Abstract
Foreign body aspiration (FBA) is a serious medical problem, also in dental practice. The case report describes the case of a patient who for 12 years has suffered from chronic cough as a result of the aspiration of a polymeric silicone resin fragment during a dental procedure. In November 2002, the patient was underwent dental care, and she points out that, when performing dental imprint, she had sensed that something “went down in the throat” but she was immediately reassured by the dentist. After lung CT was performed, the foreign body was identified and removed with benefit to the patient. The knowledge of this case report could be useful for dentists who perform dental impressions, to be aware of the fact that the material used is radiolucent e.g. cannot be seen on plan radiographs and it can be accidentally inhaled by the patient. The knowledge of the case is also important for doctors who come in contact with patients who previously underwent dental treatment, suffering from persistent cough, in the absence of positive radiological signs.
Keywords: Chronic cough, Foreign body aspiration, Medical liability, Differential diagnosis, Guidelines, Case report
1. Introduction
Foreign body aspiration (FBA) is a serious medical problem causing significant morbidity and mortality each year. Although FBA is more common in children, but adult patients are also at risk [1], [2], [3].
In adult patients, aspiration of a FBA is most common after the patient experiences a central neurological lesion due to trauma or degenerative diseases [4]. We describe the case of a patient who has suffered from persistent cough, for a period of 12 years, a situation due to the presence of an endobrochial foreign body consisting of a synthetic fragment of silicone polymer used in dental practice.
2. Case report
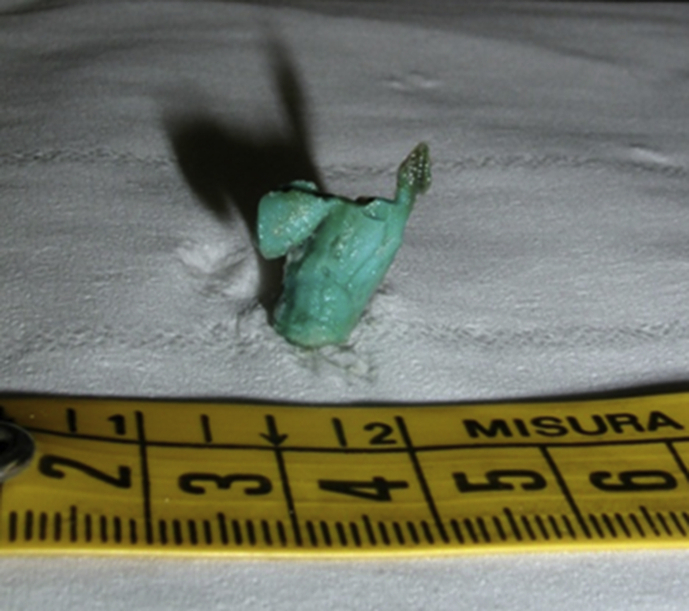
In September 2002 a 54 year old woman undergoing dental care felt, while the dentists was performing impressions, something falling into the gorge and immediately begun to cough. Immediately the dentist reassured the patient that she could not have inhalated anything. The following December, due to the persistent cough, a chest radiograph was ordered but showed no abnormalities. Due to the persistent chronic cough, the dentist prescribes antiinflammatory drugs and antibiotics; that revealed no benefits. In May 2003, the patient underwent a pneumology visit during which spirometry and bronchial responsiveness tests were done. At that time chronic inflammatory lung disease was diagnosed, without any more specific diagnosis. In August 2007, due to the persistence of the cough, an ENT visit occurred and catarrhal pharyngitis was diagnosed and inhaled corticosteroids were prescribed. Despite ICS administration, the cough did not improve. In July 2010, the patient had another pneumology visit and again she underwent chest x-ray, which resulted to be normal. In October 2012 a fiberoptic laryngeal exam did not detect diseases. In December 2012, the patient suffered from pleurisy which was successfully treated with antibiotics, but she still continued to complain of chronic cough. In July 2013 a spirometry was normal. In September 2014, the patient had another ENT visit and she was diagnosed with chronic pharyngitis and was prescribed aerosol; the otolaryngologist prescribed a computed tomography (CT scan). In November 2014, the patient underwent CT scan examination of the chest that detected “at the level of the lower lobe of the right lung (…) a solid formation hypodense of about 1.5 cm, surrounding sleeve bronchus almost to occlude it”. Following the results of the CT scan, a bronchoscopy was performed to remove the foreign body (see Fig. 1, Fig. 2). From the day after the surgery the cough decreased until it disappeared completely in two months. After further research it was discovered that the operator who, in 2002, performed the dental impression and immediately reassured the patient, was actually a fake dentist, and had not graduated.
