ABSTRACT
Purpose: To examine the retention and re-acclimation responses during a periodized heat acclimation (HA) protocol in elite sailors preparing for the 2013 World Championships in Muscat, Oman (∼27–30°C, 40–60% RH). Methods: Two elite male Laser class sailors completed 5 consecutive days of HA (60 min per day in 35°C, 60% RH). Heat response tests (HRT) were performed on day 1 and 5 of HA, then 1 (decay 1, D1) and 2 (D2) weeks following HA. Participants were then re-acclimated (RA) for 2 days, within the next week, before a final HRT ∼72 h post-RA. Rectal temperature, plasma volume, heart rate, sweat rate, as well as thermal discomfort and rating of perceived exertion were measured during each HRT. Results: Rectal temperature decreased with HA (0.46 ± 0.05°C), while individual responses following D1, D2 and RA varied. Heart rate (14 ± 7 bpm), thermal discomfort (0.6 ± 0.1 AU) and rating of perceived exertion (1.8 ± 0.6 AU) decreased across HA, and adaptations were retained by D2. Plasma volume steadily increased over the decay period (D2 = 8.0 ± 1.3%) and after RA (15.5 ± 1.1%) compared with baseline. RA resulted in further thermoregulatory improvements in each Athlete, although individual adjustments varied. Conclusion: Heat strain was reduced in elite Laser sailors following HA and most thermoregulatory adaptations were retained for 2 weeks afterwards. RA may ‘top up’ adaptations after 2 weeks of HA decay.
KEYWORDS: elite, heat, performance, periodization, re-acclimation, sailing
Introduction
Short-term heat acclimation is a commonly used strategy to prepare athletes for competition in hot environments and typically involves 4–7 days of aerobic training in artificially hot conditions (30–40°C).1 The physiological adaptations seen with heat acclimation (HA) include decreased resting and exercise core temperatures, lowered skin temperature, increased plasma volume and sweat rate and a decreased heart rate for a given workload, all of which attenuate performance impairments that are caused by hot conditions in the unacclimated state.2 An acute training session in the heat causes considerable physiological strain 3 which, accumulated over several days during HA, could misalign with training priorities during an athlete's taper phase leading in to a major competition. While some suggest incorporating HA to a precompetition taper,4,5 the added heat-induced stress may require a reduction in training intensity,6 which could hinder taper objectives where athletes often reduce training volume and increase or maintain training intensity.7 Moreover, training in hot conditions may cause an unplanned rise in internal training load.8 Therefore, examining alternate application models of HA periodization in athletes preparing for competitions in the heat is needed.
The time course of heat acclimation and re-acclimation is not yet clear in trained populations.4 Studies with untrained participants have shown that re-acclimation following moderate-term HA (8–14 d) may occur after only a short number of heat exposures (1–4 d).9,10 Highly-trained individuals may have even faster rates of HA accrual and slower rates of HA decay.11 Furthermore, it has been suggested that periodical exposure to heat following HA can allow for the retention of HA over several weeks,12 however, supporting data in athletes is lacking. The aim of this study was to examine the retention of HA adaptations and re-acclimation responses during a periodized short-term HA protocol in elite sailors preparing for the 2013 Laser World Championships in Muscat, Oman (∼27–30°C, 40–60% RH).
Methods
Participants
Two male elite Laser class sailors, who were members of the New Zealand Sailing Team, volunteered to participate in this descriptive study. The athletes (mean ± SD: age 22.5 ± 0.7 years, height 185.5 ± 3.5 cm, weight 81.4 ± 0.7 kg, maximal oxygen consumption (O2max) 60.4 ± 5.5 ml kg−1min−1 at 420 ± W) provided written informed consent for the study, which was ethically approved through the Auckland University of Technology Research Ethics Committee.
Experimental design
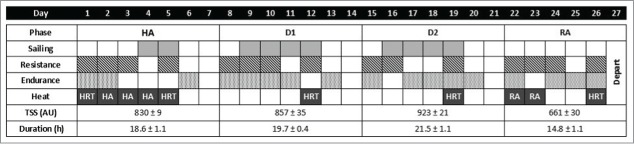
The study involved the observation of responses over a periodized 4-week training mesocycle, which included 3 heavy-load training weeks followed by 1 recovery week (Fig. 1). Training volume and duration were recorded using an online monitoring system to determine weekly training load via the training stress score (TSS; TrainingPeaks, Boulder, Colorado). HA consisted of 5 consecutive days cycling in hot conditions (35°C, 60% RH) for 45–60 min at a power output to elicit a heart rate response corresponding to 60–70% O2max. To assess the thermoregulatory response to HA, heat response tests (HRT) were performed on day 1 and 5 of HA, as well as 1 (decay 1, D1) and 2 weeks (D2) post HA, and finally 3 d post RA. The study took place during Auckland's winter where the daily ambient temperature was 12–18°C. During the 2-week decay period, all training sessions apart from the weekly HRT were performed indoors (19–20°C) or outdoors in cooler conditions.
