.3 |
Residents living at the current address since 2001 were slightly older (mean age of 51 years), had a higher percentage of people with a BMI >30 (27.8%) and 39.5% had higher education. Smoking prevalence was slightly lower (27.7%). There was no difference in the percentage of people exposed to ETS at home daily.
3.2. Air Pollution Exposure
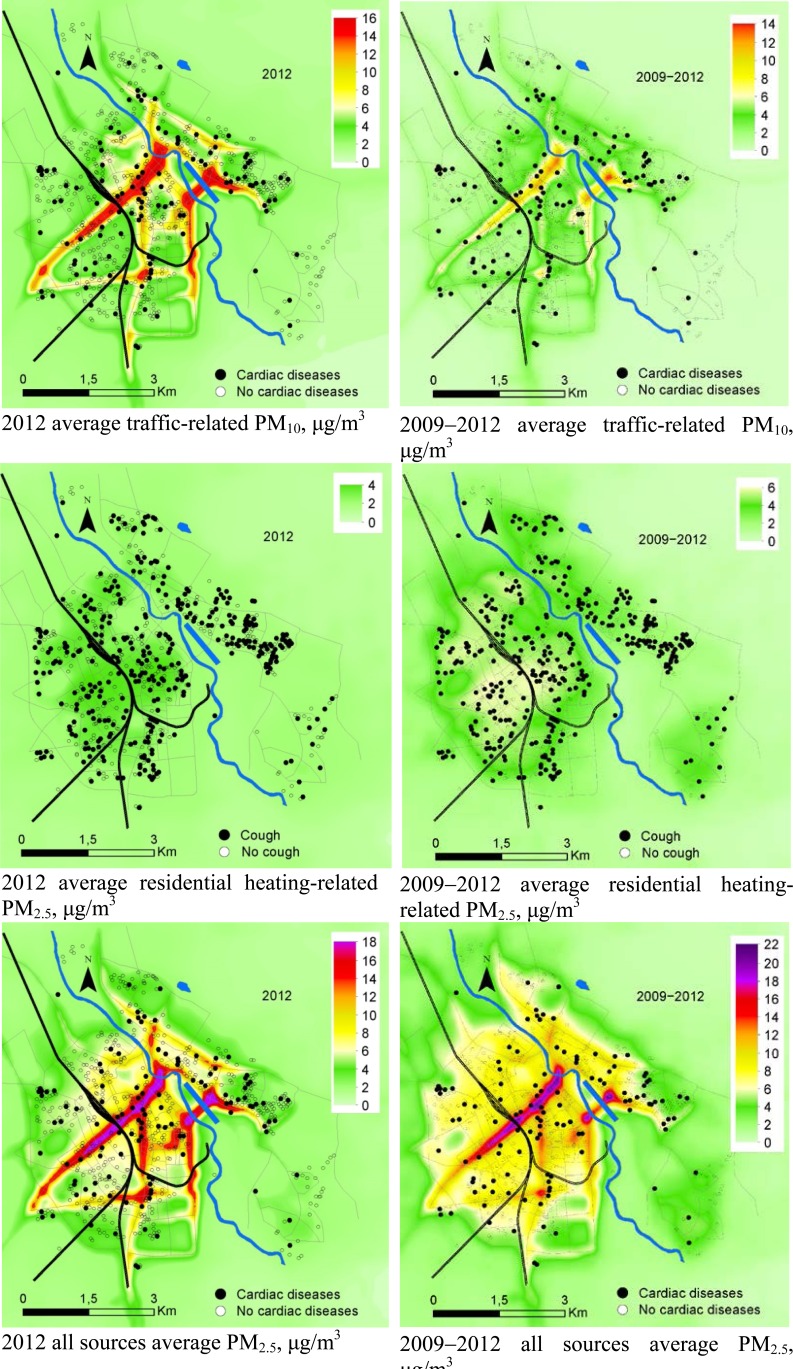
The annual mean exposure to residential heating induced particles among the respondents living in Tartu during 2012 was 2.3 μg/m3 (SD 0.9; IQR 1.5 μg/m3). However, in some areas residential heating induced PM2.5 exposures were considerably higher, with a maximum level of 4 μg/m3. The annual mean exposure to traffic induced PM10 (exhaust fumes and road dust, brake and tyre wear) was 3.3 μg/m3 (SD 2.0; IQR 2.9 μg/m3). As some streets have rather high traffic flows, the annual level of PM10 in some streets of Tartu was as high as 16 μg/m3 in 2012. The total mean PM2.5 exposure for Tartu was 5.6 μg/m3 (SD 2.5; IQR 3.8 μg/m3), with maximum concentrations in some streets up to 18 μg/m3 (Fig. 1).
Fig. (1).
Traffic induced PM10, residential heating induced PM2.5, and total PM2.5 average concentrations in 2012 and in 2009−2012 for Tartu, and the location of respondents with cardiac diseases and attack of cough.
