Abstract
Background:
Continuous femoral nerve block and fascia iliaca compartment block are 2 traditional anesthesia methods in orthopedic surgeries, but it is controversial which method is better. The objective of this study was to compare the practicality, efficacy, and complications of the 2 modalities in hip replacement surgery in the elderly and to assess the utility of a novel cannula-over-needle set.
Methods:
In this prospective, randomized controlled clinical investigation, 60 elderly patients undergoing hip replacement were randomly assigned to receive either continuous femoral nerve block or continuous fascia iliaca compartment block. After ultrasound-guided nerve block, all patients received general anesthesia for surgery and postoperative analgesia through an indwelling cannula. Single-factor analysis of variance was used to compare the outcome variables between the 2 groups.
Results:
There was a significant difference between the 2 groups in the mean visual analog scale scores (at rest) at 6 hours after surgery: 1.0 ± 1.3 in the femoral nerve block group vs 0.5 ± 0.8 in the fascia iliaca compartment block group (P < 0.05). The femoral nerve block group had better postoperative analgesia on the medial aspect of the thigh, whereas the fascia iliaca compartment block group had better analgesia on the lateral aspect of the thigh. There were no other significant differences between the groups.
Conclusions:
Both ultrasound-guided continuous femoral nerve block and fascia iliaca compartment block with the novel cannula-over-needle provide effective anesthesia and postoperative analgesia for elderly hip replacement patients.
Keywords: analgesia, fascia iliaca compartment block, femoral nerve block, hip replacement, nerve block, novel cannula-over-needle
1. Introduction
To avoid the complications and adverse effects of spinal anesthesia and intravenous opioid analgesia, multimodal analgesia with nerve block has been recommended in the perioperative period of lower extremity joint arthroplasty.[1] Among the various nerve block techniques available, 3-in-1 femoral nerve block (FNB) and fascia iliaca compartment block (FICB) are commonly used for anesthesia and analgesia in hip replacement.
3-in-1 FNB was first proposed by Winnie et al[2] who considered that the femoral, lateral femoral cutaneous, and obturator nerves could be blocked at the same time based on the theory of fascial sheath which extends up to the lumbar plexus. Although the existence of the fascial sheath has since been disproved.[3] One study, using a nerve stimulator, showed that 30 mL of local anesthetic could block the femoral nerve, the lateral femoral cutaneous nerve, and the anterior branch of the obturator nerve.[4] A prospective study[5] demonstrated that 3-in-1 FNB could achieve a success rate of 81% block of the femoral nerve, 96% of lateral femoral cutaneous nerve, and 4% of the obturator nerve (though this obturator nerve block effect was controversial). These 3 nerves could also be blocked together by FICB because the fascia iliaca compartment contains these nerves within a potential space.[6] However, it is unknown which of these 2 modalities is better for anesthesia and analgesia in hip replacement surgery.
The main objective of the current study was to compare the practicality, anesthetic, and analgesic efficacy, and complications of ultrasound-guided FNB and FICB in elderly patients undergoing hip replacement and to verify the applicability of a novel cannula-over-needle set in these cases. It was hypothesized that FNB would be easier to perform, wheras FICB would provide better anesthesia and analgesia and have fewer complications, and that the novel cannula-over-needle would be useful for nerve block in elderly patients receiving hip replacement.
2. Methods
2.1. Patients
This was a single-center, prospective, randomized controlled clinical study. Patients >65 years old, classified as American Society of Anesthesiologists (ASA) grade I-III, and undergoing hip replacement surgery during the period April 2014 through June 2015 at the Department of Orthopedics at Tongji Hospital were eligible for participation in this study. Exclusion criteria were as follows: patients with history of severe cardiovascular, respiratory, hepatic, renal, or mental disease; those with history of allergy to local anesthetics; those who had any infection at the proposed puncture site; those who had femoral nerve injury; and those who refused participation in the study. Written informed consent was obtained from all participants. The study was approved by the Institutional Review Board of Tongji Hospital of Tongji University (Shanghai, China) and was registered with the Chinese Clinical Trial Registry (ChiCTR-TRC-14004700).
