Abstract
Background
Pacing in the Bachmann's bundle (BB) area (upper atrial septum) appears superior to right atrial appendage or free wall stimulation for the prevention of paroxysmal atrial fibrillation in patients with atrial conduction delay. However, insertion of active fixation lead in the upper atrial septal position is difficult and time consuming with conventional stylet, inhibiting application of this pacing method in routine practice.
Methods
The technique of positioning the atrial lead in BB with hand-made stylet is presented with emphasis on electrocardiographic P-wave pattern and fluoroscopic landmarks.
Results
The results demonstrate an acute implantation and short-term success of BB pacing of 14 patients out of 15 patients without major complications. Pacing parameters at implantation and 3 months postprocedure were noted which were within normal limits.
Conclusion
These favorable initial results indicate that the positioning of active fixation atrial lead in BB with fluoroscopic landmarks is feasible and reproducible with a simple technique.
Keywords: Pacing, Bachmann's bundle, Hand-made stylet
1. Introduction
The conventional site for placement of right atrial (RA) lead in right atrial appendage (RAA) had been challenged as inadequate and nonphysiological in patients with inter- and intra-atrial conduction delay as it has been shown to result in a higher incidence of atrial fibrillation.1 It was believed that the prolonged time of signal conduction from high to low atrium that can occur with pacing from the RAA may play an important role in the induction of atrial fibrillation.2 In selective site atrial pacing, the atrial septum is chosen to improve intra-atrial and inter-atrial conduction and minimize dispersion of refractoriness.3 Upper atrial septal (region of Bachmann's bundle (BB)) pacing has been shown to be the method to pace both the atria simultaneously.4 This in turn may improve atrial hemodynamics and reduce the incidence of paroxysmal atrial fibrillation. In BB pacing, the target area for lead attachment is the antero-superior part or high atrial septum (Fig. 1). The area of the high RA septum involves the crista terminalis and BB, and is particularly difficult to pace with conventional tools. Special J-shaped stylets are often required. Two types of delivery systems are now available for such difficult clinical situations. The first is a steerable stylet (from St. Jude Medical). The second system builds on the concept of a catheter delivery system. A family of steerable catheters (Selectsite, Medtronic, Inc.) has been developed to guide pacing leads to selective sites. However, these devices are not always available. So, we used hand-made stylet with a single right angle curve in this study. Feasibility and safety of this hand-made stylet for BB pacing is not well validated.
Fig. 1.
Anatomical specimen showing an external view of the heart (A) and the antero-posterior view of the right atrial septum (B) The part of the atrial septum above the limbus fossa ovalis is known as upper (high) septum and the rest is lower septum. SVC = superior vena cava, IVC = inferior vena cava, TV = tricuspid valve, RAA = right atrial appendage, FO = fossa ovalis, CS = coronary sinus, US = upper septum, and LS = lower septum.
2. Method
In our hospitals, from 1st March 2014 until 30th November 2014, we had recruited 15 patients for BB pacing who were undergoing dual chamber pacemaker. We selected the patients with sinus P-wave duration of more than 100 msec (although electrocardiographically P-wave duration of more than 120 msec is considered as a marker of atrial conduction delay). With hand-shaped stylet, we positioned the atrial lead in the target area. The lead parameters (P-wave sensitivity, threshold, lead impedance) were noted during implantation and 3 months after the procedure. We used conventional active fixation leads whichever was available at the time of implantation.
After having venous access to Subclavian vein, the lead was first placed in the RAA. The position was observed in Postero-anterior and left anterior oblique fluoroscopic view, which served as the reference position, before it was moved to the BB area. The target region for the implantation of the lead in Bachman's bundle pacing was a confluence of the right atrial roof and the inter-atrial septum. The fluoroscopic criteria we used for BB pacing were: (i) the position of the lead tip in the posterior–anterior view above the RAA location, and; (ii) in the left anterior oblique view the lead tip pointing posteriorly toward the spine. To locate the Bachman's bundle region, the atrial lead was gradually pulled from atrial appendage and positioned toward the superior septum until the lead deformed, defining the roof of the right atrium in a left anterior oblique (LAO) fluoroscopic view with the help of a hand-made stylet with a single right angle curve (Fig. 2). The fluoroscope was then positioned in the right anterior oblique (RAO) view, and the lead was fixed in the anterior position. In the posterior–anterior (PA) view, the tip of the lead was slightly above the RAA location, and moved cranially in LAO view with minimal, only ‘up-and-down’ movements of the lead tip in PA view. In both LAO as well as left lateral view it faced posteriorly toward spine.
