Abstract
Study Objectives:
Drugs and psychoactive substances can cause sleepiness and when undetected, may lead to over diagnosis of central hypersomnias. We performed urine drug testing using gas chromatography-mass spectrometry in adults undergoing multiple sleep latency testing (MSLT) for a suspected central hypersomnia. We examined how the drug test results modified the treating physician's diagnosis.
Methods:
One hundred eighty-six consecutive patients with a suspected central hypersomnia who underwent clinical assessment, MSLT and urine drug testing by gas chromatography-mass spectrometry were retrospectively studied. Physicians made a diagnosis after clinical assessment and MSLT and were initially blinded to the urine drug test results.
Results:
A third of patients assessed for subjective hypersomnia had a positive urine drug test for a substance affecting sleep. Opioids, cannabis, and amphetamines were the commonest drugs detected. Using MSLT, 35 (18.8%) of 186 patients had objective hypersomnia that may have been due to a drug or substance. Drugs or substances may have confounded the MSLT in 11 (20.1%) of 53 patients who fulfilled diagnostic criteria for idiopathic hypersomnia, and 12 (52%) of 23 of those who fulfilled diagnostic criteria for narcolepsy without cataplexy. Of the 75 positive urine drug samples, 61 (81%) were substances or medications not revealed in the physician interview. The treating physician had not suspected drugs or substances as a possible cause of objective hypersomnia in 34 (97%) of the 35 patients.
Conclusions:
Drugs and psychoactive substances can confound the results of the MSLT and when undetected could lead to over diagnosis of central hypersomnias.
Citation:
Kosky CA, Bonakis A, Yogendran A, Hettiarachchi G, Dargan PI, Williams AJ. Urine toxicology in adults evaluated for a central hypersomnia and how the results modify the physician's diagnosis. J Clin Sleep Med 2016;12(11):1499–1505.
Keywords: adults, narcolepsy, hypersomnolence, idiopathic, disorders of excessive somnolence, polysomnography, amphetamines, opioid, cannabis, gas chromatography-mass spectrometry
INTRODUCTION
Excessive daytime sleepiness is defined as an inability to stay awake and alert during the major waking period of the day that persists for at least three months.1 The prevalence of excessive daytime sleepiness in the general population has been found to be 15% in Europe and 19.5% in America.2,3 Important causes of excessive daytime sleepiness are insufficient sleep, sleep disordered breathing, circadian rhythm disorders, and central hypersomnias such as narcolepsy. Drugs and illicit psychoactive substances can also cause excessive daytime sleepiness, but maybe difficult to detect without drug testing.1 Failure to detect a drug causing sleepiness may result in significant harm; the patient maybe incorrectly diagnosed with narcolepsy or idiopathic hypersomnia and inappropriately prescribed stimulants.
BRIEF SUMMARY
Current Knowledge/Study Rationale: Drugs and substances have been shown to cause hypersomnia, but little is known about their effects in patients being evaluated for excessive daytime sleepiness. In this study urine drug testing by gas chromatography-mass spectrometry was performed in adult patients undergoing clinical assessment and a multiple sleep latency test (MSLT) for a suspected central hypersomnia.
Study Impact: The study found drugs and substances are frequent among patients being evaluated for hypersomnia and if undetected, may confound the MSLT results and the physician's diagnosis. The results of this study support routine drug testing of patients undergoing assessment for a central hypersomnia.
Drugs and psychoactive substances can affect objective tests of sleepiness such as the multiple sleep latency test (MSLT). The MSLT is used in combination with clinical assessment to diagnose narcolepsy and idiopathic hypersomnia.1 False positive results for narcolepsy based on MSLT criteria have been found in adolescent patients whose urine tested positive for tetrahydrocannabinol.5 It has been recommended that patients undergoing MSLT for hypersomnia have urine drug testing.6 However, it is estimated that only 17% of European sleep laboratories routinely perform urine drug testing in patients undergoing MSLT.7 Moreover, many sleep laboratories that undertake drug screening use urine immunoassay testing which is less specific and less accurate in detecting drugs and psychoactive substances than specific, targeted analysis with techniques such as gas chromatography-mass spectrometry.8
We undertook a study of urine drug testing using analysis by gas chromatography-mass spectrometry in adult patients undergoing MSLT for excessive daytime sleepiness. Our aim was to examine the frequency and type of drugs detected, and how the results of the urine drug test modified the treating physician's diagnosis.