2.2. Grouping
Using a computer-generated randomization program, eligible patients were randomized to 2 groups: 3-in-1 continuous FNB group (group A, n = 30) and continuous FICB group (group B, n = 30). Independent researchers who were not involved in the anesthesia procedures or outcome assessment conducted patient enrollment and generated the random allocation.
2.3. Methods of nerve block
All patients were fasted for 8 hours, and received intramuscular atropine (0.05 mg) and phenobarbital (0.1 g) as premedication 30 minutes before anesthesia. Intravenous access for anesthesia was established on the upper limb. A loading infusion of 1 μg/kg dexmedetomidine was administered over 10 minutes, after which the infusion speed was regulated to 0.3 μg kg−1 h−1. Nerve block was performed after routine sterilization of the inguinal region. Sterile gel was applied to the inguinal area and a linear 6 to 13 MHz ultrasound probe wrapped in a sterilized plastic sheath was used to guide the nerve block. A novel cannula-over-needle set was used for administering the nerve block. The cannula-over-needle set (Tuoren Group, Xinxiang, China), comprising a 22-gauge needle and a 90-mm-long external indwelling cannula (Fig. 1), was invented by Dr. Bin Yu, the first author of the present article. It has a patent in China, and a related patent is pending in the USA (application number 14357772).
Figure 1.
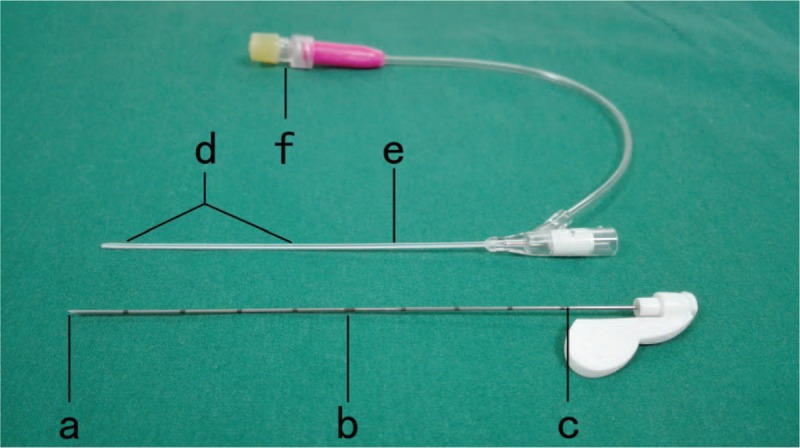
The novel cannula-over-needle: (a) tip with 30° bevel; (b) scale in needle; (c) side hole in the needle; (d) side holes in the cannula; (e) indwelling cannula can be visualized on ultrasonography; (f) injection interface.
Patients in Group A received continuous FNB. Short-axis out-of-plane ultrasound was performed according to the position of operative incision. With the ultrasound transducer placed parallel to the inguinal ligament below its midpoint, the femoral nerve could be identified lateral to the femoral artery. The puncture site was on the outward of the nerve. The site was first infiltrated with 1 mL of 1% lidocaine. The nerve block needle was then inserted at an angle of 30° to 40° to the horizontal in the direction of the long axis of body, with the needle pointing toward the head of the patient. If there was any uncertainty about the position of the needle tip, a test dose of local anesthetic was injected. Usually, a double click was felt as the needle tip penetrated the fascia iliaca and the fascia lata just before it reached the nerve. After the needle tip was correctly positioned underneath the nerve, 20 mL of 0.5% ropivacaine was injected (Fig. 2). With the needle end pressed lightly, the cannula was advanced for 6 to 8 cm and the needle was withdrawn at the same time. We checked that the cannula tip was not within a vessel by aspirating with a syringe and then fixed it to the skin with no-pressure tape. Pressure was applied over the puncture site for 5 minutes. The cannula was left indwelling for injection of local anesthetic. After surgery was completed, the cannula was connected to an electronic patient-controlled analgesia (PCA) pump for delivering postoperative analgesia.