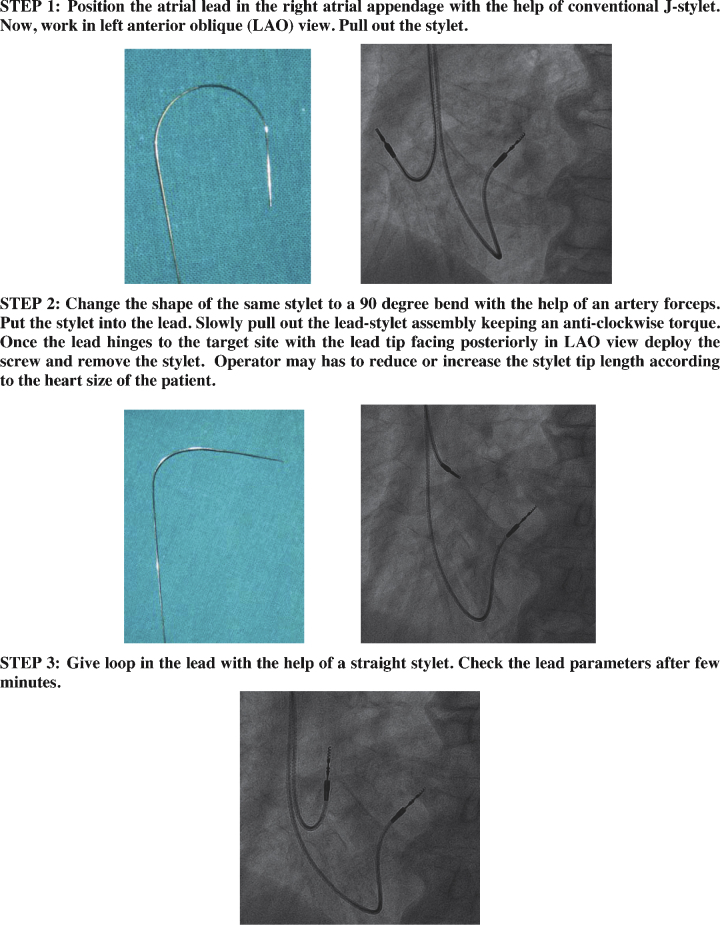
Fig. 2.
Method of Bachmann's bundle pacing. Note the ventricular lead is positioned into the interventricular septum.
The electrocardiographic criteria for BB pacing were (i) P-wave morphology: positive paced P-wave in leads I, II, and III, (ii) Absence of latency: starting immediately with the pacing spike, and (iii) P-wave duration: shorter (15–20 msec shorter than sinus P-waves measured on the 6-limb lead electrocardiogram).
Collected data were computerized and analyzed using SPSS 21 statistical package. The test was used to compare the normally distributed continuous variable between the lead parameters during implantation and 3 months postprocedure. A p value of less than 0.05 was used to indicate significance. The test was also used to analyze paced P-wave characteristics.
3. Results
Of the 15 patients, we implanted the atrial leads in high atrial septum (BB) successfully in 14 patients. In one patient, we fail to position the lead in the target area because of inaccessibility. Of these 14 patients, 8 were men and 6 were women. Mean age was 64.5 years (95% CI: 60.83–68.17). Electrocardiographic confirmation of the lead attachment to the BB region was done by noting the paced P-wave characteristics (duration, latency, and vector) in 12-lead surface ECG on 2nd postimplantation day. The ECG was taken with 50 mm/sec paper speed for better calculation of the intervals. Table 1 summarizes the paced P-wave features of these 14 patients.
Table 1.
Paced P-wave characteristics of 14 patients with pacing lead in Bachmann's bundle.
