Abstract
To study the clinical presentation and treatment outcome among children in South Western China with retinoblastoma (RB) and to determine factors predictive of poor outcome.
A retrospective review of children diagnosed with RB from 2006 to 2015 at West China Hospital was undertaken. Demographic and clinical characteristics and treatment outcomes were studied.
A total of 253 patients (unilateral 80.2%, bilateral 19.8%) were studied. Twenty six patients (10.3%) were from minority ethnic groups of China. The median onset age was 21 months. Leukocoria was the most common presenting sign (71%). Tumors were intraocular in 91.3% cases, extraocular in 8.7% cases. Extraocular RB patients had a longer median lag period than intraocular patients (9 months vs 2 months, P < 0.0001). In the intraocular group, 89.5% were advanced group D or E diseases. Enucleation was the major treatment for intraocular RB. However, over 10 years, the enucleation rate decreased constantly while more patients received chemotherapy. The Kaplan–Meier survival probability was 87.8%, 81.4%, and 74.8% at 3 years, 5 years, and 10 years, respectively. On Cox regression analysis, extraocular RB (P = 0.0008) and treatment abandonment (P < 0.0001) were associated with poor outcome; bilateral RB (P = 0.0116) and advanced pathological grade pT4 (P = 0.0011) were associated with poor outcome of intraocular RB.
Most RB patients from South Western China were diagnosed at advanced clinical stage. Delayed presentation is related to extraocular RB which is a risk factor for poor outcome. Chemotherapy increased the eye salvage but had no effects to overall survival. Education for parents and general physicians for the early signs of RB (such as leukocoria), therapeutic strategy and treatment outcomes of RB may promote early diagnosis, improve the compliance, and outcome.
Keywords: chemotherapy, enucleation, neoplasia, retina, retinoblastoma, South Western China, survival
1. Introduction
Retinoblastoma (RB) is the most common primary intraocular malignancy of childhood.[1,2] There are more than 8000 new RB cases per year all over the world,[3] about 1000 of them are in China. South Western China, home for many minority ethnic groups, covers 25% of the country land area, has a population of 192 million people. However, so far, there are few reports regarding RB patients in South Western China. West China Hospital of Sichuan University, which was established by five Western Christian Missions from the United States, the United Kingdom, and Canada in 1892 at Chengdu, is the largest hospital in South Western China. In order to improve the management of RB patients in South Western China, we conducted a retrospective study to describe the demographic, ethnic and clinical characteristics, and treatment outcomes of RB in this leading medical center between 2006 and 2015.
2. Patients and methods
In order to study the demographic and ethnic features, clinical presentations, and treatment outcomes among children in South Western China with RB and to determine factors predictive of poor outcome, the medical records of 253 patients newly diagnosed with RB between February 2006 and October 2015 were retrospectively reviewed. The study was approved by the Ethics Committee of West China Hospital of Sichuan University and followed the tenets of the Declaration of Helsinki. The diagnosis was based on clinical examination or pathological findings. Extraocular invasion at diagnosis was defined as any extension of the tumor beyond the sclera into the orbit and/or into the optic nerve. B-scan ultrasonography was used to determine tumor dimensions and calcification. Computerized tomography and magnetic resonance imaging of the orbits and brains were performed to exclude gross optic nerve and central nervous system (CNS) involvement. Color Doppler ultrasonography, fundus fluorescein angiography was used to differentiate RB from other retinal diseases if clinically required. Clinical findings were documented by color fundus imaging (Topcon Corporation, Retinal Camera TRC-50X, Japan) and/or Retcam (Massie Laboratories, Inc. Retcam II) in some cases. The International Intraocular Retinoblastoma Classification (IIRC) was used for staging of intraocular RB.[4] The extent of retinoblastoma invasion into optic nerve, uvea, and anterior chamber on histopathology was staged by pathological tumor-node-metastasis staging (pTNM) classification.[5]
The data collected included sex, residence, ethnic group, age at diagnosis, age at onset as described by the parents or patients, delay in presenting (lag period), presenting signs, family history, laterality, examination results, treatment modalities, pathological findings, final outcomes, and duration of follow-up. Minimal travel time (days) required from home to our hospital was also estimated for every patients, based on the distance and available transport modes. Data analysis was performed on 2 statistical software programs (SPSS for Windows, version 20.0; IBM-SPSS, Chicago, IL and Prism 5 for windows, GraphPad Software, Inc., La Jolla, CA). We used Mann–Whitney U test for unpaired quantitative data, Pearson chi-square tests or Fisher exact test for qualitative data. Patients alive were censored at last follow-up. The survival duration of the patients was determined as the interval between the date of onset and the date of death, or the date for last follow-up. Kaplan–Meier survival analysis was performed to study the survival rate. The log-rank test was conducted to assess the difference between two or more Kaplan–Meier curves. To find the risk factors for death, we used Cox regression to analyze the variables. All P values were two-sided and were considered statistically significant when the values were <0.05.
