Abstract
There is no consensus regarding the effects of deep brain stimulation (DBS) surgery on swallowing outcomes in Parkinson's disease (PD). No prospective studies have compared airway protective outcomes following DBS to the subthalamic nucleus (STN) versus globus pallidus interna (GPi). A recent retrospective study described swallowing outcomes pre- and post-STN vs. GPi DBS in a cohort of 34 patients with PD. The results revealed that the patients who received GPi DBS maintained their swallowing function post-DBS, while those in the STN group significantly worsened in swallowing safety. As DBS surgery becomes a common management option in PD it is important to understand the impact of DBS on airway protective outcomes; especially given that aspiration pneumonia is the leading cause of death in this population. We present a case report in which optimizing DBS settings with the goal of improving laryngeal function resulted in immediate improvements to swallowing safety.
Keywords: dysphagia, Parkinson's disease, aspiration, deep brain stimulation surgery, laryngoscopy, swallowing
Introduction
There is no consensus regarding the effects of deep brain stimulation (DBS) surgery on swallowing outcomes in Parkinson's disease (PD). No prospective studies have compared airway protective outcomes following DBS applied to the subthalamic nucleus (STN) versus globus pallidus interna (GPi) [1]. A recent retrospective study described swallowing outcomes pre- and post-STN vs. GPi DBS in a cohort of 34 patients with PD. The results revealed that the patients who received GPi DBS maintained their swallowing function post-DBS, while those in the STN group significantly worsened in swallowing safety [2]. As DBS surgery becomes a common management option in patients with PD it is important to understand the impact of DBS on airway protective outcomes; especially given that aspiration pneumonia is the leading cause of death in this population [3-4].
Aspiration pneumonia is caused by dysfunction in airway protective behaviors; specifically swallowing and cough. These two behaviors share commonalities in terms of their neural control [5], and the larynx serves a critical physiological role for executing a safe swallow as well as generating an effective cough. There is some evidence describing the impact of DBS on laryngeal function in PD, but there are no reports specifically assessing the changes to laryngeal function for airway protection following DBS surgery. We present a case report in which optimizing DBS settings with the goal of improving laryngeal function resulted in immediate improvements to swallowing performance with significant reductions in aspiration.
Case Report
This is the case report of a 62-year old left-handed male with a history of akinetic-rigid type PD diagnosed at the age of 29. At the age of 51, he underwent right STN DBS placement at an outside institution for management of PD symptoms on his dominant side. Although the patient had some acute adverse effects following DBS, he eventually received partial benefit with inconsistent control of tremor, rigidity, and bradykinesia. He presented to the University of Florida Center for Movement Disorders and Neurorestoration (UF CMDNR) for evaluation of further surgical management. The patient underwent complete interdisciplinary work-up at the CMDNR in order to assess DBS candidacy. During the evaluation process, imaging revealed that the right STN DBS lead was suboptimally positioned within the internal capsule (Figure 1). However, the patient was experiencing some mild functional benefit from stimulation at that site (Unified Parkinson's disease rating scale (UPDRS) scores: ON medication/ON right STN stimulation = 29; ON medication/OFF right STN stimulation = 34), and therefore it was decided that contralateral placement of a GPi DBS lead was reasonable to improve control of symptoms. There were no adverse events associated with the left GPi DBS placement. Repeat follow-up evaluations with the UF CMDNR were performed during the first six post-operative months to optimize stimulation parameters and adjust medications (UPDRS scores: ON medication/ON bilateral stimulation = 33; OFF medication/OFF bilateral stimulation = 47).
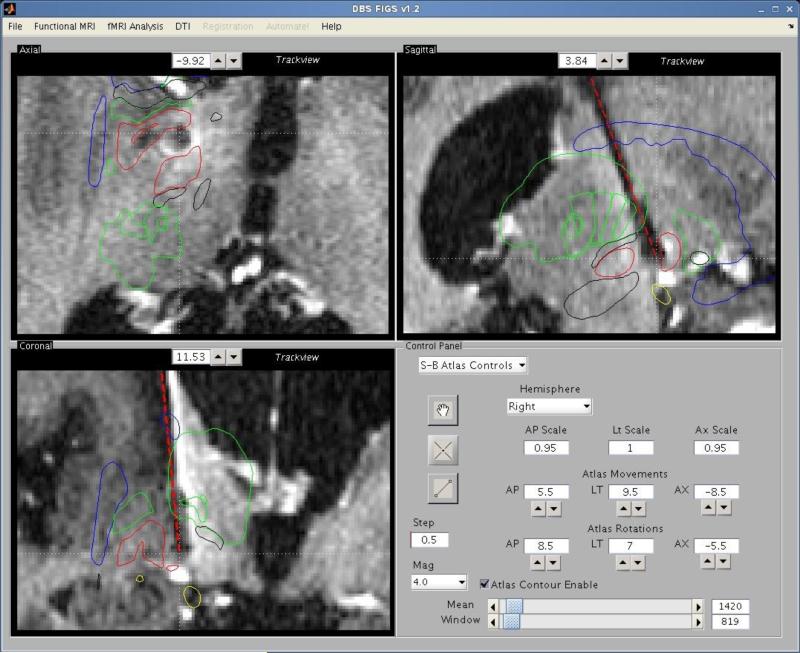
Figure 1.
Suboptimally located right STN DBS lead placed at an outside institution. Postoperative lead location based on the midcommissural point and AC-PC coordinates; anteroposterior- AP 2.29 lateral- LT15.21 Axial- Ax −2.61 AC-PC angle 79 Centerline angle- CT 8.
