Heat waves have been responsible for more deaths worldwide than all other natural disasters combined.1 In Europe, this “silent killer” caused 70000+ excess deaths in 2003, and more recently 3500+ people died during 2 separate heat waves in India (May 2015) and Pakistan (June 2015) (Fig. 1). Groups among the most vulnerable include the elderly, poor, and people with cardiovascular disease.1 Identifying simple and cost-effective cooling strategies are therefore an urgent priority. In this Discovery article, we highlight our study2 which was the first to assess the efficacy of the humble electric fan for mitigating cardiovascular and thermal strain in humans during simulated heat wave conditions. Despite the high cooling capacity of air conditioners (AC), the millions of tonnes of CO2 they generate annually potentially contribute to a vicious cycle of worsening future heat waves.3 Mass AC-use has also led to electricity blackouts or brownouts during heat waves, and in some cases catastrophic exacerbations in morbidity and mortality.4 By contrast, electric fans have an electricity requirement that is 50-fold lower than conventional AC units (55-100 W vs 1500-5000 W).
Figure 1.
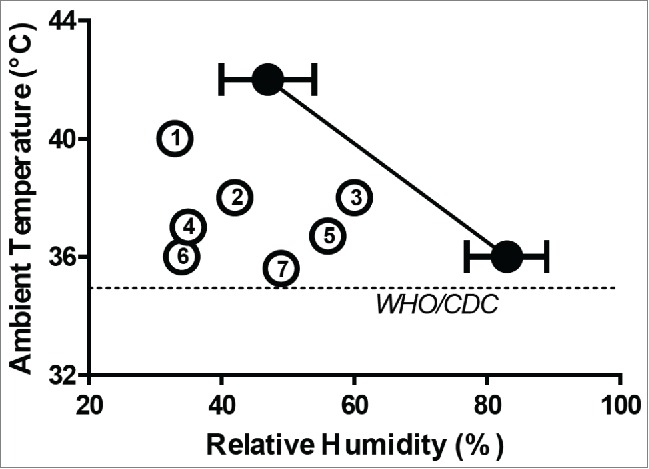
Mean critical environmental limits (with SD) for elevations in heart rate with fan use measured at 36°C and 42°C (solid circles). The dashed line represents the environmental limits for fan use proposed by the World Health Organization (WHO) and the Center for Disease Control and Prevention (CDC). Numbered circles identify the peak environmental conditions during some of the most severe recent heat waves; Karachi, Pakistan 2015 (1); New Delhi, India 2007 (2); Dhahran, Saudi Arabia 2003 (3); Paris, France 2003 (4); Chicago, USA 1999 (5); Frederick, USA 2010 (6); Washington, USA 2012 (7).
In South Korea, fans are equipped with an off-timer due to the unsubstantiated belief held since the mid-1920s that prolonged fan use can lead to asphyxiation. Meanwhile, all major international public health agencies warn against fan use during heat waves due to a similarly unsupported belief that they paradoxically increases the risk of heat related illness. Specifically, the World Health Organization (WHO) and Centers for Disease Control and Prevention (CDC) state that electric fan use above ∼35°C will critically exacerbate dehydration and “speed the onset” of heat exhaustion. In stark contrast, a 2012 Cochrane review3 identified that no empirical evidence exists to support or refute the use of fans in heat waves.
In order to maintain body temperature, the human body must balance the rate of internal heat production with the rate of heat dissipation to the surrounding environment. One avenue of heat dissipation is sensible heat transfer, which in indoor environments primarily occurs via convection, following the temperature gradient between the skin surface and ambient air. When ambient air is less than skin temperature (∼35°C), heat flows away from the body, but when the ambient air exceeds skin temperature this gradient is reversed and heat is instead added to the body.5 Since convective heat transfer increases sharply with increases in air velocity, more heat flows in to the body with forced air movement (e.g. with a fan).
“Not only do (fans) not work, they actually make (the risk of overheating) worse. We compare (fans) to a convection oven. By blowing hot air on a person, it heats them up rather than cools them down.” – Director of the Environmental Hazards and Health Effects Program at the CDC, USA (Scientific American, July 23, 2010).