METHODS
We performed a retrospective study of consecutive patients who underwent a diagnostic MSLT for a suspected central hypersomnia. The study was performed at a tertiary sleep disorders center in London from July 2005 to December 2007. Data were gathered using the departmental database, electronic records and case notes. Patients were excluded if the MSLT was incomplete, if they did not provide a urine specimen or if the patient's notes could not be obtained.
Clinical Evaluation
An experienced sleep physician assessed the patient prior to the MSLT. The physician took a detailed history, including a list of medications, and examined the patient. An MSLT was ordered if narcolepsy or idiopathic hypersomnia was suspected. Patients were also included if they had an MSLT performed for persistent sleepiness in spite of adequate treatment of obstructive sleep apnea with continuous positive airway pressure or a mandibular advancement device.
The urine drug tests were collected at the time of the MSLT and results were not available for about 2 weeks as they underwent processing in the toxicology laboratory. Sleep physicians were asked to give a provisional diagnosis at the end of the MSLT without the knowledge of urine drug tests results. The diagnosis was based upon clinical assessments before and after the sleep study and the MSLT findings, using the International Classification of Sleep Disorders criteria.4 Patients were followed-up between 2 and 6 weeks later at which stage the urine test results were available. The same physician was used throughout the clinical process but occasionally this was not possible.
Multiple Sleep Latency Testing
Nocturnal polysomnography was performed followed by MSLT according to standard guidelines and were scored by an experienced polysomnographic technologist.9–11 For the MSLT, patients undertook 4 or 5 naps under standard conditions at 2-h intervals on the day following nocturnal polysomnography. Each nap was 20 min long, extended for 15 min if one epoch of sleep was observed.
Two weeks prior to testing patients were advised to standardize sleep-wake cycles, complete sleep diaries and/or actigraphy. Patients were advised to discontinue medications known to affect sleep and REM latency. This included opioids, amphetamines, antidepressants, benzodiazepines, antipsychotics, and sedating antihistamines. Antidepressants or antipsychotics were continued if the treating physician thought there was a significant risk of suicide or relapse of mental illness.
Urine Drug Screening Tests
A plain urine sample was collected on the evening of the nocturnal polysomnography. Samples were analyzed by gas chromatography-mass spectrometry (GC-MS) allowing screening for over 1,000 pharmaceutical and illicit/recreational drugs.12 In this study we recorded drugs known to significantly affect sleep including opioids, amphetamines, antidepressants, benzodiazepines, antipsychotics, and sedating antihistamines.
Statistics
Independent sample t-tests (and Wilcoxon-Mann-Whitney tests where appropriate) were used to investigate the differences between groups. Chi-square statistics (and Fisher tests where appropriate) were used to investigate the distribution of proportions between categorical variables. Univariate and multivariate binary exact logistic regression was conducted. Odds ratios, 95% confidence intervals, and p values were obtained for the final models. Data were analyzed using the R environment for statistical computing.13
RESULTS
Patient Characteristics
A total of 234 consecutive patients with a suspected central disorder of hypersomnia underwent physician evaluation and MSLT in the 30-month study period. Forty-eight patients were excluded from the study because 23 had incomplete records, 16 patients did not provide urine samples for drug testing, and in 9 there was no record of follow-up.
A total of 186 patients were included in the study. There were 111 females and 75 males. The mean age of patients was 38.6 years (standard deviation 13.4 years). The mean body mass index was 28.8 kg/m2 (standard deviation 7.6 kg/m2).
We found no statistical differences between patients included and excluded from this study when comparing age, body mass index, proportion of females, and Epworth Sleepiness Scale score.
