Abstract
Study Objectives:
To examine the extent to which parent health behaviors and parenting practices are associated with school-age children's sleep duration.
Methods:
We surveyed 790 parents of children, aged 6 to 12 y, who had a body mass index (BMI) ≥ 90th percentile and were participating in a randomized controlled obesity trial. The main exposures were parent sleep duration, screen time and physical activity, parental limits placed on child TV viewing time and TV content, and parents' confidence regarding their ability to help their child get enough sleep. The primary outcome was child sleep duration. We used linear regression models to examine associations of parent behaviors and parenting practices with child sleep duration.
Results:
On average, children slept 9.2 h per night, whereas parents slept 6.9 h. Parents reported having an average of 1.9 h of screen time per day and 0.6 h of physical activity. There were 57.3% of parents who reported feeling very/extremely confident that they could help their child get enough sleep. In adjusted multivariate analyses, child sleep duration was 0.09 h/day (95% confidence interval: 0.03, 0.15) longer for each 1-h increment in parent sleep duration. Additionally, children whose parents reported being very/extremely confident they could help their child get age-appropriate sleep duration slept 0.67 h/day longer (95% confidence interval: 0.54, 0.81) than those whose parents were not/somewhat confident.
Conclusions:
Educating parents about their own sleep health and enhancing parent confidence to help their children get enough sleep are potential areas of intervention to increase child sleep duration.
Citation:
Rea CJ, Smith RL, Taveras EM. Associations of parent health behaviors and parenting practices with sleep duration in overweight and obese children. J Clin Sleep Med 2016;12(11):1493–1498.
Keywords: child sleep, parent confidence, parent health behaviors, parent sleep, parenting practices
INTRODUCTION
There is growing recognition that children in the United States are suffering from insufficient and poor-quality sleep. The 2004 Sleep in America Poll found that 52% of school-aged children were getting less than the recommended amount of sleep.1 Sleep problems affect 30% to 40% of the school-aged population,2,3 and approximately 10% to 18% of school-aged children complain of daytime sleepiness.3,4 Numerous studies have explored the effect of insufficient quantity and quality of sleep on child health. Insufficient sleep has been associated with being overweight and obese,5,6 decreased cognitive functioning and impaired working memory,7,8 and poor school performance.9 Sleep curtailment has also been associated with aggressive behavior,10 hyperactivity,11 and increased injury risk.12 Sleep problems in children are further associated with increased stress in parents.13
Multiple risk factors have been identified for insufficient and poor quality sleep in the pediatric population, including excessive screen time, TV in the bedroom, caffeine consumption, and late bedtime.14,15 Several studies have also examined the influence of family context on child sleep. For example, poor caregiver knowledge regarding healthy sleep habits is associated with negative sleep practices in children.16 Bedtime routines and minimal nighttime interference from parents are also associated with better sleep quality and duration in young children.17,18 Yet few studies have examined the effect of parent health behaviors and parenting practices on sleep duration among school-aged children.
BRIEF SUMMARY
Current Knowledge/Study Rationale: Several child health behaviors have been associated with insufficient sleep, but little is known about the associations of parents' own health behaviors and parenting practices with sleep duration among their school-age children.
Study Impact: Parent sleep duration and confidence in ability to help children get adequate sleep are associated with increased child sleep duration. This study suggests that family-targeted interventions may be an effective approach to increase child sleep duration and thus improve child health outcomes.
The aim of this study was to determine the extent to which parents' health behaviors and parenting practices are associated with their children's sleep duration. We hypothesized that parent health behaviors, including sleep, physical activity, and screen time, as well as limits on TV time and content and increased confidence, would be associated with child sleep duration.