| P-wave duration (msec) |
Latency (msec) | P-wave morphology |
|||
|---|---|---|---|---|---|
| Sinus (S) | Paced (P) | Shortening (S − P) | In lead I, II, III | In lead V1 | |
| 100 | 75 | 25 | 0 | All Positive | Negative |
| 110 | 80 | 30 | 0 | All Positive | Negative |
| 130 | 105 | 25 | 0 | All Positive | Negative |
| 120 | 95 | 25 | 0 | All Positive | Negative |
| 100 | 80 | 20 | 10 | All Positive | Biphasic |
| 100 | 85 | 15 | 10 | I, II Positive, III Biphasic | Negative |
| 110 | 90 | 20 | 0 | All Positive | Negative |
| 120 | 90 | 30 | 0 | All Positive | Negative |
| 100 | 75 | 25 | 0 | All Positive | Negative |
| 105 | 90 | 15 | 10 | All Positive | Negative |
| 120 | 95 | 25 | 0 | All Positive | Negative |
| 110 | 80 | 30 | 0 | I, II Positive, III Biphasic | Biphasic |
| 100 | 75 | 25 | 0 | All Positive | Negative |
| 130 | 110 | 20 | 10 | I Positive, II, III Biphasic | Biphasic |
The mean P-wave sensitivities at implantation and 3 months postprocedure were 2.44 mA (SD: 0.59) and 2.32 mA (SD: 0.60), respectively. The change was insignificant (p value is 0.59). Mean pacing thresholds at implantation and 3 months postprocedure were 0.68 V (SD: 0.21) and 0.66 V (SD: 0.17), respectively. The change in pacing threshold was not significant (p value is 0.76). The mean lead impedances at implantation and 3 months postprocedure were 749.64 ohms (SD: 100.57) and 686.93 ohms (SD: 76.91), respectively. The changes were insignificant (p value is 0.07).
The mean shortening of paced P-wave duration was 23.57 msec with 95% CI of 20.70–26.44 msec. The two-tailed p-value (compared to an expected mean shortening of at least 20 msec) is 0.0186. This is considered to be statistically significant. The correlation of paced P-wave morphology in lead I, II, III versus lead V1 shows a value of correlation coefficient (R) of 0.5758 (<0.5 indicates poor correlation). This result indicates a moderate positive correlation, which means positive paced P-wave morphology in lead I, II, III and negative paced P-wave in lead V1 have a convergent relationship.
4. Discussion
The right and left atria are activated nearly simultaneously (within 50–80 msec) during sinus rhythm. The spread of activation within each atrium and from one atrium to the other follows preferential pathways consisting of circumferential and longitudinal muscle bundles (generally not considered to be part of the specialized conduction system) for impulse propagation.5 In a study, it has been suggested that four distinct sites serve as electrical connections between the right and the left atrium: the high septal right atrium or BB, the limbus fossa ovalis, the proximal coronary sinus musculature, and the region of Koch's triangle, with left posterior extension of the AV node.6 BB, also known as the inter-atrial bundle, is well recognized as a muscular bundle comprising of parallel aligned myocardial strands connecting the right and left atrial walls and is considered to be the main pathway of inter-atrial conduction.
Atrial conduction disorders are due to either spatial dispersion of refractory periods or anisotropy resulting from scarce side-to-side electrical coupling or discrete fibrosis disrupting the arrangement of atrial muscle fiber bundles or due to major ultrastructural abnormalities.7 Electrocardiographically, P-wave duration is traditionally measured in lead II and a value of more than 120 msec is abnormal. The ECG often shows a wide and notched P-wave in lead II together with a wide terminal negativity in V1 commonly described as left atrial enlargement. Such a configuration probably reflects atrial conduction disorder rather than biatrial or left atrial hypertrophy/dilatation.1
4.1. Effects of RAA pacing
Atrial conduction delay, either spontaneous or induced by RAA pacing, delays left atrial systole and modifies, or even in extreme cases cancels, its contribution to ventricular filling with the resultant risk of left heart AV asynchrony. As a result, this increases risk of diastolic mitral regurgitation and atrial fibrillation. Besides the reduction or loss of atrial contribution and the proportional reduction of overall cardiac performance, delayed left atrial contraction may also induce major neurohumoral changes that contribute to lowering blood pressure through atrial reflexes activated by increased atrial stretch and pressure causing elevation of atrial natriuretic peptides.8 These hemodynamic disorders are particularly important when inter-atrial conduction delay is long, shifting atrial systole after the beginning of ventricular contraction and against a closed mitral valve, resulting in a derangement similar to 1:1 ventriculoatrial conduction during ventricular pacing.
