Abstract
The majority of behavioral sleep interventions for young children involve extinction procedures where parents must ignore their child's cries for a period. Many parents have difficulties with this, contributing to attrition, non-compliance, and treatment avoidance. Yet why these methods are difficult to implement has rarely been addressed in the literature. This paper discusses seven potential reasons why parents may find extinction sleep interventions difficult: enduring crying, practical considerations, fear of repercussions, misinformation, incongruence with personal beliefs, different cultural practices, and parent wellness. These reasons are discussed in relation to the current literature. Practicing health professionals and sleep researchers could benefit from an awareness of these issues when suggesting extinction interventions and offering alternatives which may be more appropriate for family circumstances and facilitate parental informed choice.
Citation:
Etherton H, Blunden S, Hauck Y. Discussion of extinction-based behavioral sleep interventions for young children and reasons why parents may find them difficult. J Clin Sleep Med 2016;12(11):1535–1543.
Keywords: child sleep problems, extinction, sleep intervention, crying
BACKGROUND
Studies estimate one-third of parents identify their infant, toddler or preschooler as having a sleep problem.1,2 Ongoing sleep problems can negatively affect children's cognitive development, mood regulation, behavior, and health (e.g., immune function and accidental injury).1,3–5 Parents' sleep and wellbeing are also impacted by a child's poor sleep and if chronically sleep restricted are more likely to suffer from stress, anxiety, depression, and reduced coping ability.1,3,6 In addition, general family functioning is often impaired,7 which, in extremes, can contribute to child abuse such as shaken baby syndrome.8 Adult sleep research also links restricted sleep and neurobehavioral deficits and physiological changes, which subsequently connect to obesity, cardiovascular morbidity, and fatigue-related accidents and deaths.9 Thus, a child's poor sleep can have far-reaching consequences for the child, their family and the health and functioning of our communities.
Practice parameter recommendations from the American Academy of Sleep Medicine1 suggest behavior-based interventions to change the child's response to bedtime and sleep, provided there are no signs of a physiological issue such as illness.10 A systematic review of behavioral sleep intervention studies for under 5-year-olds1 assessed the primary behavioral sleep treatment techniques of extinction (unmodified extinction, graduated extinction, and extinction with parent presence), positive routines/faded bedtime with response cost, scheduled awakening, and parent education/prevention. In summary, 49 (94%) studies reported treatment as efficacious and demonstrated clinically significant change in more than 80% of children. Thus, there is evidence that behavioral sleep interventions are effective. Interestingly, of the 52 studies, 42 (81%) used extinction (unmodified extinction n = 19; graduated extinction n = 19; extinction with parental presence n = 4), while only 12 (23%) used other treatment techniques. Extinction-based sleep interventions are the favored method within research. Popular literature follows this trend with 61% (24 of 39) of parent sleep advice books endorsing extinction interventions.11 This illustrates how extinction interventions are dominating treatment.
Extinction interventions are so named because they use behavior theory's principle of extinction to eliminate a previously reinforced behavioral response.12 In child sleep problems, the parent's attention is considered the reinforcer of the child's crying and protesting behavior at nighttime.13 Thus, extinction interventions aim to improve sleep by removing parent attention to the child during sleep times to eliminate their nighttime crying.14 It is believed this creates conditions for the child to learn to self-settle.
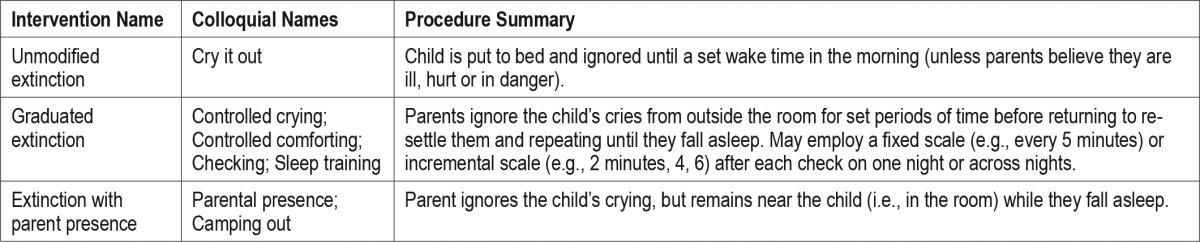
Three extinction protocols are commonly used, as reviewed by Mindell et al.1: unmodified extinction, extinction with parental presence, and graduated extinction. Table 1 presents the academic and colloquial names for these interventions along with a summary of their procedures. All involve the child's calling or crying being ignored once the child has been put to bed. Any checks are brief (typically 15–60 seconds) and use minimal interactions when re-settling, avoiding picking up, cuddling, initiating or maintaining conversations, and feeding. Parents must be consistent and ignore their child's cries every time, every night, or the behavior will be strengthened via an “intermittent reinforcement” schedule.15 Also, parents must be advised that post-extinction bursts (the reappearance of a previously extinguished behavior) are common and must also be ignored to prevent reinforcement. However, few parents are able to withstand the stress of ignoring such distress for the time required for unmodified extinction to work. As such, the modified versions were developed.16
Table 1.
Key extinction sleep intervention names and procedures.
Other behavioral sleep interventions exist, such as positive routines, faded bedtime with response cost, and scheduled awakening protocols. These aim to improve sleep by controlling arousal and physiological responses, and increasing appropriate behaviors, as opposed to reducing inappropriate behaviors, as extinction does.1 Because these interventions do not employ extinction, they will not be addressed here.
While extinction interventions are effective and dominate research, practice, and popular literature, parental resistance to these interventions has been a known issue for more than 30 years. Rickert and Johnson were surprised at the level of resistance met when recruiting for an extinction intervention study.17 Of the 50 families recruited, 5 (10%) dropped out because they refused to ignore their child's crying. Furthermore, additional parents responded to the recruitment ad, but refused to allow a home visit because they might be allocated to the ignoring condition. Other extinction studies have also experienced non-compliance and drop-out due to ethical concerns,18,19 and some report vaguely- or un-explained attrition which may be due to parent resistance to the intervention.6,20 Additional papers have also mentioned parental resistance,8,15,21,22 but often without reference to evidence. Hiscock referred to an unpublished study on stress and attachment within an extinction intervention where parental resistance undermined recruitment.23
Parental resistance has been highlighted in clinical settings, particularly relating to unmodified extinction (“cry it out”).14,15,24–26 A survey showed parents found a “bedtime pass” method, where the child was given a pass to leave their bed for something quick (e.g., a drink or hug) once each night without penalty, much more acceptable than ignoring.27 This preference was not mirrored by professionals. Pediatricians rated ignoring as more acceptable than the parents, and they rated the “bedtime pass” equally acceptable to ignoring, illustrating that parents and practitioners hold different views on the acceptability of treatments. To understand general opinion on extinction Blunden and Baills conducted a pilot study to assess Australian parents use of “controlled crying” with under 3-year-olds. They found 75% (n = 104) either never used controlled crying or started using but stopped, primarily for emotional and stress-related reasons.28
Objections to treatments can lead to attrition, avoidance, and non-compliance.17,18,22,25,27 A significant discrepancy between parent and practitioner views could also potentially harm these relationships, and in turn reduce future engagement with that practitioner or possibly other professionals. One result could be significant health issues from ongoing sleep deprivation.