METHODS
Study Design
This study was a cross-sectional analysis of a baseline survey collected as part of the Study of Technology to Accelerate Research (STAR) trial. Details of this obesity intervention have been previously published.19 Child-parent dyads were enrolled in the study between October 2011 and August 2012, and trained research assistants administered a baseline survey to parents over the phone. The study was registered with ClinicalTrials.gov (NCT01537510). Eligibility for the trial included: (1) child aged 6.0–12.9 y at baseline; (2) child's BMI ≥ 90th percentile for age and sex at the baseline well child visit; (3) child had received well child care at the study site pediatric office in the past 15 mo; and (4) at least one parent could communicate in English. Children were excluded if: (1) their sibling had already been enrolled in the study; (2) the family was planning to leave the practice during the study period; (3) the clinician did not think the study was appropriate for the child; or (4) the child had a chronic medical condition that could affect his/her diet or physical activity. In total, 817 parents or guardians completed the baseline survey. The final analysis was limited to the 790 respondents who were parents and who had complete data for the primary outcome (child sleep duration). The institutional review boards of Harvard Pilgrim Health Care and Harvard Vanguard Medical Associates approved the study protocol.
Measures
The STAR baseline survey included 58 questions asking about demographic characteristics, parent and child sleep behaviors, diet, screen time, text messaging, and physical activity. This analysis included questions related to child and parent health behaviors (sleep duration, screen time, physical activity), parental limit-setting on TV time and content, and parents' confidence regarding their ability to help their child get adequate sleep.
Sleep Variables
The primary outcome of interest was child sleep duration. This outcome was derived from the question: “In the past month, on average, how many hours per day does (your child) sleep in a usual 24-h period during the week? And on a weekend?” A weighted average was then used to calculate daily sleep duration. Parents were asked a similar question: “In the past month, how many hours of sleep did you get in an average 24-h period during the week? During the weekend?” Parent sleep duration was calculated in the same manner as child sleep duration, and refers to the parent who responded to the survey. These questions were derived from a previous study examining the health effects of sleep duration.20,21 In addition to quantifying sleep duration for parents and children, parents were asked about their confidence to help their child achieve several health behavior targets, including adequate sleep: “How confident are you that you can help your child get 10 or more hours of sleep per night?” Questions were adapted from a prior study on parent confidence.22 Answers were dichotomized into “extremely/ very confident” and “somewhat/not confident” categories.
Screen Time and Limit-Setting
To determine daily screen time for children, parents were asked how many hours a day their child spent in front of a screen on weekdays and weekends, including (1) watching TV shows; (2) watching DVDs, videos, or movies; (3) playing video or computer games; and (4) on Internet-related activities such as email, iPhone apps, Facebook, or YouTube. Homework-related screen time was not included. This measure was adapted from the National Longitudinal Study of Youth.23 Parents were asked “How much time, either in your home or elsewhere, did you spend watching television, videos, or DVDs on a typical week-day/weekend?” A weighted average was used to estimate daily screen time for the child and the parent who responded to the survey, and high screen time was defined as greater than 2 h per day for both parents and children.24 Parents were also asked whether they limited how much time their child was allowed to watch television, and whether they limited the content of that viewing. Answers were simple “yes” and “no” responses.
Physical Activity
Parents were asked how many hours per week they and their child engaged in light/moderate or vigorous recreational activities or sports during the past month. Walking was addressed in a separate question and was not included in this variable. These questions were modified from the leisure time activity section of the Physical Activity Scale for the Elderly.25 A daily average was then calculated for the child and the parent who responded to the survey. Children with 1 h or more of physical activity per day and parents with 30 min or more of physical activity per day were considered to be receiving an adequate amount. These levels were chosen to approximate national recommended amounts.26
Statistical Analysis
Descriptive statistics were used to describe the study population, including the percentage of subjects in each category for categorical variables, and the means and standard deviations for continuous variables. Unadjusted linear regression was used to examine the associations of each parent factor [parent BMI, limiting TV time, limiting TV content, parent sleep duration, parent screen time (high vs. low), parent physical activity (high vs. low), and parent confidence (high vs. low)] with child sleep duration. Next, we used multivariate linear regression, adjusted for child age, sex, race/ethnicity, and parent education, to examine the association between parent health behaviors and confidence (high vs. low) and child sleep duration. Analyses were conducted using SAS 9.4 software (SAS Institute Inc., Cary, NC).