Bachmann's bundle plays an important role in initiation and perpetuation of atrial tachyarrhythmias. Structural changes of BB may cause longitudinal dissociation in conduction of adjacent muscle fibers, thereby facilitating reentry and hence development of AF. Data obtained from clinical studies suggest a relationship between electro-pathological alterations of BB and the development of atrial fibrillation. RAARAA pacing is employed to treat Sinus node dysfunction and suppress atrial fibrillation, but may further aggravate the atrial physiology that underlies these conditions and may worsen atrial dyssynchrony.2, 9, 10 Pacing the inter-atrial septum at either upper part (BB region) or at lower part (above the coronary sinus ostium) has been advocated to achieve or maintain atrial synchrony and prevent atrial fibrillation.11, 12 Study suggests the Bachman's bundle should be considered the preferred site for atrial pacing in patients with a history of paroxysmal atrial fibrillation.13
4.2. Advantages of BB pacing
The main benefits that this selective site for right atrial pacing provides are (1) a very short inter-atrial conduction delay and a significant decrease in P-wave duration; (2) a reduction in dispersion of atrial refractoriness; (3) a more homogeneous recovery of excitability and atrial activation; and (4) electrical atrial remodeling, with a gradual reduction in left atrial diameters and volume.14, 15, 16
Studies have yielded conflicting results. Most of the studies have shown beneficial results of BB pacing in terms of atrial fibrillation incidence and recurrence in patients with sinus node dysfunction.
One recent study indicated that BB stimulation is a safe and feasible procedure, but it does not seem to provide significant benefit for prevention of paroxysmal atrial fibrillation 17, 18. The physiological nature of the BB has been questioned also by another recent study in canine model.19 The investigators have shown that both Bachmann’ bundle and coronary sinus ostial pacing induce left atrial electrical dyssynchrony. But, establishing clinical impact requires evaluation of human data. The variability in results may be attributable to the difficulty in confirming the location or positioning the lead near Bachmann’ bundle.
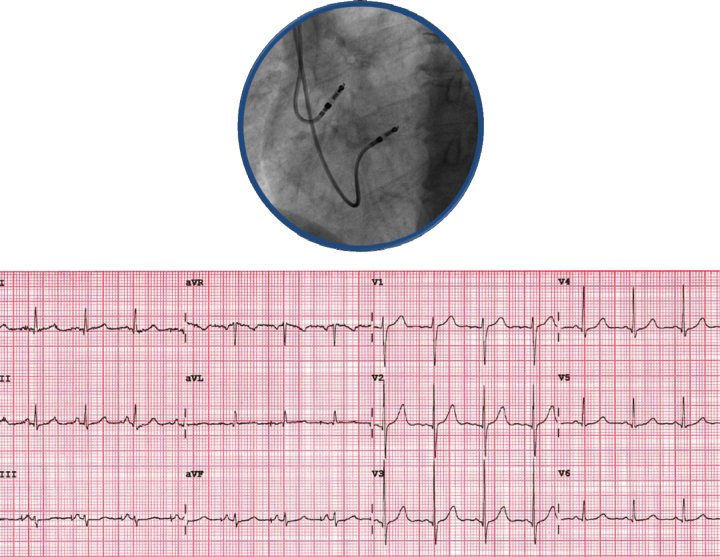
5. Electrocardiographic characteristics
During evaluation of a patient with atrial pacing, the 12-lead ECG yields important information about the site of pacing as well as the effect of pacing on atrial depolarization in terms of duration and vectoral change. The P-wave normally appears entirely upright in leftward and inferiorly oriented leads, such as I, II, III, aVF, and V4 to V6. It is negative in aVR because of the rightward orientation of that lead and is variable in other standard leads. In RAA pacing, atrial muscle bundles take considerable time to propagate the stimulation from RAA to the right atrial free wall and then to the crista terminalis and whole right atrium and subsequently to the left atrium across the atrial septum. So, there is a marked latency period with prolonged paced P-wave (equal or more than the sinus P-wave duration), specifically if there is inter- and intra-atrial conduction delay.20 The typical P-wave morphology in RAA pacing shows an inferior vector in the frontal plane and it is almost identical to sinus rhythm morphology with a terminal negative deflection in lead V1 and is caused by the normal activation sequence of the atria, right before left (Fig. 3). In BB pacing (junction of the roof right atrium atrial septum), the wave of depolarization rapidly traverses to the left atrium via the bundle and excites the left atrium and in the right atrium via crista terminalis to the whole right atrium. So, there is no latency (starting immediately with the pacing spike) period and the P-wave duration is short (shorter than the sinus P-wave; expected to be 15–20 msec shorter than sinus P-waves) (Fig. 4).21 In BB pacing, the paced P-wave is positive in leads I, II, and III, and a small negative deflection in lead V1 (Fig. 5). Lead V1 distinguishes left- versus right-sided cardiac activity. The divergence of right and left atrial activation normally produces a biphasic P-wave (initial positive deflection for right atrial and second negative deflection for left atrial activity). In BB pacing, because of its typical pattern of propagation of the atrial depolarization wave, left atrium gets stimulated little earlier or may be simultaneous with the right atrium resulting in a small negative deflection in lead V1. However, during implantation it is little difficult to get lead V1. So, paced P-wave morphology in lead V1 can be used as an additional marker to confirm the location of atrial lead in BB area subsequently.
