Supplemental Digital Content is available in the text
Keywords: diabetes mellitus, elderly, hypoglycemia
Abstract
The objective of this study was to carry out a large population-based study to understand the factors associated with hypoglycemia-related hospitalizations among older Korean adults with diabetes mellitus.
This study analyzed data from a subset of the 2013 Health Insurance and Review and Assessment service-Adult Patient Sample. A total of 307,170 subjects, comprising 41.7% men and 58.3% women, had diabetes mellitus. Hypertension (80.8%) was the most common comorbidity, and dyslipidemia (59.0%) and ischemic heart disease (21.3%) were also prevalent. Approximately half of the patients with diabetes had >2 comorbidities, and two-thirds of the patients had >3 comorbidities. The proportion of patients taking insulin or sulfonylureas was 54.9%, and 23.2% of the patients were taking other medications. About 21.9% of the patients were treated nonpharmacologically. A total of 2867 hypoglycemia-related admission occurred, the incident rate was 9.33 per 1000 person. The risk was higher among female patients and older patients with several comorbidities, including cardiovascular disease, cerebrovascular disease, chronic liver disease, chronic kidney disease, dementia, and malignancies. Treatment modalities, including insulin and sulfonylureas, were associated with a high risk of hypoglycemia. After adjustments for age, sex, the different comorbidities, and the treatment modalities, we determined that chronic kidney disease and dementia were associated with a high risk of hypoglycemia-related hospitalization (odds ratio [OR] = 2.52 and OR = 1.93, respectively). Furthermore, patients with chronic kidney disease or dementia who were treated with sulfonylureas and insulin had very high risks of hypoglycemia, and the incident rate was 66.6 and 63.75 per 1000 person, respectively.
In conclusion, the presence of comorbidities, especially chronic kidney disease and dementia, increased the risk of hypoglycemia-associated hospitalization within this population of older patients with diabetes. The impact of the treatment modality, for example, insulin or sulfonylureas, on hypoglycemia was much greater among these patients.
1. Introduction
Diabetes mellitus is highly prevalent within populations of older people.[1] Recent Korean epidemiologic data show that there has been a noticeable increase in the prevalence of diabetes mellitus, particularly among older people.[2] Since older patients with diabetes mellitus have particular characteristics, for example, the diabetes duration and the presence of comorbidities, the approach to the treatment of these patients should differ from the treatment approach used for younger patients with diabetes mellitus,[3] and the most serious problem is that older people with diabetes mellitus are very susceptible to hypoglycemia.
Hypoglycemia is a major obstacle that hinders the achievement of glycemic targets in patients with diabetes mellitus.[4] Hypoglycemia can be a life-threatening complication of diabetes mellitus, and it is a major risk factor that is associated with a variety of diabetic complications.[5,6] Furthermore, the frequency and severity of hypoglycemic events negatively impact upon the quality of patients’ lives, promoting a fear of future hypoglycemic episodes, which is associated with a reduction in a patient's ability to care for themselves and poor glucose control.[7] Since the risks of older patients having comorbidities, for example, impaired renal function and cognitive impairment, and poor nutritional statuses are higher, they are much more susceptible to hypoglycemia.[8] Also, compared with younger people, older adults with diabetes are less likely to be able to sense the warning signs associated with hypoglycemia, and the medical and financial burdens related to hypoglycemic events are much greater for older patients than they are for younger patients.[9]
For those reasons, the recent guidelines for the management of older adults with diabetes include less intensive and individualized targets to lower the risk of hypoglycemia.[10] However, most of the statements are derived from experts’ opinions, the evidence supporting these statements is limited, and a substantial level of uncertainty surrounds the detailed management plans.
The aim of this study was to gain an understanding of real-world approaches to the treatment of older people with diabetes. We undertook a large population-based study that investigated the comorbid conditions, the treatment strategies, and the factors associated with hypoglycemia-related hospitalizations among patients with diabetes mellitus who were >65 years. Furthermore, we evaluated the interactions among the different comorbidities and the treatment modalities and their impacts upon the risk of hypoglycemia in the same population.
2. Methods
2.1. Data source
Data for this population-based study came from the Health Insurance Review & Assessment services (HIRA) database; the national database of longitudinal integrated health care claims data covering entire Korean population (∼50 million people). The HIRA is a government-affiliated agency that reviews and assesses healthcare costs and healthcare service quality, as well as operating healthcare information system for supporting research in related national organization and the academia.[11] The various HIRA datasets are in the public domain and available upon request to researchers for health-related studies (http://www.hira.or.kr; http://opendata.hira.or.kr). We obtained the 2013 HIRA-Adult Patient Sample (HIRA-APS), which were constructed by a stratified random sampling method for gender and age interval of 5 year from patients aged 65 years or older who had healthcare institution visits in 2013.[12] The HIRA-APS contained information regarding 1,161,198 elderly patients (∼20% sample of whole Korean patients aged 65 or older). It includes information on patient demographics, diagnosis, prescription drugs, and type of type of medical utilization (outpatient, inpatient, or emergency department). The diagnoses were coded according to the International Classification of Disease, Tenth Revision (ICD-10). In compliance with the Act on the Protection of Personal Information Maintained by Public Agencies, patient data were fully de-identified, which made this project exempt from the requirement for institutional review board approval.