Clinical Evaluation before MSLT
An experienced sleep physician assessed patients before the overnight polysomnography and MSLT. The physician applied standardized diagnostic criteria based on the patient's symptoms.4 Patients were suspected to have narcolepsy without cataplexy (narcolepsy type 2) if they had hypersomnia, absence of typical cataplexy and at least one other symptom of narcolepsy. Symptoms of narcolepsy included sleep paralysis, hypnogogic or hypnopompic hallucinations, rapid onset vivid dreams, or dream enactment. Patients were suspected to have idiopathic hypersomnia if they had hypersomnia with no other symptoms to suggest narcolepsy.
Of the 186 patients with a suspected central disorder of hypersomnolence, 125 patients were thought to have idiopathic or an unclassifiable hypersomnia, 33 patients were suspected of having narcolepsy without cataplexy (narcolepsy type 2), 3 patients were thought to have narcolepsy with cataplexy (narcolepsy type 1), and 3 patients were suspected of having hypersomnia due to a medication or substance. In addition, 25 patients had persistent sleepiness despite adequately treated obstructive sleep apnea. The mean Epworth Sleepiness Scale score was 15.6 (SD 4.3).
Overnight Polysomnograph and MSLT
Results from 186 patients overnight polysomnographs showed a mean total sleep time of 408.1 minutes (SD 81.3 min), apnea hypopnea index of 2.3/h (standard deviation 5.2/h), and periodic limb movement index of 3.8 h (standard deviation 10/h). Results from of the MSLT were a mean sleep latency of 8.1 min (SD 5.1 min). One hundred twelve patients had a sleep latency ≤ 8 minutes. Thirty-two patients had ≥ 2 naps that contained sleep onset REM sleep epochs. Twenty-six patients had both a sleep latency ≤ 8 min and ≥ 2 naps containing sleep onset REM.
Clinical Evaluation after the MSLT without Urine Drug Test Results
Physicians made a diagnosis following the MSLT without urine drug results being available. Of 186 patients, 73 were classified as normal, 53 were diagnosed with idiopathic hypersomnia, 23 with narcolepsy without cataplexy, 13 with OSA persistent sleepiness, 9 with periodic limb movement disorder, 4 with behaviorally induced inadequate sleep syndrome (BISS), 3 with narcolepsy with cataplexy, 3 with drug related hypersomnia, 2 with phase delay, 2 with upper airways resistance syndrome, and 1 with depression.
Urine Drug Test Results
Of the 186 participants, 62 (33%) patients had positive urine drug test for a drug known to effect sleep. Fifty patients were positive for a single drug, 10 patients had 2 drugs detected, and 2 patients had 3 drugs detected. Patients excluded from the study had the same proportion of positive urine drug tests as those that were included (both groups 33%, p = 0.98).
Of the 75 positive urine drug samples, 46 (61%) were illicit substances or prescribed substances not revealed in the physician interview, 15 (20%) were over-the-counter medications not revealed in the physician interview and 14 (19%) were prescribed medications that could not be stopped for the MSLT. Medications available over the counter in the United Kingdom and detected in this study were codeine and the sedating antihistamines.
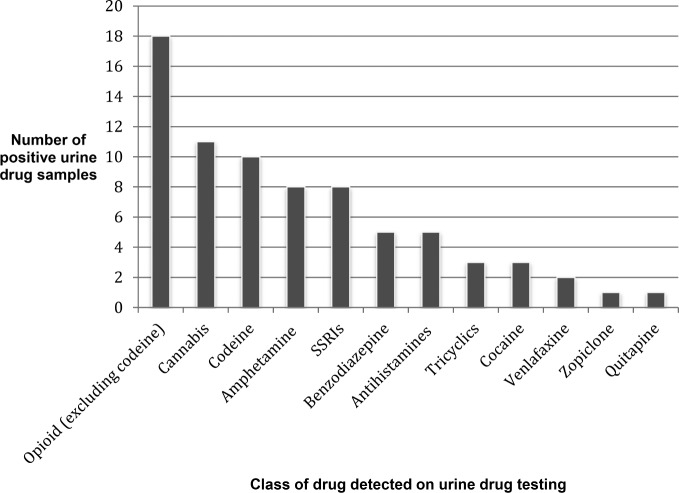
Opioids and cannabis were the commonest drugs detected by urine testing (Figure 1). Of the 28 samples positive for opioids, 10 were for codeine. Stimulants were also commonly detected, with 11 patients positive for amphetamines or cocaine.
