Highlights
-
•
Primary leiomyosarcomas of the greater omentum are extremely rare tumors.
-
•
It appears that early surgical management is a key factor for the treatment of this disease.
-
•
More cases are needed in literature to define the optimal treatment.
Keywords: Leiomyosarcoma, Greater omentum, Primary tumor, Case report
Abstract
Introduction
Greater omentum leiomyosarcomas are rare tumors with only a few cases reported in literature.
Presentation of case
We report the case of a 68-year-old man who consulted complaining of diffuse abdominal pain without a palpable mass at physical examination. Imaging studies revealed a solid-cystic lesion in the right lower quadrant. Surgical resection was performed and the tumor was diagnosed as a leiomyoscarcoma by histological and immunohistochemical examinations.
Discussion
Surgical resection of all lesions seems to be a reasonable therapeutic approach if resection is feasible. Chemotherapy may be used in selected cases.
Conclusion
More cases are needed to define the best treatment approach of this disease.
1. Introduction
The greater omentum is a double-layered fibroadipose tissue that originates from the greater curvature of the stomach and hangs from there to cover the abdominal hollow viscera, then folding back on itself to join the transverse colon. Its main function is to protect the abdomen from any inflammatory, infectious or traumatic process by isolating the compromised organs from the rest of the abdomen. Tumors of the greater omentum are rare, being malignant tumors even rarer. To date, 23 cases of leiomyosarcoma of the greater omentum have been reported after the first case described by Sanes et al. in 1934 [1]. Here we report the case of a patient with a greater omentum leiomyosarcoma and its clinical management.
2. Presentation of case
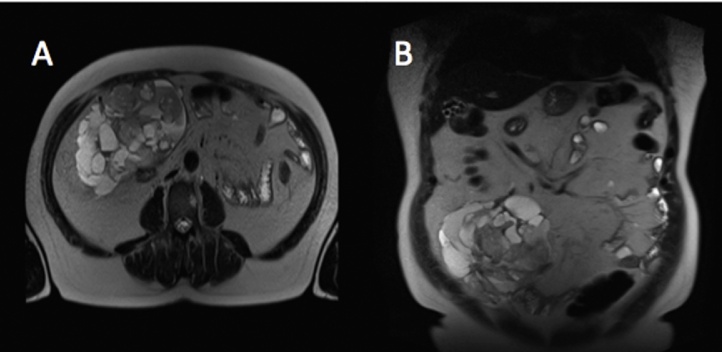
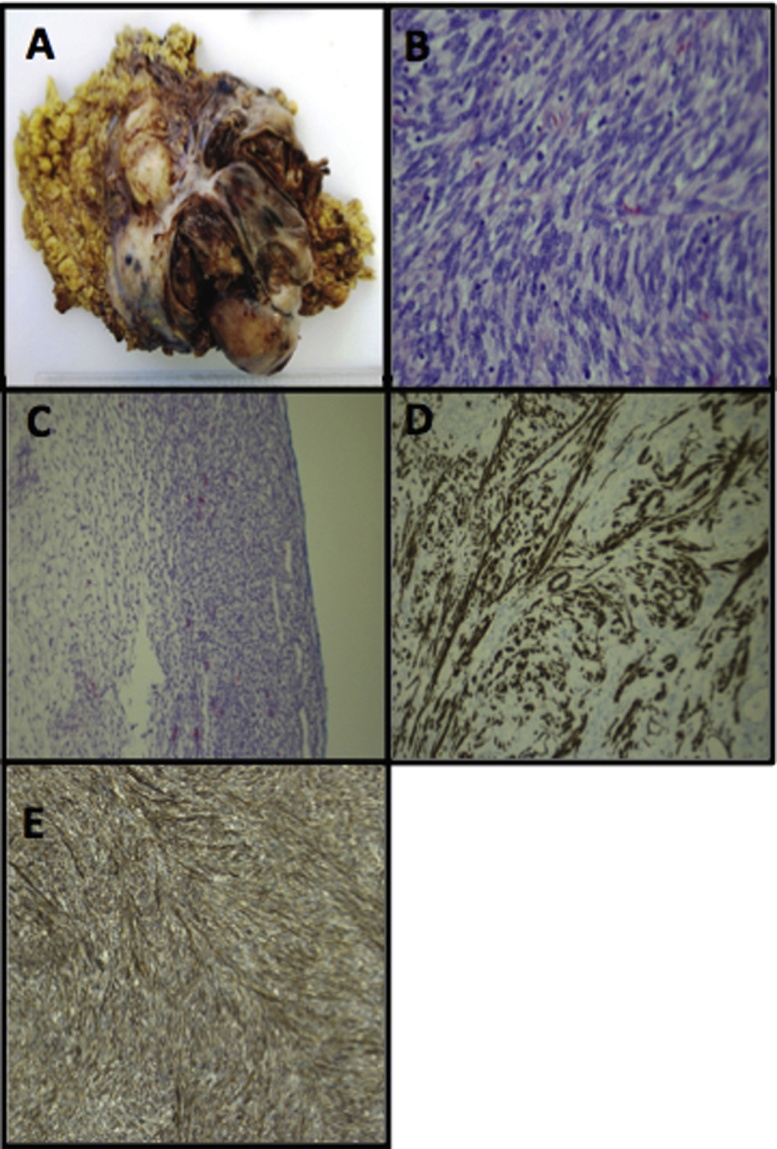
A 68-year-old man without past medical history consulted to the outpatient clinics complaining of one month of diffuse abdominal pain. Thereafter the pain localized to the right lower quadrant. No history of nausea, vomiting, diarrhea, weight loss or fevers was documented. Physical exam revealed right lower quadrant pain, with no peritoneal signs and no evident masses. Abdominal magnetic resonance showed a solid-cystic loculated right lower quadrant mass originating from the omentum (Fig. 1). No signs of intraabdominal dissemination were observed. All laboratory tests were normal as well as upper gastrointestinal endoscopy and colonoscopy. An exploratory laparotomy was performed finding a low volume free hemoperitoneum and a ruptured hemorrhagic mass in the greater omentum. Exploration through the whole abdominal cavity did not reveal peritoneal dissemination. The mass was excised completely with 3 cm margins of normal tissue and sent to pathological study. The procedure lasted one hour and it did not present intraoperative complications. The patient was discharged at postoperative day 4 without any complications related to the surgery. Biopsy revealed a solid and cystic tumor measuring 26 × 17 × 6 cm, weighting 778 g (Fig. 1). Pathological analysis showed long and fusiform cells, with necrosis and hemorrhagic zones and a mitotic index of 22 mitosis in each ten high-power fields. Immunohistochemistry analysis was positive for H-caldesmon, Actin, CD99 and BCL2, and negative for Desmin, CD34, DOG-1, CD117, S-100, EMA and total cytokeratines (Fig. 2). Based on this immunohistochemical pattern, a leiomyosarcoma of the greater omentum was established.
Fig. 1.
Transverse (A) and coronal (B) sections of a T2-weighted magnetic resonance imaging showing a solid-cystic mass in the right lower quadrant originating from de greater omentum.