2.2. Study population
The study population consisted of elderly patients with type 2 diabetes who had 2 or more healthcare institution visits with a diagnosis of type 2 diabetes (ICD-10: E11–14) during the study period between 1 January 2013 and 31 December 2013. The prevalence of the following co-morbid conditions was assessed: hypertension, dyslipidemia, cerebrovascular diseases, cardiovascular disease (ischemic heart diseases or heart failure), chronic kidney disease (CKD), chronic liver disease (CLD), dementia, malignancies, and alcohol-related disorders. A patient was classified as a patient with each comorbidity if he or she had 2 or more healthcare institution visits with corresponding diagnosis codes (see Table, Supplemental Content, which illustrates code lists of each comorbidity) during the study period. The Charlson comorbidity index was also calculated by a method proposed by Quan et al.[13]
2.3. Treatment modality and hypoglycemic event
We categorized the types of diabetes treatment into 3 groups based on the risk of hypoglycemia with the treatment, as follows: pharmacological treatment with insulin or sulfonylureas, pharmacological treatment with neither insulin nor sulfonylureas, and nonpharmacological treatment. We defined insulin or sulfonylureas users as patients with at least 1 prescription for a sulfonylurea or insulin during the study period, patients with pharmacological treatment with neither insulin nor sulfonylureas as those who had at least 1 any other antihyperglycemic medication (except for insulin and sulfonylureas) during study period, and patient with nonpharmacological treatment as those who had no evidence of anti-hyperglycemic prescription (any insulin or oral agent) during the study period. We also captured specific antidiabetic medication classes (metformin, sulfonylureas, thiazolidinediones [TZDs], a-glucosidase inhibitors, meglitinides, dipeptidyl peptidase-4 [DPP-4] inhibitors, insulin, and glucagon-like peptide-1 [GLP-1] receptor agonists) that patients used in this time period.
Hypoglycemic events were defined as hospitalization or a visit to an emergency department with a primary diagnosis of hypoglycemia (ICD-10 codes E11.63, E12.63, E13.63, E14.63, E16.0, E16.1, E16.2, and T38.3). Patients with at least 1 hypoglycemic event during the study period were identified.
2.4. Statistical analysis
Descriptive statistics were used to summarize the baseline characteristics of elderly patients with type 2 diabetes (gender, age, health insurance type, presence of hypertension, dyslipidemia, cerebrovascular disease, chronic kidney disease, ischemic heart diseases, heart failure, CKD, CLD, dementia, malignancies, and alcohol-related disorders). Using the chi-square test, we compared differences of the types of diabetes treatment according to the presence of co-morbid conditions of interest, including CKD, CLD, cardiovascular disease, cerebrovascular disease, dementia, and malignancies. Cumulative incidence of hypoglycemia-related hospitalization was calculated on the stratification of study population by gender, age group, health insurance type, comorbidities, and the types of diabetes treatment. Logistic regression analysis was performed to evaluate the effect of each characteristic on hypoglycemia-related hospitalization. Adjusted odds-ratios with 95% confidence intervals