RESULTS
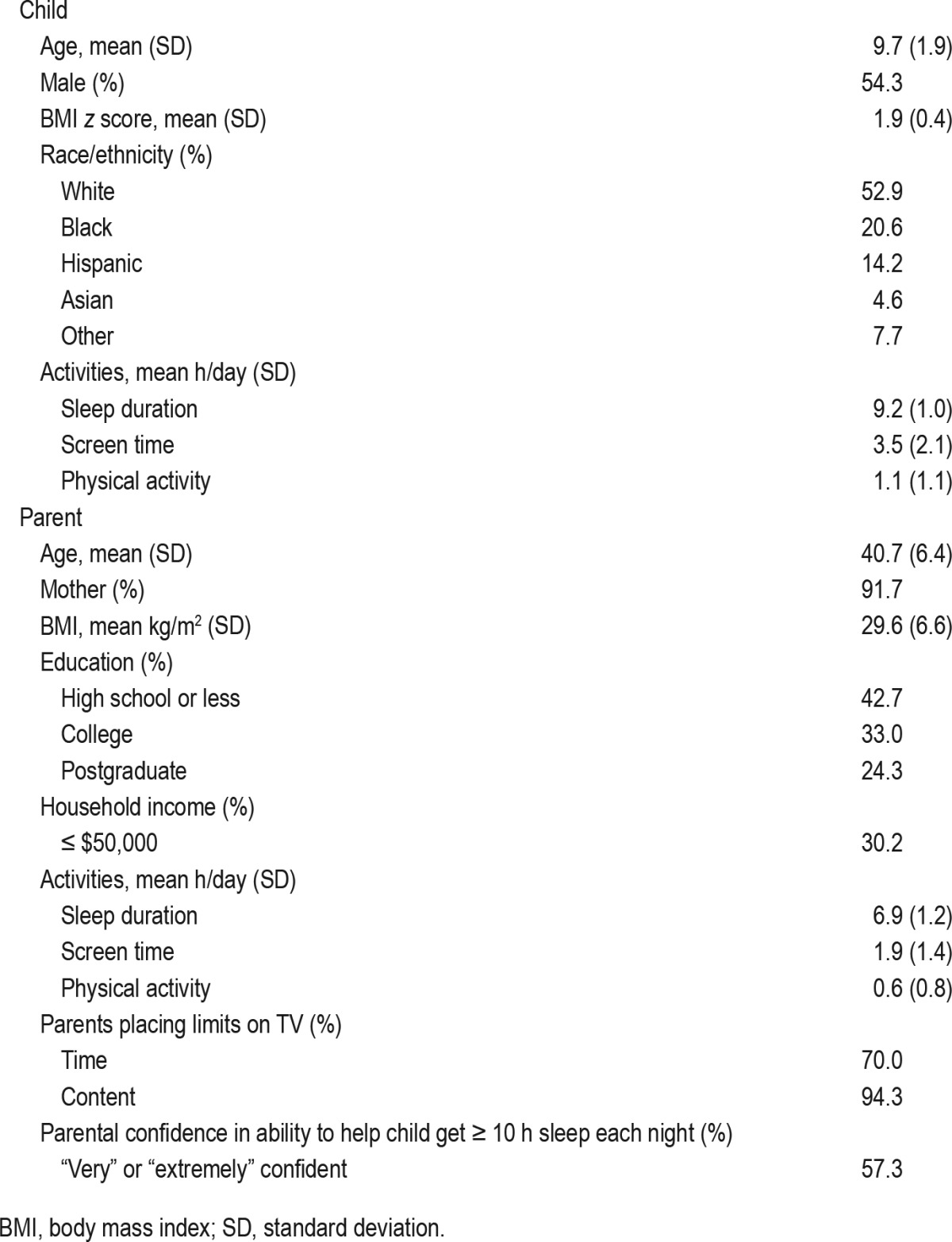
Demographic characteristics of the study population are summarized in Table 1. The majority of respondents were mothers (91.7%). The mean child age was 9.7 y and the mean parent age was 40.7 y. A little over half of the children were male, including 52.9% white, 20.6% black, 14.2% Hispanic, and 4.6% Asian. Over half of parents had a college education or higher (57.3%), and 30.2% of families had a household income less than or equal to $50,000 per year. Average daily sleep duration was 9.2 h for children and 6.9 h for parents. Average daily screen time was 3.5 h for children and 1.9 h for parents. Average daily physical activity was 1.1 h for children and 0.6 h for parents. The majority of parents placed limits on their child's TV viewing, with 70.0% reporting that they limited the amount of time their children spent watching TV and 94.3% reporting they limited TV content. Most parents (57.3%) also stated feeling “very” or “extremely” confident that they could help their child get 10 or more hours of sleep per night.