Figure 1. Frequency of positive urine drug test results by class of drug in 186 patients undergoing evaluation for excessive daytime sleepiness.
Drug classes include opioids, cannabis, amphetamines, serotonin reuptake inhibitors (SSRIs).
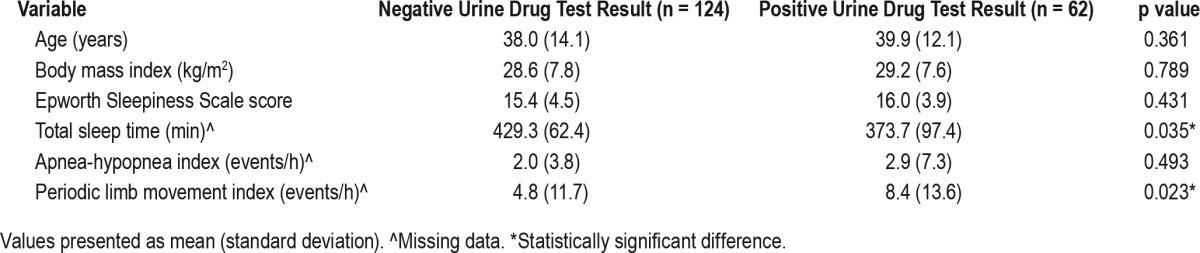
We compared patients who were drug positive and those that were drug negative (Table 1). There were no significant differences in age, body mass index, and Epworth Sleepiness Scale score between patients who were urine drug positive compared to those who were urine drug negative. The proportion of sexes was not statistically different between the 2 groups (p value = 0.75). Patients who were urine drug positive had a lower total sleep time compared to urine drug negative patients, with a difference in means of 56 minutes (p = 0.035). There was a statistical difference in periodic limb movement index between urine drug test positive and urine drug test negative (8.4 vs 4.8 periodic limb movements per hour, respectively, p = 0.02).
Table 1.
Characteristics of patients undergoing evaluation for excessive daytime sleepiness separated by overall urine test result
Three patients had suspected drug-induced hypersomnia prior to the MSLT. One patient was positive for cannabis however their mean sleep latency test was in the normal range (11 min). One patient stopped the quetiapine and sodium valproate prior to the MSLT with resolution of symptoms but an abnormal MSLT (6.5 min). The third patient was positive for an SSRI and was objectively sleepy (4.3 min).
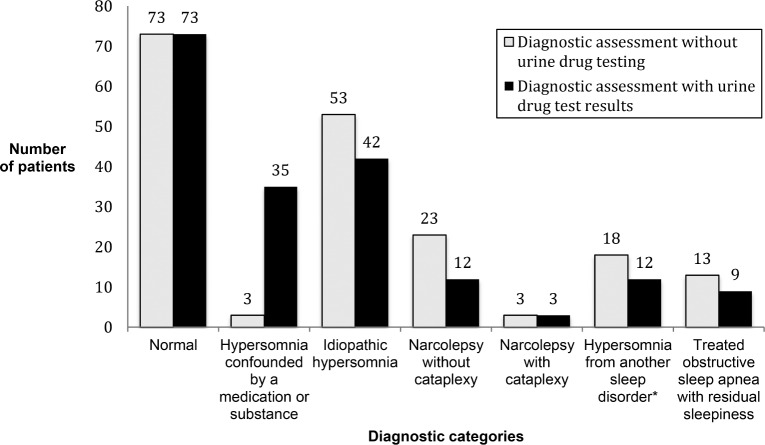
Effect of Urine Drug Testing on Modifying the Physician's Diagnosis
Of 186 patients studied, 62 (33%) had subjective hypersomnia that could have been due to a drug or psychoactive substance. Using the MSLT, 35 (18.8%) patients had objective hypersomnia that may have been due to a drug or substance. Objective hypersomnia was defined as a mean sleep latency ≤ 8 min, with ≥ 6 h total sleep time on polysomnograph the preceding night. When urine drug results were not available, physicians did not suspect that the objective hypersomnia was due to a medication or substance (Figure 2). Prior to the urine drug results being known, the treating physician had not suspected that a psychoactive substance maybe contributing to hyper-somnia in 34 (97%) of the 35 patients. Drugs detected in those patients with objective hypersomnia were; opioids (17 patients), cannabis (6 patients), amphetamine (6 patients), cocaine (3 patients), benzodiazepines (2 patients), SSRI (1 patient), sedating antihistamine (1 patient), and quetiapine (1 patient). Two patients had a positive urine drug test for 2 drugs
Figure 2. Compares the physician's diagnosis made without and with the urine drug test results in 186 patients undergoing a multiple sleep latency test for hypersomnia.