3. Results
3.1. Demographic, ethnic, and clinical features
The demographic, ethnic, and clinical features of 253 patients are presented in Table 1 and Fig. 1. Of 253 patients, 143 (56.5%) were men, and 110 (43.4%) were women; the man/woman ratio is 1.3:1. The retinoblastoma occurred unilaterally in 203 (80.2%) patients, and bilaterally in 50 (19.8%) patients. Patients were from South Western China, including Sichuan (223 cases, 88%), Tibet (8 cases, 3.2%), Yunnan (7 cases, 2.8%), and Guizhou province (7 cases, 2.8%). The median estimated travel time from home to hospital was 1 day (range, 1–7 days). One hundred eighty nine patients (75%) and 64 patients (25%) were from rural and urban, respectively. In our series, the median age at which the first sign was noted by the parents or family members (onset age) was 21 months (range, 0–611 months), whereas the median age at diagnosis was 25 months (range, 1–617 months). The median lag period (time interval between the onset age and age at diagnosis) was 2 months (range, 0–48 months) (Table 1). A comparison of demographic features between unilateral and bilateral cases is shown in Table 2. The median age at onset (8 months vs 23 months) and at diagnosis (14 months vs 27 months) was younger in bilateral cases as compared with unilateral cases (P < 0.0001, Mann–Whitney U test), but the median lag period was comparable between both groups (P = 0.1797, Mann–Whitney U test) (Table 2). While 74% of bilateral cases were diagnosed before 2 years of age, 64% of unilateral cases were diagnosed after the age of 2 years (Fig. 1A). As shown in Table 1, leukocoria was the most common presenting sign (182 cases, 71.1%). Other presenting signs were red eye (29 cases, 11.3%), poor vision (27 cases, 10.5%), strabismus (20 cases, 7.8%), ocular pain (11 cases, 4.3%), proptopsis (9 cases, 3.5%), lacrimation (7 cases, 2.7%). Some of these signs appeared simultaneously in a single patient.
Table 1.
Demographic, ethnic, and clinical features of 253 cases with RB.
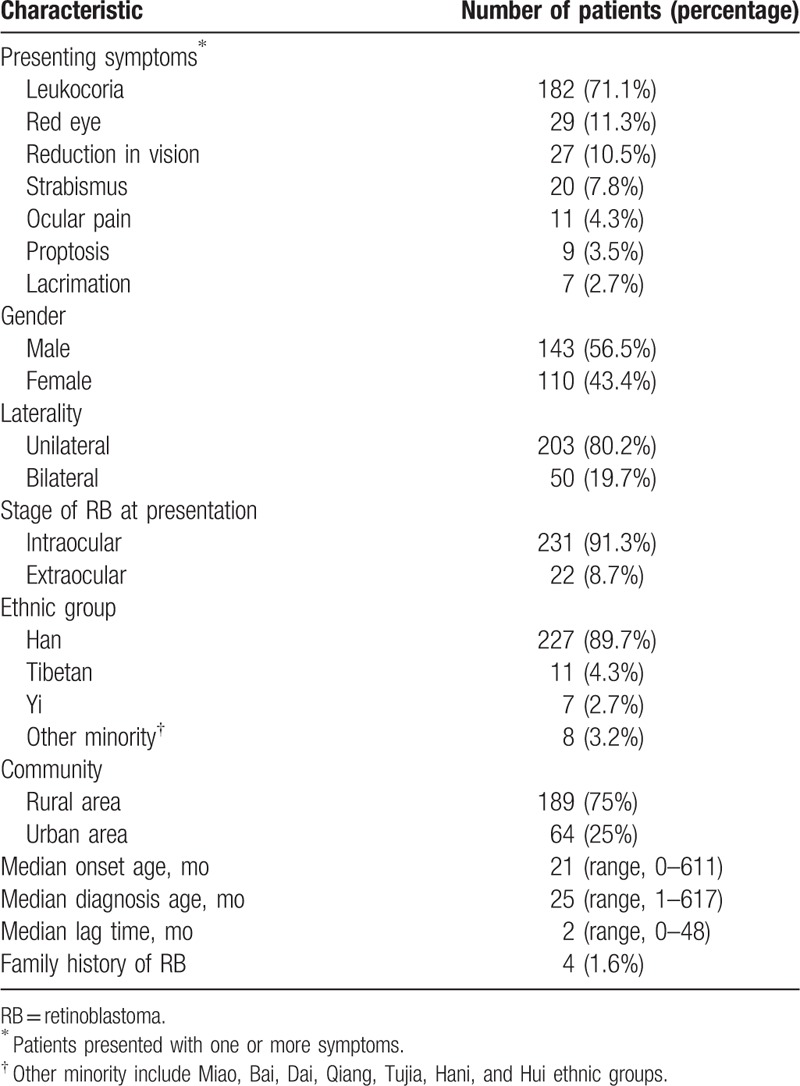
Figure 1.