Over 20 years ago, France discussed concerns and assumptions of parents which reduced their engagement.25 That paper raised the issue of parent concerns, but all points raised were based on the assumption that parents' concerns were due to a lack of knowledge. However, other factors also contribute to resistance to extinction interventions. For example, interventions may be too traumatic for parents or children, contradict their beliefs about child-rearing, or are impractical.18 Owens et al.15 briefly discussed how a lack of parental acceptance influences behavioral sleep interventions, but did not discuss the reasons for this resistance.
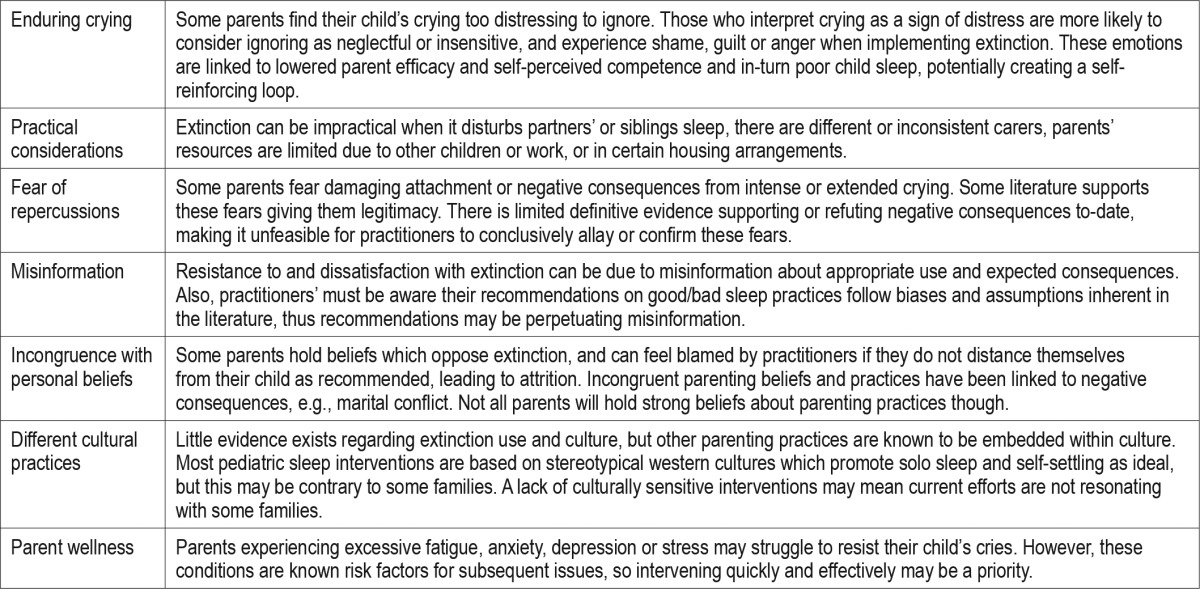
It is important we understand difficulties which may prevent parents from engaging with treatments to enable development of effective solutions and alternatives.5 This narrative review aims to begin this process by discussing reasons which explain why parents find extinction difficult to implement and maintain. The reasons presented in the following sections were assembled through searches of key literature on behavioral sleep interventions for under-5-year olds, collating all relevant findings and general comments and sorting them into appropriate themes. Few sources contained or referenced any primary evidence on parent difficulties with extinction interventions. More numerous were brief comments about parent resistance to extinction from authors while reporting on other sleep intervention outcomes or reviewing child sleep problems more broadly. So this review, although not systematic due to the paucity of empirical data, is as exhaustive a collection as possible. Seven difficul-ties with use of extinction were identified using this method: (1) enduring crying, (2) practical considerations, (3) fear of repercussions, (4) misinformation; (5) incongruence with personal beliefs, (6) different cultural practices, and (7) parent wellness. Table 2 presents a summary of these difficulties with extinction. Papers addressing related sleep- and parent-practice topics (e.g., co-sleeping and feeding), where more research has been undertaken on parents' perspectives, have also been used in some sections to help explain how these barriers may prevent parents implementing extinction interventions.
Table 2.
Reasons for parents' difficulties with extinction interventions.
DIFFICULTIES WITH IMPLEMENTING EXTINCTION INTERVENTIONS
Enduring Crying
Difficulty with enduring crying is often cited as a reason for parents resisting or stopping extinction sleep interventions.16,17,20,28–30 A cry is a powerful biological signal, which parents find diffi-cult to ignore as it goes against biological instincts24 and causes them distress.30 Crying is inherent in extinction interventions; otherwise it would not be necessary as the child would simply fall asleep on their own. Crying increases when an extinction intervention begins and is called an “extinction burst.”15 That is, when the child's behavior (crying) does not elicit the usual response (parents attending) the behavior will initially increase in severity, frequency and/or duration to draw the desired response. For example, in Rickert and Johnson's study, baseline crying was 35–40 minutes, but this increased to more than 70 minutes for the first 2 intervention nights.17 Extinction may also provoke variability in the child's behavior, such as throwing objects or banging on walls. Jones and Verduyn did not even suggest “cry it out” in an intervention study they conducted because “few parents are able to consign their child to such distress and a late response may exacerbate the problem”31 These protests make it harder for parents to ignore and occur even in modified forms of extinction. Some parents have stated they do not have the will to change behavior.18 Other parents reported they did not use graduated extinction because they could not bear to listen to their child cry alone.28
Cognitive psychology highlights the importance of parents' interpretation of the cry. Parents who regard crying as a sign of distress typically consider ignoring it as neglectful or insensitive.32 For these parents, ignoring their child would lead to negative emotions such as shame, guilt, and anger; and these act as negative reinforcers against behavior change.33 These significant negative beliefs and emotions are connected to lowered parent efficacy and self-perceived competence,34 which in turn are related to poor child sleep.33 Thus, these negative self-beliefs and emotions and child sleep behaviors can create a self-reinforcing loop.