*Patients included: periodic limb movement disorder (n = 9), behaviorally induced insufficient sleep syndrome (n = 4), upper airway resistance syndrome (n = 2), circadian rhythm sleep wake disorder (n = 2), depression (n = 1).
In patients diagnosed with idiopathic hypersomnia based on physician and MSLT assessment alone, 11 (20.7%) of 53 patients had a positive urine drug test. Drugs detected were opioids (4 patients), cannabis (3 patients), benzodiazepine (1 patient), cocaine (1 patient), and sedating antihistamine (1 patient).
In patients diagnosed with narcolepsy without cataplexy based on physician and MSLT assessment alone, 12 (52.2%) of 23 patients had a positive urine drug test. Drugs detected were opioids (6 patients), amphetamines (3 patients), cocaine (2 patients), and cannabis (1 patient). Patients who tested positive for amphetamines and cocaine were more likely to have a clinical diagnosis of narcolepsy compared to those patients who were urine negative (odds ratio 12.5, 95% CI 2.5–62.0, p value 0.002, multivariate logistical regression). We found no difference in the frequency of narcolepsy in those patients who were urine positive for opioids (p value = 0.18) or cannabis (p value = 0.5) compared to those patients with a negative urine test.
In the 13 patients with obstructive sleep apnea who complained of persistent sleepiness despite treatment, 4 (30.7%) had a positive urine drug test. Drugs detected were opioids (3 patients) and cannabis (1 patient).
DISCUSSION
We found a third of patients undergoing MSLT for excessive daytime sleepiness had a positive urine drug test for a substance affecting sleep. Opioids, cannabis, and amphetamines were the commonest drugs detected. Thirty-five (18.8%) of 186 patients had objective hypersomnia that may have been due to a drug or substance. Patients with persistent sleepiness despite controlled obstructive sleep apnea were also frequently drug positive. We found that physicians rarely suspected that a substance could be responsible for a patients' sleepiness. The majority of the substances detected by urine drug testing were not identified in the physician interview. The substances were illicit, prescribed but not revealed in the interview or were over the counter medications. In the United Kingdom, sedating antihistamines and codeine are available over the counter. Had the physician known the urine drug results prior to ordering an MSLT, we estimate approximately 25% of the MSLTs could have been avoided.
We have found that the effects of drugs can confound the diagnosis of sleep disorders that rely on the MSLT as part of the diagnostic criteria. The diagnosis of narcolepsy without cataplexy and Idiopathic hypersomnia are based upon clinical assessment and MSLT values.1,4 The MSLT criteria for narcolepsy without cataplexy is a mean sleep latency of less than or equal to 8 minutes and 2 or more naps containing sleep onset REM sleep. The MSLT criteria for idiopathic hypersomnia is a mean sleep latency of less than or equal to 8 minutes and fewer than 2 naps containing sleep onset REM sleep. The MSLT findings must not be better explained by the effect of a medication or substance or their withdrawal.4 In this study, 24.5% patients who fulfilled the diagnostic criteria for idiopathic hypersomnia had a urine positive for a drug known to cause sleepiness with use or withdrawal. In those patients who met the diagnostic criteria for narcolepsy without cataplexy, 52% had urine drug results that could cause sleepiness or alter REM sleep. A positive urine test confounds the diagnosis for idiopathic hypersomnia or narcolepsy without cataplexy because the substance detected might also explain the MSLT results.