Figure 2.

Continuous femoral nerve block. After the needle tip was correctly positioned underneath the nerve, 20 mL of 0.5% ropivacaine was injected.
In group B, the puncture site was 2 cm below the outer third of the inguinal ligament, at the inner edge of the sartorius muscle. FICB was also performed under short-axis out-of-plane ultrasound with the transducer placed parallel to the ligament. The needle was advanced until the “double click” was felt, and 20 mL of 0.5% ropivacaine was injected. In the ultrasound image, it was observed that the local anesthetic separated the iliopsoas and the fascia iliaca and also expanded to the femoral nerve. The cannula was also fixed to the skin for postoperative analgesia (Fig. 3). The remaining steps were the same as in group A.
Figure 3.

Continuous fascia iliaca compartment block. The indwelling cannula was fixed to the skin and was connected to an electronic PCA pump for postoperative analgesia. PCA = patient-controlled analgesia.
2.4. General anesthesia
Sensation over the anterior, medial, and lateral aspects of the thigh was measured by response to needle prick 10 to 15 minutes after injection of local anesthetic. Obvious alleviation or total absence of pain indicated a satisfactory nerve block. After ensuring that a satisfactory nerve block had been established, general anesthesia was induced. Sevoflurane and propofol were titrated to maintain stable vital signs during the surgery. Just before completion of surgery, 30 mg ketorolac tromethamine was injected intramuscularly and 0.3 mg ramosetron was administered intravenously. After surgery was over, the indwelling cannula was connected to a digital analgesia pump. The pump was loaded with 300 mL of 0.2% ropivacaine and 50 μg sufentanil. It was set to 6 mL/h of basal flow rate, 3 mL of single dose, and 20 minutes of locking time. Intravenous dezocine, 40 mg, was given to achieve multimodal analgesia. Dezocine was administered whenever the patient complained of unbearable pain after surgery. Parecoxib was prescribed for pain occurring 12 hours after surgery.
2.5. Measurement and recording
The general condition of the patient before surgery, age, sex, weight, ASA grade, operation type, operation time, and anesthesia time were recorded. The primary outcome measurements related to the performance of the nerve block were success rate of cannula placement, depth of cannula insertion, procedure performance time, incidence of nerve injury, toxicity to local anesthetic, infection at the puncture site, occlusion or slipping of the cannula, cannula indwelling time, and patient satisfaction. Outcome measurements related to efficacy of analgesia included visual analog scale (VAS) score (at rest and during movement); pain in the distribution of the femoral, lateral femoral cutaneous, and obturator nerves; need for supplementary dezocine; incidence of nausea and vomiting; and sedation score at 6, 12, 24, and 48 hours after surgery. The VAS score was categorized as follows: 0 to 2, no or slight pain; 3 to 6, moderate and tolerable pain; and 7 to 10, severe and intolerable pain. A modified Ramsay Sedation Scale was used to assess sedation as follows: 0, conscious; 1, occasional hypersomnia but easy to rouse; 2, frequent hypersomnia but easy to rouse; 3, hypersomnia and difficult to rouse. Lower limb motor block was graded using a Bromage score, as follows [7]: 0, nil block-free movement of legs and feet; 1, partial block-able to flex knees with free movement of feet; 2, almost complete block-unable to flex knees, but with free movement of feet; 3, complete block-unable to move legs or feet. Respiratory depression was defined as a respiratory rate <8/minutes. Infection was identified when the skin at the puncture site was swollen, warm, and painful. If a patient complained of numbness or paresthesia on the operated side, a nerve electromyogram was obtained to identify any nerve injury. Patient satisfaction was measured on a scale ranging from 0 for very dissatisfied to 10 for very satisfied.