The average residential heating induced concentration in 2009-2012 PM2.5 was 3.4 μg/m3 (SD 1.2; IQR 2.3 μg/m3), with a maximum level of 6 μg/m3. Mean exposure to traffic induced PM10 was 2.7 μg/m3 (SD 1.8; IQR 2.2 μg/m3) and the maximum level 14 μg/m3. Total particle exposure over 2009-2012 was 7.4 μg/m3 (SD 2.8; IQR 3.6 μg/m3), with a maximum concentration of 22 μg/m3 (Fig. 1).
3.3. Particle Exposure and Health Symptoms
Among the studied health symptoms of the Tartu residents in 2012 there appeared to be an association between an IQR increase in traffic induced PM10 and cardiac diseases (OR=1.45, 95% CI 1.06−1.93). The association was also significant (p < 0.05) for IQR increase in total PM2.5 exposure and cardiac disease (OR=1.42, 95% CI 1.02-1.95). As residents exposed to traffic induced particles were simultaneously also exposed to wood smoke particles, a multi-source model was built. When also taking into account the potential risk factors from residential heating, the odds ratio for an IQR increase in traffic induced particles and cardiac disease increased slightly (OR=1.45, 95% CI 1.09-2.02). Nevertheless, we found no associations with residential heating induced particles and respiratory or cardiac health symptoms. A protective effect appeared between an IQR increase in residential heating induced particles and allergic rhinitis in single-source (OR=0.68, 95% CI 0.47-1.00) and in multi-source model (OR=0.63, 95% CI 0.42-0.94) (Table 2).
Table 2. Association between health symptoms and 2012 particle exposure among respondents living in their recent address.
| OR (95% CI) per increase in interquartile range exposure | ||||||||
|---|---|---|---|---|---|---|---|---|
| Traffic induced PM10 | Residential heating induced PM2.5 | Total all sources induced PM2.5 | ||||||
| Crude model | Adjusted model1 | Multi-source model2 | Crude model | Adjusted model1 | Multi-source model2 | Crude model | Adjusted model1 | |
| Attack of cough | 1.06 (0.89−1.28) | 1.09 (0.86−1.35) | 1.09 (0.86−1.38) | 0.98 (0.78−1.22) | 1.00 (0.77−1.30) | 0.95 (0.72−1.29) | 1.04 (0.85−1.30) | 1.08 (0.85−1.34) |
| Wheeze without cold | 1.06 (0.81−1.35) | 1.06 (0.79−1.45) | 1.03 (0.74−1.45) | 0.98 (0.72−1.36) | 1.16 (0.78−1.73) | 1.14 (0.75−1.73) | 1.04 (0.79−1.39) | 1.12 (0.79−1.60) |
| Ever had asthma | 1.09 (0.76−1.60) | 1.09 (0.69−1.76) | 1.06 (0.65−1.72) | 1.19 (0.74−1.94) | 1.19 (0.64−2.17) | 1.16 (0.60−2.19) | 1.16 (0.76−1.71) | 1.16 (0.70−1.89) |
| Allergic rhinitis | 1.21 (0.94–1.56) | 1.09 (0.79–1.45) | 1.25 (0.89–1.72) | 0.87 (0.63–1.17) | 0.68 (0.47–1.00)* | 0.63 (0.42–0.94)* | 1.12 (0.85–1.49) | 0.93 (0.67–1.30) |
| Attack of breathlessness | 1.15 (0.89–1.45) | 1.21 (0.89–1.60) | 1.21 (0.89–1.64) | 0.97 (0.70–1.32) | 1.06 (0.71–1.56) | 0.97 (0.64–1.48) | 1.12 (0.85–1.44) | 1.21 (0.85–1.65) |
| Chest tightness | 1.12 (0.89–1.42) | 1.15 (0.86–1.49) | 1.12 (0.84–1.49) | 0.98 (0.74–1.32) | 1.09 (0.78–1.56) | 1.05 (0.72–1.51) | 1.08 (0.85–1.39) | 1.16 (0.85–1.55) |
| Cardiac disease | 1.28 (1.01–1.64)* | 1.45 (1.06–1.93)* | 1.45 (1.09–2.02)* | 1.02 (0.74–1.39) | 1.09 (0.74–1.60) | 0.92 (0.60–1.39) | 1.25 (0.96–1.65) | 1.42 (1.02–1.95)* |
| Hypertension | 1.15 (0.94–1.42) | 1.06 (0.81–1.38) | 1.12 (0.84–1.49) | 0.85 (0.66–1.11) | 0.82 (0.59–1.16) | 0.78 (0.54–1.12) | 1.08 (0.89–1.39) | 0.99 (0.73–1.34) |
| Stroke | 1.09 (0.53–2.21) | 1.21 (0.53–2.77) | 1.28 (0.51–3.12) | 0.79 (0.31–1.97) | 0.94 (0.33–2.76) | 0.85 (0.27–2.71) | 1.01 (0.45–2.28) | 1.16 (0.47–2.99) |
| Heart infarction or angina pectoris | 1.18 (0.74–1.89) | 1.49 (0.81–2.72) | 1.64 (0.89–3.12) | 0.62 (0.33–1.16) | 0.85 (0.39–1.86) | 0.67 (0.28–1.56) | 0.98 (0.56–1.71) | 1.34 (0.70–2.66) |
1Logistic regression model adjusted for gender, age, BMI, education, smoking history in the last 10 years (current, ex–, never) and ETS; * p < 0.05
2Logistic regression model also adjusted for residential heating PM2.5 or traffic PM10 respectively; * p < 0.05
Study results were similar in residents living at the same address since 2001 compared to those who had any Tartu city address in 2012. IQR increase in traffic-related particle exposure was also associated with cardiac disease (OR=1.39, 95% CI 1.02-1.88) among long-term residents. However, we didn’t saw an association with multi-source model. The ORs for an IQR increase in all sources total particle exposure and cardiac disease were slightly higher (OR=1.44, 95% CI 1.04-1.97) compared to people with exposure only to 2012 air pollution. No significant association with residential heating induced PM2.5 and health symptoms was found (Table 3).