Children with fussy-difficult temperaments are more likely to be seen as having sleep problems.21 It is likely that the parents suffer from decision-making and self-control fatigue35 as they are constantly managing a fussing child. For these families the added pressure of resisting their crying child, when they are physically fatigued, can lead to inconsistent responses or withdrawal from the treatment. Therefore, for certain parents or children, extinction interventions may be too stressful or inappropriate.
Despite the crying, one argument for using extinction is how quickly it works.36 However, Rickert and Johnson17 found that it took 3 or more weeks for awakening and crying to reduce to less than 4 per week. This study (although small, n = 33 children) indicates that not all children's wakings abate within a few nights. Therefore, misinformation about rapid success could lead to frustration, doubt and subsequent attrition for parents whose children take longer to treat.
Practical Considerations
Although many authors cite intense crying as a reason for discarding extinction interventions, others have found external factors and practicalities prevented uptake or continuation of extinction,17,18 such as the crying disturbing other children or a spouse needing to work. Also, it is unlikely a child would be ignored consistently when sharing the same sleep space, potentially strengthening protesting behaviors.15 Inconsistent carers or carer availability can compromise extinction interventions as different carers can respond differently to the child, including during periods of distress.18 A lack of human resources can also prevent implementation of extinction interventions, for example, where there are competing demands for parents' time such as other children or work-related duties.15 Disturbing neighbors is another practical problem for some families.24,30 This situation can be a concern in densely occupied buildings or areas, where noise complaints may lead to eviction and difficulty finding future housing. Thus, extinction interventions potentially carry additional risks. Parents may seek to intervene differently while balancing other demands in their lives instead of refusing to comply.18 However, if not under the guidance of a professional with behavioral knowledge, parents risk altering essential aspects of the intervention and potentially strengthening undesirable behaviors.
Fear of Repercussions
Another reason for parental resistance is fear about intense or extended crying being detrimental to the child's health or fear of creating a poor attachment between parent and child.13,18,22,25 Some researchers, clinicians, popular authors and parenting organizations express these concerns and advocate against cry-intensive methods.37–41 However, other researchers and clinicians do not support these concerns and defend the safety of extinction.1,3,13,42 Parents are able to obtain summaries and discussions of the academic literature via media releases, social media and online parenting groups, thus they may make parenting decisions based on what they interpret to be evidence-based practice. However, there is limited evidence to conclusively support or deny that there are any lasting negative effects of extinction, and what exists is complicated by methodological issues such as measurement methods, participant samples and experiment protocols which most parents are unlikely to understand.
The literature conclusively shows that excessive stress harms young children,43,44 but it is unclear how much crying equates to too much stress. Chronic stress, such as from abuse and neglect, is linked with a range of internalizing and externalizing symptoms and disorders, such as withdrawal, helplessness, somatic disorders, anxiety disorders, self-harm, hypervigilance, impulsivity, sleep problems, substance abuse and aggression.44 The psychobiology of stress explains how early caregiving responsiveness is essential in promoting beneficial developmental growth and child outcomes.45,46 Certain early life experiences, such as co-sleeping, have been found to contribute to more optimal stress responses.47–49 It is not surprising that parents who hear that science has found that excessive stress can cause serious disorders and that more responsive parenting can benefit children's stress responses fear negative consequences of extinction. But other research indicates there are no lasting negative effects of the crying associated with extinction42 and early life experiences, such as co-sleeping, have also been shown to cause poorer stress responses in different situations.48,50 Often these conflicting findings are not presented or are poorly explained in the media and parenting networks, and the information presented in many parenting networks share a similar ideological stance and wish to show evidence to support it. Parents can be left with the impression these findings are definitive and that extinction is or is not harmful.
Some studies are presented as conclusive evidence that there are or are not harms caused by extinction42,51 by researchers, professionals and popular writers alike. Unsurprisingly parents can be concerned when they hear in a recent study that infants' stress responses to extinction remained high even after the child had stopped crying because their stress levels were still elevated.51 This was despite a reported decrease in maternal stress levels, presumably due to the lack of crying, causing asynchrony in the mother-child dyad. Synchronicity of this dyad is foundational for the child's cognitive, social-emotional and self-regulatory skills,52 and secure mother-infant attachment.53 Findings from that study51 suggested there could be unintended risks of extinction interventions, and many online parenting groups cited this study as “proof” of extinction being harmful. What some parents may not have seen was the response to this study from some pediatric sleep researchers who questioned study features which had the potential to alter the interpretation of findings.54 However, based on other significant published works,1,13 even their response was not comprehensive in their arguments, and it missed the concern for potential harm to the child. Therefore, academics and professionals are still debating whether the stress of extinction is a sufficient to cause harm and warrant its cessation as a recommended practice.38,54 Understandably therefore parents too may be confused.
The other concern is the potential for extinction to compromise a child's attachment to caregiver(s).23,55 Ideally parent and child form a secure attachment to each other whereby the child's activity or signals (such as crying or smiling) maintain caregiver proximity and responsiveness.56 Secure attachment is foundational in a young child's development and impacts on social, emotional, cognitive and behavioral outcomes. Poor early attachments impair these abilities.57 Secure attachment is established through warm, sensitive and consistent parent responses to the infant which assist the child in developing confidence, self-reliance, and emotional and behavioral regulation. This is especially important in the first few years of life. Orphanage studies have shown that children who are placed in a foster care home before 24 months are most likely to develop a secure attachment to a consistent caregiver, but the likelihood decreases with increasing age of placement.58
Like stress, it is unclear the extent of negligent or inconsistent caregiving required to adversely impact a child's attachment. Therefore, it is unclear whether non-responsive night-time parenting could cause attachment issues for a child. Studies have examined proxies of attachment in relation to extinction interventions42,55,59,60 and found no indication of adverse effects, and some indications of positive effects. However, the measures used are vulnerable to parents' biases, making it is unclear whether the sleep interventions impacted the child's actual behavior and attachment or simply the parents' perception of the child's behavior. Various forms of insecure attachment (e.g., ambivalent, disorganized, resistant, and avoidant) have been linked to problematic sleep in infants and young children21,61,62 via gold standard testing, providing additional support for the accuracy of their findings. Parents are unlikely to be aware of these tools and their strengths, weaknesses and alternatives, making it virtually impossible for them to understand the strengths and limitations of the findings. Parents may also not understand that these findings do not provide evidence for causal relationships, and these studies have focussed on whether attachment affects sleep, rather than whether sleep affects attachment. So currently it is impossible to conclude whether parent-child sleep interactions can damage attachment. It is worth noting that Morrell and Steele's21 research on insecure attachment in infants and sleep problems led them to conclude that parental attempts to use extinction interventions with infants classified as already having an insecure ambivalent attachment, would lead to exaggerated responses from the child and likely failure. Also, these methods were likely to reinforce the sleep problems and maintain the ambivalent attachment. Thus it is plausible that extinction interventions may exacerbate attachment issues in children for whom attachment and sleep are already impaired, but whether they can cause them is still unknown. It would be difficult and unlikely most parents would read or understand the subtleties and limitations surrounding research such as this, and they may misinterpret the overall message that extinction can contribute to poor attachment.