Table 1.
Characteristics of survey participants (n = 790).
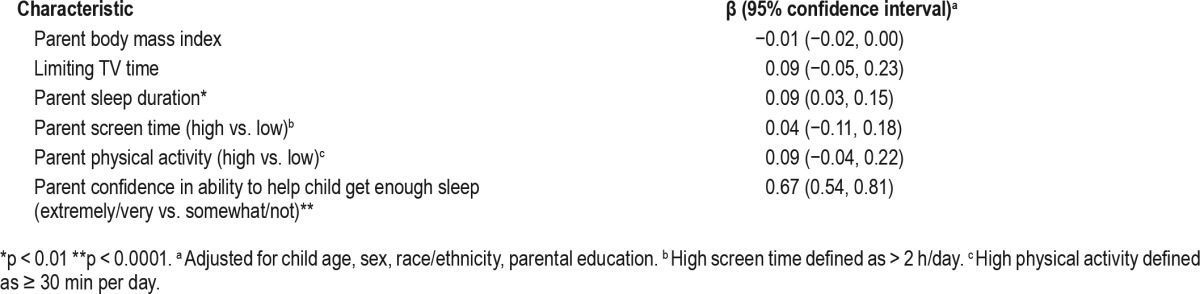
In univariate analysis (Table 2), higher parent BMI and parent screen time were associated with shorter child sleep duration (−0.02 h/day; [95% CI: −0.04, −0.01] and −0.24 h/day; [95% CI: −0.39, −0.08], respectively). In contrast, limiting TV time and parents' report of being very/extremely confident (v. somewhat/ not confident) they could help their child get age-appropriate sleep were associated with longer child sleep duration (0.20 h/day; [95% CI: 0.04, 0.36] and 0.81 h/day; [95% CI: 0.67, 0.94], respectively). Longer parent sleep duration and higher parent physical activity were also associated with longer child sleep duration (0.14 h/day; [95% CI: 0.08, 0.20] and 0.20 h/day; [95% CI: 0.06, 0.35], respectively). In multivariate analysis adjusted for child age, gender, race/ethnicity, and parent education, longer parent sleep duration and higher parent confidence were associated with longer child sleep duration (0.09 h/day; [95% CI: 0.03, 0.15] and 0.67 h/day; [95% CI: 0.54, 0.81], respectively). The associations with parent BMI, limiting TV time, parent screen time, and parent physical activity were attenuated after adjustment and were no longer significant (Table 3).
Table 2.
Univariate relationship of parent behaviors and parenting practices with child sleep duration.
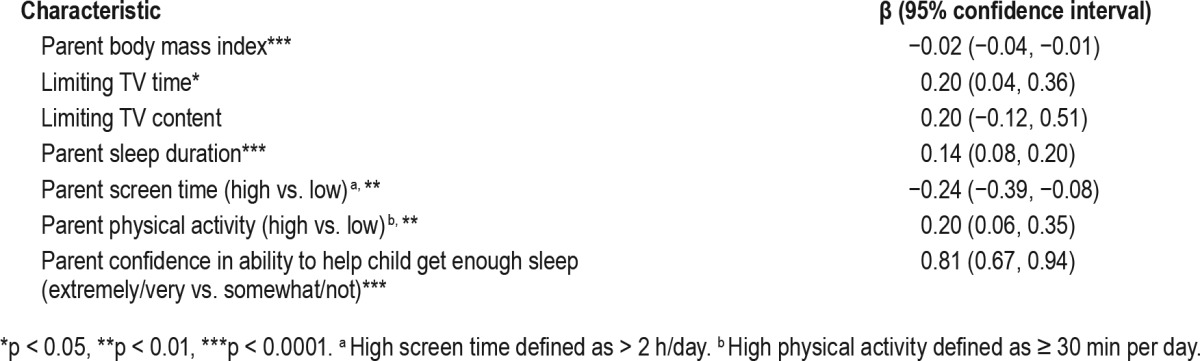
Table 3.