2.6. Statistical Analysis
Data analysis was performed using SPSS version 12.0. All quantitative data were expressed as means ± standard deviation (SD) unless otherwise specified. Fisher's exact test was used for statistical analysis of the enumeration data. Single-factor analysis of variance was used to compare data between groups. P < 0.05 was considered statistically significant.
3. Results
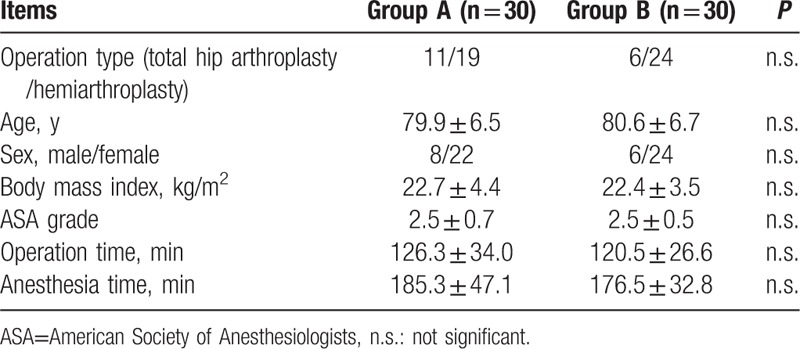
Sixty patients were included in this study. The characteristics of the patients are shown in Table 1. The age, sex, body mass index, ASA grade, operation time, operation type, and anesthesia time were not significantly different between the 2 groups.
Table 1.
General characteristics of the participants.
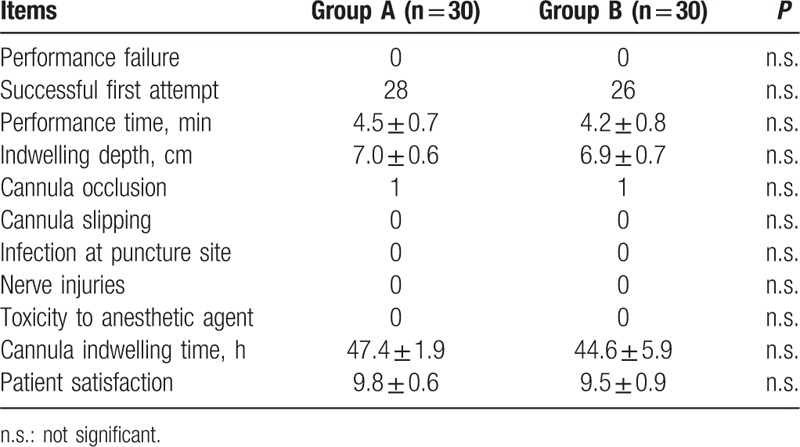
Data related to the performance of the procedure and the complications encountered are shown in Table 2. There were no significant differences between the groups with regard to any of these parameters. Each group had 1 patient in whom the cannula got occluded, but in both cases this was resolved with slight repositioning of the cannula. In group B, 1 patient complained of chest discomfort 34 hours after surgery and requested that the analgesia pump be turned off and the cannula removed. One patient in group A experienced numbness over the skin of the anterior thigh for 4 days; however, muscle strength was not affected and sensation returned to normal by the fifth day.
Table 2.
Performance-related variables and complications in the 2 groups.