of hypoglycemia-related hospitalization for use of medication compared to nonpharmacological treatment were calculated using multivariable logistic regression model. To determine the effect of different comorbidities and treatment options on hypoglycemia-related hospitalization, incidence rates were calculated according to the total number of comorbidities and types of treatment options. We also conducted an additional analysis in study patients with comorbid conditions associated with very high risks of hypoglycemia, CKD, and dementia.[8] Incidence rate of hypoglycemia-related hospitalization in these patients were calculated according to the presence of each comorbid condition, insulin, or sulfonylureas use.
All statistical analyses were performed using SAS software Version 9.4 (SAS Institute Inc., Cary, NC).
3. Results
3.1. Baseline characteristics of the older people with diabetes mellitus
Table 1 presents the baseline demographic characteristics of the study population that comprised 307,170 patients with diabetes mellitus. Within the study cohort, 41.7% of the patients were male, and 57.8% of the patients were aged between 65 years and 75 years. Most of the patients (88.4%) were covered by national health insurance. Hypertension (80.8%) was the most common comorbidity, followed by dyslipidemia (59.0%), ischemic heart disease (21.3%), CLD (18.8%), and cerebrovascular disease (15.5%). Around 10% of the patients had dementia, and 4.4% of the patients had CKD.
Table 1.
Baseline characteristics of the study participants.
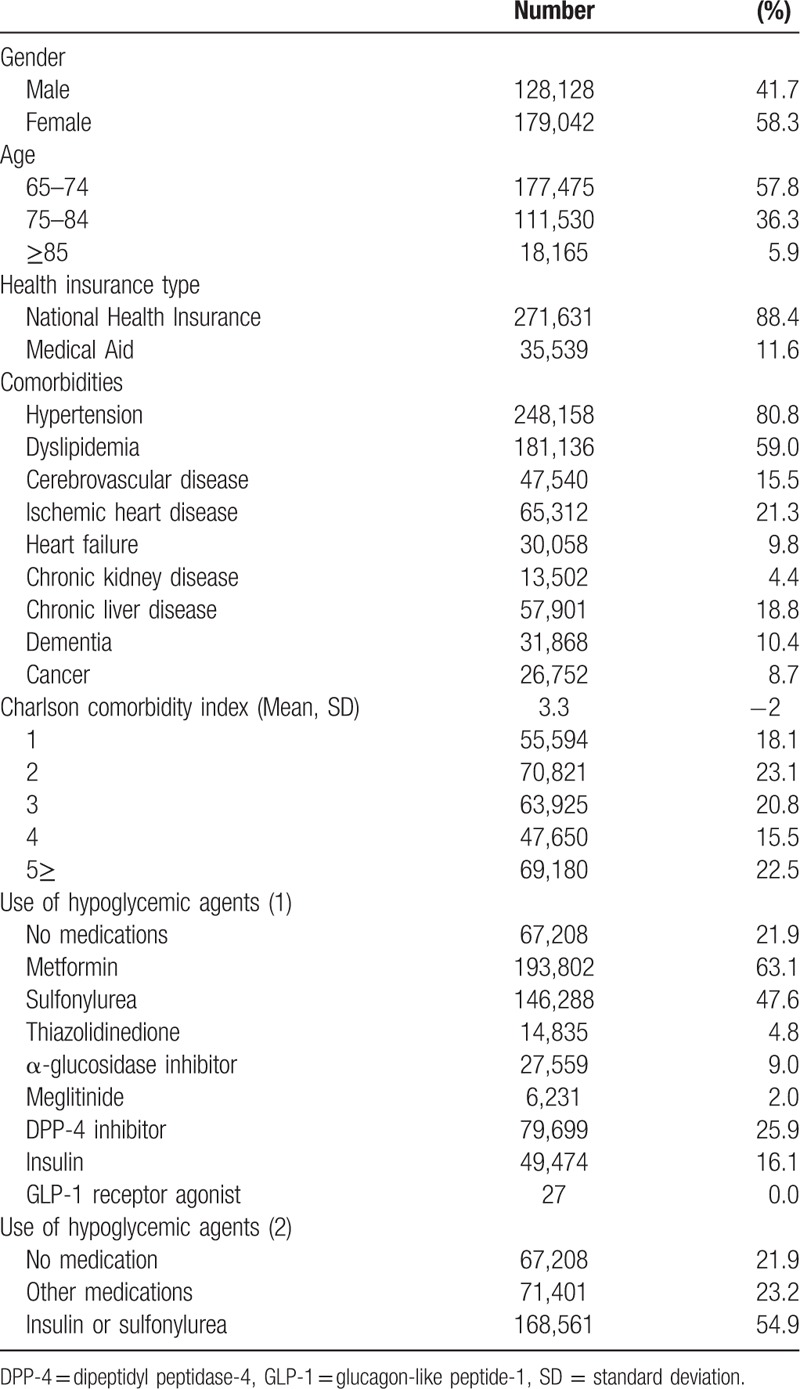
With respect to pharmacological treatments, 63.1% of the study population received metformin, 47.6% of the population received sulfonylureas, 25.9% of the population received DPP-4 inhibitor, and 16.1% of the population used insulin. TZDs and GLP-1 receptor agonists were less frequently prescribed to older patients, with frequencies of 4.8% and <1%, respectively. About 21.9% of the patients were treated nonpharmacologically.
3.2. Treatment modalities in older diabetic patients with specific comorbidities
We compared the treatment modalities used to manage older diabetic patients with different comorbidities. Since there are about 10 treatment options for diabetes, we categorized the options into 3 groups based on the risk of hypoglycemia associated with the treatment, as follows: pharmacological treatment with insulin or sulfonylureas, pharmacological treatment with neither insulin nor sulfonylureas, and nonpharmacological treatment. Patients with CKD were more likely to be administered insulin or sulfonylureas compared with those who did not have CKD (68.2% vs 54.3%, P < 0.01). Differences in the approaches to treatment were also apparent in patients with cardiovascular disease, cerebrovascular disease, or any type of malignancy; however, the difference was greatest between the patients who had and did not have CKD. The proportions of nonpharmacologically treated patients were higher among the patients with CLD or dementia, and these patients were less likely to be treated with insulin or sulfonylureas (Fig. 1).
Figure 1.
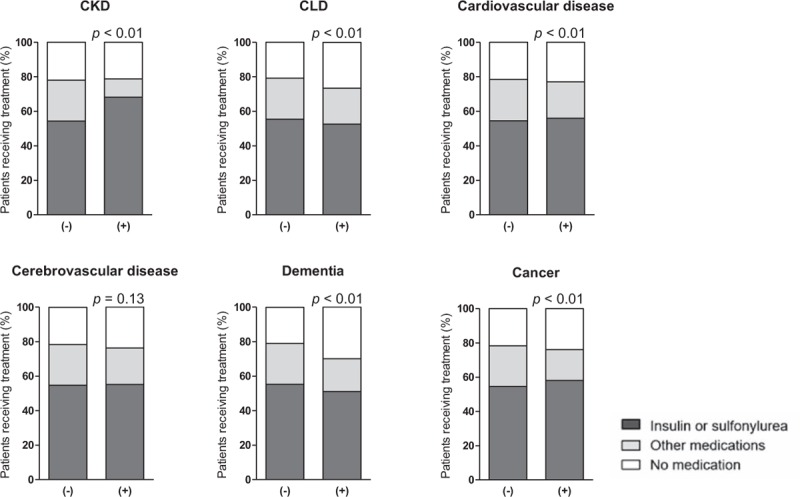
Comparison of treatment modality according to the presence of medical comorbidities in elderly patients with diabetes mellitus. CKD = chronic kidney disease, CLD = chronic liver disease.