Multivariate-adjusted relationship of parent behaviors and parenting practices with child sleep duration.
DISCUSSION
In this study we found a significant association between parent and child sleep duration. Higher parent confidence in the ability to help children get enough sleep was also associated with increased child sleep duration. In univariate analysis, parent screen time and BMI were associated with shorter child sleep duration, and limiting TV time and higher parent physical activity were associated with increased child sleep duration, but these effects were attenuated after controlling for child age, sex, race/ethnicity, and parent education.
Our findings related to parent sleep duration are consistent with other work linking parent and child health behaviors. Although the effect was modest (each 1-h increase in parent sleep was associated with a 0.09 h/day increase for the child), this daily amount aggregates over time and may represent a clinically important difference. In a study of school-aged children in China, Li et al. found that both maternal and paternal sleep duration of fewer than 6 h were significantly associated with child sleep duration of less than 9 hours.27 Zhang et al. also found an association between child and parent sleep/wake times and time in bed in a school-aged population.28 Another study in Chinese adolescents found correlations between sleep/ wake patterns, sleep quality, and insomnia in children and parents.29 There are a number of possible mediators for the association between parent and child sleep duration. Parents may be influencing child sleep duration by serving as role models for their children or by encouraging and supporting their child's healthy choices. Parent-child sleep may also be directly linked through co-sleeping or a family bedtime. There may also be genetic factors unrelated to parent values or health habits.30 Finally, it is possible that rather than parents' behaviors influencing their children, children who experience short or poor quality sleep may detrimentally affect their parents' sleep.31 Unfortunately, our cross-sectional study design does not allow us to infer causality.
Our study further associated parent confidence in the ability to help children get enough sleep with increased child sleep duration. Social cognitive theory suggests that people with high levels of confidence, or self-efficacy, are more likely to change a health behavior than those with low levels of confidence.32 Several studies have found associations between parents' confidence in their ability to influence their children's behaviors and the behaviors themselves. Child screen time, physical activity,33 diet,22 and performance in weight loss interventions34 have all been associated with parent confidence. It is understandable that parents whose children already get 10 or more hours of sleep each night would feel confident in their ability to help them get enough sleep, but it is interesting to note that although 57.3% of parents said they were “very” or “extremely” confident in their ability to help their child get 10 or more hours of sleep per night, only 28.6% of children had met that recommendation. In future work it will be important to examine whether parent confidence is a predictive factor in children's ability to increase their sleep duration.
Previous work has demonstrated an association between parent and child screen time, and multiple studies have shown that screen time negatively affects sleep duration.35 However, although both parent screen time and limiting TV time were associated with child sleep duration in univariate analysis, these associations were no longer significant after controlling for demographic characteristics. Results are mixed regarding the effect of physical activity on sleep duration and quality.36,37 Similar to our findings for parent screen time, the association between parent physical activity and child sleep was no longer significant after adjustment. Our survey relied on parent self-report, and our findings may be limited by recall and social desirability bias. However, these results may also suggest that individual parent behaviors do not reflect a comprehensive “family lifestyle,” but rather that parent sleep is directly linked to child sleep irrespective of other health behaviors.
Most sleep interventions for children have targeted infant and toddler sleep patterns or specific sleep disorders rather than focusing on increasing sleep duration among school-aged children.38 The majority of large-scale sleep interventions are also school-based and rarely involve parent education or behavior modification strategies. Furthermore, although these interventions are usually successful at increasing sleep knowledge, they rarely change sleep behavior.39,40 Our study suggests that educating parents about their sleep health and promoting increased confidence in their ability to help their children get enough sleep are potential areas of intervention to increase child sleep duration. Further study is needed to clarify the relationship between parent sleep and confidence and child sleep duration.