While convection in a hot [190°C (375°F)] oven is the ideal environment for cooking the main component of a typical thanksgiving dinner, there are two major limitations to this analogy. Firstly, the hottest day ever recorded on Earth was 57.6°C in Death Valley, California; a far cry from the interior of a conventional cooking vessel. Second and most importantly, humans are able to physiologically wet their skin surface with sweat secreted primarily from eccrine glands and the evaporation of this sweat promotes latent heat loss. Evaporation is enhanced greatly with higher air velocities, leading to the evaporation of sweat that would otherwise sit on the skin or drip off the body altogether and provide no cooling. However, sweat evaporation is greatly dependent on ambient humidity meaning that under more humid conditions fan use may not prevent heat related elevations in heart rate and core temperature.
We compared the maximum ambient humidity that could be physiologically tolerated with and without fan use at 36°C and 42°C – the range of temperatures typically experienced during heat waves.5 Eight young healthy males wearing a t-shirt and shorts sat for 135 minutes facing an 18” diameter electric fan set at maximum speed (∼4 m/s) from a distance of 1.0 m. The ambient humidity at which an upward inflection in heart rate (HR) and then in core temperature (Tcore) were identified in each trial using an incremental humidity ramp protocol starting at 1.6 kPa and ending at 5.6 kPa. At 36°C, the ambient temperature above which the use of electric fans is discouraged by public health agencies, a clear benefit of electric fan use was evident. Specifically, the critical humidity for elevations in HR was much higher with a fan (4.9 ± 0.4 kPa, 83 ± 6% RH; Fig. 1) than without (3.7 ± 0.5 kPa, 62 ± 9% RH; P<0.001); whereas elevations in Tcore were observed in only 2 of 8 participants with fan use, but 7 of 8 participants without fan use. At 42°C, which is ∼7°C above the current recommendation for fan use worldwide, benefits of fan use, albeit of a smaller magnitude, were still observed for HR (fan: 3.8 ± 0.6 kPa, 47 ± 7% RH; no fan: 3.1 ± 0.6 kPa, 38 ± 7% RH; P=0.01; Fig. 1) and Tcore (fan: 4.5 ± 0.5 kPa, 55 ± 6% RH; no fan: 3.9 ± 0.7 kPa, 48 ± 9% RH; P=0.04). In support of greater latent cooling, whole body sweat loss was greater with a fan at 36°C (fan: 398 ± 23 g, no fan: 337 ± 39 g; P=0.01) and 42°C (fan: 882 ± 58 g, no fan: 532 ± 102 g; P<0.001).
In summary, we clearly demonstrate the benefits of fan use during simulated heat wave conditions, however our findings do not yet apply to individuals with compromised thermoregulatory responses such as the elderly, or to very dry environments where the complete evaporation of sweat would occur even without fan use. Nevertheless, other simultaneous cooling strategies such as wetting the skin or garments with water may further improve the efficacy of fan use for different subpopulations in different types of heat waves. While fan use may hasten dehydration, based on our findings this can be easily negated by drinking between 25 to 175 ml/h of water. In sum, simply turning on a fan may yet prove to be an affordable and sustainable strategy for cooling down in a heat wave.
References
- [1]. Luber G, et al. Am J Prev Med 2008; 35:429–35; PMID:18929969; http://dx.doi.org/ 10.1016/j.amepre.2008.08.021 [DOI] [PubMed] [Google Scholar]
- [2]. Ravanelli NM, et al. J Am Med Assoc 2015; 313:724–5; http://dx.doi.org/ 10.1001/jama.2015.153 [DOI] [PubMed] [Google Scholar]
- [3]. Gupta S, et al. Cochrane Database Syst Rev 2012; 7:CD009888; PMID:22786530; http://dx.doi.org/ 10.1002/14651858.CD009888.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4]. WHO Heatwaves and Health: Guidance on Warning-System Development Geneva. 2015. [Google Scholar]
- [5]. Jay O, et al. Applied Ergonomics 2015; 43:137–43; http://dx.doi.org/ 10.1016/j.apergo.2014.07.013 [DOI] [PubMed] [Google Scholar]