Figure 1.
Overview of the periodized heat acclimation (HA) protocol used for 2 elite Laser sailors preparing for the World Championships in Oman. A 4-week mesocycle included 3 heavy-build weeks and 1 recovery week (TSS = training stress score). HA (35°C, 65% RH) occurred during the first week with a heat response test (HRT) on day 1 and 5 of HA. HRTs were repeated during the two following weeks of decay (D1 and D2), and 3 d post re-acclimation (RA).
Heat response test
All HRTs were conducted in the afternoon at the same time of day as HA sessions (15:00), while resting blood samples were taken at 08:00 prior to any routine morning training sessions. Each HRT consisted of 30-min walking (5.5 km h−1 and 10% incline) in an environmental chamber (35°C, 60% RH; Design Environmental, Wales, UK). Rectal temperature, measured to 0.01°C, was continuously recorded with a data logger (Squirrel SQ2020, Cambridge, UK) connected to a probe (Thermistor 400, Mon-a-Therm, Mansfield MA, USA) and self-inserted ∼12 cm past the anal sphincter. Heart rate was recorded every 15 s, while rating of perceived exertion (RPE) and thermal discomfort were recorded at 5-min intervals. Sweat rate was estimated using the change in total body mass (shorts only, body dried; Weightec, Albany, NZ) that occurred during the HRT and was measured to 0.01 kg. Participants then remained in the heat chamber and completed 45 min of submaximal cycling on an ergometer (SRM Indoortrainer, Jülich, Germany), clamped to an RPE of 13, without heart rate or power output feedback. Power output was recorded every 0.5 s, and heart rate as described above. Power to heart rate ratio was calculated to determine power output changes relative to the cardiovascular response. The combination of the HRT followed by submaximal cycling was considered as a HA exposure on days 1 and 5.
Blood sample
On each testing day, athletes were instructed to consume 500 ml of water before arriving for their morning blood sample, at which point they sat for 20 min to allow plasma stability. Resting blood samples were collected via venepuncture in K2EDTA vacutettes (Greiner Bio-One, Mon-a-Therm Kremsmunster, Austria). The samples were immediately refrigerated and analyzed in triplicate within 1 h for red blood cell count, haematocrit and haemoglobin concentration (AcT 5diff, Beckman Coulter, Miami FL, USA). Estimated change in plasma volume (PV) with HA was calculated using the Dill and Costill equations.13
Statistical analysis
All physiological and perceptual data collected during the 30 min HRTs and individual mean power output during 45 min of cycling post HRT are presented as the means ± SDs for each athlete (A and B). The average weekly training duration, for both athletes combined, is presented as mean ± SD (n = 2). The differences in power output, physiological and subjective measurements were analyzed using a magnitude-based inference approach.14 This method is used to indicate the possible benefit or harm of each trial. The smallest worthwhile change (SWC) in rectal temperature and plasma volume changes were based off the typical error of published reliability data,15 while the SWC for heart rate, RPE and cycling power output were calculated from multiple baseline measurements used to determine the coefficient of variation within an athlete. Changes in sweat rate were determined using