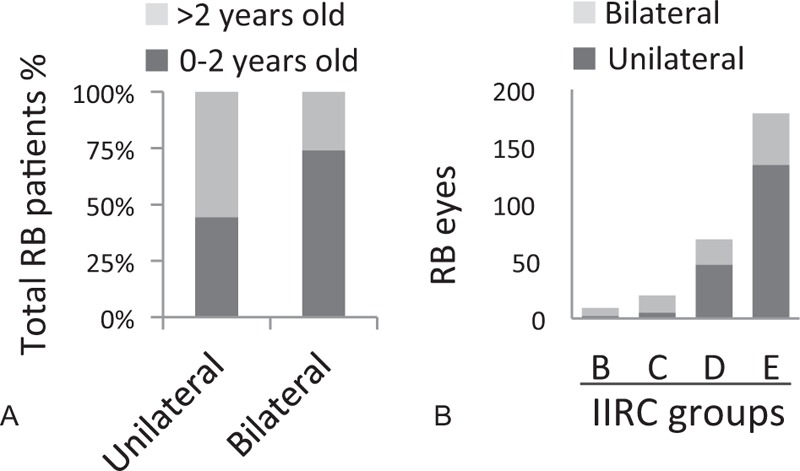
Clinical features of retinoblastoma (RB) patients from South Western China. A. The relationship between diagnosis age and laterality of RB. B. The IIRC groups of unilateral and bilateral intraocular RB eyes. IIRC = The International Intraocular Retinoblastoma Classification.
Table 2.
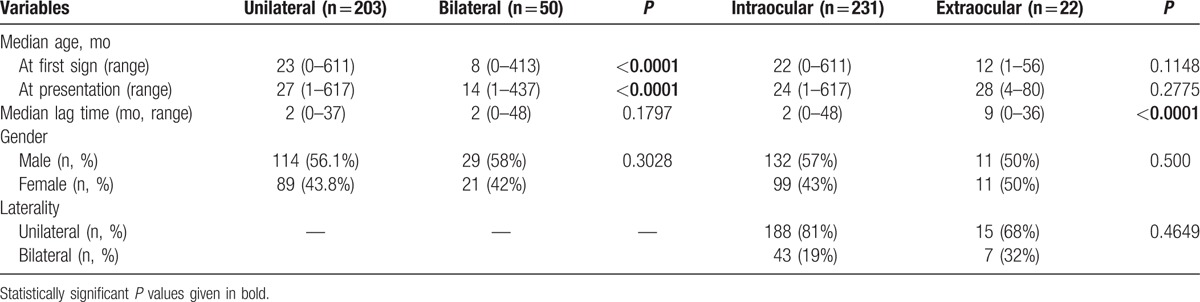
Comparison of demographic features at presentation between unilateral and bilateral groups and between extraocular and intraocular groups.
Of 253 cases, 91.3% (n = 231 cases, 272 eyes) had intraocular tumors (Table 1). These included 188 unilateral cases (81.4%) and 43 bilateral cases (18.6%). Extraocular invasion was noted at initial diagnosis in 8.7% cases (n = 22 cases, 24 eyes). These included 15 unilateral cases (68%) and 7 bilateral cases (32%, 2 cases with both extraocular diseases, 5 cases with 1 intraocular RB eye and 1 extraocular RB eye). A comparative evaluation of intraocular and extraocular groups for the onset age and diagnosis age is shown in Table 2, a statistically significant difference was observed with respect to the median lag period (2 months vs 9 months, P < 0.0001), but the onset age and diagnosis age were comparable. Of 272 eyes with intraocular diseases, as shown in Fig. 1B, the majority of affected eyes were IIRC group E (64.3%), followed by group D (25.4%), group C (7%), and group B (3.3%), there were no group A eyes. As the tumor stage increased from group B to group E, the proportion of bilateral cases became lower and unilateral cases increased (P < 0.0001, Fisher exact test). Among unilateral cases, 96% were group D or E eyes as compared with 4% in group B or C. On the other hand, among bilateral cases, 25% were group B or C eyes.
3.2. Treatment modalities
Treatment strategies were made mainly based on the disease stages (intraocular/extraocular), laterality (unilateral/bilateral), IIRC group, and pTNM staging. The most common treatments for intraocular RB patients (n = 231 cases, 272 eyes) were primary enucleation in 206 eyes (75.7%), and secondary enucleation (after failure of attempted globe salvage treatments) in 7 eyes (2.6%) (Fig. 2A). Forty two eyes (15.4%) only received conservative treatments including systemic chemotherapy, focal therapy, and radiotherapy, and the other 17 eyes (6.3%) did not receive any treatment (refusal to medical advice) (Fig. 2A). Difference of treatment modalities for unilateral and bilateral intraocular eyes was significant (P < 0.001) (Fig. 2A). The overall enucleation ratio was 90.4% (170/188) for unilateral eyes, significantly higher than that of bilateral eyes (51.2%, 43/84). 41.7% (35/84) bilateral eyes received conservative therapy, much higher than 3.7% (7/188) of unilateral eyes (Fig. 2A). Most enucleated eyes were studied for pathologic evidence of tumor invasion to evaluate risk of tumor spread outside the eye. Of 202 enucleated eyeballs from 199 intraocular RB patients with pathological reports, there were 51 eyes (25%) of pT1, 82 eyes (41%) of pT2, 34 eyes (17%) of pT3, and 35 (17%) eyes of pT4. For 205 intraocular RB patients received enucleation, 103 patients underwent adjuvant therapy, including chemotherapy for 97 patients and external beam radiation therapy (EBRT) for 6 patients. Based on IIRC stages of the enucleated eyes, 33.3% of group B-C patients received adjuvant therapy, while 50.3% of group D-E patients had not (Fig. 2B). Based on the pathological findings of the enucleated eyes (pTNM staging), 43.8% of pT1–2 group received adjuvant chemotherapy and/or EBRT; however 40% of pT3–4 group had not received any adjuvant therapy (Fig. 2B). Fisher exact test did not suggest that the decision to give adjuvant therapy was associated with laterality (P = 0.092) or IIRC group (P = 0.6571) or pTNM stage (P = 0.1373). Over 10 years, the enucleation rate (per eyes) decreased constantly while more patients received chemotherapy including intravenous chemotherapy (IVC) and intra-arterial chemotherapy (IAC) (Fig. 2C).