Post-GPi DBS Swallowing Evaluation
A videofluoroscopic swallowing evaluation performed six months post-GPi DBS (on medication; on stimulation; UPDRS score = 33) revealed a severe sensorimotor oropharyngeal dysphagia. More specifically, the patient's oral stage was impaired with evidence of pre-swallow spill of thin liquid consistencies to the pyriform sinuses, and slow oral transit time. The pharyngeal stage of swallowing was markedly impaired. Most concerning was the repeated and consistent aspiration of thin, nectar-thickened and pudding consistencies without a cough response. Additionally, there was residue in the valleculae and pyriform sinuses, and inadequate duration and extent of cricopharyngeal opening. Aspiration was not reduced with postural adjustments including chin tuck maneuver.
Post-GPi DBS Laryngoscopic Evaluations
Laryngoscopic evaluations were completed in order to assess laryngeal structure and function and determine its contribution to airway protective dysfunction. A flexible nasopharyngoscope was passed transnasally to the level of the oropharynx, providing panoramic visualization of the pharynx and larynx during phonatory and swallowing tasks. All examinations were performed without topical anesthetic agents which might influence swallowing function. Given the knowledge that the right STN DBS lead was suboptimally placed, laryngeal evaluations were completed in four DBS conditions. The four conditions were: 1) ON bilaterally, OFF bilaterally, ON right STN/OFF left GPi, and ON left GPi/OFF right STN. With bilateral DBS stimulation in the ON condition the patient exhibited: 1) markedly asymmetric adduction of the arytenoids and 2) adventitious arytenoid movements during rest. With the suboptimally placed right STN DBS lead ON and the left GPi DBS lead OFF the patient continued to exhibit: 1) markedly asymmetric adduction of the arytenoids and 2) adventitious arytenoid movements during rest. With the right STN DBS lead OFF and the left GPi DBS lead ON the patient exhibited symmetrical arytenoid movements. Finally, with both leads in the OFF condition the patient exhibited symmetrical arytenoid movements, but there was the presence of an epiglottic tremor. A 30-60 minute wash-out period was provided between laryngoscopic evaluations. Results of the laryngoscopic evaluations are summarized and visualized in Video 1.
Post – DBS Optimization Evaluations
Given the marked improvement to laryngeal motor function with the suboptimally placed right STN lead in the OFF condition, the results of the laryngoscopic evaluation were discussed with the Neurology team and it was decided that DBS re-programming would be completed with laryngeal outcomes as the primary indicator of success. Laryngoscopic evaluations were completed as part of the DBS optimization process in conjunction with the DBS nurse practitioner. An optimal setting which mitigated laryngeal adverse events while maintaining adequate control of tremor and bradykinesia was determined (see video – post-DBS optimization). Optimized DBS parameters for the right STN lead were set to 135 Hz frequency, 90 (ms) impulse width, 3.8 V, and impedance 1229. The left GPi lead was adjusted to 135 Hz frequency, 120 (ms) impulse width, 2.9 V, and impedance 692. The UPDRS score ON medication and with the optimized DBS settings ON was 35. Repeat videofluorosopic evaluations were then completed to identify whether improved laryngeal function translated to enhanced swallowing safety. Repeat videofluoroscopic evaluation of swallowing at the modified DBS program, revealed marked and immediate improvement to swallowing safety as compared with the previous DBS settings. While the patient still aspirated small amounts of thin liquid during the presentation of the large sequential swallowing task, there was no aspiration of nectar or pudding-thick consistencies. Additionally, voluntary cough was more effective for clearance of aspirate material from the airway.
Discussion
In summary, although the patient continued to have airway protective deficits post-DBS optimization, there were marked, immediate, and clinically significant improvements associated with optimizing DBS settings based on laryngeal and associated swallowing function. The immediate changes to airway protection translated not only to potentially improved health outcomes, but an enhanced ability to participate in behavioral therapy targeting swallowing and cough deficits. Given the growing body of evidence demonstrating similar motoric symptom control and long-term benefits of both GPi and STN DBS, it is important to consider the impact of lead location and associated DBS settings on airway protective function. Patients post-DBS should receive interdisciplinary care to optimize long-term motor outcomes, including airway protection.
Supplementary Material
Highlights.
Pneumonia secondary to airway protective deficits is a leading cause of death in PD
There is limited research regarding the impact of DBS surgery on airway protection
Optimizing DBS settings in a PD patient resulted in improved airway protection
It is important to consider the impact of DBS settings on airway protection in PD
Acknowledgments
This work was funded in part by an NIH (NCATS) CTSA through the University of Florida (UL1TR000064 and KL2TR000065).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Financial Disclosures: The authors report no specific conflicts of interest related to this study.
References
- 1.Troche MS, Brandimore AE, Foote KD, et al. Swallowing and Deep Brain Stimulation in Parkinson's disease: A systematic review. Parkinsonism Relat Disord. 2013;19:783–8. doi: 10.1016/j.parkreldis.2013.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Troche MS, Brandimore AE, Foote KD, et al. Swallowing outcomes following unilateral STN vs. GPi surgery: A retrospective analysis. Dysphagia. 2014;29:425–31. doi: 10.1007/s00455-014-9522-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fall PA, Saleh A, Fredrickson M, et al. Survival time, mortality, and cause of death in elderly patients with Parkinson's disease: A 9-year follow-up. Mov Disord. 2003;18:1312–6. doi: 10.1002/mds.10537. [DOI] [PubMed] [Google Scholar]
- 4.Fernandez HH, Lapane KL. Predictors of mortality among nursing home residents with a diagnosis of Parkinson's disease. Med Sci Monit. 2002;8:CR241–6. [PubMed] [Google Scholar]
- 5.Troche MS, Brandimore AE, Godoy J, et al. A framework for understanding shared substrates of airway protection. J Appl Oral Sci. 2014;22:251–60. doi: 10.1590/1678-775720140132. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.