4. DISCUSSION
4.1. Variations in Associations Between Health Symptoms and Different Sources of PM
Of the investigated sources and health symptoms, the potential association between traffic induced particles and cardiac disease appeared to be the most important. This is in line with several other studies that have found association between traffic-related PM and cardio-respiratory diseases [11, 40]. In our study we did not find any statistically significant association between traffic induced particles and respiratory symptoms. However, a recent study associated increasing PM10 and chest tightness or coughing in adults [41] and several other studies have found relationships between traffic-related air pollution and the development of asthma in children and COPD in adults [42]. Studies have also reported that children and the elderly are at a higher risk of developing respiratory diseases when exposed to very high particle concentration levels (PM2.5 over 250 µg/m3 and PM10 over 1500 µg/m3) [43, 44] and living close to streets with high traffic flows increases the risk of wheezing among schoolchildren [45].
We did not find any significant association between residential heating-related particles and self-reported health symptoms in a single-pollutant model; protective effect appeared in multi-source model between allergic rhinitis and residential heating. Study among children suggested that, protective role of residential heating might be the reason for increased risk of respiratory tract infections in childhood [46]. Earlier analysis with RHINE II data (2000/2001) showed higher odds of having respiratory symptoms such as wheeze and attack of cough in areas with higher levels of residential heating induced particles in Tartu [47]. Possible differences between these two analyses could be the lower exposure to residential heating induced particles, as levels in 2012 were lower than in average of 2009-2012 (Fig. 1). Also earlier modelling was done with different dispersion model with less accurate residential heating database, as used in the current study. Wood smoke in general has also been found to be toxic as studies have reported associations between wood smoke toxicity and systemic inflammation respiratory diseases (wheeze, cough) and cardiac hospital admissions [48-50].
Toxicological studies indicate that biomass smoke could also be associated with inflammatory effects [51-53] that could later induce cardio-respiratory problems. However, it has been suggested that the inflammatory potential of wood smoke particles is smaller than that of traffic-related particle [54]. In addition, biomass combustion particles often grow in size within the human respiratory tract and therefore deposition is less efficient [55]. The higher deposition and toxicity of traffic particles compared to wood smoke could be the reason why we only saw statistically significant association between traffic induced PM and cardiac symptoms.
4.2. Dispersion Modelling to Separate Exposures from Different Sources
In our analysis dispersion modelling with separating different sources of PM was used for air pollution exposure assessments that seemed to be a good method differentiating exposure for different sources for epidemiological studies. Moreover, research community has now started focusing more on assessing PM from different sources (wood combustion, traffic) [56]. However, there are some concerns regarding air pollution assessment in general. Firstly, a resident’s exposure is calculated based on the exposures at their home address, rather than in every day locations. Recent studies using GPS tracking have found that people only spend 15 hours a day in their homes [57]. However, to get annual personal exposure data with GPS tracking is expensive and the probable number of recruits is likely small. Unfortunately, we didnot ask people’s work address, only occupation was inquired and then average exposure from home location was assessed. Secondly, we used self-reported answers to a questionnaire and related them with personal PM levels. Thus, over/under-estimation of peoples’ health symptoms is also possible in the current work.
Some earlier studies also used a source apportionment approach to define the sources of particulate matter [58, 59]; however, this is usually based on measuring station data and is therefore too crude for epidemiological studies in areas with few measuring stations.