Parents confronted with opposing arguments such as those relating to negative consequences of extinction would likely feel unease, uncertainty and reluctance to accept practitioner recommendations to use it. Although many pediatric sleep experts affirm the safety of extinction interventions,13,29,42,63 they also admit there are limited causative findings, evidence on the effects of extinction on vulnerable populations, or objective measures of attachment and stress. Price and colleagues42 longitudinal study has greatly contributed by examining the long-term effects of graduated extinction on a range of child and parent-child relationship factors, finding no positive or negative effects at 6 years of age. Unfortunately, the study utilized parent-report measures, making it difficult to know whether effects were due to parent perceptions or actual behavior. There is a difference between having no evidence of harm and evidence of no harm and researchers must provide evidence of no harm across populations, circumstances and methods so we can address this difficulty with parents.
Misinformation
Parents can be misinformed about the risks, methods, benefits and assumptions of extinction interventions which can lead to immediate resistance, or dissatisfaction or shock at unexpected consequences and subsequent resistance. Parents obtain most of their child sleep information from social networks64 or general literature,11 including online networks, some of which present specific parenting ideologies and provide information to validate their parenting narratives. Published articles can be shared widely and a single study supporting or refuting a position can be used to show scientific “proof” for their chosen methods (e.g., McKay66). Ramos and Youngclarke11 analyzed sleep advice books available in the United States and found that nearly half were published by non-professionals, while the medical profession (who typically advocate extinction1) dominated those with a professional author. Lacking representation were researchers, child development specialists, and psychologists. Generally, child sleep issues are not medical, but social, psychological, and developmental. Also most of the books analyzed11 took an explicit stance on extinction, either for or against, leading to directly conflicting advice. For example, many opposed co-sleeping because it would impede parents' sleep, and many supported co-sleeping because it would increase parents' sleep. Overall it is likely that the primary sources of sleep information accessed by parents may be biased and confusing.
Misinformation can also negatively impact families who are willing to try extinction interventions.15 Extinction bursts are expected (where crying initially increases), but it can appear the intervention is not working. Spontaneous reoccurrence of crying is another possibility following extinction interventions. Parents must be advised of these otherwise they are likely to discontinue the intervention prematurely and/or perceive it as ineffective. Tse and Hall18 found parents' self-confidence was shattered when they tried different interventions unsuccessfully, leaving them feeling desolate and vulnerable. These parents felt sceptical about trying further interventions because they feared another failure. Some parents in their study also felt dispirited by relapses, believing once the problem was resolved it would be gone permanently, despite being told sleep-problem relapses could occur posttreatment (usually due to disruptions like illness, travel and moving house). Providing information on extinction may not be sufficient to override parents' emotional reactions.
Similarly, parents willing to use extinction interventions must be informed of the appropriate conditions around their use.15 General information available through non-professionals (e.g., websites, books, and support networks) is not always prefaced with important details on how, at what age, under what conditions and why these methods should be implemented. For example, many professionals agree that extinction interventions should not be used with infants under 6 months of age,3,54 and some argue even older, around 8–12 months, to allow for natural developmental changes in sleep patterns and learning abilities.26 Sources which do not provide this conditional and operational information leave parents at risk of inappropriately executing extinction interventions.
Interestingly, we know little about parents' perceptions around child sleep problems,66 such as what constitutes problematic sleep and what is normal. Yet parent identification of a sleep problem is usually used for clinical and research purposes. It is not clear whether parents, particularly first-time parents, understand how infant sleep patterns develop and change over time, including the normalcy of erratic patterns at certain times. Neither is it clear whether they have strategies for coping with these changes. Present educational parenting materials may be at levels inappropriate to meet the needs of families.67
As researchers and practitioners, we must also think critically about providing information that perpetuates misinformation. Underlying extinction interventions is the premise that bedtime noncompliance has been trained by the behaviors of the parents.30 But it would be unwise to assume all child sleep problems have been trained by the parents. Some data suggests maladaptive parenting behaviors can follow early infancy sleep difficulties, not the other way around.68 It is interesting is that extinction interventions were first conducted not to improve sleep, but to decrease crying and tantrum behaviors at bedtime.69,70 The ability of extinction interventions to improve sleep has been extrapolated and explained as an increase in self-soothing ability. However, there is little research examining self-soothing ability explicitly so caution is needed when assuming extinction interventions promote self-soothing. Indeed, some practitioners and researchers question this assumption and propose that it teaches children to “give-up,” inciting learned helplessness,38,71 and some findings may support this.51 Limited data still restrict confidence in this proposition.
Parent education in programs also follows a specific philosophy and this must be recognized. For example, reflecting their learning in a treatment program a participant stated, “…if their parents are always helping them to fall asleep, then you could have a five-year old that still needs parents to fall asleep…”18 This participant had been taught that self-soothing is a skill which parents must teach by being “hands-off.” While most pediatric sleep literature suggests this, and thus the parent education is in line with expert advice, the premise that children will not learn to self-soothe without the parents removing themselves has not been conclusively supported. One study found no relationship “between self-soothing status during the first year of life and later sleep problems as defined by the research criteria or parental report.”72
In summary, misinformation about extinction interventions can lead to negative emotions in parents, such as confusion, frustration and reduced self-confidence, as well as resistance to or early cessation of extinction use. Professionals must also be aware of the underlying assumptions and beliefs contained in the educational material they provide to parents to avoid perpetuating misrepresentative messages based on limited evidence.