Fig. 1.
The foreign body extracted with bronchoscopy.
Fig. 2.
The foreign body in the position where it was positioned in the bronchus.
3. Discussion
The case report here presented is of peculiar interest for the wide temporal range between suction and diagnosis, that is twelve years. We have detected few cases in the literature in which there is a so ample time between the event of aspiration of a foreign body and the diagnosis [5], [6], [7], [8], [9], [10], [11], [12], [13]. The discussion about the professional liability undertakes special evidence: a) the fake dentist immediately denied the possibility that the synthetic polymer has been aspirated and did not conduct further investigations; b) the doctors who performed afterward then underestimated the statements and the symptoms of the patient; c) none of the questioned doctors in the course of medical history prescribed a CT scan examination despite the persistent cough referred by the patient. The foreign body inhaled during the dental procedure was trapped in a small bronchus and the lung had created a zone of chronic inflammation that was the cause of the persistent cough. The aspirated foreign body was made of synthetic polymer material, not radiopaque, thus invisible to the chest X-rays that the patient repeatedly underwent. Radiological examinations carried out through CT scan would have immediately revealed the presence of the foreign body and thus permitted an early removal. The symptoms presented by the patient were sine materia, therefore without an anatomical or pathophysiological support who attribute the persistence of symptoms. This difficulty is tackled without reference to good clinical practice and the recommendations issued by international scientific societies published during the wide time interval in which the patient presented cough (2002–2014). The British Thoracic Society in the document “Recommendations for the cough management in adults”, published in 2006 defines chronic cough as a manifestation of over eight weeks and suggests the use of CT scan in the case of negative X-rays and the presence of persistent symptoms. The Task Force of the European Respiratory Society in recommendations issued in 2004 published in the European Respiratory Journal [14], for the management in case of suspicion of foreign body aspiration or when x-rays are negative and there is no evidence of gastroesophageal reflux, it is necessary to perform a bronchoscopy. We believe that the knowledge of this case report is important for health professionals in dentistry as well as those in the other fields who evaluated this patient for chronic cough. It is helpful to know that the silicone material used in the execution of dental impressions may be subject to accidental aspiration without immediate symptoms [15], [16], [17] and that this type of material is not visible to X-rays but only in the most advanced diagnostic techniques, such as CT scan. The case shows that it is mandatory to investigate the clinical situation of a patient who is suspected to have inhaled a foreign body, through CT scan imaging studies or endoscopy. Further, it is important to remember that inhaled materials may be radiolucent and therefore limit the value of chest radiographs in evaluating possible FBA.