3.3. Risk of hypoglycemia-related hospitalization among older diabetic patients
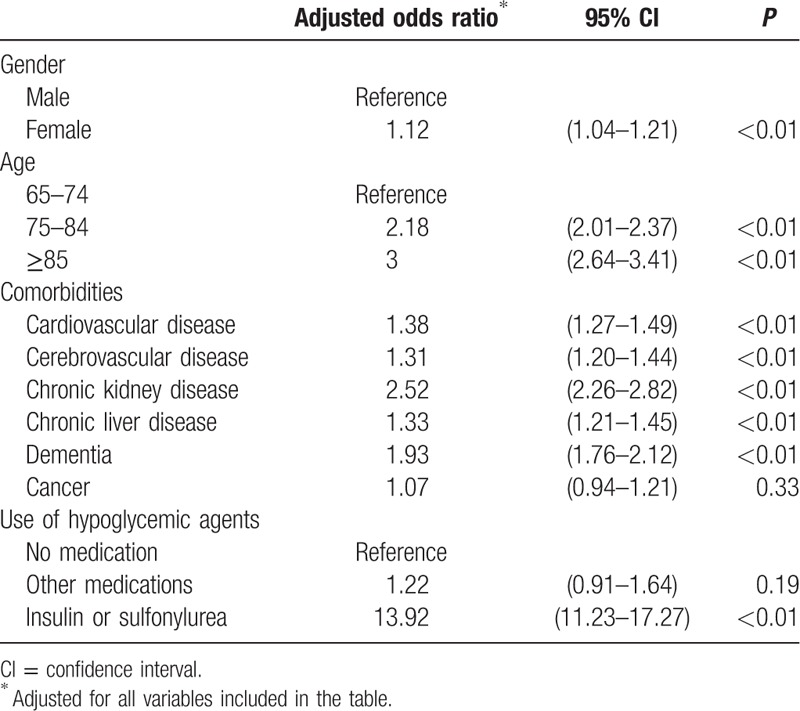
A total of 2867 hypoglycemia-related admission occurred, the incident rate being 9.33 per 1000 person. Being female, being older, having insurance that was covered by medical aid, the presence of different comorbidities, the total number of comorbidities, and the use of insulin or sulfonylureas were associated with higher numbers of hypoglycemia-related hospitalization events in the older diabetic population (Table 2). After adjusting for the different variables, being female, being older, and the presence of several comorbid conditions, including cardiovascular disease, cerebrovascular disease, CKD, CLD, and dementia, were associated with hypoglycemia-related hospitalization events. Among the comorbidities, CKD and dementia were strong risk factors for hypoglycemia (odds ratio [OR] = 2.52 and OR = 1.93, respectively). Insulin or sulfonylurea treatment was definitively associated with hypoglycemia (OR = 13.92) (Table 3).
Table 2.
Risk of hypoglycemia-related hospitalization in elderly diabetic patients.
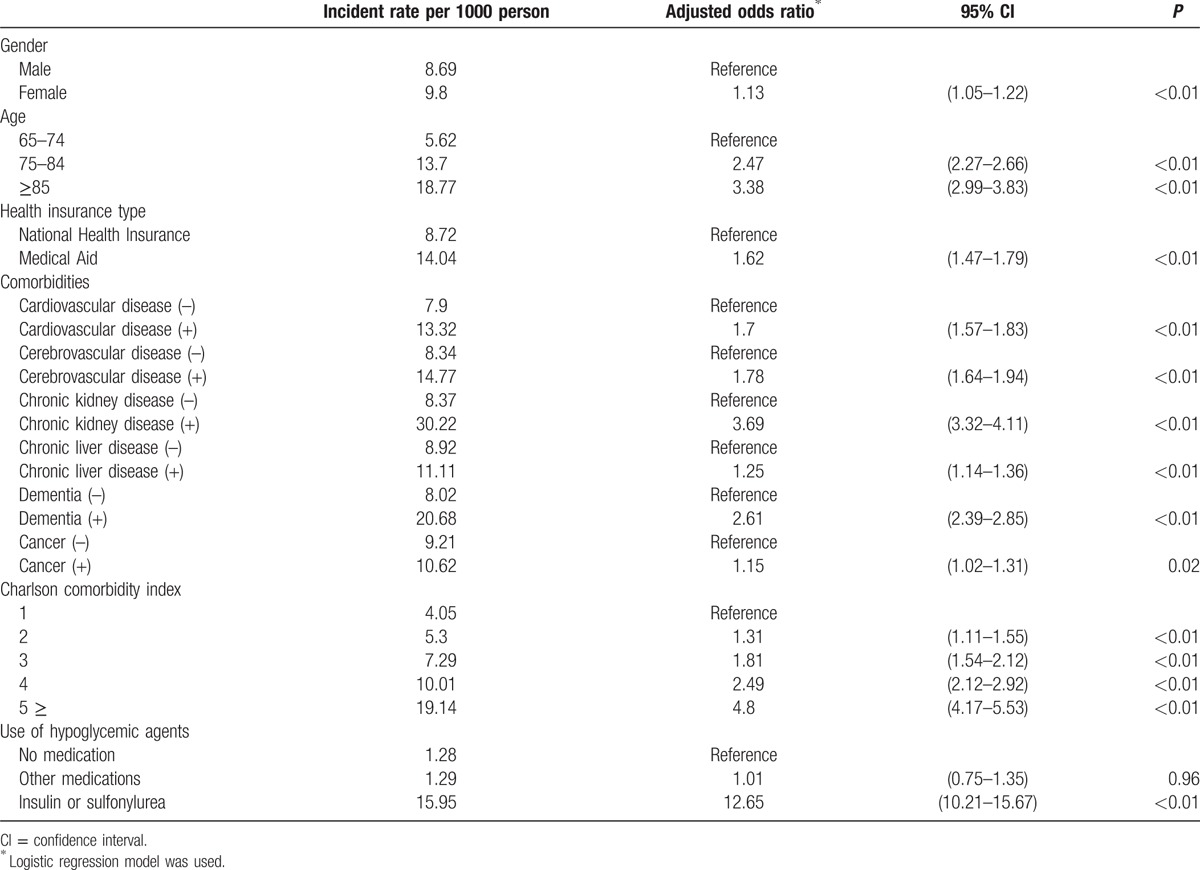
Table 3.
Multivariable logistic regression analysis for hypoglycemia-related hospitalization.