Drugs screened for in this study have been shown to alter sleep or REM sleep latencies and may therefore affect the MSLT. Reduced sleep latency or hypersomnolence has been reported with the use of cannabis, most tricyclic anti-depressants, most antipsychotics, opioids, benzodiazepines, first-generation antihistamines, and withdrawal from cocaine and amphetamines.14–18 REM sleep rebound can occur with withdrawal from cannabis, benzodiazepine, cocaine, tricyclic antidepressants, and SSRIs.14–21 Drug effects on sleep architecture may therefore make the MSLT difficult to interpret in those patients with hypersomnia and a positive drug test.
Other investigators have also found that a positive urine drug test confounds the diagnosis of narcolepsy and idiopathic hypersomnia. Dzodzomenyo et al. performed immunoassay urine drug testing in 383 adolescents who had a MSLT.5 The authors found 14 patients had urine positive for tetrahydrocannabinol (THC). A significantly higher number of those with urine positive for THC had MSLT findings consistent with narcolepsy compared to those that were urine negative. The authors suggested marijuana use or withdrawal might be associated with a false positive on MSLT. We did not find this association, however only one patient in our study was positive for cannabis also fulfilled diagnostic criteria for narcolepsy. We found patients who tested positive for amphetamines and cocaine were more likely to have a clinical diagnosis of narcolepsy than those patients who were urine negative. This may be explained by patients with narcolepsy self-medicating with stimulants. Alternatively, withdrawal from amphetamines and cocaine in normal patients may have resulted in a positive MSLT for narcolepsy. In another study reported in abstract by Anniss et al., immunoassay urine drug testing was performed on patients undergoing MSLT or maintenance of wakefulness testing (MWT).22 Of the 53 patients undergoing MSLT or MWT, 9 (17%) had positive urine drug screening. Two patients met MSLT criteria for narcolepsy and 4 met MSLT criteria for idiopathic hypersomnia if urine drug testing had not taken place.
We found a greater frequency of positive urine tests in patients undergoing MSLT than studies that used immunoassay urine drug testing.5,22 This result may be explained because drug testing by gas chromatography-mass spectrometry has higher sensitivity and specificity compared to immunoassay.8 It is also possible the higher rate of urine drug positive patients in our study reflects different drug use patterns in adults from London, United Kingdom, compared to the those of the previous studies of adolescents in Ohio, United States, and of adults in Melbourne, Australia.5,22
Our study has several strengths. It is the first study to perform gas chromatography-mass spectrometry on urine samples of consecutive adult patients undergoing assessment for a central hypersomnia. Gas chromatography-mass spectrometry allows a greater range of drugs to be screened. Urine drug testing by immunoassay is usually limited to detecting a specific class of drug and false positives can occur from over the counter medications and foods.8 A positive immunoassay result is considered presumptive until confirmed by another independent chemical technique such as gas chromatography-mass spectrometry.8 Second, the subjects were consecutive clinic patients with suspected central hypersomnia undergoing physician assessment and MSLT. Third, physicians were blinded to the results of the urine drugs tests when formulating a diagnosis based on clinical and MSLT assessment alone.
Our study has limitations. Firstly, hypersomnia may not have been due to drug detected and may have been due to an underlying or co-existing sleep or psychiatric disorder. The drug or psychoactive substance detected may not have been contributing to the patient's symptoms or MSLT result. Drug doses were not measured, and we do not know if drugs detected were neurologically active. Secondly, urine drug testing will not show when the patient used the drug. Urine drug testing provides a single snapshot in time and gives an insight into the patient's habits. Typical detection times in urine of drugs are: opioids 1 to 2 days, cocaine 1 to 3 days, amphetamines 2 to 5 days, and cannabis 3 to 28 days. Benzodiazepines can be detected in urine 1 to 7 days; depending on the half-life of the drug.23 However, detection of a drug is dependent on the type of drug used, the dose, the sensitivity of test and whether the use is acute or chronic. Thirdly, while physicians took a list of the patient's medications, we cannot be sure they asked specifically about illicit or over the counter medications. Fourthly, the MSLT itself is imperfect with both false positive and false negative results for narcolepsy.24 A recent study also found the repeatability of MSLT results after 4 years was low.25 As a result, the MSLT's validity as a gold standard test for narcolepsy has been called into question.26 Fifthly, our study suffers from the usual limitations of a retrospective study with bias and missing data. However, the study does reflect real-life reasoning by physicians in trying to reach a diagnosis based clinical and MSLT assessment.