Figure 2.
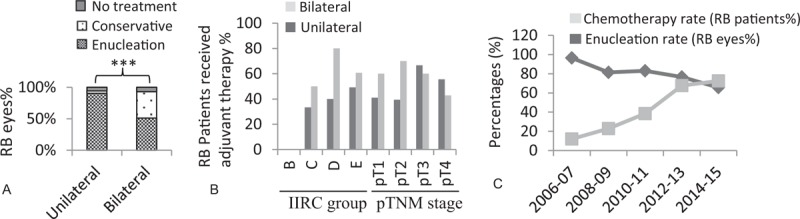
Treatment modalities of intraocular retinoblastoma (RB) patients from South Western China. A. The treatment modalities for unilateral and bilateral RB (∗∗∗P < 0.001, chi-square test). B. The percentage of intraocular RB patients who received adjuvant therapies after enucleation with different IIRC and pTNM staging. C. The rate of enucleation (per eye) and chemotherapy (per case) during 2006 to 2015 at 2-year intervals. IIRC = The International Intraocular Retinoblastoma Classification, pTNM = pathological tumor-node-metastasis staging.
Among extraocular patients (n = 22), 2 bilateral cases only received IVC. 14 cases received exenteration and orbit reconstruction, 6 cases received primary enucleation. Five cases received adjuvant IVC, 4 cases received adjuvant EBRT.
3.3. Follow up, outcomes, risk factors
The median follow-up period of 253 cases was 16 (range, 0.3–119) months. The follow up time of 11.4% cases were more than 60 months, 29.6% were 24 to 60 months, 16.2% were 12 to 24 months, 14.6% were 6 to 12 months, and 28% were 0.3 to 6 months. A total of 23 children died, which included 17 children (7.4%) in the intraocular group and 6 children (27.2%) in the extraocular group. All deaths were due to metastasis of RB but not second malignant neoplasm, maybe related with relatively short follow up time. Death was associated with IIRC stage, as there was no death in 9 patients with IIRC group B or C patients, but there were 17 deaths in 222 patients with IIRC group D or E eyes (chi-square test, P = 0.0227). The overall mortality was 9.1%. The Kaplan–Meier survival probability was 87.8%, 81.4%, and 74.8% at 3, 5, and 10 years, respectively (Fig. 3A). Over 10 years, the survival rate had not changed (P = 0.9472, log-rank test).
Figure 3.
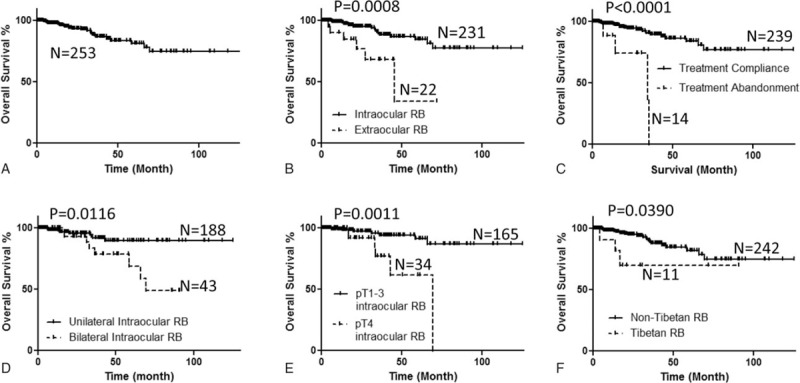
Kaplan–Meier survival curves are shown for (A) overall survival, (B) survival probability and clinical stage (intraocular or extraocular), (C) survival probability and treatment abandonment, (D) survival probability and laterality of intraocular RB, (E) survival probability and pathological stages of intraocular RB, (F) survival probability and Tibetan ethnicity. P values were calculated using the unadjusted log-rank test. RB = retinoblastoma.
The survival probability in the extraocular group was lesser than the intraocular group (P = 0.0008, log-rank test, Fig. 3B). Up to 14 patients (5.5%) in our study received no treatment. Treatment abandonment in our study population was only related to late onset age (P = 0.017). The survival probability in the treatment abandonment was lesser than the treatment compliance group (P < 0.0001, log-rank test, Fig. 3C). For intraocular RB, the survival probability in the bilateral group was lesser than the unilateral group (P = 0.0072, log-rank test, Fig. 3D). The survival probability in the pT4 group was lesser than the pT1–3 group (P = 0.0011, log-rank test, Fig. 3E). The Cox regression showed that extraocular diseases, treatment abandonment, bilateral disease, and pathological stage pT4 were risk factors for death.