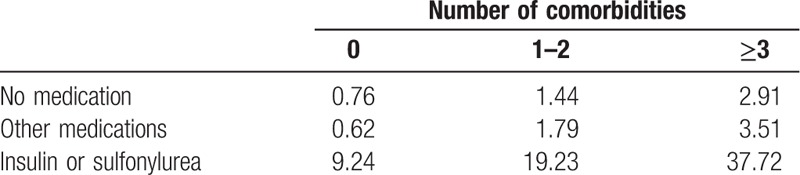
Furthermore, we analyzed the effects of the total number of comorbid conditions and the treatment options on hypoglycemia-related hospitalization events. In patients who had diabetes and did not have any comorbidity, the risk of hypoglycemia was very low, the incidence rate was 0.76 per 1000 person, if they were treated either nonpharmacologically or with medications other than insulin nor sulfonylureas. Insulin or sulfonylurea treatment increased the hypoglycemia-related risk by 12 times, the incident rate being 9.24 per 1000 person. If a diabetic patient had >3 comorbid conditions, they had a 3.8-times greater risk of hospitalization as a consequence of spontaneous hypoglycemia compared with patients without comorbidities. If a patient was treated with insulin or sulfonylureas, they had a 13-times greater risk of hospitalization as a consequence of spontaneous hypoglycemia (2.91 vs 37.72 per 1000 person) (Table 4).
Table 4.
Incidence rate of hypoglycemia-related hospitalizations according to the treatment modalities and medical comorbidities in elderly patients with diabetes.
3.4. Influence of the comorbid conditions and the treatment modalities on the risk of hypoglycemia-related hospitalization among older diabetic patients
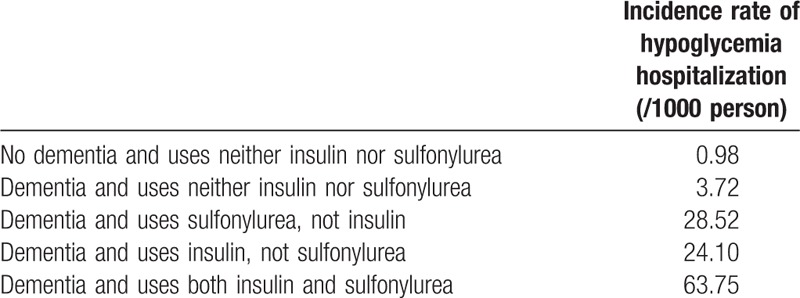
We evaluated the influence of the treatment modalities on hypoglycemia-related hospitalization among the patients with comorbid conditions that were associated with very high risks of hypoglycemia. The incidence of hypoglycemia was 1.18 per 1000 people among the patients whose kidney function was normal and who did not use insulin or sulfonylureas. There was a 4-fold increase in the incidence of hypoglycemia among the diabetic patients with CKD who did not use insulin or sulfonylureas. Using either insulin or sulfonylureas increased the risk of hypoglycemia by about 30 times. There was a >60-times greater risk of hypoglycemia among older patients with CKD who used insulin and sulfonylureas compared with patients who did not have CKD and did not use insulin or sulfonylureas (1.18 vs 66.6 per 1000 person) (Table 5). Dementia had similar effects on the risk of hypoglycemia-related hospitalization. Older diabetic patients with dementia who used insulin only, sulfonylureas only, or insulin and sulfonylureas, had markedly increased risks of hypoglycemia-related hospitalization (Table 6).
Table 5.
Incidence rate of hypoglycemia-related hospitalizations according to insulin or sulfonylurea use and CKD in elderly patients with diabetes.
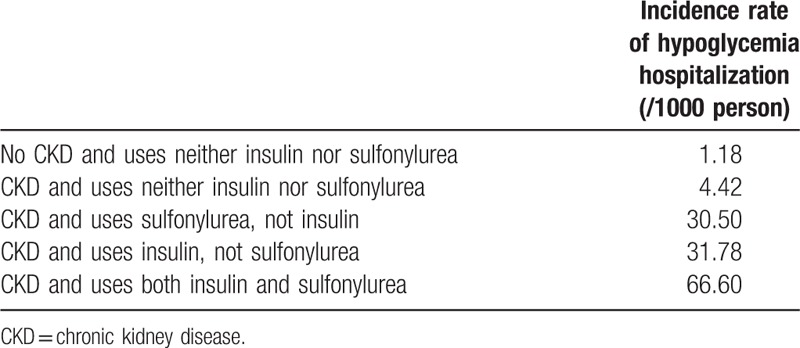
Table 6.
Incidence rate of hypoglycemia-related hospitalizations according to insulin or sulfonylurea use and dementia in elderly patients with diabetes.
4. Discussion
Recent recommendations regarding the management of diabetes in older populations have emphasized the importance of the individualization of treatment with appropriate glycated hemoglobin (HbA1c) targets to prevent hypoglycemic events.[10] However, the detailed advice and descriptions remain poorly defined and much of the information is derived from experts’ opinions. Therefore, understanding the comorbid conditions, the treatment strategies, and the major risk factors for hypoglycemia is helpful. In this study of older diabetic patients, a substantial proportion of the patients had a variety of comorbidities, and many of the patients were treated with insulin or sulfonylureas, which are agents that carry the highest risks of hypoglycemic events. Several clinical factors, including being older, being female, using insulin or sulfonylureas, and different comorbid conditions were associated with hypoglycemia-related hospitalization.