4.3. Traffic-related Particle Composition and Their Health Effects
In urban areas in the UK, background organic carbon, sulphates and nitrates in composition of PM2.5 have also been found in high concentrations [60]. After only five hours of exposure to PM that includes fine organic carbon, sulphates and nitrates, significant changes in biomarker levels associated with acute cardiovascular risk can occur [61], which adds weight to the finding of the current study for a potential relationship between ambient traffic PM and risk of cardiac disease.
One of the earlier studies used indicators of oxidative capacity and possible toxicity was hydroxyl radical formation. During the ECRHS II study (2000/2001) it was found that PM2.5 with hydroxyl radicals in Tartu contained high amounts of some heavy metals, such as Zn, Pb and Ti in the PM2.5 fraction [6]. Some heavy metals (e.g. Zn, Pb, Cu) can be related to vehicular traffic, as measurements in a road tunnel (where traffic is the main source of air pollution) showed that heavy metals could contribute up to 19% of total PM10 mass and 11.6% of total PM2.5 mass [62]. Studies showing toxicity of heavy metals [23] and the presence of heavy metals in particles from traffic could be one of the explanations among others (e.g. particle size and deposition level), why we saw significant health effects with traffic particles but did not with wood smoke particles.
We found that traffic induced PM compared to residential heating induced PM are more strongly associated with health symptoms, especially with cardiac diseases. This study is in line with other research about PM and cardiovascular disease and supports results from few studies that analysed mainly short-term association between multiple PM sources and health symptoms [25-28]. Our modelling results show that traffic induced PM had higher concentration in Tartu city environment than residential heating induced PM. Similar results have been indicated by Lee et al. [63]. in Southeastern US, where they saw relatively higher motor vehicle source impacts in populated urban areas and relatively higher impacts of biomass burning in less urbanized area. Also, we saw that the health effects can appear at very low levels, as the annual average PM concentrations in Tartu were below limit values set by Estonian and EU legislation. Thus, propagating activities as using more public transport and re-organizing vehicle traffic as well as better access to alternative low-emission heating technologies should lower the PM levels and thereby affect health of less people.
ACKNOWLEDGEMENTS
We thank our co-workers in the RHINE team, especially the supporting staff in Estonia. This study was financed by grants IUT20–11 and IUT34–17 from The Estonian Ministry of Education and Research, and grant ETF8523 from The Estonian Science Foundation.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
REFERENCES
- 1.Karvosenoja N., Tainio M., Kupiainen K., Tuomisto J.T., Kukkonen J., Johansson M. Evaluation of the emissions and uncertainties of PM2.5 originated from vehicular traffic and domestic wood combustion in Finland. Boreal Environ Res. 2008;13:465–474. [Google Scholar]
- 2.Forsberg B., Hansson H.C., Johansson C., Areskoug H., Persson K., Järvholm B. Comparative health impact assessment of local and regional particulate air pollutants in Scandinavia. Ambio. 2005;34(1):11–19. doi: 10.1579/0044-7447-34.1.11. [DOI] [PubMed] [Google Scholar]
- 3.Saarikoski S., Sillanpaa M.K., Saarnio K.M., Hillamo R.E., Pennanen A.S., Salonen R.O. Impact of biomass combustion on urban fine particulate matter in Central and Northern Europe. Water Air Soil Pollut. 2008;191:265–277. doi: 10.1007/s11270-008-9623-1. [DOI] [Google Scholar]
- 4.Wu C.F., Larson T.V., Wu S.Y., Williamson J., Westberg H.H., Liu L.J. Source apportionment of PM (2.5) and selected hazardous air pollutants in Seattle. Sci. Total Environ. 2007;386(1-3):42–52. doi: 10.1016/j.scitotenv.2007.07.042. [DOI] [PubMed] [Google Scholar]
- 5.Yttri K.E., Dye C., Braathen O.A., Simpson D., Steinnes E. Carbonaceous aerosols in Norwegian urban areas. Atmos. Chem. Phys. 2009;9:2007–2020. doi: 10.5194/acp-9-2007-2009. [DOI] [Google Scholar]