a SWC score (6.1%) based on results from a similar HA protocol conducted at our laboratory (J Casadio, 2013; unpublished data). Thereafter, chances of change scores within an individual due to HA, decay and RA were determined using published spreadsheets (xPrecisionSubject.xls) found at sportsci.org.16 Thresholds for quantitative chances to assess whether a change was clinically increased, clinically decreased or clinically trivial were described as follows: <1%, almost certainly not; 1–5%, very unlikely; 5–25%, unlikely; 25–75%, possible; 75–95%, likely; 95–99%, very likely; >99% almost certainly.14 When an effect was >5% for both benefit and harm, the true value of the difference was described as unclear. Pearson's product moment correlation analysis was used to assess the association between PV change and submaximal power output. The magnitude of the correlation (r) between these measures was defined as: <0.1, trivial; 0.1–0.3, small; >0.3–0.5, moderate; >0.5–0.7, large; >0.7–0.9, very large; and >0.9–1.0, almost perfect.14
Results
Initial HA adaptations were similar in both athletes (Fig. 2), with reductions in mean HRT rectal temperature (Athlete A = 71% possible; Athlete B = 83% likely decrease), heart rate (Athlete A = 94% likely; Athlete B = 74% possible decrease), and RPE (Athlete A = 100% almost certain; Athlete B = 94% likely decrease) compared with baseline. Physiological and perceptual HA adaptations were retained at D1 (trivial change, D1 vs. HA), and D2 (trivial change, D2 vs. HA), with the exception of mean rectal temperature in Athlete A (55% possible increase, D1 vs. HA; 66% possible increase, RA vs. HA). Compared with baseline values, PV increased substantially at each time point (99% very likely to 100% almost certain) following HA in Athlete B, and following D1 in Athlete A. Average power output during submaximal exercise increased meaningfully above baseline following RA (very likely increase Athlete A = 97%; Athlete B = 98%; Table 1). Mean heart rate during submaximal cycling decreased in both athletes (likely to almost certain), following HA, decay and RA compared with baseline values. Compared with baseline values, Athlete A showed trivial changes with HA and RA, and a 69% possible decrease in sweat rate during the two week decay period (D1 and D2 = 0.28 L · h−1) (Fig. 2). Following RA, Athlete A showed a 95% very likely increase (0.52 L · h−1) in sweat rate compared with D2. Sweat rate changes for Athlete B were 94% very likely to 100% almost certainly trivial at all-time points compared with pre HA values.
Figure 2.
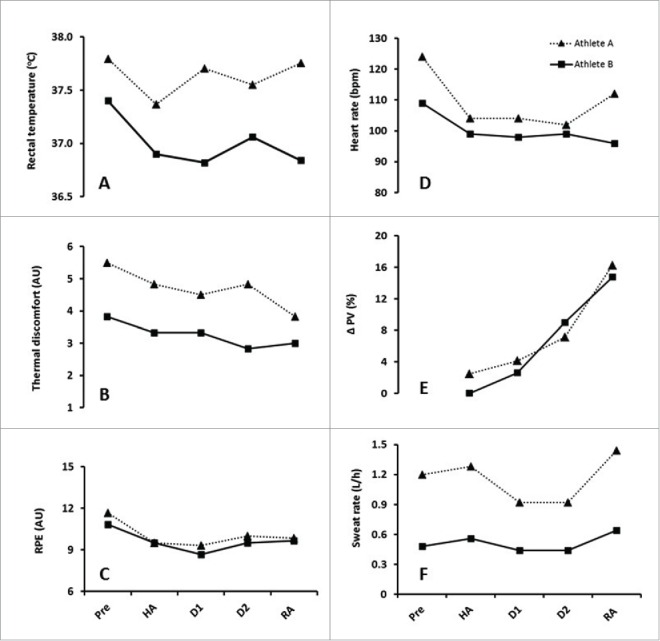
Mean physiological and psychophysical changes (rectal temperature, A; thermal discomfort, B; rating of perceived exertion (RPE), C; heart rate, D; plasma volume change (PV), E; and sweat rate, F) during a heat response test in hot conditions (35°C, 60% RH) from before (pre), to after heat acclimation (HA), and after 1 and 2 weeks decay (D1, D2) and 2-d re-acclimation (RA) in two elite Laser sailors (Athlete A & Athlete B).
Table 1.
Individual mean power output, heart rate (HR) and power to HR ratio (Power: HR) during 45 min cycling at a clamped RPE of 13 in hot conditions (35°C, 60% RH) in elite male Laser sailors (n = 2) before (Pre), after heat acclimation (HA), after 1 (D1) and 2 (D2) weeks decay and after re-acclimation (RA).