Globally, older patients who present with diabetes are becoming increasingly common in clinical practice, because of the reduced mortality rates among people with diabetes and the obesity epidemic.[1,14,15] Recent epidemiologic data from Korea has shown a noticeable increase in the prevalence of diabetes mellitus, particularly among older people. In 2013, 1 person out of every 5 Korean people aged >65 years had diabetes mellitus.[2] As older diabetic patients have particular characteristics, a different approach to the management of diabetes is required compared with the approach used for young patients with diabetes, and the most serious problem is that older diabetic patients are very susceptible to hypoglycemia.[16] Longer diabetes durations, the presence of multiple comorbidities, and poor nutritional statuses could increase the risk of hypoglycemia among older patients. Indeed, the findings from studies that used hypoglycemic clamp techniques have shown that protective responses against hypoglycemia are reduced in older men compared with younger men.[9] Older patients showed similar hormonal counter-regulatory responses to hypoglycemia compared with younger patients and marked subjective unawareness about hypoglycemia during hypoglycemic clamping.[17] These factors contribute to the increased severity of hypoglycemic events among older people with diabetes compared with those that occur among younger patients with diabetes.
Despite the marked increase in the number of older people with diabetes and the risk of hypoglycemia, data that describe the risk of hypoglycemia among older patients with diabetes in Korea is insufficient. Noh et al[18] reported that 5.5% of the Korean patients with type 2 diabetes who were admitted to hospital because of severe hypoglycemia were >65 years. Very recently, the hypoglycemia incidence rates have been reported to be 9.34 per 1000 person-years among patients aged 60 to 69 years and 25.75 per 1000 person-years among patients aged >70 years.[19] In our study, the incidence of hypoglycemia-related hospitalizations among patients aged >65 years was 9.33 per 1000 person, and this rate is comparable with those determined from previous cohort studies. However, the risk of hypoglycemia-related hospitalization differed greatly according to the treatment modality and the patients’ comorbidities. The risk factors for hypoglycemia among older patients with diabetes were similar to those within the entire diabetic population, namely, the use of insulin or insulin secretagogues, the diabetes duration, previous hypoglycemic events, and renal insufficiency.[8] In addition, hospital discharge within the previous 30 days, an advanced age, and the use of 5 or more concomitant medications were independent risk factors for hypoglycemia among older patients who had diabetes.[20]
This study provides valuable information about the treatment modalities used to manage older people with diabetes in Korea and particularly important information about patients with several comorbidities who are at a high risk of hypoglycemia. Among older diabetic patients, 63.1% of the subjects were treated with metformin, 47.6% of the subjects were treated with sulfonylureas, 25.9% of the patients were administered DPP-4 inhibitors, and 16.1% of the patients were prescribed insulin therapy. We compared these to the results from another data in the same year, 2013.[2] Those data included people over the age of 30 with type 2 diabetes mellitus using the National Health Information Database and evaluated the treatment options for diabetes. The proportions of the patients who were treated with metformin (63.1% vs 80.4%) and DPP-4 inhibitors (25.9% vs 38.4%) were lower for the patients of all ages in our study population, but the use of sulfonylureas (47.6% vs 58.5%) and insulin (16.1% vs 16.4%) were comparable. Metformin is not recommended for patients with CKD, and it should not be newly prescribed to very old patients. Furthermore, given that the metformin dose is more likely to be reduced or metformin may be discontinued in older patients, because of the side effects that include loss of appetite and gastrointestinal problems, it is reasonable that the metformin treatment rate was lower among older patients compared with patients of all ages. However, the current trend of fewer DDP-4 inhibitor prescriptions being given to older patients compared with the number of DDP-4 inhibitor prescriptions being given to all age groups is not desirable. In Korea, the usage of a DDP-4 inhibitor, which was licensed in 2009, is rapidly increasing currently, it is associated with a lower risk of hypoglycemia, and it can be prescribed safely to patients whose renal function is reduced, or even to patients with end-stage renal disease. Since it does not have many side effects, it has no other contraindications except for pancreatitis and pancreatic cancer. Despite the increased usage of DDP-4 inhibitors, they were only prescribed to one-quarter of the older patients with diabetes. Often, patients who are newly diagnosed with diabetes and are prescribed drugs because of inadequate glycemic control will not change their routine medication to a DDP-4 inhibitor. However, since the effectiveness of DDP-4 inhibitors is maximized in older patients, the aggressive administration of DDP-4 inhibitors should be considered if their usefulness is anticipated, even if other medications have been prescribed previously.
Diabetes is accompanied by different comorbidities in older patients,[21] and comorbidities that included hypertension, renal disease, heart disease, stroke, a history of cancer, and liver disease were associated with hypoglycemia in a nationwide cohort study.[5] In the current study, the patients had an average of 3.3 comorbidities, and one-third of the patients had many comorbid conditions and Charlson comorbidity index scores that were higher than 3. The total number of comorbid conditions was an important predictor of hypoglycemia, even among the patients who were treated nonpharmacologically. Furthermore, CKD and dementia were the strongest risk factors for severe hypoglycemia after adjusting for a variety of clinical factors.
CKD is a clear risk factor for hypoglycemia and it increases the mortality associated with hypoglycemia.[22] Moreover, as the prevalence of CKD increases with age, it will further increase the risk of hypoglycemia in older patients. In a study undertaken in 2009, the incidence of hypoglycemia among diabetic patients with CKD was 10.72 people per 100 person-months,[22] and in our study it was 30.22 per 1000 person. The findings from previous studies have shown that hypoglycemia increased in patients who did not have diabetes, in patients with diabetes who did not receive medication, and in patients who had CKD. This may have been a consequence of a decline in gluconeogenesis in the kidney because of a reduction in renal capacity,[23] or it may have been a consequence of a loss of appetite and malnutrition caused by uremia in patients who had impaired renal function.[24] The most important finding from our study is that the risk of hypoglycemia that is associated with the different drugs used to treat diabetes mellitus is higher in patients with CKD. Insulin and sulfonylureas, which are associated with high risks of hypoglycemia, were prescribed to more than two-thirds of the patients with CKD in this study. This value is differentiated from the results of another study in which insulin was used to treat 30% and sulfonylureas were used to treat 3% of the patients with CKD.[25] Of course, drugs that are associated with comparatively lower risks of hypoglycemia, for example, metformin, cannot be used in patients who have reduced renal function, CKD, cardiac failure, or osteoporosis, and TZDs cannot be prescribed to many patients with diabetes. Since there are many restrictions surrounding the use of some drugs, using insulin or sulfonylureas is inevitable for some cases. However, the findings from our study showed that using insulin or sulfonylureas was associated with a 30-fold increase in hypoglycemia-related hospital admissions, and using these drugs simultaneously doubled the risk of hypoglycemia compared with the use of a single drug alone. Avoiding the simultaneous use of these drugs is mandatory to reduce the risk of hypoglycemia.