- 6.Orru H., Kimmel V., Kikas U., Soon A., Künzli N., Schins R.P., Borm P.J., Forsberg B. Elemental composition and oxidative properties of PM(2.5) in Estonia in relation to origin of air masses - results from the ECRHS II in Tartu. Sci. Total Environ. 2010;408(7):1515–1522. doi: 10.1016/j.scitotenv.2009.12.006. [DOI] [PubMed] [Google Scholar]
- 7.Pettersson E., Boman C., Westerholm R., Bostrom D., Nordin A. Stove Performance and Emission Characteristics in Residential Wood Log and Pellet Combustion, Part 2: Wood Stove. Energy Fuels. 2011;25:315–323. doi: 10.1021/ef1007787. [DOI] [Google Scholar]
- 8.Kocbach Bølling A., Pagels J., Yttri K.E., Barregard L., Sallsten G., Schwarze P.E., Boman C. Health effects of residential wood smoke particles: the importance of combustion conditions and physicochemical particle properties. Part. Fibre Toxicol. 2009;6:29. doi: 10.1186/1743-8977-6-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bølling A.K., Totlandsdal A.I., Sallsten G., Braun A., Westerholm R., Bergvall C., Boman J., Dahlman H.J., Sehlstedt M., Cassee F., Sandstrom T., Schwarze P.E., Herseth J.I. Wood smoke particles from different combustion phases induce similar pro-inflammatory effects in a co-culture of monocyte and pneumocyte cell lines. Part. Fibre Toxicol. 2012;9:45. doi: 10.1186/1743-8977-9-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Johansson C., Norman M., Gidhagen L. Spatial & temporal variations of PM10 and particle number concentrations in urban air. Environ. Monit. Assess. 2007;127(1-3):477–487. doi: 10.1007/s10661-006-9296-4. [DOI] [PubMed] [Google Scholar]
- 11.Brunekreef B., Beelen R., Hoek G., Schouten L., Bausch-Goldbohm S., Fischer P., Armstrong B., Hughes E., Jerrett M., van den Brandt P. Effects of long-term exposure to traffic-related air pollution on respiratory and cardiovascular mortality in the Netherlands: the NLCS-AIR study. Res. Rep. Health Eff. Inst. 2009;139(139):5–71. [PubMed] [Google Scholar]
- 12.Orru H., Kaasik M., Antov D., Forsberg B. Evolution of traffic flows and traffic-induced air pollution due to structural changes and development during 1993–2006 in Tartu (Estonia). Balt. J. Road Bridge Eng. 2008;3:206–212. doi: 10.3846/1822-427X.2008.3.206-212. [DOI] [Google Scholar]
- 13.Pope CAr Dockery DW. Health effects of fine particulate air pollution: lines that connect. J. Air Waste Manage. Assoc. 2006;56:709–742. doi: 10.1080/10473289.2006.10464485. [DOI] [PubMed] [Google Scholar]
- 14.Rückerl R., Schneider A., Breitner S., Cyrys J., Peters A. Health effects of particulate air pollution: A review of epidemiological evidence. Inhal. Toxicol. 2011;23(10):555–592. doi: 10.3109/08958378.2011.593587. [DOI] [PubMed] [Google Scholar]
- 15.Brook R.D., Rajagopalan S., Pope C.A., III, Brook J.R., Bhatnagar A., Diez-Roux A.V., Holguin F., Hong Y., Luepker R.V., Mittleman M.A., Peters A., Siscovick D., Smith S.C., Jr, Whitsel L., Kaufman J.D., American Heart Association Council on Epidemiology and Prevention, Council on the Kidney in Cardiovascular Disease, and Council on Nutrition, Physical Activity and Metabolism Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation. 2010;121(21):2331–2378. doi: 10.1161/CIR.0b013e3181dbece1. [DOI] [PubMed] [Google Scholar]
- 16.Schwarze P.E., Ovrevik J., Låg M., Refsnes M., Nafstad P., Hetland R.B., Dybing E. Particulate matter properties and health effects: consistency of epidemiological and toxicological studies. Hum. Exp. Toxicol. 2006;25(10):559–579. doi: 10.1177/096032706072520. [DOI] [PubMed] [Google Scholar]
- 17.Meister K., Johansson C., Forsberg B. Estimated short-term effects of coarse particles on daily mortality in Stockholm, Sweden. Environ. Health Perspect. 2012;120(3):431–436. doi: 10.1289/ehp.1103995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brunekreef B., Forsberg B. Epidemiological evidence of effects of coarse airborne particles on health. Eur. Respir. J. 2005;26(2):309–318. doi: 10.1183/09031936.05.00001805. [DOI] [PubMed] [Google Scholar]
- 19.Jerrett M., Burnett R.T., Ma R., Pope C.A., III, Krewski D., Newbold K.B., Thurston G., Shi Y., Finkelstein N., Calle E.E., Thun M.J. Spatial analysis of air pollution and mortality in Los Angeles. Epidemiology. 2005;16(6):727–736. doi: 10.1097/01.ede.0000181630.15826.7d. [DOI] [PubMed] [Google Scholar]