Limitations
Although the sample size in our dataset is large, the cross-sectional design limits our ability to draw conclusions about causality. The survey also relied on parent self-report, which may not reflect parent and child behaviors with complete accuracy. In particular, studies have shown only moderate correlation between self-reported and objectively measured sleep.41 The sample also consisted of predominantly middle-income, white, English-speaking families, and thus may not be generalizable to other populations. Finally, as this study was designed as an obesity intervention, all children in the sample had a BMI ≥ 90th percentile. Given the complex association of sleep and obesity, it is possible that the relationships between parent sleep duration and parent confidence and child sleep duration would be different in a nonobese population. Specifically, obesity is a risk factor for developing sleep-disordered breathing, including obstructive sleep apnea syndrome, thus our population may have had a higher rate of sleep-disordered breathing than a normal weight population.42 Furthermore, the mean parent BMI of our sample was elevated at 29.6 (6.6), which may have affected parent sleep duration.43,44
CONCLUSIONS
Our results demonstrate that parent sleep duration and parent confidence are associated with child sleep duration among overweight and obese children. These findings suggest that a family-based intervention model may be an appropriate way to address insufficient child sleep and thus improve child health outcomes. Given the adverse effects of insufficient sleep on child health, it is critical to identify modifiable risk factors that could be the targets for intervention. Further study should focus on clarifying the relationship between parent and child sleep to determine how parent sleep influences child sleep duration. It will also be important to determine whether parent confidence can predict an improvement in child sleep over time, or whether it is merely a reflection of current child sleep status.
DISCLOSURE STATEMENT
This was not an industry supported study. This study was supported by the American Recovery and Reinvestment Act (award R 18 AE000026, Dr. Elsie M. Taveras) and by the NIH/NIDDK (K24DK105989, Dr. Elsie M. Taveras). The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors are grateful to the children and families who participated in this study, the Harvard Vanguard Medical Associates health care providers and clinical sites, and the STAR research staff.
REFERENCES
- 1.2004 Children and Sleep - National Sleep Foundation. [Accessed May 14, 2015]. Available at: http://sleepfoundation.org/sleep-polls-data/sleep-in-america-poll/2004-children-and-sleep.
- 2.Fricke-Oerkermann L, Plück J, Schredl M, et al. Prevalence and course of sleep problems in childhood. Sleep. 2007;30:1371–7. doi: 10.1093/sleep/30.10.1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Owens JA, Spirito A, McGuinn M, et al. Sleep habits and sleep disturbance in elementary school-aged children. J Dev Behav Pediatr. 2000;21:27–36. doi: 10.1097/00004703-200002000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Stein MA, Mendelsohn J, Obermeyer WH, et al. Sleep and behavior problems in school-aged children. Pediatrics. 2001;107:E60. doi: 10.1542/peds.107.4.e60. [DOI] [PubMed] [Google Scholar]
- 5.Nixon GM, Thompson JMD, Han DY, et al. Short sleep duration in middle childhood: risk factors and consequences. Sleep. 2008;31:71–8. doi: 10.1093/sleep/31.1.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lumeng JC, Somashekar D, Appugliese D, et al. Shorter sleep duration is associated with increased risk for being overweight at ages 9 to 12 years. Pediatrics. 2007;120:1020–9. doi: 10.1542/peds.2006-3295. [DOI] [PubMed] [Google Scholar]
- 7.Steenari M-R, Vuontela V, Paavonen EJ, et al. Working memory and sleep in 6- to 13-year-old schoolchildren. J Am Acad Child Adolesc Psychiatry. 2003;42:85–92. doi: 10.1097/00004583-200301000-00014. [DOI] [PubMed] [Google Scholar]