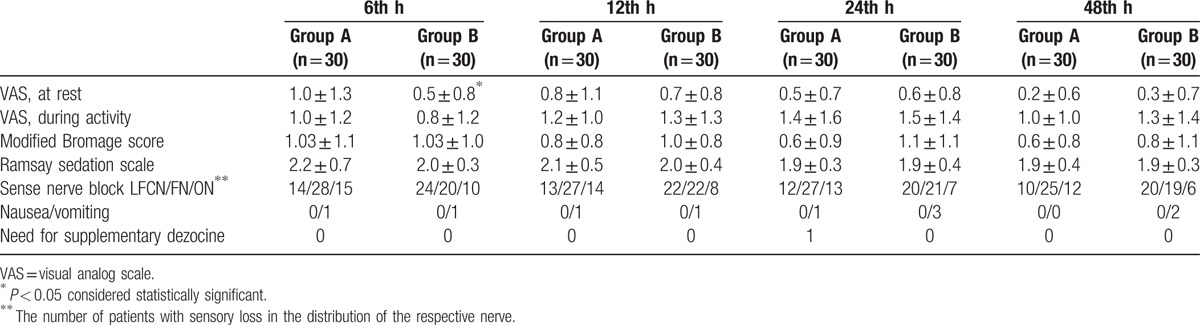
Comparisons of the analgesic efficacy and the related complications are shown in Table 3. The mean VAS score (at rest) at 6 hours after surgery was significantly lower in group B (P < 0.05). However, in both groups, the mean VAS score at rest (<1) and that during activity (<1.5) indicated that patients experienced only slight pain. In both groups, all patients experienced mild motor block, with the highest mean Bromage score being 1.03 ± 1.1 in group A vs 1.03 ± 1.0 in group B, both at 6 hours after surgery, indicated that patients got only partial motor block. During the postoperative period, nausea and vomiting as well as the need for supplementary dezocine for pain relief were infrequent, and the differences between the 2 groups were not significant.
Table 3.
Analgesic efficacy and complications in the 2 groups.
4. Discussion
The most important finding of this study was that ultrasound-guided continuous FNB and continuous FICB were safe and effective methods for anesthesia and postoperative analgesia in elderly hip replacement patients. Contrary to our hypothesis, both procedures were relatively straightforward to perform with ultrasound guidance. Continuous FICB provided better analgesia over the skin innervated by the lateral femoral cutaneous nerve, whereas continuous FNB did better on the skin innervated by the obturator nerve. Overall, in this study, the 2 modalities were similar with regard to practicality, anesthetic and analgesic efficacy, and complications; this is consistent with the findings of other investigators.[8,9] In this study, we additionally demonstrated the safety and practicality of the novel cannula-over-needle set for delivering anesthesia and postoperative analgesia in hip replacement patients.
Because of the aging of the population, the number of elderly patients accepting hip replacement is increasing by the year. Both general anesthesia and regional anesthesia can be used in these patients. However, the neurotoxic effects of general anesthetics, with the potential for postoperative cognitive dysfunction and other complications, may be the reason why general anesthesia is not preferred in some cases. Regional anesthesia can not only decrease the stress response caused by surgery and pain but can also shorten hospital stay, reduce medical bills, and allow early postoperative rehabilitation.[10] For regional anesthesia, continuous nerve block (CNB) has many advantages. CNB, by using local anesthetics, allows the patient to avoid the adverse effects of opioid analgesics, such as nausea, vomiting, drowsiness, constipation, and respiratory depression.[11] By blocking the conduction channel of pain, CNB decreases central and peripheral sensitization and thus reduces the risk of postoperative chronic pain.[12] With the use of low concentrations of local anesthetics for postoperative analgesia, it is possible to selectively block the sensory nerve fibers; preservation of motor function promotes early functional rehabilitation[13] and decreases the risk of deep venous thrombosis.[14,15] Compared with general anesthesia, CNB is also less likely to cause postoperative cognitive dysfunction.[16] Furthermore, the use of peripheral nerve block permits reduction in the dose of the general anesthetic; does not interfere with gastrointestinal function after surgery; decreases intraoperative blood loss and improves blood circulation [17]; and reduces the incidence of postoperative delirium, complex regional pain syndrome, and cardiovascular complications.
The use of nerve block for anesthesia in hip replacement surgery poses obvious difficulties due to the complexity of the hip joint innervation. Four nerves—the obturator nerve, the femoral nerve, the superior gluteal nerve, and the articular branches of the sciatic nerve—dominate the nerve supply to hip joint. This is why continuous lumbar plexus-sciatic nerve block has been traditionally used for postoperative analgesia in hip replacement patients. In practice, continuous lumbar plexus-sciatic nerve block is inconvenient because it involves the performance of 2 complex nerve blocks and requires the patient to be in a lateral position. It has been stated that the hip joint innervation comprises mainly the obturator, femoral, and sciatic nerves.[18] The fascia iliaca compartment contains the femoral, lateral femoral cutaneous, obturator, and genitofemoral nerves, which led Dalens et al[19] to consider blocking the femoral, lateral femoral cutaneous, and obturator nerves together by diffusing local anesthetic into the fascia iliaca compartment. We too achieved satisfactory postoperative analgesia with an initial large dose of local anesthetic, followed by low doses delivered through an indwelling cannula. This method was simple to perform and reduced the pain triggered by changes of posture.