For 205 intraocular RB patients received enucleation, 103 patients underwent adjuvant therapy, however, no statistically significant association was observed between adjuvant therapy and survival (P = 0.9417, log-rank test). For 209 intraocular group D or E patients who received treatments, 22 patients received attempted globe salvage treatment. However, no statistically significant associations were observed between attempted globe salvage treatment and survival in our cohort (P = 0.1270, log-rank test).
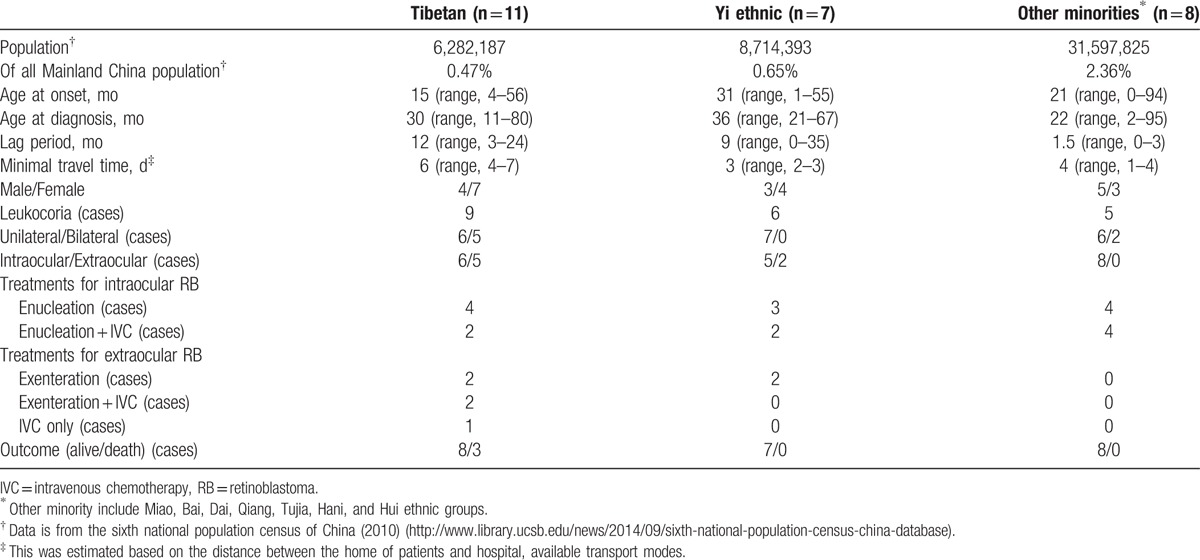
3.4. Minority ethnic group, rural, or urban group
Due to the special geographical location of this patient cohort, 26 patients (10.2%) were minority ethnics (Table 1). In total these minority ethnics account for 3.5% of all population in mainland China. The demographic and clinical features of these 26 patients are summarized in Table 3. The median onset age of minority patients was 22 (range, 0–94) months, enucleation rate was 81.3%, there were no significant differences between patients from Han nationality and minorities in onset age (P = 0.66) and treatment modalities (P = 0.82), while the median lag period of minority patients was longer than that of patients from Han nationality (5 months vs 2 months) (P = 0.047), the median minimal travel time from home to hospital of minority patients was much longer than that of patients from Han nationality (4 days vs 1 day, P < 0.0001). 5/11 (45%) Tibetan patients had extraocular RB, much higher than non-Tibetan patients (P = 0.0443, Fisher exact test), and they also had a relative longer lag time (12 months vs 2 months, P < 0.0001) and minimal travel time (6 days vs 1 day, P < 0.0001). While the overall survival probability in the minority patients was not different from Han ethnic patients (P = 0.4558, log-rank test), the survival probability in Tibetan patients was less than non-Tibetan patients (P = 0.039, log-rank test, Fig. 3F).
Table 3.
Demographic and clinical features of 26 cases of minority ethnic group with RB.
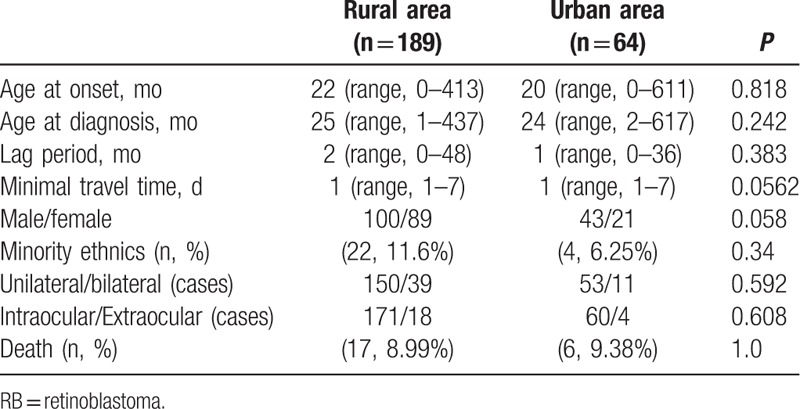
Many patients of this cohort (189/253, 74.7%) were from rural areas (Table 4). There were no significant differences between patients from rural and urban areas in onset age (P = 0.818), age at diagnosis (P = 0.242), lag period (P = 0.383), sex (P = 0.058), minority ethnics (P = 0.34), laterality (P = 0.592), disease stages (intraocular or extraocular) (P = 0.608), minimal travel time (P = 0.0562), and death (P = 1.00). The overall survival probability in the rural patients was not different from the urban patients (P = 0.8416, log-rank test).