- 8.Sadeh A, Gruber R, Raviv A. Sleep, neurobehavioral functioning, and behavior problems in school-age children. Child Dev. 73:405–17. doi: 10.1111/1467-8624.00414. [DOI] [PubMed] [Google Scholar]
- 9.Wolfson AR, Carskadon MA. Sleep schedules and daytime functioning in adolescents. Child Dev. 1998;69:875–87. [PubMed] [Google Scholar]
- 10.Aronen ET, Paavonen EJ, Fjällberg M, et al. Sleep and psychiatric symptoms in school-age children. J Am Acad Child Adolesc Psychiatry. 2000;39:502–8. doi: 10.1097/00004583-200004000-00020. [DOI] [PubMed] [Google Scholar]
- 11.Touchette E, Côté SM, Petit D, et al. Short nighttime sleep-duration and hyperactivity trajectories in early childhood. Pediatrics. 2009;124:e985–93. doi: 10.1542/peds.2008-2005. [DOI] [PubMed] [Google Scholar]
- 12.Boto LR, Crispim JN, de Melo IS, et al. Sleep deprivation and accidental fall risk in children. Sleep Med. 2012;13:88–95. doi: 10.1016/j.sleep.2011.04.010. [DOI] [PubMed] [Google Scholar]
- 13.Byars KC, Yeomans-Maldonado G, Noll JG. Parental functioning and pediatric sleep disturbance: an examination of factors associated with parenting stress in children clinically referred for evaluation of insomnia. Sleep Med. 2011;12:898–905. doi: 10.1016/j.sleep.2011.05.002. [DOI] [PubMed] [Google Scholar]
- 14.Garrison MM, Liekweg K, Christakis DA. Media use and child sleep: the impact of content, timing, and environment. Pediatrics. 2011;128:29–35. doi: 10.1542/peds.2010-3304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mindell JA, Meltzer LJ, Carskadon MA, et al. Developmental aspects of sleep hygiene: findings from the 2004 National Sleep Foundation Sleep in America Poll. Sleep Med. 2009;10:771–9. doi: 10.1016/j.sleep.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 16.Owens JA, Jones C. Parental knowledge of healthy sleep in young children: results of a primary care clinic survey. J Dev Behav Pediatr. 32:447–53. doi: 10.1097/DBP.0b013e31821bd20b. [DOI] [PubMed] [Google Scholar]
- 17.Sheridan A, Murray L, Cooper PJ, et al. A longitudinal study of child sleep in high and low risk families: relationship to early maternal settling strategies and child psychological functioning. Sleep Med. 2013;14:266–73. doi: 10.1016/j.sleep.2012.11.006. [DOI] [PubMed] [Google Scholar]
- 18.Mindell JA, Li AM, Sadeh A, et al. Bedtime routines for young children: a dose-dependent association with sleep outcomes. Sleep. 2015;38:717–22. doi: 10.5665/sleep.4662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Taveras EM, Marshall R, Horan CM, et al. Rationale and design of the STAR randomized controlled trial to accelerate adoption of childhood obesity comparative effectiveness research. Contemp Clin Trials. 2013;34:101–8. doi: 10.1016/j.cct.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 20.Taveras EM, Rifas-Shiman SL, Rich-Edwards JW, et al. Association of maternal short sleep duration with adiposity and cardiometabolic status at 3 years postpartum. Obesity. 2011;19:171–8. doi: 10.1038/oby.2010.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Taveras EM, Rifas-Shiman SL, Oken E, et al. Short sleep duration in infancy and risk of childhood overweight. Arch Pediatr Adolesc Med. 2008;162:305–11. doi: 10.1001/archpedi.162.4.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Taveras EM, Mitchell K, Gortmaker SL. Parental confidence in making overweight-related behavior changes. Pediatrics. 2009;124:151–8. doi: 10.1542/peds.2008-2892. [DOI] [PubMed] [Google Scholar]
- 23.Baker PC, Keck CK, Mott FL, Quinlan SV. A Guide to the 1986-1990 National Longitudinal Survey of Youth Child Data. Columbus, OH: Center for Human Resource Research, Ohio State University; 1993. NLSY Child Handbook-Revised Edition. [Google Scholar]
- 24.Policy Statement: Council on Communications and Media. Children, adolescents, and the media. Pediatrics. 2013;132:958–61. doi: 10.1542/peds.2013-2656. doi: 10.1542/peds.2013-2656. [DOI] [PubMed] [Google Scholar]
- 25.Washburn RA, Smith KW, Jette AM, et al. The Physical Activity Scale for the Elderly (PASE): development and evaluation. J Clin Epidemiol. 1993;46:153–62. doi: 10.1016/0895-4356(93)90053-4. [DOI] [PubMed] [Google Scholar]