Neurocognitive disorders, including dementia, are major public health problems among older people.[26] A review concluded that type 2 diabetes was associated with a 1.5- to 2.5-fold higher risk of developing dementia, and that the dementia risk was related to the number of hypoglycemic episodes.[27] Older patients with both diabetes and dementia have very high risks of hypoglycemia, even with tight glycemic control.[28] Diabetic patients who have dementia are less able to recognize hypoglycemia, to avoid hypoglycemia by initiating appropriate responses, and to communicate their needs for help to manage the symptoms of hypoglycemia. Furthermore, these patients are likely to take drug overdoses and hypoglycemic events may occur repeatedly. In our study, the proportion of patients who had dementia and were prescribed insulin or sulfonylureas was not higher than the proportion of patients who did not have dementia, which was consistent with the findings from an analysis of the data in the German/Austrian diabetes registry.[29] However, more than half of the patients with dementia were treated with insulin or sulfonylureas. Like the diabetic patients with CKD, the influence of the treatment modalities on the risk of hypoglycemia was considerable, particularly in those patients who used both insulin and sulfonylureas. Indeed, the incidence of hypoglycemia among patients with dementia who were treated with both insulin and sulfonylureas was 20-times higher than the incidence of hypoglycemia among dementia patients who were treated using other treatment options. This is the first report that describes the treatment patterns among diabetic people with dementia in Korea, and it should be emphasized that to reduce the risk of hypoglycemia, insulin, and sulfonylureas should not be used simultaneously in these patents.
There are limitations to this study. First, this was a cross-sectional study that had a duration of only 1 year. Furthermore, it is possible that the present study underestimated the frequency of the hypoglycemic events. The risk of hypoglycemia was assessed based on the HIRA diagnostic codes that are used when patients visit emergency units or are discharged from hospital; therefore, mild-to-moderate hypoglycemic events, which were not registered using the HIRA diagnostic codes, were missed. This could explain the comparable risks of hypoglycemia between the group of patients who were not treated with insulin nor sulfonylureas and the group of patients who were treated nonpharmacologically in our study. Furthermore, we were unable to assess several important factors that are associated with hypoglycemia, including the diabetes duration, body mass index, and the dosages of insulin and the oral antidiabetic agents. A particularly weak aspect of the study is that data relating to the HbA1c level, which is the index of glycemic control, were not available. Also, all-cause mortality and hypoglycemia-related mortality were not determined in our study, so we could not employ the risk factors to determine the prognoses of the hypoglycemia events. Despite these limitations, the findings from this study are significant, because it is the first study to investigate hypoglycemia among older diabetic patients using data from a large nationwide sample. The HIRA-APS includes data from >1 million older people and from about 300,000 diabetic subjects, which corresponds to 20% of the entire population of older patients with diabetes in Korea. This study also provides valuable information about the frequencies and types of diseases that accompany diabetes in older patients. Furthermore, the results demonstrate the marked influence of the treatment modality and comorbidities on the risk of hypoglycemia.
In conclusion, several factors, including age, being female, insulin or sulfonylurea use, and different comorbidities, were associated with an increased risk of hypoglycemia-related hospitalization among older people with diabetes. Among the comorbidities, CKD and dementia were the major contributors to hypoglycemia-related hospitalization. Furthermore, when a patient has CKD or dementia, the influence of the treatment modality on the hypoglycemia risk is much greater. Hence, we must be particularly cautious when determining treatment regimens for older patients with diabetes who have these comorbidities. In addition, the development of clear statements within management guidelines will help physicians manage their older patients in the safest and most effective manner.
Supplementary Material
Footnotes
Abbreviations: CKD = chronic kidney disease, CLD = chronic liver disease, DPP-4 = dipeptidyl peptidase-4, GLP-1 = glucagon-like peptide-1, HbA1c = glycated hemoglobin, HIRA = Health Insurance Review & Assessment services, HIRA-APS = Health Insurance Review & Assessment services-Adult Patient Sample, ICD = International Classification of Disease, OR = odds ratio, TZDs = thiazolidinediones.
H.M.K. and J-M.S. contributed contributed equally to this study.
The authors have no funding and conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Website (www.md-journal.com).