In conclusion, drugs and substances may be confounders of the MSLT and physician assessment of patients with a suspected central hypersomnia. The influence of drug dose, pharmacogenetics, and the timing of medication on the MSLT remain unanswered. We recommend routinely asking patients with hypersomnia about illicit and over-the-counter medications. Those patients undergoing MSLT should have urine drug testing to exclude confounding drugs or substances not revealed in the interview. We think initial urine drug screening could be performed by immunoassay techniques (approximately US $28.00 to screen for opiates, amphetamines, and benzodiazepines). No further testing would be needed if the immunoassay drug screen were negative. However, if a class of drug is detected by immunoassay, the specific compound should be confirmed by a second technique such as Mass Spec-trometry (US $75–200 per compound).8 It might be cost-effective to perform urine drug screening before ordering a MSLT, but further studies are needed to explore this question.
DISCLOSURE STATEMENT
This was not an industry supported study. Dr. Kosky has consulted for Teva Pharmaceuticals. Dr. Bonakis has received research support from UCB. Dr. Williams has consulted for and been on the speakers bureau of UCB and has received research support from Takeda. The other authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors thank Ms. Chrianna Bharat for the statistical analysis.
ABBREVIATIONS
- BMI
body mass index GC-MS gas chromatography-mass spectrometry
- MSLT
multiple sleep latency test
- OSA
obstructive sleep apnea
- REM
rapid eye movement
- SSRIs
selective serotonin reuptake inhibitors
REFERENCES
- 1.American Academy of Sleep Medicine. 3rd ed. Darien, IL: American Academy of Sleep Medicine; 2014. International classification of sleep disorders. [Google Scholar]
- 2.Ohayon MM. Determining the level of sleepiness in the American population and its correlates. J Psychiatr Res. 2012;46:422–7. doi: 10.1016/j.jpsychires.2011.06.008. [DOI] [PubMed] [Google Scholar]
- 3.Ohayon MM, Priest RG, Zulley J, Smirne S, Paiva T. Prevalence of narcolepsy symptomatology and diagnosis in the European general population. Neurology. 2002;58:1826–33. doi: 10.1212/wnl.58.12.1826. [DOI] [PubMed] [Google Scholar]
- 4.American Academy of Sleep Medicine. Diagnostic and coding manual. 2nd edition. Westchester, IL: American Academy of Sleep Medicine; 2005. International classification of sleep disorders. [Google Scholar]
- 5.Dzodzomenyo S, Stolfi A, Splaingard D, Earley E, Onadeko O, Splaingard M. Urine toxicology screen in multiple sleep latency test: the correlation of positive tetrahydrocannabinol, drug negative patients, and narcolepsy. J Clin Sleep Med. 2015;11:93–9. doi: 10.5664/jcsm.4448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Littner MR, Kushida C, Wise M, et al. Practice parameters for clinical use of the multiple sleep latency test and the maintenance of wakefulness test. Sleep. 2005;28:113–21. doi: 10.1093/sleep/28.1.113. [DOI] [PubMed] [Google Scholar]
- 7.Pataka A, Yoon CH, Poddar A, Riha RL. Assessment of multiple sleep latency testing in adults in Europe. Sleep Med. 2013;14:136–9. doi: 10.1016/j.sleep.2012.09.025. [DOI] [PubMed] [Google Scholar]
- 8.Saitman A, Park HD, Fitzgerald RL. False-positive interferences of common urine drug screen immunoassays: a review. J Anal Toxicol. 2014;38:387–96. doi: 10.1093/jat/bku075. [DOI] [PubMed] [Google Scholar]