Incongruence with Personal Beliefs
Data indicate parents' beliefs about sleep influence their parenting behaviors, which then affect the child.73 Parenting beliefs which contradict extinction are likely to lead to attrition. Evidence of the importance of congruent parenting beliefs and practices can be found in the co-sleeping literature. For example, spousal conflicts are more likely “when there is a lack of consensus between parents and their preferred sleep arrangements.”74 Marital conflict is related to increased child sleep problems, possibly due to increased tension between parents causing behavioral disruption to the child, or the child's disruptive behavior placing strain on the parents' emotions and coping abilities. With the former, it is then important to assist parents in maintaining congruent parenting practices and beliefs. Keller and Goldberg's research into the differences between families using solitary sleeping, intentional co-sleeping (those who choose to co-sleep and usually from an early age) and reactive co-sleeping (those who co-sleep to ease child sleep disturbances) found the success parents experienced with their chosen sleep practice depended on their beliefs, parenting styles and goals rather than the practice itself.75 Similarly, reactive co-sleeping mothers held positive views about both solitary sleep and co-sleeping, and were more likely to view their child's sleep as problematic, whereas solitary sleeping mothers and intentionally co-sleeping mothers only viewed their respective practices more favorably and were less likely to view their child's sleep as problematic. While this research focused on solitary and co-sleeping arrangements it may be applicable to sleep intervention practices too.
The majority of research on parents' child-sleep-related beliefs has focused on their agreement with limit-setting (e.g. resisting night-time requests and limiting parent interaction through the night) and active comforting (e.g. holding, patting and bed-sharing). Lower agreement with limit-setting and higher agreement with active comforting have been linked to greater parent involvement at night, which in turn has been linked to increased child sleep problems.21,73,76 Therefore, most literature advocates increased limit-setting by parents to decrease potential sleep issues. This may be in conflict with parents' core beliefs. To decrease resistance to interventions some clinicians attempt to reshape parents' beliefs when parents perceive decreased night-time responsiveness as insensitive or abusive. They know that “changing parental perceptions and concerns is necessary to prepare the parents toward the behavioral intervention and to facilitate cooperation with the intervention.”22 While this may be necessary in some clinical populations due to significant health risks of continued sleep deprivation (e.g., postnatal depression), its ethical basis is questionable when parents are not in crisis. Also, the practitioner belief that limit-setting practices are the ideal could lead to an undercurrent of blame towards the parents if they seek help for child sleep problems and do not distance themselves from their child at night. It is worth considering whether the link between agreement with nighttime active comforting and sleep problems is moderated by a third factor, such as parent anxiety or parent-efficacy.
Parenting beliefs are only one factor regarding the uptake of extinction and not all parents will hold strong beliefs for or against extinction interventions.18
Different Cultural Practices
Culture and biases can underpin the methods used and outcomes expected. For example, it was stated that Tse and Hall's18 intervention promoted positive day and night-time routines and avoidance of negative sleep associations. But not all routines and sleep associations are consistently considered positive or negative by all researchers, health professionals, educators or other community members.11 Thus the information provided followed beliefs about parenting methods and health behaviors.77 This is noticeable in some reported strategies undertaken by parents for example, avoiding feeding, rocking or cuddling to sleep, co-sleeping, and short naps.18 Avoiding these behaviors aligns with the extinction model favored in the medical model and supports the general Western cultural view of promoting independence from a young age and limit-setting. But avoiding these behaviors is also considered cruel, negligent, and nonsensical for others who ascribe to different parenting practices.32
Little evidence exists relating to sleep intervention uptake and culture; however, there are examples of how other parenting practices are influenced by culture. For example, breast-feeding, co-sleeping and transitioning to solid foods are deeply embedded within cultural practices67 and may oppose the general narrative in the wider community. In some cultures, leaving a child to sleep alone is considered “bad parenting,”78 which has significant implications for treatment, especially in relation to extinction interventions.30 Most current pediatric sleep interventions and parent training models are based upon a stereotypical Western, middle-class family set-up, which sleeps children and adults in different rooms and beds and fosters independence in their children over social dependence.38 But even among Caucasian Australian families this is not always the case and the cultural context of night-time parenting is rarely addressed explicitly in sleep interventions.5 Parents participating in Tse and Hall's18 extinction intervention reported avoiding discussing the intervention with friends and only implementing the intervention when no one was present, for fear of being judged. This may relate to cultural norms within their social circles. A lack of culturally sensitive models of intervention may mean current efforts are not resonating with their intended audiences.67 Further research is needed to understand cross-cultural sleep contexts and develop culturally-sensitive interventions.
Parent Wellness
Finally, parents must be well enough to persist with extinction interventions. Parents who are sleep deprived are likely to struggle to resist their child's demands, or may even fall asleep in the child's room due to exhaustion.15 This can inadvertently strengthen the child's protesting behavior prolonging sleep difficulties. Also, parents' mental health problems, such as depression, may impede their use of extinction interventions.15 However, Hiscock and colleagues3 use extinction sleep interventions to improve child sleep and maternal depression. They argue this is an important time to intervene with a quick and effective sleep intervention to help mothers cope and recover as postnatal depression is a known risk factor for adverse child development, family breakdown and maternal anxiety. Also, mothers may present with depressive symptoms when sleep deprived, in which case improving their child's sleep can also decrease the depressive symptoms.59 Physical health is unlikely to have a major impact on the execution of extinction interventions as the physical demands are likely the same as other caring practices.
SUMMARY AND CONCLUSIONS
Parental resistance remains the largest barrier to the implementation of extinction interventions,30 and preliminary data28 would suggest the majority of Australian parents find graduated extinction too difficult and stressful to implement. Despite being a known issue for decades, few researchers have explicitly addressed it.15,25
The explanations for parent resistance have been compiled from a wide range of sources, as there is little data on parent perspectives on behavioral sleep interventions. Tse and Hall's work18 is the most comprehensive to date, but as it examined parent perspectives embedded within a specific education and treatment protocol it is unclear whether these perspectives are representative of general populations. More data is needed to refine our understanding of the challenges parents face. Nonetheless, explanations of the difficulties of extinction interventions can be found scattered among the literature and this review has discussed a range of reasons contributing to parental resistance.
No single intervention is likely to overcome such a wide range of challenges. Therefore, it is important that a range of options be offered to parents as standard practice. Alternatives to extinction have been developed, such as positive routines, faded bedtime and scheduled awakening,1 and more continue to be developed, but have received little attention in the literature making it difficult to assess their efficacy and acceptability. For example, parents who had previously attempted extinction reported an intervention which did not involve ignoring their child's cries as successful, achievable and respectful of both children's emotions and parental choices.28 But this was a small, uncontrolled study with limited measures of intervention effectiveness, acceptability and secondary outcomes, so further evaluation is required to conclusively support its use.