Fig. 2.
Multiloculated tumor with solid and cystic component and hemorrhagic areas, partially surrounded by adipose tissue (A). Ovoid cells with vesicular nucleus and eosinophilic cytoplasm showing numerous mitosis (H&E, ×40) (B). Moderately cellular area with fusiform cells arranged in a reticular pattern in fibromixoid stroma (H&E, ×4) (C). Immunohistochemistry study showing fusiform cells positive for H-caldesmon (×10) (D). Tumor cells positive for Actin (×10) (E).
Six months after surgery, patient complained of fullness and abdominal pain. Imaging study showed peritoneal recurrence. An exploratory laparotomy was performed in order to evaluate potential peritoneal metastasis resection. Nevertheless, there was extensive peritoneal, bowel and liver compromise making impossible a R0 resection. Patient was discussed in a multidisciplinary team suggesting a palliative chemotherapy consisting of doxorubicin, which was administered for one cycle. Later on, the patient presented respiratory distress and died 10 months after the first surgery.
3. Discussion
Primary malignant tumors of the greater omentum are rare neoplasms in contrary to metastatic tumors originated from the stomach, gallbladder, pancreas, large bowel and ovaries. The embriologic origin of these tumors is variable because of the different tissues that can be found in the omentum, namely vessels, lymphatics and fat. Leiomyosarcomas of the greater omentum are extremely rare, with only few cases reported in literature. Because of its low frequency, little is known about their origin and behavior. Clinically these tumors present at the fifth decade of life[2], but they have been reported in patients ranging from 26 to 85 years old [3]. The aggressive behavior of these tumors makes relapse a common problem and long-term survival is anecdotal [4], [5].
Clinical presenting symptoms are generally non-specific being the most frequent abdominal distension, pain and palpable abdominal mass. In occasions they can present with intra-abdominal hemorrhage [6]. Therefore, to achieve a correct diagnosis, it is important to discard any other tumors in the abdomen since metastatic tumors to the omentum are more common. However, they may also be discovered as an incidental finding in imaging studies performed for other reasons, which may be associated with a better prognosis [7]. Intravenous contrast-enhanced abdomino-pelvic CT scan and magnetic resonance imaging are the best radiological methods for diagnosis, giving accurate information about the origin and tumor characteristics [8]. Usually these lesions have similar characteristics in imaging studies, presenting in most cases as a solid-cystic, multilobulated tumor [9].
Due to its malignant behavior, good prognosis is only achieved by complete excision [10], [11]. It seems that the most important prognostic factor is the presence of metastatic disease at diagnosis, most of them being located at the liver or at other sites in the abdominal cavity. Reported cases demonstrated that 36% of all patients presented with metastatic disease [3]. In these cases, any attempt to resect all neoplastic lesions must be done. In non-resectable disease, some authors have employed different non-standardized chemotherapy schemes obtaining variable results [3], [12]. Multimodality therapy has also been tested to rescue patients with disseminated disease. Koga et al. reported a case of leiomyosarcoma of the greater omentum with liver metastasis, which was successfully treated with resection of the primary mass, transarterial chemoembolization (TACE), partial resection of the liver lesions and microwave coagulation therapy to the remnant liver metastasis achieving at least one year survival [3].