- 20.Krewski D., Jerrett M., Burnett R.T., et al. Extended follow-up and spatial analysis of the American Cancer Society study linking particulate air pollution and mortality. Cambridge, MA: Research Report Health Effects Institute; 2009. [PubMed] [Google Scholar]
- 21.Bell M.L., HEI Health Review Committee Assessment of the health impacts of particulate matter characteristics. Res. Rep. Health Eff. Inst. 2012;161(161):5–38. [PubMed] [Google Scholar]
- 22.Ghio A.J., Carraway M.S., Madden M.C. Composition of air pollution particles and oxidative stress in cells, tissues, and living systems. J. Toxicol. Environ. Health B Crit. Rev. 2012;15(1):1–21. doi: 10.1080/10937404.2012.632359. [DOI] [PubMed] [Google Scholar]
- 23.Valavanidis A., Fiotakis K., Vlachogianni T. Airborne particulate matter and human health: toxicological assessment and importance of size and composition of particles for oxidative damage and carcinogenic mechanisms. J Environ Sci Health C Environ Carcinog Ecotoxicol Rev. 2008;26(4):339–362. doi: 10.1080/10590500802494538. [DOI] [PubMed] [Google Scholar]
- 24.Pindus M., Orru H., Modig L. Close proximity to busy roads increases the prevalence and onset of cardiac disease--Results from RHINE Tartu. Public Health. 2015;129(10):1398–1405. doi: 10.1016/j.puhe.2015.07.029. [DOI] [PubMed] [Google Scholar]
- 25.Ostro B., Tobias A., Querol X., Alastuey A., Amato F., Pey J., Pérez N., Sunyer J. The effects of particulate matter sources on daily mortality: a case-crossover study of Barcelona, Spain. Environ. Health Perspect. 2011;119(12):1781–1787. doi: 10.1289/ehp.1103618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Laden F., Neas L.M., Dockery D.W., Schwartz J. Association of fine particulate matter from different sources with daily mortality in six U.S. cities. Environ. Health Perspect. 2000;108(10):941–947. doi: 10.1289/ehp.00108941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mar T.F., Ito K., Koenig J.Q., Larson T.V., Eatough D.J., Henry R.C., Kim E., Laden F., Lall R., Neas L., Stölzel M., Paatero P., Hopke P.K., Thurston G.D. PM source apportionment and health effects. 3. Investigation of inter-method variations in associations between estimated source contributions of PM2.5 and daily mortality in Phoenix, AZ. J. Expo. Sci. Environ. Epidemiol. 2006;16(4):311–320. doi: 10.1038/sj.jea.7500465. [DOI] [PubMed] [Google Scholar]
- 28.Ito K., Christensen W.F., Eatough D.J., Henry R.C., Kim E., Laden F., Lall R., Larson T.V., Neas L., Hopke P.K., Thurston G.D. PM source apportionment and health effects: 2. An investigation of intermethod variability in associations between source-apportioned fine particle mass and daily mortality in Washington, DC. J. Expo. Sci. Environ. Epidemiol. 2006;16(4):300–310. doi: 10.1038/sj.jea.7500464. [DOI] [PubMed] [Google Scholar]
- 29.Boman B.C., Forsberg A.B., Järvholm B.G. Adverse health effects from ambient air pollution in relation to residential wood combustion in modern society. Scand. J. Work Environ. Health. 2003;29(4):251–260. doi: 10.5271/sjweh.729. [DOI] [PubMed] [Google Scholar]
- 30.Naeher L.P., Brauer M., Lipsett M., Zelikoff J.T., Simpson C.D., Koenig J.Q., Smith K.R. Woodsmoke health effects: a review. Inhal. Toxicol. 2007;19(1):67–106. doi: 10.1080/08958370600985875. [DOI] [PubMed] [Google Scholar]
- 31.Tainio M., Tuomisto J.T., Pekkanen J., et al. Uncertainty in health risks due to anthropogenic primary fine particulate matter from different source types in Finland. Atmos. Environ. 2010;44:2125–2132. doi: 10.1016/j.atmosenv.2010.02.036. [DOI] [Google Scholar]
- 32.Pierse N., Rushton L., Harris R.S., Kuehni C.E., Silverman M., Grigg J. Locally generated particulate pollution and respiratory symptoms in young children. Thorax. 2006;61(3):216–220. doi: 10.1136/thx.2004.036418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Orru H., Maasikmets M., Lai T., et al. Health impacts of particulate matter in five major Estonian towns: main sources of exposure and local differences. Air Qual. Atmos. Health. 2011;4:247–248. doi: 10.1007/s11869-010-0075-6. [DOI] [Google Scholar]
- 34.Teinemaa E., Maasikmets M., Vainumäe K., Heinsoo A., Arumäe T., Lehes L. Fulfilling the requirements of Convention on Long-Range Transboundary Air Pollution (Geneva) Convention. Estonian Environmental Research Centre. 2013. Available from: http://envir.ee/sites/ default/files/genfi_aruanne_final.pdf .