Table 4.
Demographic and clinical features of RB patients from rural areas and urban areas.
3.5. Family history, older patients, and phthisis bulbi
Only 4 patients had certain family history, the proportion was 1.58%. Two of them were bilateral and their onset age was 2 and 3 months, respectively, one's older sibling was dead for RB, another one's father was diagnosed with bilateral RB. The other 2 were unilateral RB with onset age at 28 and 30 months, respectively, one's mother was unilateral RB, and the other patient's great uncle was unilateral RB (Table 1). Also there were two mothers of our patients had thyroid cancer, one is bilateral with onset age at 14 months and the other one is unilateral with onset age at 30 months.
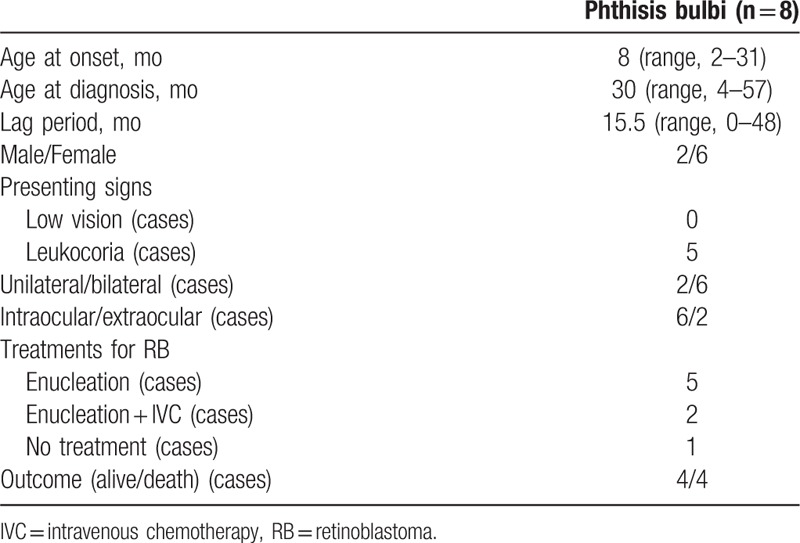
Twenty one patients (8.2%) in our cohort were more than 5 years old when the signs were first noticed. The demographic and clinical features of these 21 patents are summarized in Table 5. Twenty eyes (91%) were enucleated with 5 eyes of pT1, 6 eyes of pT2, 3 eyes of pT3, and 4 eyes of pT4. There was one woman adult bilateral patient declared no family history. Primary phthisis bulbi was seen in 8 patients (3.2%). The demographic and clinical features of these 8 patents are summarized in Table 6. The occurrence was significantly associated with late lag time (P = 0.004) and bilateral RB (P = 0.042). Four patients died during the follow-ups, while according to the Cox regression, phthisis bulbi was not a risk factor for death (P = 0.09).
Table 5.
Demographic and clinical features of older RB cases.
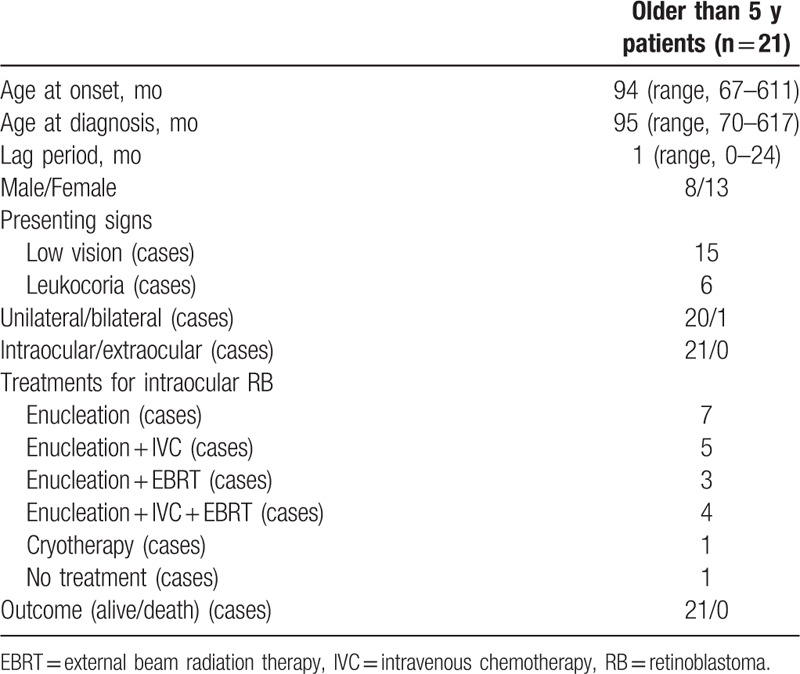
Table 6.
Demographic and clinical features of phthisis bulbi RB cases.