| Power (W) |
HR (bpm) |
Power : HR (W/b) |
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Athlete A | Athlete B | Athlete A | Athlete B | A | B | |||||||||||||
| Pre | 211 | ± | 17 | 216 | ± | 27 | 156 | ± | 14 | 143 | ± | 10 | 1.37 | ± | 0.21 | 1.52 | ± | 0.24 |
| HA | 206 | ± | 8 | 210 | ± | 9 | 135 | ± | 6**** | 133 | ± | 8** | 1.53 | ± | 0.08 | 1.59 | ± | 0.14 |
| D1 | 188 | ± | 30 | 215 | ± | 17 | 142 | ± | 4*** | 135 | ± | 5** | 1.33 | ± | 0.23 | 1.59 | ± | 0.16 |
| D2 | 207 | ± | 11 | 210 | ± | 11 | 136 | ± | 11**** | 134 | ± | 9** | 1.54 | ± | 0.12 | 1.58 | ± | 0.16 |
| RA | 230 | ± | 20*** | 237 | ± | 4*** | 138 | ± | 6**** | 135 | ± | 4** | 1.68 | ± | 0.16 | 1.86 | ± | 0.16 |
D1 = 1 week decay, D2 = 2 week decay, HA = heat acclimation, RA = re-acclimation. Pre vs. following HRT time points.
almost certain increase (power output) or decrease (HR).
very likely increase or decrease.
likely increase or decrease.
Discussion
The key observations made from this study were that following HA, most thermoregulatory adaptation markers appeared retained following 2 weeks of training in thermoneutral conditions within the athlete's normal training environment, and that only 2 days of RA returned several of these markers to near the level attained after 5 days of HA. Although there were individual variances during decay and RA phases, these results provide practitioners with a useful model to consider to enable both HA and essential training elements within an athlete's training program.
HA induced the expected thermoregulatory and cardiovascular adaptations, including reduced rectal temperature (Athlete A = 0.42°C; Athlete B = 0.50°C), heart rate (Athlete A = 20 bpm; Athlete B = 10 bpm), RPE (Athlete A = 2.2 AU; Athlete B = 1.3 AU) and thermal discomfort (Athlete A = 0.67 AU; Athlete B = 0.50 AU) (Fig. 2). These results compare with Garrett et al. (2012) who used a similar 5-d HA protocol in a highly-trained population (Rowers; V02max = 65 ± 3 ml kg−1 min−1 at 400 W) and showed reductions in heart rate (14 bpm), core temperature (0.30°C), and 2000-m rowing ergometer time (1.5%) in the heat. In the current study, with the exception of rectal temperature, most HA adaptations (heart rate, RPE, thermal discomfort) were retained in both athletes at 1 and 2 weeks following HA. A lower rectal temperature was retained over 2 weeks in Athlete B, but not Athlete A, highlighting the individual nature of HA responses (Fig. 2A). In both athletes, sweat rate adjustments were shown to be trivial, which is in line with other short-term HA studies,17-20 and serves as a reminder to practitioners that sudomotor adaptations require moderate-term HA (8–14 d).2
The retention of most HA adaptations shown in the current study are similar to other studies showing that many thermoregulatory adaptations can be retained for up to 2–3 weeks in active to highly-trained men.9,11 Our findings differ, however, from those of Garrett et al.,15 who showed decayed adaptations at 2 weeks post-HA in moderately-trained men.15 Two consecutive days of RA showed further thermoregulatory improvements with additional reductions in thermal discomfort, as well as rectal temperature and heart rate (Athlete B only). Plasma volume continued to increase with RA in both athletes, while sweat rate was enhanced in Athlete A. The ability to re-adapt or make further gains with only 2 d has been shown previously,9,11 but never in highly-trained athletes and supports the concept that heat acclimated individuals may acquire thermal ‘memory’ as evident through rapid RA.21
This study also showed comparable rises in both PV and submaximal power output in the heat over the 4-week training block. While a substantial increase in PV was not shown immediately following HA (Athlete A = 2.5%; Athlete B = 0.0%), meaningful PV expansion was shown as training volume continually increased at D2 (Athlete A = 7.1%; Athlete B = 9.0%; 100% almost certain increase) and following RA (Athlete A = 16.2%; Athlete B = 14.7%; 100% almost certain increase), and may be attributed to a sustained high-volume training load (TSS = 860–920 AU) during the HA decay period. Power output during submaximal cycling (∼ aerobic threshold) was similar (within 5–12 W) following HA and during the decay period, but increased in both athletes (20 W; very likely increase) following RA during the reduced volume week prior to departure (Table 1). While the relationship between PV expansion and aerobic performance in the literature is unclear,22 our findings showed a very large (r = 0.70) relationship between PV change and submaximal power output. While supercompensation following heavy-build weeks and a subsequent download week cannot be ignored,23 this increase was larger than what is normally seen in these athletes during a focused sailing block, where aerobic gains are not expected, thus highlighting the potential ergogenic ‘boost’ that frequent HA sessions could produce within an athlete's season.4
Practical applications
This study demonstrates that HA can be scheduled up to 3 weeks before departing for competition in a hot environment, when accompanied with ‘top up’ RA sessions. As adding environmental stress to training is an additive physiological stressor, and could cause an increase in internal training load, potentially leading to overreaching,8,24 the approach shown in the present study could allow athletes and coaches to periodize the timing of HA so as to reduce interference with more critical training goals. Specifically, we suggest that implementing HA 2–3 weeks prior to competing in a hot environment, along with 2 additional RA sessions, may preserve precompetition taper quality while restoring HA adaptations, thus serving as an alternative and possibly more appropriate HA strategy for elite athletes. Finally, while adaptations followed a similar time course between the two athletes in this study, individual variances during the decay and RA period were noted, highlighting the importance of considering individual athlete responses.