For alternatives to be offered, high quality research must be conducted to demonstrate the efficacy and acceptability of varying interventions. The current literature is dominated by extinction sleep interventions and limits the ability of health professionals to offer appropriate and evidence-based options to facilitate parents making an informed choice. The narrow focus of current literature also influences lay literature, media publications, social media and community groups within the public domain. If options are not researched to allow for choice and informed decision making by parents, families will be unable to effectively address their children's sleep problems, with the attendant negative consequences for the family and the community.
DISCLOSURE STATEMENT
This was not an industry supported study. This research has been supported by the CQUniversity HEALTH CRN www.cqu.edu.au/crn and the Australian Government's Collaborative Research Networks Program. The authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Mindell JA, Kuhn B, Lewin DS, Meltzer LJ, Sadeh A American Academy of Sleep Medicine. Behavioral treatment of bedtime problems and night wakings in infants and young children. Sleep. 2006;29:1263–76. [PubMed] [Google Scholar]
- 2.Sadeh A, Mindell JA, Rivera L. “My child has a sleep problem”: a cross-cultural comparison of parental definitions. Sleep Med. 2011;12:478–82. doi: 10.1016/j.sleep.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 3.Hiscock H, Bayer JK, Hampton A, Ukoumunne OC, Wake M. Long-term mother and child mental health effects of a population-based infant sleep intervention: cluster-randomized, controlled trial. Pediatrics. 2008;122:e621–7. doi: 10.1542/peds.2007-3783. [DOI] [PubMed] [Google Scholar]
- 4.Scher A. Infant sleep at 10 months of age as a window to cognitive development. Early Hum Dev. 2005;81:289–92. doi: 10.1016/j.earlhumdev.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 5.Mindell JA, Owens J, Alves R, et al. Give children and adolescents the gift of a good night's sleep: a call to action. Sleep Med. 2011;12:203–4. doi: 10.1016/j.sleep.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 6.Hiscock H, Wake M. Randomised controlled trial of behavioural infant sleep intervention to improve infant sleep and maternal mood. BMJ. 2002;324:1062. doi: 10.1136/bmj.324.7345.1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hiscock H, Canterford L, Ukoumunne OC, Wake M. Adverse associations of sleep problems in Australian preschoolers: national population study. Pediatrics. 2007;119:86–93. doi: 10.1542/peds.2006-1757. [DOI] [PubMed] [Google Scholar]
- 8.St. James-Roberts I. Helping parents to manage infant crying and sleeping: a review of the evidence and its implications for services. Child Abuse Rev. 2007;16:47–69. [Google Scholar]
- 9.Banks S, Dinges DF. Behavioral and physiological consequences of sleep restriction. J Clin Sleep Med. 2007;3:519–28. [PMC free article] [PubMed] [Google Scholar]
- 10.Hill C. Practitioner review: effective treatment of behavioural insomnia in children. J Child Psychol Psychiatry. 2011;52:731–40. doi: 10.1111/j.1469-7610.2011.02396.x. [DOI] [PubMed] [Google Scholar]
- 11.Ramos KD, Youngclarke DM. Parenting advice books about child sleep: cosleeping and crying it out. Sleep. 2006;29:1616–23. doi: 10.1093/sleep/29.12.1616. [DOI] [PubMed] [Google Scholar]
- 12.Bouton ME. Sinauer Associates; 2007. Learning and behavior: a contemporary synthesis. [Google Scholar]
- 13.Thomas JH, Moore M, Mindell JA. Controversies in Behavioral Treatment of Sleep Problems in Young Children. Sleep Med Clin. 2014;9:251–9. [Google Scholar]
- 14.Owens LJ, France KG, Wiggs L. Behavioural and cognitive-behavioural interventions for sleep disorders in infants and children: a review. Sleep Med Rev. 1999;3:281–302. doi: 10.1053/smrv.1999.0082. [DOI] [PubMed] [Google Scholar]
- 15.Owens JA, Palermo TM, Rosen CL. Overview of current management of sleep disturbances in children: II—Behavioral interventions. Curr Ther Res. 2002;63:B38–52. [Google Scholar]
- 16.Meijer AM. Infant sleep consolidation: new perspectives. Sleep Med Rev. 2011;15:209–10. doi: 10.1016/j.smrv.2011.01.004. [DOI] [PubMed] [Google Scholar]
- 17.Rickert VI, Johnson CM. Reducing nocturnal awakening and crying episodes in infants and young children: a comparison between scheduled awakenings and systematic ignoring. Pediatrics. 1988;81:203–12. [PubMed] [Google Scholar]
- 18.Tse L, Hall W. A qualitative study of parents' perceptions of a behavioural sleep intervention. Child Care Hlth Dev. 2008;34:162–72. doi: 10.1111/j.1365-2214.2007.00769.x. [DOI] [PubMed] [Google Scholar]
- 19.Seymour FW, Bayfield G, Brock P, During M. Management of night-waking in young children. Aust J Fam Ther. 1983;4:217–23. [Google Scholar]
- 20.Reid MJ, Walter AL, O'Leary SG. Treatment of young children's bedtime refusal and nighttime wakings: a comparison of “standard” and graduated ignoring procedures. J Abnorm Child Psychol. 1999;27:5–16. doi: 10.1023/a:1022606206076. [DOI] [PubMed] [Google Scholar]
- 21.Morrell JMB, Steele H. The role of attachment security, temperament, maternal perception, and care-giving behavior in persistent infant sleeping problems. Inf Mental Hlth J. 2003;24:447. [Google Scholar]
- 22.Tikotzky L, Sadeh A. The role of cognitive–behavioral therapy in behavioral childhood insomnia. Sleep Med. 2010;11:686–91. doi: 10.1016/j.sleep.2009.11.017. [DOI] [PubMed] [Google Scholar]
- 23.Hiscock H. Rock-a-bye baby? Parenting and infant sleep. Sleep Med Rev. 2010;14:85–7. doi: 10.1016/j.smrv.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 24.Bax MC. Sleep disturbance in the young child. BMJ. 1980;280:1177–9. doi: 10.1136/bmj.280.6224.1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.France KG. Handling parents' concerns regarding the behavioural treatment of infant sleep disturbance. Behav Change. 1994;11:101. [Google Scholar]