References
- 1.Selvin E, Coresh J, Brancati FL. The burden and treatment of diabetes in elderly individuals in the U.S. Diabetes Care 2006; 29:2415–2419. [DOI] [PubMed] [Google Scholar]
- 2.Ko SH, Kim DJ, Park JH, et al. Trends of antidiabetic drug use in adult type 2 diabetes in Korea in 2002-2013: Nationwide population-based cohort study. Medicine (Baltimore) 2016; 95:e4018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang ES, Zhang Q, Gandra N, et al. The effect of comorbid illness and functional status on the expected benefits of intensive glucose control in older patients with type 2 diabetes: a decision analysis. Ann Intern Med 2008; 149:11–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ha WC, Oh SJ, Kim JH, et al. Severe hypoglycemia is a serious complication and becoming an economic burden in diabetes. Diabetes Metab J 2012; 36:280–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hsu PF, Sung SH, Cheng HM, et al. Association of clinical symptomatic hypoglycemia with cardiovascular events and total mortality in type 2 diabetes: a nationwide population-based study. Diabetes Care 2013; 36:894–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zoungas S, Patel A, Chalmers J, et al. Severe hypoglycemia and risks of vascular events and death. N Engl J Med 2010; 363:1410–1418. [DOI] [PubMed] [Google Scholar]
- 7.Laiteerapong N, Karter AJ, Liu JY, et al. Correlates of quality of life in older adults with diabetes: the diabetes & aging study. Diabetes Care 2011; 34:1749–1753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fu H, Xie W, Curtis B, et al. Identifying factors associated with hypoglycemia-related hospitalizations among elderly patients with T2DM in the US: a novel approach using influential variable analysis. Curr Med Res Opin 2014; 30:1787–1793. [DOI] [PubMed] [Google Scholar]
- 9.Matyka K, Evans M, Lomas J, et al. Altered hierarchy of protective responses against severe hypoglycemia in normal aging in healthy men. Diabetes Care 1997; 20:135–141. [DOI] [PubMed] [Google Scholar]
- 10.Moreno G, Mangione CM, Kimbro L, et al. American Geriatrics Society Expert Panel on Care of Older Adults with Diabetes M. Guidelines abstracted from the American Geriatrics Society Guidelines for Improving the Care of Older Adults with Diabetes Mellitus: 2013 update. J Am Geriatr Soc 2013; 61:2020–2026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.The Health Insurance Review & Assessment services. HIRA System. Healthcare big data analysis. http://www.hira.or.kr/eng/ebook/00_Page_img/extra/00.pdf. [Google Scholar]
- 12.Kim L, Kim JA, Kim S. A guide for the utilization of Health Insurance Review and Assessment Service National Patient Samples. Epidemiol Health 2014; 36:e2014008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 2005; 43:1130–1139. [DOI] [PubMed] [Google Scholar]
- 14.Cheng YJ, Imperatore G, Geiss LS, et al. Secular changes in the age-specific prevalence of diabetes among U.S. adults: 1988–2010. Diabetes Care 2013; 36:2690–2696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gregg EW, Cheng YJ, Saydah S, et al. Trends in death rates among U.S. adults with and without diabetes between 1997 and 2006: findings from the National Health Interview Survey. Diabetes Care 2012; 35:1252–1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huang ES, Laiteerapong N, Liu JY, et al. Rates of complications and mortality in older patients with diabetes mellitus: the diabetes and aging study. JAMA Intern Med 2014; 174:251–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bremer JP, Jauch-Chara K, Hallschmid M, et al. Hypoglycemia unawareness in older compared with middle-aged patients with type 2 diabetes. Diabetes Care 2009; 32:1513–1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Noh JH, Kim SK, Cho YJ, et al. Current status of diabetes management in elderly Koreans with diabetes. Diabetes Res Clin Pract 2007; 77 suppl 1:S71–75. [DOI] [PubMed] [Google Scholar]
- 19.Rhee SY, Hong SM, Chon S, et al. Hypoglycemia and medical expenses in patients with type 2 diabetes mellitus: an analysis based on the Korea National Diabetes Program Cohort. PLoS One 2016; 11:e0148630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shorr RI, Ray WA, Daugherty JR, et al. Incidence and risk factors for serious hypoglycemia in older persons using insulin or sulfonylureas. Arch Intern Med 1997; 157:1681–1686. [PubMed] [Google Scholar]
- 21.Kirkman MS, Briscoe VJ, Clark N, et al. Diabetes in older adults. Diabetes Care 2012; 35:2650–2664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moen MF, Zhan M, Hsu VD, et al. Frequency of hypoglycemia and its significance in chronic kidney disease. Clin J Am Soc Nephrol 2009; 4:1121–1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Snyder RW, Berns JS. Use of insulin and oral hypoglycemic medications in patients with diabetes mellitus and advanced kidney disease. Semin Dial 2004; 17:365–370. [DOI] [PubMed] [Google Scholar]
- 24.Horton ES, Johnson C, Lebovitz HE. Carbohydrate metabolism in uremia. Ann Intern Med 1968; 68:63–74. [DOI] [PubMed] [Google Scholar]
- 25.Luk AO, Li X, Zhang Y, et al. Quality of care in patients with diabetic kidney disease in Asia: The Joint Asia Diabetes Evaluation (JADE) Registry. Diabet Med 2016; 33:1230–1239. http://dx.doi.org/10.1111/dme.13014 [DOI] [PubMed] [Google Scholar]
- 26.Prince M, Bryce R, Albanese E, et al. The global prevalence of dementia: a systematic review and metaanalysis. Alzheimers Dement 2013; 9:63–75.e62. [DOI] [PubMed] [Google Scholar]
- 27.Whitmer RA, Karter AJ, Yaffe K, et al. Hypoglycemic episodes and risk of dementia in older patients with type 2 diabetes mellitus. JAMA 2009; 301:1565–1572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Thorpe CT, Gellad WF, Good CB, et al. Tight glycemic control and use of hypoglycemic medications in older veterans with type 2 diabetes and comorbid dementia. Diabetes Care 2015; 38:588–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Prinz N, Stingl J, Dapp A, et al. High rate of hypoglycemia in 6770 type 2 diabetes patients with comorbid dementia: A multicenter cohort study on 215,932 patients from the German/Austrian diabetes registry. Diabetes Res Clin Pract 2016; 112:73–81. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