- 35.Kaasik M., Orru H., Tekkel E., Vals P. Situation and tendencies in air quality in a north European medium-sized town. In: Proceedings of the 6th; International Conference on Urban Air Quality; Larnaca, Cyprus: University of Hertfordshire 2007. [Google Scholar]
- 36.EEA . Technical report No 16/2007. Copenhagen, Denmark: 2007. EMEP/CORINAIR Emission Inventory Guidebook - 2007. Available from: http://www.eea.europa.eu/ publications/EMEPCORINAIR5 . [Google Scholar]
- 37.Ng N.L., Herndon S.C., Trimborn A., et al. An Aerosol chemical speciation monitor (ACSM) for routine monitoring of the composition and mass concentrations of ambient aerosol. Aerosol Sci. Technol. 2011;45:780–794. doi: 10.1080/02786826.2011.560211. [DOI] [Google Scholar]
- 38.Canonaco F., Crippa M., Slowik J.G., Baltensperger U., Prévôt A.S. SoFi, an IGOR-based interface for the efficient use of the generalized multilinear engine (ME-2) for the source apportionment: ME-2 application to aerosol mass spectrometer data. Atmos. Meas. Tech. 2013;6:3649–3661. doi: 10.5194/amt-6-3649-2013. [DOI] [Google Scholar]
- 39.Zhang Q., Alfarra M.R., Worsnop D.R., Allan J.D., Coe H., Canagaratna M.R., Jimenez J.L. Deconvolution and quantification of hydrocarbon-like and oxygenated organic aerosols based on aerosol mass spectrometry. Environ. Sci. Technol. 2005;39(13):4938–4952. doi: 10.1021/es048568l. [DOI] [PubMed] [Google Scholar]
- 40.Hoek G., Krishnan R.M., Beelen R., Peters A., Ostro B., Brunekreef B., Kaufman J.D. Long-term air pollution exposure and cardio- respiratory mortality: a review. Environ. Health. 2013;12(1):43. doi: 10.1186/1476-069X-12-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Willers S.M., Eriksson C., Gidhagen L., Nilsson M.E., Pershagen G., Bellander T. Fine and coarse particulate air pollution in relation to respiratory health in Sweden. Eur. Respir. J. 2013;42(4):924–934. doi: 10.1183/09031936.00088212. [DOI] [PubMed] [Google Scholar]
- 42.Laumbach R.J., Kipen H.M. Respiratory health effects of air pollution: update on biomass smoke and traffic pollution. J. Allergy Clin. Immunol. 2012;129(1):3–11. doi: 10.1016/j.jaci.2011.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Delfino R.J., Brummel S., Wu J., Stern H., Ostro B., Lipsett M., Winer A., Street D.H., Zhang L., Tjoa T., Gillen D.L. The relationship of respiratory and cardiovascular hospital admissions to the southern California wildfires of 2003. Occup. Environ. Med. 2009;66(3):189–197. doi: 10.1136/oem.2008.041376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kunii O., Kanagawa S., Yajima I., Hisamatsu Y., Yamamura S., Amagai T., Ismail I.T. The 1997 haze disaster in Indonesia: its air quality and health effects. Arch. Environ. Health. 2002;57(1):16–22. doi: 10.1080/00039890209602912. [DOI] [PubMed] [Google Scholar]
- 45.Andersson M., Modig L., Hedman L., Forsberg B., Rönmark E. Heavy vehicle traffic is related to wheeze among schoolchildren: a population-based study in an area with low traffic flows. Environ. Health. 2011;10:91. doi: 10.1186/1476-069X-10-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.von Mutius E., Illi S., Nicolai T., Martinez F.D. Relation of indoor heating with asthma, allergic sensitisation, and bronchial responsiveness: survey of children in south Bavaria. BMJ. 1996;312(7044):1448–1450. doi: 10.1136/bmj.312.7044.1448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Orru H., Jogi R., Maasikmets M., Kaasik M., Ardi L., Kukk E. Effects of Chronic PM Exposure From Local Heating on Self-reported Respiratory and Cardiovascular Health in the RHINE Tartu Cohort. Joint Conference of International Society of Exposure Science/International Society for Environmental Epidemiology. Seoul, North Korea: Epidemiology; 2011. pp. S225–S26. [Google Scholar]
- 48.Hersoug L.G., Husemoen L.L., Sigsgaard T., Madsen F., Linneberg A. Indoor exposure to environmental cigarette smoke, but not other inhaled particulates associates with respiratory symptoms and diminished lung function in adults. Respirology. 2010;15(6):993–1000. doi: 10.1111/j.1440-1843.2010.01758.x. [DOI] [PubMed] [Google Scholar]
- 49.McGowan J.A., Hider R.N., Chacko E., Town G.I. Particulate air pollution and hospital admissions in Christchurch, New Zealand. Aust. N. Z. J. Public Health. 2002;26(1):23–29. doi: 10.1111/j.1467-842X.2002.tb00266.x. [DOI] [PubMed] [Google Scholar]