Conflicts of interest
None.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
References
- 1.Baharloo F., Veyckemans F., Francis C., Biettlot M.P., Rodenstein D.O. Tracheobronchial foreign bodies: presentation and management in children and adults. Chest. 1999;115:1357–1362. doi: 10.1378/chest.115.5.1357. [DOI] [PubMed] [Google Scholar]
- 2.Hasdiraz L., Bicer C., Bilgin M., Oguzkaya F. Turban pin aspiration: non-asphyxiating tracheobronchial foreign body in young islamic women. Thorac. Cardiovasc. Surg. 2006;54:273–275. doi: 10.1055/s-2006-923954. [DOI] [PubMed] [Google Scholar]
- 3.Boyd M., Chatterjee A., Chiles C., Chin R. Tracheobronchial foreign body aspiration in adults. South. Med. J. 2009;102:171–174. doi: 10.1097/SMJ.0b013e318193c9c8. [DOI] [PubMed] [Google Scholar]
- 4.Gonullu H., Ozturk Y., Akay S., Boncu M., Erkan N. Turban pin: an unusual cause of foreign body aspiration in young islamic adult. Iran. Red. Crescent. Med. J. 2014;16:e2975. doi: 10.5812/ircmj.2975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kam J.C., Doraiswamy V., Dieguez J.F., Dabu J., Cholankeril M., Govind M., Miller R., Adelman M. Foreign body aspiration presenting with asthma-like symptoms. Case Rep. Med. 2013;2013:317104. doi: 10.1155/2013/317104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bain A., Barthos A., Hoffstein V., Batt J. Foreing body aspiration in the adult: presentation and management. Can. Respir. J. 2013;20:e98–e99. doi: 10.1155/2013/754121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen C.H., Lai C.L., Tsai T.T., Lee Y.C., Perng R.P. Foreing body aspiration into the lower air way in Chinese adults. Chest. 1997;112:129–133. doi: 10.1378/chest.112.1.129. [DOI] [PubMed] [Google Scholar]
- 8.Willett L.L., Barney J., Saylors G., Dransfield M. An unusual cause of chronic cough foreign body aspiration. J. Gen. Intern. Med. 2006;21:C1–C3. doi: 10.1111/j.1525-1497.2005.00224.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Quinn K., Rowan S.A., Rendall J. An unusual cause of pneumonia: seen but not heard. BMJ Case. Rep. 2013;29:2013. doi: 10.1136/bcr-2013-008572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Inayama Y., Udaka N., Amano T., Watanuki Y., Odagiri S., Kawano N., Nakatani Y. Fatal aspiration of sardine fry in a patient with lung cancer. J. Forensic Sci. 2000;45:478–482. [PubMed] [Google Scholar]
- 11.Tanner N.T., Gomez M., Silvestri G.A. Denture misadventure: an unusual cause of hemoptysis. J. Bronchol. Interv. Pulmonol. 2009;16:216–218. doi: 10.1097/LBR.0b013e3181aa1fe0. [DOI] [PubMed] [Google Scholar]
- 12.Lebiedz P., Domschke W., Pohle T. An unusual cause of dysphagia. Dtsch. Med. Wochenschr. 2004;129:1065–1068. doi: 10.1055/s-2004-824848. [DOI] [PubMed] [Google Scholar]
- 13.Pasquette R. A persistent cough related to aspiration of a nonradiopaque bone. JAAPA. 2014;27 doi: 10.1097/01.JAA.0000446356.36860.07. [DOI] [PubMed] [Google Scholar]
- 14.Fontana G.A., Sovijarvi A.R.A., Pistolesi M., Chung K.F., Widdicombe J., O'Connell F., Geppetti P., Gronke L., De Jongste J., Belvisi M., Dicpinigaitis P., Fischer A., McGarvey L., Fokkens W.J., Kastelik J., ERS Task Force The diagnosis and management of chronic cough. Eur. Respir. J. 2004;24:481–492. doi: 10.1183/09031936.04.00027804. [DOI] [PubMed] [Google Scholar]
- 15.Baharloo F., Veyckemans F., Francis C., Biettlot M.P., Rodenstein D.O. Tracheobronchial foreign bodies: presentation and management in children and adults. Chest. 1999;115:1357–1362. doi: 10.1378/chest.115.5.1357. [DOI] [PubMed] [Google Scholar]
- 16.Morice A.H., Fontana G.A., Belvisi M.G., Birring S.S., Chung K.F., Dicpinigaitis P.V., Fischer A., McGarvey L., Fokkens W.J., Kastelik J., ERS Task Force ERS guidelines on the assessment of cough. Eur. Respir. J. 2007;29:1256–1276. doi: 10.1183/09031936.00101006. [DOI] [PubMed] [Google Scholar]
- 17.Morice A.H., McGarvey L., Pavord I., on behalf of the British Thoracic Society Cough Guideline Group Recommendations for the management of cough in adults. Thorax. 2006;61:i1–i24. doi: 10.1136/thx.2006.065144. [DOI] [PMC free article] [PubMed] [Google Scholar]