4. Discussion
In this retrospective study, we investigated the demographic, ethnic, and clinical features of RB patients from South Western China. Most of these features are similar to previous reports from other countries or regions.[6–9] In our study, the median age at diagnosis was 25 months. Bilateral RB had a significant younger presentation age than that of unilateral RB (14 months vs 27 months). The most common presenting sign was leukocoria. 8.3% patients were aged more than 5 years, in agreement with other studies,[9,10] decreased vision was the most common presenting sign. Most patients aged over 5 years were unilateral RB, only one patient in our study was bilateral. The rate of phthisis bulbi was 3.2% in our study cohort, comparable with other studies.[11]
The majority of our patients presented at advanced stage. The lag period in extraocular patients was significantly longer than that in intraocular patients (Table 2), indicating delay in presentation was a main reason for extraocular diseases. Ethnic and socioeconomic disparities exist among children with retinoblastoma.[12] South Western China has a large population of minority ethnics. Our study showed that patients from minority ethnics have a longer lag period than patients from Han ethnics. Tibetan patients had more extraocular RB and had a lower survival rate (Table 3, Fig. 3F), which may be related with lower economic level and educational standard, and longer travel time to our hospital, as most of these patients lived in remote areas in Tibet, Qinghai, and Sichuan province where lack modern transportation means.
Due to advanced stage at presentation, the management of RB is challenging. Almost all the affected extraocular RB eyes were enucleated or exenterated, and adjuvant chemotherapy and/or EBRT applied to these patients too. Still metastasis to the CNS was noted in 22.7% (5/22) of extraocular cases and all resulted in death. For intraocular RB, overall 90% unilateral and 46% bilateral RB eyes were enucleated. Globe salvage rates for Group B, C, and D disease were 89%, 67%, and 24%, respectively, which was lower than reports from India (94%, 83%, and 54%)[9] and USA (93%, 90%, and 47%).[13]
In our cohort, 33.3% of IIRC group B-C patients and 43.8% of patients of pT1–2 group received adjuvant chemotherapy and/or EBRT, although no published data suggests that low or moderate-risk justifies adjuvant therapy,[14] this result is similar to a report from Beijing, China.[15] On the other hand, 40% of patients of pT3–4 group, 50.3% of group D-E patients had not received any adjuvant therapy which conventionally might be clinically indicated (Fig. 2B). Fisher exact test did not suggest that the decision to give adjuvant therapy was associated with laterality or IIRC group or pTNM stage, and log-rank test also did not suggest any effects of adjuvant therapy for the survival of our patients received enucleation. Consistent with this result, over the 10 years of period, even though chemotherapy was applied to more and more RB patients in our hospital (Fig. 2C), the survival rate during this period had not changed very much, while more RB eyes were salvaged (Fig. 2C). This may be due to the fact most of our patients presented at advanced stages, but also indicates we need a standard guideline for the use of adjuvant chemotherapy or EBRT to treat RB patients. Previous study indicated that neoadjuvant chemotherapy of group E eyes increase the risk of metastatic death,[15] but in our cohort attempted globe salvage therapy for IIRC D/E eyes also had no effects on survival.
A total of 14 patients in our cohort received no treatment at all. The abandonment in our study was only related to late onset age, while another study showed the abandonment rate is higher in rural than urban place.[16] In order to improve the outcome of RB patients, the exact causes for treatment abandonment in retinoblastoma need to be closely examined.
Survival rate in our cohort was in consistent with a previous study in Singapore,[17] while much higher than that in low-income countries,[9] and lower than that in high-income countries[18] indicating that survival of RB is strongly related to the economic level. As reported in other studies, advanced clinical stage,[8,9] bilateral RB,[19] high pathological stage,[20] and treatment abandonment[16] were significantly associated with poor outcome, while other studies[9,21] find that late diagnosis and longer lag period are risk factors, too.
Our study had several limitations. First, it was a hospital-based study with a small study sample, so the results may just represent South Western China of this specific time period. Second, it was a retrospective study with all the weakness of this study design, some data in our study were not complete, especially the fundus examination and pathological data, so actually the study sample in some aspects were even smaller which might lack capability to find statistically significant difference if it objectively existed. Third, the follow up time in our cohort is relatively short, so there might be changes in laterality, treatment, recurrence metastases, second malignancies, and survival in the future.
In conclusion, this is a comprehensive study reviewing RB patients in South Western China. Most RB patients were diagnosed at advanced clinical stage, especially for Tibetan patients. Delayed presentation is related to extraocular RB which is a risk factor for poor outcome. Treatment abandonment, bilateral disease, and high risk pathological features are also risk factors for death. Recently, adjuvant chemotherapy was widely used for RB patients, while increased the eye salvage, it had no significant effects on survival of RB patients. A national standard guideline for the use of adjuvant chemotherapy or EBRT to treat RB patients need to be established. Education for parents and general physicians for the early signs of RB such as leukocoria, therapy strategy of RB may promote early diagnosis, improve the compliance and outcome.
Acknowledgments
The authors thank Brenda Gallie for critical reading and comments.
Footnotes
Abbreviations: CNS = central nervous system, EBRT = external beam radiation therapy, IAC = intra-arterial chemotherapy, IIRC = The International Intraocular Retinoblastoma Classification, IVC = intravenous chemotherapy, pTNM = pathological tumor-node-metastasis staging, RB = retinoblastoma.
JG and JZ have contributed equally to this paper.