In the case reported here, the initial differential diagnosis was a ruptured primary omental hematoma due to its macroscopic intraoperative characteristics. Pathological report confirmed a primary leiomyosarcoma. We believe that the spontaneous tumor rupture seen in the initial surgery determined peritoneal spreading which altered the long-term prognosis. In this case, we confirm the aggressive behavior of these tumors resembling most of the reported cases published in literature.
4. Conclusion
Leiomyosarcomas of the greater omentum are rare tumors, with few cases reported in literature. Metastatic disease has been found in more than one third of all the reported cases, which gives an idea of the biological behavior and late diagnosis of these tumors. Surgical resection of all lesions seems to be a reasonable therapeutic approach if it is feasible. If the disease is disseminated at the time of diagnosis, multimodality therapy may be used. More cases are needed to increase the experience and to ultimately define the best treatment for this disease.
Conflict of interest
None of the authors declare conflicts of interest.
Sources of funding
No sources of funding to declare.
Consent
Written informed consent was obtained from the patient for the publication of this case report and accompanying images.
Ethical approval
Not applicable.
Author contribution
Alejandro Brañes: study concept and design, information collection, writing the paper.
Nicolás Quezada: study concept and design, information collection, writing the paper.
Fernando Pimentel: study concept and design, information collection, writing the paper
José Valbuena: pathologic analysis.
Caroll Bustamante: pathologic analysis.
Research studies
Not applicable.
Guarantor
Alejandro Brañes.
Nicolás Quezada.
Fernando Pimentel.
References
- 1.Sanes S., Kenny F.E. Primary sarcoma of the great omentum. Am. J. Cancer. 1934;21:795–804. [Google Scholar]
- 2.Ishida H., Ishida J. Primary tumours of the greater omentum. Eur. Radiol. 1988;8(9):1598–1601. doi: 10.1007/s003300050594. [DOI] [PubMed] [Google Scholar]
- 3.Koga T., Kusumoto T., Kakeji Y., Kishikawa K., Maehara Y., Yonemura T., Irie K., Sugimachi K. Leiomyosarcoma of the greater omentum with liver metastasis: report of a case. Surg. Today. 2002;32(5):434–438. doi: 10.1007/s005950200070. [DOI] [PubMed] [Google Scholar]
- 4.Weinberger H.A., Ahmed M.S. Mesenchymal solid tumors of the omentum and mesentery: report of four cases. Surgery. 1977;82(5):754–759. [PubMed] [Google Scholar]
- 5.Tanimura A., Cho T., Nohara M., Yamashita M., Hosokawa Y., Yamamoto H., Uchiyama H. Primary leiomyosarcoma of the omentum. Kurume Med. J. 1980;27(2):101–105. doi: 10.2739/kurumemedj.27.101. [DOI] [PubMed] [Google Scholar]
- 6.Dixon A.Y., Reed J.S., Dow N., Lee S.H. Primary omental leiomyosarcoma masquerading as hemorrhagic ascites. Hum. Pathol. 1984;15(1):233–237. doi: 10.1016/s0046-8177(84)80185-9. [DOI] [PubMed] [Google Scholar]
- 7.Xia C.Y., Cong W.M., Han W.J., Wang B. Primary leiomyosarcoma with multiple nodules arising from the greater omentum. Dig. Liver Dis. 2010;42(11):828–829. doi: 10.1016/j.dld.2010.05.014. [DOI] [PubMed] [Google Scholar]
- 8.Harder T., Koischwitz D., Engel C. Primary tumors of the mesentery and greater omentum. Rofo. 1983;139(3):274–280. doi: 10.1055/s-2008-1055888. [DOI] [PubMed] [Google Scholar]
- 9.Lee J.T., Kim M.J., Yoo H.S., Suh J.H., Jeong H.J. Primary leiomyosarcoma of the greater omentum: CT findings. J. Comput. Assist. Tomogr. 1991;15(1):92–94. doi: 10.1097/00004728-199101000-00013. [DOI] [PubMed] [Google Scholar]
- 10.Mahon D.E., Carp N.Z., Goldhahn R.T., Schmutzler R.C. Primary leiomyosarcoma of the greater omentum: case report and review of the literature. Am. Surg. 1993;59(3):160–163. [PubMed] [Google Scholar]
- 11.Tsurumi H., Okada S., Koshino Y., Oyama M., Higaki H., Shimokawa K., Yamauchi O., Moriwaki H., Muto Y. A case of leiomyoblastoma (epithelioid leiomyosarcoma) of the greater omentum. Gastroenterol. Jpn. 1991;26(3):370–375. doi: 10.1007/BF02781927. [DOI] [PubMed] [Google Scholar]
- 12.Niwa K., Hashimoto M., Hirano S., Mori H., Tamaya T. Primary leiomyosarcoma arising from the greater omentum in a 15-year-old girl. Gynecol. Oncol. 1999;74(2):308–310. doi: 10.1006/gyno.1999.5441. [DOI] [PubMed] [Google Scholar]