- 26.2008 Physical Activity Guidelines for Americans: Index. [Accessed May 14, 2015]. Available at: http://www.health.gov/paguidelines/guidelines/
- 27.Li S, Zhu S, Jin X, et al. Risk factors associated with short sleep duration among Chinese school-aged children. Sleep Med. 2010;11:907–16. doi: 10.1016/j.sleep.2010.03.018. [DOI] [PubMed] [Google Scholar]
- 28.Zhang J, Li AM, Fok TF, et al. Roles of parental sleep/wake patterns, socioeconomic status, and daytime activities in the sleep/wake patterns of children. J Pediatr. 2010;156:606–12.e5. doi: 10.1016/j.jpeds.2009.10.036. [DOI] [PubMed] [Google Scholar]
- 29.Liu X, Zhao Z, Jia C, et al. Sleep patterns and problems among chinese adolescents. Pediatrics. 2008;121:1165–73. doi: 10.1542/peds.2007-1464. [DOI] [PubMed] [Google Scholar]
- 30.Dauvilliers Y, Maret S, Tafti M. Genetics of normal and pathological sleep in humans. Sleep Med Rev. 2005;9:91–100. doi: 10.1016/j.smrv.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 31.Hagen EW, Mirer AG, Palta M, et al. The sleep-time cost of parenting: sleep duration and sleepiness among employed parents in the Wisconsin Sleep Cohort Study. Am J Epidemiol. 2013;177:394–401. doi: 10.1093/aje/kws246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31:143–64. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 33.Smith BJ, Grunseit A, Hardy LL, et al. Parental influences on child physical activity and screen viewing time: a population based study. BMC Public Health. 2010;10:593. doi: 10.1186/1471-2458-10-593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gunnarsdottir T, Njardvik U, Olafsdottir AS, et al. The role of parental motivation in family-based treatment for childhood obesity. Obesity. 2011;19:1654–62. doi: 10.1038/oby.2011.59. [DOI] [PubMed] [Google Scholar]
- 35.Falbe J, Davison KK, Franckle RL, et al. Sleep duration, restfulness, and screens in the sleep environment. Pediatrics. 2015;135:e367–75. doi: 10.1542/peds.2014-2306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ortega FB, Ruiz JR, Labayen I, et al. Sleep duration and activity levels in Estonian and Swedish children and adolescents. Eur J Appl Physiol. 2011;111:2615–23. doi: 10.1007/s00421-011-1883-6. [DOI] [PubMed] [Google Scholar]
- 37.Stone MR, Stevens D, Faulkner GEJ. Maintaining recommended sleep throughout the week is associated with increased physical activity in children. Prev Med (Baltim) 2013;56:112–7. doi: 10.1016/j.ypmed.2012.11.015. [DOI] [PubMed] [Google Scholar]
- 38.Owens LJ, France KG, Wiggs L. Behavioural and cognitive-behavioural interventions for sleep disorders in infants and children: a review. Sleep Med Rev. 1999;3:281–302. doi: 10.1053/smrv.1999.0082. [DOI] [PubMed] [Google Scholar]
- 39.Blunden SL, Chapman J, Rigney GA. Are sleep education programs successful? The case for improved and consistent research efforts. Sleep Med Rev. 2012;16:355–70. doi: 10.1016/j.smrv.2011.08.002. [DOI] [PubMed] [Google Scholar]
- 40.Cassoff J, Knäuper B, Michaelsen S, et al. School-based sleep promotion programs: effectiveness, feasibility and insights for future research. Sleep Med Rev. 2013;17:207–14. doi: 10.1016/j.smrv.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 41.Lauderdale DS, Knutson KL, Yan LL, et al. Self-reported and measured sleep duration: how similar are they? Epidemiology. 2008;19:838–45. doi: 10.1097/EDE.0b013e318187a7b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Verhulst SL, Van Gaal L, De Backer W, et al. The prevalence, anatomical correlates and treatment of sleep-disordered breathing in obese children and adolescents. Sleep Med Rev. 2008;12:339–46. doi: 10.1016/j.smrv.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 43.Patel SR. Reduced sleep as an obesity risk factor. Obes Rev. 2009;10(Suppl 2):61–8. doi: 10.1111/j.1467-789X.2009.00664.x. [DOI] [PubMed] [Google Scholar]
- 44.Taheri S, Lin L, Austin D, et al. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004;1:e62. doi: 10.1371/journal.pmed.0010062. [DOI] [PMC free article] [PubMed] [Google Scholar]