All authors listed contributed to conception and design, analysis, and interpretation of data.
Ethics approval: Ethics Committee of West China Hospital of Sichuan University.
This study was supported by grants to DC from the National Natural Science Foundation of China (81371022, 81570860).
All authors have no conflicts of interest to disclose.
References
- 1.Dimaras H, Kimani K, Dimba EA, et al. Retinoblastoma. Lancet 2012; 379:1436–1446. [DOI] [PubMed] [Google Scholar]
- 2.Dimaras H, Corson TW, Cobrinik D, et al. Retinoblastoma. Nat Rev Dis Primers 2015; 1:15062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kivelä T. The epidemiological challenge of the most frequent eye cancer: retinoblastoma, an issue of birth and death. Br J Ophthalmol 2009; 93:1129–1131. [DOI] [PubMed] [Google Scholar]
- 4.Linn Murphree A. Intraocular retinoblastoma: the case for a new group classification. Ophthalmol Clin North Am 2005; 18:41–53.viii. [DOI] [PubMed] [Google Scholar]
- 5.Finger P, Harbour J, Murphree A. Springer Science and Business Media, Chapter 52: Retinoblastoma in AJCC Cancer Staging Manual, 7th Edn. (eds S.B. Edge, D.R. Byrd, C.C. Compton, A.G. Fritz, F.L. Greene, A. Trotti). Berlin:2010. [Google Scholar]
- 6.Bai S, Ren R, Shi J, et al. Retinoblastoma in the Beijing Tongren Hospital from 1957 to 2006: clinicopathological findings. Br J Ophthalmol 2011; 95:1072–1076. [DOI] [PubMed] [Google Scholar]
- 7.Subramaniam S, Rahmat J, Rahman NA, et al. Presentation of retinoblastoma patients in Malaysia. Asian Pac J Cancer Prev 2014; 15:7863–7867. [DOI] [PubMed] [Google Scholar]
- 8.Waddell KM, Kagame K, Ndamira A, et al. Clinical features and survival among children with retinoblastoma in Uganda. Br J Ophthalmol 2015; 99:387–390.bjophthalmol-2014-305564. [DOI] [PubMed] [Google Scholar]
- 9.Chawla B, Hasan F, Azad R, et al. Clinical presentation and survival of retinoblastoma in Indian children. Br J Ophthalmol 2016; 100:172–178. [DOI] [PubMed] [Google Scholar]
- 10.Shields CL, Shields JA, Shah P. Retinoblastoma in older children. Ophthalmology 1991; 98:395–399. [DOI] [PubMed] [Google Scholar]
- 11.Taha H, Amer HZ, El-Zomor H, et al. Phthisis bulbi: clinical and pathologic findings in retinoblastoma. Fetal Pediatr Pathol 2015; 34:176–184. [DOI] [PubMed] [Google Scholar]
- 12.Truong B, Green AL, Friedrich P, et al. Ethnic, racial, and socioeconomic disparities in retinoblastoma. JAMA Pediatr 2015; 169:1096–1104. [DOI] [PubMed] [Google Scholar]
- 13.Shields C, Mashayekhi A, Au A, et al. The International Classification of retinoblastoma predicts chemoreduction success. Ophthalmology 2006; 113:2276. [DOI] [PubMed] [Google Scholar]
- 14.Chantada GL, Fandino AC, Guitter MR, et al. Results of a prospective study for the treatment of unilateral retinoblastoma. Pediatr Blood Cancer 2010; 55:60–66. [DOI] [PubMed] [Google Scholar]
- 15.Zhao J, Dimaras H, Massey C, et al. Pre-enucleation chemotherapy for eyes severely affected by retinoblastoma masks risk of tumor extension and increases death from metastasis. J Clin Oncol 2011; 29:845–851. [DOI] [PubMed] [Google Scholar]
- 16.Kumar A, Moulik NR, Mishra RK, et al. Causes, outcome and prevention of abandonment in retinoblastoma in India. Pediatr Blood Cancer 2013; 60:771–775. [DOI] [PubMed] [Google Scholar]
- 17.Aung L, Chan YH, Yeoh EJ, et al. Retinoblastoma: a recent experience at the National University Hospital, Singapore. Ann Acad Med Singapore 2009; 38:693–698. [PubMed] [Google Scholar]
- 18.Canadian RS. National retinoblastoma strategy Canadian guidelines for care: Stratégie thérapeutique du rétinoblastome guide clinique canadien. Can J Ophthalmol 2009; 44:S1. [DOI] [PubMed] [Google Scholar]
- 19.Naseripour M, Nazari H, Bakhtiari P, et al. Retinoblastoma in Iran: outcomes in terms of patients’ survival and globe survival. Br J Ophthalmol 2009; 93:28–32. [DOI] [PubMed] [Google Scholar]
- 20.Yang I, Kuo H, Chen Y, et al. Review of 20 years’ clinical experience with retinoblastomas in southern Taiwan. Chang Gung Med J 2008; 31:484. [PubMed] [Google Scholar]
- 21.Singh A, Shields C, Shields J. Prognostic factors in retinoblastoma. J Pediatr Ophthalmol Strabismus 2000; 37:134. [DOI] [PubMed] [Google Scholar]