- 9.Iber C, Ancoli-Israel S, Chesson A, Quan SF for the American Academy of Sleep Medicine. 1st ed. Westchester, IL: American Academy of Sleep Medicine; 2007. The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications. [Google Scholar]
- 10.Carskadon MA, Dement WC, Mitler MM, Roth T, Westbrook PR, Keenan S. Guidelines for the multiple sleep latency test (MSLT): a standard measure of sleepiness. Sleep. 1986;9:519–24. doi: 10.1093/sleep/9.4.519. [DOI] [PubMed] [Google Scholar]
- 11.Littner MR, Kushida C, Wise M, et al. Practice parameters for clinical use of the multiple sleep latency test and the maintenance of wakefulness test. Sleep. 2005;28:113–21. doi: 10.1093/sleep/28.1.113. [DOI] [PubMed] [Google Scholar]
- 12.Lillsunde P, Korte T. Comprehensive drug screening in urine using solid-phase extraction and combined TLC and GC/MS identification. J Anal Toxicol. 1991;15:71–81. doi: 10.1093/jat/15.2.71. [DOI] [PubMed] [Google Scholar]
- 13.R Core Team. Vienna, Austria: R Foundation for Statistical Computing; 2013. R: A language and environment for statistical computing. http://www.R-project.org/ [Google Scholar]
- 14.Schierenbeck T, Riemann D, Berger M, Hornyak M. Effect of illicit recreational drugs upon sleep: cocaine, ecstasy and marijuana. Sleep Med Rev. 2008;12:381–9. doi: 10.1016/j.smrv.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 15.Qureshi A, Lee-Chiong T., Jr Medications and their effects on sleep. Med Clin North Am. 2004;88:751–66. doi: 10.1016/j.mcna.2004.01.007. [DOI] [PubMed] [Google Scholar]
- 16.Seidel WF, Cohen SA, Wilson L, Dement WC. Effects of alprazolam and diazepam on the daytime sleepiness of non-anxious subjects. Psychopharmacology. 1985;87:194–7. doi: 10.1007/BF00431806. [DOI] [PubMed] [Google Scholar]
- 17.Post RM, Gillin JC, Wyatt RJ, Goodwin FK. The effect of orally administered cocaine on sleep of depressed patients. Psychopharmacologia. 1974;37:59–66. doi: 10.1007/BF00426683. [DOI] [PubMed] [Google Scholar]
- 18.Mayers AG, Baldwin DS. Antidepressants and their effect on sleep. Hum Psychopharmacol. 2005;20:533–59. doi: 10.1002/hup.726. [DOI] [PubMed] [Google Scholar]
- 19.Guilleminault C. Benzodiazepines, breathing, and sleep. Am J Med. 1990;88:25S–8S. doi: 10.1016/0002-9343(90)90282-i. [DOI] [PubMed] [Google Scholar]
- 20.Cousens K, DiMascio A. (-) Delta 9 THC as an hypnotic. An experimental study of three dose levels. Psychopharmacologia. 1973;33:355–64. doi: 10.1007/BF00437513. [DOI] [PubMed] [Google Scholar]
- 21.Feinberg I, Jones R, Walker JM, Cavness C, March J. Effects of high dosage delta-9-tetrahydrocannabinol on sleep patterns in man. Clin Pharmacol Ther. 1975;17:458–66. doi: 10.1002/cpt1975174458. [DOI] [PubMed] [Google Scholar]
- 22.Anniss A, Young A, O'Driscoll D. Importance of urinary screening in the multiple sleep latency test and maintenance of wakefulness test. Abstracts. Sleep Biol Rhythms. 2015;13:1–98. [Google Scholar]
- 23.Gerostamoulos D. Urinary drug screening. Aust Prescr. 2013;36:62–64. [Google Scholar]
- 24.Aldrich MS, Chervin RD, Malow BA. Value of the multiple sleep latency test (MSLT) for the diagnosis of narcolepsy. Sleep. 1997;20:620–9. [PubMed] [Google Scholar]
- 25.Goldbart A, Peppard P, Finn L, et al. Narcolepsy and predictors of positive MSLTs in the Wisconsin Sleep Cohort. Sleep. 2014;37:1043–51. doi: 10.5665/sleep.3758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Myers G, Lammers GJ. The MSLT: more objections than benefits as a diagnostic gold standard. Sleep. 2014;37:1027–8. doi: 10.5665/sleep.3748. [DOI] [PMC free article] [PubMed] [Google Scholar]