Postoperative analgesia with CNB has been difficult to implement in China because of the nonavailability of the CNB catheter set. To address this problem, we invented a novel cannula-over-needle. The cannula-over-needle set comprises a hollow needle with a side hole, a needle tip with a 30° bevel, and an indwelling cannula with side holes outside the needle. Both needle and cannula were visible under ultrasound. Compared with the Braun continuous peripheral nerve block catheter set, our cannula-over-needle set is easier to use, is less likely to cause effusion and infection, and is relatively inexpensive; these factors make it ideally suited for use in China.[7] The cannula-over-needle set has been successfully used for continuous brachial plexus block and continuous femoral nerve block.[20,21] In the current investigation also, it proved to be safe and practical.
Each of the 2 methods used in this study had its advantages. Continuous FICB could be used without ultrasound depending solely on anatomical landmarks and is suited for hip replacement performed using a lateral or posterolateral incision because of the better analgesia it provides on skin innervated by the lateral femoral cutaneous nerve. Continuous FNB produced its best effect on skin innervated by the femoral nerve and was better than FICB for providing analgesia in the regions innervated by the obturator nerve. FNB was best performed with ultrasound guidance.
In summary, the novel cannula-over-needle is effective, convenient, and safe for use in ultrasound-guided FNB and FICB in hip replacement patients. We found no significant differences between the 2 techniques with regard to operability, anesthetic, and analgesic effect, and complications in hip replacement patients. The limitation of our study was that we were not able to examine the exact position of the indwelling cannula and the diffusion of local anesthetic in the 2 groups. In the next phase, we plan to use T2-weighted magnetic resonance imaging to study the position of the indwelling cannula and the diffusion of the local anesthetic.
Acknowledgments
The authors thank the Department of Orthopaedics of Tongji Hospital of Tongji University for cooperation.
Footnotes
Abbreviations: ASA = American Society of Anesthesiologists, CNB = continuous nerve block, FICB = fascia iliaca compartment block, FNB = femoral nerve block, PCA = patient-controlled analgesia, VAS = visual analog scale.
Funding: This study was supported by the Shanghai Municipal Commission of Health and Family Planning.
The authors have no conflicts of interest to disclose.
References
- 1.Barrington JW, Halaszynski TM, Sinatra RS. Expert Working Group On Anesthesia, Orthopaedics Critical Issues In Hip and Knee Replacement Arthroplasty FT. Perioperative pain management in hip and knee replacement surgery. Am J Orthop (Belle Mead, NJ) 2014; 43 (4 suppl):S1–S16. [PubMed] [Google Scholar]
- 2.Winnie AP, Ramamurthy S, Durrani Z. The inguinal paravascular technic of lumbar plexus anesthesia: the “3-in-1 block”. Anesth Analg 1973; 52:989–996. [PubMed] [Google Scholar]
- 3.Xu ZY, Ren YH, Tu LL, et al. Anatomy of the femoral fascia sheath and its adjacent structures. Acta Anatom Sinic 2013; 44:364–367. [Google Scholar]
- 4.Marhofer P, Nasel C, Sitzwohl C, et al. Magnetic resonance imaging of the distribution of local anesthetic during the three-in-one block. Anesth Analg 2000; 90:119–124. [DOI] [PubMed] [Google Scholar]
- 5.Lang SA, Yip RW, Chang PC, et al. The femoral 3-in-1 block revisited. J Clin Anesth 1993; 5:292–296. [DOI] [PubMed] [Google Scholar]