Conclusion
Short-term HA decreased heat strain in two elite Laser sailors through decreased rectal temperature, heart rate, RPE and thermal discomfort. Most thermoregulatory adaptations were retained over the 2 subsequent weeks, without HA, except for rectal temperature in one athlete. Additional RA sessions provided further thermoregulatory enhancement with varied responses between the two athletes. The results of this study suggest that RA may be used to ‘top up’ heat tolerance adaptations after 2 weeks of decay from HA. Further investigation involving greater subject samples is needed to confirm these observations.
Abbreviations
- AU
Arbitrary units
- D1
Decay 1
- D2
Decay 2
- HA
Heat acclimation
- HR
Heart rate
- HRT
Heat response test
- PV
Plasma volume
- RA
Re-acclimation
- RH
Relative humidity
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
Acknowledgments
The authors would like to thank the athletes for their time in participating in this study and the use of their data.
References
- [1].Garrett AT, Creasy R, Rehrer NJ, Patterson MJ, Cotter JD. Effectiveness of short-term heat acclimation for highly trained athletes. Eur J Applied Physiol 2012; 112:1827-37; http://dx.doi.org/ 10.1007/s00421-011-2153-3 [DOI] [PubMed] [Google Scholar]
- [2].Armstrong LE, Maresh CM. The induction and decay of heat acclimatisation in trained athletes. Sports Med 1991; 12:302-12; PMID:1763248; http://dx.doi.org/ 10.2165/00007256-199112050-00003 [DOI] [PubMed] [Google Scholar]
- [3].Périard JD, Cramer MN, Chapman PG, Caillaud C, Thompson MW. Cardiovascular strain impairs prolonged self-paced exercise in the heat. Exp Physiol 2011; 96:134-44; http://dx.doi.org/ 10.1113/expphysiol.2010.054213 [DOI] [PubMed] [Google Scholar]
- [4].Chalmers S, Esterman A, Eston R, Bowering KJ, Norton K. Short-term heat acclimation training improves physical performance: a systematic review, and exploration of physiological adaptations and application for team sports. Sports Med 2014; 44:971-88; PMID:24817609; http://dx.doi.org/ 10.1007/s40279-014-0178-6 [DOI] [PubMed] [Google Scholar]
- [5].Périard JD, Racinais S, Sawka MN. Adaptations and mechanisms of human heat acclimation: applications for competitive athletes and sports. Scandinavian J Med Sci Sports 2015; 25:20-38; http://dx.doi.org/ 10.1111/sms.12408 [DOI] [PubMed] [Google Scholar]
- [6].Pyne DB, Mujika I, Reilly T. Peaking for optimal performance: Research limitations and future directions. J Sports Sci 2009; 27:195-202; PMID:19153861; http://dx.doi.org/ 10.1080/02640410802509136 [DOI] [PubMed] [Google Scholar]
- [7].Mujika I, Padilla S. Scientific bases for precompetition tapering strategies. Med Sci Sports Exercise 2003; 35:1182-7; http://dx.doi.org/ 10.1249/01.MSS.0000074448.73931.11 [DOI] [PubMed] [Google Scholar]
- [8].Crowcroft S, Duffield R, McCleave E, Slattery K, Wallace LK, Coutts AJ. Monitoring training to assess changes in fitness and fatigue: The effects of training in heat and hypoxia. Scandinavian J Med Sci Sports 2015; 25:287-95; http://dx.doi.org/ 10.1111/sms.12364 [DOI] [PubMed] [Google Scholar]
- [9].Weller AS, Linnane DM, Jonkman AG, Daanen HAM. Quantification of the decay and re-induction of heat acclimation in dry-heat following 12 and 26 days without exposure to heat stress. Eur J Applied Physiol 2007; 102:57-66; http://dx.doi.org/ 10.1007/s00421-007-0563-z [DOI] [PubMed] [Google Scholar]