- 26.Leeson R, Barbour J, Romaniuk D, Warr R. Management of infant sleep problems in a residential unit. Child Care Hlth Dev. 1994;20:89–100. doi: 10.1111/j.1365-2214.1994.tb00856.x. [DOI] [PubMed] [Google Scholar]
- 27.Friman PC, Hoff KE, Schnoes C, Freeman KA, Woods DW, Blum N. The bedtime pass: an approach to bedtime crying and leaving the room. Arch Pediatr Adol Med. 1999;153:1027–9. doi: 10.1001/archpedi.153.10.1027. [DOI] [PubMed] [Google Scholar]
- 28.Blunden S, Baills A. Treatment of behavioural sleep problems: asking the parents. J Sleep Disord Treat Care. 2013;2:7. [Google Scholar]
- 29.Sadeh A, Tikotzky L, Scher A. Parenting and infant sleep. Sleep Med Rev. 2010;14:89–96. doi: 10.1016/j.smrv.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 30.Ortiz C, McCormick L. behavioral parent-training approaches for the treatment of bedtime noncompliance in young children. J Early Intensive Behav Interv. 2007;4:511–25. [Google Scholar]
- 31.Jones D, Verduyn C. Behavioural management of sleep problems. Arch Dis Child. 1983;58:442–4. doi: 10.1136/adc.58.6.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sadeh A. Cognitive–behavioral treatment for childhood sleep disorders. Clin Psychol Rev. 2005;25:612–28. doi: 10.1016/j.cpr.2005.04.006. [DOI] [PubMed] [Google Scholar]
- 33.Morrell JMB. The role of maternal cognitions in infant sleep problems as assessed by a new instrument, the maternal cognitions about infant sleep questionnaire. J Child Psychol Psychiatry. 1999;40:247–58. [PubMed] [Google Scholar]
- 34.Coleman PK, Karraker KH. Self-efficacy and parenting quality: findings and future applications. Dev Rev. 1998;18:47–85. [Google Scholar]
- 35.Vohs K, Baumeister R, Schmeichel B, Twenge J, Nelson N, Tice D. Making choices impairs subsequent self-control: a limited-resource account of decision making, self-regulation, and active initiative. J Pers Soc Psychol. 2008;94:883. doi: 10.1037/0022-3514.94.5.883. [DOI] [PubMed] [Google Scholar]
- 36.Sadeh A, Mindell JA, Owens JA. Why care about sleep of infants and their parents? Sleep Med Rev. 2011;15:335–7. doi: 10.1016/j.smrv.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 37.Blunden S, Willcocks A. Adelaide, South Australia: Wakefield Press; 2012. The sensible sleep solution: a guide to sleep in your baby's first year. [Google Scholar]
- 38.Blunden S, Thompson KR, Dawson D. Behavioural sleep treatments and night time crying in infants: challenging the status quo. Sleep Med Rev. 2011;15:327–34. doi: 10.1016/j.smrv.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 39.McKenna JJ, Ball HL, Gettler LT. Mother–infant cosleeping, breastfeeding and sudden infant death syndrome: what biological anthropology has discovered about normal infant sleep and pediatric sleep medicine. Am J Phys Anthropol. 2007;134:133–61. doi: 10.1002/ajpa.20736. [DOI] [PubMed] [Google Scholar]
- 40.Douglas PS, Hill PS. Behavioral sleep interventions in the first six months of life do not improve outcomes for mothers or infants: a systematic review. J Dev Behav Pediatr. 2013;34:497–507. doi: 10.1097/DBP.0b013e31829cafa6. [DOI] [PubMed] [Google Scholar]
- 41.Australian Association for Infant Mental Health Inc. Double Bay, New South Wales: Australian Association for Infant Mental Health Inc.; 2013. Position Paper 1 (updated): controlled crying. [Google Scholar]
- 42.Price A, Wake M, Ukoumunne OC, Hiscock H. Outcomes at six years of age for children with infant sleep problems: longitudinal community-based study. Sleep Med. 2012;13:991–8. doi: 10.1016/j.sleep.2012.04.014. [DOI] [PubMed] [Google Scholar]
- 43.Gunnar MR, Donzella B. Social regulation of the cortisol levels in early human development. Psychoneuroendocrinology. 2002;27:199–220. doi: 10.1016/s0306-4530(01)00045-2. [DOI] [PubMed] [Google Scholar]
- 44.Perry BD, Pollard R. Homeostasis, stress, trauma, and adaptation: a neurodevelopmental view of childhood trauma. Child Adolesc Psychiatr Clin N Am. 1998;7:33–51. viii. [PubMed] [Google Scholar]
- 45.Loman MM, Gunnar MR. Early experience and the development of stress reactivity and regulation in children. Neurosci Biobehav Rev. 2010;34:867–76. doi: 10.1016/j.neubiorev.2009.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gunnar M, Quevedo K. The neurobiology of stress and development. Annu Rev Psychol. 2007;58:145–73. doi: 10.1146/annurev.psych.58.110405.085605. [DOI] [PubMed] [Google Scholar]
- 47.Tollenaar MS, Beijers R, Jansen J, Riksen-Walraven JMA, de Weerth C. Solitary sleeping in young infants is associated with heightened cortisol reactivity to a bathing session but not to a vaccination. Psychoneuroendocrino. 2012;37:167–77. doi: 10.1016/j.psyneuen.2011.03.017. [DOI] [PubMed] [Google Scholar]
- 48.Beijers R, Riksen-Walraven JMA, de Weerth C. Cortisol regulation in 12-month-old human infants: associations with the infants' early history of breastfeeding and co-sleeping. Stress. 2013;16:267–77. doi: 10.3109/10253890.2012.742057. [DOI] [PubMed] [Google Scholar]
- 49.Waynforth D. The influence of parent–infant cosleeping, nursing, and childcare on cortisol and SIgA immunity in a sample of british children. Dev Psychobiol. 2007;49:640–8. doi: 10.1002/dev.20248. [DOI] [PubMed] [Google Scholar]
- 50.Lucas-Thompson R, Goldberg WA, Germo GR, Keller MA, Davis EP, Sandman CA. Sleep arrangements and night waking at 6 and 12 months in relation to infants' stress-induced cortisol responses. Inf Child Dev. 2009;18:521–44. [Google Scholar]
- 51.Middlemiss W, Granger DA, Goldberg WA, Nathans L. Asynchrony of mother– infant hypothalamic–pituitary–adrenal axis activity following extinction of infant crying responses induced during the transition to sleep. Early Hum Dev. 2012;88:227–32. doi: 10.1016/j.earlhumdev.2011.08.010. [DOI] [PubMed] [Google Scholar]
