Sinus histiocytosis with massive lymphadenopathy, also known as Rosai-Dorfman disease (RDD), is an uncommon benign histioproliferative disorder with systemic symptoms and lymphadenopathy. Mostly affecting lymph nodes, RDD typically presents as substantial painless bilateral cervical lymphadenopathy associated with fever, leukocytosis, anemia, polyclonal hypergammaglobulinemia, and increased erythrocyte sedimentation rate.1 Extranodal manifestations occur in approximately 43% of patients.2 Common extranodal sites include skin, respiratory tract, orbit, paranasal sinuses, soft tissue and bone, whereas CNS involvement is considered extremely rare. Herein, we describe a unique case of intracranial RDD presenting with multifocal lesions.
Case report.
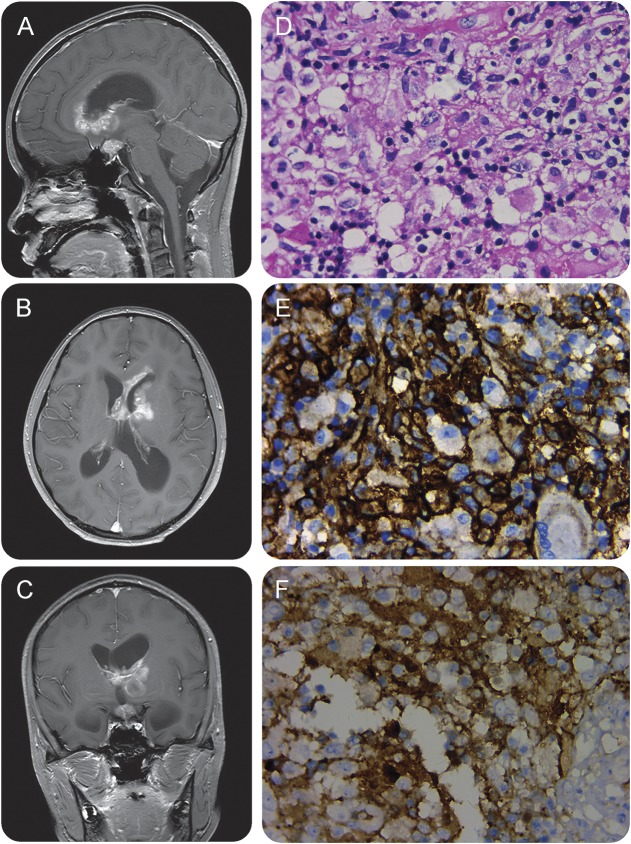
A 13-year-old girl presented with a 2-month history of headaches, nausea, and vomiting. One year before her main complaints, she had experienced excessive urination and extreme thirst for a few months, with no cause found. The patient was alert, orientated, and apyrexial. Her vital signs were normal. Neurologic examination was unremarkable. Brain MRIs with gadolinium showed multifocal enhancing lesions in the bilateral ependymal/subependymal zone and suprasellar cistern with perilesional edema and hydrocephalus (figure, A–C). Repeated CSF analyses revealed elevated pressure and protein levels with negative culture. CT of the chest and the abdomen were normal. She underwent a stereotactic brain biopsy. Further light microscopic examination demonstrated a dense proliferation of mixed inflammatory cells. Small lymphocytes predominated, but scattered large histiocytes and plasma cells were also observed (figure, D). The histiocytes were immunoreactive for CD68 and S-100 protein and were negative for CD1a (figure, E and F). Such findings indicated the histopathologic diagnosis of intracranial RDD.
Figure. MRIs and histopathology of the biopsy specimens.
Sagittal (A), axial (B), and coronal (C) gadolinium-enhanced T1-weighted MRIs demonstrate extensive enhancing extra-axial masses in the bilateral ependymal/subependymal zones and suprasellar region, with perilesional edema and severe obstructive hydrocephalus. Hematoxylin & eosin–stained (D) specimen shows a dense proliferation of mixed inflammatory cells. Small lymphocytes predominate, but scattered large histiocytes and plasma cells are also observed. Histiocytic cells showing CD68 (E) and S-100 (F) immunoreactivity. Magnification 400× (D–F).
Her headache resolved after temporary external ventricular drainage. After the administration of steroids, she had a good response with complete resolution of symptoms. She remained headache-free and experienced no recurrence at 24-month follow-up.
Discussion.
RDD with involvement of the CNS is rare. Intracranial cases account for 75% and spinal canal involvement for 25%.3 In cases of RDD with CNS involvement, the most common imaging findings are dural-based extra-axial enhancing masses, which tend to mimic meningioma in the convexity or the skull base.4 In rare instances, RDD in the brain and spine has been reported to occur intraparenchymally.5 At least 11 cases of sellar/suprasellar region RDD have been reported previously, while ependymal/subependymal zone involved by RDD has not been documented. The patient reported herein is the first description of intracranial RDD involving intraventricular ependymal/subependymal zone as well as suprasellar region. The episode of increased urination and thirst reported in this patient was presumptively related to the suprasellar lesion producing symptoms of pituitary compression and diabetes insipidus. The majority of patients with RDD have a benign course, but in some cases, it can be fatal because of its location, compression, and progression. The extranodal form of RDD should be included as one of differential diagnoses in the list of intracranial space-occupying lesions.
Footnotes
Author contributions: H. Chen collected, analyzed, and interpreted all the clinical and radiologic data, drafted and revised the manuscript for intellectual content. H. Chen takes responsibility for the integrity of the data and the accuracy of the data analysis. H. Zhou collected and interpreted all the histological data, drafted and revised the manuscript for the pathologic content. Z. Song analyzed and interpreted all the clinical and radiologic data, revised the manuscript for intellectual content.
Study funding: This work is supported by a grant from New Xiangya Talents Project of the Third Xiangya Hospital of Central South University (Han Chen).
Disclosure: The authors report no disclosures. Go to Neurology.org/nn for full disclosure forms. The Article Processing Charge was paid by the authors.
References
- 1.Foucar E, Rosai J, Dorfman R. Sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease): review of the entity. Semin Diagn Pathol 1990;7:19–73. [PubMed] [Google Scholar]
- 2.Kidd DP, Revesz T, Miller NR. Rosai-Dorfman disease presenting with widespread intracranial and spinal cord involvement. Neurology 2006;67:1551–1555. [DOI] [PubMed] [Google Scholar]
- 3.Lou X, Chen ZY, Wang FL, et al. . MR findings of Rosai-Dorfman disease in sellar and suprasellar region. Eur J Radiol 2012;81:1231–1237. [DOI] [PubMed] [Google Scholar]
- 4.Raslan OA, Schellingerhout D, Fuller GN, et al. . Rosai-Dorfman disease in neuroradiology: imaging findings in a series of 10 patients. AJR Am J Roentgenol 2011;196:W187–W193. [DOI] [PubMed] [Google Scholar]
- 5.Juric G, Jakic-Razumovic J, Rotim K, et al. . Extranodal sinus histiocytosis (Rosai-Dorfman disease) of the brain parenchyma. Acta Neurochir 2003;145:145–149; discussion 149. [DOI] [PubMed] [Google Scholar]