- 50.Bølling A.K., Pagels J., Yttri K.E., et al. Health effects of residential wood smoke particles: the importance of combustion conditions and physicochemical particle properties. Part. Fibre Toxicol. 2009;6:29. doi: 10.1186/1743-8977-6-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Barregard L., Sällsten G., Gustafson P., Andersson L., Johansson L., Basu S., Stigendal L. Experimental exposure to wood-smoke particles in healthy humans: effects on markers of inflammation, coagulation, and lipid peroxidation. Inhal. Toxicol. 2006;18(11):845–853. doi: 10.1080/08958370600685798. [DOI] [PubMed] [Google Scholar]
- 52.Swiston J.R., Davidson W., Attridge S., Li G.T., Brauer M., van Eeden S.F. Wood smoke exposure induces a pulmonary and systemic inflammatory response in firefighters. Eur. Respir. J. 2008;32(1):129–138. doi: 10.1183/09031936.00097707. [DOI] [PubMed] [Google Scholar]
- 53.Tan W.C., Qiu D., Liam B.L., Ng T.P., Lee S.H., van Eeden S.F., D’Yachkova Y., Hogg J.C. The human bone marrow response to acute air pollution caused by forest fires. Am. J. Respir. Crit. Care Med. 2000;161(4 Pt 1):1213–1217. doi: 10.1164/ajrccm.161.4.9904084. [DOI] [PubMed] [Google Scholar]
- 54.Kocbach A., Herseth J.I., Låg M., Refsnes M., Schwarze P.E. Particles from wood smoke and traffic induce differential pro-inflammatory response patterns in co-cultures. Toxicol. Appl. Pharmacol. 2008;232(2):317–326. doi: 10.1016/j.taap.2008.07.002. [DOI] [PubMed] [Google Scholar]
- 55.Löndahl J., Pagels J., Boman C., Swietlicki E., Massling A., Rissler J., Blomberg A., Bohgard M., Sandström T. Deposition of biomass combustion aerosol particles in the human respiratory tract. Inhal. Toxicol. 2008;20(10):923–933. doi: 10.1080/08958370802087124. [DOI] [PubMed] [Google Scholar]
- 56.Gustafsson M., Forsberg B., Orru H., Åström S., Tekie H., Sjöberg K. Quantification of population exposure to NO2, PM2.5 and PM10 and estimated health impacts in Sweden 2010. Göteborg: IVL Swedish Environmental Research Institute Ltd; 2014. [Google Scholar]
- 57.Steinle S., Reis S., Sabel C.E., Semple S., Twigg M.M., Braban C.F., Leeson S.R., Heal M.R., Harrison D., Lin C., Wu H. Personal exposure monitoring of PM2.5 in indoor and outdoor microenvironments. Sci. Total Environ. 2015;508:383–394. doi: 10.1016/j.scitotenv.2014.12.003. [DOI] [PubMed] [Google Scholar]
- 58.Park S.K., O’Neill M.S., Stunder B.J., Vokonas P.S., Sparrow D., Koutrakis P., Schwartz J. Source location of air pollution and cardiac autonomic function: trajectory cluster analysis for exposure assessment. J. Expo. Sci. Environ. Epidemiol. 2007;17(5):488–497. doi: 10.1038/sj.jes.7500552. [DOI] [PubMed] [Google Scholar]
- 59.Hopke P.K., Ito K., Mar T., Christensen W.F., Eatough D.J., Henry R.C., Kim E., Laden F., Lall R., Larson T.V., Liu H., Neas L., Pinto J., Stölzel M., Suh H., Paatero P., Thurston G.D. PM source apportionment and health effects: 1. Intercomparison of source apportionment results. J. Expo. Sci. Environ. Epidemiol. 2006;16(3):275–286. doi: 10.1038/sj.jea.7500458. [DOI] [PubMed] [Google Scholar]
- 60.Harrison R.M., Yin J. Chemical speciation of PM2.5 particles at urban background and rural sites in the UK atmosphere. J. Environ. Monit. 2010;12(7):1404–1414. doi: 10.1039/c000329h. [DOI] [PubMed] [Google Scholar]
- 61.Strak M., Hoek G., Godri K.J., Gosens I., Mudway I.S., van Oerle R., Spronk H.M., Cassee F.R., Lebret E., Kelly F.J., Harrison R.M., Brunekreef B., Steenhof M., Janssen N.A. Composition of PM affects acute vascular inflammatory and coagulative markers - the RAPTES project. PLoS One. 2013;8(3):e58944. doi: 10.1371/journal.pone.0058944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lough G.C., Schauer J.J., Park J.S., Shafer M.M., Deminter J.T., Weinstein J.P. Emissions of metals associated with motor vehicle roadways. Environ. Sci. Technol. 2005;39(3):826–836. doi: 10.1021/es048715f. [DOI] [PubMed] [Google Scholar]
- 63.Lee S., Russell A.G., Baumann K. Source apportionment of fine particulate matter in the southeastern United States. J. Air Waste Manag. Assoc. 2007;57(9):1123–1135. doi: 10.3155/1047-3289.57.9.1123. [DOI] [PubMed] [Google Scholar]