- 6.Khoo ST, Brown TC. Femoral nerve block—the anatomical basis for a single injection technique. Anaesth Intensive Care 1983; 11:40–42. [DOI] [PubMed] [Google Scholar]
- 7.Yu B, Hu X, Zou T, et al. Effects of postoperative continuous femoral nerve block analgesia with Braun continuous peripheral nerve block catheter set versus novel needle-over-cannula after total knee arthroplasty. Med Sci Monit 2015; 21:1843–1849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McMeniman TJ, McMeniman PJ, Myers PT, et al. Femoral nerve block vs fascia iliaca block for total knee arthroplasty postoperative pain control: a prospective, randomized controlled trial. J Arthroplasty 2010; 25:1246–1249. [DOI] [PubMed] [Google Scholar]
- 9.Farid IS, Heiner EJ, Fleissner PR. Comparison of femoral nerve block and fascia iliaca block for analgesia following reconstructive knee surgery in adolescents. J Clin Anesth 2010; 22:256–259. [DOI] [PubMed] [Google Scholar]
- 10.Neuman MD, Rosenbaum PR, Ludwig JM, et al. Anesthesia technique, mortality, and length of stay after hip fracture surgery. JAMA 2014; 311:2508–2517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shah A, Rowlands M, Krishnan N, et al. Thoracic intercostal nerve blocks reduce opioid consumption and length of stay in patients undergoing implant-based breast reconstruction. Plast Reconstr Surg 2015; 136:584e–591e. [DOI] [PubMed] [Google Scholar]
- 12.Savage C, McQuitty C, Wang D, et al. Postthoracotomy pain management. Chest Surg Clin N Am 2002; 12:251–263. [DOI] [PubMed] [Google Scholar]
- 13.McClellan KJ, Faulds D. Ropivacaine: an update of its use in regional anaesthesia. Drugs 2000; 60:1065–1093. [DOI] [PubMed] [Google Scholar]
- 14.Adali S, Erkalp K, Erden V, et al. Spinal anesthesia and combined sciatic nerve/lumbar plexus block techniques in lower extremity orthopedic surgery. Acta Orthopaedica Traumatologica Turcica 2011; 45:225–232. [DOI] [PubMed] [Google Scholar]
- 15.Wang H, Boctor B, Verner J. The effect of single-injection femoral nerve block on rehabilitation and length of hospital stay after total knee replacement. Regional Anesth Pain Med 2002; 27:139–144. [DOI] [PubMed] [Google Scholar]
- 16.Perrier V, Julliac B, Lelias A, et al. Influence of the fascia iliaca compartment block on postoperative cognitive status in the elderly. Annales Francaises d’anesthesie et de Reanimation 2010; 29:283–288. [DOI] [PubMed] [Google Scholar]
- 17.Stevens RD, Van Gessel E, Flory N, et al. Lumbar plexus block reduces pain and blood loss associated with total hip arthroplasty. Anesthesiology 2000; 93:115–121. [DOI] [PubMed] [Google Scholar]
- 18.Chen ZG, Xie Y, Tao SX, et al. Anatomy study on nervous ramification to hip joint and its clinical significance. Chin J Clin Anatom 2004; 22:565–567. [Google Scholar]
- 19.Dalens B, Vanneuville G, Tanguy A. Comparison of the fascia iliaca compartment block with the 3-in-1 block in children. Anesth Analg 1989; 69:705–713. [PubMed] [Google Scholar]
- 20.Yu B, Zhang X, Sun P, et al. Non-stimulation needle with external indwelling cannula for brachial plexus block and pain management in 62 patients undergoing upper-limb surgery. Int J Med Sci 2012; 9:766–771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yu B, Zou T, He M, et al. Special needle over cannula for postoperative analgesia in geriatric lower extremity joint arthroplasty. Int J Clin Exp Med 2015; 8:3907–3911. [PMC free article] [PubMed] [Google Scholar]