- [10].Wyndham CH, Jacobs GE. Loss of acclimatization after six days of work in cool conditions on the surface of a mine. J Appl Physiol 1957; 11:197-8; PMID: 13475163908323 [DOI] [PubMed] [Google Scholar]
- [11].Pandolf KB, Burse RL, Goldman RF. Role of physical fitness in heat acclimatisation, decay and reinduction. Ergonomics 1977; 20:399-408; PMID:908323; http://dx.doi.org/ 10.1080/00140137708931642 [DOI] [PubMed] [Google Scholar]
- [12].Moseley PL. Heat shock proteins and heat adaptation of the whole organism. J Appl Physiol 1997; 83:1413-7; PMID: 937530023215944 [DOI] [PubMed] [Google Scholar]
- [13].Dill DB, Costill DL. Calculation of percentage changes in volumes of blood, plasma, and red cells in dehydration. J Appl Physiol 1974; 37:247-8; PMID: 485085423215944 [DOI] [PubMed] [Google Scholar]
- [14].Hopkins WG, Marshall S, Batterham A, Hanin J. Progressive statistics for studies in sports medicine and exercise science. Med Sci Sports Exercise 2009; 41:3; http://dx.doi.org/ 10.1249/MSS.0b013e31818cb278 [DOI] [PubMed] [Google Scholar]
- [15].Garrett AT, Goosens NG, Rehrer NG, Patterson MJ, Cotter JD. Induction and decay of short-term heat acclimation. Eur J Appl Physiol 2009; 107:659-70; http://dx.doi.org/ 10.1007/s00421-009-1182-7 [DOI] [PubMed] [Google Scholar]
- [16].Hopkins WG. How to interpret changes in an athletic performance test. Sport Sci 2004; 8:1-7 [Google Scholar]
- [17].Brade C, Dawson B, Wallman K. Effect of precooling and acclimation on repeat-sprint performance in heat. J Sports Sci 2013; 31:779-86; PMID:23215944; http://dx.doi.org/ 10.1080/02640414.2012.750006 [DOI] [PubMed] [Google Scholar]
- [18].Chen TI, Tsai PH, Lin JH, Lee NY, Liang MT. Effect of short-term heat acclimation on endurance time and skin blood flow in trained athletes. Open Access J Sports Med 2013; 4:161-70; PMID:24379721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Petersen CJ, Portus MR, Pyne DB, Dawson BT, Cramer MN, Kellett AD. Partial heat acclimation in cricketers using a 4-day high intensity cycling protocol. Int J Sports Physiol Performance 2010; 5:535-45 [DOI] [PubMed] [Google Scholar]
- [20].Cotter JD, Patterson MJ, Taylor NAS. Sweat distribution before and after repeated heat exposure. Eur J Appl Physiol 1997; 76:181-6; http://dx.doi.org/ 10.1007/s004210050232 [DOI] [PubMed] [Google Scholar]
- [21].Horowitz M. Heat acclimation: phenotypic plasticity and cues to the underlying molecular mechanisms. J Thermal Biol 2001; 26:357-63; http://dx.doi.org/ 10.1016/S0306-4565(01)00044-4 [DOI] [Google Scholar]
- [22].Corbett J, Neal RA, Lunt HC, Tipton MJ. Adaptation to heat and exercise performance under cooler conditions: a new hot topic. Sports Med 2014; 44:1323-31; PMID:24943043; http://dx.doi.org/ 10.1007/s40279-014-0212-8 [DOI] [PubMed] [Google Scholar]
- [23].Fry RW, Morton AR, Keast D. Periodisation of training stress: a review. Canadian J Sport Sci 1992; 17:234-40 [PubMed] [Google Scholar]
- [24].Taylor NAS, Cotter JD. Heat adaptation: Guidelines for the optimisation of human performance. Int Sport Med J 2006; 7:33-57. [Google Scholar]