Fig. 3.
Right atrial appendage pacing: fluoroscopic left anterior oblique view and 12-lead surface ECG.
Fig. 4.
Bachmann's bundle pacing: mechanism of impulse propagation – spread of activation wave-front and appearance of P-wave in 6-lead surface ECG during BB pacing in 50 mm/sec speed. In Bachmann's bundle pacing, the wave of depolarization rapidly crosses to the left atrium through the bundle itself, limbus fossa ovalis, along the proximal coronary sinus musculature, and extension from AV node. Along the Crista terminalis, the impulse gets propagated longitudinally in the right atrium. Thus, the left atrium gets stimulated simultaneously or may be little earlier with the right atrium and results in short and sharp P-wave with minimal or no latency period.
Fig. 5.
Bachmann's bundle pacing: fluoroscopic left anterior oblique view and 12-lead surface ECG in another patient.
Delivering the atrial lead to the BB region (upper atrial septum) is difficult with conventional stylets. Special tools like steerable stylet or steerable catheters are required frequently. But, these equipments are not widely available. Some previous studies have showed the feasibility of BB pacing with conventional tools.16 The method of BB pacing with conventional stylets is not well elucidated. Our study showed that the BB pacing is feasible and reproducible with a simple technique (hand-made stylet).
The major limitation of the present study was the relatively small sample size. So, the results may not be generalized. We followed up the patients for short term (for only 3 months). Another major drawback of this study was that it did not include data collection during follow-up with respect to the occurrence of atrial arrhythmia and pacing burden. Further studies that involve larger sample of patients and follow-up for a longer time are required to confirm the present findings. Finally, we relied on fluoroscopic and electrocardiographic features for confirmation of the lead position in BB. However, we did not confirm the position with other imaging modalities or electrophysiologic signal.
Conflicts of interest
The authors have none to declare.
References
- 1.Daubert J.C., Pavin D., Jauvert G., Mabo P. Intra- and interatrial conduction delay: implications for cardiac pacing. Pacing Clin Electrophysiol. 2004;27:507–525. doi: 10.1111/j.1540-8159.2004.00473.x. [DOI] [PubMed] [Google Scholar]
- 2.Epstein A.E., DiMarco J.P., Ellenbogen K.A., Estes N.A., 3rd American College of Cardiology/American Heart Association Task Force on Practice Guidelines; American Association for Thoracic Surgery; Society of Thoracic Surgeons: ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to revise the ACC/AHA/NASPE 2002 guideline update for implantation of cardiac pacemakers and antiarrhythmia devices): developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic Surgeons. Circulation. 2008;117:e350–e408. doi: 10.1161/CIRCUALTIONAHA.108.189742. [DOI] [PubMed] [Google Scholar]
- 3.Kindermann M., Schwaab B., Berg M., Frohlig G. The influence of right atrial septal pacing on the interatrial contraction sequence. Pacing Clin Electrophysiol. 2000;23:1752–1757. doi: 10.1111/j.1540-8159.2000.tb07012.x. [DOI] [PubMed] [Google Scholar]
- 4.Spencer W.H., Zhu D.W., Markowitz T., Badruddin S.M., Zoghbi W.A. Atrial septal pacing: a method for pacing both atria simultaneously. Pacing Clin Electrophysiol. 1997;20:2739–2745. doi: 10.1111/j.1540-8159.1997.tb05431.x. [DOI] [PubMed] [Google Scholar]
- 5.Bachmann G. The inter-auricular time interval. Am J Physiol. 1907;1:1. [Google Scholar]
- 6.Leclercq J.F., DeSisti A., Fiorello P. Is dual site better than single site atrial pacing in the prevention of atrial fibrillation? PACE. 2000;23:2101. doi: 10.1111/j.1540-8159.2000.tb00783.x. [DOI] [PubMed] [Google Scholar]