- 52.Feldman R. From biological rhythms to social rhythms: physiological precursors of mother-infant synchrony. Dev Psychol. 2006;42:175. doi: 10.1037/0012-1649.42.1.175. [DOI] [PubMed] [Google Scholar]
- 53.Isabella RA, Belsky J. Interactional synchrony and the origins of infant-mother attachment: a replication study. Child Dev. 1991;62:373–84. [PubMed] [Google Scholar]
- 54.Price A, Hiscock H, Gradisar M. Let's help parents help themselves: a letter to the editor supporting the safety of behavioural sleep techniques. Early Hum Dev. 2013;89:39–40. doi: 10.1016/j.earlhumdev.2012.07.018. [DOI] [PubMed] [Google Scholar]
- 55.France KG. Behavior characteristics and security in sleep-disturbed infants treated with extinction. J Pediatr Psychol. 1992;17:467–75. doi: 10.1093/jpepsy/17.4.467. [DOI] [PubMed] [Google Scholar]
- 56.Ainsworth MDS. Object relations, dependency, and attachment: a theoretical review of the infant-mother relationship. Child Dev. 1969;40:969–1025. [PubMed] [Google Scholar]
- 57.Moullin S, Waldfogel J, Washbrook E. Sutton Trust; 2014. Baby bonds: parenting, attachment and a secure base for children. [Google Scholar]
- 58.Smyke AT, Zeanah CH, Fox NA, Nelson CA, Guthrie D. Placement in foster care enhances quality of attachment among young institutionalized children. Child Dev. 2010;81:212–23. doi: 10.1111/j.1467-8624.2009.01390.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lam P, Hiscock H, Wake M. Outcomes of infant sleep problems: a longitudinal study of sleep, behavior, and maternal well-being. Pediatrics. 2003;111:e203–7. doi: 10.1542/peds.111.3.e203. [DOI] [PubMed] [Google Scholar]
- 60.Eckerberg B. Treatment of sleep problems in families with young children: effects of treatment on family well-being. Acta Paediatr. 2004;93:126–34. doi: 10.1080/08035250310007754. [DOI] [PubMed] [Google Scholar]
- 61.Beijers R, Jansen J, Riksen-Walraven M, de Weerth C. Attachment and infant night waking: a longitudinal study from birth through the first year of life. J Dev Behav Pediatr. 2011;32:635–43. doi: 10.1097/DBP.0b013e318228888d. [DOI] [PubMed] [Google Scholar]
- 62.Zentall SR, Braungart-Rieker JM, Ekas NV, Lickenbrock DM. Longitudinal assessment of sleep–wake regulation and attachment security with parents. Inf Child Dev. 2012;21:443–57. [Google Scholar]
- 63.Meltzer LJ, Mindell JA. Sleep and sleep disorders in children and adolescents. Psychiatr Clin N Am. 2006;29:1059–76. doi: 10.1016/j.psc.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 64.Johnson CM. Infant and toddler sleep: a telephone survey of parents in one community. J Dev Behav Pediatr. 1991;12:108–14. [PubMed] [Google Scholar]
- 65.McKay P. Pink McKay; 2015. Baby sleep trainers – do you have the guts to tell them to bugger off? [Google Scholar]
- 66.Tsai S-Y, Hu W-Y, Lee Y-L, Wu C-Y. Infant sleep problems: a qualitative analysis of first-time mothers' coping experience. Midwifery. 2014;30:750–5. doi: 10.1016/j.midw.2013.08.005. [DOI] [PubMed] [Google Scholar]
- 67.Gazmararian J, Dalmida S, Merino Y, Blake S, Thompson W, Gaydos L. What new mothers need to know: perspectives from women and providers in Georgia. Matern Child Hlth J. 2014;18:839–51. doi: 10.1007/s10995-013-1308-8. [DOI] [PubMed] [Google Scholar]
- 68.Simard V, Nielsen TA, Tremblay RE, Boivin M, Montplaisir JY. Longitudinal study of preschool sleep disturbance: the predictive role of maladaptive parental behaviors, early sleep problems, and child/mother psychological factors. Arch Pediatr Adol Med. 2008;162:360–7. doi: 10.1001/archpedi.162.4.360. [DOI] [PubMed] [Google Scholar]
- 69.Williams CD. The elimination of tantrum behavior by extinction procedures. J Abnorm Soc Psychol. 1959;59:269. doi: 10.1037/h0046688. [DOI] [PubMed] [Google Scholar]
- 70.Rolider A, Van Houten R. Training parents to use extinction to eliminate nighttime crying by gradually increasing the criteria for ignoring crying. Educ Treat Child. 1984;7:119–24. [Google Scholar]
- 71.McKenna JJ. Cultural influences on infant and childhood sleep biology and the science that studies it. In: Loughlin G, Carroll JL, Marcus CL, editors. Toward a more inclusive paradigm, in sleep and breathing in children: a developmental approach. New York, NY: Marcel Dekker; 2000. pp. 199–230. [Google Scholar]
- 72.Gaylor EE, Burnham MM, Goodlin-Jones BL, Anders TF. A longitudinal follow-up study of young children's sleep patterns using a developmental classification system. Behav Sleep Med. 2005;3:44–61. doi: 10.1207/s15402010bsm0301_6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Tikotzky L, Sadeh A. Maternal sleep-related cognitions and infant sleep: a longitudinal study from pregnancy through the 1st year. Child Dev. 2009;80:860–74. doi: 10.1111/j.1467-8624.2009.01302.x. [DOI] [PubMed] [Google Scholar]
- 74.Germo GR, Chang ES, Keller MA, Goldberg WA. Child sleep arrangements and family life: perspectives from mothers and fathers. Inf Child Dev. 2007;16:433–56. [Google Scholar]
- 75.Keller MA, Goldberg WA. Co-sleeping: help or hindrance for young children's independence? Inf Child Dev. 2004;13:369–88. [Google Scholar]
- 76.Bessey M, Coulombe JA, Smith IM, Corkum P. Assessing parental sleep attitudes and beliefs in typically developing children and children with ADHD and ASD. Child Hlth Care. 2013;42:116–33. [Google Scholar]
- 77.McKenna JJ, McDade T. Why babies should never sleep alone: a review of the co-sleeping controversy in relation to SIDS, bedsharing and breast feeding. Paediatr Respir Rev. 2005;6:134–52. doi: 10.1016/j.prrv.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 78.Jenni OG, O'Connor BB. Children's sleep: an interplay between culture and biology. Pediatrics. 2005;115:204–16. doi: 10.1542/peds.2004-0815B. [DOI] [PubMed] [Google Scholar]