- 7.van Campenhout M.J.H., Yaksh A., Kik C. Bachmann's bundle: a key player in the development of atrial fibrillation? Circ Arrhythm Electrophysiol. 2013;7:1041–1046. doi: 10.1161/CIRCEP.113.000758. [DOI] [PubMed] [Google Scholar]
- 8.Strangl K., Weil J., Seitz K. Influence of AV synchrony on the plasma levels of atrial natriuretic peptide (ANP) in patients with total AV block. PACE. 1988;11:1176–2118. doi: 10.1111/j.1540-8159.1988.tb03969.x. [DOI] [PubMed] [Google Scholar]
- 9.Eicher J.C., Laurent G., Mathé A. Atrial dyssynchrony syndrome: an overlooked phenomenon and a potential cause of ‘diastolic’ heart failure. Eur J Heart Fail. 2012;14:248–258. doi: 10.1093/eurjhf/hfr169. [DOI] [PubMed] [Google Scholar]
- 10.Adelstein E., Saba S. Right atrial pacing and the risk of post implant atrial fibrillation in cardiac resynchronization therapy recipients. Am Heart J. 2008;155:94–99. doi: 10.1016/j.ahj.2007.08.030. [DOI] [PubMed] [Google Scholar]
- 11.Yasuoka Y., Abe H., Umekawa S. Interatrial septum pacing decreases atrial dyssynchrony on strain rate imaging compared with right atrial appendage pacing. Pacing Clin Electrophysiol. 2011;34:370–376. doi: 10.1111/j.1540-8159.2010.02976.x. [DOI] [PubMed] [Google Scholar]
- 12.Bailin S.J., Adler S., Giudici M. Prevention of chronic atrial fibrillation by pacing in the region of Bachmann's bundle: results of a multicenter randomized trial. J Cardiovasc Electrophysiol. 2001;12:912–917. doi: 10.1046/j.1540-8167.2001.00912.x. [DOI] [PubMed] [Google Scholar]
- 13.Bailin S.J. Is Bachmann's bundle the only right site for single-site pacing to prevent atrial fibrillation? Results of a multicenter randomized trial. Card Electrophysiol Rev. 2003;7:325–328. doi: 10.1023/B:CEPR.0000023131.13609.ab. [DOI] [PubMed] [Google Scholar]
- 14.Noguchi H., Kumagai K., Tojo H. Effect of Bachmann's bundle pacing on atrial fibrillation: electrophysiologic assessment. Clin Cardiol. 2004;27:50–53. doi: 10.1002/clc.4960270113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chavan C., Karmalkar M., Badani R. Evaluation of Bachmann bundle pacing versus right atrial pacing in prevention of atrial fibrillation after coronary artery bypass surgery. Indian Pacing Electrophysiol J. 2010;10:529–535. [PMC free article] [PubMed] [Google Scholar]
- 16.Bailin S.J., Machado C., Nsah E. Bachmann's bundle versus right atrial appendage capture. PACE. 2003;26:264–267. doi: 10.1046/j.1460-9592.2003.00029.x. [DOI] [PubMed] [Google Scholar]
- 17.Nigro G., Russo V., Politano L. Does Bachmann's bundle pacing prevent atrial fibrillation in myotonic dystrophy type 1 patients? A 12 months follow-up study. Europace. 2010;12:1219–1223. doi: 10.1093/europace/euq170. [DOI] [PubMed] [Google Scholar]
- 18.Hermida J-.S., Carpentier C., Kubala M. Atrial septal versus atrial appendage pacing: feasibility and effects on atrial conduction, interatrial synchronization, and atrioventricular sequence. Pacing Clin Electrophysiol. 2003;26:26–35. doi: 10.1046/j.1460-9592.2003.00146.x. [DOI] [PubMed] [Google Scholar]
- 19.Choudhuri I., Krum D., Agarwal A. Bachmann's bundle and coronary sinus ostial pacing accentuate left atrial electrical dyssynchrony in an acute canine model. J Cardiovasc Electrophysiol. 2014;25:1400–1406. doi: 10.1111/jce.12511. [DOI] [PubMed] [Google Scholar]
- 20.Goyal S.B., Spodick D.H. Electromechanical dysfunction of the left atrium associated with interatrial block. Am Heart J. 2001;142:823–827. doi: 10.1067/mhj.2001.118110. [DOI] [PubMed] [Google Scholar]
- 21.Kristensen L., Nielsen J.C., Mortensen P.T. Sinus and paced P wave duration and dispersion as predictors of atrial fibrillation after pacemaker implantation inpatients with isolated sick sinus syndrome. PACE. 2004;27:606–614. doi: 10.1111/j.1540-8159.2004.00494.x. [DOI] [PubMed] [Google Scholar]